Abstract
Introduction
Sepsis and septic shock represent severe pathological states, characterized by the systemic response to infection, which can lead to organ dysfunction and high mortality. Early diagnosis and rapid intervention are crucial for improving survival chances. However, the diagnosis of sepsis is complex due to its nonspecific symptoms and the variability of patient responses to infections.
Methods
The objective of this research was to analyze the implications of using artificial intelligence (AI) in the diagnosis of sepsis and septic shock. The research method applied in the analysis of the implications of using artificial intelligence (AI) in the diagnosis of sepsis and septic shock is the literature review.
Results
Among the benefits of using AI in the diagnosis of sepsis, it is noted that artificial intelligence can rapidly analyze large volumes of clinical data to identify early signs of sepsis, sometimes even before symptoms become evident to medical staff. AI models can use predictive algorithms to assess the risk of sepsis in patients, allowing for early interventions that can save lives. AI can contribute to the development of personalized treatment plans, adapting to the specific needs of each patient based on their medical history and response to treatment. The use of patient data to train AI models raises concerns regarding data privacy and security.
Conclusions
Artificial intelligence has the potential to revolutionize the diagnosis and treatment of sepsis, offering powerful tools for early identification and management of this critical condition. However, to realize this potential, close collaboration between researchers, clinicians, and technology developers is necessary, as well as addressing ethical and implementation challenges.
Keywords: Machine learning, clinical decision support systems, biomarkers, outcome prediction, predictive modeling
Introduction
Sepsis and septic shock represent severe pathological conditions characterized by the systemic response to infection, which can lead to organ dysfunction and high mortality. Early diagnosis and rapid intervention are crucial for improving survival chances. However, sepsis diagnosis is complex due to its nonspecific symptoms and variability in patient responses to infections.1
Artificial intelligence (AI) and machine learning (ML) provide innovative approaches for the prompt detection of sepsis and septic shock. By examining vast amounts of clinical data, ML algorithms can detect signs and predictors of sepsis more precisely than older methods. Notably, deep learning techniques have been applied to review information from electronic health records (EHR), effectively pinpointing individuals who are at significant risk for sepsis well before symptoms become apparent.2
Implementing AI in sepsis diagnosis can lead to faster and more precise detection, allowing for early therapeutic interventions that can save lives. Additionally, AI-based systems can assist in personalizing treatment, adapting it to the specific needs of each patient, which can improve clinical outcomes and reduce costs associated with sepsis treatment.
The incorporation of artificial intelligence (AI) into diagnosing and managing sepsis and septic shock represents a considerable advancement, yielding optimistic outcomes for early detection, forecasting, and therapeutic approaches. This literature review delves into the latest advancements and consequences of employing AI in this domain, emphasizing early identification, predictive precision, and the use of algorithms for decision support in medical environments.
The development of AI algorithms for early diagnosis of sepsis in intensive care units is a critical area of research. Yuan et al. (2020) developed an AI algorithm for early sepsis diagnosis in intensive care, highlighting AI's potential to improve patient outcomes through timely intervention.3 Similarly, Wu et al. (2021) discussed the benefits of AI in sepsis diagnosis, including early prediction and mortality prediction, emphasizing AI's role in enhancing clinical decision-making in sepsis management.4
The role of AI extends beyond diagnosis, including clinical decision support. For example, Goh et al. (2021) presented an AI algorithm that combines structured data and unstructured clinical notes, demonstrating high predictive accuracy for sepsis up to 12 hours before onset, which could significantly improve early detection and reduce false positives.5 Furthermore, Shashikumar et al. (2021) introduced COMPOSER, a deep learning model for early sepsis prediction that flags indeterminate cases instead of making false predictions, providing an actionable early warning system for high-risk patients.6
The accuracy of AI algorithms in diagnosing early-stage sepsis has been demonstrated through various techniques. For example, Par et al. (2022) showed that algorithms like Multilayer Perceptron and Random Forest can diagnose early-stage sepsis with high precision, especially when connected algorithms are used.7 Similarly, Dhungana et al. (2019) developed a calculable phenotype for diagnosing sepsis and septic shock in intensive care units using a supervised machine learning method, achieving high sensitivity and specificity.8
Methods
The objective of this research is to analyze the implications of using artificial intelligence in the diagnosis of sepsis/septic shock. Within the analysis of the implications of using artificial intelligence (AI) in the diagnosis of sepsis and septic shock, the research method applied is literature review. This method involves collecting, evaluating, and synthesizing existing research and publications regarding the use of artificial intelligence in the diagnosis of sepsis/septic shock to provide a comprehensive and up-to-date understanding of the topic.
