Abstract
Context:
The implementation of case investigation and contact tracing (CICT) for controlling COVID-19 (caused by SARSCoV-2 virus) has proven challenging due to varying levels of public acceptance and initially constrained resources, especially enough trained staff. Evaluating the impacts of CICT will aid efforts to improve such programs.
Objectives:
Estimate the number of COVID-19 cases and hospitalizations averted by CICT and identify CICT processes that could improve overall effectiveness.
Design:
We used data on the proportion of cases interviewed, contacts notified or monitored, and days from testing to case and contact notification from 14 jurisdictions to model the impact of CICT on cumulative case counts and hospitalizations over a 60-day period. Using the Centers for Disease Control and Prevention’s COVIDTracer Advanced tool, we estimated a range of impacts by assuming either contacts would quarantine only if monitored or would do so upon notification of potential exposure. We also varied the observed program metrics to assess their relative influence.
Results:
Performance by jurisdictions varied widely. Jurisdictions isolated between 12% and 86% of cases (including contacts that became cases) within 6 to 10 days after infection. We estimated that CICT-related reductions in transmission ranged from 0.4% to 32%. For every 100 remaining cases after other nonpharmaceutical interventions were implemented, CICT averted between 4 and 97 additional cases. Reducing time to case isolation by 1 day increased averted case estimates by up to 15 percentage points. Increasing the proportion of cases interviewed or contacts notified by 20 percentage points each resulted in at most 3 or 6 percentage point improvements in averted cases.
Conclusions:
We estimated that CICT reduced the number of COVID-19 cases and hospitalizations among all jurisdictions studied. Reducing time to isolation produced the greatest improvements in impact of CICT.
Keywords: case investigation, cases averted, contact tracing, COVID-19, hospitalizations averted, modeling, transmission
Case investigation and contact tracing (CICT) is a core public health activity routinely used to reduce transmission of communicable diseases. However, COVID-19 CICT programs have found it difficult to keep pace with exponential growth in caseloads. As early as April 2020, reports surfaced that the US public health workforce was insufficient to keep pace with new COVID-19 pandemic infections.1 In addition, public acceptance and participation in CICT programs have been low in some jurisdictions.2–4 Health departments were also challenged, particularly in the early phases of the pandemic, to balance financial and human resource allocations for these programs with other community-wide interventions and policies.3,5 These difficulties created considerable variation in how COVID-19 CICT was implemented across the United States.3
Several modeling studies suggest that CICT for COVID-19 can be effective; however, these were based on simulation data rather than data collected from health departments.6,7 While a few studies reported COVID-19 CICT program performance in the United States, only 2 studies systematically evaluated programs from multiple jurisdictions.2,4,8,9 Lash et al2 reported that while CICT programs in14 jurisdictions could successfully identify and interview cases, only 1 in 3 cases reported any contacts to be notified. Spencer et al9 reported that higher caseloads per contact tracer were correlated with longer times to contact notifications. Neither study, however, estimated CICT effectiveness in terms of cases averted.
In this study, we use metrics from CICT (eg, proportion of cases interviewed, contacts notified or monitored, and days from index case testing to notification) from the 14 jurisdictions assessed by Lash et al2 to estimate the number of potential cases and hospitalizations averted. We also varied the program metrics to assess their relative influence and identify how public health officials might improve the effectiveness of CICT.
Methods
Overview
We used the Centers for Disease Control and Prevention’s (CDC’s) COVID Tracer Advanced modeling tool10 to estimate cases and hospitalizations averted because of CICT programs in 14 health departments from 11 states (including 6 counties, 2 health districts [ie, several adjacent counties], 5 entire states, and 1 tribal nation) over a 60-day observation period. The 60-day observation periods spanned from approximately June through October 2020 (before COVID-19 vaccines were approved) and were based on locations’ availability to participate in the Lash et al evaluation. COVIDTracer Advanced is a spreadsheet-based modeling tool, estimating the spread of COVID-19 and impact of interventions (including CICT strategies) in a user-defined population. All locations included in this study employed, concurrent with their CICT efforts, other nonpharmaceutical interventions (other NPIs) such as face mask policies, restrictions on large gatherings, and school and business closures. We used COVIDTracer Advanced to proportionately attribute reductions in transmission to either CICT or all other NPIs (details later).
