Abstract
Background
Understanding the epidemiological information of a certain disease is the first step in related prevention and control work. This article aims to understand the prevalence and associated risk factors of sarcopenia among the older adult (≥60 years old) in China and to provide an evidence-based basis for early identification, management, and prevention of sarcopenia patients.
Methods
We searched seven databases: CNKI, Wanfang, VIP, PubMed, Web of Science, Embase, and Cochrane Library databases from the establishment of the database until January 31, 2024. The Quality evaluation criteria of cross-sectional studies recommended by the Agency for Healthcare Research and Quality (AHRQ) were used for literature quality evaluation. Stata 18.0 software was used for statistical analysis.
Results
We finally included 45 studies, involving a total of 37,571 cases. After statistical analysis, we found that the prevalence of sarcopenia among the older adult in China was 20.7% [95% CI (18.3, 23.0%)]. The results of subgroup analysis suggest that: ① According to gender, the prevalence rate of sarcopenia in women (21.6%) is higher than that in men (19.2%); ② According to age, the prevalence rate of older adult people aged ≥80 (45.4%) was the highest, followed by 70–79 (27.2%) and 60–69 (15.7%). ③ According to region, the prevalence rate of the older adult in the south (21.7%) is higher than that in the north (19.0%); ④ According to the time of publication, the prevalence of sarcopenia among the older adult in China has increased (from 19.2% in 2014–2018 to 21.4% in 2019–2024); ⑤ According to the diagnostic criteria, the detection rate of AWGS (2019) is higher than that of AWGS (2014) (24.5% vs. 19.3%). Finally, aging, low BMI, low leg circumference, smoking, depression, osteoporosis, malnutrition and malnutrition risk are all risk factors for sarcopenia among the older adult in China.
Conclusion
The prevalence of sarcopenia in the older adult in China was higher (20.7%), which should be paid attention to by relevant health authorities. In addition, aging, low BMI, low calf circumference, smoking, depression, osteoporosis, malnutrition and malnutrition risk are risk factors for the development of sarcopenia in the older adult in China. For these high-risk populations, early identification, prevention, and intervention can be carried out to delay the occurrence and progression of sarcopenia.
Keywords: sarcopenia, prevalence, risk factors, older adult, Chinese, meta-analysis
1. Introduction
Sarcopenia is a common senile disease, which refers to the symptoms of a decline in skeletal muscle mass and muscle strength caused by aging (1). Sarcopenia is highly associated with a variety of adverse outcomes (such as fractures, cognitive decline, metabolic disorders, etc.), and its development process is generally hidden and not easily detected by patients until the occurrence of the above-mentioned adverse consequences (2, 3). Sarcopenia not only seriously affects the quality of life of the older adult, but the follow-up medical care will also bring a heavy economic burden to the family and society (4). An epidemiological study in South Korea showed that the prevalence of sarcopenia in the older adult aged 60 years and above was about 13.1% (5); Japan also reported that the prevalence of sarcopenia in the older adult aged 60 years and above was 9.9% (6). A global epidemiological study of sarcopenia shows that: sarcopenia seriously affects the quality of life of 10–16% of the older adult worldwide (7).
Sarcopenia is an aging disease, and with the global trend of the aging population, the phenomenon of sarcopenia in the older adult will become increasingly common (8, 9). As is well known, China has entered a stage of rapid population aging. According to the results of the 7th National Population Census (10): the population aged 60 and above in China is approximately 264 million, accounting for 18.7% of the total population. At present, sarcopenia has received attention from various countries, but a unified diagnostic standard has not yet been established (8, 11). Among them, the most commonly used diagnostic criteria include the European Working Group on Sarcopenia in Older People (EWGSOP), the Asian Working Group on Sarcopenia (AWGS), and the International Working Group on Sarcopenia (IWGS) (12–15). These diagnostic criteria all recognize that muscle mass, muscle strength, and daily activity ability are the three important factors for diagnosing sarcopenia. However, due to significant differences in factors such as country, region, diet, environment, and race, accurately assessing the epidemiological situation of sarcopenia and carrying out related prevention and treatment work still pose certain challenges (16).
Collecting epidemiological evidence of sarcopenia in the older adult is the first step to formulating preventive procedures or health care services. In the case of insufficient literature reports, systematic evaluation of prevalence and risk factors data is becoming more and more important for policy formulation and implementation of preventive measures. At present, we find that China has begun to pay attention to the epidemiological information of sarcopenia in the older adult, but the conclusions on its epidemiological characteristics, risk factors, and complications are not satisfactory (17–19). At the same time, in the past few years, several large-scale sample studies have been published at home and abroad, which can be used for systematic review and meta-analysis. Therefore, we plan to assess the prevalence and risk factors of sarcopenia among the older adult in China aged 60 and above in China, and provide evidence-based evidence for early identification, management and prevention of sarcopenia among the older adult in China.
2. Methods
2.1. Search strategy
This study is based on the PRISMA statement (20). Because this study is an epidemiological survey, ethical approval is not required. The systematic review and meta-analysis have been registered in PROSPERO with the number CRD42023494338. We used the following principles of the PICOS algorithm to guide the initial retrieval:
P (population): China older adult people over 60 years old;
I (intervention): no intervention;
C (comparison): no comparison;
O (outcome): the prevalence and risk factors of sarcopenia among the older adult in China;
S (study): cross-sectional study/retrospective study.
2.2. Literature search
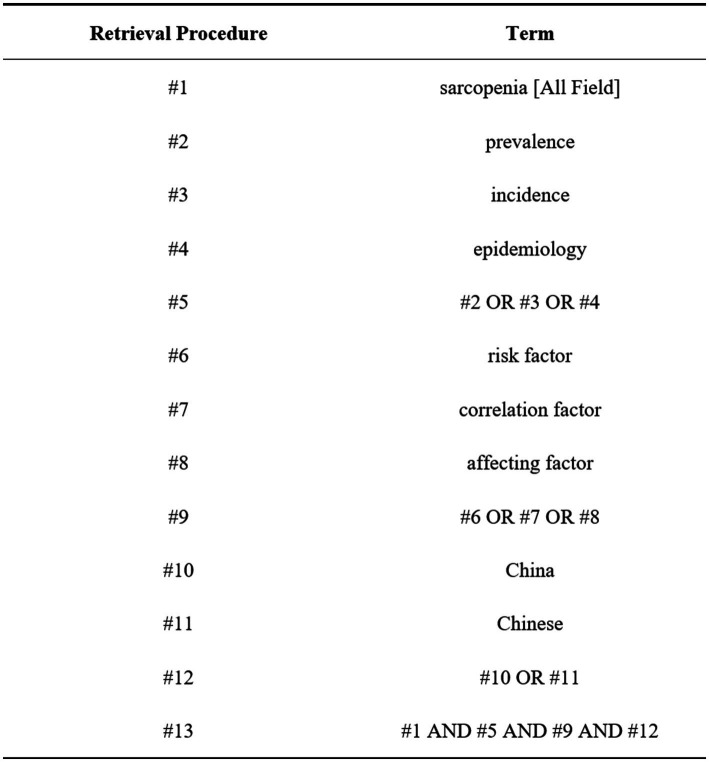
We searched seven databases: CNKI, Wanfang, VIP, PubMed, Web of Science, Embase, and Cochrane Library from the establishment of the database until January 31, 2024. The method of “subject word + the free word” was used to search, and the Chinese search terms were “sarcopenia”; “prevalence, incidence, epidemiology”; “Influencing factors, related factors, risk factors”; English search terms are: “sarcopenia”; “prevalence, incidence, epidemiology”; “risk factor, correlation factor, affecting factor”; “China, Chinese.”
The literature retrieval strategy takes PubMed as an example. The detailed retrieval formula of PubMed is as follows: (“sarcopenia”[MeSH Terms] OR “sarcopenia”[All Fields] OR “sarcopenia s”[All Fields]) AND (“epidemiology”[MeSH Subheading] OR “epidemiology”[All Fields] OR “prevalence”[All Fields] OR “prevalence”[MeSH Terms] OR “prevalance”[All Fields] OR “prevalences”[All Fields] OR “prevalence s”[All Fields] OR “prevalent”[All Fields] OR “prevalently”[All Fields] OR “prevalents”[All Fields] OR (“epidemiology”[MeSH Subheading] OR “epidemiology”[All Fields] OR “incidence”[All Fields] OR “incidence”[MeSH Terms] OR “incidences”[All Fields] OR “incident”[All Fields] OR “incidents”[All Fields]) OR (“epidemiologies”[All Fields] OR “epidemiology”[MeSH Subheading] OR “epidemiology”[All Fields] OR “epidemiology”[MeSH Terms] OR “epidemiology s”[All Fields])) AND ((“risk factors”[MeSH Terms] OR (“risk”[All Fields] AND “factors”[All Fields]) OR “risk factors”[All Fields]) AND ((“correlate”[All Fields] OR “correlated”[All Fields] OR “correlates”[All Fields] OR “correlating”[All Fields] OR “correlation”[All Fields] OR “correlation s”[All Fields] OR “correlations”[All Fields] OR “correlative”[All Fields] OR “correlatives”[All Fields]) AND (“factor”[All Fields] OR “factor s”[All Fields] OR “factors”[All Fields])) AND ((“affect”[MeSH Terms] OR “affect”[All Fields] OR “affects”[All Fields] OR “affected”[All Fields] OR “affecteds”[All Fields] OR “affecting”[All Fields]) AND (“factor”[All Fields] OR “factor s”[All Fields] OR “factors”[All Fields]))) AND (“china”[MeSH Terms] OR “china”[All Fields] OR “china s”[All Fields] OR “chinas”[All Fields] OR (“chineses”[All Fields] OR “east asian people”[MeSH Terms] OR (“east”[All Fields] AND “asian”[All Fields] AND “people”[All Fields]) OR “east asian people”[All Fields] OR “chinese”[All Fields])). (For the specific search process, see Figure 1 and Supplementary File 1).
