Abstract
Abstract
Introduction
With digital and social media advances, animated health communications (health animations) are highly prevalent globally, yet the evidence base underpinning them remains unclear and limited. While individual studies have attempted to explore the effectiveness, acceptability and usability of specific features of health animations, there is substantial heterogeneity in study design, comparators and the animation design and content. Consequently, there is a need to synthesise evidence of health animations using an approach that recognises this contextual complexity, which may affect their impact.
Methods and analysis
This project aims to understand why, how, for whom, to what extent and in which contexts health animations are expected to promote preventive health behaviours. We will conduct a realist review following Pawson’s five iterative stages to (1) define the review scope and locate existing theories; (2) search for evidence; (3) select and appraise evidence; (4) extract data and (5) synthesise data and refine theory. Engagement with stakeholders involved in developing, testing, implementing or commissioning health communications, including animations, will allow the initial programme theory to be tested and refined. The findings will be reported in accordance with Realist and Meta-narrative Evidence Syntheses: Evolving Standards.
Ethics and dissemination
Ethical approval for the public stakeholder work was provided by the Northumbria University Research Ethics Committee. We will disseminate the findings widely through outputs tailored to target specific professional, public and patient audiences. Dissemination will occur through stakeholder engagement as part of the research, a peer-reviewed publication and conference presentations.
PROSPERO registration number
CRD42023447127.
Keywords: Health Literacy, PUBLIC HEALTH, PREVENTIVE MEDICINE, Behavior
Strengths and limitations of this study.
The realist review approach will allow the contextual complexity of health animations to be explored, drawing on evidence from published and grey literature from multiple disciplines.
Stakeholder engagement by professionals from different backgrounds (public health, government, voluntary sector, health professional, design and academic) will allow the initial programme theory to be tested and refined from multiple perspectives.
The methodological approach will cut across linguistic, cultural and geographic boundaries.
There is a modest literature pool in this emerging field, necessitating the use of broad inclusion criteria to capture the breadth of animation types and uses.
Introduction
The individual, societal and economic costs of preventable ill health and disease are significant, accounting for between a quarter and a half of the burden on health and social care and deaths globally.1,3 Modifiable behavioural risk factors such as sedentary behaviour, unhealthy diet, not attending health screenings and high-risk sexual behaviours contribute to the increasing global burden of ill health and disease.4 Public health communication science can play a crucial role in ensuring that accurate and accessible health messages are communicated to individuals, communities and populations to promote health and health behaviours and reduce morbidity and mortality.5 Health literacy—the knowledge and competencies needed to access, understand and use information to promote health6—is critical to the effectiveness of these communications. Studies have found that poor health literacy relates to less healthy behaviours, worse health outcomes and health inequalities.7 Disadvantaged groups, including those with local language and cultural barriers, face additional health literacy barriers,8 and therefore, the transmission of public health messages that do not rely on language or text can help to address these barriers.
Make it visual
‘Make it visual’ is one of four tactics set out within the WHO Strategic Communications Framework to apply to make health communications understandable.9 Underpinning this is evidence from (1) cognitive psychology demonstrating that visual information is more memorable than textual information (Picture Superiority Effect)10 and (2) reviews of health communication using pictures, which have concluded that knowledge, understanding, attention and recall are improved when pictures are used compared with using text alone.11 12 Importantly, these effects are robust and extend to those who may find text-only information more challenging, for example, individuals who lack literacy skills12 and those with cognitive impairment.13
Digital advances, together with evidence from literature outside of health that demonstrates the benefits to learning and cognitive load of animations14 (a simulated motion picture depicting the movement of drawn (or simulated) objects15) compared with static pictures, have resulted in visual health communications commonly adopting an animated format to digitally deliver health messages using moving pictures and either complementing or replacing written text. These animations can be made using traditional animation or other techniques (eg, three-dimensional, whiteboard and stop motion) and can be formatted in multiple ways, including video, Graphics Interchange Format and Animated Portable Network Graphics. Consequently, animated health communications (hereafter referred to as health animations) have the potential to be easily and widely shared via the internet, apps and social media, which, in turn, has catalysed their widespread global application to deliver public health information and promote health behaviour change.
