Abstract
This comprehensive review explores the integration of artificial intelligence (AI) in the field of social pediatrics, emphasizing its potential to revolutionize child healthcare. Social pediatrics, a specialized branch within the discipline, focuses on the significant influence of societal, environmental, and economic factors on children’s health and development. This field adopts a holistic approach, integrating medical, psychological, and environmental considerations. This review aims to explore the potential of AI in revolutionizing child healthcare from social pediatrics perspective. To achieve that, we explored AI applications in preventive care, growth monitoring, nutritional guidance, environmental risk factor prediction, and early detection of child abuse. The findings highlight AI’s significant contributions in various areas of social pediatrics. Artificial intelligence’s proficiency in handling large datasets is shown to enhance diagnostic processes, personalize treatments, and improve overall healthcare management. Notable advancements are observed in preventive care, growth monitoring, nutritional counseling, predicting environmental risks, and early child abuse detection. We find that integrating AI into social pediatric healthcare aims to enhance the effectiveness, accessibility, and equity of pediatric health services. This integration ensures high-quality care for every child, regardless of their social background. The study elucidates AI’s multifaceted applications in social pediatrics, including natural language processing, machine learning algorithms for health outcome predictions, and AI-driven tools for health and environmental monitoring, collectively fostering a more efficient, informed, and responsive pediatric healthcare system.
Keywords: Social pediatrics, artificial intelligence, machine learning, breastfeeding, immunization
Introduction
Social Pediatrics
Social pediatrics, a specialized branch within pediatrics, highlights the significant role of societal, environmental, and economic elements in shaping the health and development of children and teenagers. This field values a comprehensive approach to child healthcare, integrating medical, psychological, and environmental considerations.1-3 Key aspects of social pediatrics encompass a range of critical elements including infant and young child feeding, growth monitoring, promoting early childhood development, immunization, environmental health, newborn screening, age-appropriate child care, anticipatory guidance, managing prevalent pediatric conditions such as acute respiratory infections and gastroenteritis and the early identification and prevention of child abuse, all grounded in the principle of children’s rights. This approach recognizes the intricate interplay between a child’s well-being and their broader environment, striving to address disparities in healthcare accessibility with the ultimate goal of enhancing overall health outcomes.4-6
Artificial Intelligence—Basics and Terms
Artificial intelligence (AI) has gained significant popularity in recent years, and its application across various medical fields has also become increasingly prevalent.7 Artificial intelligence is a technology that allows computers to mimic human behavior and thinking. It includes anything from understanding speech to making decisions.
Machine learning (ML) is a subset of AI that enables computers to learn from data. Rather than being programmed with specific rules, like a calculator, ML systems adapt their behavior based on new information they receive. This iterative process improves their predictive capabilities and decision-making over time.8
Deep learning is a specialized type of ML that uses structures similar to the human brain, called neural networks, to process data. This method is particularly good at recognizing patterns like voices or faces.9
Neural networks are a set of algorithms modeled loosely after the human brain. They are designed to recognize patterns by interpreting data through a kind of machine perception, labeling, or clustering.10
Supervised learning involves training a machine using pre-labeled data. For instance, it might be given a set of photographs along with the names of the individuals in them, enabling it to learn to recognize specific people. This method is analogous to a teacher providing correct answers during the learning process. Unsupervised learning, on the other hand, requires the machine to interpret and find patterns in data without any labels. The machine must analyze the data independently to identify structures and relationships. This process can be likened to deciphering a book written in an unfamiliar language by identifying recurring words and phrases.11
Natural language processing (NLP) is a branch of AI that helps computers understand, interpret, and respond to human language in a way that is valuable. It involves teaching machines to process and analyze large amounts of natural language data, enabling them to perform tasks like translating text from one language to another, responding to spoken commands, and summarizing large documents. This technology is fundamental in creating applications that interact with users in a human-like manner, such as chatbots and virtual assistants.12
These technologies have diverse applications, ranging from recommending movies based on previous viewing history to aiding medical professionals in predicting disease progression in patients.