Figure 1.
PubMed retrieval procedure flowchart.
2.3. Literature inclusion and exclusion criteria
2.3.1. Inclusion criteria
① According to the author’s language ability, literature in English, and Chinese were eligible; ② The study subjects include the older adult population aged ≥60 in China; ③ The study includes risk factors that may lead to sarcopenia in the older adult; ④ The definition and diagnostic criteria for sarcopenia were proposed in the study; ⑤ The study provided data on the prevalence of sarcopenia, or data that can be used to calculate the prevalence; ⑥ OR values and 95% CI were provided in the study; and ⑦ Cross-sectional or retrospective studies.
2.3.2. Exclusion criteria
① Repeated published research; ② Research published in the form of reviews, conference abstracts, etc.; ③ Research that cannot obtain full text or extract complete data; ④ The sample size of the older adult is too small (≤100 studies); and ⑤ Low-quality research (AHRQ score < 6 points).
2.4. Literature screening and data extraction
We import the retrieved literature into EndNoteX9.1 software and first remove the duplicate literature. The second step is to make a preliminary screening by reading the titles and abstracts of the literature. Finally, read the rest of the literature in full, and make the final inclusion and exclusion in strict accordance with the inclusion and exclusion criteria. In this process, two evaluators (W.L. and X.Z.) independently cross-checked the included literature repeatedly. If there is any dispute, it will be resolved through discussion between the two parties or the introduction of the third researcher (XL.F.) for review.
In the data extraction stage, two researchers (W.L. and X.Z.) independently used Excel tables to extract data. The main contents of the extraction are as follows: (1) Basic information included in the literature: first author, publication year, investigation place, etc. (2) Calculate the prevalence rate of sarcopenia and related data of risk factors; (3) Key information of biased risk assessment. After the data is extracted, it shall be summarized, exchanged, and reviewed. If there is disagreement, it shall be submitted to the third researcher (XL.F.) for review.
2.5. Literature quality evaluation
We adopt the cross-sectional study quality evaluation criteria recommended by the Agency for Healthcare Research and Quality (AHRQ) for literature quality evaluation (21). The evaluation criteria consist of 11 items, with a rating scale of 1 point for “yes” and 0 points for “no/unclear.” A total score of 8–11 indicates high quality, 4–7 indicates moderate quality, and 0–3 indicates low quality (see Table 1 for details).
Table 1.
AHRQ cross-sectional study quality evaluation standard table.
| Item content | Yes | No/Unclear | |
|---|---|---|---|
| 1 | Define the source of information (survey or record review?) | ||
| 2 | List inclusion and exclusion criteria for exposed and unexposed subjects (cases and control) or refer to previous publications | ||
| 3 | Indicate period used for identifying patients | ||
| 4 | Indicate whether or not subjects were consecutive if not population-based | ||
| 5 | Indicate if evaluators of subjective components of the study were masked to other aspects of the status of the participants | ||
| 6 | Describe any assessments undertaken for quality assurance purposes (e.g., test/retest of primary outcome measurements) | ||
| 7 | Explain any patient exclusions from the analysis | ||
| 8 | Describe how confounding was assessed and/or controlled | ||
| 9 | lf applicable, explain how missing data were handled in the analysis | ||
| 10 | Summarize patient response rates and completeness of data collection | ||
| 11 | Clarify what follow-up, if any, was expected and the percentage of patients for which incomplete data or follow-up was obtained |
2.6. Statistics
We used Stata18.0 software to statistically analyze the data on the prevalence rate and risk factors of sarcopenia and analyzed the heterogeneity of the included studies through the Q test and I2 value. If I2 > 50%, and p < 0.1, it shows that there is high heterogeneity among the studies, and the random effect model is used for analysis. Otherwise, the fixed effect model will be used for statistical analysis (22). If the heterogeneity between the included research results is large, it is necessary to further analyze the sources of heterogeneity, and the subgroup analysis method can be used to try to find out the obvious sources of heterogeneity. The subgroups set in this paper include: gender, age, region, publication time, and diagnostic criteria, and the statistical significance p-value in all statistical analyses is set to 0.05.
In this study, we did not check the publication bias. The reasons are as follows: publication bias is a phenomenon in which studies with significant results are easier to publish than those with insignificant results, which may lead to systematic differences between published and unpublished studies (23). However, in the observational study of prevalence, there are no significant or insignificant results, and it is not recommended to use mature methods to test this deviation in the systematic evaluation of prevalence research. Therefore, we did not check the publication bias.
3. Results
3.1. Literature screening process and results
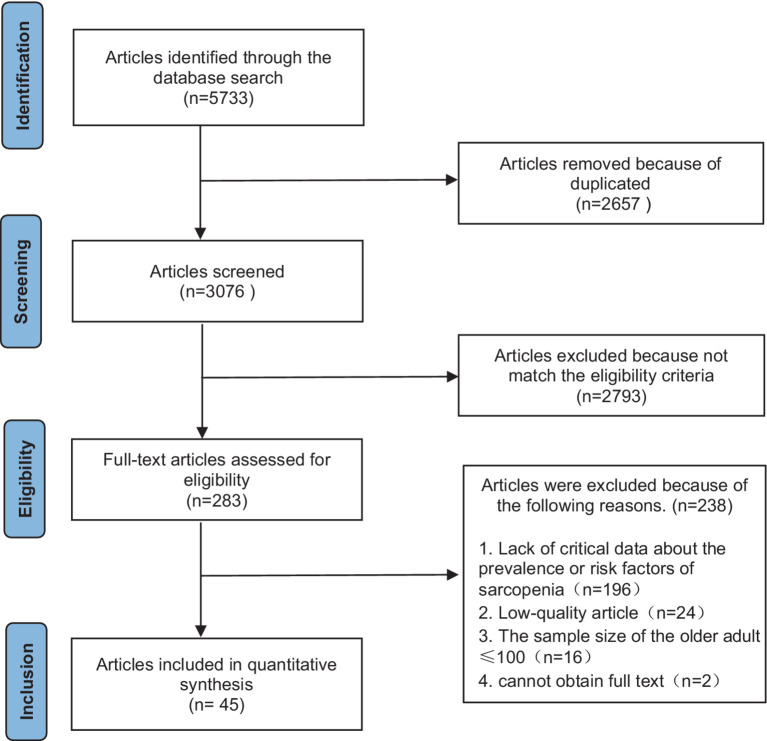
After a preliminary search, we obtained a total of 5,733 related articles, and after a layer-by-layer screening, we finally included 45 studies, with a total of 37,571 subjects. (For the process and results of literature screening, see Figure 2).
Figure 2.
Literature retrieval process diagram.
3.2. Basic characteristics and quality evaluation results of included literature
To ensure the quality of the included literature, we set the inclusion quality standard (AHRQ Score ≥ 6). A total of 45 literatures were included in this study, involving 37,571 older adult people over 60 years old in China in 31 provinces and cities. The general situation and quality evaluation results of the included literature are shown in Table 2. (For the detailed results of literature evaluation, see Supplementary File 2; for the general information of literature, see Supplementary File 3).
Table 2.
General information and quality evaluation results of the included literature.