Current evidence base for health animations
Despite the increasing use and potential reach of health animations, the evidence base underpinning them remains unclear, partly due to the significant differences between study designs and comparators. For example, one study of polio vaccination messages found that animated messages led to greater improvement of health knowledge when compared with written messages,16 whereas a study of colorectal screening messages found that only when animated messages were combined with spoken text was greater message recall observed in people with low health literacy.17 This lack of clarity also somewhat stems from a lack of research into what elements and features of videos, including health animations, are most engaging and impactful in delivering health messages.18 This gap in research is noted in a WHO case study of a highly viewed and award-winning health animation by the Global Health Media Project that communicated information about COVID-19 transmission during the pandemic. Even though the case study describes the features of the animation and how the content was informed by science, the animation has not been formally evaluated.19
A recent systematic review has synthesised literature specifically in relation to the effectiveness of video animations as information tools when compared with other formats of delivery and concluded that video animations over other formats have promise to improve knowledge but that the evidence is highly variable.20 Similarly, a recent review and meta-analysis of the effectiveness of animated videos on patient learning concluded that animated videos can improve patient knowledge over a range of health and clinical contexts.21 Evidence from health animations designed to promote public health preventive behaviours more broadly has yet to be reviewed.
Within the literature, not only are there significant differences between studies of health animations in terms of the study design and comparators, but there are also significant differences between the design and content features of the animations themselves, including the length, tone, number of messages, health context, target audience and use of text, language, sound and behaviour change theory. The use of cultural identifiers in the characters and settings and voiceovers in local languages and accents have also been considered in health animation design.22 One such health animation, ‘The Magic Glasses’, was developed as part of a larger intervention for Chinese schoolchildren to prevent soil-transmitted helminth infection.23 The 12-min animation is in narrative form with cultural identifiers in the characters, settings, language and music, and has also been culturally adapted for use in the Philippines. Contrastingly, a health animation where the intended audience was global was designed to have no cultural indicators, be wordless and have featureless characters.24 This 2-min 30-s animation was able to successfully increase knowledge and intentions for preventive behaviours, such as hand hygiene, during the COVID-19 pandemic across cultures. Given the heterogeneity and contextual complexity of health animations, syntheses of studies need to recognise the different factors or contexts that may affect their impact. Additionally, as health animations have not always been formally evaluated, it could be helpful to look beyond published research at other sources of information to be able to uncover the specific causal mechanisms being triggered that facilitate certain outcomes.
Therefore, we will use a realist review approach to understand why, how, for whom, to what extent and in which contexts health animations are expected to produce their effects. We will not consider health animations to be uniform but rather identify the underlying and context-sensitive causal mechanisms and the specific outcome(s) affected by these mechanisms. In doing so, we will generate knowledge about the causes of outcomes in particular circumstances in terms of context-mechanism-outcome configurations (CMOCs) of realist reviews and syntheses. When considering CMOCs, a useful heuristic can be to ask ‘if, then, because’ where ‘if’ identifies the context, ‘then’ the outcome, and ‘because’ the mechanism.25 These CMOCs will become part of an initial programme theory of health animations to be tested and refined, ultimately informing recommendations for the design of health animations.
In line with global agendas on the prevention and control of communicable and non-communicable diseases, we will focus this realist review on studies of health animations that have been designed to promote public health behaviours through primary, secondary or tertiary prevention. Such behaviours include lifestyle (eg, being more physically active and stopping smoking), hygiene (eg, handwashing to reduce the chance of spreading infectious diseases) and attending preventive health appointments (eg, screenings and health checks). We will not focus on animations designed to treat illness and disease, which are more likely to adopt a clinical rather than public health angle.
Aim and review questions
We aim to identify and synthesise evidence about health animations to inform the development of hypotheses and an initial programme theory and to answer the following review questions:
What are the mechanisms by which health animations are believed to result in the intended outcomes?