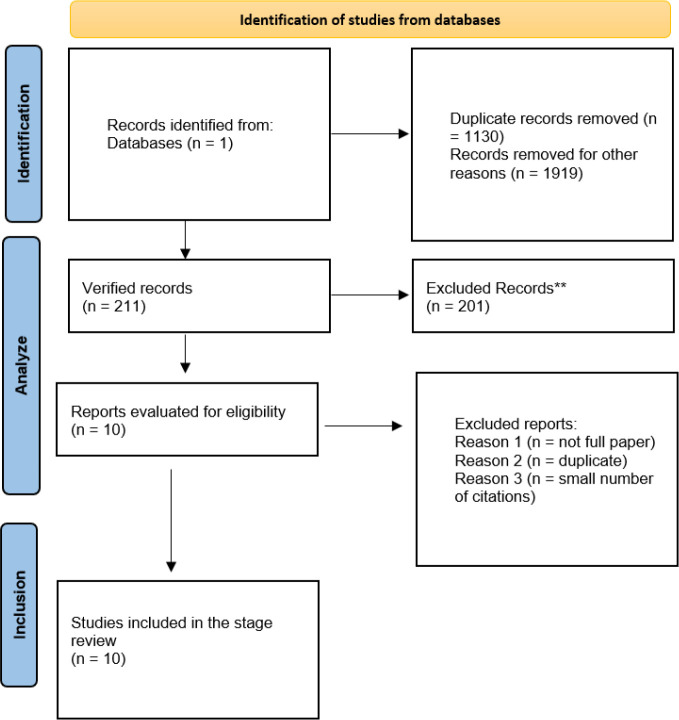
To achieve this, the Google Scholar database was consulted to search for studies on the use of artificial intelligence in diagnosing sepsis and septic shock, resulting in a total of 1130 identified works. To narrow down the dataset, it was decided to examine articles published between 2018 and 2023, resulting in 819 results. Subsequently, the focus was placed on analyzing 10 articles, selected based on specific criteria: they must be complete articles, free from duplications, and have a significant number of citations (Figure 1).
Figure 1.
PRISMA flow diagram of articles related to artificial intelligence in diagnosing sepsis and septic shock
Results
We present the results of 10 articles, each following a detailed analysis process, which includes the category, key aspects, studies, challenges, proposed solutions, and performance indicators. Following the evaluation process, we have compiled the obtained results in Table 1.
Table 1. Study characteristics of articles related to artificial intelligence in diagnosing sepsis and septic shock reported in the literature.
| Category | Key aspects | Studies | Challenges | Proposed solutions | Performance indicators |
|---|---|---|---|---|---|
| Trust in medical AI | Factors influencing trust in medical AI | Zhang and Zhang (2023) | Data quality, algorithmic bias, opacity, safety and security, attribution of responsibility | Ethical, legal and regulatory approaches to improving trust in AI | The degree of trust of professionals and patients in medical AI |
| Advances in diagnostics | Improving sensitivity and specificity in diagnosis | Nagendra et al. (2023) | - | Using AI to overcome the limits of traditional methodology | Comparison of diagnostic performance between AI and traditional methods |
| Implementing AI in health | The potential and challenges of AI implementation | Date et al. (2023) | Data quality, interpretability, data protection | Addressing the challenges through appropriate regulation and the development of advanced technologies | AI adoption rate and user satisfaction |
| AI in specific diagnostics | Using AI for complex medical conditions | Ying et al. (2021) | Accuracy in complex clinical conditions | Improving algorithms for clinical specificities | Diagnostic accuracy and reduction in mortality rates |
| Prediction of complications | Anticipating complications and improving patient management | Ou et al. (2022) | Identification of effective predictive markers | Using advanced machine learning models | Diagnostic accuracy and reduction in mortality rates |
| Clinical data analysis through AI | AI's ability to identify early signs of sepsis | Rajendran et al. (2018) | The need for fast and accurate analysis of voluminous clinical data | Implementation of AI algorithms for efficient data processing and analysis | Accuracy in identifying early signs of sepsis; treatment response time |
| Integrating AI into clinical practices | Intensive monitoring of patients with sepsis by AI | Mollura et al. (2021) | The need for real-time data analysis and early intervention | Development of AI systems for rapid and accurate analysis of physiological data | Time to identification of sepsis; survival rate |
| Integration of ultrasound and biomarkers | Improving diagnosis through AI in ultrasound and biomarker analysis | Tullo et al. (2023) | Accuracy of diagnosis and optimization of therapy | Using AI to improve ultrasound characterizations and biomarker data integration | Accuracy of diagnosis; the success rate of the optimized therapy |
| Prognosis and treatment optimization | Prognostic capabilities of AI and optimization of sepsis treatment | Ruiz-Sanmartin et al. (2022) | Prediction of patients' evolution and personalization of treatments | Using omics and AI technologies to predict patient outcomes and tailor treatments | Mortality rate; organ dysfunction rate |
| Use of biomarker data by AI | Improving AI mortality risk diagnosis and stratification | Spoto et al. (2019) | Complex integration and interpretation of biomarker data | Using AI for advanced biomarker data analysis and clinical decision improvement | Diagnostic accuracy; the effectiveness of mortality risk stratification |
Discussion