| Study | Region | Population source | Diagnostic criteria | Muscle mass assessment methods | Sarcopenia size | Sample size | AHRQ score | |
|---|---|---|---|---|---|---|---|---|
| 1 | Wang et al. 2024 (24) | Yunnan-guizhou Plateau region* | Community population | AWGS (2019) | BIA | 194 | 1,327 | 8 |
| 2 | Dai et al. 2023 (25) | China | Community population | AWGS (2019) | BIA | 919 | 5,016 | 6 |
| 3 | Wan et al. 2023 (26) | Gansu | Inpatients | AWGS (2019) | BIA | 232 | 540 | 6 |
| 4 | Zou et al. 2023 (27) | Anhui | Community population | AWGS (2019) | BIA | 214 | 1716 | 6 |
| 5 | Ma et al. 2023 (28) | Shandong | Inpatients | AWGS (2019) | BIA | 143 | 606 | 6 |
| 6 | Chen et al. 2023 (29) | Xiangtan | Community population | AWGS (2019) | BIA | 87 | 556 | 7 |
| 7 | Musha et al. 2023 (30) | Xinjiang | Community population | AWGS (2019) | BIA | 184 | 1,561 | 7 |
| 8 | He et al. 2022 (31) | Shanghai | Community population | AWGS (2019) | BIA | 275 | 1,407 | 9 |
| 9 | Zhong et al. 2022 (32) | Hunan | Community population | AWGS (2019) | BIA | 282 | 1,040 | 7 |
| 10 | Tang et al. 2022 (33) | Inner Mongolia | Community population | AWGS | —— | 92 | 526 | 7 |
| 11 | Han et al. 2022 (34) | Urumqi | Inpatients | SARC-F Scale | —— | 113 | 695 | 6 |
| 12 | Li et al. 2022 (35) | Tianjin | Community population | IWGS (2011) | BIA | 115 | 475 | 7 |
| 13 | Zhang et al. 2022 (36) | Dali | Community population | AWGS (2019) | BIA | 21 | 103 | 8 |
| 14 | Li et al. 2022 (37) | Zhejiang | Community population | AWGS (2014) | BIA | 278 | 1,420 | 6 |
| 15 | Ko et al. 2021 (38) | Taiwan | Health examination population | AWGS (2019) | BIA | 138 | 500 | 8 |
| 16 | Chang et al. 2021 (39) | Taiwan | Nursing home population | AWGS (2019) | BIA | 88 | 170 | 7 |
| 17 | Pan et al. 2021 (40) | Xining | Inpatients | AWGS (2014) | BIA | 30 | 150 | 6 |
| 18 | Zhang et al. 2021 (41) | Jiangsu | Inpatients | AWGS (2019) | BIA | 173 | 445 | 7 |
| 19 | Liu et al. 2020 (42) | Western China* | Community population | AWGS | BIA | 556 | 1712 | 7 |
| 20 | Yang et al. 2020 (43) | Urumqi | Community population | EWGSOP (2018) EWGSOP (2014) AWGS (2014) IWGS (2011) |
BIA | 483 | 22 76 44 78 |
6 |
| 21 | Chen et al. 2020 (44) | Nanjing | Community population | EWGSOP | DXA | 27 | 249 | 7 |
| 22 | Xu et al. 2020 (45) | Chengdu | Inpatients | AWGS (2014) | DXA | 63 | 142 | 6 |
| 23 | Liang et al. 2020 (46) | Beijing | Inpatients | AWGS (2014) | DXA | 80 | 180 | 8 |
| 24 | Meng et al. 2020 (47) | Xinxiang | Community population | AWGS (2014) | BIA | 131 | 1,004 | 7 |
| 25 | Che et al. 2020 (48) | Urumqi | Community population | Ishii Scale | – | 287 | 740 | 8 |
| 26 | Tian et al. 2020 (49) | Urumqi | Community population | AWGS (2014) | BIA | 35 | 395 | 8 |
| 27 | Yang et al. 2019 (50) | Suzhou | Nursing home population | AWGS (2014) | BIA | 91 | 316 | 8 |
| 28 | Yao et al., 2019 (51) | Xiangtan | Inpatients | AWGS | BIA | 47 | 378 | 7 |
| 29 | Liu et al. 2019 (52) | Chongqing | Community population | AWGS (2014) | BIA | 14 | 247 | 7 |
| 30 | He et al. 2019 (53) | Beijing | T2DM patients | AWGS (2014) | BIA | 75 | 650 | 6 |
| 31 | Hao et al. 2018 (54) | Chengdu | Inpatients | AWGS | BIA | 127 | 407 | 7 |
| 32 | Zeng et al. 2018 (55) | Chengdu | Nursing home population | EWGSOP AWGS IWGS |
BIA | 277 | 90 95 106 |
7 |
| 33 | Zhang et al. 2018 (56) | Shanghai | Community population | AWGS | BIA | 164 | 1,148 | 8 |
| 34 | Wang et al. 2018 (57) | Chengdu | Community population | AWGS (2014) | BIA | 71 | 915 | 7 |
| 35 | Yang et al. 2018 (58) | Suzhou | Community population | AWGS | DXA | 91 | 316 | 8 |
| 36 | Liao et al. 2018 (59) | Chongqing | Nursing home population | AWGS (2014) | BIA | 86 | 225 | 6 |
| 37 | Wang et al. 2018 (60) | Nantong | Outpatient | AWGS (2014) | BIA | 92 | 407 | 8 |
| 38 | Hai et al. 2017 (61) | Chengdu | Community population | AWGS | BIA | 88 | 836 | 8 |
| 39 | Hu et al. 2017 (62) | Sichuan | Community population | AWGS (2014) | DXA | 112 | 607 | 7 |
| 40 | Han et al. 2016 (63) | Tianjin | Community population | AWGS (2014) | BIA | 99 | 1,069 | 6 |
| 41 | Xia et al. 2016 (64) | Beijing | Community population | AWGS (2014) | BIA | 137 | 683 | 6 |
| 42 | Gao et al. 2015 (65) | Sichuan | Community population | AWGS | — | 60 | 612 | 9 |
| 43 | Meng et al. 2015 (66) | Taiwan | Community population | EWGSOP | DXA | 44 | 771 | 7 |
| 44 | Wu et al. 2014 (67) | Taiwan | Community population | EWGSOP | BIA | 39 | 549 | 6 |
| 45 | Yu et al. 2014 (68) | Hong Kong | Community population | EWGSOP | — | 361 | 4,000 | 8 |
AWGS, Asian Working Group on Sarcopenia; EWGSOP, European Working Group on Sarcopenia in Older People; IWGS, International Working Group on Sarcopenia; SARC-F Scale, a simple five-item scoring questionnaire for sarcopenia; Ishii Scale, a simple three-item scoring questionnaire for sarcopenia; BIA, bioelectrical impedance method; DXA, dual-energy X-ray absorption method; AHRQ, Agency for Healthcare Research and Quality; T2DM, type 2 diabetes. Yunnan-guizhou Plateau region*, specifically Liupanshui City and Kunming City; Western China*, specifically Yunnan, Guizhou, Sichuan and Xinjiang.
3.3. Meta-analysis results
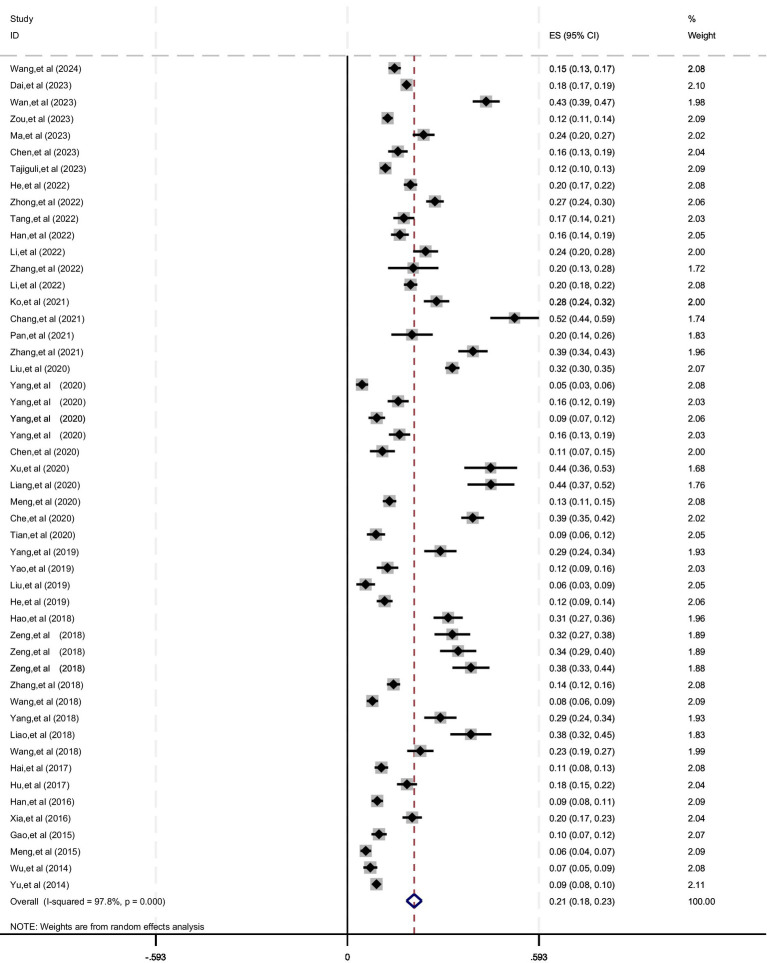
3.3.1. Meta-analysis of the prevalence of sarcopenia among the older adult in China
We studied the prevalence of sarcopenia in the older adult in 45 literatures. The result of the meta-analysis showed that I2 = 97.8%, p < 0.001, which indicated that the heterogeneity among the studies was high. The sensitivity analysis was carried out by the one-by-one elimination method, and no literature that had a significant impact on the overall results was found, so the random effect model was used for combined analysis. Meta-analysis shows that the prevalence of sarcopenia among the older adult (≥60) in China is 20.7% [95% CI (18.3, 23.0%)], as shown in Figure 3 and Table 3.
Figure 3.
Meta-analysis forest figure of the prevalence of sarcopenia among the older adult in China.
Table 3.
