Abstract
Tumoral calcinosis (TC) is a rare condition defined by the accumulation of calcium salts in soft tissues surrounding joints, most commonly large joints. Chronic joint inflammation in the setting of local hyperphosphatemia leads to interruption and dysfunction of tissue repair and generates breakdown products that subsequently calcify and accumulate. We present a case of a 42-year-old man with a history of end-stage renal disease on dialysis presenting to the clinic with a painless digital mass of his right long finger at the proximal interphalangeal joint. Our initial impression was a splinter abscess based on presentation and patient history. Although our patient’s presentation of traumatic, painless TC of the hand secondary to end-stage renal disease is rare, the pathogenic mechanisms behind TC support this presentation. The authors recommend including TC within the differential of presentations similar to that of chronic abscess or giant cell tumor, especially when their medical history includes end-stage renal disease.
Key words: Calcinosis, Finger abscess, Finger infection, Finger mass, Tumoral calcinosis
Tumoral calcinosis (TC) is a rare condition marked by the accumulation of calcium salts in soft tissues surrounding joints, first described in 1943.1 It most commonly presents in the periarticular spaces of larger joints, such as that of the hip, shoulder, and elbow.2 TC can be divided into two distinct forms, primary and secondary, based on the etiology of excess calcium deposition.3 The primary idiopathic form is characterized by normocalcemia and is further differentiated according to phosphorus levels. Normophosphatemic TC is commonly associated with solitary lesions and SAMD9 gene mutations. Hyperphosphatemic TC has been shown to have a familial etiology based on mutations in the GalNac transferase 3 gene (GALNT3) and KLOTHO that lead to reduced phosphate excretion.4 In contrast, secondary TC is caused by hypercalcemic conditions, such as chronic renal failure, hyperparathyroidism, and hypervitaminosis D.5
In all forms of TC, the pathogenesis is believed to be largely influenced by the accumulation of calcium phosphate product with hyperphosphatemia being the proposed driving factor. In primary and secondary hyperphosphatemic patients, the laboratory abnormality is derived from previously mentioned genetic mutations and secondary hyperparathyroidism, respectively. In contrast, patients with normophosphatemic TC are proposed to still show hyperphosphatemia transiently at the local tissue level from trauma.2 In this state, chronic inflammation can lead to hemorrhages in the periarticular tissue.6 The initiated foamy histiocytic response leads to interference with the reparative process of neobursae formation and eventual breakdown of histiocytic products preventing formation of functional bursae and bone. The resulting loculi are then filled with calcified debris, leading to bone formation and subsequent fibrosis surrounding the lesion.7
Case Report
We present a case of a 42-year-old man with a history of end-stage renal disease (ESRD) on dialysis presenting to the clinic with a digital mass of his right long finger at the proximal interphalangeal joint (Fig. 1). The patient reported having sustained a splinter in the finger approximately 3 months prior to presentation. He had been unable to remove it and thereafter developed what he thoughts was an abscess. Our initial impression was a splinter abscess. He described it as nonpainful and had no functional deficits or loss of sensation. Due to the fluctuant appearance of the lesion, a bedside incision and drainage was performed in the clinic. We encountered a multiloculated, hypervascular mass with pockets of purulent debris, but a majority of the tissue was spongy with areas of calcification (Fig. 2). At that time, cultures and tissue were collected for pathology, which resulted in sterile abscess and multinucleated giant cells with acute inflammation, respectively. Wound cultures showed no growth. The pathology specimen was described as skin with dermal necrosis and calcifications surrounded by multinucleated giant cell reaction and acute inflammation. Because the mass persisted on repeat examination, the patient was taken to the operating room for complete excision. Intraoperatively, the mass had a brown-yellow appearance similar to a giant cell tumor. The proper digital nerve was found to be involved within the mass as well as the tendon sheath and a portion of the joint capsule. No evidence of the reported splinter was encountered. The lesion was removed en bloc and sent for permanent pathology. Final pathology resulted in the diagnosis of TC. The patient went on to recover uneventfully.