Human subject participation in this research was reviewed by CDC and was conducted consistent with applicable federal law and CDC policy.*
Assessing net impact
We assessed the net impact of CICT in each jurisdiction by calculating low and high estimates of cases and hospitalizations averted. We also calculated the percentage of cases or hospitalizations averted by CICT out of the remaining cases after other NPIs were implemented. Essentially, for every 100 remaining cases (or hospitalizations) after other NPIs were implemented, we calculated the additional cases (and hospitalizations) averted because of CICT. These percentages allowed for comparisons of CICT impact between different sized jurisdictions.
Defining case investigation and contact tracing effectiveness
We defined CICT effectiveness as a combination of the proportion of cases (including contacts that became cases) that were effectively isolated and the time taken from infection to effective isolation. We defined effective isolation (for confirmed cases) and effective quarantine (for contacts of confirmed cases) as being placed or going into isolation or quarantine such that onward transmission of COVID-19 was essentially stopped. We used data observed by Lash et al2 at each location (Table 1) to calculate CICT Effectiveness. The observations provided the time from specimen collection to when the public health department interviewed the cases and subsequently notified contacts. In the absence of data recording when contacts were potentially infected, we assumed that, on average, 5 days passed from when a case was infected to when they became symptomatic11,12 and that cases were tested (ie, specimen collected) the day following symptom onset. We further assumed that interviewed cases and contacts isolated and quarantined themselves the day after being interviewed and notified by CICT programs. Detailed descriptions of how we estimated the time from infection to isolation and quarantine are provided in the Supplemental Digital Content Technical Appendix (available at http://links.lww.com/JPHMP/A847; see the Timing of Quarantine and Isolation section) and include a sensitivity analyses on the number of days from infection to quarantine and isolation.
TABLE 1.
Observed Case Investigation and Contact Tracing Performance Measures and Summarized Program Effectiveness for Selected Locationsa
| Location 1 | Location 2 | Location 3 | Location 4 | |
|---|---|---|---|---|
|
| ||||
| Population b | Category B | Category A | Category C | Category A |
| COVID-19 incidence c | <1/100 000 population | 6/100 000 population | 12/100 000 population | 26/100 000 population |
| Performance measures (observed d ) | ||||
| Community receptivity metrics | ||||
| % of cases interviewed | 99% | 83% | 91% | 33% |
| % of interviewed cases who named their contacts | 87% | 87% | 44% | 21% |
| Program logistics metrics | ||||
| % of all contacts identifiede | 86% | 72% | 40% | 7% |
| % of identified contacts notified | 95% | 61% | 85% | 54% |
| % of identified contacts monitored | 19% | 56% | 0% | 48% |
| Median days from testing to results notification (25th and 75th percentiles)f | 2 (1–2) | 3 (2–4) | 2 (1–4) | 5 (2–9) |
| Median days from testing to contact notification (25th and 75th percentiles)g | 2(2–7) | 5(3–10) | 7(5–12) | 7(5–12) |
| Summary effectiveness measures (calculated h ) | ||||
| % of cases and contacts isolatedi | 39.5%-86.0% | 52.7%-55.0% | 26.1%-50.5% | 11.8%-12.1% |
| Days from infection to contact isolationj | 6 | 8 | 9 | 10 |
Equivalent data for all 14 jurisdictions available in Supplemental Digital Content Appendix Table A4 (available at http://links.lww.com/JPHMP/A847).
To preserve anonymity, location populations are categorized by population size as follows: Category A >1 million; Category B >500 000 to ≤ 1 million; Category C: ≤ 500 000.
Mean daily incidence for the 60 days of the observation period.
From Lash et al.2
The number of named contacts divided by the expected number of contacts per case (Supplemental Digital Content Appendix, available at http://links.lww.com/JPHMP/A847; Equations for Case Investigation and Contact Tracing Effectiveness).
This is the reported median days from specimen collection to positive test result reported to health departments. The range in the parentheses is the 25th and 75th percentiles (ie, interquartile range).
This is the reported median days from specimen collection to contact notification. The range in the parentheses is the 25th and 75th percentiles (ie, interquartile range). This includes the days from testing to results notification.
These values were used as inputs in COVIDTracer Advanced. They were calculated from the Observed Performance Measures. See Supplemental Digital Content Appendix (available at http://links.lww.com/JPHMP/A847; Equations for Case Investigation and Contact Tracing Effectiveness section).
Low value assumes monitoring is required for effective isolation of contacts. High value assumes contact notifications are sufficient for behavior changes in notified contacts such that there is effective isolation of contacts.
The calculated length of time from infection to case isolation and contact quarantine.