A crucial aspect of adopting AI in medicine is trust in the technology. Zhang and Zhang (2023) discuss the ethical aspects and governance of trustworthy medical AI, identifying five factors influencing trust in medical AI: data quality, algorithmic bias, opacity, safety and security, and accountability assignment. The authors propose solutions from ethical, legal, and regulatory perspectives to address these issues and make medical AI more trustworthy.9 The study showed that AI models can perpetuate or amplify existing biases in training data, leading to unfair or inaccurate recommendations for certain patient groups. Although not directly related to sepsis, the study by Nagendra et al. (2023) on advancements in diagnosing thyroid cancer with AI demonstrates significant improvements in sensitivity and specificity compared to traditional diagnostic methods, highlighting AI's potential to revolutionize diagnosis in various areas of medicine.10 Date et al. (2023) explore the potential of machine learning and AI to improve diagnosis and treatment in health, highlighting challenges such as data quality, interpretability, execution, generalizability, data protection, and legal compliance. These challenges must be addressed for the efficient implementation and acceptance of AI technologies in the health sector.11
The research conducted by Ying et al. (2021) investigates the application of an artificial neural network algorithm, enhanced with pulse-coupled neural network (PCNN) techniques, for diagnosing severe sepsis complicated by acute kidney injury (AKI), utilizing data from ultrasonographic images.12 The algorithm showed promising results in enhancing the information from ultrasonographic images, and the change in renal resistive index (RRI) measured through ultrasonographic images is associated with AKI.12 The study concluded that there is a risk that doctors may rely too much on AI algorithm recommendations, neglecting detailed clinical evaluation and professional judgment. However, using patient data to train AI models raises concerns about privacy and data security.
Ou et al. (2022) uses a machine learning-based approach to predict future risks of rehospitalization with acute kidney injury (AKI) in sepsis survivors. Machine learning models, especially LGBM and GBDT models, have shown promise in predicting AKI rehospitalization, with the most important five features being C-reactive protein, white blood cell count, the use of inotropes, blood urea nitrogen, and the use of diuretics.13
Studies have demonstrated AI's ability to rapidly analyze large volumes of clinical data, identifying early signs of sepsis with greater accuracy and speed than traditional methods. Rajendran et al. (2018) highlighted the utility of the shock index as a marker for mortality in pediatric sepsis, underlining the potential of data analysis through AI.14
Integrating AI into clinical practices for sepsis management offers a multidimensional approach to patient care. Mollura et al. (2021) proposed an AI-based intensive care unit monitoring system that uses physiological waveforms to identify sepsis within the first hour of ICU admission, highlighting AI's potential to assist clinicians in early decision-making processes.15 This approach highlights the importance of real-time data analysis in critical care settings, where early intervention can significantly affect outcomes. AI's role extends to improving diagnostic tools, such as ultrasound and biomarker analysis. Tullo et al. (2023) discussed the benefits of ultrasound in diagnosing and treating sepsis and septic shock, suggesting that AI could further enhance the utility of ultrasound through more accurate characterizations and therapy optimizations.16
Similarly, Choo et al. (2020) explored the utility of ischemia-modified albumin as a biomarker in the diagnosis of sepsis, indicating that AI could improve predictive power by integrating biomarker data with clinical observations.17 The prognostic capabilities of AI are also noteworthy. Ruiz-Sanmartin et al. (2022) characterized a proteomic profile associated with organ dysfunction and mortality in sepsis patients using omics techniques, providing a basis for AI algorithms to predict patient outcomes and accordingly tailor treatments.18
Similarly, Spoto et al. (2019) demonstrated the combined use of procalcitonin and MR-proadrenomedullin for diagnosing sepsis and stratifying mortality risk, showing how AI can use biomarker data for improved clinical decision-making.19 AI represents a promising frontier in the fight against sepsis, offering new perspectives and innovative solutions for a persistent medical challenge. However, realizing its full potential will require a balanced approach that weighs innovation against caution, ensuring that the benefits of technology are accessible and positively impact patient care in an ethical and sustainable manner. Although the benefits of artificial intelligence in managing sepsis are evident, challenges remain in its implementation. These include concerns about data privacy, the need for standardized datasets for training algorithms, and ensuring that AI systems are interpretable and explainable to healthcare providers. Overcoming these challenges requires ongoing research, interdisciplinary collaboration, and policy development to ensure that AI tools are ethical, efficient, and seamlessly integrated into healthcare systems.