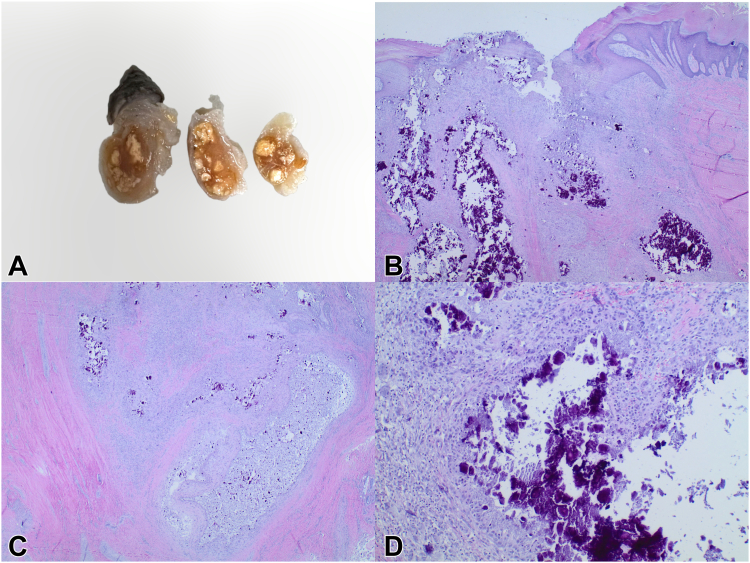
Figure 1.
Gross specimen and histologic appearance. A Gross appearance of excised lesion (top left). B Micrograph of the lesion showing active calcification process adjacent to the skin at ×20 magnification (top right). C Micrograph of the lesion showing fibrosis surrounding and infiltrating calcified debris at ×20 magnification (bottom left). D Micrograph of the lesion showing numerous multinucleated osteoclast-like cells surrounding calcified debris at ×100 magnification (bottom right).
Figure 2.

Clinical photograph of the lesion during incision and drainage procedure.
Discussion
Relatively few case reports exist documenting TC in smaller joints. One example is presented by Kadowaki et al3 describing TC of the left great toe in a normocalcemic, normophosphatemic 67-year-old woman with no history of renal disease or traumatic mechanism. The mass had been present and painless for 3 years prior to the pain symptoms that prompted her presentation to the clinic. Even fewer reports describe the TC of the hand. Viegas et al8 reported a case of atraumatic, painful TC in a normocalcemic, hyperphosphatemic 17-year-old woman presenting with bilateral hand involvement and additional masses in the feet, hips, elbows, and buttocks. These lesions similarly enlarged over the years before becoming painful. Gonzalez et al9 reported a case of atraumatic, painful TC of the flexor sheath of the right little finger in a 34-year-old woman with normal laboratory results, growing slowly over 6 months. Sebesta et al10 described a 52-year-old woman with elevated C-reactive protein and white blood cell count but otherwise normal laboratory results, who presented with a painful, indurated, and swollen mass on the metacarpophalangeal joint of the left index finger.10 In contrast, Amati et al11 presented a case of a 22-year-old woman with painless TC of the right index finger, with normal laboratory results and no renal disease. Bogumill et al12 described another atraumatic, painless case of TC affecting multiple digits across both hands without laboratory abnormalities or renal involvement. Several other case reports exist describing atraumatic TC presentations of the hand with no underlying renal disease or laboratory abnormalities.13, 14, 15, 16 The vast majority of these cases were successfully treated with surgical excision of the mass.
This case report describes a patient with a similar location of TC and treatment but varied presentation. In contrast to patients with atraumatic, painful lesions without underlying renal disease, our patient with ESRD had traumatic onset in the form of a splinter with painless formation of a lesion.8, 9, 10,13, 14, 15, 16 There are minimal reports in the literature regarding secondary TC formation in the joints of the hand in patients with ESRD. One report by Sin et al17 details the case of a 26-year-old woman with ESRD presenting with bilateral TC of the hand involving her left little finger and right thumb. This patient’s case was refractory to surgical excision and other treatments such as hemodialysis and parathyroidectomy. Clinical improvement was only noted after treatment with teriparatide injections. Another report by Hammert and Lindsay18 presented an additional case of suspected TC of the multiple digits of the right hand and wrist in a 51-year-old woman with renal insufficiency requiring hemodialysis. These lesions demonstrated progressive enlargement over a 15-month period, and the excised lesions did not recur.
Although our patient’s presentation of traumatic, painless TC of the hand secondary to ESRD is rare, the pathogenic mechanisms behind TC support this presentation. While our patient had normal calcium levels, it is proposed that local tissue trauma led to a transient hypercalcemic, hyperphosphatemic microenvironment further amplified by ESRD. A splinter that remained in the periarticular tissue likely assumed this role, which is supported by the abscess that developed at the splinter site. Inflammation likely contributed histiocytes and their associated breakdown products to the site, creating the necessary conditions for accumulation of calcium debris and subsequent fibrosis necessary for the formation of TC. While this presentation can be similar to that of a chronic abscess or giant cell tumor, the authors recommend including TC within the differential, especially when their medical history includes ESRD.
Consent for Publication
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Conflicts of Interest
No benefits in any form have been received or will be received related directly to this article.