Summary table of meta-analysis results of prevalence of sarcopenia in the older adult in China.
| Subgroup | Number of included literature | Results of heterogeneity test | Effect model | The prevalence % (95%Cl) | |
|---|---|---|---|---|---|
| I2 | p | ||||
| Total prevalence rate (24–68) | 45 | 99.2% | <0.001 | Random effect model | 20.7 (18.3, 23.0) |
| Sex | |||||
| Men (24, 25, 27, 29–33, 35, 37–41, 43–45, 47, 48, 50, 51, 54–64, 66, 67) | 34 | 94.7% | <0.001 | Random effect model | 19.2 (16.6, 21.8) |
| Women (24, 25, 27, 29–33, 35, 37–41, 43–45, 47, 48, 50, 51, 54–64, 66, 67) | 34 | 96.5% | <0.001 | Random effect model | 21.6 (18.7, 24.5) |
| Age | |||||
| 60–69 (26, 27, 31–33, 35, 41, 48, 64, 65) | 10 | 96.0% | <0.001 | Random effect model | 15.7 (10.6, 20.7) |
| 70–79 (26, 27, 31–33, 35, 41, 48, 64, 65) | 10 | 95.4% | <0.001 | Random effect model | 27.2 (20.2, 34.3) |
| ≥80 (26, 27, 31–33, 35, 41, 48, 64, 65) | 10 | 88.8% | <0.001 | Random effect model | 45.4 (35.9, 54.9) |
| Region | |||||
| South (24, 29, 31, 32, 36–39, 41, 44, 45, 50–52, 54–62, 65–68) | 27 | 97.7% | <0.001 | Random effect model | 21.7 (18.5, 24.9) |
| North (26, 28, 30, 33–35, 40, 43, 46–49, 53, 63, 64) | 15 | 97.6% | <0.001 | Random effect model | 19.0 (14.9, 23.1) |
| Publication year | |||||
| 2014–2018 (54–68) | 15 | 97.3% | <0.001 | Random effect model | 19.2 (15.8, 22.7) |
| 2019–2024 (24–53) | 30 | 97.6% | <0.001 | Random effect model | 21.4 (18.4, 24.3) |
| Diagnostic criteria | |||||
| AWGS (2019) (24–32, 36, 38, 39, 41) | 13 | 97.6% | <0.001 | Random effect model | 24.5 (20.3, 28.7) |
| AWGS (2014) (37, 40, 43, 45–47, 49, 50, 52, 53, 57, 59, 60, 62–64) | 16 | 96.4% | <0.001 | Random effect model | 19.3 (15.5, 23.1) |
3.3.2. Subgroup analysis of the prevalence of sarcopenia among the older adult in China
Meta-analysis of the prevalence of sarcopenia suggests that there is high heterogeneity among studies. We intend to use subgroup analysis to try to identify the source of clinical heterogeneity. The subgroups in this study included: gender (male; Female), age range (60–69; 70–79; ≥80), region (South/North; With Qinling Mountains and Huaihe River as the boundary, north of Qinling Mountains and Huaihe River is north, and south of Huaihe River is south), publication time (2014–2018; 2019–2024), diagnostic criteria (AWGS2019; AWGS2014). The results of the subgroup analysis are shown in Table 3.
3.3.3. Meta-analysis of the risk factor of sarcopenia among the older adult in China
We included 45 articles related to the risk factors of sarcopenia. After extraction, induction, and data processing by relevant personnel, we found that there were 10 risk factors involved in 2 or more studies. We made a meta-analysis of these risk factors of sarcopenia, and the results showed that aging, low BMI, low leg circumference, smoking, depression, osteoporosis, malnutrition and malnutrition risk were all risk factors of sarcopenia among the older adult in China. The results of the meta-analysis of influencing factors of sarcopenia are shown in Table 4.
Table 4.
Summary table of meta-analysis results of risk factors of sarcopenia in the older adult in China.
| Risk factor | Number of included literature | Results of heterogeneity test | Effect model | Result | ||
|---|---|---|---|---|---|---|
| I 2 | p | OR (95%CI) | p | |||
| Sex (women vs. men) (24–26, 31, 36, 38, 39, 43, 47, 54, 65–68) | 14 | 94.3% | <0.001 | Random effect model | 1.056 (0.936, 1.191) | 0.376 |
| Age (Continuous variable) (24, 25, 29, 32, 38, 43, 45, 49–51, 56, 59, 65, 67, 68) | 15 | 67.5% | <0.001 | Random effect model | 1.128 (1.117, 1.139) | <0.001* |
| BMI (Continuous variable) (27, 29, 31, 33, 38, 45, 47, 49–52, 54, 59, 66, 67) | 15 | 82.0% | <0.001 | Random effect model | 0.706 (0.686, 0.727) | <0.001* |
| Leg circumference (Continuous variable) (29, 47, 48, 55) | 4 | 89.3% | <0.001 | Random effect model | 0.743 (0.702, 0.786) | <0.001* |
| Smoking (Yes vs. NO) (24, 47, 54) | 3 | 66.8% | 0.049 | Random effect model | 2.092 (1.469, 2.977) | <0.001* |
| Depression (Yes vs. NO) (31, 36, 41, 47) | 4 | 0.0% | 0.508 | Fixed effect model | 2.432 (1.716, 3.447) | <0.001* |
| Osteoporosis (Yes vs. NO) (34, 41, 49, 59) | 4 | 0.0% | 0.980 | Fixed effect model | 2.778 (1.918, 4.026) | <0.001* |
| Malnutrition (Yes vs. NO) (32, 55) | 2 | 0.0% | 0.587 | Fixed effect model | 2.656 (1.679, 4.200) | <0.001* |
| Malnutrition risk (Yes vs. NO) (28, 32, 39) | 3 | 36.9% | 0.205 | Fixed effect model | 2.224 (1.712, 2.891) | <0.001* |
| Malnutrition and malnutrition risk (Yes vs. NO) (36, 37, 65) | 3 | 89.5% | <0.001 | Random effect model | 1.641 (1.334, 2.019) | <0.001* |
4. Discussion
4.1. The prevalence of sarcopenia in Chinese older adult
In October 2016, sarcopenia was officially included in the International Classification of Diseases (ICD-10) disease code, marking that sarcopenia has been recognized as a new type of geriatric syndrome and has attracted worldwide attention (69). In 2021, Petermann-Rocha et al. reported on the global prevalence of sarcopenia (4): the prevalence of sarcopenia in people aged 60 and above in the world is about 10–27%. A Korean meta-analysis reported that (5): the prevalence of sarcopenia in the older adult aged 60 years and older in Korea was 13.1%. A similar study in Japan reported that the prevalence of sarcopenia in the older adult (≥60) in Japan was 9.9% (6). Diz et al. (70) reported that the overall prevalence of sarcopenia in older adult people aged 60 years and above in Brazil was 17.0% [95%CI (13.0, 22.0%)]. Our results show that the prevalence of sarcopenia in the older adult in China is 20.7%, which is much higher than in similar Asian countries such as Japan (9.9%) (6) and South Korea (13.01%) (5). The specific reason may be that these Asian countries entered the aging society earlier than China, and have gradually established medical security systems that adapt to their national conditions. In general, there are differences in diet, environment, culture, and ethnically specific genetics among countries and regions, which may be the main reasons for the differences in the prevalence of sarcopenia among countries.
Subgroup analysis showed that there was an association between gender and the incidence of sarcopenia, and the prevalence of sarcopenia was higher in women than in men. Our results are consistent with Dai, Yang et al. (25, 43). The specific reasons may be related to the following reasons: First, the ovarian function of older adult women after menopause decreases, and the content of metabolic hormones (such as estradiol and androgen) in the body will also decrease, which seriously affects the generation of muscle cells and protein synthesis (71). On the other hand, women are more focused on body image management, leading to inadequate nutrient intake, which may also be related to the higher prevalence of sarcopenia in women. However, Chinese scholars Ren, Chen et al. reported the opposite result (17, 19): the prevalence of sarcopenia in older adult Chinese men was higher. They suggest that this difference may be related to the unhealthy lifestyle of men (such as smoking and drinking). As we age, the effects of an unhealthy lifestyle may significantly increase, and these factors can all contribute to sarcopenia (5). In addition, a 12-year cohort study in Japan showed that (72): men were more likely to experience muscle mass loss than women. About this difference, we suggest that future multi-center, large-sample prospective studies can be conducted to continue to explore the relationship between gender and the occurrence of sarcopenia in the older adult, to better implement precise prevention.
Sarcopenia is a well-recognized age-related degenerative condition. With the global rise in aging populations, the prevalence of sarcopenia is expected to increase significantly. This was also confirmed in our study: by age, the prevalence was highest in the older age group ≥80 years (45.4%), followed by 70–79 years (27.2%), and finally 60–69 years (15.7%). Under normal physiological conditions, human skeletal muscle mass reaches its peak at around 25 years of age, and then the number and volume of skeletal muscle fibers begin to decline, and the decline rate gradually accelerates with the increase of age, which is the result of synergistic regulation of multiple aging mechanisms in the human body (1). In addition, with the growth of age, the incidence of various basic diseases in the older adult will also increase, which will also affect the regulation of various hormones and the absorption of nutrients, thereby indirectly affecting the decline of muscle mass (73). Compared with the north (19.0%), the prevalence of sarcopenia was higher in the older adult in the south (21.7%). Our study was consistent with Mao et al. (74), but some studies reported the opposite result (17). China’s vast territory, the climate environment, and the dietary habits of different regions are quite different, which may be the main reason for the difference in prevalence. The climate in the north is mostly cold. Due to the influence of climate, the local people’s diet mainly includes “beef and mutton, dairy products and nuts,” and the incidence of malnutrition and malnutrition risk is relatively low (75). So far, there are few studies on regional differences in the prevalence of sarcopenia in China, which can be further verified with more relevant epidemiological studies in the future.