Note, a portion of cases reported to the health department were unable to be reached for interview by CICT programs, and even when reached, some cases chose not to complete the interview or did not name potential contacts (Table 1; see Supplemental Digital Content Appendix Table A4, available at http://links.lww.com/JPHMP/A847).2,9 Finally, we assumed that our calculated program effectiveness values were constant (ie, not time-varying) over our 60-day observation periods.
Estimating cases averted
We used COVIDTracer Advanced to proportionately attribute reductions in transmission due to either CICT or all other NPIs. First, we entered epidemiological data that define the transmission of COVID-19 into COVIDTracer Advanced (eg, daily risk of onward transmission since infection, persons infected per infectious person, percent cases that are asymptomatic (see Supplemental Digital Content Appendix Tables A1 and A2, available at http://links.lww.com/JPHMP/A847). We also entered each jurisdiction’s population and daily COVID-19 cases13 (Table 1; see Supplemental Digital Content Appendix Table A4, available at http://links.lww.com/JPHMP/A847). Then, to define CICT effectiveness in each jurisdiction, we entered the estimated proportion of cases and contacts isolated and the days from infection to case isolation or contact quarantine (Table 1; see Supplemental Digital Content Appendix Table A4, available at http://links.lww.com/JPHMP/A847). We then entered an initial estimate of the level of reduction in transmission due to other NPIs, thus causing COVIDTracer Advanced to produce an initial plot of cumulative cases after accounting for reduction in transmission due to both CICT and other NPIs. We then adjusted our initial estimate of the effectiveness of other NPIs until the resultant plot of the cumulative cases produced by COVIDTracer Advanced closely matched the plot of actual cases (ie, we “fitted the plot”; see Supplemental Digital Content Appendix Figure A1, available at http://links.lww.com/JPHMP/A847). After estimating the effectiveness of other NPIs, we “switched off” CICT-attributed effectiveness (by setting its effectiveness to zero) in COVIDTracer Advanced while maintaining the estimated effectiveness of other NPIs. This simulated what would have happened if CICT had not occurred.
Cases averted: Low and high estimates
For each jurisdiction, we calculated a low and high estimate of cases effectively isolated due to CICT (see Supplemental Digital Content Appendix Equations 1–2, available at http://links.lww.com/JPHMP/A847). To calculate a high estimate, we assumed that all notified contacts effectively quarantined after notification of their exposure (regardless of any monitoring). That is, we assumed that just the notification of exposure would be sufficient to change the contact’s behavior and cause the contact to quarantine. To calculate a low estimate, we assumed that effective quarantine was achieved only if a contact agreed to be actively monitored for adherence to such isolation requirements (ie, follow-up phone, text, or e-mail inquiries after the initial notification from public health authorities). We also analyzed the potential that compliance with quarantine and isolation guidance was different than assumed here (see the “Sensitivity Analyses” section).
Estimating hospitalizations averted
The number of averted hospitalizations was calculated in COVIDTracer Advanced by multiplying the estimated number of averted cases by age-stratified infection-to-hospitalization rates. To simplify and maintain anonymity of locations, we used the COVIDTracer Advanced age-based default values for risks of hospitalizations for all 14 jurisdictions (see Supplemental Digital Content Appendix Table A3, available at http://links.lww.com/JPHMP/A847).
Case investigation and contact tracing scenarios
Although we analyzed the impact of CICT in all 14 locations, we selected 4 locations to highlight the range of health impacts associated with CICT implementation and the characteristics that influence program effectiveness. Our selected locations illustrate different combinations of COVID-19 burden, community receptivity to CICT (illustrated by factors such as willingness of cases to complete the interview or name contacts), and time from patient testing to when the CICT program interviewed cases and notified contacts (Table 1).
Among all 14 jurisdictions, location 1 had the lowest COVID-19 incidence (<1 daily case per 100 000 population), the greatest community receptivity to CICT, and matched several jurisdictions able to notify contacts most quickly. Location 4 was characterized by values on the other extreme: the fourth highest daily incidence (26 daily cases per 100 000 population), lowest receptivity to CICT, and longest time to notify contacts among all 14 jurisdictions. Locations 2 and 3 were characterized by values nearer to the medians of each measure. Supplemental Digital Content Appendix Table A4 (available at http://links.lww.com/JPHMP/A847) contains data similar to those in Tables 1 and 2 for all 14 locations.
TABLE 2.