References
- 1.Inclan A., Leon P., Camejo M.G. Tumoral calcinosis. JAMA. 1943;121(7):490–495. [Google Scholar]
- 2.Fathi I., Sakr M. Review of tumoral calcinosis: a rare clinico-pathological entity. World J Clin Cases. 2014;2(9):409–414. doi: 10.12998/wjcc.v2.i9.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kadowaki M., Naito K., Tobita M., et al. A case of symptomatic tumoral calcinosis on the great toe and review of the literature. Arch Orthop Trauma Surg. 2008;128(6):551–554. doi: 10.1007/s00402-007-0310-2. [DOI] [PubMed] [Google Scholar]
- 4.Smack D., Norton S.A., Fitzpatrick J.E. Proposal for a pathogenesis-based classification of tumoral calcinosis. Int J Dermatol. 1996;35(4):265–271. doi: 10.1111/j.1365-4362.1996.tb02999.x. [DOI] [PubMed] [Google Scholar]
- 5.Polykandriotis E.P., Beutel F.K., Horch R.E., et al. A case of familial tumoral calcinosis in a neonate and review of the literature. Arch Orthop Trauma Surg. 2004;124(8):563–567. doi: 10.1007/s00402-004-0715-0. [DOI] [PubMed] [Google Scholar]
- 6.Thomson J.G. Calcifying collagenolysis (tumoural calcinosis) Brit. J. Radiol. 1966;39(463):526–532. doi: 10.1259/0007-1285-39-463-526. [DOI] [PubMed] [Google Scholar]
- 7.Slavin R.E., Wen J., Kumar D., et al. Familial tumoral calcinosis. A clinical, histopathologic, and ultrastructural study with an analysis of its calcifying process and pathogenesis. Am J Surg Pathol. 1993;17(8):788–802. [PubMed] [Google Scholar]
- 8.Viegas S.F., Evans E.B., Calhoun J., et al. Tumoral calcinosis: a case report and review of the literature. J Hand Surg. 1985;10(5):744–748. doi: 10.1016/s0363-5023(85)80225-2. [DOI] [PubMed] [Google Scholar]
- 9.Gonzalez M., Rettig M., Ayalon O. Extensive tumoral calcinosis of the hand. J Hand Surg. 2021;46(11):1031.e1–1031.e6. doi: 10.1016/j.jhsa.2020.10.030. [DOI] [PubMed] [Google Scholar]
- 10.Sebesta A., Kamineni S., Dumont C.E. Idiopathic tumoral calcinosis of the index finger. Case report. Scand J Plast Reconstr Surg Hand Surg. 2000;34(4):405–408. doi: 10.1080/028443100750059237. [DOI] [PubMed] [Google Scholar]
- 11.Amati C., Pesce V., Armenio A., et al. Tumoral calcinosis of the hand. J Surg Case Rep. 2015;2015(4) doi: 10.1093/jscr/rjv036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bogumill G.P., Lloyd R.J. Tumoral calcinosis in multiple digits: a case report. J Hand Surg Am. 1985;10(5):739–743. doi: 10.1016/s0363-5023(85)80223-9. [DOI] [PubMed] [Google Scholar]
- 13.Kim H.S., Suh J.S., Kim Y.H., et al. Tumoral calcinosis of the hand: three unusual cases with painful swelling of small joints. Arch Pathol Lab Med. 2006;130(4):548–551. doi: 10.5858/2006-130-548-TCOTHT. [DOI] [PubMed] [Google Scholar]
- 14.Xu C., Potter J.A., Carter C.D., et al. Idiopathic tumoral calcinosis in hand: a case report. Eplasty. 2014;14:e28. [PMC free article] [PubMed] [Google Scholar]
- 15.Malik M., Acharya S. Tumoral calcinosis of the fingers. A report of two cases. Int Orthop. 1993;17(5):279–281. doi: 10.1007/BF00181698. [DOI] [PubMed] [Google Scholar]
- 16.Henry G.I., Teven C.M. Case report idiopathic tumoral calcinosis of the nontraumatic thumb. Eplasty. 2012;12:e29. [PMC free article] [PubMed] [Google Scholar]
- 17.Sin H.K., Wong P.N., Lo K.Y., et al. Treatment of severe tumoral calcinosis with teriparatide in a dialysis patient after total parathyroidectomy. Case Rep Nephrol. 2021;2021 doi: 10.1155/2021/6695906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hammert W.C., Lindsay L.R. Tumoral calcinosis–or is it? A case report and review. Hand. 2009;4(2):119–122. doi: 10.1007/s11552-008-9132-0. [DOI] [PMC free article] [PubMed] [Google Scholar]