Potential Roles of Artificial Intelligence in Healthcare
The introduction of AI in healthcare is a pivotal moment and this combination has the potential to revolutionize patient care, diagnostic processes, treatment modalities, and healthcare management. Artificial intelligence excels in processing and analyzing large datasets, such as electronic health records, with a speed and accuracy that not only extends beyond human analytical capabilities, but also addresses tasks that would be excessively time-consuming or hard for human analysts.13
In diagnostic procedures, AI algorithms may demonstrate high accuracy in identifying diseases from images or genetic data.14 When it comes to treatment, AI may offer personalized care options by taking into account individual patient profiles, leading to more effective and specifically tailored or personalized treatments.15 Artificial intelligence can contribute to healthcare administration by optimizing resource allocation, predicting patient admissions, thus enhancing the overall efficiency of health systems.16
Integrating Artificial Intelligence with Social Pediatrics
Utilizing AI within social pediatrics may greatly improve child health outcomes in several ways. For example, it can improve preventive care by detecting the children who are likely to miss immunization schedules using demographic and epidemiological data.17 In the realm of growth monitoring and nutrition, AI may provide personalized recommendations and early warnings about growth failure issues, or find new growth monitoring techniques.18 Artificial intelligence’s predictive capabilities may be valuable in identifying environmental risk factors, diagnostics, and potential outbreaks of diseases like gastroenteritis or respiratory infections.19-22 Moreover, AI tools may support the detection of child abuse by analyzing patterns in clinical, radiological, or social data that might indicate abuse, thus enabling earlier intervention.23,24
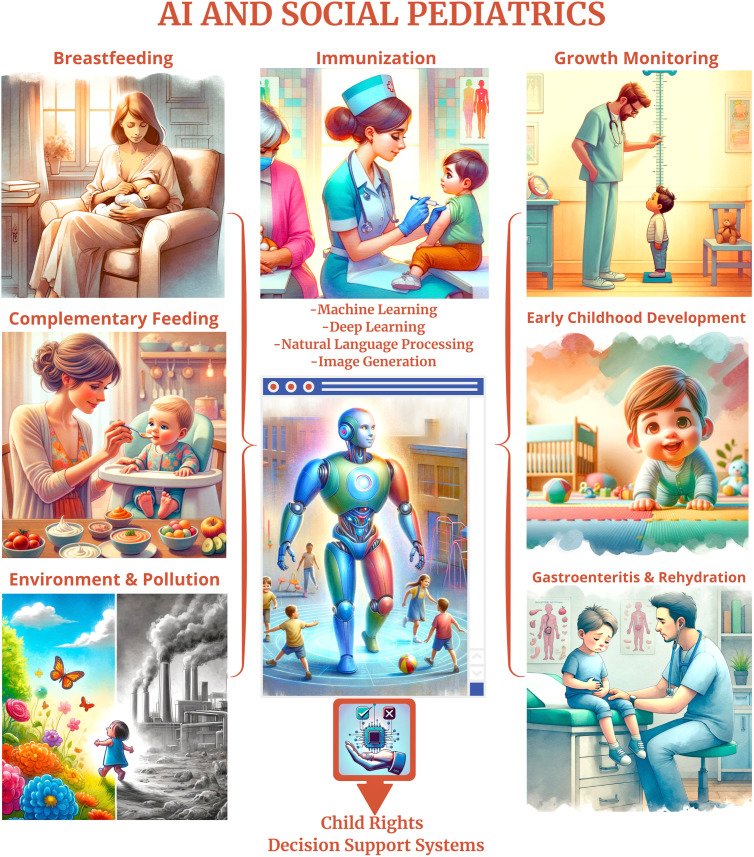
Figure 1 showcases a series of AI-generated images that depict various aspects of social pediatrics, produced through commands given to ChatGPT. This illustration serves as a demonstration of the advanced capabilities of AI in generating educational and informative visual content. The purpose of including these images is 2-fold: first, to exemplify how AI can be leveraged to create impactful visual aids that enhance understanding and dissemination of complex medical subjects; and second, to inspire medical professionals to utilize similar AI technologies to develop and share their own educational materials, thereby enhancing both clinical practice and academic environment in their own fields of study.
Figure 1.
This abstract figure displays artificial intelligence (AI)-generated images depicting critical domains in social pediatrics, showcasing AI’s potential in creating educational materials to enhance understanding and communication in medical practice.
The primary aim of integrating AI in social pediatric healthcare is to enhance the effectiveness, accessibility, and equality of pediatric health services. This ensures that every child, irrespective of their family background and the values of their community, receives the utmost quality of care and support to ensure a healthy start in life.
Childhood Immunization
Immunizing children is crucial not only for reducing disease incidence and mortality but also for strengthening community immunity, which is essential for protecting vulnerable populations and preventing outbreaks.25,26 However, addressing challenges such as vaccine hesitancy and disruptions in vaccination programs is critical to achieving optimal vaccination coverage and fully harnessing the benefits of immunization.27,28
In today’s expanding digital world, the impact of social media on childhood vaccination programs is undeniable, exerting both positive and negative influences.29 The nature of social media platforms enables users to selectively engage with content of their choosing. This interaction often leads the user to be included in similar/ideologically homogenous groups, referred to as “echo chambers.”30 Consequently, groups hesitant about vaccines tend to interact amongst themselves, reinforcing their anti-vaccine sentiments even more. Therefore, it is crucial to strategically utilize social media in advocating for vaccination programs.28,31,32
Healthcare professionals and authorities can identify and address misinformation about vaccination programs by harnessing the NLP methods. The Vaccine Sentimeter, a platform utilizing automated data collection from mainstream media and Twitter, coupled with natural language processing and manual curation, effectively tracks and characterizes real-time global online conversations about vaccination, demonstrating its potential as a tool for public health professionals to monitor vaccine sentiment and hesitancy.33 A ML-system using support vector machines, trained on a combination of strictly and laxly labeled data, significantly outperforms traditional sentiment analysis in classifying the stance toward vaccination in Dutch Twitter messages.34 Some AI models successfully classified health-related webpages about early childhood vaccination as “reliable” or “unreliable,” with high accuracy, using key textual indicators, demonstrating their potential as tools for assisting in the evaluation of online health information.35
It is important to monitor vaccine adverse effects to ensure public confidence in immunization programs. An ML-based active surveillance system using national claim data, developed to monitor vaccine adverse events, demonstrated high accuracy in predicting anaphylaxis and agranulocytosis post-flu vaccination, validating the utility of integrating health record databases for vaccine safety surveillance.36
In addition to the aforementioned applications, AI can be used to contribute to technological advancements in terms of vaccine design, protein structure prediction, immune repertoire analysis, and phylogenetic analysis.37-39
Breastfeeding
Breastfeeding holds paramount importance for both the mother and the baby. The composition of breast milk, rich in antibodies and essential nutrients, provides infants with comprehensive protection against infections and diseases. Moreover, breastfeeding fosters an unparalleled bond between mother and child, crucial for the child’s emotional and psychological development. From a maternal perspective, breastfeeding contributes significantly to the mother’s health by reducing the risk of various types of cancer, including breast and ovarian cancer, and aids in faster postpartum recovery. The World Health Organization and numerous health authorities emphasize the significance of exclusive breastfeeding for the first 6 months of life, followed by continued breastfeeding along with appropriate complementary foods for up to 2 years or beyond.40-42
Having information about how to breastfeed is important for mothers, especially if she is young and the baby is her first child.43 Artificial intelligence-driven chatbots and virtual assistants may provide 24/7 support to new mothers, offering immediate answers to common breastfeeding queries. The observational study on LactApp, a mobile application for breastfeeding support, revealed that mothers frequently consult topics such as breastfeeding technique, infant sleep, and milk management, with their information needs evolving in line with their infant’s developmental stages, from physiological issues in the early days to weaning and tandem breastfeeding as the child ages.44
Mothers utilize social media platforms not only to exchange their own breastfeeding experiences but also to gain insights from others. The data found on these platforms may play a role in recognizing misinformation and detecting prevalent issues encountered in breastfeeding.45 In a research study, using sentiment analysis with ML methods on tweets related to breastfeeding has been effective in uncovering a range of influences on breastfeeding habits. This includes identifying health, social, psychological, and circumstantial obstacles, alongside recognizing the advantages and support systems available.46
Using ML algorithms may be useful to predict the likelihood of early cessation of breastfeeding.47,48 By identifying these probabilities, healthcare providers can focus their efforts on mothers at higher risk. This focused strategy ensures that these mothers receive dedicated assistance and advice, enhancing the likelihood of sustaining breastfeeding.
