Abstract
Context:
The Centers for Disease Control and Prevention supports the engagement of community health workers (CHWs) to help vulnerable populations achieve optimum health through a variety of initiatives implemented in several organizational units.
Program:
This article provides a unified and comprehensive logic model for these initiatives that also serves as a common framework for monitoring and evaluation.
Implementation:
We developed a logic model to fully describe the levels of effort needed to effectively and sustainably engage CHWs. We mapped monitoring and evaluation metrics currently used by federally funded organizations to the logic model to assess the extent to which measurement and evaluation are aligned to programmatic efforts.
Evaluation:
We found that the largest proportion of monitoring and evaluation metrics (61%) currently used maps to the “CHW intervention level” of the logic model, a smaller proportion (37%) maps to the “health system and community organizational level,” and a minimal proportion (3%) to the “statewide infrastructure level.”
Discussion:
Organizations engaging CHWs can use the logic model to guide the design as well as performance measurement and evaluation of their CHW initiatives.
Keywords: chronic disease, community health workers, evaluation
Community health workers (CHWs), including promotores de Salud, community health representatives, patient navigators, and community health advisors, are frontline public health workers. The American Public Health Association defines CHWs as trusted members of the communities they serve or as having a close understanding of these communities. This quality enables them to serve as effective liaisons between community members and health and social service organizations, facilitating community members’ access to services and improving service quality and cultural competence.1 CHWs assist in preventing and managing conditions such as cardiovascular disease (CVD) and type 2 diabetes and improve cancer screening rates.2–7 CHW interventions can also reduce health disparities by addressing the social determinants of health, such as food security, housing, transportation, and child care.7–9
The Centers for Disease Control and Prevention (CDC) funds initiatives that engage CHWs to prevent and manage chronic conditions through several of its organizational units. These units use a variety of implementation approaches and monitoring and evaluation (M&E) metrics. While the units are able to successfully implement their own initiatives, there is an absence of an overarching framework for these initiatives. To address this gap, the authors sought to provide a unified approach for the design, measurement, and evaluation of these varied initiatives through a comprehensive logic model.
Methods
The authors conducted this study in 3 phases: (1) gathering and organizing M&E metrics currently used by various CDC organizational units; (2) developing a logic model; and (3) mapping M&E metrics to the logic model. A protocol approval by an ethics committee was not needed to conduct this study.
Phase 1: Gathering and organizing M&E metrics
The CDC’s National Center for Chronic Disease Prevention and Health Promotion funds state health departments, community-based organizations, and local health systems to engage CHWs in chronic disease prevention and control. We gathered 2 categories of M&E metrics—performance measures and evaluation metrics—from the authors’ organizational units supporting CHW initiatives focused on chronic conditions and underlying risk factors including cancer, diabetes, heart disease and stroke, obesity, and nutrition and physical activity. Performance measures are standard or uniform metrics developed by the CDC and used by all grantees to report on progress toward preestablished goals. Evaluation metrics are metrics uniquely identified by funded recipients to evaluate their CHW initiatives in a more in-depth way by focusing on the how and why of implementation success, facilitators, barriers, and challenges. While performance measures focus on outcome measures related to behavioral and health outcome changes, evaluation metrics focus on both process and outcome measures and may include proximal outcomes that precede behavioral and health outcome changes.
To organize these metrics, first, individual authors mapped metrics from their organizational units to the roles of CHWs as delineated in the following resources: the Community Health Worker Core Consensus (C3) Project10 and the Community Preventive Services Task Force reviews (the Community Guide) on engaging CHWs for the prevention of CVD and for the prevention and management of type 2 diabetes.2–4 The C3 Project identified 10 major roles that CHWs play,10 and the Community Guide identified 5 CHW roles that were effective in achieving outcomes for patients or clients2–4 (Table 1). Second, the authors reviewed the mappings as a group to resolve any different opinions among themselves and to select, as appropriate, a role for each metric.
TABLE 1.
