Abstract
Purpose
Pediatric trigger thumb is a common condition resulting in referral from primary care to specialty care. Access to pediatric hand specialty care is a complex issue influenced by a multitude of social factors, including socioeconomic status. The aim of this study is to investigate the relationship between area deprivation and the time from primary care referral to presentation to specialty care for pediatric trigger thumb.
Methods
Participants were pediatric patients with trigger thumb. Patient-level area deprivation was reflected by the area deprivation index (ADI). We analyzed the relationship of the ADI to patient demographics (age and sex), trigger thumb treatment (surgical vs nonsurgical), and time to initial hand surgical visit after referral and surgical management when indicated.
Results
Among 163 patients with trigger thumb, 52% were men. Mean age at referral for trigger thumb was 2.9 ± 1.7 years. Mean ADI for patients diagnosed with trigger thumb was 57.8 ± 23.4 for the 2018 data set and 57.3 ± 23.6 for the 2021 data set, on a scale of 1 (low) to 100 (high). The median time from referral from primary care to presentation to orthopedic care for trigger thumb was 34 days. Upon presentation to treating hand surgeon, 118 patients (72.4%) underwent surgical release. We found no difference in ADI between men and women nor between patients treated operatively or with nonsurgical management. We found a weak positive correlation between ADI and time from initial referral to presentation to the treating hand surgeon. There was no correlation between ADI and time from initial hand surgical evaluation and surgical management in patients indicated for surgery.
Conclusions
Pediatric trigger thumb patients from areas with higher ADI have a slightly longer delay between initial referral and their initial visit with an orthopedic hand specialist. Although we found a delay in initial evaluation by the treating hand surgeon in patients with higher ADI, ADI status was not different between patients managed with surgical and nonsurgical treatment nor between men and women.
Clinical relevance
Neighborhood ADI weakly correlated with increased time from referral to accessing specialty orthopedic care for trigger thumb. This may suggest a need for more equitable access to specialty care for patients with pediatric trigger thumb from high ADI areas.
Key words: Pediatric orthopedic surgery, Social determinants of health, Trigger thumb
Timely access to pediatric specialists is a multifaceted issue in the American health care system. Pediatric patients are commonly managed by a sole pediatrician and seek referrals to other specialists. Specialty care is limited by insurance status, provider availability, proximity to specialty care, parent health literacy, and other factors that impede access to care at baseline.1,2 Emerging evidence in the field of public health and medicine suggests that socioeconomic status is a strong correlate to access to care, follow-up appointments, and ultimately patient outcomes.
The area deprivation index (ADI) is a quantitative metric for socioeconomic status. Neighborhood deprivation incorporates factors for income, education, employment, and housing quality.3 Area deprivation index has been used in hand surgery, oncology, primary care, and other specialties to investigate the relationship between the social determinants of health and patient outcomes.4, 5, 6 In prior orthopedics research, increased neighborhood deprivation has been associated with a longer time to seek specialized care following anterior cruciate ligament injury and undergo surgery following injury, as well as disparities in time to surgery for distal radius fracture.7,8
Within the field of pediatric orthopedics, there are disparities in patients seeking specialty care.2,9 Pediatric trigger digit is one of the most common, nontraumatic pediatric hand surgery indications. Incidence of pediatric trigger thumb is between 1 and 3 in 1,000 children.10 Patients typically are referred from their primary care provider for specialist intervention. The aim of this study was to investigate the relationship between the ADI national percentile ranking and the time from primary care referral to presentation for specialty care for pediatric trigger thumb as well as the influence of ADI and patient demographics on surgical versus nonsurgical management.
Materials and Methods
After approval from the institutional review board, an International Classification of Diseases, Ninth Revision/International Classification of Diseases, Tenth Revision query was performed for the diagnosis of a trigger thumb using our institution’s electronic medical record system. Included codes were M65.30–M65.352. Inclusion criteria were the following: (1) patient diagnosed under one of the included International Classification of Diseases, Ninth Revision/International Classification of Diseases, Tenth Revision codes and were determined to have a trigger thumb after chart review, (2) patient younger than 18 years of age, (3) patient evaluated and treated by one of the two fellowship-trained orthopedic hand and upper-extremity surgeons between January 1, 2000, and August 31, 2021, and (4) patient had a record of current house address at the time of visit. Patients with no record of a provider referral to hand surgery were excluded. Patients with addresses that the United States Postal Service lists as group quarters were unable to receive an ADI score from the database and were excluded as these regions are unable to be quantitatively compared with the remainder of the data set. After calculating the time between initial referral and presentation to the treating hand surgeon as well as the time from initial hand surgery evaluation and surgical management (for patients undergoing surgery), outliers from each data set were removed according to Grubb’s test using a P value of < .05.
