Abstract
Background:
The use of acupuncture is related to patients’ expectations, and the therapeutic interaction effect remains a topic of debate in the literature. Accordingly, it is still unclear whether acupuncture can generate positive clinical effects in patients with fibromyalgia (FM).
Objective:
To determine the effectiveness of acupuncture versus placebo for clinical outcomes and determine the overall effect not attributed to specific effects in patients with FM.
Design:
Umbrella review of systematic reviews (SRs) and meta-analyses.
Data sources and methods:
An electronic search was performed in MEDLINE (via PubMed), Web of Science, CENTRAL, EMBASE, LILACS, CINAHL, PEDro, and SPORTDiscus databases from inception until December 2023. We selected studies with a clinical diagnosis of FM and that analyzed the effectiveness of acupuncture compared with a placebo. Pain intensity, functional status, fatigue, sleep quality, and depression symptoms were assessed. Effect sizes were calculated as the mean difference (MD) or standard mean difference (SMD). The quality of intervention reporting was assessed using the Grading of Recommendations Assessment, Development, and Evaluation approach.
Results:
Eleven SRs with 8399 participants were included. Compared with placebo, acupuncture was associated with reductions in pain intensity (MD = −1.13 cm, 95% CI −2.09 to −0.17, p < 0.001), physical function (SMD = −0.63, 95% CI −1.67 to 0.41, p = 0.06), sleep quality (SMD = −0.25, 95% CI −1.39 to 0.88, p = 0.06), and fatigue (SMD = 0.20, 95% CI = 0.17 to 0.22, p < 0.001). The proportion not attributable to specific effects (PCE) of acupuncture was 58% for pain intensity (PCE = 0.58, 95% CI 0.45 to 0.71), 57% for physical function (PCE = 0.57, 95% CI −0.07 to 1.20), and 69% for fatigue (PCE = 0.69, 95% CI 0.18 to 1.21).
Conclusion:
Acupuncture showed a statistically significant difference in decreased pain intensity and fatigue in women with FM. However, the certainty of evidence was low to very low; its effects are not clinically important, and more than 50% of the overall treatment effects were not attributed to the specific effects of acupuncture.
PROSPERO registration number:
CRD42023487315.
Keywords: acupuncture, Fibromyalgia, pain, systematic review, umbrella review
Plain language summary
Acupuncture versus placebo in Fibromyalgia
Acupuncture is often used by people with Fibromyalgia, a condition that causes widespread pain and fatigue, but it’s still unclear if it truly helps. This study looked at previous research to compare the effects of acupuncture and fake (placebo) treatments on symptoms like pain, physical function, fatigue, sleep quality, and depression in people with Fibromyalgia. The review included 11 studies with 8,399 participants. It found that acupuncture was slightly better than placebo at reducing pain and fatigue but did not significantly improve physical function or sleep quality. However, most of the benefits could not be specifically attributed to the acupuncture treatment itself but were likely due to other factors, such as patients’ expectations. In summary, while acupuncture showed some small benefits for pain and fatigue in Fibromyalgia, the overall evidence was weak, and more than half of the improvement was not directly related to the acupuncture treatment.
Introduction
Fibromyalgia (FM) is a diffuse pain syndrome with widespread pain, fatigue, sleep disorders, and cognitive dysfunction as the main symptoms caused by the dysfunction of central nervous system sensory afferent processing. 1 FM is the third most common cause of chronic musculoskeletal pain, with a prevalence of 2%–3% worldwide, having a greater predominance in women.2,3 FM symptoms are difficult to treat effectively, and only a minority of individuals experience a clinically relevant benefit from any single intervention. 3 This is because FM is a clinical condition in which the pathophysiological mechanisms are completely unknown and therefore, treatment is based on the control of symptoms. 1 Second, FM is considered a condition of exacerbations or decompensations of symptoms, which then return to the initial state of spontaneous resolution. This regressive phenomenon impacts the real effect of the interventions, due to the different periods of severity of the condition. Due to this, treatments do not respond immediately or generate important changes in clinical outcomes in this type of patient.2,4
Recent clinical guidelines recommend a stepwise graduated approach depending on the key symptoms and the extent of disability, starting with education, defining realistic goals for treatment (improvement of daily functioning), and non-pharmacology such as exercise (i.e., strength, aerobic, aquatic, and flexibility exercise), patient education, physiotherapy, and multimodal rehabilitation programs. 4 Therefore, it is necessary to find effective complementary and alternative medicine therapies.4,5
Research has demonstrated that FM is among the most prominent conditions treated with acupuncture.4–6 Acupuncture, a traditional oriental therapy, is increasingly being adopted globally, and its clinical effectiveness has been evaluated for various musculoskeletal conditions.5–8 Although the effects of acupuncture have been studied, the evidence for clinical effectiveness in FM is controversial.9,10 Several systematic reviews (SRs) have reported inconsistent results regarding the effectiveness of acupuncture versus placebo or sham for pain relief in FM.9–12 Recent reviews with meta-analysis have demonstrated that acupuncture can alleviate pain intensity, anxiety, depression, fatigue, and sleep disturbances in FM patients.13–15 A network meta-analysis showed that acupuncture decreases pain intensity in patients with FM. 14 However, no significant differences have been observed between acupuncture and sham treatments concerning general stiffness in these patients. 14 Finally, another SR concluded that acupuncture does not significantly improve fatigue, sleep quality, physical function, and stiffness in patients with FM. 15
Regarding the placebo effect, the evidence is strong in relation to the effects on pain control in different clinical conditions.16,17 The main explanation could be a traditional psychological theory, which includes the expectations of the patients, the relationship between the patient and therapist, and beliefs. 17 In this sense, the use of acupuncture is related to patients’ expectations, and therapeutic interactions are the most important to make it. Despite this, the placebo effect in acupuncture remains a topic of debate in the literature.17,18 In addition, one study showed that biopsychosocial factors such as level of education, familiarity, and setting of the rehabilitation treatment, including the type of environment and location can influence the placebo effect perceived by an intervention. 19
Accordingly, it is still unclear whether acupuncture can generate positive clinical effects in patients with FM. This inconsistency creates confusion in clinical practice for the physiotherapist. Furthermore, the variety of symptoms that FM patients may report could limit the success of the treatment and explain the different results of previous studies. This umbrella review of SRs and meta-analyses aimed to rate the quality of reporting of acupuncture interventions in the included studies using a specific tool. In addition, the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) method was used to rate the quality and strength of the evidence. Therefore, this umbrella review of SR aimed to determine the effectiveness of acupuncture versus placebo for clinical outcomes and determine the overall effect not attributed to specific effects in patients with FM.
Materials and methods
This umbrella review of SRs was reported according to the guidelines of the Preferred Reporting Item for Systematic Review and Meta-Analyses statement and followed the recommendations of the Cochrane Collaboration Handbook and Preferred Reporting Items for Overviews of Systematic Reviews, including harms pilot checklist (PRIO-harms) to promote a more balanced reporting of benefits and harms.20–22 This umbrella of SRs was registered in the International Prospective Register of Systematic Reviews (PROSPERO) with the number CRD42023487315.
Identification and selection of studies
Trials were included if they met the predetermined eligibility criteria summarized according to the Population, Intervention, Comparator, Outcome, and Study (PICOS) model.
Inclusion criteria
Design
Umbrella review of SRs and meta-analyses.
Participants
Females >18 years of age with a clinical diagnosis of FM based on American College of Rheumatology criteria, 23 regardless of residential status (e.g., community-dwelling, foundation, or institutionalized).