Growth Monitoring
Growth monitoring is a crucial aspect of routine pediatric healthcare, serving as an essential tool for easily assessing the health of children easily.49 By regularly tracking parameters such as weight, height, and head circumference, healthcare providers can identify potential growth abnormalities at an early stage. This proactive approach enables timely intervention, addressing nutritional deficiencies or underlying health conditions that might impede a child’s growth. Also, growth monitoring provides valuable insights into the child’s overall well-being, offering a comprehensive view in relation to established growth standards, which ensures that children achieve their full potential.50,51
AI can be used to predict growth for a child in the future. For example, a study successfully employed ML techniques to predict discharge weight and weight gain in hospitalized newborns, revealing length of hospital stay, parenteral nutrition, and other clinical factors as key predictors, with high predictive accuracy.52 Machine learning algorithms have proven highly effective, achieving 97% accuracy in predicting intrauterine growth restriction using fetal heart rate parameters, suggesting the potential for developing improved and cost-effective screening methods to enhance pregnancy outcomes.53
With AI, it might be possible to find new growth monitoring techniques. For example, an automated deep learning pipeline to measure temporalis muscle thickness from brain magnetic resonance imagings was developed to generate sex-specific growth charts for ages 4-35, and the muscle thickness was linked to several physiological traits and health conditions, thereby enhancing clinical decision-making.18
Environment and Child Health
Children exhibit a greater vulnerability to environmental influences compared to adults, primarily due to several physiological and behavioral factors. First, children have a more rapid metabolism, which necessitates a higher intake of food and water per unit of body weight. This increased consumption can lead to greater exposure to potential contaminants. Second, children’s faster respiration rates contribute to a heightened intake of airborne substances. Moreover, their shorter stature positions them closer to the ground, exposing them to heavier air pollutants that tend to settle at lower levels, along with a higher concentration of dust particles found near the floor. Additionally, children often explore their surroundings orally, increasing the risk of ingesting harmful substances. The relative thinness of children’s skin facilitates quicker absorption of materials through their skin. Adolescents tend to be more “brave,” so they may enter hazardous environments more frequently. These factors collectively make children susceptible to environmental hazards.54
Utilizing AI for predictive modeling is a significant method to evaluate environmental risks that affect children’s health. These algorithms can anticipate potential health risks by analyzing existing environmental patterns, thus aiding in devising proactive public health strategies. Predictive models are also instrumental in understanding the potential long-term impacts of environmental changes on children’s health. This predictive capability may be vital for planning and executing effective environmental health policies and preventive measures. For instance, a study demonstrated that ML models, which integrated socioeconomic factors, housing characteristics, and water quality data, successfully predicted elevated blood lead levels in children across diverse regions in the United States. The predictions closely aligned with the actual observed levels.55
In urban areas, AI-driven systems may be used to analyze patterns in air pollution and predict high-risk periods for pollutants like PM2.5. It is an effective way for air pollution forecasting, surpassing traditional models in accuracy due to its ability to handle the complex, non-linear nature of air pollutants.22 Acquiring this information can inform public advisories and help parents minimize children’s exposure during peak pollution times.
A review inspected studies about early-life exposures to the environment and outlined that the majority of studies focused on prenatal exposure to air pollution, weather or the built environment, heavy metals, and endocrine disruptors. These studies primarily investigated postnatal health outcomes, such as respiratory illnesses and neurodevelopmental effects, with a notable portion introducing novel ML methods for analyzing chemical mixtures and disease predictions.56 Exposure to a variety of environmental pollutants and factors, including persistent organic pollutants, inorganic arsenic, air pollution, dichlorodiphenyltrichloroethane, pyrethroids, phthalates, and heavy metals, has been linked to health outcomes such as altered thyroid function, increased blood pressure, changes in body composition and body mass index, neurodevelopmental trajectories, low birth weight, attention deficit hyperactivity disorder, and altered gut bacteria composition in children.56
Artificial intelligence algorithms can be deployed to monitor water quality in real-time, identifying contaminants like pesticides or microbial agents.57 This monitoring is crucial in preventing waterborne diseases and ensuring safe drinking water for children.