Community Health Worker Roles
| Source | Roles |
|---|---|
| C3 Project10 | 1. Providing cultural mediation among individuals, communities, and health and social service systems 2. Providing culturally appropriate health education and information 3. Providing care coordination, case management, and system navigation 4. Providing coaching and social support 5. Advocating for individuals and communities 6. Building individual and community capacity 7. Providing direct service 8. Implementing individual and community assessments 9. Conducting outreach 10. Participating in evaluation and research |
|
| |
| Community Guide2–4 | 1. Screening and health education 2. Outreach, enrollment, and information 3. Team-based care 4. Patient navigation 5. Community organization |
Through this process, we found that while many of the compiled M&E metrics aligned to CHW roles, there were several metrics that could not be organized solely based on “CHW roles.” These included metrics that were related to health system and community-based organizational efforts to engage CHWs as well as some that were related to infrastructural components for building a sustainable workforce. To address this limitation, the authors agreed there was a need for a comprehensive tool, beyond the list of CHW roles, that could serve as a frame of reference for the complete compilation of M&E metrics. Through a process of iterative discussion and consideration of various approaches and options, we decided to use a logic model, as this offers a comprehensive visual depiction of a program, including the resources, activities under-taken, and the outcomes accomplished in the short, intermediate, and long terms. The authors are evaluators and program and policy staff members who have effectively used logic models to describe programs and as a frame of reference for evaluation.
Phase 2: Developing a logic model
We developed a logic model through a 2-part process comprising a brief phase of reviewing pertinent literature and an extended phase of building the logic model. We began by conducting a literature search for existing logic models that describe engaging CHWs. Our initial goal was to identify a model that could adequately reflect CHW initiatives supported across our organizational units. We found several models relating to CHW initiatives in governmental, nonprofit, and international organizations and addressing a variety of disease conditions.11–18 These models had overlapping content, especially in terms of articulating activities undertaken by CHWs or CHW roles and resulting behavioral changes and health outcome changes among program participants and patients in health systems. Several reflected specific areas of focus such as a trained CHW workforce,13 factors affecting CHW performance such as health system and intervention design factors and mediating processes,15 and factors affecting the availability of CHWs.12 One of these models broadly resonated with our understanding of activities and outcomes at the health systems, population, and participant levels and included a “policy” component, critical for the sustainable engagement of CHWs.17 However, several modifications were needed for this model to be a comprehensive and accurate representation of CHW initiatives. Our model needed to reflect distinct bodies of work occurring at a statewide policy level, within the community-based or health system organizational context where CHWs work, and at the level of the direct interaction between CHWs and patients or program participants and community members. In light of these considerations, the authors decided that we needed to build our own model to serve as an accurate and comprehensive representation of CHW initiatives across our organizational units.
The authors provided summary statements of work done by funded recipients to engage CHWs within the organizational units that they represented. These summary statements focused on implementation strategies and outcomes to be accomplished. We populated the conventional template of a logic model with the content of these summary statements starting with the “activities and outcomes” column. Next, the authors collectively looked across the populated rows of activities and corresponding outcomes and eliminated duplicative activity statements and outcomes, maintaining all unique and critical statements. We followed an iterative process to group these activity sets based on type of activity undertaken. One group of activity statements reflected the roles played by CHWs in funded interventions such as providing culturally competent health education, conducting outreach to communities, and providing social support services. This set of activities mirrored the roles that we had previously synthesized from the C3 document and the Community Guide reviews. Another group of activities were those undertaken by funded recipients to promote the engagement of CHWs. Examples of these were working with and within health systems to incorporate CHWs in care teams or promote intervention-specific trainings. We then identified the inputs needed for these activities and articulated the short, intermediate, and long-term outcomes associated with these activities. We then determined the links between inputs, activity groups, and outcome statements.
It became evident that several activities were missing from this logic model. Examples included the authors’ firsthand knowledge of the work of various stakeholders (eg, CHW associations, academic partners), the authors’ own work (eg, technical assistance guides on CHW certification), and activities and insights of CHW subject matter experts. Included in these missing activities were aspects related to ways to enhance the capacity of the CHW workforce (eg, clarifying their scope of practice, establishing pathways to credentialing) and efforts to advance sustainable payment through a variety of partners. We developed summary statements for these and placed them into a third level of the logic model that we called the statewide infrastructural level. These policy and systems-level changes included the key components needed for the establishment of a sustainable CHW workforce to achieve better health outcomes for program participants and patients.