In what contexts are mechanisms being triggered to produce the intended outcomes?
Why do these mechanisms work to promote preventive health behaviours?
What CMOCs are at work?
Methods and analysis
Realist review stages
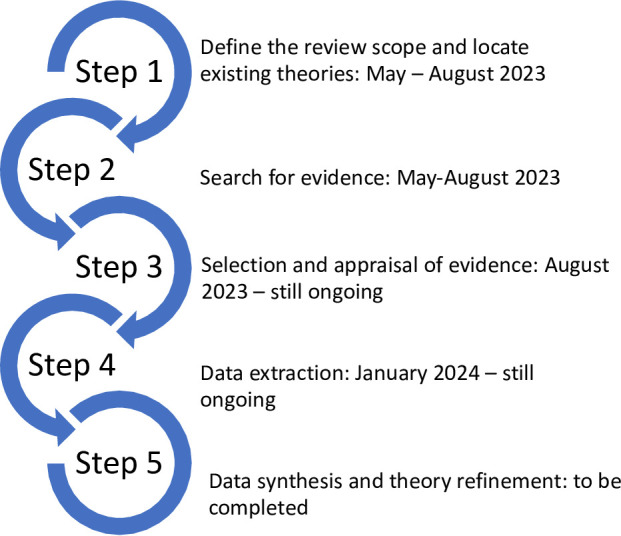
This realist review protocol has been guided by Pawson’s five iterative stages of a realist review,26 27 including involving stakeholders in the review to test and refine the initial programme theory. The review stages and a timeline are detailed in figure 1. The protocol has been registered with the International Prospective Register of Systematic Reviews: CRD42023447127. The findings will be reported in accordance with Realist and Meta-narrative Evidence Syntheses: Evolving Standards (RAMESES) quality and publication standards.28
Figure 1. Review stages with a timeline.
Patient and public involvement
We will explore engaging with a range of stakeholders during the review, recruited from within the research team’s international and UK networks. We will conduct online workshops with international professional stakeholders to test and validate the initial programme theory by bringing together different voices and perspectives from across systems and around particular services or interventions. These professional stakeholders will have expertise and/or an interest in developing, testing, implementing or commissioning health communications, including animations and improving health literacy. Stakeholders will have public health, government, voluntary sector, health professional, design and academic backgrounds.
We will also conduct in-person or online workshops with public and community stakeholders in the UK to sense-check our refined programme theory and to co-design recommendations for the future design of health animations.
Step 1: define the review scope and locate existing theories
The first step in a realist review is to define the review scope, identify the review question and identify key theories and models. In defining the review scope, we conducted exploratory literature searches on PubMed and Google Scholar using keywords to identify reviews of health communication interventions and approaches, inclusive of animated formats of delivery and primary studies on health animations specifically. Consequently, the scope of the review was defined to include evaluations of health animations targeting children and young people (under 18 years old) in addition to those targeting adult populations and to not place any restrictions on the dates when the evaluations were conducted or published. Identified primary studies confirmed that health animations have been used in a variety of different contexts and for a range of different public health purposes. In accordance with realist review guidance and its iterative processes, the scope of the review may be refined further at later stages.29
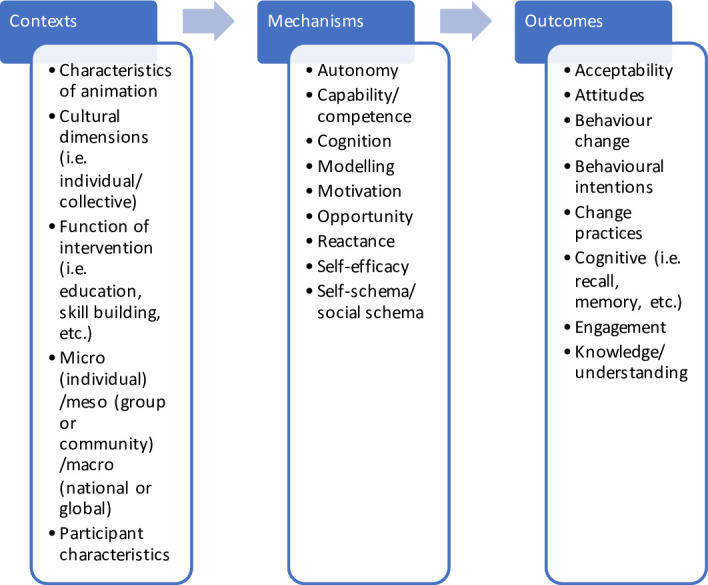
We conducted a further exploratory search of the literature to locate existing theories and models within a range of academic disciplines, such as psychology and behavioural science, education, design, communication science and sociology (figure 2). We were looking for theories to help us explain how, when and for whom health animations are expected to work (or not work) in terms of the potential mechanisms being triggered to produce the intended outcomes. The identified theories and models formed the basis of the initial programme theory (figure 3) to be tested in relation to the studies identified in the review and by stakeholders in later stages.