In addition to the differences in demographic characteristics, the different diagnostic criteria of sarcopenia also directly affect the detection rate of sarcopenia. Based on the fact that China is in Asia, and to ensure the comparability of this study in Asian populations, we selected AWGS for subgroup analysis in terms of diagnostic criteria. Compared with AWGS (2014), the latest AWGS (2019) has significantly improved the evaluation criteria of walking speed and male grip strength (among which, walking speed has been increased from 0.8 m/s to 1.0 m/s, and male grip strength has been increased from 26 kg to 28 kg). As a result, the AWGS (2019) will have a higher rate of sarcopenia detection, and our study also confirms this result. Domestic studies on the evaluation of sarcopenia in the older adult based on AWGS (2014) criteria also generally reported a low incidence [Xinxiang 13.1% (47), Chengdu 10.6% (61), Tianjin 9.3% (63)]. Finally, in the last 5 years, the prevalence of sarcopenia in the older adult in China has been on the rise. It increased from 19.2% in 2014–2018 to 21.4% in 2019–2024. We infer that this difference may be due to past and present differences in health and medical resources. At the same time, the widening of diagnostic criteria may also be one of the reasons for the significant increase in the prevalence of sarcopenia reported in China in recent years.
4.2. The risk factor of sarcopenia in Chinese older adult
The occurrence of sarcopenia in the older adult is related to many factors. Our study shows that aging, low BMI, low calf circumference, smoking, depression, osteoporosis, malnutrition and malnutrition risk are risk factors for sarcopenia in the older adult in China.
There is no doubt that aging is one of the risk factors for sarcopenia. Pang et al. reported the epidemiology of sarcopenia in the Singapore community population (76): the prevalence of sarcopenia was 13.6% in the community as a whole (21–90 years), but 32% in people over 60 years of age. A study in Thailand also found that (77): older adult people (≥80 years old) had the highest prevalence of sarcopenia (68%). A 12-year prospective population study in Sweden showed that (78): even subjects without sarcopenia had a 5.1% probability of developing suspected sarcopenia over 10 years. This is consistent with our findings that the older people get, the higher their risk of sarcopenia.
Secondly, bad lifestyle habits can also affect the prevalence of sarcopenia, of which smoking is considered to be a risk factor for sarcopenia. Previous studies have reported that the risk of sarcopenia in older adult smokers in Asia is 2.69 times that of non-smokers (79). The risk of sarcopenia among older smokers in Europe is 2.36 times that of non-smokers (80). We speculate that the reason may be related to the following reasons: on the one hand, smoking directly damages the health of skeletal muscle. Smoking can damage muscle metabolism, increase inflammation and oxidative stress, increase the overexpression of genes related to muscle atrophy, and activate various intracellular signaling pathways, thus causing skeletal muscle injury (81). On the other hand, smoking will increase the risk of cancer, respiratory diseases, and cardiovascular and cerebrovascular diseases (82), thus increasing energy consumption and reducing the activity capacity of the older adult, indirectly leading to the occurrence of sarcopenia. Therefore, not smoking or quitting early may be important for the prevention and treatment of sarcopenia.
There is also a link between depression, osteoporosis, and sarcopenia. Turkish scholar Olgun-Yazar et al. pointed out that (83): depression and sarcopenia are closely related. Symptoms associated with depression, such as weakness, loss of appetite, and decreased activity, may contribute to the onset and progression of sarcopenia (84). Meanwhile, some inflammatory cytokines secreted by the musculoskeletal system are closely related to the occurrence of depression, such as IL-6, TNF-a, and 5-HT (85). In the early prevention and treatment of sarcopenia, it is necessary to pay attention to and care for the depressed older adult.
Osteoporosis is a systemic bone metabolic disease characterized by low bone mass and mass, which can increase susceptibility to sarcopenia (86). Sarcopenia and osteoporosis are both associated with aging, low quality of life, and low condition of health, and they often occur together. At present, some scholars have shown that there is a close relationship between muscle and bone, namely, osteosarcopenia, and sarcopenia-osteoporosis (87, 88). Maurel et al. (89) investigated the relationship between sarcopenia and osteoporosis and showed that osteoporosis increases the risk of developing sarcopenia. Our study also found that osteoporosis is a risk factor for sarcopenia. Specific reasons may be related to the connection between muscle and bone. For example, Bone cells secrete osteocalcin, insulin-like, etc., affecting muscle quality and function, and the decrease of bone cells will lead to the decline of muscle mass and function (90). Therefore, we should pay attention to the role of bone health in the occurrence of sarcopenia, and reduce the incidence of sarcopenia while maintaining bone health in the older adult.
Finally, there is also a close relationship between the nutritional status of the body and sarcopenia (91). BMI and calf circumference can be used to evaluate the nutritional status of the older adult. Among them, calf circumference is currently recognized as an alternative marker of muscle mass and is used as one of the diagnostic criteria for sarcopenia (92, 93). To a certain extent, BMI can also reflect the nutritional status of the body. A higher BMI is a protective factor for sarcopenia and is positively correlated with muscle mass (94). It is worth noting that there is a special condition here, that is, sarcopenic obesity. This is a condition that occurs based on excessive obesity, with decreased muscle tissue and increased fat infiltration between muscle fibers and muscle cells (10, 12). Medical and health workers should pay attention to health education: the older adult can properly maintain a high BMI level under the premise of not obesity. In addition, physiological evidence shows that when the body is in poor nutritional condition, amino acids, and muscles are broken down and oxidized to produce energy to maintain normal life functions. If sustained for a longer period, it will result in a negative nitrogen balance, as well as a gradual loss of muscle mass and function (95). In addition, poor nutritional status can also lead to micronutrient deficiencies (such as vitamin D and vitamin B12), which further leads to muscle loss and decreased function (96, 97). In conclusion, timely screening and assessment of the nutritional status of the older adult may be an effective strategy for early detection, diagnosis, and management of patients with sarcopenia. Proven and easy-to-use nutrition screening tools are necessary, such as a simple nutritional assessment profile (Mini Nutritional Assessment Short Form, MNA – SF) can be used to determine the nutritional status of the older adult and the poor nutrition risk (98).
So far, this study is currently the most geographically diverse and has the highest number of subjects in the epidemiological study of sarcopenia in older adult people in China, and involves risk factors for sarcopenia. We reported the latest data and risk factors for sarcopenia in older adult people aged 60 and above in China. We conducted differences in gender, age, region (southern/northern), diagnostic criteria, and other factors through subgroup analysis. These works provide more information and evidence-based evidence for the epidemiology of sarcopenia and are the first step in developing preventive measures or health services for the older adult. In addition, our study also found that aging, low BMI, low calf circumference, smoking, depression, osteoporosis, malnutrition and malnutrition risk are risk factors for the development of sarcopenia in the older adult in China. For the older adult population with high-risk factors, timely prevention and screening is very necessary.
There are some limitations to the study. First, we collected representative data for each region but were limited by the characteristics of individual studies and differences between different cities, which may affect comparisons between included studies. Secondly, some studies reported prevalence rates for different age groups and different risk factors, and relevant data could not be included in subgroups, resulting in fewer studies included in some subgroups (such as smoking, malnutrition, and malnutrition, etc. risk factors), which may also affect comparisons between included studies. Finally, this study is based primarily on evidence from observational studies that cannot provide information about causation for the observed associations. Currently, there is a lack of high-quality prospective cohort studies on sarcopenia, especially in exploring the risk factors for sarcopenia. In addition to focusing on clinical patients susceptible to sarcopenia, cohort studies with accurate measurements of muscle quantity and function in the general healthy population are needed to provide evidence for developing primary prevention strategies.
5. Conclusion
The results of this study show that the overall prevalence of sarcopenia in the older adult aged 60 and above in China is relatively high (20.7%), and it shows a gradual increasing trend in the past 5 years. This phenomenon should arouse the attention and concern of public health departments. Finally, we suggest that the public health sector should carry out early screening, intervention, and management of sarcopenia promptly, especially for the older adult population with high-risk factors (such as osteoporosis and depression).
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
SM: Writing – original draft, Writing – review & editing, Data curation, Formal analysis, Investigation, Project administration, Software. XH: Writing – original draft, Data curation, Investigation, Software, Writing – review & editing. XF: Conceptualization, Writing – review & editing, Data curation, Formal analysis, Software. XZ: Writing – review & editing, Data curation, Software. MT: Writing – review & editing, Data curation, Project administration, Software, Supervision, Validation. WL: Writing – original draft, Writing – review & editing, Data curation, Methodology, Software. WZ: Writing – original draft, Conceptualization, Data curation, Formal analysis, Software. XS: Writing – original draft, Writing – review & editing, Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Supervision. KL: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Acknowledgments
We thank all our colleagues in the Department of Epidemiology and Health Statistics at Zhejiang Chinese Medicine University.
Funding Statement
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was funded by the National Natural Science Foundation of China (82274272); Zhejiang Traditional Chinese Medicine Administration (2022ZZ020); and Department of Education of Zhejiang Province (Y202248737). These funders had no role in the study design, data collection, and analysis, interpretation of data, and writing the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1415398/full#supplementary-material
The detailed information of literature retrieval strategy.
The detailed results of literature evaluation.
The general information of included literature.
The corresponding PRISMA checklist.