Intervention
Manual needle, acupuncture, and electroacupuncture with or without other co-interventions. For this umbrella review, acupuncture was considered manually or associated with Transcutaneous Electrical Nerve Stimulation, applied at different points following the principles of traditional Chinese medicine.
Comparator
Placebo or sham acupuncture. For this umbrella review, a placebo is the insertion of a short needle over a patch at the acupoint on the skin without reaching the muscle. Sham consisted of a guided simulation of acupuncture with tubes, without inserting the needle, and about 1 or 2 cm away from the acupoints.
Outcome measures
Pain intensity, functional status, sleep quality, fatigue, and depression symptoms.
Study design
SRs of randomized clinical trials published in English or Spanish. While trials must have compared interventions of acupuncture, placebo, or sham, data were also included where the same additional interventions were completed concurrently in both groups.
Electronic searches
We systematically searched MEDLINE (via PubMed), Web of Science, the Cochrane Central Register of Controlled Trials (CENTRAL), EMBASE, the Latin American and the Caribbean Literature in Health Sciences (LILACS), the Cumulative Index to Nursing and Allied Health Literature (CINAHL), Physiotherapy Evidence Database (PEDro), and SPORTDiscus databases from inception until December 2023. All databases were searched using a customized algorithm (see Supplemental Table S1). To increase search sensitivity, citation tracking for prior and derivative papers was performed using Connected Papers. Finally, retractions or errata from the included studies were searched for using PubMed. No limits were placed on the geographical location or date of publication. Manual searches were also performed to identify references to clinical trials that were potentially relevant.
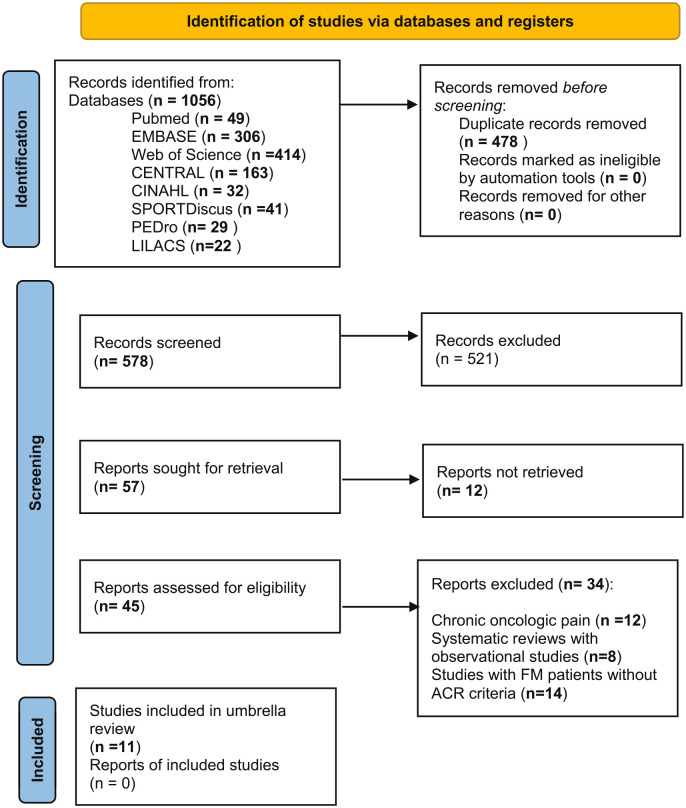
Each paper retrieved by the searches was evaluated by two reviewers. The search strategy used included SRs in English and Spanish and a combination of the following Medical Subject Headings (MeSH) terms: “Fibromyalgia,” “Fatigue Syndrome, Chronic,” “Acupuncture,” “Acupuncture therapy,” “Acupuncture analgesia,” and “Systematic Review.” With the free-text terms, we used the following terms: “Fibromyositis Syndrome” and “electroacupuncture.” For the searches in the MEDLINE and CENTRAL databases, the Cochrane Highly Sensitive Search Strategies for identifying eligibility studies were used with the PICOS strategy. 24 We also manually searched the references of the selected articles to identify additional potentially relevant studies. The flow diagram search is shown in Figure 1.
Figure 1.
PRISMA flow chart diagram.
PRISMA, Preferred Reporting Item for Systematic Review and Meta-Analyses.
Outcome measures
Trials had to report an objective measure of pain intensity, which was the primary endpoint. The minimal clinical important difference (MCID) for pain intensity in patients with FM was considered to be 2.0 points. 25 The secondary endpoint was functional status. The MCID for functional status measured with Fibromyalgia Impact Questionnaire (FIQ) in patients with FM was considered to be 14 points. 26 For the level of depression measured with the Beck Depression Inventory (BDI), the MCID was considered to be 17 points. 27 For sleep quality and fatigue, the MCID has not been established.
Data management and selection process
One reviewer extracted data, and a second reviewer independently cross-checked the accuracy of data extraction for all papers. Subsequently, one reviewer entered study data into the Cochrane Collaboration’s Review Manager 5.4 software. The following data were extracted for syntheses and meta-analyses from the original reports: (1) study design, (2) number of studies included, (3) total number of patients, (4) intervention, (5) comparator, (6) outcome measures, (7) meta-analysis results, and (8) evaluation of the methodological quality of the studies.
Assessment of methodological quality
The assessment of the methodological quality of SRs was performed as recommended by the Cochrane Collaboration Handbook, 22 using the AMSTAR 2 tool. 28 This tool assesses quality according to 16 questions about the quality, results, and meta-analyses. The rating overall for the review is high, moderate, low, and critically low. The agreement rate between reviewers (FA-Q and HG-E) was calculated using kappa statistics. Updated meta-analyses with risk of bias (ROB) for clinical trials by Cochrane ROB 2.0 were performed.
Data analysis
The analyses were conducted using STATA software (version 17.0; StataCorp, College Station, TX, USA), using the random-effects inverse-variance model with the Hartung–Knapp–Sidik–Jonkman variance estimator based on DerSimonian–Laird estimate of tau. Pooled Mean differences (MDs) were estimated for pain intensity, sleep quality, and depression symptoms. Pooled Standard Mean Differences (SMDs) were estimated for fatigue. The calculation of proportion not attributable to specific effects, traditionally named as PCE of acupuncture involved dividing the mean change score of the placebo arm by the mean change score of the intervention arm, following methods outlined in earlier studies. 29 Subsequently, the resulting PCE was subjected to log transformation to normalize the distribution for analysis purposes and then transformed back for reporting. PCEs, along with their 95% CI, were pooled for each outcome. A minimum of three studies was required to perform the meta-analysis for each outcome. Statistical heterogeneity was assessed by both visual inspection of forest plots and formal statistical tests. For visual inspection, heterogeneity was ascertained by the overlap of CIs for each study, with little or no overlap indicating substantial heterogeneity. The heterogeneity of results across studies was evaluated using the I2 statistic, which is considered as may not be important (0%–40%) and may represent moderate (30%–60%), substantial (50%–90%), or considerable (75%–100%) variability due to between-study heterogeneity. 30
Given the limited number of studies (fewer than 10) for each outcome, we utilized Doi plots to examine small study effects since these are useful to identify whether smaller studies tend to report different effect sizes compared to larger studies. Quantification of asymmetry in the Doi plot was performed using the Luis Furuya-Kanamori (LFK) index. Doi plots were categorized as having no asymmetry (LFK index <1), minor asymmetry (LFK index = 1–2), and major asymmetry (LFK index >2), respectively. 31
The GRADE approach was used to assess the overall certainty of evidence. 32 The GRADE included the assessment of study limitations, consistency of effect, indirectness, imprecision, and publication bias. The quality of the evidence was classified into four categories: high, moderate, low, and very low. 32 We used the GRADE profiler (GRADEpro) to create a “summary of findings.”