Figure 2. Academic disciplines with example theories and models to inform the initial programme theory.
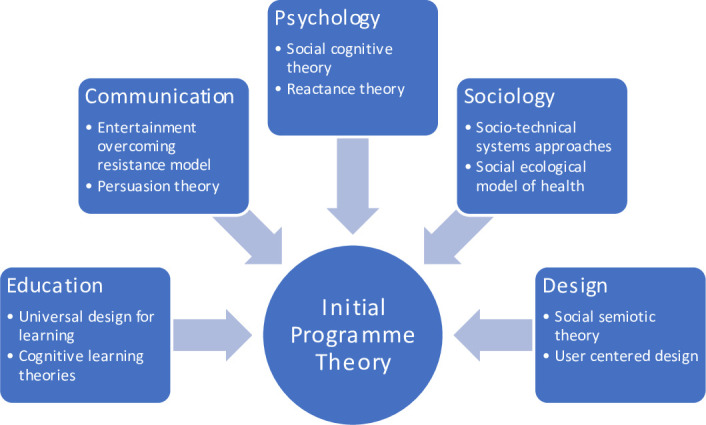
Figure 3. Draft initial programme theory showing potential contexts, mechanisms and outcomes. At this point and in this figure, no context, mechanism or outcome configurations are suggested or displayed.
Step 2: search for evidence
To identify studies to test the initial programme theory, we are conducting a formal, systematic search. The searches have been designed, piloted and conducted by an information specialist (LE) in collaboration with the research team. These searches were initially conducted on 10 July 2023. The search strategy (see online supplemental material) combines relevant terms for concepts of animation, health behaviour and behaviour change. Databases have been searched since inception (MEDLINE, Scopus, CINAHL, EMBASE, PsycINFO, Proquest Social Science, Web of Science and the Cochrane Library), plus supplementary searches of key non-indexed journals and reference lists. We are also contacting known academic experts and searching organisation websites, such as the WHO, UNICEF, the Centres for Disease Control and Prevention and relevant non-governmental organisations, to identify other published and grey literature (unpublished reports or documents). As required, additional searches will be conducted at later stages to further test and develop the initial programme theory, as per realist review guidance.
The screening process began with title and abstract screening by one reviewer (KMC) and a random 10% sample independently screened by a second reviewer (NO’B). Full-text screening will be conducted by two independent reviewers (KMC and NO’B), with a third reviewer (GM) providing consensus in case of disagreement. In keeping with the iterative nature of the realist review methodology, papers not selected will be held in reserve in case they are later deemed to be relevant to an aspect of the programme theory (eg, a CMOC).
The following inclusion criteria will be applied, which are deliberately broad to capture all relevant evidence:
Population: all participants of any age where the animation has been designed to promote public health behaviours through primary, secondary or tertiary prevention.
Intervention: health communications (messages) that use animation (digital moving pictures) and have been designed to promote public health behaviours.
Comparators: other intervention, usual care, no intervention or no comparator.
