Abstract
Background
Epigenetics and clinical observations referring to Betacoronavirus lead to the conjecture that Sarbecovirus may have the ability to infect lymphocytes using a different way than the spike protein. In addition to inducing the death of lymphocytes, thus drastically reducing their population and causing a serious immune deficiency, allows it to remain hidden for long periods of latency using them as a viral reservoir in what is named Long-Covid Disease. Exploring possibilities, the hypothesis is focused on that N protein may be the key of infecting lymphocytes.
Method
The present article exhibits a computational assay for the latest complete sequences reported to GISAID, correlating N genotypes with an enhancement in the affinity of the complex that causes immune deficiency in order to determine a good docking with the N protein and some receptors in lymphocytes.
Results
A novel high-interaction coupling of N-RBD and CD147 is presented as the main way of infecting lymphocytes, allowing to define those genotypes involved in their affinity enhancement.
Conclusion
The hypothesis is consistent with the mutagenic deriving observed on the in-silico assay, which reveals that genotypes N/120 and N/152 are determinant to reduce the Immune Response of the host infecting lymphocytes, allowing the virus persists indefinitely and causing an Acquire Immune Deficiency Syndrome.
Keywords: Long-Covid disease, SARS-CoV-2, Acquired Immune Deficiency Syndrome, AIDS, Artificial intelligence, Bioinformatics
Graphical abstract
Highlights
-
•
Genotypes N/120 and N/152 of SARS-CoV-2 have been identified in the acquired immuno-deficiency scope caused by Sarbecovirus.
-
•
A new binding site for the Sarbecovirus N protein is proposed as the main route of infection of lymphocytes through CD147 receptors.
-
•
Immune dysregulation caused by infection of CD147 lymphocytes is consistent with clinical data of severe and Long Covid cases.
At a glance commentary
Scientific background on the subject
The study of pathogen genotypes, in correlation with their pathogenesis, provides the basis for the phenotypes of different clades of specimens. By providing a theory that explains these correlations, phenotypes are well defined. Computing molecular dynamics is a powerful method to define the proteomic interactions that explain these correlations.
What this study adds to the field
In genomics, defining phenotypes is the objective. This in-silico assay provides the scientific rationale to define phenotypes that can cause acquired immunodeficiency following acute virosis due to some sarbecoviruses. This phenotypes are essential knowledge for biomedical science
Introduction
In SARS outbreak of 2003 lymphopenia (in particular T lymphopenia) was the most common clinical evidence (98% of patients) during the course of illness. A notable drop in CD4 and CD8 lymphocyte counts occurred early in the course of the syndrome and it was associated with adverse outcomes [1]. In contrast, in SARS-CoV-2 lymphopenia is not the most common clinical entity (40% of patients) [2], which suggests that some important tropism related to the metabolic pathways where lymphocytes are involved is an evolutionary key in SARS coronavirus.
Lymphopenia as a major immunological abnormality that occurs in the majority (72%) [3] of severe COVID-19 patients, can cause general immunosuppression facilitating viral persistence [4]. Lymphopenia can be inherited or acquired. Acquired lymphopenia can be due to different biological conditions and disorders, however it is mainly related to HIV and other viral infections. Thus, various molecular and cellular mechanisms participate in the occurrence of acquired lymphopenia.
Clinical data reveals bone marrow impairment [3] by suppressing the development of hematopoietic precursor cells through elevated expression of CXCL10 (IP-10) and CCL2 (MCP-1). Dysregulation of the host immune response, as a hallmark of severe SARS-CoV-2 infections [5], results in an uncontrolled release of serum cytokines, especially interleukin-6 (IL-6), which correlates with disease severity [6] suppressing lymphopoiesis via direct effects on hematopoietic stem/progenitor cells [[7], [8], [9]].
Other studies point to clinical observations related to metabolic pathways of apoptosis. A high expression of P53 was measured in COVID-19 patients [3] suggesting that lymphopenia may be secondary to apoptosis triggered by P53 [10] over-expression. In addition, Antibody-Dependent Enhancement can as well induce apoptosis [11].
But the major evidence we found for the primary etiology is that lymphocytes are infected by SARS-CoV-2 [12] and when it happens viroporin 3a (ORF3a) [13] interacts with NLRP3 causing pyroptosis [14]. Pyroptotic immune cell-secreted pro-inflammatory cytokines might worse lymphopenia via the direct killing of lymphocytes, contributing to the dysfunction of adaptive immunity in COVID-19, and it is very well correlated with COVID-19 immunopathogenesis [15].