Phase 3: Mapping M&E metrics to the logic model
First, the authors mapped the metrics from their individual organizational units to the appropriate activities and outcomes of the logic model. Second, the authors reviewed the results of the mapping exercise and independently mapped all metrics and noted the results. Third, a program evaluator, who was not one of the authors, reviewed the mapped metrics and results and shared an independent and objective perspective to ensure the authors had accurately mapped the metrics to the logic model. We worked with the independent evaluator to resolve differences in mapping that emerged from this process. We then assessed the proportion of metrics that mapped to the different levels and parts of the logic model in order to understand the current focus of M&E efforts. We originally mapped 134 metrics across 5 organizational units. After eliminating duplicates there were 106 metrics, accounting for about a 20% overlap among the metrics used by organizational entities. At the health system and community organizational level, the metrics mapped to short- and intermediate-term outcomes, whereas at the CHW intervention level the metrics mapped to activities, as well as short- and intermediate-term outcomes.
Results
The logic model follows a linear organization and includes inputs and activities; short, intermediate, and long-term outcomes; and the intended impact (Figure). The model is divided into 3 interdependent levels: (1) statewide infrastructure; (2) health systems and community organizations; and (3) CHW interventions.
FIGURE.
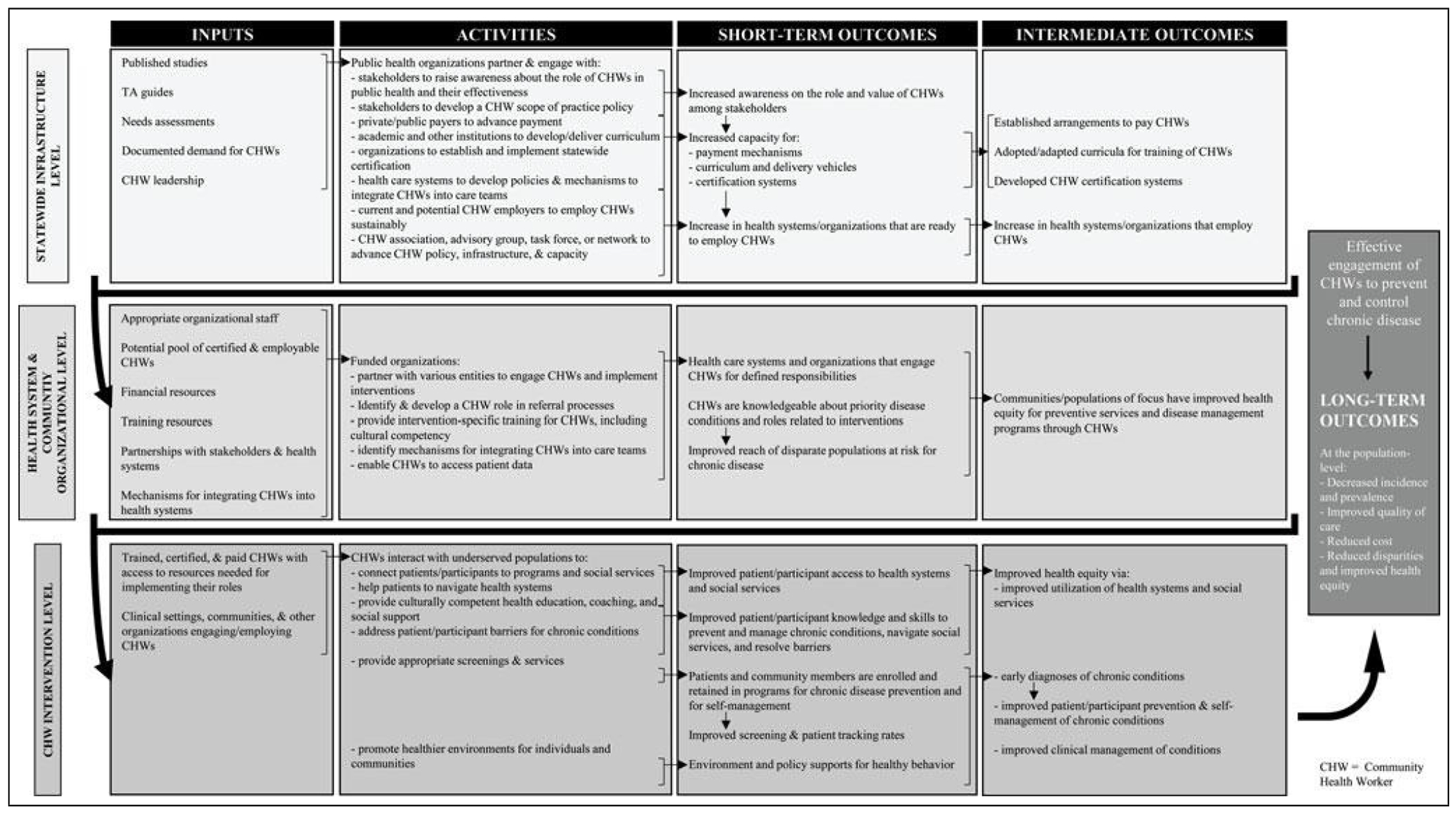
Approach to Designing and Measuring CHW Initiatives to Prevent and Improve Chronic Health Conditions
Abbreviations: CHW, community health worker; TA, technical assistance.