Social deprivation in the patient’s home area was reported using the ADI. Area deprivation index is a validated composite measure that includes factors for income, education, employment, and housing quality. Scores for neighborhoods ranged between 1 and 100, where higher scores indicate greater neighborhood socioeconomic deprivation.3 We calculated the ADI for each patient using the 9-digit zip code from the home address. The publicly available 2018 and 2021 national ADI percentile rankings were obtained for each patient. The 2018 ADI data set was chosen for the primary analysis, given that it more closely represents the population at the time of referral (mean: 2.8- vs 4.2-year difference, respectively).
To determine whether ADI influences time to care, we analyzed the relationship between ADI and the time between referral and presentation to the treating orthopedic hand surgeon and the time from initial office visit to surgical management for patients undergoing surgical treatment. Additionally, we investigated whether ADI, time between referral and presentation, and patient age at referral were different between surgical and nonsurgical treatment groups. Finally, we investigated the role of age and sex on the time between referral and presentation to the treating hand surgeon.
Statistics were conducted using GraphPad Prism 7.0. Correlations between continuous variables were conducted using Spearman’s rank correlation coefficient as well as linear regression. Differences between means (ADI, age, and times) were compared using two-tailed Mann-Whitney U tests. A P value < .05 was determined to be significant. Correlation coefficients were graded by the following scale: 0 < |R| < 0.1 = no correlation, 0.1 ≤ |R| < 0.3 = poor correlation, 0.3 ≤ |R| < 0.6 = fair correlation, 0.6 ≤ |R| < 0.8 = moderate correlation, 0.8 ≤ |R| < 1.0 = very strong correlation, and |R| = 0.8 = perfect correlation.
Results
Across the study period, 388 patients who presented for evaluation of a trigger thumb to one of the two hand surgeons at our institution between January 2000 and August 2021 were identified. A total of 163 patients with trigger thumb (52% men, all unilateral; Table 1) met the inclusion criteria and were reviewed in the study. Mean number of days from referral to presentation for trigger thumb was 34 days. Patient ages at referral to orthopedic specialty care ranged from 1 month to 9 years (mean = 2.9 years, SD = 1.7 years), and ages upon presentation to the treating hand surgeon ranged from 2.5 months to 9 years (mean = 3.0 years, SD = 1.7 years). Area deprivation index scores from the 2018 data set had a range of 4 to 99 (mean = 57.8, SD = 23.4) and from the 2021 data set had a range of 4 to 99 (mean = 57.3, SD = 23.6). The mean absolute difference in ADI between the 2018 and 2021 data sets was 4.5.
Table 1.
Demographic Characteristics of Included Patients
| Total Patients: n | 163 |
| Male: n (%) | 85 (52%) |
| Bilateral: n | 0 |
| Days between referral and presentation: mean | 34 |
| Age at referral, y: mean (SD) | 2.9 (1.7) |
| Age at presentation, y: mean (SD) | 3.0 (1.7) |
| Area deprivation index (ADI): mean (SD) | |
| 2018 Data set: mean (SD) | 57.8 (23.5) |
| 2021 Data set: mean (SD) | 57.3 (23.6) |
| Patient primary treatment | |
| Surgical: n (%) | 118 (72.4%) |
| Nonsurgical: n (%) | 45 (27.6%) |
| Surgical complications: n (%) | 9 (7.6%) |
| Contracture/stiffness | 6 |
| Suture abscess | 2 |
| Postoperative respiratory distress | 1 |
| Nonsurgical treatment | |
| Observation: n (%) | 33 (73.3%) |
| Splinting: n (%) | 12 (26.7%) |
Upon presentation to the treating hand surgeon, 118 patients (72.4%) underwent surgical release, whereas 45 patients (27.6%) underwent nonsurgical treatment. For operatively treated patients, there were nine complications (7.6%) including six instances of interphalangeal joint stiffness or flexion contracture, two suture abscesses, and one patient who was admitted for postoperative respiratory distress that required cardiopulmonary resuscitation. The reoperation rate was 0%. For nonoperatively treated patients, 33 (73.3%) were treated with observation and 12 (26.7%) were treated with splinting.