Conclusions
Integrating AI with diagnostic tools such as ultrasound and biomarker analysis can further refine diagnosis and treatment plans. This has demonstrated how AI can enhance the utility of these tools, offering more precise and personalized therapeutic options.
AI's ability to predict outcomes and optimize treatment strategies underscores its value in prognosis and the personalization of care, which can lead to improved survival rates and reduced healthcare costs. In our examination of ten articles, it was discovered that AI possesses the potential to significantly alter the diagnosis and treatment of sepsis. It provides methods for swiftly and precisely detecting patients at risk, alongside customizing treatment strategies.
The studies highlighted, from the use of the shock index as a prognostic marker to the prediction of rehospitalization with AKI in sepsis survivors, illustrate the diversity of AI applications and its contribution to improving patient outcomes. AI enhances the clinical decision-making process by analyzing intricate clinical data and producing insightful information. This enables faster and better-informed actions that can lower mortality rates and elevate the standard of care.
Regarding implementation challenges, the risk of excessive reliance on algorithmic recommendations and the presence of bias in AI models are major concerns that require ongoing attention and concerted efforts to minimize their impact on clinical decisions.
Protecting patient data and ensuring an ethical implementation of AI represent fundamental challenges that require robust legal and regulatory frameworks, as well as advanced technological solutions for data security. Despite promising developments, the implementation of AI in sepsis care faces challenges, including data privacy, the need for standardized and interpretable algorithms, and integration into existing clinical workflows. Addressing these issues requires concerted efforts from researchers, clinicians, and policymakers to ensure that AI tools are ethical, efficient, and seamlessly integrated into healthcare systems. AI holds the promise of transforming sepsis care through improved early detection, diagnostic accuracy, support for clinical decisions, and personalized treatment strategies.
However, realizing its full potential requires overcoming existing challenges and ensuring that AI tools are designed and implemented in ways that complement and enhance clinical reasoning and patient care. As the field advances, ongoing research, interdisciplinary collaboration, and clinical validation are essential to harness the power of artificial intelligence in the fight against sepsis and septic shock, ultimately leading to better patient outcomes and more efficient healthcare delivery.
Regarding future directions, the efficient and responsible integration of AI in medicine will depend on close collaboration between engineers, doctors, researchers, and policymakers to develop solutions that are technologically advanced, clinically relevant, and ethically sound. Developing AI competencies for healthcare professionals and improving patients' digital literacy are essential for successfully navigating the new era of digital medicine. Investments in fundamental and applied research are crucial for overcoming the current limitations of AI and exploring new horizons in the diagnosis and treatment of sepsis.
Footnotes
Author contributions statement: GPG and DC designed and supervised the study, ISC and VTG drafted the manuscript. LP, AMP, DT and RMS collected and analyzed the data and performed the background literature review for the manuscript. SD and CS carried out the laboratory work, conducted the statistical analyses. All authors read and approved the final version of the manuscript.
Conflicts of interest: All authors – none to declare.
Funding: None to declare.