Statewide infrastructure level
The top level of the logic model reflects activities that help facilitate and support changes that occur at the other levels as evidenced by the large number of states taking action to build statewide infrastructure.19 The infrastructure level captures activities that stakeholders undertake at the state level to support the CHW workforce. Stakeholders and partners come together to raise awareness about the value of CHWs; conduct studies to build evidence, including impact and cost-effectiveness studies; establish partnerships to increase the network of CHWs and CHW allies; and create supportive environments for health systems and other organizations to engage CHWs. An example activity at this level is developing a policy on scope of practice with a CHW association, advisory council, task force, or network. This policy defines the CHW tasks and services under a state-recognized workforce identification and may allow CHW services to be covered by health insurance providers.
Other activities at this level include engaging academic and other institutions to develop or adapt and deliver a CHW core competency curriculum, as well as developing the processes and procedures for establishing a certification or credentialing process. Such activities may result in the establishment of CHW certification, a credentialing body, and associated rules and regulations. Organizations may also undertake activities to establish sustainable payment mechanisms for CHWs. These include working with public payers (eg, Medicaid) to establish policies for reimbursing the work of CHWs. Outcomes may include a State Plan Amendment, establishment and implementation of a Medicaid 1115 Demonstration Waiver, or other arrangements to reimburse CHWs sustainably.
Health system and community organizational level
The next level down in the logic model, “health system and community organizational level,” denotes activities and outcomes that occur within private and public organizations, such as hospitals and health systems, community-based organizations, and other entities that employ, partner with, or support CHWs. While work that occurs at the statewide level is aimed at ensuring the sustainability of the CHW workforce, work at the organizational level integrates CHWs into specific organizational structures. Activities at this level include determining CHW roles within a health system or community-based organization, providing intervention-specific or culturally competent training to CHWs within organizations, and enabling CHWs to access key patient or participant data. When organizations undertake these activities, they engage CHWs either directly as employees or through partnerships or business arrangements with other organizations that employ them. Key short-term outcomes resulting from these activities include improved organizational engagement of CHWs, improved knowledge of priority disease conditions and intervention roles among CHWs, and improved reach of populations at risk for chronic disease. Eventually, this has the potential to improve health equity for preventive and disease management services among at-risk populations.
CHW intervention level
At the “CHW intervention level,” CHWs interact with patients in health systems, participants in disease prevention and disease management programs, or with members of communities. This level of the logic model captures the synthesized set of roles that were identified from the C3 Project and the Community Guide reviews as these closely mirrored the activities that we had gleaned from the summary statements of authors describing the work of CHWs within CHW initiatives in their organizational units. With the landscape set up to support the CHW profession from the prior 2 levels, CHWs can perform their responsibilities more effectively. CHW activities include connecting patients or community members to programs and social services; helping patients navigate health systems; providing culturally competent health education, coaching, and social support; and helping patients to address barriers to chronic disease prevention and management. CHWs may also promote healthier environments in communities or may provide limited health screenings. Several short-term outcomes can result from these activities. For example, improved connection of patients or program participants to programs and social services can result in better access to these services. This, in turn, may result in earlier patient enrollment into programs and earlier diagnosis of chronic conditions, timely treatment initiation, and improved clinical outcomes.