Even when SARS-related coronaviruses (SARS-CoVs) can hardly replicate in lymphocytes [16] due to rapid apoptosis or pyroptosis, and even when only a few times pyroptosis happens, virions from inside the lymphocyte can release intact outside, ready to infect another T-cells.
This casuistic is a very clear picture of the strategy for viral persistence. The natural evolution of SARS-CoVs, in addition to spread-out more effectively by air, is to reduce the response capacity of the immune system to persist longer in the host, causing Acquired Immune Deficiency Syndrome.
However, the way that SARS-CoV-2 can infect T-cells is not very clear nowadays. ACE2 is not very much expressed in lymphocytes [17] so other ligands must be considered, such as CD147, cyclophilins, CD26 and LFA-1 [18] very well expressed in lymphocytes. Interaction between CD147 and the N protein of SARS-CoV-2 (CoV2N) through CypA has been described in 2021 by Cervera-Grau and Bermejo-Valdés [19]. However, not only does protein N interact with CD147, but the SARS-CoV-2 S-RBD [20] can also bind to it.
CD147 is a transmembrane glycoprotein of the immunoglobulin superfamily also known as basigin or extracellular matrix metalloprotease inducer (EMMPRIN). It is the main tissue inducer of matrix metalloproteases (MMPs), and also induces vascular endothelial growth factor production. It plays a role in intercellular recognition and cancer cell survival (mostly by controlling lactate transport), its expression is increased in hypoxic states and in many cancers, and it is considered to be a biomarker for cancer diagnosis and prognosis [21]. In addition, it has been observed that CD147 expression levels correlate with SARS-CoV-2 infection extent, vascular damage, and an increased expression of vascular endothelial growth factor and thrombosis.
Serum CD147 is involved in Plasmodium falciparum infection, and an antibody produced in that disease (HP6H8) blocks the entry to the host cells, as in this clinical trial was purposed [22]. Despite the undesirable, and very unknown, effects of blocking CD147 functionality, which is not only restricted to transmembrane signaling, if this monoclonal can avoid the binding of CoV2N an aligned docking with that must contain that N-genotypes that cause a higher rate of AIDS following SARS-CoV-2 infection.
Following that observations, we focus on the hypothesis that Betacoronavirus, especially from the phylogenesis of Sarbecovirus, has the potential to cause an Acquired Immune Deficiency Syndrome as the main objective of persistence, potentiated by respiratory disease as a vehicle of rapid propagation and dissemination for its maturation affinity to infect lymphocytes.
Thus, in order to elevate this hypothesis to theory we perform an artificial intelligence-driven assay wrangling the latest full-length sequences reported to GISAID, correlating those genotypes with the protein complexes implied in the clinical scope of immunodeficiency, specifically with those receptors that are very expressed in lymphocytes.
Materials and methods
Primary Data Set has been retrieved from GISAID [23], NEXTSTRAIN [24], The Protein Data Bank [25] and worldwide data on COVID-19 sources [26]. Scopes have been defined by an Associative Information Model with this Primary Data Set and the clinical information crawled by the keywords supported during the proceeding.
The prototype (TRL9) of CliniXy platform for Clinical Research Artificial Intelligence Driven, produce bioinformatics analysis proceeding with the aim of determining which genotypes exhibit an evolutionary potential to gain for the objective targeted, by wrangling scopes dynamically integrating the following modules and subsystems:
-
•APBS Electrostatics Plug-in [27], to calculate electrostatic potential molecular surface.
- The Poisson–Boltzmann equation allows determining the electrical potential distribution of the molecular surface of a protein. These values are essential to determine how electrostatic interactions will affect the molecules in their coupling.
-
•ColabFold [28] based on AlphaFold2 [29] framework under Colab environment for modeling molecular structures from amino-acid sequences.
- AlphaFold2 is the most accurate and fastest method to predict molecular structures. It is based on a Deep Learning mechanism of an Artificial Intelligence model based on experimental data structures weighted by vectors of amino acid sequences that raise the precision above 90%.
-
•Implementation of MM-ISMSA [30] method which is used for fast and accurate docking/binding.
- This method is based on the calculation of Implicit Solvent Model, including hydrogen bonding term and individual desolvation penalties for each protein-ligand complex atom neighbors, and the Surface Area contribution of the protein–protein complex formation due to the loss of water bindings, in addition of Molecular Mechanics based on 12-6 Lennard-Jones potential for docking accuracy.
Pymol 2.4 [31] has been used for analysis interpretation and graphical representations for report results.
Results
Correlated receptors for the objective targeted were found in the following PDB entries:
6LZG: Structure of novel coronavirus spike receptor-binding domain complexed with its receptor ACE2.