Artificial intelligence could present innovative strategies for promoting a cleaner environment. The Adaptive Intelligent Dynamic Water Resource Planning model employs AI along with a Markov Decision Process to refine urban water management. This approach aids in achieving sustainable environmental planning by advancing decision-making processes and boosting economic efficiency at the local level.58
Artificial intelligence models are being used to study the effects of climate change on child health, predicting increases in heat-related illnesses or the spread of vector-borne diseases like malaria.59,60
Acute Respiratory Infections
Acute respiratory infections (ARIs) in children are a major health issue, especially as these infections are a primary cause of death among children below 5 years old, particularly in developing countries. Acute respiratory infections cover a spectrum of diseases affecting the upper and lower respiratory tracts, including conditions like bronchiolitis and pneumonia, caused by various pathogens. It is vital to not only differentiate between severe infections and more commonplace infections but also to prioritize the rapid management and treatment of the serious cases.61
It is shown that ML models utilizing clinical features such as age, event pattern, and C-reactive protein effectively predict respiratory pathogens in hospitalized children with ARIs, potentially improving diagnostic accuracy and reducing medical costs.62
A web application integrating a chatbot and AI, coupled with an electronic device measuring vital signs, demonstrates a 91% accuracy rate in diagnosing respiratory diseases like coronavirus disease 2019 (COVID-19), common cold, and allergic rhinitis, enhancing remote diagnosis capabilities.63
A review indicates that AI algorithms show dependable performance in diagnosing respiratory diseases such as pneumonia, tuberculosis, and COVID-19 by analyzing cough sounds. This approach may be a promising way of improving disease detection, particularly in settings with limited resources. The specificity of these different algorithms ranges from 71% to 99.6%, while their sensitivity varies between 44% and 100%. This data underscores the potential of AI in medical diagnostics, though it also highlights the variability in accuracy across different conditions and implementations.20
An ML model using pediatric electronic health record data exhibits high accuracy in the early prediction of Respiratory Syncytial Virus in hospitalized children, aiding rapid and cost-effective patient management and infection control.64
Gastroenteritis
Gastroenteritis is a common and potentially severe condition in children, leading to inflammation of the gastrointestinal tract, manifesting in symptoms such as vomiting, diarrhea, and abdominal pain. This illness is significant due to its widespread impact; a child under 5 years typically has 1-5 acute diarrhea attacks each year. Its potential for serious complications like dehydration poses a significant risk in infants and young children and can be life-threatening. To address this, dehydration and electrolyte imbalances can be effectively treated with oral rehydration solutions, which are accessible either in powder form for convenience or can be prepared at home using simple, readily available ingredients.65-67
A lot of pathogens causing gastroenteritis are transmitted through water. Early detection of these outbreaks is important to stop the spread of illness. By processing large volumes of data from various sources, including healthcare facilities, public health records, and even social media, AI algorithms may identify trends and potential outbreak sources. Artificial intelligence’s predictive capabilities may also forecast future outbreaks based on current data trends, environmental conditions, and population movements. A study demonstrated that the long short-term memory ML algorithm effectively predicts weekly norovirus outbreaks in South Korea (92.5% accuracy), identifying critical factors such as the last norovirus detection rate, minimum temperature, and day length.21
Sometimes it is important to differentiate viral or bacterial gastroenteritis, especially to choose whether to give an antibiotic or not.68 An algorithm estimates pediatric bacterial acute gastroenteritis using blood cell counts, with platelet and lymphocyte ratio, eosinophil count, and leukocyte count as key features.69
Child Abuse
In the United States, 1 in every 7 children is subjected to either abuse or neglect.24 It is imperative for pediatricians to recognize and address instances of abuse, which can often be concealed behind a normal childhood during regular health examinations and vaccination appointments. This situation demands a better understanding of the patterns of abuse, increased awareness of less obvious signs, and a stronger partnership with social services and legal entities to protect vulnerable children.
Advancements in AI have significantly influenced pediatric radiology, offering notable potential in enhancing the prediction, identification, and investigation of child abuse cases with pediatric trauma.23
A decision support system using artificial neural networks demonstrated 99.2% accuracy in predicting post-traumatic stress disorder and major depressive disorder in children exposed to sexual abuse, utilizing various abuse-related parameters for early psychiatric assessment.70
AI systems can analyze vast amounts of data, including healthcare records, school reports, and social services data, to identify patterns that may indicate abuse or neglect. Text mining and ML techniques successfully identified and predicted child abuse cases in a Dutch public health institution, with a high classification accuracy based on over 500 child specialists’ assessments.71
Natural language processing algorithms may be useful in determining suspected child abuse cases in broad hospital settings. In a study, a refined NLP algorithm was tested it in “silent mode” across multiple emergency departments, leading to enhanced specificity in detecting injuries linked to child abuse, while also uncovering demographic disparities in the evaluation and reporting processes related to child protective services.72
Considerations and Downsides
While the integration of AI presents substantial opportunities in enhancing pediatric care, it is accompanied by several crucial considerations that require attention.