M&E metrics aligned to the logic model
As a third phase of this work, after developing the logic model based on the steps described previously, we mapped the M&E metrics that we had originally gathered from across our organizational units onto the developed logic model. This mapping process showed some important patterns in the current measurement of CHW initiatives and pointed to gaps. We found that almost two-thirds of the metrics (60.4%; n = 64) mapped to the CHW intervention level (Table 2). These metrics measured the implementation of CHW roles and short- and intermediate-term outcomes, such as better access to health care services; improved knowledge among patients and program participants about disease prevention and management; increased enrollment and retention in disease prevention and management programs; early diagnosis of conditions; and improved self-management and clinical management. More than a third of all metrics (36.8%; n = 39) mapped to the “health system and community organizational level.” Many of these metrics measured short- and intermediate-term outcomes of activities undertaken by funded recipients in working with health systems and community-based organizations. Only a minimal number of indicators (2.8%; n = 3) mapped to the statewide infrastructure level, highlighting a major gap in current programmatic activities and M&E metrics for this level.
TABLE 2.
Frequency of Indicators Mapped to the Logic Model (n = 106)
| Inputs, n (%) | Activities, n (%) | Indicators, n (%) | |||
|---|---|---|---|---|---|
| Short-term Outcomes | Intermediate-term Outcomes | Total | |||
| Statewide infrastructure level | 0 | 1 (33.3) | 0 | 2 (66.7) | 3 (2.8) |
| Health system and organizational level | 3 (7.7) | 6 (15.4) | 17 (43.6) | 13 (33.3) | 39 (36.8) |
| CHW intervention level | 1 (1.6) | 19 (29.7) | 21 (32.8) | 23 (35.9) | 64 (60.4) |
| Total across all levels | 4 (3.7) | 26 (24.5) | 38 (35.8) | 38 (35.8) | 106 (100) |
Abbreviation: CHW, community health worker.
Discussion and Conclusion
We developed a logic model to articulate the types of inputs and activities needed at different levels of CHW initiatives and the corresponding outcomes. Each level of the logic model builds on the previous one and is connected to each consecutive level. That is, a statewide policy could establish the infrastructure to engage CHWs as a workforce. Organizations, such as health systems and community-based organizations, could, in turn, develop appropriate structures, systems, and processes to integrate CHWs into their organizations. CHWs would then be well poised to meaningfully interact with patients or program participants through outreach to medically underserved populations, provide culturally competent education, and facilitate access to health and social services. When the CHW workforce is supported and engaged in this way, it becomes feasible to measure the results of their efforts in terms of improved health behaviors and health outcomes for populations of focus.
The logic model and associated metrics have several potential applications. First, CHW program stakeholders can refer to the logic model to determine the appropriate level or levels at which they might implement a particular CHW initiative. Second, they can use the model to guide assessment of their capacity and readiness to implement CHW initiatives at each level (eg, the state policy environment or readiness of health care organizations to engage and integrate CHWs). This will help practitioners select the appropriate level at which to focus their initiatives and determine potential outcomes they can measure. Third, organizations can use the logic model to guide performance measurement and evaluation of CHW initiatives. Organizations spearheading CHW initiatives can consider using this logic model as a guide and visual to ensure that performance measurement and evaluation occur at appropriate levels with corresponding outcomes. This can illustrate to funders and stakeholders the level(s) of implementation of the proposed initiatives and associated outcomes and could garner further support for continued implementation and evaluation of CHW initiatives in the future.
For some time now, evidence has clearly pointed to the benefits of collaborations between primary care and public health in reducing health disparities.20 CHW programs can improve the completion time for screening and diagnosis among medically underserved populations served in safety-net clinics.9 However, the limited ability to bill for and reimburse CHW services continues to be a barrier in implementing CHW initiatives. Some of the factors that facilitate CHW initiatives include initial and ongoing training for CHWs, allowing CHWs access to electronic health records, and incorporating Community Guide–recommended strategies into CHW interventions.21–23 CHW initiatives reduce disparities that are associated with the social determinants of health such as race, ethnicity, income, and education in the intervention populations in which they are implemented.9 The logic model shows how the statewide and systems-level activities are associated with the conditions for sustainable engagement of CHWs; the activities at the organizational level may result in the successful integration of CHWs in clinical and community organizations; and the activities at the CHW intervention level can demonstrate positive results for patients and program participants. Activities and associated short-term outcomes at all 3 levels of the logic model can result in longer-term outcomes, including better quality of care for patients, early diagnosis and treatment, costs averted related to avoidable complications, and decreased overall incidence and prevalence of chronic conditions.