5X07T: Crystal structure of CD147 C2 domain in complex with Fab of its monoclonal antibody 6H8.
4U0Q: Plasmodium falciparum reticulocyte-binding protein homologue 5 (PfRH5) bound to basigin.
7R98: Structure of the SARS-CoV-2 N protein RNA-binding domain bound to single-domain antibody B6.
2OFZ: Ultrahigh Resolution Crystal Structure of RNA Binding Domain of SARS Nucleocapsid (N Protein) at 1.1 Angstrom Resolution in Monoclinic Form.
4J3K: Structure of the N-terminal domain of human coronavirus OC43 nucleocapsid protein.
7LGT: HLA-B∗07:02 in complex with 229E-derived coronavirus nucleocapsid peptide N75-83.
7N45: Solution NMR structure of the N-terminal globular domain of the endemic HKU1 coronavirus nucleocapsid protein.
6LZ6: Crystal structure of MERS-CoV N-NTD complexed with ligand P4-3.
5N4K: N-terminal domain of a human Coronavirus NL63 nucleocapsid protein.
7T9L: Cryo-EM structure of SARS-CoV-2 Omicron spike protein in complex with human ACE2 (focused refinement of RBD and ACE2)
From these items, several domains were identified, isolated, and cleaned for wrangle dockings. Docking between CD147 and monoclonal antibody 6H8 was calculated and ranked with the best fit [Fig. 1] and desolvation energy for the complex (ΔG) was estimated in −141.28499 kcal/mol by MM-ISMSA method1.
Fig. 1.
Meplazumab 6H8 monoclonal docking with CD147 Domain 1.
Docking between SARS-CoV-2 spike protein (CoV2S) was found [Fig. 2] very close to the same ligand domain with a ΔG estimated of −62.58 kcal/mol. That result fits very well with the MMGBSA calculation exposed in Molecular basis of the potential interaction of SARS-CoV-2 spike protein to CD147 in COVID-19 associated-lymphopenia table 1 [20].
Fig. 2.
SARS-CoV-2 Spike protein docking with CD147 D1.
Different good bindings for the protein N of SARS-CoV-2 (CoV2N) were found, precisely one in the same domain area of ligand CD147 with the 6H8 monoclonal at a ΔG estimated on −142.23 kcal/mol as can be seen in the top of [Fig. 3]. Crawling sequences uploaded to GISAID, mutations of CoV2N for this docking were found at 135, 136, 141, 142, 151, and 152 positions. Main mutation from protein N of SARS-CoV (CoV1N) is focused in 152 position (correlated with the sequence of CoV2N) as can be seen in the bottom picture of [Fig. 3]. In addition binding of CoV1N-CD147D1 was 8% higher (−154.39 kcal/mol) due to this mutation than the wild-type CoV2N from Wuhan. Similarly, CoV1N has worse binding than HKU1 protein N (HKU1N) with CD147-D1 due to mutations on 152 and 158 which shows a very good affinity where relative to CoV2N codon 120 is determinant [Fig. 4].
Fig. 3.
SARS-CoV-2 N and SARS-CoV N protein mutations in docking with CD147 D1.
Fig. 4.
HKU1 N protein docking with CD147 D1.
Mutations for a better fitting in the same domain from NL63 and OC43 protein N with the same ligand domain of CD147 were evidenced [Fig. 5], as well as a very good binding (−143 kcal/mol) in the same area with the MERS-CoV of 2012 [Fig. 6]. No evidence of docking with CD147 in the same place was found for 299E coronavirus but a weak alignment with OC-43.
Fig. 5.
Mutations for enhance fitting N-CD147 in NL63 and OC43.
Fig. 6.
Docking of MERS-Cov N protein with CD147.
No other significant protein interactions with the SARS-CoV-2 N protein were found in the scope of immunodeficiency.