References
- 1.Cui H, Wang Z, Wu J, Liu Y, Zheng J, Xiao W, et al. Chinese expert consensus on prevention and intervention for elderly with sarcopenia (2023). Aging Med. (2023) 6:104–15. doi: 10.1002/agm2.12245, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xia L, Zhao R, Wan Q, Wu Y, Zhou Y, Wang Y, et al. Sarcopenia and adverse health-related outcomes: an umbrella review of meta-analyses of observational studies. Cancer Med. (2020) 9:7964–78. doi: 10.1002/cam4.3428, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cruz-Jentoft AJ, Sayer AA. Sarcopenia. Lancet. (2019) 393:2636–46. doi: 10.1016/S0140-6736(19)31138-9 [DOI] [PubMed] [Google Scholar]
- 4.Petermann-Rocha F, Balntzi V, Gray SR, Lara J, Ho FK, Pell JP, et al. Global prevalence of sarcopenia and severe sarcopenia: a systematic review and meta-analysis. J Cachexia Sarcopenia Muscle. (2022) 13:86–99. doi: 10.1002/jcsm.12783, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Choo YJ, Chang MC. Prevalence of sarcopenia among the elderly in Korea: a meta-analysis. J Preven Med Public Health. (2021) 54:96–102. doi: 10.3961/jpmph.21.046, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Makizako H, Nakai Y, Tomioka K, Taniguchi Y. Prevalence of sarcopenia defined using the Asia working Group for Sarcopenia criteria in Japanese community-dwelling older adults: a systematic review and meta-analysis. Phys Ther Res. (2019) 22:53–7. doi: 10.1298/ptr.R0005, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yuan S, Larsson SC. Epidemiology of sarcopenia: prevalence, risk factors, and consequences. Metab Clin Exp. (2023) 144:155533. doi: 10.1016/j.metabol.2023.155533, PMID: [DOI] [PubMed] [Google Scholar]
- 8.Sayer AA, Cruz-Jentoft A. Sarcopenia definition, diagnosis and treatment: consensus is growing. Age Ageing. (2022) 51:afac220. doi: 10.1093/ageing/afac220, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bauer J, Morley JE, Schols A, Ferrucci L, Cruz-Jentoft AJ, Dent E, et al. Sarcopenia: a time for action. An SCWD position paper. J Cachexia Sarcopenia Muscle. (2019) 10:956–61. doi: 10.1002/jcsm.12483, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Bureau of Statistics, Office of the Leading Group of the Seventh National Population Census of the State Council. Bulletin of the 7th National Population Census (no. 5) – age composition of the population. China Stat. (2021) 5:10–1. [Google Scholar]
- 11.Coletta G, Phillips SM. An elusive consensus definition of sarcopenia impedes research and clinical treatment: a narrative review. Ageing Res Rev. (2023) 86:101883. doi: 10.1016/j.arr.2023.101883, PMID: [DOI] [PubMed] [Google Scholar]
- 12.Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. (2019) 48:16–31. doi: 10.1093/ageing/afy169, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah KS, et al. Sarcopenia in Asia: consensus report of the Asian working Group for Sarcopenia. J Am Med Dir Assoc. (2014) 15:95–101. doi: 10.1016/j.jamda.2013.11.025, PMID: [DOI] [PubMed] [Google Scholar]
- 14.Fielding RA, Vellas B, Evans WJ, Bhasin S, Morley JE, Newman AB, et al. Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc. (2011) 12:249–56. doi: 10.1016/j.jamda.2011.01.003, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European working group on sarcopenia in older people. Age Ageing. (2010) 39:412–23. doi: 10.1093/ageing/afq034, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dent E, Morley JE, Cruz-Jentoft AJ, Arai H, Kritchevsky SB, Guralnik J, et al. International clinical practice guidelines for sarcopenia (ICFSR): screening, diagnosis and management. J Nutr Health Aging. (2018) 22:1148–61. doi: 10.1007/s12603-018-1139-9, PMID: [DOI] [PubMed] [Google Scholar]
- 17.Ren X, Zhang X, He Q, du L, Chen K, Chen S, et al. Prevalence of sarcopenia in Chinese community-dwelling elderly: a systematic review. BMC Public Health. (2022) 22:1702. doi: 10.1186/s12889-022-13909-z, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xin C, Sun X, Lu L, Shan L. Prevalence of sarcopenia in older Chinese adults: a systematic review and meta-analysis. BMJ Open. (2021) 11:e041879. doi: 10.1136/bmjopen-2020-041879, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen Z, Li WY, Ho M, Chau PH. The prevalence of sarcopenia in Chinese older adults: meta-analysis and meta-regression. Nutrients. (2021) 13:1441. doi: 10.3390/nu13051441, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. (2015) 4:1. doi: 10.1186/2046-4053-4-1, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zeng XT, Liu H, Chen X, Leng WD. Meta-analysis series IV: quality evaluation tools for observational studies. Chinese J Evid Based Cardiovasc Med. (2012) 4:297–9. doi: 10.3969/j.1674-4055.2012.04.004 [DOI] [Google Scholar]
- 22.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21:1539–58. doi: 10.1002/sim.1186, PMID: [DOI] [PubMed] [Google Scholar]
- 23.Easterbrook PJ, Gopalan R, Berlin JA, Matthews DR. Publication bias in clinical research. Lancet. (1991) 337:867–72. doi: 10.1016/0140-6736(91)90201-Y [DOI] [PubMed] [Google Scholar]
- 24.Wang J, Hu L, Yang Z, Han P. Cross-sectional investigation on the prevalence and risk factors of sarcopenia in elderly people in some areas of Yunnan-Guizhou plateau. J Tissue Eng. (2024) 28:2197–201. doi: 10.12307/2024.330 [DOI] [Google Scholar]
- 25.Dai S, Wang S, He Y, Dai C, Yu J, Ma X. Association between anemia and sarcopenia among Chinese elderly: a cross-sectional study based on the China health and retirement longitudinal study. Exp Gerontol. (2023) 177:112183. doi: 10.1016/j.exger.2023.112183, PMID: [DOI] [PubMed] [Google Scholar]
- 26.Wan R, Shang Y, Wan Y, Zhao SH. Study on incidence and influencing factors of inpatients with sarcopenia based on body composition analysis. Chinese J Geriatr Med. (2023) 21:59–63. doi: 10.3969/j.issn.1672-2671.2023.04.012 [DOI] [Google Scholar]
- 27.Zou HY, Wang YH, Gao M, Li GD, Gao LS, Ma ZZ. Status and influencing factors of sarcopenia among elderly people in the community. J Pract Gerontol. (2023) 37:246–50. doi: 10.3969/j.issn.1003-9198.2023.03.009 [DOI] [Google Scholar]
- 28.Ma JD, Wang L, Cai TT, Jiao XF, Chen QP. Status and influencing factors of sarcopenia in inpatients with abdominal surgery. Chinese J Gen Surg. (2023) 17:69–74. doi: 10.3877/cma.j.issn.1674-0793.2023.01.015 [DOI] [Google Scholar]
- 29.Chen JW, Li ZY, Peng K, Xiao L, Liu X. Prevalence and prediction model construction of sarcopenia among elderly people in Xiangtan City. Chinese J Geriatr Multi Organ Dis. (2019) 22:663–8. doi: 10.11915/j.issn.1671-5403.2023.09.139 [DOI] [Google Scholar]
- 30.Musha TJGL, Maimaitiwusiman ZY, Bai X, Xiang H, Wang HM. Investigation of sarcopenia in the aged natural population. China Sci Technol J Database Med. (2023) 12:13–6. [Google Scholar]
- 31.He X, Song Y, Ma L, Ainsworth BE, Liu Y, Chen N. Prevalence and factors influencing sarcopenia among community-dwelling older adults using the Asian working Group for Sarcopenia Definition. Clin Interv Aging. (2022) 17:1707–27. doi: 10.2147/CIA.S388319, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhong J, Xie W, Wang X, Dong X, Mo Y, Liu D, et al. The prevalence of sarcopenia among Hunan Province community-dwelling adults aged 60 years and older and its relationship with lifestyle: diagnostic criteria from the Asian working Group for Sarcopenia 2019 update. Medicina. (2022) 58:1562. doi: 10.3390/medicina58111562, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tang J, Zhang LN, Gerile WY, Geer DL. Prevalence and related factors of sarcopenia among elderly people in Inner Mongolia. Nursing. (2022) 11:753–62. doi: 10.12677/NS.2022.116117 [DOI] [Google Scholar]
- 34.Han T, Qian XF, Wang QF, Cheng XC, Guo JM, Xiao JQ. Analysis of influencing factors on the risk of sarcopenia in elderly hospitalized patients based on logistic regression and decision tree model. J Nurs. (2022) 29:56–62. doi: 10.16460/j.issn1008-9969.2022.12.056 [DOI] [Google Scholar]
- 35.Li DH, Tian XF, Ma HM, Zhang KX, Liu HB, Zhang HT, et al. Prevalence and influencing factors of sarcopenia among elderly people in Tianjin. Chinese Convalescent Medicine. (2022) 31:633–7. doi: 10.13517/j.cnki.ccm.2022.06.022 [DOI] [Google Scholar]