Results
Flow of studies through the review and characteristics of the included studies
A total of 11 SRs were found through the electronic searches.9–15,33–36 A total of 125 studies were included in these 11 SRs; the number of studies that overlapped among the meta-analyses is given in supplementary material (Supplemental Table S2). The overall population included in all SRs was 8399 patients with FM. In comparing acupuncture versus placebo or sham for the quantitative synthesis, pain intensity had 262 and 267 patients, physical function had 78 and 75, sleep quality had 85 and 82, and fatigue had 79 and 73, respectively. The mean age was 49.2 years old (SD = 2.1), and the mean follow-up was 8 weeks (range 4 to >12 weeks). The main characteristics of SRs, interventions, comparators, outcomes measures, and results are summarized in Table 1. The kappa agreement rate between reviewers was 0.89.
Table 1.
Characteristics of included systematic reviews.
| Study | Included study design | Criteria diagnostic of Fibromyalgia | No. included studies | No. total patients | Intervention | Comparison | Outcomes measures | Quantitative synthesis | Assessment quality of studies | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Quality of life | Physical function | Pain intensity | Depression | Stiffness | Quality of sleep | Fatigue | |||||||||
| Almutari et al. (2022) | RCT | ACR criteria 1990 and cual2016 | 23 | 1409 | Acupuncture, physiotherapy, fluoxetine, weight reduction, nutraceutical, soy, lidocaine, IGUBAC-Diet, Cupping | Sham, placebo | Quality of life: FIQ, SF36 Pain intensity: VAS, NRS, CPGS, WPI, SF MPQ. Depression: CES-D, HDRS Stiffness: VAS, FIQ Stiffness |
Acupuncture vs sham: SMD = −0.28 |
NR | Acupuncture vs sham: SMD = −1.69 |
Acupuncture vs sham: SMD = −9.64 |
Acupuncture vs sham: SMD = −8.52 |
NR | NR | Cochrane’s risk of bias tool |
| Cao et al. (2013) | RCT | ACR criteria 1990 | 16 | 1081 | Acupuncture, electroacupuncture, acupuncture plus cupping therapy, and western medication | Sham Acupuncture, Sham electroacupuncture, anti-depression drugs, cupping therapy, medications alone, amitriptyline | Quality of life: FIQ Pain intensity: VAS, NRS, SF MPQ, MPQ, FIQ, PPI, MPI Depression: HAMD Quality of sleep: VAS Fatigue: MFI, FIQ |
NR | NR | Acupuncture vs sham acupuncture SMD = −0.22 Acupuncture vs medication SMD = −0.74 Acupuncture plus cupping therapy and medication vs medication SMD = −1.65 |
Electroacupuncture vs sham SMD = −0.67 |
NR | Acupuncture vs amitriptyline SMD = −0.32 |
Acupuncture vs sham SMD = 0.05 |
Cochrane’s risk of bias tool |
| Deare et al. (2016) | RCT or QRT | ACR criteria 1990 | 9 | 395 | Acupuncture, electroacupuncture, manual acupuncture | Non- intervention, sham acupuncture | Quality of life: FIQ, VAS Pain intensity: VAS, NRS, MPI, SF-MPQ Quality of sleep: Stiffness: FIQ Physical function: SF36 Fatigue: VAS, MFI, FIQ |
Acupuncture vs sham SMD = 0.29 Manual acupuncture vs electroacupuncture SMD = 0.65 |
NR | Acupuncture vs sham SMD = −0.14 Manual acupuncture vs electroacupuncture SMD = −0.63 |
NR | Electroacupuncture vs Sham SMD = −0.45 |
Acupuncture vs sham SMD = 0.16 Electroacupuncture vs Manual acupuncture SMD = 0.40 |
Acupuncture vs sham SMD = −0.1 Electroacupuncture vs Manual acupuncture SMD = −0.85 |
Cochrane’s risk of bias tool |
| Kim et al. (2019) | RCT | ACR criteria 1990 | 10 | 690 | Verum acupuncture | Placebo | Pain intensity: VAS, PPT Quality of sleep: Sleep of NHP Fatigue: FSS, MFI Depression: HAMD, mental SF-12 |
NR | NR | Verum acupuncture vs sham SMD = −0.49 |
NR | NR | Verum acupuncture vs sham SMD = −0.46 |
Verum acupuncture vs sham SMD = −0.10 |
Cochrane’s Risk of Bias tool |
| Langhorst et al. (2010) | RCT | ACR criteria 1990 | 7 | 385 | Acupuncture, electroacupuncture, manual acupuncture | Sham, non-intervention | Pain intensity: VAS, MPQ Quality of sleep: VAS Stiffness: FIQ Physical function: SF36 Fatigue: VAS, MFI |
NR | Acupuncture vs control SMD = −0.15 |
Acupuncture vs control SMD = −0.25 |
NR | NR | Acupuncture vs control SMD = 0.05 |
Acupuncture vs control SMD = 0.04 |
Van Tulder Score Modified Cochrane’s risk of bias tool |
| Martin-Sanchez et al. (2009) | RCT | ACR criteria 1990 | 6 | 323 | Acupuncture, electroacupuncture | Placebo acupuncture | Pain intensity: VAS | NR | NR | Acupuncture vs sham SMD = 0.02 |
NR | NR | NR | NR | NE |
| Mayhew and Ernst (2007) | RCT | ACR criteria 1990 | 5 | 316 | Acupuncture, electroacupuncture | Sham acupuncture, sham needling, Sham Laser, Amitriptyline, non-intervention | Quality of life: FIQ Pain intensity: MPI, VAS Quality of sleep: VAS Stiffness: FIQ Physical function: SF36 Fatigue: VAS |
NR | NR | NR | NR | NR | NR | NR | Jadad Score |
| Valera-Calero et al. (2022) | RCT | ACR criteria 1990 | 21 | 1497 | Acupuncture | Dietary therapy, abdominal or Scalp acupuncture, moxibustion, music, vibratory therapy, electroacupuncture, sham, education, TENS, Physiotherapy | Quality of life: FIQ Pain intensity: VAS; MPQ, PPT, PDQ, WBFPS |
Acupuncture vs control SMD = −0.26 |
NR | Acupuncture vs control SMD = −0.30 |
Acupuncture vs control SMD = −0.68 |
NR | Acupuncture vs control SMD = −0.31 |
NR | PEDro Scale |
| Zhang et al. (2019) | RCT | ACR criteria 1990 | 12 | 788 | Acupuncture, Manual Electroacupuncture | Placebo acupuncture, Sham needling, Amitriptyline | Quality of life: FIQ Pain intensity: VAS, SF MPQ, NRS |
Acupuncture vs Sham MD = −13.39 Manual acupuncture vs sham manual acupuncture MD = −16.72 Electroacupuncture vs sham electroacupuncture MD = −2.7 |
NR | Acupuncture vs Sham MD = −1.04 Manual acupuncture vs sham Manual acupuncture MD = −1.14 Electroacupuncture vs sham electroacupuncture MD = −0.94 |
NR | NR | NR | NR | Cochrane’s risk of bias tool |
| Zhang et al. (2022) | RCT or QRT | ACR criteria 1990 | 13 | 923 | Acupuncture, Manual Electroacupuncture | Sham acupuncture, sham needling, non-intervention, mock laser acupuncture | Quality of life: FIQ Pain intensity: FIQ, SF MPQ, VAS, BPI Stiffness: FIQ Physical function: FIQ, SF36, NHP Quality of sleep: NHP Fatigue: FIQ |
Acupuncture vs control SMD = −0.86 |
Acupuncture vs control SMD = 0.14 |
Acupuncture vs control SMD = −0.42 |