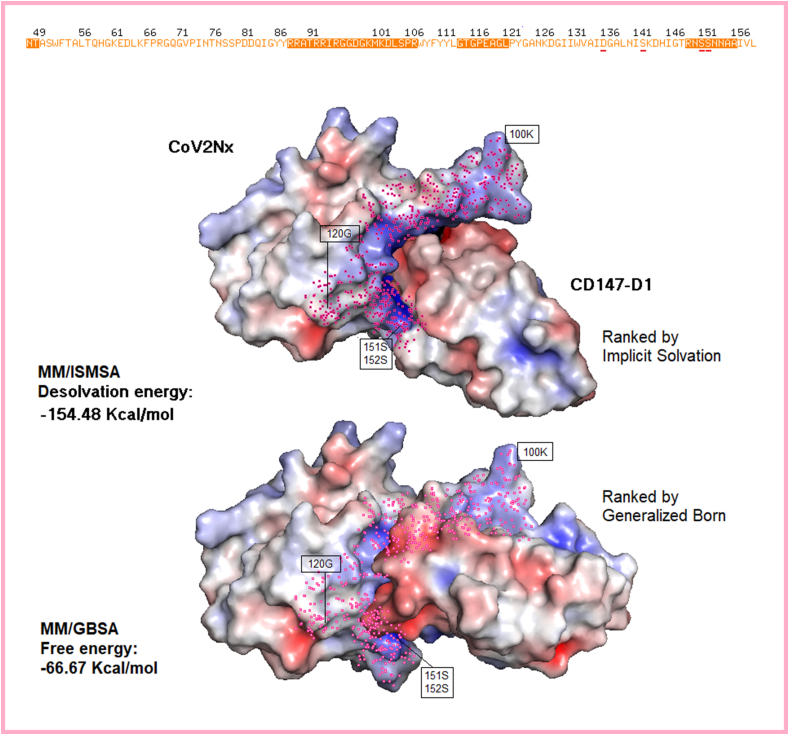
A new structure (CoV2Nx) has been predicted in [Fig. 7]as evolution in the short time of the SARS-CoV-2 N protein having into account mutations crawled from GISAID records. This new structure gains more than 8% affinity to raise −154.48 kcal/mol, similar to N protein of SARS-CoV (CoV1N).
Fig. 7.
Dockings of new predicted SARS-CoV-2 N protein with CD147.
Antibodies with high affinity for this receptor domain were not found in the Protein Data Bank, except monoclonal B6. Antibody B6 is reducing its affinity directly for mutations 120 and 136 as well as by allosteric regulation of others [Fig. 8 top]. Positions 68, 136, 137 and 139 from predicted new N protein collide with the antibody NAb-B6 [Fig. 8 down].
Fig. 8.
Nano-body B6 affinity with wild type SARS-CoV-2 N protein versus predicted new protein N.
Discussion
The hypothesis presented in the introduction states that Betacoronavirus, especially from the phylogenesis of Sarbecovirus, has the potential to cause an Acquired Immune Deficiency Syndrome as the main objective of persistence, potentiated by respiratory disease as a vehicle of rapid propagation and dissemination for its maturation affinity to infect lymphocytes.
As it has been exposed as well in the introduction the objective of this manuscript is to elevate this hypothesis to theory by performing an artificial intelligence-driven assay wrangling the latest full-length sequences reported to GISAID, correlating those genotypes with the protein complexes implied in the clinical scope of immunodeficiency.
Without prejudice to the fact that it would be desirable to extend this research with observational trials and other empirical assays, In-Silico assays, as a purely logical method, are sufficient to consolidate a hypothesis based on observations as theories, as it is widely accepted in science and biotechnology [32] after Karl Popper stated in various books and very well compiled in “The Two Fundamental Problems of the Theory of Knowledge” [33]. GISAID sequences are experiments that complement clinical observations referred and while no observation (nor another logical assertion) contradicts the results of the logical method, the hypothesis may be considered a correct theory. As Karl Popper said, experiments do not confirm hypotheses, but theories must be falsifiable, and this theory can be falsifiable easily as long as lymphocytes will not be infected (or have a very low incidence) by SARS-CoV-2 when a subject has a high titer of spike's protein neutralizing antibodies. As we have observed during more than 2 years of vaccination with SARS-CoV-2 S protein, people with high titer of antibodies against S protein are being hospitalized with lymphopenia.
Due to the results of the in-silico assay, it is obvious that positions 27, 28, and 100 of the CD147-D1 protein compete for binding with both protein N and protein S. However, competition for the best binding in these corresponding positions of protein S (specifically the positions 481, 484 and 493) are determinant in binding to ACE2.
Improvement in the affinity of S protein with CD147 is compromising the affinity of protein S with ACE2, which finds its best genotype in the S/493Q genotype, as was already reported in January 2022 [34], and as well with S/484K which was advised in march 2021 [35].
A triple mutation that improves the affinity in both ligands (ACE2 and CD147) is extremely remote, so as it is advantageous for propagation to infect respiratory tissue, the natural evolution of SARS-CoVs is to improve the affinity of S with ACE2 to the detriment of lymphocyte invasion.
However, infecting lymphocytes gives coronaviruses the ability to prolong the period of contagiousness by delaying the immune response, obviously, without causing a sudden fatality, as was the case in 2003 with SARS-CoV.