Data safety and security: the application of AI in healthcare settings involves handling of sensitive health data. Ensuring robust security measures to prevent data breaches is vital. Strict data governance protocols and secure encryption methodologies must be established to protect this data from unauthorized access, thereby safeguarding patient confidentiality and trust.73
Mitigating biases: AI systems may inadvertently become biased because of their training data. In pediatric care, this could result in biased health outcomes that disproportionately affect certain demographic groups. It is essential to utilize diverse datasets for training AI models and implement regular audits to ensure AI systems are fair and equitable in their functionality.74
Ethical concerns: the integration of AI in healthcare raises critical ethical questions concerning patient consent, autonomy, and the potential replacement of human judgment by AI systems. To address these challenges, it is essential to develop comprehensive policies that govern the use and deployment of AI. These policies should guarantee that AI tools are used to assist healthcare professionals, not replace them, by enhancing their ability to make detailed and informed clinical decisions. Artificial intelligence should primarily serve as a decision-support tool, enhancing the quality of care provided by human practitioners while maintaining and respecting patient autonomy. Also, more sensitive subjects like child abuse require extra careful consideration of privacy, ethical implications, and the potential for both false positives and false negatives. The integration of AI tools in such sensitive areas must be handled with the highest ethical standards.73
Transparency and explainability: the opaque nature of some AI algorithms (often referred to as “black box” models) can obscure how decisions are made, making it difficult for practitioners to trust and verify AI outputs. Developing explainable AI models is crucial so that healthcare providers can understand and validate the AI-driven recommendations and decisions.75
Interoperability challenges: For AI to be effectively integrated into existing healthcare systems, it must be compatible with various electronic health record systems and other healthcare technologies. Standardizing data formats and fostering open standards can alleviate potential interoperability challenges, facilitating smoother integration and more coordinated care.
By addressing these considerations, the deployment of AI in pediatric care can be optimized to enhance service delivery while mitigating potential downsides. As this field evolves, continuous monitoring and adaptation of AI applications will be necessary to address new challenges and ensure that AI’s integration into healthcare serves to augment, not undermine, the quality and integrity of pediatric care.
Conclusion
The integration of AI in social pediatrics presents a groundbreaking shift in child healthcare, harnessing the power of data analytics and ML to enhance various aspects of pediatric care. From advancing growth monitoring and breastfeeding support to improving childhood immunization rates, AI’s capabilities are transformative. Its application in environmental health analysis and the early detection of child abuse marks a significant step forward in protecting and nurturing children’s well-being. As AI continues to evolve, its integration into social pediatrics promises a future where healthcare is more personalized, proactive, and accessible, ensuring a healthier start in life for every child. This integration not only enhances the quality of care but also addresses disparities, moving toward an equitable healthcare system for children across different social environments. This review provides valuable insights into the potential of AI in revolutionizing pediatric care, paving the way for further research and application in this vital field.
Funding Statement
This study received no funding.
Footnotes
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – M.G., S.S.Y.; Design – M.G., S.S.Y.; Supervision – S.S.Y.; Resources – M.G.; Materials – M.G.; Data Collection and/or Processing – M.G., S.S.Y.; Analysis and/or Interpretation – M.G., S.S.Y.; Literature Search – M.G.; Writing – M.G.; Critical Review – M.G., S.S.Y.
Acknowledgments: M.G. is a pediatrician and has a master’s degree in the interdisciplinary artificial intelligence technologies program. S.S.Y. author is the director of the Social Pediatrics PhD Program and the Child Neglect and Abuse Master’s Program at the Child Health Institute, and the Vaccine Studies Master’s Program at the Vaccine Institute, all at Hacettepe University.
Declaration of Interests: The authors have no conflicts of interest to declare.
References
- 1. Gökçay G, Kural B, Keskindemirci G, Neyzi O. Social pediatrics training in turkey. Çocuk Derg J Child. 2021;21(3):266 269. ( 10.26650/jchild.2021.995008) [DOI] [Google Scholar]
- 2. Van Den Heuvel M, Martimianakis MAT, Levy R, Atkinson A, Ford-Jones E, Shouldice M. Social pediatrics: weaving horizontal and vertical threads through pediatric residency. BMC Med Educ. 2017;17(1):12. ( 10.1186/s12909-016-0845-4) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Yurdakök K. Sosyal pediatri nedir? In: Yurdakök K, Yalçın SS, eds. Yurdakök Pediatri. 1st ed. Ankara: Güneş Tıp Kitabevleri; 2017:85 87. [Google Scholar]