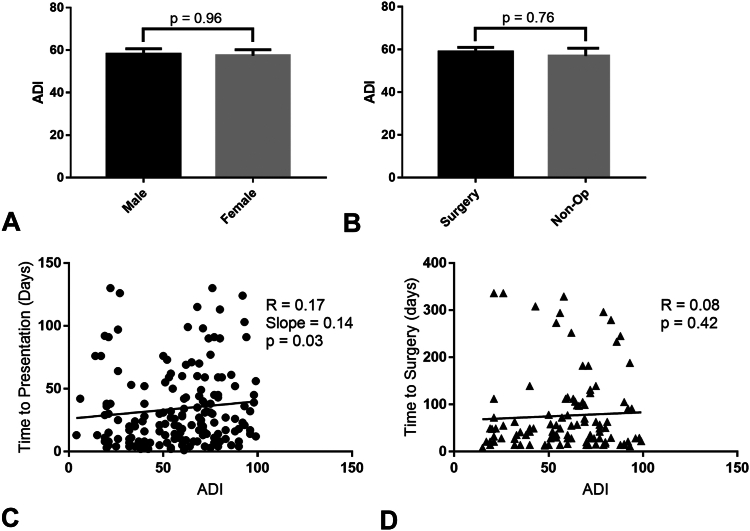
We found no difference in ADI between men and women (Fig. 1A). Similarly, patients treated with surgical and nonsurgical management had equivalent ADIs (Fig. 1B). We found a notable poor positive correlation between ADI and time from initial referral to presentation to the treating hand surgeon (Fig. 1C). There was no correlation between ADI and time from initial hand surgical evaluation and surgical management in patients indicated for surgery (Fig. 1D).
Figure 1.
Influence of area deprivation index (ADI) on the timing of care and relationship to patient demographics in patients with pediatric trigger thumb. Area deprivation index is reported as a function of patient sex A and nonsurgical versus surgical treatment for trigger thumb B. Area deprivation index exhibits a positive correlation with time to initial hand surgical evaluation after referral C, whereas no correlation is observed with regards to timing to surgical management D. Spearman correlation coefficient (R) and P values are reported, with a significance level of P < .05. For significant correlations, the linear slope is reported.
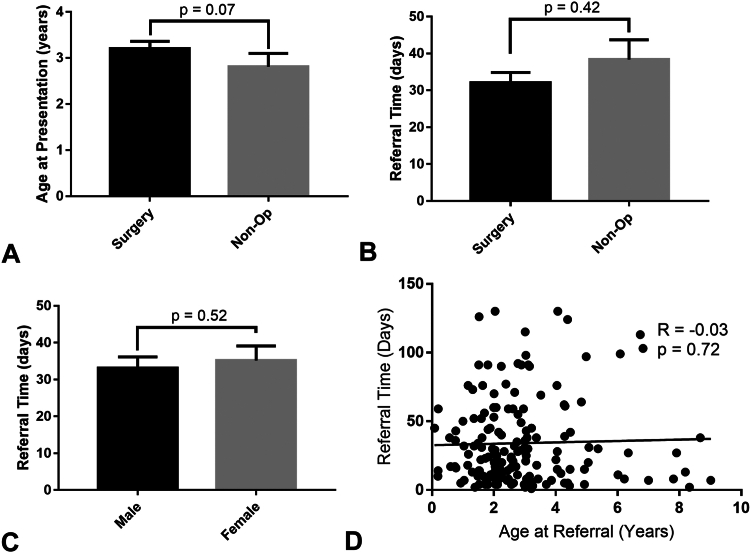
Patients treated with nonsurgical management tended to be younger, but this was not statistically significant (Fig. 2A, P = .07). There was no considerable difference in time from initial referral to presentation in patients treated with surgical or nonsurgical management (Fig. 2B). There was no influence of sex (Fig. 2C) or patient age at referral (Fig. 2D) on time from referral to presentation.
Figure 2.
Influence of referral time on patient age and sex as well as surgical versus nonsurgical management. There is a trend to significantly younger patients observed in the nonoperatively managed group A. No difference is observed in referral time between operatively and nonoperatively managed patients B, male and female patients C, nor any significant correlation between referral time and patient age at initial referral D. Spearman correlation coefficient (R) and P values are reported, with a significance level of P < .05.