References
- 1.Caraballo C, Jaimes F. Organ dysfunction in sepsis: an ominous trajectory from infection to death. Yale J Biol Med. 2019;92:629–40. [PMC free article] [PubMed] [Google Scholar]
- 2.Misra D, Avula V, Wolk DM, et al. Early detection of septic shock onset using interpretable machine learners. J Clin Med. 2021;10:301. doi: 10.3390/jcm10020301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yuan KC, Tsai LW, Lee KH, et al. The development of an artificial intelligence algorithm for early sepsis diagnosis in the intensive care unit. Int J Med Inform. 2020;141:104176. doi: 10.1016/j.ijmedinf.2020.104176. [DOI] [PubMed] [Google Scholar]
- 4.Wu M, Du X, Gu R, Wei J. Artificial intelligence for clinical decision support in sepsis. Front Med (Lausanne) 2021;8:665464. doi: 10.3389/fmed.2021.665464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goh KH, Wang L, Yeow AKK, et al. Artificial intelligence in sepsis early prediction and diagnosis using unstructured data in healthcare. Nat Commun. 2021;12:711. doi: 10.1038/s41467-021-20910-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shashikumar SP, Wardi G, Malhotra A, Nemati S. Artificial intelligence sepsis prediction algorithm learns to say "I don't know". NPJ Digit Med. 2021;4:134. doi: 10.1038/s41746-021-00504-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Par OE, Sezer EA, Sever H. Application of artificial intelligence in early-stage diagnosis of sepsis. Proceedings of the 2022 5th Artificial Intelligence and Cloud Computing Conference (AICCC '22) 2022:196–206. doi: 10.1145/3582099.3582129. [DOI] [Google Scholar]
- 8.Dhungana P, Serafim LP, Ruiz AL, et al. Machine learning in data abstraction: a computable phenotype for sepsis and septic shock diagnosis in the intensive care unit. World J Crit Care Med. 2019;8:120–6. doi: 10.5492/wjccm.v8.i7.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang J, Zhang ZM. Ethics and governance of trustworthy medical artificial intelligence. BMC Med Inform Decis Mak. 2023;23:7. doi: 10.1186/s12911-023-02103-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nagendra L, Pappachan JM, Fernandez CJ. Artificial intelligence in the diagnosis of thyroid cancer: recent advances and future directions. Artif Intell Cancer. 2023;4:1–10. doi: 10.35713/aic.v4.i1.1. [DOI] [Google Scholar]
- 11.Date P, Pimprale V, Mandke S. Explorative study on potential of machine learning and artificial intelligence for improved healthcare diagnosis and treatment. J Autonomous Intell. 2024;7:1–11. doi: 10.32629/jai.v7i3.1084. [DOI] [Google Scholar]
- 12.Ying F, Chen S, Pan G, He Z. Artificial intelligence pulse coupled neural network algorithm in the diagnosis and treatment of severe sepsis complicated with acute kidney injury under ultrasound image. J Healthc Eng. 2021;2021:6761364. doi: 10.1155/2021/6761364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ou SM, Lee KH, Tsai MT, Tseng WC, Chu YC, Tarng DC. Artificial intelligence for risk prediction of rehospitalization with acute kidney injury in sepsis survivors. J Pers Med. 2022;12:43. doi: 10.3390/jpm12010043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rajendran A, Sivalingam B, Srinivasan R. Prognostic Value of Shock Index in Children with Sepsis/Septic Shock. J Evolution Med Dent Sci. 2018;7:2737–41. doi: 10.14260/jemds/2018/618. [DOI] [Google Scholar]
- 15.Mollura M, Lehman LW, Mark RG, Barbieri R. A novel artificial intelligence based intensive care unit monitoring system: using physiological waveforms to identify sepsis. Philos Trans A Math Phys Eng Sci. 2021;379:20200252. doi: 10.1098/rsta.2020.0252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tullo G, Candelli M, Gasparrini I, Micci S, Franceschi F. Ultrasound in sepsis and septic shock-from diagnosis to treatment. J Clin Med. 2023;12:1185. doi: 10.3390/jcm12031185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Choo SH, Lim YS, Cho JS, Jang JH, Choi JY, Choi WS, Yang HJ. Usefulness of ischemia-modified albumin in the diagnosis of sepsis/septic shock in the emergency department. Clin Exp Emerg Med. 2020;7:161–9. doi: 10.15441/ceem.19.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ruiz-Sanmartín A, Ribas V, Suñol D, et al. Characterization of a proteomic profile associated with organ dysfunction and mortality of sepsis and septic shock. PLoS One. 2022;17:e0278708. doi: 10.1371/journal.pone.0278708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Spoto S, Fogolari M, De Florio L, et al. Procalcitonin and MR-proAdrenomedullin combination in the etiological diagnosis and prognosis of sepsis and septic shock. Microb Pathog. 2019;137:103763. doi: 10.1016/j.micpath.2019.103763. [DOI] [PubMed] [Google Scholar]