NR | Acupuncture vs control SMD =−0.38 |
Acupuncture vs control SMD = −0.38 |
Acupuncture vs control SMD = −0.03 |
Cochrane’s risk of bias tool |
| Yang Bai et al. (2014) | RCT or CCT | ACR criteria 1990 | 9 | 592 | Acupuncture, Manual Electroacupuncture | Sham acupuncture, Amitriptyline, Fluoxetine, Placebo | Pain intensity: VAS Functional status: FIQ Quality of life: SF-36 Pressure pain threshold: PPT Fatigue: Multidimensional fatigue inventory |
NR | NR | Acupuncture vs sham MD = 4.19 | NR | NR | NR | NR | Cochrane’s Risk of Bias tool |
ACR, American College Rheumatology; BPI, brief pain inventory; CCT, controlled clinical trial; CES-D, Center for Epidemiologic Studies Depression Scale; CPGS, Chronic Pain Grade Scale; FIQ, Fibromyalgia Impact Questionnaire; FSS, Fatigue Severity Scale; HAMD, Hamilton Depression Scale; HDRS, Hamilton Depression Rating Hetero-Evaluation Scale; MFI, multidimensional fatigue inventory; MPI, multidimensional pain inventory; MPQ, McGill Pain Questionnaire; NE, not assessed; NHP, Nottingham health profile; NR, not reported; NRS, Numeric Rating Scale; PDQ, Pain Detect Questionnaire; PPI, present pain intensity; PPT, pressure pain threshold; QRT, quasi-randomized trials; RCT, randomized controlled trial; SF MPQ, Short Form of the McGill Pain Questionnaire; SF36, Short Form-36; SMD, standardized mean difference; TENS, transcutaneous electrical nerve stimulation; VAS, Visual Analog Scale; WBFPS, Wong-Baker Faces Pain Scale; WPI, Widespread Pain Index.
Risk of bias
Regarding the methodological quality of the included SRs, four SRs were rated as having moderate methodological quality,9,14,15,33 three SRs had low quality,11–13 and four had critically low quality (Table 2).10,34–36 Details of the ROB assessment for nine included trials are found in Supplemental Figures S1 and S2. Overall, 66.7% of the trials were judged as having a high overall ROB, 11.1% were deemed as having some concerns, and 22.2% of trials were judged as having a low overall ROB.
Table 2.
Methodological quality of the included systematic reviews by AMSTAR 2.
| Study | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | Rating overall |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cao et al. (2013) | Yes | No | Yes | Yes | Yes | Yes | No | PY | Yes | No | Yes | No | Yes | No | No | Yes | Critically low quality |
| Deare et al. (2013) | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Moderate quality |
| Kim et al. (2019) | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | No | No | Yes | Yes | Yes | Low quality |
| Langhorst et al. (2010) | Yes | No | Yes | Yes | Yes | Yes | No | Yes | PY | No | Yes | No | Yes | Yes | No | Yes | Low quality |
| Martin-Sanchez et al. (2010) | Yes | No | Yes | PY | Yes | Yes | No | PY | No | No | Yes | No | Yes | No | No | Yes | Critically low quality |
| Mayhew et al. (2007) | Yes | No | Yes | PY | Yes | No | No | Yes | PY | No | NMC | No | No | No | NMC | Yes | Critically low quality |
| Zhang et al. (2019) | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Moderate quality |
| Zheng et al. (2022) | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | Yes | Yes | No | No | Yes | Moderate quality |
| Valero-Calero et al. (2022) | Yes | Yes | Yes | PY | Yes | Yes | No | Yes | Yes | No | Yes | Yes | No | Yes | No | Yes | Low quality |
| Almutairi et al. (2022) | Yes | No | Yes | No | Yes | Yes | No | Yes | Yes | No | Yes | No | Yes | Yes | Yes | Yes | Moderate quality |
| Bai et al. (2014) | Yes | PY | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | No | No | Yes | No | Yes | Critically low quality |
High: Zero or one non-critical weakness: The systematic review provides an accurate and comprehensive summary of the results of the available studies that address the question of interest. Moderate: More than one non-critical weakness: The systematic review has more than one weakness, but no critical flaws. It may provide an accurate summary of the results of the available studies that were included in the review. Low: One critical flaw with or without non-critical weaknesses: The review has a critical flaw and may not provide an accurate and comprehensive summary of the available studies that address the question of interest. Critically low: More than one critical flaw with or without non-critical weaknesses: The review has more than one critical flaw and should not be relied on to provide an accurate and comprehensive summary of the available studies.
NMC, no meta-analyses conducted; PY, partial yes.
Participants
Of the 8399 randomized participants, 1676 were lost to follow-up, resulting in follow-up data being available for 6719 participants. The mean participant age ranged from 40.9 to 57.6 years.
Interventions
The intervention period ranged from 4 to 12 weeks, with a mean period of 4.6 weeks. Intervention frequency was 2–4 sessions per week. The session duration ranged from 20 to 60 min. Most studies defined acupuncture as “manual and electroacupuncture with TENS, and the placebo interventions were simulation guide tubes without needles.”
Outcomes
Harms
In this umbrella review, six SRs reported adverse events regarding the effects of acupuncture.9,10,12,13,15,33 However, all SRs reported low adverse events such as local discomfort of needle insertion, tiredness, low soreness, and mild bruising.
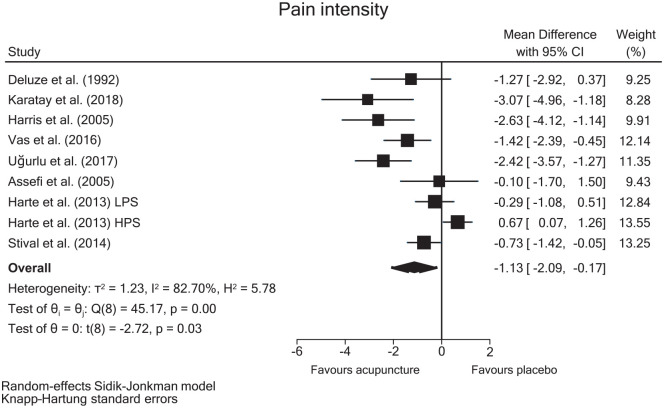
Pain intensity
Data from eight randomized clinical trials were included in the meta-analysis of pain intensity, which was measured with the Visual Analog Scale (VAS). The overall pooled MD estimate showed statistically significant differences for pain intensity favoring acupuncture (MD = −1.13 cm, 95% CI −2.09 to −0.17, p < 0.001) (Figure 2). The effect of acupuncture on pain, as assessed at different time points after the intervention, revealed a greater effect when measurements were taken beyond a 4-week period following the intervention (MD = −1.87 cm, 95% CI 3.24 to −0.50), as opposed to assessments conducted prior to that timeframe (MD = −0.84 cm, 95% CI −1.85 to 0.17) (Supplemental Figure S3). There was a very low quality of evidence according to the GRADE rating (Table 3).