- 4. Pierce MC, Kaczor K, Thompson R. Bringing back the social history. Pediatr Clin North Am. 2014;61(5):889 905. ( 10.1016/j.pcl.2014.06.010) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Van Den Heuvel M, Hopkins J, Biscaro A, et al. A comparative analysis of early child health and development services and outcomes in countries with different redistributive policies. BMC Public Health. 2013;13(1):1049. ( 10.1186/1471-2458-13-1049) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kanatlı MÇ, Yalcin SS. Social determinants screening with social history: pediatrician and resident perspectives from a middle-income country. Matern Child Health J. 2021;25(9):1426 1436. ( 10.1007/s10995-021-03191-7) [DOI] [PubMed] [Google Scholar]
- 7. Can Demirbaş KC, Yıldız M, Saygılı S, Canpolat N, Kasapçopur Ö. Artificial intelligence in pediatrics: learning to walk together. Turk Arch Pediatr. 2024;59(2):121 130. ( 10.5152/TurkArchPediatr.2024.24002) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dey A. Machine learning algorithms: a review. Int J Comput Sci Inf Technol. 2016;7(3):1174 1179. [Google Scholar]
- 9. Bini SA. Artificial intelligence, machine learning, deep learning, and cognitive computing: what do these terms mean and how will they impact health care? J Arthroplasty. 2018;33(8):2358 2361. ( 10.1016/j.arth.2018.02.067) [DOI] [PubMed] [Google Scholar]
- 10. Choi RY, Coyner AS, Kalpathy-Cramer J, Chiang MF, Campbell JP. Introduction to machine learning, neural networks, and deep learning. Transl Vis Sci Technol. 2020;9(2):14. ( 10.1167/tvst.9.2.14) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Deo RC. Machine learning in medicine. Circulation. 2015;132(20):1920 1930. ( 10.1161/CIRCULATIONAHA.115.001593) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Esteva A, Robicquet A, Ramsundar B, et al. A guide to deep learning in healthcare. Nat Med. 2019;25(1):24 29. ( 10.1038/s41591-018-0316-z) [DOI] [PubMed] [Google Scholar]
- 13. Lo Barco T, Kuchenbuch M, Garcelon N, Neuraz A, Nabbout R. Improving early diagnosis of rare diseases using natural language processing in unstructured medical records: an illustration from Dravet syndrome. Orphanet J Rare Dis. 2021;16(1):309. ( 10.1186/s13023-021-01936-9) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hsieh TC, Bar-Haim A, Moosa S, et al. GestaltMatcher facilitates rare disease matching using facial phenotype descriptors. Nat Genet. 2022;54(3):349 357. ( 10.1038/s41588-021-01010-x) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Álvarez-Machancoses Ó, DeAndrés Galiana EJ, Cernea A, Fernández de la Viña J, Fernández-Martínez JL. On the role of artificial intelligence in genomics to enhance precision medicine. Pharmgenomics Pers Med. 2020;13:105 119. ( 10.2147/PGPM.S205082) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ali O, Abdelbaki W, Shrestha A, Elbasi E, Alryalat MAA, Dwivedi YK. A systematic literature review of artificial intelligence in the healthcare sector: benefits, challenges, methodologies, and functionalities. J Innov Knowl. 2023;8(1). ( 10.1016/j.jik.2023.100333) [DOI] [Google Scholar]
- 17. Chandir S, Siddiqi DA, Hussain OA, et al. Using predictive analytics to identify children at high risk of defaulting from a routine immunization program: feasibility study. JMIR Public Heal Surveill. 2018;4(9):1 12. ( 10.2196/publichealth.9681) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Zapaishchykova A, Liu KX, Saraf A, et al. Automated temporalis muscle quantification and growth charts for children through adulthood. Nat Commun. 2023;14(1):6863. ( 10.1038/s41467-023-42501-1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Malik YS, Sircar S, Bhat S, et al. How artificial intelligence may help the Covid-19 pandemic: pitfalls and lessons for the future. Rev Med Virol. 2021;31(5):1 11. ( 10.1002/rmv.2205) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Alqudaihi KS, Aslam N, Khan IU, et al. Cough sound detection and diagnosis using artificial intelligence techniques: challenges and opportunities. IEEE Access. 2021;9:102327 102344. ( 10.1109/ACCESS.2021.3097559) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lee S, Cho E, Jang G, Kim S, Cho G. Early detection of norovirus outbreak using machine learning methods in South Korea. PLoS One. 2022;17(11):e0277671. ( 10.1371/journal.pone.0277671) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Masood A, Ahmad K. A review on emerging artificial intelligence (ai) techniques for air pollution forecasting: fundamentals, application and performance. J Clean Prod. 2021;322(12):129072. ( 10.1016/j.jclepro.2021.129072) [DOI] [Google Scholar]
- 23. Sorensen JI, Nikam RM, Choudhary AK. Artificial intelligence in child abuse imaging. Pediatr Radiol. 2021;51(6):1061 1064. ( 10.1007/s00247-021-05073-0) [DOI] [PubMed] [Google Scholar]
- 24. Lupariello F, Sussetto L, Di Trani S, Di Vella G. Artificial intelligence and child abuse and neglect: a systematic review. Children (Basel). 2023;10(10). ( 10.3390/children10101659) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. World Health Organization. Vaccines and immunization. Available at: https://www.who.int/health-topics/vaccines-and-immunization. Accessed December 25, 2023 [Google Scholar]
- 26. Quadri-Sheriff M, Hendrix KS, Downs SM, Sturm LA, Zimet GD, Finnell SME. The role of herd immunity in parents’ decision to vaccinate children: a systematic review. Pediatrics. 2012;130(3):522 530. ( 10.1542/peds.2012-0140) [DOI] [PubMed] [Google Scholar]
- 27. Fadl N, Abdelmoneim SA, Gebreal A, Youssef N, Ghazy RM. Routine childhood immunization in sub-Saharan Africa: addressing parental vaccine hesitancy. Public Health. 2024;226:66 73. ( 10.1016/j.puhe.2023.10.049) [DOI] [PubMed] [Google Scholar]