Discussion
This study investigated the time between referral and presentation to orthopedic specialty care for patients with pediatric trigger thumb. This study is the first to examine the relationship between neighborhood deprivation status and time to orthopedic specialty care. We found that in patients with a higher ADI (more deprivation), there is a statistically significant positive correlation between ADI and time from initial referral to presentation to the treating hand surgeon. This correlation was found to be poor in nature (R = 0.17, P = .03), which reflects the large range of days after referral until initial patient presentation. Although there was found to be a delay in initial evaluation by the treating hand surgeon in patients with higher ADI, ADI status was not different between patients managed with surgical and nonsurgical treatment nor between men and women. The former suggests that once patients are evaluated by the treating hand surgeon, their neighborhood deprivation does not influence their treatment trajectory. This is further reflected by the fact that we saw no correlation between ADI and time between initial hand surgical evaluation and surgical treatment in patients indicated for surgery (R = 0.08, P = .42).
Although there was a trend for younger patients to receive nonsurgical care, this did not reach statistical significance. There was no difference in referral time between patients managed with surgical and nonsurgical management. Similarly, there was no influence of sex nor age at the initial referral on time to presentation to the treating hand surgeon’s office. These data suggest that neighborhood deprivation plays a more important role in delay to care for pediatric trigger thumb than patient age or sex.
In the past, individual factors like insurance status or mean income have been used as markers for access to specialty orthopedic care, but these factors alone may not capture the full complexity of a patient’s access to specialty orthopedic care.11,12 Recent evidence suggests that ADI is a different marker that can be used to quantify a patient’s socioeconomic status. The ADI algorithm is built using factor analysis and principal components13 and accounts for 17 different socioeconomic factors including income, education, employment, and housing quality. It is an easily accessible online resource that quantifies a patient’s level of deprivation in relation to others at a national level; hence, it can be reliably compared across studies. By using a large scale (1–100), the ADI is able to precisely portray an individual’s socioeconomic environment.3
Relatively few studies have investigated the relationship between individual socioeconomic factors and access to orthopedic care. Ayoade and Fowler14 found that a pediatric patient who has Medicaid coverage is less likely to obtain an orthopedic appointment for trigger thumb than patients with private insurance who have the same diagnosis. Additionally, Montgomery et al15 found that patients who were non-White, resided in zip codes with the lowest median income (< $42,999 annually), and were treated in metropolitan areas were more likely to receive nonsurgical treatments for supracondylar humerus fractures. They also found that women with a femoral shaft fracture were less likely to be treated with open reduction and internal fixation versus intramedullary fixation.
Other orthopedic studies using ADI did find a correlation between ADI and their outcome of interest,7,8 which supports the findings in this study that pediatric trigger thumb patients with a higher ADI have a longer delay between initial referral and their initial visit with a hand specialist. This delay may result from several factors, including the lack of treatment algorithms by the primary care pediatricians for the referral process. Moreover, it should be noted that this study was performed at a major tertiary center with a large catchment area, so patients with more socioeconomic barriers to care may have difficulty traveling several hours from their home for initial specialist evaluation.
This study has several limitations. First, the age at initial presentation to primary care was not reliably recorded. Many patients initially saw providers outside of the study health system that are not available in our electronic medical record. As such, there may be additional delays from the initial primary care evaluation course that are not captured by purely analyzing the time from referral to hand specialist presentation. Second, the study is limited by the availability of the neighborhood ADI data. In this study, we analyzed publicly available ADI data sets for the years 2018 and 2021. Although there was only a mean difference of 4.5 in ADI score for each patient across this time span, patient enrollment took place over a longer timeframe. If further ADI sets were available for use, using an ADI set for each patient according to their year of referral would be more accurate. However, given the small mean difference observed between these two collected sets, we believe that this would not greatly impact the conclusions of this study. Finally, this study does not directly analyze other barriers to care such as health insurance, travel distance, and parental education level. Herein, we use the ADI score as a corollary for socioeconomic impediments to care, which is influenced by many of these parameters. Direct analysis of all these factors is beyond the scope of this study.
In conclusion, we found a significant although quite weak positive correlation between socioeconomic hardship and delay in specialist evaluation for pediatric trigger thumb. It is hoped that this awareness will motivate outreach initiatives to ensure timely care for all patients.