Types of studies: all study designs.
Contexts: all contexts and settings.
Outcomes: all outcomes related to public health animations, including, but not limited to: health behaviour, behavioural cognition (attitude, intention, self-efficacy, etc), knowledge, awareness, opinion, emotional response, cognition and memory.
Studies where the health animation has been designed to clinically treat illness and disease will be excluded so that this review can explore the contexts of health animations designed to promote preventive public health behaviours.
Step 3: selection and appraisal of evidence
In keeping with realist review methodology, as described in Pawson27 and the RAMESES publication standards,28 the usual hierarchy of evidence will not be applied, such that evidence from lower-quality studies will be considered in terms of its potential to make a valuable contribution to the development of the initial programme theory. Consistent with RAMESES training materials and quality standards,30 this review will consider full texts identified in step 2 in terms of relevance, richness and rigour.
Relevance—Does the evidence help develop CMOCs and contribute to their advancement? Is the building and testing of programme theory supported by this evidence? Does it speak to the research question?
Richness—Is there a sufficient level of description about the development of the intervention and the theories and concepts underpinning it? Was there discussion about factors that impacted the functioning or outcomes of the intervention? Were details provided about how the intervention was meant to work? Was this information general or specific to the intervention?
Rigour—What methods were used to generate the data? What are the credibility and trustworthiness of these methods?
Full texts will be selected for inclusion when they are deemed to provide knowledge that can help us develop and test the initial programme theory of the impact of health animations. Quality appraisal of evidence will initially occur during screening, considering relevance, richness and rigour separately. Further appraisal will occur later, alongside data extraction, when a more in-depth assessment is possible.
Step 4: data extraction
Data extraction will be performed by one reviewer (KMC) and checked by a second reviewer (NO’B). Data extraction will focus on data that support developing the initial programme theory and CMOCs, including information about the characteristics of the animations (length and use of colour, language, sound, characters, etc), the study sample, outcomes, findings and quality. To enable a more detailed examination of the design and content features of the health animations, we will contact the study authors to request a digital link to the health animation where it is not provided in the study/document. Bespoke data extraction forms will be created in Excel by the review team to record extracted data from quantitative, qualitative and mixed-method studies. The data extraction forms will be revised as required as the review progresses, in line with the iterative nature of realist reviews.
Step 5: data synthesis and theory refinement
In step 5, we will build CMOCs aiming to explain the outcomes resulting from the health animations that are reported in the included documents. Approaching the data from a realist perspective will include the use of retroduction, which involves inductive, deductive and instinctive reasoning as we search for causal mechanisms and their outcomes, looking to see how different contexts influence these configurations.31 We will conduct data synthesis and theory refinement as part of conversations between the review team. We will interrogate evidence and question the integrity of the programme theory by considering interpretations and judgements about data while recognising the appraisal of relevance, richness and rigour conducted in step 3. In so doing, we will explore whether each included data source can explain a particular CMOC fully or partially, whether data from other included sources can help inform this CMOC and how a particular CMOC relates to others already developed. In building theory to explain CMOCs, we will also pay attention to demi-regularities, or patterns of CMOCs that reoccur, potentially leading to the development of a more general theory speaking to these patterns should they emerge.29 Synthesis will also involve making judgements about data in relation to methodological strengths and weaknesses, considering CMOCs in different comparative settings and comparing official expectations with actual practice.
Ethics and dissemination
Ethical approval has been granted by the Northumbria University Research Ethics Committee for the stakeholder workshops with members of the public and community groups (reference #6803). Ethical approval for the professional stakeholder workshops was not required, as confirmed by the Northumbria University Research Ethics Committee, but informed participation will be sought.
We will disseminate findings through outputs tailored to specific audiences and with support from our stakeholders and the research team’s international and national networks. Subsequently, findings will be shared with a range of professional audiences, members of the public and patients, including the stakeholders already engaged with them.
supplementary material
Footnotes
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Prepublication history and additional supplemental material for this paper are available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2023-083013).