Mutations on S and N genes from SARS-CoV (CoV1) to SARS-Cov-2 (CoV2) according to the results are a natural evolution of CoV1 to improve the affinity with ACE2 at the cost of reducing the invasive capacity of lymphocytes, and this is how it behaved.
The N protein of the 2003 SARS-CoV coronavirus (CoV1N) respecting the Wild Type of SARS-CoV-2, has 8 mutations in the NTD zone. Taking the SARS-CoV-2 alignment as a reference, these mutations occur at codons 63, 94, 103, 120, 128, 131, 152 and 157. Mutations A120G, P152A, and A157I of the N protein directly affect binding to CD147-D1, reducing its affinity by 8% [142:154] compared to SARS-CoV 2003. However, CoV2-S binds ACE2 30% [85:65] better than CoV1-S to ACE2.
Reduction in affinity with CD147, as has been observed, leads to a reduction of lethality. However, it is still enough to compromise the immune system, postpone the humoral response and promote viral persistence.
On the other hand, these 8 mutations are enough so that the same antibodies that are capable of neutralizing the entry of SARS-CoV-1 into CD8+ lymphocytes are incompetent with SARS-CoV-2.
SARS-CoV-1 antibody-dependent enhancement (ADE) of infection was related in 2005 [36] hypothesizing that it was due to a previous infection with other Betacoronavirus. ADE has also been well documented in cats infected with the Feline Infectious Peritonitis Coronavirus, in which disease severity is increased following previous immunization against this virus.
Just as the S protein only has a receptor in the Sarbecovirus sub-lineages that include SARS, the N protein is present in other sub-lineages of the Betacoronavirus genera.
Coronaviruses OC43, NL63, HKU1, and 229E are responsible for the common cold [37] and since the 1970s they have been suspected of contributing negatively to the co-infection with other viruses, reducing the response of the immune system.
Although the sequences of the N protein in other coronaviruses may appear very different, their morphology, especially regarding the amino acids closest to the CD147-D1 ligand, shows fairly well-conserved homology.
Specifically, positions 50 and 123 of OC43 have mutated to improve affinity with CD147-D1. Despite the N protein of Coronavirus 229E (229E-N) does not show a good morphological coupling with CD147-D1, a clear alignment with OC43-N is observed, suggesting a recombination or evolution from that.
Protein N of HKU1 (HKU1N) shows a very clear homology with CoV2N. HKU1N results in a better binding than CoV1N mainly due to codon number 120 (over the numeration of the CoV2N sequence). As we have seen before, the mutation in this codon directly affects the binding. So we can say that the N/120N genotype is decisive in improving affinity. Likewise, the region between positions 148 and 154 allows a considerable improvement. In fact, any mutation at positions close to 148 and 154 must be considered decisively evolutionary.
Even when HKU1 does not present good affinity with ACE2, since HCoV-OC43 and HCoV-HKU1 employ glycan-based receptors carrying 9-O-acetylated sialic acid [38] and it is very well conserved between them [39] it presented in 2016 (from February to March) a very high rate of hospitalizations (54%) and a very high rate of ICU admission (30%) [40], so in fact, HKU1 severity must be due to HKU1N-CD147 binding.
Furthermore, although more unlikely, recombination is possible as Patrick Y.C. Wooo warned already in 2006 [41].
Therefore, people who have been exposed to previous Coronavirus SARS-CoV-1, HKU1, OC43, NL63 or MERS, will see their cellular response affected against the N protein of CoV2 as well as in the production of new neutralizing antibodies, making lymphocytes more vulnerable and thus aggravating the course of the disease.
Based on the available data on COVID-19 patients and data from the previous SARS-CoV-1 and MERS outbreaks, there is substantial evidence that cross-reactive B and T cell responses may establish an unfavorable environment for the primary immune response to SARS-CoV-2 virus [42].
Due to cross-reaction to related coronavirus strains from earlier infections, and after results here exposed, the patient's viral history of coronavirus infection might be crucial to the severity of the course of the current infection with SARS-CoV-2; a phenomenon that has been called “original antigenic sin” [43].
Results are showing that the most recent mutations for the binding zone with CD147-D1, are deriving in an enhanced affinity and immune evasion of previous CoV2N antibodies, as well as compromise the reliability of rapid antigen tests that are directed to this protein [44].
The sequence (CoV2Nx) contains the 4 highest-risk mutations that have emerged in recent months2:
The structure of this sequence predicted by AlphaFold2 shows a very high morphological alteration. According to molecular dynamics simulation, CoV2Nx improves affinity to CD147-D1 by 8% [142:154] relative to CoV2N, matching the lethal capacity of CoV1N. With this new structure, the antibodies that recognize the antigens of the CoV2N protein suffer collisions at positions 68, 136, 137, and 139.