Disclaimer
Given his role as Editor-in-Chief of The Journal of Hand Surgery Global Online, Dr. Fowler had no involvement in the peer-review of this article and has no access to information regarding its peer-review. Full responsibility for the editorial process for this article was delegated to Aviram M. Giladi, MD, MS.
Conflicts of Interest
No benefits in any form have been received or will be received related directly to this article.
References
- 1.Skinner A.C., Mayer M.L. Effects of insurance status on children’s access to specialty care: a systematic review of the literature. BMC Health Serv Res. 2007;7(1):194. doi: 10.1186/1472-6963-7-194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mayer M.L., Skinner A.C., Slifkin R.T., National Survey of Children With Special Health Care Needs Unmet need for routine and specialty care: data from the national survey of children with special health care needs. Pediatrics. 2004;113(2):e109–e115. doi: 10.1542/peds.113.2.e109. [DOI] [PubMed] [Google Scholar]
- 3.Kind A.J.H., Buckingham W.R. Making neighborhood-disadvantage metrics accessible - the neighborhood atlas. N Engl J Med. 2018;378(26):2456–2458. doi: 10.1056/NEJMp1802313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stephens A.R., Tyser A.R., Kazmers N.H. The impact of social deprivation on orthopaedic outpatient satisfaction using the press ganey outpatient medical practice survey. J Am Acad Orthop Surg. 2020;28(24):e1111–e1120. doi: 10.5435/JAAOS-D-19-00852. [DOI] [PubMed] [Google Scholar]
- 5.Rosenzweig M.Q., Althouse A.D., Sabik L., et al. The association between area deprivation index and patient-reported outcomes in patients with advanced cancer. Health Equity. 2021;5(1):8–16. doi: 10.1089/heq.2020.0037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hu J., Kind A.J.H., Nerenz D. Area deprivation index predicts readmission risk at an urban teaching hospital. Am J Med Qual. 2018;33(5):493–501. doi: 10.1177/1062860617753063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cherelstein R., Kuenze C., Curley A., et al. Paper 30: lower socioeconomic status adversely affects timing of care and rate of re-injury following anterior cruciate ligament reconstruction. Orthop J Sports Med. 2023;11(7 suppl3) [Google Scholar]
- 8.Rahman R., Xu A.L., Dhanjani S.A., et al. Does time to imaging and surgery for distal radius fractures vary based on geographic socioeconomic disadvantage? HAND (N Y) 2022;17(1_suppl):95S–102S. doi: 10.1177/15589447221075669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arant K.R., Modest J.M., Gil J.A., Cruz A.I., Jr. What’s new in pediatric orthopaedic health care disparities? J Pediatr Orthop. 2022;42(9):e954–e959. doi: 10.1097/BPO.0000000000002224. [DOI] [PubMed] [Google Scholar]
- 10.Bauer A.S., Bae D.S. Pediatric trigger digits. J Hand Surg Am. 2015;40(11):2304–2309. doi: 10.1016/j.jhsa.2015.04.041. [DOI] [PubMed] [Google Scholar]
- 11.Gatto A.P., Feeley B.T., Lansdown D.A. Low socioeconomic status worsens access to care and outcomes for rotator cuff repair: a scoping review. JSES Rev Rep Tech. 2021;2(1):26–34. doi: 10.1016/j.xrrt.2021.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Segal D.N., Grabel Z.J., Shi W.J., Gottschalk M.B., Boden S.D. The impact of insurance coverage on access to orthopedic spine care. J Spine Surg. 2018;4(2):260–263. doi: 10.21037/jss.2018.05.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Singh G.K. Area deprivation and widening inequalities in US mortality, 1969–1998. Am J Public Health. 2003;93(7):1137–1143. doi: 10.2105/ajph.93.7.1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ayoade O.F., Fowler J.R. Effect of insurance type on access to orthopedic care for pediatric trigger thumb. J Hand Surg Am. 2020;45(9):881.e1–881.e5. doi: 10.1016/j.jhsa.2020.03.003. [DOI] [PubMed] [Google Scholar]
- 15.Montgomery B.K., Joseph G., Segovia N., et al. The influence of race, income, and sex on treatment and complications of common pediatric orthopedic fractures. Orthopedics. 2023;46(3):e156–e160. doi: 10.3928/01477447-20230104-06. [DOI] [PubMed] [Google Scholar]