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not applicable.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Contributor Information
Kathleen McCorry, Email: katie.mccorry@uni-heidelberg.de.
Gregory Maniatopoulos, Email: gregory.maniatopoulos@leicester.ac.uk.
Linda Errington, Email: linda.errington@newcastle.ac.uk.
Ellie Land, Email: ellie_land@yahoo.co.uk.
Michael Craig, Email: michael2.craig@northumbria.ac.uk.
Santosh Vijaykumar, Email: SANTOSH.VIJAYKUMAR@NORTHUMBRIA.AC.UK.
Till Bärnighausen, Email: till.baernighausen@uni-heidelberg.de.
Nicola O'Brien, Email: nicki.obrien@northumbria.ac.uk.
References
- 1.The Health Foundation The health foundation - written evidence (NHS0172) 2016. https://www.parliament.uk/globalassets/documents/lords-committees/NHS-Sustainability/long-term-sustainability-nhs-committee-written-evidence.pdf Available.
- 2.Martinez R, Lloyd-Sherlock P, Soliz P, et al. Trends in premature avertable mortality from non-communicable diseases for 195 countries and territories, 1990-2017: a population-based study. Lancet Glob Health. 2020;8:e511–23. doi: 10.1016/S2214-109X(20)30035-8. [DOI] [PubMed] [Google Scholar]
- 3.Bolnick HJ, Bui AL, Bulchis A, et al. Health-care spending attributable to modifiable risk factors in the USA: an economic attribution analysis. Lancet Public Health. 2020;5:e525–35. doi: 10.1016/S2468-2667(20)30203-6. [DOI] [PubMed] [Google Scholar]
- 4.Murray CJL, Aravkin AY, Zheng P, et al. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1223–49. doi: 10.1016/S0140-6736(20)30752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bernhardt JM. Communication at the core of effective public health. Am J Public Health. 2004;94:2051–3. doi: 10.2105/ajph.94.12.2051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization Health literacy development for the prevention and control of noncommunicable diseases: volume 2. A globally relevant perspective. 2022. https://www.who.int/publications/i/item/9789240055353 Available.
- 7.Walters R, Leslie SJ, Polson R, et al. Establishing the efficacy of interventions to improve health literacy and health behaviours: a systematic review. BMC Public Health. 2020;20:1040. doi: 10.1186/s12889-020-08991-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vamos S, Okan O, Sentell T, et al. Making a Case for “Education for Health Literacy”: An International Perspective. Int J Environ Res Public Health. 2020;17:1436. doi: 10.3390/ijerph17041436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization World Health Organization strategic communications framework for effective communications. 2017. https://cdn.who.int/media/docs/default-source/documents/communication-framework.pdf Available.
- 10.Nelson DL, Reed VS, Walling JR. Pictorial superiority effect. J Exp Psychol Hum Learn. 1976;2:523–8. [PubMed] [Google Scholar]
- 11.Schubbe D, Scalia P, Yen RW, et al. Using pictures to convey health information: A systematic review and meta-analysis of the effects on patient and consumer health behaviors and outcomes. Pat Educ Couns. 2020;103:1935–60. doi: 10.1016/j.pec.2020.04.010. [DOI] [PubMed] [Google Scholar]
- 12.Houts PS, Doak CC, Doak LG, et al. The role of pictures in improving health communication: a review of research on attention, comprehension, recall, and adherence. Patient Educ Couns. 2006;61:173–90. doi: 10.1016/j.pec.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 13.Ally BA, Gold CA, Budson AE. The picture superiority effect in patients with Alzheimer’s disease and mild cognitive impairment. Neuropsychologia. 2009;47:595–8. doi: 10.1016/j.neuropsychologia.2008.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Höffler TN, Leutner D. Instructional animation versus static pictures: A meta-analysis. Learn Instr. 2007;17:722–38. doi: 10.1016/j.learninstruc.2007.09.013. [DOI] [Google Scholar]
- 15.Mayer RE, Moreno R. Animation as an Aid to Multimedia Learning. Educ Psychol Rev. 2002;14:87–99. doi: 10.1023/A:1013184611077. [DOI] [Google Scholar]
- 16.Leiner M, Handal G, Williams D. Patient communication: a multidisciplinary approach using animated cartoons. Health Educ Res. 2004;19:591–5. doi: 10.1093/her/cyg079. [DOI] [PubMed] [Google Scholar]
- 17.Meppelink CS, van Weert JCM, Haven CJ, et al. The effectiveness of health animations in audiences with different health literacy levels: an experimental study. J Med Internet Res. 2015;17:e11. doi: 10.2196/jmir.3979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Campbell IH, Rudan I. Effective approaches to public engagement with global health topics. J Glob Health. 2020;10:01040901. doi: 10.7189/jogh.10.010901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organization Case study. The story of coronavirus: using animation to help audiences understand COVID-19 transmission. 2022. https://cdn.who.int/media/docs/default-source/science-translation/case-studies-1/cs6_storyofcoronavirus.pdf?sfvrsn=2e3308f9_4 Available.