Figure 2.
Forest plot showing estimates of acupuncture versus placebo on pain intensity.
Table 3.
Summary of findings and quality of evidence (GRADE) for acupuncture versus sham/placebo in patients with fibromyalgia.
| Certainty assessment | No. of patients | Effect | Quality of evidence (GRADE) | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of studies | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Publication bias | Acupuncture | Sham/placebo | Relative (95% CI) | MD or SMD (95% CI) | ||
| Pain intensity (overall) at rest (Scale of 0–10) | ||||||||||||
| 9 | RCT | Serious | Serious | Not serious | No concerns | Detected (major) | 262 | 267 | — | MD = −1.13 cm (−2.09 to −0.17) |
⨁◯◯◯ Very low |
CRITICAL |
| Physical function (FIQ) | ||||||||||||
| 3 | RCT | Serious | Serious | Not serious | Serious | Not detected | 78 | 75 | — | SMD = −0.63 (−1.67 to 0.41) |
⨁⨁◯◯ Low |
CRITICAL |
| Fatigue | ||||||||||||
| 3 | RCT | Not serious | Not serious | Not serious | No concerns | Not detected | 79 | 73 | — | SMD = 0.20 (0.17 to 0.22) |
⨁⨁◯◯ Low |
CRITICAL |
| Sleep quality | ||||||||||||
| 3 | RCT | Serious | Serious | Not serious | Serious | Not detected | 85 | 82 | — | SMD = −0.25 (−1.39 to 0.88) |
⨁⨁◯◯ Low |
CRITICAL |
Quality of evidence: High: The research provides a very good indication of the likely effect. The probability that the effect is different is low. Moderate: The research provides a good indication of the likely effect. The probability that the effect is substantially different is Moderate. Low: The research gives some indication of the probable effect. However, the probability that the effect is substantially different is high. Very low: The research does not provide a reliable estimate of the probable effect. The probability that the effect is substantially different is very high. Downgrading: The GRADE approach has four reasons for possible rating down the quality of evidence. 32 Begins with the study designs (trials or observational studies), secondly downgrading the evidence to two levels: (1) for study limitation if the majority of studies (>50%) was rated as high risk of bias; (2) for inconsistency, if heterogeneity was greater than the accepted low level I2 >40% and. point estimates vary widely across studies; Confidence intervals (CIs) show minimal or no overlap; The statistical test for heterogeneity which tests the null hypothesis that all studies in a meta-analysis have the same underlying magnitude of effect shows a low p-value. The I2 which quantifies the proportion of the variation in point estimates due to among-study differences is large); (3) for indirectness, directness was undoubled; (4) for imprecision, if meta-analysis had a small sample size (n < 400) or a confidence interval very wide.
CI, confidence interval; GRADE, Grading of Recommendations Assessment, Development, and Evaluation; MD, mean difference; RCT, randomized clinical trial; SMD, standard mean difference.
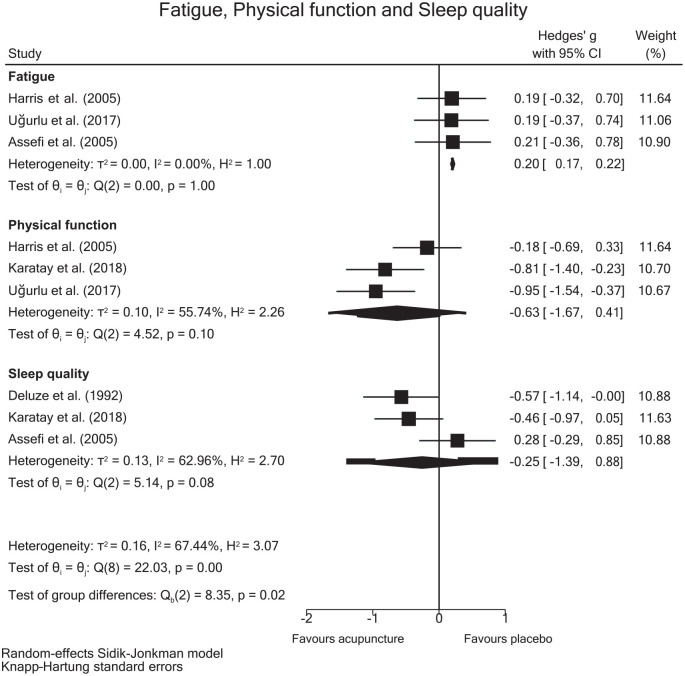
Physical function
Data from three randomized clinical trials were included to perform the meta-analysis for functional status, which was measured with the Fibromyalgia Impact Questionnaire (FIQ) and the 36-Item Short Form Survey (SF-36) physical function domain. The overall pooled SMD estimate showed no statistically significant differences in physical function favoring acupuncture (SMD = −0.63, 95% CI −1.67 to 0.41, p = 0.06) (Figure 3), with moderate heterogeneity (I2 = 55.74%, p = 0.10). There was a low quality of evidence according to the GRADE rating (Table 3).
Figure 3.
Forest plot showing estimates of acupuncture versus placebo on fatigue, physical function, and sleep.
Fatigue
Data from three randomized clinical trials were included in the meta-analysis of the level of fatigue. The overall pooled SMD estimate showed statistically significant differences in the level of fatigue (SMD = 0.20 points, 95% CI 0.17 to 0.22, p < 0.001) (Figure 3), with no important heterogeneity (I2 = 0%, p = 1.00). There was a low quality of evidence according to the GRADE rating (Table 3).
Sleep quality
Data from three randomized clinical trials were included to perform the meta-analysis for sleep quality. The overall pooled SMD estimate showed no statistically significant differences for sleep quality favoring sham/placebo (SMD = −0.25 points, 95% CI −1.39 to 0.88, p = 0.06) (Figure 3), with no important heterogeneity (I2 = 62.96%, p = 0.08). There was a low quality of evidence according to the GRADE rating (Table 3).
PCEs of acupuncture on clinical outcomes
For the examination of PCEs of acupuncture, the clinical outcomes analyzed in at least three studies were limited to pain intensity, physical function, and fatigue (Figure 4). Regarding pain intensity, data from eight randomized placebo-controlled trials revealed that 58% of acupuncture’s overall treatment effects were not attributed to specific effects (PCE = 0.58, 95% CI 0.45 to 0.68). For physical function and fatigue, analysis of three studies indicated that 57% of acupuncture’s overall effect was not due to specific effects (PCE = 0.57, 95% CI −0.07 to 1.20) for physical function, and 69% for fatigue (PCE = 0.69, 95% CI 0.18 to 1.21). Forest plots for each clinical outcome are shown in the supplementary material (Supplemental Figure S4).
Figure 4.
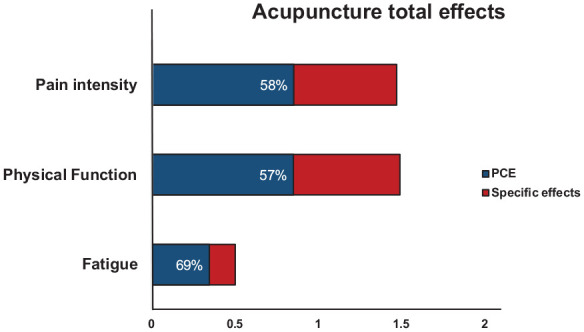
Overall treatment effect and the proportion not attributable to specific effects for pain intensity, physical function, and fatigue of acupuncture interventions in patients with fibromyalgia.