Desolvation energy at the antigenic recognition region by previous antibodies is reduced below 30% (61% according to the simulation) which suggests that both cellular memory and previous antibodies may be incompetent for these new variants.
From the process of more than 8 million experimental data registered in GISAID, an immunological escape mechanism and a greater probability of developing Acquired Immune Deficiency Syndrome by SARS-CoV-2 are observed, according to the mutations in the N gene deriving towards a Variant of Concern with a higher rate of systemic commitment.
Conclusions
According to the results of the In-Silico, it is evidenced a natural evolution of the Betacoronavirus genera in order to balance propagation, infectivity and persistence. The main genotypes are evidenced in S/493, S/484, N/120 and N/152. Optimizing S/493 and S/484 means better airborne spread by infecting more the lungs and nasopharyngeal tissue meanwhile N/120 and N/152 genotypes reduce the Immune Response infecting lymphocytes allowing the virus to persist indefinitely, causing an Acquire Immune Deficiency Syndrome and other related syndromes to chronic viremia, especially with viruses that cause respiratory and blood diseases.
Acknowledgments
First of all, we thank the authors and the laboratories of origin, for the more than 8 million sequences sent to the GISAID database, which are the raw material for this research, as well as to the contributors of The Protein Data Bank and NEXSTRAIN for their extensive and excellent work that allows us to make science more accessible for everyone.
This document is the result of independent research work carried out by the authors without any profit motive and with no greater interest than the science behind it.
Special thanks to Alexander Ariel Padrón González, David Abia Holgado, Jose Manuel Cervera Grau, Francisco Javier García Palomo and Patricia Obregón Calderón for helping us better understand the science and technique underlying this article.
Peer review under responsibility of Chang Gung University.
The desolvation energy value from the MMISMSA method represents the sum of the nonpolar energy of the complex to the solvation energies of the individual ligand and protein. These values are presented only to evaluate and compare the affinity in different dockings, they should not be considered as the Gibbs free energy.
Updates and discussion can be followed at https://ixilka.net/CoV2Nx
References
- 1.Wong Raymond SM, Wu Alan, To KF, Lee Nelson, Lam Christopher WK. Wong CK, et al. Haematological manifestations in patients with severe acute respiratory syndrome: retrospective analysis. Br Med J. 2003;326(7403):1358–1362. doi: 10.1136/bmj.326.7403.1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z,et al. Clinical course and risk factors for mortality of adult inpatients with covid-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jafarzadeh A, Jafarzadeh S, Nozari P, Mokhtari P, Nemati M. Lymphopenia an important immunological abnormality in patients with covid-19: possible mechanisms. Scand J Immunol. 2021;93(2) doi: 10.1111/sji.12967. [DOI] [PubMed] [Google Scholar]
- 4.Lamontagne Lucie, Descoteaux JP, Jolicoeur Pierre. Mouse hepatitis virus 3 replication in t and b lymphocytes correlate with viral pathogenicity. J Immunol. 1989;142(12):4458–4465. [PubMed] [Google Scholar]
- 5.Domingo P, Mur I, Pomar V, Corominas H, Casademont J, de Benito N. The four horsemen of a viral apocalypse: the pathogenesis of sars-cov-2 infection (covid-19) EBioMedicine. 2020;58 doi: 10.1016/j.ebiom.2020.102887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wan S, Yi Q, Fan S, Lv J, Zhang X, Guo L, et al. Relationships among lymphocyte subsets, cytokines, and the pulmonary inflammation index in coronavirus (covid-19) infected patients. Br J Haematol. 2020;189(3):428–437. doi: 10.1111/bjh.16659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maeda K, Malykhin A, Teague-Weber BN, Sun XH, Farris AD, Coggeshall KM. Interleukin-6 aborts lymphopoiesis and elevates production of myeloid cells in systemic lupus erythematosus–prone B6.Sle1.Yaa animals. Blood. 2009;113(19):4534–4540. doi: 10.1182/blood-2008-12-192559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Channappanavar R, Perlman S. Pathogenic human coronavirus infections: causes and consequences of cytokine storm and immunopathology. Semin Immunopathol. 2017;39(5):529-39 doi: 10.1007/s00281-017-0629-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Masiá Mar, Fernández-González M, García JA, Padilla S, García-Abellán J Botella Ángela, et al. Robust long-term immunity to SARS-CoV-2 in patients recovered from severe COVID-19 after interleukin-6 blockade. EBioMedicine. 