- 28. Yalçin SS, Bakacak AG, Topaç O. Unvaccinated children as community parasites in national qualitative study from turkey. BMC Public Health. 2020;20(1):1087. ( 10.1186/s12889-020-09184-5) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Rodrigues F, Ziade N, Jatuworapruk K, Caballero-Uribe CV, Khursheed T, Gupta L. The impact of social media on vaccination: a narrative review. J Korean Med Sci. 2023;38(40):e326. ( 10.3346/jkms.2023.38.e326) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Getman R, Helmi M, Roberts H, Yansane A, Cutler D, Seymour B. Vaccine hesitancy and online information: the influence of digital networks. Health Educ Behav. 2018;45(4):599 606. ( 10.1177/1090198117739673) [DOI] [PubMed] [Google Scholar]
- 31. Puri N, Coomes EA, Haghbayan H, Gunaratne K. Social media and vaccine hesitancy: new updates for the era of Covid-19 and globalized infectious diseases. Hum Vaccin Immunother. 2020;16(11):2586 2593. ( 10.1080/21645515.2020.1780846) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Limaye RJ, Holroyd TA, Blunt M, et al. Social media strategies to affect vaccine acceptance: a systematic literature review. Expert Rev Vaccines. 2021;20(8):959 973. ( 10.1080/14760584.2021.1949292) [DOI] [PubMed] [Google Scholar]
- 33. Bahk CY, Cumming M, Paushter L, Madoff LC, Thomson A, Brownstein JS. Publicly available online tool facilitates real-time monitoring of vaccine conversations and sentiments. Health Aff (Millwood). 2016;35(2):341 347. ( 10.1377/hlthaff.2015.1092) [DOI] [PubMed] [Google Scholar]
- 34. Kunneman F, Lambooij M, Wong A, Bosch AVD, Mollema L. Monitoring stance towards vaccination in twitter messages. BMC Med Inform Decis Mak. 2020;20(1):33. ( 10.1186/s12911-020-1046-y) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Yadav D, Malik P, Dabas K, Singh P. FeedPal: understanding opportunities for chatbots in breastfeeding education of women in india. Proc ACM Hum Comput Interact. 2019;3(CSCW):1 30. ( 10.1145/3359272)34322658 [DOI] [Google Scholar]
- 36. Kim Y, Jang JH, Park N, et al. Machine learning approach for active vaccine safety monitoring. J Korean Med Sci. 2021;36(31):e198. ( 10.3346/jkms.2021.36.e198) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Maserat E. Integration of artificial intelligence and crispr/cas9 system for vaccine design. Cancer Inform. 2022;21:11769351221140102. ( 10.1177/11769351221140102) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Lv H, Shi L, Berkenpas JW, et al. Application of artificial intelligence and machine learning for Covid-19 drug discovery and vaccine design. Brief Bioinform. 2021;22(6):1 10. ( 10.1093/bib/bbab320) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hederman AP, Ackerman ME. Leveraging deep learning to improve vaccine design. Trends Immunol. 2023;44(5):333 344. ( 10.1016/j.it.2023.03.002) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Verbeek T, Quittner L, De Cock P, De Groot N, Bockting CLH, Burger H. Personality traits predict meeting the who recommendation of 6 months’ breastfeeding: a prospective general population cohort study. Adv Neonatal Care. 2019;19(2):118 126. ( 10.1097/ANC.0000000000000547) [DOI] [PubMed] [Google Scholar]
- 41. Balogun OO, Dagvadorj A, Anigo KM, Ota E, Sasaki S. Factors influencing breastfeeding exclusivity during the first 6 months of life in developing countries: a quantitative and qualitative systematic review. Matern Child Nutr. 2015;11(4):433 451. ( 10.1111/mcn.12180) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Anothaisintawee T, Wiratkapun C, Lerdsitthichai P, et al. Risk factors of breast cancer: a systematic review and meta-analysis. Asia Pac J Public Health. 2013;25(5):368 387. ( 10.1177/1010539513488795) [DOI] [PubMed] [Google Scholar]
- 43. Yalçın SS, Erdal İ, Erat Nergiz M. Emzirme reklamı ve toplumda yüceltilmesi çalıştay kurulu. emzirmenin reklamı. In: Karabayır N, ed. Her Hekimin Anne Sütü Ile Beslenme Konusunda Bilmesi Gerekenler. 1st ed. Ankara: Türkiye Klinikleri; 2021:124 130. [Google Scholar]
- 44. Padró-Arocas A, Quifer-Rada P, Aguilar-Camprubí L, Mena-Tudela D. Description of an mhealth tool for breastfeeding support: lactapp. analysis of how lactating mothers seek support at critical breastfeeding points and according to their infant’s age. Res Nurs Health. 2021;44(1):173 186. ( 10.1002/nur.22095) [DOI] [PubMed] [Google Scholar]
- 45. Çelik M, Yalçin S. Literacy of healthcare personnel in türkiye about the international code of marketing of breastmilk substitutes. East Mediterr Health J. 2023;29(5):335 342. ( 10.26719/emhj.23.048) [DOI] [PubMed] [Google Scholar]
- 46. Oyebode O, Lomotey R, Orji R. ‘I tried to breastfeed but...’: exploring factors influencing breastfeeding behaviours based on tweets using machine learning and thematic analysis. IEEE Access. 2021;9:61074 61089. ( 10.1109/ACCESS.2021.3073079) [DOI] [Google Scholar]
- 47. Yusuf JO, Miyim AM. Predicting breastfeeding practice of Nigerian child using machine learning and deep learning algorithms. Dutse J Pure Appl Sci. 2022;7(4a):183 193. ( 10.4314/dujopas.v7i4a.19) [DOI] [Google Scholar]
- 48. Oliver-Roig A, Rico-Juan JR, Richart-Martínez M, Cabrero-García J. Predicting exclusive breastfeeding in maternity wards using machine learning techniques. Comput Methods Programs Biomed. 2022;221:106837. ( 10.1016/j.cmpb.2022.106837) [DOI] [PubMed] [Google Scholar]
- 49. Yalçın SS. Büyümenin izlenmesi ve değerlendirilmesi. In: Yurdakök K, Yalçın SS, eds. Yurdakök Pediatri. 1st ed. Ankara: Güneş Tıp Kitabevleri; 2017:115 187. [Google Scholar]