We presented this logic model to nearly 100 CHWs and CHW allies at a national conference and to more than 30 state health department staff members working on CHW initiatives who agreed that the model is useful for their own implementation of CHW initiatives. On the basis of the work of developing a logic model and mapping metrics currently used for M&E, we had learned that there was a gap in the statewide infrastructural level of CHW initiatives. The project has since resulted in a new collaboration with a network of CHW organizations working on common indicators for measuring the impact of CHWs, which will begin to address this gap and to advance the evidence base for CHW sustainability. A recent publication does address this gap to some extent by focusing on workforce and community outcomes and offers a limited focus on the policy/statewide infrastructure level. However, policies are only inputs in the model in this recent publication, and CHW development is reflected only at the program level.24 Our model, on the contrary, adds substantively to the policy aspects of CHW initiatives by clearly articulating the inputs and activities needed and the short- and long-term outcomes that result from these activities.
Limitations
This project focused on metrics used by partners supported through a large federal agency and spanned several types of organizations, including state and local health departments and community organizations. This list is not exhaustive and may not include all types of entities that implement and evaluate CHW initiatives and may not meet the needs of some entities. Also, the entities of focus were those addressing chronic disease conditions and therefore did not cover CHW initiatives that were focused on other disease conditions such as HIV/AIDs. This, too, may impact the applicability of the results to some degree. However, the logic model was purposefully developed to apply to a broad variety of conditions and contexts. As such, the authors are confident that readers can use the model and the findings of this research in their day-to-day work and unique settings.
Implications for policy & practice.
The logic model presents the policy activities needed at a statewide infrastructural level, related inputs, and the outcomes resulting from these. CHW stakeholders can use these to guide their policy initiatives to sustainably engage CHWs.
The logic model provides a multilevel structure that organizations can use to design their interventions to engage CHWs. The 3 separate levels offer distinct areas of focus that build upon each other to together ensure meaningful and sustainable engagement of the CHW workforce and population-level health improvements.
Based on the outcomes that one wishes to accomplish, the activities in the logic model offer directions that are clear and can lead to the desired outcomes.
Public health practitioners can use the logic model to improve their capacity and readiness to implement CHW initiatives for disease prevention and management.
Public health practitioners can use existing metrics or develop new ones to measure the outcomes reflected in the logic model.
Acknowledgments
The authors thank John Chapel, BS, for his support and valuable insight in designing the logic model, and Joanna Elmi, MPH, for her efforts in mapping the monitoring and evaluation metrics to the developed logic model.
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
The authors declare that they have no conflicts of interest.
Contributor Information
Bina Jayapaul-Philip, Centers for Disease Control and Prevention, Atlanta, Georgia.
Sharada S. Shantharam, IHRC, Inc, Atlanta, Georgia.
Refilwe Moeti, Centers for Disease Control and Prevention, Atlanta, Georgia.
Gayathri S. Kumar, Centers for Disease Control and Prevention, Atlanta, Georgia.
Colleen Barbero, Centers for Disease Control and Prevention, Atlanta, Georgia.
Elizabeth A. Rohan, Centers for Disease Control and Prevention, Atlanta, Georgia.
Yvonne Mensa-Wilmot, Centers for Disease Control and Prevention, Atlanta, Georgia.
Robin Soler, Centers for Disease Control and Prevention, Atlanta, Georgia.
References
- 1.American Public Health Association. Community health workers. https://www.apha.org/apha-communities/member-sections/community-health-workers. Published 2017. Accessed November 11, 2017.
- 2.The Community Guide. Cardiovascular disease: interventions engaging community health workers. https://www.thecommunityguide.org/findings/cardiovascular-disease-prevention-and-control-interventions-engaging-community-health. Published 2015. Accessed October 26, 2017.
- 3.The Community Guide. Diabetes prevention: interventions engaging community health workers. https://www.thecommunityguide.org/findings/diabetes-prevention-interventions-engaging-community-health-workers. Published 2016. Accessed October 25, 2017.
- 4.The Community Guide. Diabetes management: interventions engaging community health workers. https://www.thecommunityguide.org/findings/diabetes-management-interventions-engaging-community-health-workers. Published 2017. Accessed October 25, 2017.