2022;82:104153. doi: 10.1016/j.ebiom.2022.104153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aubrey BJ, Kelly GL, Janic A, Herold MJ, Strasser A. How does P53 induce apoptosis and how does this relate to P53-mediated tumour suppression? Cell Death Differ. 2018;25(1):103–113. doi: 10.1038/cdd.2017.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ricke D O. Two different Antibody-Dependent Enhancement (ADE) risks for SARS-CoV-2 antibodies. Front Immunol. 2021;12 doi: 10.3389/fimmu.2021.640093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brunetti NS, Davanzo GG, de Moraes D, Ferrari AJR, Souza GF, et al. SARS-CoV-2 uses CD4 to infect T helper lymphocytes. Elife. 2023;12 doi: 10.7554/eLife.84790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang J, Ejikemeuwa A, Gerzanich V, Nasr M, Tang Q, Simard JM, et al. Understanding the role of SARS-CoV-2 ORF3a in viral pathogenesis and COVID-19. Front Microbiol. 2022;13 doi: 10.3389/fmicb.2022.854567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen IY, Miyu Moriyama, Chang MF, Takeshi Ichinohe. Severe acute respiratory syndrome coronavirus viroporin 3a activates the NLRP3 inflammasome. Front Microbiol. 2019;10:50 doi: 10.3389/fmicb.2019.00050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang M, Chang W, Zhang L, Zhang Y. Pyroptotic cell death in sars-cov-2 infection: revealing its roles during the immunopathogenesis of covid-19. Int J Biol Sci. 2022;18(15):5827–5848. doi: 10.7150/ijbs.77561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yilla M, Harcourt BH, HickMan CJ, McGrew M, Tamin A, Goldsmith C S., et al. SARS-coronavirus replication in human peripheral monocytes/macrophages. Virus Res. 2005;107(1):93–101. doi: 10.1016/j.virusres.2004.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Radzikowska U, Ding M, Tan G, Zhakparov D, Peng Y, Wawrzyniak P, et al. Distribution of ACE2, CD147, CD26, and other SARS-CoV-2 associated molecules in tissues and immune cells in health and in asthma, copd, obesity, hypertension, and COVID-19 risk factors. Allergy. 2020;75(11):2829–2845. doi: 10.1111/all.14429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shen XR, Geng R, Li Q, Chen Y, Li SF, Wang Q, et al. ACE2-independent infection of T lymphocytes by SARS-CoV-2. Signal Transduct Target Ther. 2022;7(1):83. doi: 10.1038/s41392-022-00919-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bermejo-Valdés AJ, Cervera-Grau JM. Lighting up dark areas of COVID-19. Ann Case Report. 2020;14:394. [Google Scholar]
- 20.Helal M A, Shouman S, Abdelwaly A, Elmehrath A O. Essawy M, Sayed SM, et al. Molecular basis of the potential interaction of SARS-CoV-2 spike protein to CD147 in COVID-19 associated-lymphopenia. J Biomol Struct Dyn. 2022;40(3):1109–1119. doi: 10.1080/07391102.2020.1822208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Łacina P, Butrym A, Turlej E, Stachowicz-Suhs M, Wietrzyk J, Mazur G, et al. BSG (CD147) serum level and genetic variants are associated with overall survival in acute myeloid leukaemia. J Clin Med. 2022;11(2):332. doi: 10.3390/jcm11020332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tang-Du Hospital. Clinical study of anti-CD147 humanized meplazumab for injection to treat with 2019-nCoV pneumonia. https://clinicaltrials.gov/study/NCT04275245
- 23.GISAID (Global Initiative on Sharing All Influenza Data),https://gisaid.org/. [DOI] [PMC free article] [PubMed]
- 24.Hadfield J, Megill C, Bell SM, Huddleston J, Potter B, et al. Nextstrain: real-time tracking of pathogen evolution. Bioinformatics. 2018;34(23):4121-3. [DOI] [PMC free article] [PubMed]
- 25.Berman HM, Westbrook J, Feng Z, Gilliland G, Bhat TN, Weissig H, et al. The Protein Data Bank. Nucleic Acids Res. 2000;28(1):235-42. [DOI] [PMC free article] [PubMed]
- 26.European Centre for Disease Prevention and Control. Sources - Worldwide data on COVID-19, https://www.ecdc.europa.eu/en/publications-data/sources-worldwide-data-covid-19.
- 27.Jurrus E, Engel D, Star K, Monson K, Brandi J, Felberg LE, et al. Improvements to the APBS biomolecular solvation software suite. Protein Sci. 2018;27(1):112–128. doi: 10.1002/pro.3280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mirdita M, Schütze K, Moriwaki Y, Heo L, Ovchinnikov S, Steinegger M. ColabFold: making protein folding accessible to all.Nat Methods. 2022 ;19(6):679-82. [DOI] [PMC free article] [PubMed]
- 29.AlphaFold - DeepMind, https://deepmind.google/technologies/alphafold/.