Sensitivity meta-analysis
The results of meta-regression analyses indicate that mean age (β = 0.06, p = 0.552, 95% CI −0.16 to 0.27), the number of acupuncture sessions (β = −0.013, p = 0.860, 95% CI −0.18 to 0.16), and the duration of FM in years (β = −0.226, p = 0.414, 95% CI −0.39 to 0.84) did not exert a statistically significant influence on the effect size estimates for the effectiveness of acupuncture in reducing pain intensity (Supplemental Figures S5–S7). In addition, sensitivity meta-analyses were performed, systematically excluding each study from the overall analysis to evaluate the robustness of the pooled effect of acupuncture on pain intensity. Using the leave-one-out method, the MD estimates remained stable, with overlapping confidence intervals ranging from −0.95 (95% CI −1.75 to −0.15) to −1.39 (95% CI −2.16 to −0.62 points) (Supplemental Figure S8).
Publication bias
Visual examination of the Doi plots revealed major asymmetry in pain intensity (LFK = −3.46), suggesting a potential presence of publication bias or small study effects.31,37 Conversely, no asymmetry was noted for physical function, fatigue, and sleep quality (Supplemental Figure S9); however, the limited number of studies may have constrained the thorough examination of Doi plots for these outcomes.
Discussion
This umbrella review of SRs aimed to determine the effectiveness of acupuncture versus placebo for clinical outcomes in patients with FM. The main findings were (1) acupuncture was effective in reducing both pain intensity and fatigue compared to placebo and (2) for physical function and sleep quality, there were no statistically significant differences between groups. However, none of the between-group differences reached the minimum threshold to be considered clinically important, and more than 50% were attributed to contextual effects.
Regarding non-pharmacology approaches for the treatment of FM is still controversial. 38 However, some studies have demonstrated minimal effect in patients with myofascial pain and FM. A recent scoping review showed the beneficial role of extracorporeal shockwave for improving clinical and functional outcomes in people with myofascial pain syndrome; however, no evidence was found for FM. 39 Other studies showed that electrotherapy could have a minimal effect on pain relief in patients with FM with minor adverse events. 40 However, further studies to long-term are needed to identify the optimal dose of electrotherapy in this clinical condition.
In contrast with our study, previous overviews have only evaluated the effectiveness of acupuncture on pain intensity and sleep in chronic musculoskeletal pain.38,41,42 Our results on pain intensity differ from some of those reported in the overviews published to date. For example, Lauche et al. included seven SRs, of which only two showed strong evidence in favor of acupuncture versus control in pain relief in patients with FM. 42 On the other hand, Bidonde et al. reported with low certainty evidence that there are no differences between acupuncture and sham acupuncture. 38 Nevertheless, the results are based on an SR that included three clinical trials in the meta-analysis (n = 200). 9 Another study showed statistically significant differences in favor of acupuncture versus placebo for pain relief with a moderate level of evidence. 38 Nonetheless, the results rely on eight clinical trials in their meta-analysis, showing substantial heterogeneity (I2 = 59%). Regarding sleep quality, while we demonstrated that there are no differences between acupuncture and placebo, Lu et al. reported statistically significant differences with a moderate effect size for sleep quality. 41 The differences can be explained by the number of clinical trials included in the meta-analyses. For example, Lu et al. based their results on evidence mapping that included clinical trials with osteoarthritis patients and insomnia disorders. 41 Furthermore, all studies used the Pittsburg Sleep Quality Questionnaire, a valid, reliable, and gold-standard instrument for assessing sleep quality.43,44 In our umbrella review, the three included studies assessed sleep quality with different instruments. Thus, our results should be interpreted with caution due to statistical heterogeneity (I2 = 62%).
Regarding the placebo effect, robust evidence supports its impact on pain control across various clinical conditions.16,17 The predominant explanation often revolves around traditional psychological theories, encompassing patient expectations, the patient–therapist relationship, and beliefs. 17 Within this context, the utilization of acupuncture is closely tied to patient expectations and therapeutic interactions as pivotal elements. Despite this, the role of the placebo effect in acupuncture remains a subject of debate within the literature.17,18 Regarding the mechanism of acupuncture, one theory postulates improvements in health from the perspective of energy flows. 45 However, the molecular and physiological mechanisms are not yet fully described.45,46 Despite this, some studies suggest that the acupoints present a greater level of mast cells.46,47 This theory proposes that mechanical stimulation using needles could promote the degranulation of mast cells and release chemical mediators such as histamine, interleukins, prostaglandin D2, and substance P, which would increase the discharge threshold of pain nerve fibers. 47 An alternate theory argues that the needle application increases the blood flow in the nerve and muscle and promotes the release of catecholamine secretion, decreasing the skeletal muscle tone. 48 Finally, an alternative interpretation suggests that the stimulation of Aδ and C fibers in the afferent pathways acts on the spinal cord, leading to the downregulation of glial cell activity, resulting in a decrease in pain hypersensitivity. 49
While it is acknowledged that complementary therapies play a role in musculoskeletal pain management, the precise mechanisms of action remain unclear. The overall effect of these techniques is thought to stem from a combination of different factors, including but not limited to the placebo effect, 50 the natural history of the disease, regression to the mean, the Hawthorne effect, and contextual effects.51,52 Our results indicate that over 50% of the total treatment effect of acupuncture is due to contextual effects, in terms of reduction of pain intensity (58%), improvement of physical function (57%), and reduction of fatigue (69%). This aligns with the findings of a previous Cochrane review, 53 which demonstrated that in clinical trials, approximately half of the overall treatment effect could be attributed to contextual effects, emphasizing the significance of factors beyond the specific treatment impact, such as patient–therapist interaction. It is known that patient motivation, expectations, and context play a fundamental role in the activation of endogenous opioids and descending pain modulation. 54 In addition, some evidence showed that the periaqueductal gray matter and the release of dopaminergic systems are activated by therapeutic strategies that can manage the context and expectations in patients with chronic pain. 55 Therefore, therapeutic strategies that involve a patient-positive context can be strongly influenced by the placebo effect.54,55 Consequently, this topic should be considered when assessing treatment strategies in clinical practice.
Some limitations in our study may influence the reliability of our findings. First, the variability of symptoms in patients with FM could generate an important clinical heterogeneity, which could impact acupuncture effects in the meta-analysis. This heterogeneity in our study may stem from different forms of acupuncture point applications, variations in doses, and types of acupuncture across trials, as well as the variability and periods of symptom remission in FM patients. These factors likely contribute to the diversity of results and the observed heterogeneity in our study and may impact the reliability of our results. Second, it was not possible to perform a meta-analysis for the variables of fear of movement and catastrophizing, due to the limited availability of data from the included studies. Finally, although we searched eight different databases and manually checked the references of the included studies, we may have missed potentially eligible studies. Consequently, our results should be interpreted with caution.
Conclusion
This umbrella review of SR showed that there was low to very low evidence, and there were statistically significant differences in pain intensity and fatigue symptoms in favor of acupuncture. For physical function and sleep quality, there were no statistically significant differences between acupuncture and placebo or sham. However, all these differences were not clinically significant in patients with FM. In addition, more than 50% of the total treatment effect of acupuncture can be attributed to contextual effects in terms of reduction of pain intensity (58%), improvement of physical function (57%), and reduction of fatigue (69%). These findings have very important clinical implications, underscoring the importance of considering not only the direct physiological effects of acupuncture but also the broader contextual factors that contribute to its therapeutic impact in patients with FM. In addition, it is necessary to use high-value therapeutic strategies with long-term effects for patients with chronic musculoskeletal pain. Future research should assess treatments applied to patients with more standardized doses and methodological deficiencies in the clinical trials reported.