- 36.Zhang XL. Status and influencing factors of sarcopenia in the elderly of Bai nationality in Wanqiao town, Dali University. (2022). doi: 10.27811/d.cnki.gdixy.2022.000206 [DOI]
- 37.Li CC, Zhang FY, Wang X, Yu LX, Wang L, Fu ML. Investigation and analysis of incidence, TCM syndrome type distribution and influencing factors of sarcopenia in some areas of Zhejiang Province. Chinese Modern Doctor. (2022) 60:14–17+22. [Google Scholar]
- 38.Ko YC, Chie WC, Wu TY, Ho CY, Yu WR. A cross-sectional study about the relationship between physical activity and sarcopenia in Taiwanese older adults. Sci Rep. (2021) 11:11488. doi: 10.1038/s41598-021-90869-1, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chang CF, Yeh YL, Chang HY, Tsai SH, Wang JY. Prevalence and risk factors of sarcopenia among older adults aged ≥65 years admitted to Daycare Centers of Taiwan: using AWGS 2019 guidelines. Int J Environ Res Public Health. (2021) 18:8299. doi: 10.3390/ijerph18168299, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pan SQ, Li YM, Li XF, Xiong R. Sarcopenia in geriatric patients from the plateau region of Qinghai-Tibet: a cross-sectional study. World J Clin Cases. (2021) 9:5092–101. doi: 10.12998/wjcc.v9.i19.5092, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhang TY, Mo YZ, Ouyang XJ, Pan XD, Wang J, Shen XX, et al. Prevalence and related factors of sarcopenia in hospitalized elderly patients. J Gerontol Health Care. (2021) 27:64–7. doi: 10.3969/j.issn.1008-8296.2021.01.016 [DOI] [Google Scholar]
- 42.Liu X, Hou L, Xia X, Liu Y, Zuo Z, Zhang Y, et al. Prevalence of sarcopenia in multi ethnics adults and the association with cognitive impairment: findings from West-China health and aging trend study. BMC Geriatr. (2020) 20:63. doi: 10.1186/s12877-020-1468-5, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yang L, Yao X, Shen J, Sun G, Sun Q, Tian X, et al. Comparison of revised EWGSOP criteria and four other diagnostic criteria of sarcopenia in Chinese community-dwelling elderly residents. Exp Gerontol. (2020) 130:110798. doi: 10.1016/j.exger.2019.110798 [DOI] [PubMed] [Google Scholar]
- 44.Chen S, Yu J, Di WJ, Lin W, Sheng YL, Zhu QQ. Epidemiological investigation and influencing factors of senile sarcopenia in Nanjing community. Pract Gerontol. (2020) 34:793–6. doi: 10.3969/j.issn.1003-9198.2020.08.010 [DOI] [Google Scholar]
- 45.Xu TY, Xu XH, Zhang R. Correlation analysis of serum 25-hydroxyvitamin D level and sarcopenia in elderly patients. J Gerontol Health Care. (2020) 26:976–9. doi: 10.3969/j.issn.1008-8296.2020.06.021 [DOI] [Google Scholar]
- 46.Liang YH, Xue L, Gao YY, Hou YP, Wang XJ. Analysis of sarcopenia in elderly hospitalized patients and its influencing factors. Chin J Gerontol. (2020) 39:1042–5. doi: 10.3760/cma.j.issn.0254-9026.2020.09.012 [DOI] [Google Scholar]
- 47.Meng XY. Status and influencing factors of sarcopenia in the elderly: a case study of the elderly in Xinxiang City, Xinxiang Medical College. (2020). doi: 10.27434/d.cnki.gxxyc.2020.000127 [DOI] [Google Scholar]
- 48.Che YJ, Yang XX, Zhang K, Wang YN, Wang YS, Yan P. Prevalence and related factors of sarcopenia among elderly people in Urumqi city. Chinese J Osteoporosis Bone Min Salt Dis. (2019) 13:304–10. doi: 10.3969/j.issn.1674-2591.2020.04.004 [DOI] [Google Scholar]
- 49.Tian XL, Yang L, Shen J, Li XX, Li X, Xiao H. Prevalence and influencing factors of sarcopenia among middle-aged and elderly in Midong District community of Urumqi City. Chinese J Osteoporosis Bone Mineral Salt Dis. (2020) 13:21–6. doi: 10.3969/j.issn.1674-2591.2020.01.004 [DOI] [Google Scholar]
- 50.Yang LJ, Wu GH, Yang YL, Wu YH, Zhang L, Wang MH, et al. Nutrition, physical exercise, and the prevalence of sarcopenia in elderly residents in nursing homes in China. Med Sci Monitor. (2019) 25:4390–9. doi: 10.12659/MSM.914031, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yao SH. Prevalence, risk factors and correlation analysis of sarcopenia and osteoporosis in elderly hospitalized patients. (2019).
- 52.Liu LL, Zhao KX, Luo C, Xiao Q, Zhou J. Prevalence and risk factors of sarcopenia among middle-aged and elderly people in Chongqing city. Chinese Gen Med. (2019) 17:1762–7. doi: 10.16766/j.cnki.issn.1674-4152.001050 [DOI] [Google Scholar]
- 53.He QH, Sun M, Yue YF, Wang XZ, Jing HJ, Yang CZ. Prevalence of sarcopenia in middle-aged and elderly patients with type 2 diabetes mellitus in Beijing and its influencing factors. Chinese J Diabetes. (2019) 11:328–33. doi: 10.3760/cma.j.issn.1674-5809.2019.05.004 [DOI] [Google Scholar]
- 54.Hao Q, Hu X, Xie L, Chen J, Jiang J, Dong B, et al. Prevalence of sarcopenia and associated factors in hospitalised older patients: a cross-sectional study. Australas J Ageing. (2018) 37:62–7. doi: 10.1111/ajag.12492 [DOI] [PubMed] [Google Scholar]
- 55.Zeng Y, Hu X, Xie L, Han Z, Zuo Y, Yang M. The prevalence of sarcopenia in Chinese elderly nursing home residents: a comparison of 4 diagnostic criteria. J Am Med Dir Assoc. (2018) 19:690–5. doi: 10.1016/j.jamda.2018.04.015 [DOI] [PubMed] [Google Scholar]
- 56.Zhang Y, Tan YT, Huang XX, Zhang ZH, Bai JJ, Zhang M, et al. Prevalence and related risk factors of sarcopenia among elderly people in Shanghai. J Gerontol Health Care. (2018) 24:608–13. doi: 10.3969/j.issn.1008-8296.2018.06.014 [DOI] [Google Scholar]
- 57.Wang YT, Hao QK, Su L, Hai S, Wang H, Cao L, et al. Study on the relationship between sarcopenia and impaired cognitive function in Chinese community elderly. J Sichuan Univ. (2018) 49:793–6. doi: 10.13464/j.scuxbyxb.2018.05.022 [DOI] [Google Scholar]
- 58.Yang LJ. Research on related factors of sarcopenia in the elderly in Suzhou City, Nanjing Medical University. (2018)
- 59.Liao SW, Liu LL, Zhao KX, Zhu QL, Luo C, Lv Q, et al. Prevalence of sarcopenia and related risk factors in nursing homes in Chongqing. Int J Gerontol. (2018) 39:1–5. doi: 10.3969/j.issn.1674-7593.2018.01.001 [DOI] [Google Scholar]
- 60.Wang YN, Xu JL, Song HL. Investigation and analysis of the status quo and influencing factors of sarcopenia in the elderly. Modern Clin Nurs. (2018) 17:45–50. doi: 10.3969/j.issn.1671-8283.2018.09.009 [DOI] [Google Scholar]
- 61.Hai S, Cao L, Wang H, Zhou J, Liu P, Yang Y, et al. Association between sarcopenia and nutritional status and physical activity among community-dwelling Chinese adults aged 60 years and older. Geriatr Gerontol Int. (2017) 17:1959–66. doi: 10.1111/ggi.13001, PMID: [DOI] [PubMed] [Google Scholar]
- 62.Hu X, Jiang J, Wang H, Zhang L, Dong B, Yang M. Association between sleep duration and sarcopenia among community-dwelling older adults: a cross-sectional study. Medicine. (2017) 96:e6268. doi: 10.1097/MD.0000000000006268, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Han P, Kang L, Guo Q, Wang J, Zhang W, Shen S, et al. Prevalence and factors associated with sarcopenia in suburb-dwelling older Chinese using the Asian working Group for Sarcopenia Definition. J Gerontol A Biol Sci Med Sci. (2016) 71:529–35. doi: 10.1093/gerona/glv108, PMID: [DOI] [PubMed] [Google Scholar]
- 64.Xia Z, Meng L, Man Q, Li L, Song P, Li Y, et al. Analysis of the dietary factors on sarcopenia in elderly in Beijing. J Hyg Res. (2016) 45:388–93. PMID: [PubMed] [Google Scholar]
- 65.Gao L, Jiang J, Yang M, Hao Q, Luo L, Dong B. Prevalence of sarcopenia and associated factors in Chinese community-dwelling elderly: comparison between rural and urban areas. J Am Med Dir Assoc. (2015) 16:1003.e1–6. doi: 10.1016/j.jamda.2015.07.020 [DOI] [PubMed] [Google Scholar]
- 66.Meng NH, Li CI, Liu CS, Lin CH, Lin WY, Chang CK, et al. Comparison of height-and weight-adjusted sarcopenia in a Taiwanese metropolitan older population. Geriatr Gerontol Int. (2015) 15:45–53. doi: 10.1111/ggi.12227, PMID: [DOI] [PubMed] [Google Scholar]
- 67.Wu CH, Chen KT, Hou MT, Chang YF, Chang CS, Liu PY, et al. Prevalence and associated factors of sarcopenia and severe sarcopenia in older Taiwanese living in rural community: the Tianliao old people study 04. Geriatr Gerontol Int. (2014) 14:69–75. doi: 10.1111/ggi.12233, PMID: [DOI] [PubMed] [Google Scholar]