- 30.Klett J, Núñez-Salgado A, Dos Santos HG, Cortés-Cabrera Á, Perona A, Gil-Redondo R, et al. MM-ISMSA: an ultrafast and accurate scoring function for protein–protein docking. J Chem Theory Comput. 2012;8(9):3395–3408. doi: 10.1021/ct300497z. [DOI] [PubMed] [Google Scholar]
- 31.Schrödinger, LLC. The PyMOL molecular graphics system. https://pymol.org/support.html version 2.4.
- 32.Khan A, Khan S, Shoaib S, Nizam-Uddin N, Mohammad A Khan T, et al. Immunogenomics guided design of immunomodulatory multi-epitope subunit vaccine against the SARS-CoV-2 new variants, and its validation through in silico cloning and immune simulation. Comput Biol Med. 2021;133:104420. doi: 10.1016/j.compbiomed.2021.104420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Popper KR. R.Die beiden Grundprobleme der Erkenntnistheorie. German : Mohr Siebeck; 1979. [Google Scholar]
- 34.Ximeno-Rodríguez Iñigo, Gil-Edwards Sara, Mera-Cordero Francisco, March-Villalba Jose A, Rodrigo Abad-Rodríguez, et al. 2022. Genotype S/493Q omicron - emerging variant of high biological risk. [DOI] [Google Scholar]
- 35.Khan A, Zia T, Muhammad M, Khan T, Ali SS, Abbasi AA, et al. Higher infectivity of the sars-cov-2 new variants is associated with k417n/t, e484k, and n501y mutants: an insight from structural data. J Cell Physiol. 2021;236(10):7045–7057. doi: 10.1002/jcp.30367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yang ZY, Werner HC, Kong WP, Leung K, Traggiai E, et al. Evasion of antibody neutralization in emerging severe acute respiratory syndrome coronaviruses. Proc Natl Acad Sci U S A. 2005;102(3):797–801. doi: 10.1073/pnas.0409065102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gaunt ER, Hardie A., Claas EC, Simmonds P, Templeton KE. Epidemiology and clinical presentations of the four human coronaviruses 229E, HKU1, NL63, and OC43 detected over 3 years using a novel multiplex real-time PCR method. J Clin Microbiol. 2010;48(8):2940–2947. doi: 10.1128/JCM.00636-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liu DX, JQ Liang., TS Fung. In: Encyclopedia of virology. 4th ed. Bamford D.H., Zuckerman M., editors. Academic Press; Oxford: 2021. Human Coronavirus-229E, -OC43, -NL63, and -HKU1 (coronaviridae) pp. 428–440. [Google Scholar]
- 39.Hulswit R JG, Lang Y, Bakkers M JG, Li W, Li Z, Schouten A, et al. Human coronaviruses OC43 and HKU1 bind to 9-O-acetylated sialic acids via A conserved receptor-binding site in spike protein domain a. Proc Natl Acad Sci U S A. 2019;116(7):2681–2690. doi: 10.1073/pnas.1809667116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kanwar A, Selvaraju S, Esper F. Human Coronavirus-HKU1 infection among adults in Cleveland, Ohio. Open Forum Infect Dis. 2017;4(2):ofx052. doi: 10.1093/ofid/ofx052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Woo P C., Lau S K, Yip C C, Huang Y, Tsoi HW., Chang Kwok-Hung, et al. Comparative analysis of 22 coronavirus HKU1 genomes reveals a novel genotype and evidence of natural recombination in coronavirus HKU1. J Virol. 2006;80(14):7136–7145. doi: 10.1128/JVI.00509-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Beretta A, Cranage M, Zipeto D. Is cross-reactive immunity triggering COVID-19 immunopathogenesis? Front Immunol. 2020;11 doi: 10.3389/fimmu.2020.567710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fierz W, Walz B. Antibody Dependent Enhancement due to Original Antigenic Sin and the development of SARS. Front Immunol. 2020;11:1120. doi: 10.3389/fimmu.2020.01120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bekliz M, Adea K, Puhach O, Perez-Rodriguez F, Marques Melancia S, Baggio S, et al. Analytical sensitivity of eight different SARS-CoV-2 Antigen-Detecting rapid tests for Omicron-BA.1 variant. Microbiol Spectr. 2022;10(4) doi: 10.1128/spectrum.00853-22. [DOI] [PMC free article] [PubMed] [Google Scholar]