Supplemental Material
Supplemental material, sj-docx-1-tab-10.1177_1759720X241271775 for Effects of acupuncture versus placebo on clinical status and potential specific effects in Fibromyalgia: an umbrella review of 11 meta-analyses by Felipe Araya-Quintanilla, Robinson Ramirez-Vélez, Guillermo Mendez-Rebolledo, Iván Cuyul-Vásquez, Alexis Arce-Álvarez, Yasmin Ezzatvar and Héctor Gutiérrez-Espinoza in Therapeutic Advances in Musculoskeletal Disease
Acknowledgments
None.
Footnotes
ORCID iD: Héctor Gutiérrez-Espinoza  https://orcid.org/0000-0002-4650-3426
https://orcid.org/0000-0002-4650-3426
Supplemental material: Supplemental material for this article is available online.
Contributor Information
Felipe Araya-Quintanilla, Escuela de Kinesiología, Facultad de Odontología y Ciencias de la Rehabilitación, Universidad San Sebastián, Santiago, Chile.
Robinson Ramirez-Vélez, Department of Health Sciences, Public University of Navarra, Navarrabiomed-IdiSNA, Complejo Hospitalario de Navarra (CHN), Pamplona, Spain; CIBER of Frailty and Healthy Aging (CIBERFES), Instituto de Salud Carlos III, Madrid, Spain; Facultad de Ciencias de la Educación, Unidad Central del Valle del Cauca (UCEVA), Tuluá, Valle del Cauca, Colombia.
Guillermo Mendez-Rebolledo, Escuela de Kinesiología, Facultad de Salud, Universidad Santo Tomás, Talca, Chile.
Iván Cuyul-Vásquez, Departamento de Procesos Terapéuticos, Facultad de Ciencias de la Salud, Universidad Católica de Temuco, Temuco, Chile.
Alexis Arce-Álvarez, Escuela de Kinesiología, Facultad de Odontología y Ciencias de la Rehabilitación, Universidad San Sebastián, Santiago, Chile.
Yasmin Ezzatvar, Department of Nursing, University of Valencia, Valencia, Spain.
Héctor Gutiérrez-Espinoza, One Health Research Group, Universidad de las Americas, Vía a Nayon s/n, Quito 170124, Ecuador.
Declarations
Ethics approval and consent to participate: Not applicable.
Consent for publication: Not applicable.
Author contributions: Felipe Araya-Quintanilla: Conceptualization; Data curation; Methodology; Project administration; Writing – original draft.
Robinson Ramirez-Vélez: Formal analysis; Methodology; Visualization; Writing – original draft.
Guillermo Mendez-Rebolledo: Data curation; Methodology; Software; Visualization.
Iván Cuyul-Vásquez: Data curation; Methodology; Writing – original draft.
Alexis Arce-Álvarez: Data curation; Writing – original draft; Writing – review & editing.
Yasmin Ezzatvar: Data curation; Formal analysis; Writing – original draft.
Héctor Gutiérrez-Espinoza: Conceptualization; Visualization; Writing – original draft; Writing – review & editing.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
The authors declare that there is no conflict of interest.
Availability of data and materials: Not applicable.
References
- 1. Sarzi-Puttini P, Giorgi V, Marotto D, et al. Fibromyalgia: an update on clinical characteristics, etiopathogenesis and treatment. Nat Rev Rheumatol 2020; 16: 645–660. [DOI] [PubMed] [Google Scholar]
- 2. Wolfe F, Walitt B, Perrot S, et al. Fibromyalgia diagnosis and biased assessment: sex, prevalence and bias. PLoS One 2018; 13: e0203755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cabo-Meseguer A, Cerda-Olmedo G, Trillo-Mata JL. Fibromyalgia: prevalence, epidemiologic profiles and economic costs. Med Clin 2017; 149: 441–448. [DOI] [PubMed] [Google Scholar]
- 4. Macfarlane GJ, Kronisch C, Dean LE, et al. EULAR revised recommendations for the management of Fibromyalgia. Ann Rheum Dis 2017; 76: 318–328. [DOI] [PubMed] [Google Scholar]
- 5. Vas J, Méndez C, Perea-Milla E, et al. Acupuncture as a complementary therapy to the pharmacological treatment of osteoarthritis of the knee: randomised controlled trial. BMJ 2004; 329: 1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mu J, Furlan AD, Lam WY, et al. Acupuncture for chronic nonspecific low back pain. Cochrane Database Syst Rev 2020; 12: CD013814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Araya-Quintanilla F, Cuyúl-Vásquez I, Gutiérrez-Espinoza H. Does acupuncture provide pain relief in patients with osteoarthritis knee? An overview of systematic reviews. J Bodyw Mov Ther 2022; 29: 117–126. [DOI] [PubMed] [Google Scholar]
- 8. Zhang Y, Wang C. Acupuncture and chronic musculoskeletal pain. Curr Rheumatol Rep 2020; 22: 80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Deare JC, Zheng Z, Xue CC, et al. Acupuncture for treating Fibromyalgia. Cochrane Database Syst Rev 2013; 2013: CD007070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cao H, Li X, Han M, et al. Acupoint stimulation for Fibromyalgia: a systematic review of randomized controlled trials. Evid Based Complement Alternat Med 2013; 2013: 362831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kim J, Kim SR, Lee H, et al. Comparing verum and sham acupuncture in Fibromyalgia syndrome: a systematic review and meta-analysis. Evid Based Complement Alternat Med 2019; 2019: 8757685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Langhorst J, Klose P, Musial F, et al. Efficacy of acupuncture in Fibromyalgia syndrome—a systematic review with a meta-analysis of controlled clinical trials. Rheumatology (Oxford) 2010; 49: 778–788. [DOI] [PubMed] [Google Scholar]
- 13. Valera-Calero JA, Fernández-de-Las-Peñas C, Navarro-Santana MJ, et al. Efficacy of dry needling and acupuncture in patients with Fibromyalgia: a systematic review and meta-analysis. Int J Environ Res Public Health 2022; 19: 9904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Almutairi NM, Hilal FM, Bashawyah A, et al. Efficacy of acupuncture, intravenous lidocaine, and diet in the management of patients with Fibromyalgia: a systematic review and network meta-analysis. Healthcare (Basel) 2022; 10: 1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Zheng C, Zhou T. Effect of acupuncture on pain, fatigue, sleep, physical function, stiffness, well-being, and safety in Fibromyalgia: a systematic review and meta-analysis. J Pain Res 2022; 15: 315–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Vase L, Wartolowska K. Pain, placebo, and test of treatment efficacy: a narrative review. Br J Anaesth 2019; 123: e254–e262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kaptchuk TJ, Hemond CC, Miller FG. Placebos in chronic pain: evidence, theory, ethics, and use in clinical practice. BMJ 2020; 370: m1668. [DOI] [PubMed] [Google Scholar]
- 18. McGeeney BE. Acupuncture is all placebo and here is why. Headache 2015; 55: 465–469. [DOI] [PubMed] [Google Scholar]
- 19. Iolascon G, Moretti A. Myths and truths about placebo effect in rehabilitation for musculoskeletal pain. Adv Ther 2021; 38(10): 4995–5001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 2009; 6: e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bougioukas KI, Liakos A, Tsapas A, et al. Preferred reporting items for overviews of systematic reviews including harms checklist: a pilot tool to be used for balanced reporting of benefits and harms. J Clin Epidemiol 2018; 93: 9–24. [DOI] [PubMed] [Google Scholar]