- 5.Donaldson EA, Holtgrave DR, Duffin RA, Feltner F, Funderburk W, Freeman HP. Patient navigation for breast and colorectal cancer in 3 community hospital settings. Cancer. 2012;118(19):4851–4859. [DOI] [PubMed] [Google Scholar]
- 6.Krok-Schoen JL, Brewer BM, Young GS, et al. Participants’ barriers to diagnostic resolution and factors associated with needing patient navigation. Cancer. 2015;121(16):2757–2764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wells KJ, Luque JS, Miladinovic B, et al. Do community health worker interventions improve rates of screening mammography in the United States? A systematic review. Cancer Epidemiol Biomarkers Prev. 2011;20(8):1580–1598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kangovi S, Grande D, Trinh-Shevrin C. From rhetoric to reality—community health workers in post-reform U.S. health care. N Engl J Med. 2015;372(24):2277–2279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roland KB, Milliken EL, Rohan EA, et al. Use of community health workers and patient navigators to improve cancer outcomes among patients served by federally qualified health centers: a systematic literature review. Health Equity. 2017;1(1):61–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rosenthal EL, Rush CH, Allen CG. Understanding Scope and Competencies: A Contemporary Look at the United States Community Health Worker Field. Progress Report of the Community Health Worker (CHW) Core Consensus (C3) Project: Building National Consensus on the CHW Core Roles, Skills and Qualities. Houston, TX: University of Texas-Houston School of Public Health, Institute for Health Policy; 2016. [Google Scholar]
- 11.Foreit J, Raifman S. Increasing Access to Family Planning (FP) and Reproductive Health (RH) Services Through Task Sharing Between Community Health Workers (CHWs) and Mid-Level Community Professionals in Large-Scale Public-Sector Programs: A Literature Review to Help Guide Case Studies. New York, NY: Population Council; 2011. [Google Scholar]
- 12.Huicho L, Dieleman M, Campbell J, et al. Increasing access to health workers in underserved areas: a conceptual framework for measuring results. Bull World Health Organ. 2010;88(5):357–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hurtado M, Spinner JR, Yang M, et al. Knowledge and behavioral effects in cardiovascular health: community health worker health disparities initiative, 2007-2010. Prev Chronic Dis. 2014;11:E22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Katigbak C, Van Devanter N, Islam N, Trinh-Shevrin C. Partners in health: a conceptual framework for the role of community health workers in facilitating patients’ adoption of healthy behaviors. Am J Public Health. 2015;105(5):872–880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kok MC, Dieleman M, Taegtmeyer M, et al. Which intervention design factors influence performance of community health workers in low- and middle-income countries? A systematic review. Health Policy Plan. 2015;30(9):1207–1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu A, Sullivan S. A Call for One Million Community Health Workers. State of the Planet. Vol 2017. New York, NY: Earth Institute; 2011. [Google Scholar]
- 17.Naimoli JF, Frymus DE, Wuliji T, Franco LM, Newsome MH. A community health worker “logic model”: towards a theory of enhanced performance in low- and middle-income countries. Hum Resour Health. 2014;12:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Osuji TA, House M, Xu Y, Fine J, Mirambeau A, Elmi J. Implementation Guide for Public Health Practitioners: The St. Johnsbury Community Health Team Model. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services; 2015. [Google Scholar]
- 19.National Academy for State Health Policy. State community health worker models. https://nashp.org/state-community-health-worker-models. Accessed November 29, 2019.
- 20.Institute of Medicine. Primary Care and Public Health: Exploring Integration to Improve Population Health. Washington, DC: The National Academies Press; 2012. [PubMed] [Google Scholar]
- 21.Battaglia TA, Bak SM, Heeren T, et al. Boston Patient Navigation Research Program: the impact of navigation on time to diagnostic resolution after abnormal cancer screening. Cancer Epidemiol Biomarkers Prev. 2012;21(10):1645–1654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Honeycutt S, Green R, Ballard D, et al. Evaluation of a patient navigation program to promote colorectal cancer screening in rural Georgia, USA. Cancer. 2013;119(16):3059–3066. [DOI] [PubMed] [Google Scholar]
- 23.Lasser KE, Murillo J, Lisboa S, et al. Colorectal cancer screening among ethnically diverse, low-income patients: a randomized controlled trial. Arch Intern Med. 2011;171(10):906–912. [DOI] [PubMed] [Google Scholar]
- 24.Agarwal S, Sripad P, Johnson C, et al. A conceptual framework for measuring community health workforce performance within primary health care systems. Hum Resour Health. 2019;17(1):86–86. [DOI] [PMC free article] [PubMed] [Google Scholar]