- 68.Yu R, Wong M, Leung J, Lee J, Auyeung TW, Woo J. Incidence, reversibility, risk factors and the protective effect of high body mass index against sarcopenia in community-dwelling older Chinese adults. Geriatr Gerontol Int. (2014) 14:15–28. doi: 10.1111/ggi.12220, PMID: [DOI] [PubMed] [Google Scholar]
- 69.Anker SD, Morley JE, Von Haehling S. Welcome to the ICD-10 code for sarcopenia. J Cachexia Sarcopenia Muscle. (2016) 7:512–4. doi: 10.1002/jcsm.12147, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Diz JB, Leopoldino AA, Moreira BS, Henschke N, Dias RC, Pereira LS, et al. Prevalence of sarcopenia in older Brazilians: a systematic review and meta-analysis. Geriatr Gerontol Int. (2017) 17:5–16. doi: 10.1111/ggi.12720, PMID: [DOI] [PubMed] [Google Scholar]
- 71.Laakkonen EK, Soliymani R, Lalowski M. Estrogen regulates muscle bioenergetic signaling. Aging. (2018) 10:160–1. doi: 10.18632/aging.101380, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Shimokata H, Ando F, Yuki A, Otsuka R. Age-related changes in skeletal muscle mass among community-dwelling Japanese: a 12-year longitudinal study. Geriatr Gerontol Int. (2014) 14:85–92. doi: 10.1111/ggi.12219, PMID: [DOI] [PubMed] [Google Scholar]
- 73.Papadopoulou SK, Tsintavis P, Potsaki P, Papandreou D. Differences in the prevalence of sarcopenia in community-dwelling, nursing home and hospitalized individuals. A systematic review and meta-analysis. J Nutr Health Aging. (2020) 24:83–90. doi: 10.1007/s12603-019-1267-x, PMID: [DOI] [PubMed] [Google Scholar]
- 74.Mao S, Zhao A, Zhang J, Wang M, Wang Y, Meng L, et al. Association between dietary energy and protein intake and sarcopenia among the elderly in 8 cities across China. J Hyg Res. (2021) 50:242–55. doi: 10.19813/j.cnki.weishengyanjiu.2021.02.013, PMID: [DOI] [PubMed] [Google Scholar]
- 75.Ji CH, Pei HL, Li Y, Jiang Y, Luo ZH. Influencing factors and correlation of dietary patterns on sarcopenia in middle-aged and elderly people in Xinjiang. Chinese J Food Nutr. (2019) 28:73–9. doi: 10.19870/j.cnki.11-3716/ts.2022.10.006 [DOI] [Google Scholar]
- 76.Pang BWJ, Wee SL, Lau LK, Jabbar KA, Seah WT, Ng DHM, et al. Prevalence and associated factors of sarcopenia in Singaporean adults-the Yishun study. J Am Med Dir Assoc. (2021) 22:885.e1–885.e10. doi: 10.1016/j.jamda.2020.05.029 [DOI] [PubMed] [Google Scholar]
- 77.Khongsri N, Tongsuntud S, Limampai P, Kuptniratsaikul V. The prevalence of sarcopenia and related factors in a community-dwelling elders Thai population. Osteoporosis Sarcopenia. (2016) 2:110–5. doi: 10.1016/j.afos.2016.05.001, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Trevisan C, Vetrano DL, Calvani R, Picca A, Welmer AK. Twelve-year sarcopenia trajectories in older adults: results from a population-based study. J Cachexia Sarcopenia Muscle. (2022) 13:254–63. doi: 10.1002/jcsm.12875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wu LC, Kao HH, Chen HJ, Huang PF. Preliminary screening for sarcopenia and related risk factors among the elderly. Medicine. (2021) 100:e25946. doi: 10.1097/MD.0000000000025946, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Locquet M, Bruyère O, Lengelé L, Reginster JY, Beaudart C. Relationship between smoking and the incidence of sarcopenia: the SarcoPhAge cohort. Public Health. (2021) 193:101–8. doi: 10.1016/j.puhe.2021.01.017 [DOI] [PubMed] [Google Scholar]
- 81.Kim JY, Oh S, Park HY, Jun JH, Kim HJ. Author correction: comparisons of different indices of low muscle mass in relationship with cardiometabolic disorder. Sci Rep. (2020) 10:750. doi: 10.1038/s41598-020-57828-8, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Mackenbach JP, Damhuis RA, Been JV. The effects of smoking on health: growth of knowledge reveals even grimmer picture. Ned Tijdschr Geneeskd. (2017) 160:D869. [PubMed] [Google Scholar]
- 83.Olgun Yazar H, Yazar T. Prevalence of sarcopenia in patients with geriatric depression diagnosis. Ir J Med Sci. (2019) 188:931–8. doi: 10.1007/s11845-018-01957-7 [DOI] [PubMed] [Google Scholar]
- 84.Byeon CH, Kang KY, Kang SH, Kim HK, Bae EJ. Sarcopenia is not associated with depression in Korean adults: results from the 2010-2011 Korean National Health and nutrition examination survey. Korean J Fam Med. (2016) 37:37–43. doi: 10.4082/kjfm.2016.37.1.37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Zhang XT, Wang Y, Li L. Research status of the relationship between et al inflammatory factors and other depression-related factors. Chinese J Clin Pharmacol. (2018) 34:2568–71. doi: 10.13699/j.cnki.1001-6821.2018.21.024 [DOI] [Google Scholar]
- 86.Yang Q, Chan P. Skeletal muscle metabolic alternation develops sarcopenia. Aging Dis. (2022) 13:801–14. doi: 10.14336/AD.2021.1107, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Huang HX, Shi XL, Li SH, et al. Expert consensus on sarcopenia and osteoporosis. Chinese J Osteoporosis. (2022) 28:1561–70. doi: 10.3969/j.issn.1006-7108.2022.11.001 [DOI] [Google Scholar]
- 88.Papadopoulou SK, Papadimitriou K, Voulgaridou G, Georgaki E, Tsotidou E, Zantidou O, et al. Exercise and nutrition impact on osteoporosis and sarcopenia-the incidence of osteosarcopenia: a narrative review. Nutrients. (2021) 13:4499. doi: 10.3390/nu13124499, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Maurel DB, Jähn K, Lara-Castillo N. Muscle-bone crosstalk: emerging opportunities for novel therapeutic approaches to treat musculoskeletal pathologies. Biomedicines. (2017) 5:62. doi: 10.3390/biomedicines5040062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Lin X, Hanson E, Betik AC, Brennan-Speranza TC, Hayes A, Levinger I. Hindlimb immobilization, but not castration, induces reduction of undercarboxylated osteocalcin associated with muscle atrophy in rats. J Bone Miner Res Off J Am Soc Bone Miner Res. (2016) 31:1967–78. doi: 10.1002/jbmr.2884, PMID: [DOI] [PubMed] [Google Scholar]
- 91.Chew STH, Tey SL, Yalawar M, Liu Z, Baggs G, How CH, et al. Prevalence and associated factors of sarcopenia in community-dwelling older adults at risk of malnutrition. BMC Geriatr. (2022) 22:997. doi: 10.1186/s12877-022-03704-1, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Chen LK, Woo J, Assantachai P, Auyeung TW, Chou MY, Iijima K, et al. Asian working Group for Sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc. (2020) 21:300–307.e2. doi: 10.1016/j.jamda.2019.12.012 [DOI] [PubMed] [Google Scholar]
- 93.Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. (2019) 48:601. doi: 10.1093/ageing/afz046, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Volpato S, Bianchi L, Cherubini A, Landi F, Maggio M, Savino E, et al. Prevalence and clinical correlates of sarcopenia in community-dwelling older people: application of the EWGSOP definition and diagnostic algorithm. J Gerontol A Biol Sci Med Sci. (2014) 69:438–46. doi: 10.1093/gerona/glt149, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Prado CM, Landi F, Chew STH, Atherton PJ, Molinger J, Ruck T, et al. Advances in muscle health and nutrition: a toolkit for healthcare professionals. Clin Nutr. (2022) 41:2244–63. doi: 10.1016/j.clnu.2022.07.041, PMID: [DOI] [PubMed] [Google Scholar]
- 96.Chae SA, Kim HS, Lee JH, Yun DH, Chon J, Yoo MC, et al. Impact of vitamin B12 insufficiency on sarcopenia in community-dwelling older Korean adults. Int J Environ Res Public Health. (2021) 18:12433. doi: 10.3390/ijerph182312433, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Dzik KP, Kaczor JJ. Mechanisms of vitamin D on skeletal muscle function: oxidative stress, energy metabolism and anabolic state. Eur J Appl Physiol. (2019) 119:825–39. doi: 10.1007/s00421-019-04104-x, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Skipper A, Coltman A, Tomesko J, Charney P, Porcari J, Piemonte TA, et al. Adult malnutrition (undernutrition) screening: an evidence analysis Center systematic review. J Acad Nutr Diet. (2020) 120:669–708. doi: 10.1016/j.jand.2019.09.010, PMID: [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The detailed information of literature retrieval strategy.
The detailed results of literature evaluation.
The general information of included literature.
The corresponding PRISMA checklist.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.