- 20.Moe-Byrne T, Evans E, Benhebil N, et al. The effectiveness of video animations as information tools for patients and the general public: A systematic review. Front Digit Health . 2022;4:1010779. doi: 10.3389/fdgth.2022.1010779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Feeley TH, Keller M, Kayler L. Using Animated Videos to Increase Patient Knowledge: A Meta-Analytic Review. Health Educ Behav. 2023;50:240–9. doi: 10.1177/10901981221116791. [DOI] [PubMed] [Google Scholar]
- 22.O’Brien N, Vijaykumar S, Craig M, et al. A pre- and post-intervention study testing the effect of exposure to languageless animated images communicating COVID-19 preventive behaviours on behavioural intentions and beliefs of Guatemalan adults. J Glob Health. 2022;12:05018. doi: 10.7189/jogh.12.05018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bieri FA, Gray DJ, Williams GM, et al. Health-education package to prevent worm infections in Chinese schoolchildren. N Engl J Med. 2013;368:1603–12. doi: 10.1056/NEJMoa1204885. [DOI] [PubMed] [Google Scholar]
- 24.Vandormael A, Adam M, Greuel M, et al. The Effect of a Wordless, Animated, Social Media Video Intervention on COVID-19 Prevention: Online Randomized Controlled Trial. JMIR Public Health Surveill. 2021;7:e29060. doi: 10.2196/29060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hunter R, Gorely T, Beattie M, et al. Realist review. Int Rev Sport Exerc Psychol. 2022;15:242–65. doi: 10.1080/1750984X.2021.1969674. [DOI] [Google Scholar]
- 26.Pawson R, Greenhalgh T, Harvey G, et al. Realist review--a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy. 2005;10 Suppl 1:21–34. doi: 10.1258/1355819054308530. [DOI] [PubMed] [Google Scholar]
- 27.Pawson R. Evidence-Based Policy: A Realist Perspective. London, UK: Sage Publications Ltd; 2006. [Google Scholar]
- 28.Wong G, Greenhalgh T, Westhorp G, et al. RAMESES publication standards: realist syntheses. BMC Med. 2013;11:21. doi: 10.1186/1741-7015-11-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wong G, Westhorp G, Pawson R, et al. Realist synthesis: RAMESES training materials. the RAMESES projects. Standards and training material. 2013. https://www.ramesesproject.org/media/Realist_reviews_training_materials.pdf Available.
- 30.Dada S, Dalkin S, Gilmore B, et al. Applying and reporting relevance, richness and rigour in realist evidence appraisals: Advancing key concepts in realist reviews. Res Synth Methods. 2023;14:504–14. doi: 10.1002/jrsm.1630. [DOI] [PubMed] [Google Scholar]
- 31.Greenhalgh T, Pawson R, Wong G, et al. Retroduction in realist evaluation: the RAMESES II project. 2017. https://www.ramesesproject.org/media/RAMESES_II_Retroduction.pdf Available.