- 50. Force CT, Care PH. Recommendations for growth monitoring, and prevention and management of overweight and obesity in children and youth in primary care. Can Med Assoc J. 2015;187(6):411 421. ( 10.1503/cmaj.141285) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Hall DMB. Growth monitoring. Arch Dis Child. 2000;82(1):10 15. ( 10.1136/adc.82.1.10) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Yalçın N, Kaşıkcı M, Çelik HT, Demirkan K, Yiğit Ş, Yurdakök M. Development and validation of machine learning-based clinical decision support tool for identifying malnutrition in nicu patients. Sci Rep. 2023;13(1):5227. ( 10.1038/s41598-023-32570-z) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Rescinito R, Ratti M, Payedimarri AB, Panella M. Prediction models for intrauterine growth restriction using artificial intelligence and machine learning: a systematic review and meta-analysis. Healthcare (Basel). 2023;11(11):1 17. ( 10.3390/healthcare11111617) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Agency for Toxic Substances and Disease Registry. Why Are Children often Especially Susceptible to the Adverse Effects of Environmental Toxicants? available at https://www.atsdr.cdc.gov/csem/pediatric-environmental-health/why_children.html accessed Accessed December 20 2023. [Google Scholar]
- 55. Lobo GP, Kalyan B, Gadgil AJ. Predicting childhood lead exposure at an aggregated level using machine learning. Int J Hyg Environ Health. 2021;238:113862. ( 10.1016/j.ijheh.2021.113862) [DOI] [PubMed] [Google Scholar]
- 56. Oskar S, Stingone JA. Machine learning within studies of early-life environmental exposures and child health: review of the current literature and discussion of next steps. Curr Environ Heal Rep. 2020;7(3):170 184. ( 10.1007/s40572-020-00282-5) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Rana R, Kalia A, Boora A, et al. Artificial intelligence for surface water quality evaluation, monitoring and assessment. Water. 2023;15(22):3919. ( 10.3390/w15223919) [DOI] [Google Scholar]
- 58. Xiang X, Li Q, Khan S, Khalaf OI. Urban water resource management for sustainable environment planning using artificial intelligence techniques. Environ Impact Assess Rev. 2021;86:106515. ( 10.1016/j.eiar.2020.106515) [DOI] [Google Scholar]
- 59. Nkiruka O, Prasad R, Clement O. Prediction of malaria incidence using climate variability and machine learning. Inform Med Unlocked. 2021;22. ( 10.1016/j.imu.2020.100508) [DOI] [Google Scholar]
- 60. Hirano Y, Kondo Y, Hifumi T, et al. Machine learning-based mortality prediction model for heat-related illness. Sci Rep. 2021;11(1):9501. ( 10.1038/s41598-021-88581-1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Rudan I, Tomaskovic L, Boschi-Pinto C, Campbell H, WHO Child Health Epidemiology Reference Group. Global estimate of the incidence of clinical pneumonia among children under five years of age. Bull World Health Organ. 2004;82(12):895 903. [PMC free article] [PubMed] [Google Scholar]
- 62. Chang TH, Liu YC, Lin SR, et al. Clinical characteristics of hospitalized children with community-acquired pneumonia and respiratory infections: using machine learning approaches to support pathogen prediction at admission. J Microbiol Immunol Infect. 2023;56(4):772 781. ( 10.1016/j.jmii.2023.04.011) [DOI] [PubMed] [Google Scholar]
- 63. Villafuerte N, Manzano S, Ayala P, García MV. Artificial intelligence in virtual telemedicine triage: a respiratory infection diagnosis tool with electronic measuring device. Futur Internet. 2023;15(7):227. ( 10.3390/fi15070227) [DOI] [Google Scholar]
- 64. Tso CF, Lam C, Calvert J, Mao Q. Machine learning early prediction of respiratory syncytial virus in pediatric hospitalized patients. Front Pediatr. 2022;10(August):886212. ( 10.3389/fped.2022.886212) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Graves NS. Acute gastroenteritis. Prim Care. 2013;40(3):727 741. ( 10.1016/j.pop.2013.05.006) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Guarino A, Aguilar J, Berkley J, et al. Acute gastroenteritis in children of the world: what needs to be done? J Pediatr Gastroenterol Nutr. 2020;70(5):694 701. ( 10.1097/MPG.0000000000002669) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Yurdakök K, Yalçin SS, Ozmert E. Experience with oral rehydration therapy in moderately dehydrated children due to diarrhea. Turk J Pediatr. 1997;39(1):19 25. [PubMed] [Google Scholar]
- 68. Kim YJ, Park KH, Park DA, et al. Guideline for the antibiotic use in acute gastroenteritis. Infect Chemother. 2019;51(2):217 243. ( 10.3947/ic.2019.51.2.217) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Miyagi Y. Identification of pediatric bacterial gastroenteritis from blood counts and interviews based on machine learning. Cureus. 2023;15(8):e43644. ( 10.7759/cureus.43644) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Ucuz I, Ari A, Ozcan OO, Topaktas O, Sarraf M, Dogan O. Estimation of the development of depression and ptsd in children exposed to sexual abuse and development of decision support systems by using artificial intelligence. J Child Sex Abus. 2022;31(1):73 85. ( 10.1080/10538712.2020.1841350) [DOI] [PubMed] [Google Scholar]
- 71. Amrit C, Paauw T, Aly R, Lavric M. Identifying child abuse through text mining and machine learning. Expert Syst Appl. 2017;88:402 418. ( 10.1016/j.eswa.2017.06.035) [DOI] [Google Scholar]
- 72. Shum M, Hsiao A, Teng W, Asnes A, Amrhein J, Tiyyagura G. Natural language processing — a surveillance stepping stone to identify child abuse. Acad Pediatr. 2024;24(1):92 96. ( 10.1016/j.acap.2023.08.015) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Morley J, Machado CCV, Burr C, et al. The ethics of ai in health care: a mapping review. Soc Sci Med. 2020;260(June):113172. ( 10.1016/j.socscimed.2020.113172) [DOI] [PubMed] [Google Scholar]
- 74. Shrestha S, Das S. Exploring gender biases in ml and ai academic research through systematic literature review. Front Artif Intell. 2022;5:976838. ( 10.3389/frai.2022.976838) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Anderson M, Anderson SL. How should ai be developed, validated, and implemented in patient care? AMA J Ethics. 2019;21(2):E125 E130. ( 10.1001/amajethics.2019.125) [DOI] [PubMed] [Google Scholar]



 Content of this journal is licensed under a
Content of this journal is licensed under a