- 22. Higgins JPT, Thomas J, Chandler J, et al. (eds.). Cochrane handbook for systematic reviews of interventions version 6.4 (updated August 2023). Cochrane, 2023. www.training.cochrane.org/handbook [Google Scholar]
- 23. Wolfe F, Clauw DJ, Fitzcharles MA, et al. The American College of Rheumatology preliminary diagnostic criteria for Fibromyalgia and measurement of symptom severity. Arthritis Care Res (Hoboken) 2010; 62(5): 600–610. [DOI] [PubMed] [Google Scholar]
- 24. Eriksen MB, Frandsen TF. The impact of patient, intervention, comparison, outcome (PICO) as a search strategy tool on literature search quality: a systematic review. J Med Libr Assoc 2018; 106: 420–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Salaffi F, Stancati A, Silvestri CA, et al. Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. Eur J Pain 2004; 8: 283–291. [DOI] [PubMed] [Google Scholar]
- 26. Bennett RM, Bushmakin AG, Cappelleri JC, et al. Minimal clinically important difference in the Fibromyalgia impact questionnaire. J Rheumatol 2009; 36: 1304–1311. [DOI] [PubMed] [Google Scholar]
- 27. Button KS, Kounali D, Thomas L, et al. Minimal clinically important difference on the Beck Depression Inventory—II according to the patient’s perspective. Psychol Med 2015; 45: 3269–3279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Shea BJ, Reeves BC, Wells G, et al. Amstar 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017; 21: j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Whiteside N, Sarmanova A, Chen X, et al. Proportion of contextual effects in the treatment of Fibromyalgia-a meta-analysis of randomised controlled trials. Clin Rheumatol 2018; 37: 1375–1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002; 21: 1539–1558. [DOI] [PubMed] [Google Scholar]
- 31. Furuya-Kanamori L, Barendregt JJ, Doi SAR. A new improved graphical and quantitative method for detecting bias in meta-analysis. Int J Evid Based Healthc 2018; 16: 195–203. [DOI] [PubMed] [Google Scholar]
- 32. Balshem H, Helfand M, Schünemann HJ, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 2011; 64: 401–406. [DOI] [PubMed] [Google Scholar]
- 33. Zhang XC, Chen H, Xu WT, et al. Acupuncture therapy for Fibromyalgia: a systematic review and meta-analysis of randomized controlled trials. J Pain Res 2019; 12: 527–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Martin-Sánchez E, Torralba E, Díaz-Domínguez E, et al. Efficacy of acupuncture for the treatment of Fibromyalgia: systematic review and meta-analysis of randomized trials. Open Rheumatol J 2009; 3: 25–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Mayhew E, Ernst E. Acupuncture for Fibromyalgia—a systematic review of randomized clinical trials. Rheumatology (Oxford) 2007; 46: 801–804. [DOI] [PubMed] [Google Scholar]
- 36. Yang B, Yi G, Hong W, et al. Efficacy of acupuncture on Fibromyalgia syndrome: a meta-analysis. J Tradit Chin Med 2014; 34: 381–391. [DOI] [PubMed] [Google Scholar]
- 37. Sterne JA, Egger M, Smith GD. Systematic reviews in health care: investigating and dealing with publication and other biases in meta-analysis. BMJ 2001; 323: 101–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Bidonde J, Fisher E, Perrot S, et al. Effectiveness of non-pharmacological interventions for Fibromyalgia and quality of review methods: an overview of Cochrane reviews. Semin Arthritis Rheum 2023; 63: 152248. [DOI] [PubMed] [Google Scholar]
- 39. Paoletta M, Moretti A, Liguori S, et al. Efficacy and effectiveness of extracorporeal shockwave therapy in patients with myofascial pain or Fibromyalgia: a scoping review. Medicina (Kaunas) 2022; 58(8): 1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Coskun Benlidayi I. The effectiveness and safety of electrotherapy in the management of Fibromyalgia. Rheumatol Int 2020; 40(10): 1571–1580. [DOI] [PubMed] [Google Scholar]
- 41. Lu L, Zhang Y, Ge S, et al. Evidence mapping and overview of systematic reviews of the effects of acupuncture therapies. BMJ Open 2022; 12: e056803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Lauche R, Cramer H, Häuser W, et al. A systematic overview of reviews for complementary and alternative therapies in the treatment of the Fibromyalgia syndrome. Evid Based Complement Alternat Med 2015; 2015: 610615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Backhaus J, Junghanns K, Broocks A, et al. Test-retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J Psychosom Res 2002; 53: 737–740. [DOI] [PubMed] [Google Scholar]
- 44. Larche CL, Plante I, Roy M, et al. The Pittsburgh Sleep Quality Index: reliability, factor structure, and related clinical factors among children, adolescents, and young adults with chronic pain. Sleep Disord 2021: 5546484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Zhang D, Ding G, Shen X, et al. Role of mast cells in acupuncture effect: a pilot study. Explore (NY) 2008; 4: 170–177. [DOI] [PubMed] [Google Scholar]
- 46. Wen J, Chen X, Yang Y, et al. Acupuncture medical therapy and its underlying mechanisms: a systematic review. Am J Chin Med 2021; 49: 1–23. [DOI] [PubMed] [Google Scholar]
- 47. Li Y, Yu Y, Liu Y, et al. Mast cells and acupuncture analgesia. Cells 2022; 11: 860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Kagitani F, Uchida S, Hotta H. Afferent nerve fibers and acupuncture. Auton Neurosci 2010; 157: 2–8. [DOI] [PubMed] [Google Scholar]
- 49. Ji RR, Chamessian A, Zhang YQ. Pain regulation by non-neuronal cells and inflammation. Science 2016; 354: 572–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Colloca L, Klinger R, Flor H, et al. Placebo analgesia: psychological and neurobiological mechanisms. Pain 2013; 154: 511–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. McCambridge J, Witton J, Elbourne DR. Systematic review of the Hawthorne effect: new concepts are needed to study research participation effects. J Clin Epidemiol 2014; 67: 267–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Miller FG, Kaptchuk TJ. The power of context: reconceptualizing the placebo effect. J R Soc Med 2008; 101: 222–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Hafliðadóttir SH, Juhl CB, Nielsen SM, et al. Placebo response and effect in randomized clinical trials: meta-research with focus on contextual effects. Trials 2021; 22: 493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Aigner C, Svanum S. Motivation and expectancy influences in placebo responding: the mediating role of attention. Int J Psychol 2014; 49: 488–497. [DOI] [PubMed] [Google Scholar]
- 55. Migliorini F, Maffulli N, Eschweiler J, et al. Placebo effect in pharmacological management of Fibromyalgia: a meta-analysis. Br Med Bull 2021; 139: 73–85. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-tab-10.1177_1759720X241271775 for Effects of acupuncture versus placebo on clinical status and potential specific effects in Fibromyalgia: an umbrella review of 11 meta-analyses by Felipe Araya-Quintanilla, Robinson Ramirez-Vélez, Guillermo Mendez-Rebolledo, Iván Cuyul-Vásquez, Alexis Arce-Álvarez, Yasmin Ezzatvar and Héctor Gutiérrez-Espinoza in Therapeutic Advances in Musculoskeletal Disease