Estimated Impacts of CICT, and Other NPIs, by Locationa Over 60-day Period After Contact Tracing Evaluations Initiated
| Location 1 | Location 2 | Location 3 | Location 4 | |
|---|---|---|---|---|
|
| ||||
| Transmission fraction | ||||
| Reduction from CICT | 8.6%-26.2% | 5.0%-5.2% | 1.4%-2.7% | 0.4%-0.4% |
| Reduction from other NPIsb | 54.6%-36.6% | 57.6%-57.3% | 63.5%-62.0% | 61.0%-61.0% |
| Remaining transmission (100% minus above values) | 36.8%-37.2% | 37.4%-37.5% | 35.1%-35.3% | 38.6%-38.6% |
| Additional cases averted by CICT (%c), 60 days | 651–9 480 | 12 598–13 568 | 344–768 | 859–882 |
| (67.1%-96.8%) | (47.1%-48.8%) | (15.4%-28.8%) | (4.4%-4.5%) | |
| Additional hospitalizations averted by CICT (%c), 60 days | 16–233 | 310–333 | 8–19 | 21–22 |
| (67.1%-96.8%) | (47.1%-48.8%) | (15.4%-28.8%) | (4.4%-4.5%) | |
Abbreviations: CICT, case investigation and contact tracing; other NPIs, other nonpharmaceutical interventions.
CICT implemented per scenarios in Table 1 and effects were assumed constant over 60 days.
Other NPI interventions including masks use, social distancing, school and restaurant closures, etc. Low NPI effectiveness values were generated with the fitting process when CICT effectiveness was high; similarly, high NPI effectiveness values were generated when CICT effectiveness was low.
Percent calculated as (Total Cases when only other NPIs implemented - Total Cases when both CICT and other NPIs implemented)/(Total Cases when only other NPIs implemented). Essentially, for every 100 remaining cases after other NPIs were implemented, CICT averted between 4.4 and 96.8 additional cases.
Sensitivity analyses
For the 4 selected locations, we evaluated the relative importance of 3 process measures to determine which had the most influence on the impact of CICT. The 3 process measures that we varied were as follows: (1) the proportion of cases interviewed, varied by 20 percentage points higher and lower; (2) the percentage of contacts notified or monitored, also varied by 20 percentage points higher and lower; and (3) the time (in days) needed to isolate cases, varied by 1 to 3 days faster and slower. We chose to vary these 3 measures in order to evaluate (respectively) the effect of better or worse community receptivity for CICT, compliance with quarantine and isolation guidance, and process efficiencies on CICT impacts. When a location’s baseline proportion of cases interviewed or contacts notified or monitored was above 80% (or below 20%), we capped the varied proportion at a maximum of 100% or a minimum of 0%.
We also examined the effects of adjusting the number of reported cases for underreporting and underdetection of cases. It is estimated that up to 40% of COVID-19 cases never develop any symptoms (ie, asymptomatic) and are likely not detected or reported.14 In addition, CDC’s seroprevalence surveys found that cases may be underreported and underdetected by a factor of 2 to 5 in the United States, with large variabilities across jurisdictions.15 Therefore, we performed a sensitivity analysis by increasing the reported cases by a factor of 2 and then refitting the epidemic curves to estimate impacts of CICT.
Results
Case investigation and contact tracing effectiveness
CICT metrics varied across the 14 locations, from 12% of cases and contacts isolated or quarantined 10 days postinfection at location 4 to 86% of cases and contacts isolated or quarantined 6 days postinfection at location 1 (Table 1; see Supplemental Digital Content Table A4, available at http://links.lww.com/JPHMP/A847). Assuming a 3-day preinfectious period (see Supplemental Digital Content Table A1, available at http://links.lww.com/JPHMP/A847), the days before isolation or quarantine equate to a range of 3 to 7 days of potential transmission before infected contacts were quarantined in locations 1 and 4, respectively.
The differences between a location’s low and high estimates of cases averted were greatest when the difference between the percentage of contacts notified and actively monitored was also large. For example, in locations 1 and 3, the percentage of contacts monitored was less than a quarter of the contacts notified (Table 1). This caused the high estimates of cases averted for these 2 locations to exceed the low estimate by at least twice the low estimate itself (Table 2).
Cases and hospitalizations averted
In location 1, the CICT program averted 67% to 97% of additional cases and hospitalizations over a 60-day period, measured as percentages of cases and hospitalizations averted out of the remaining cases after other NPIs were implemented (Table 2 and Figure 1).
FIGURE 1.
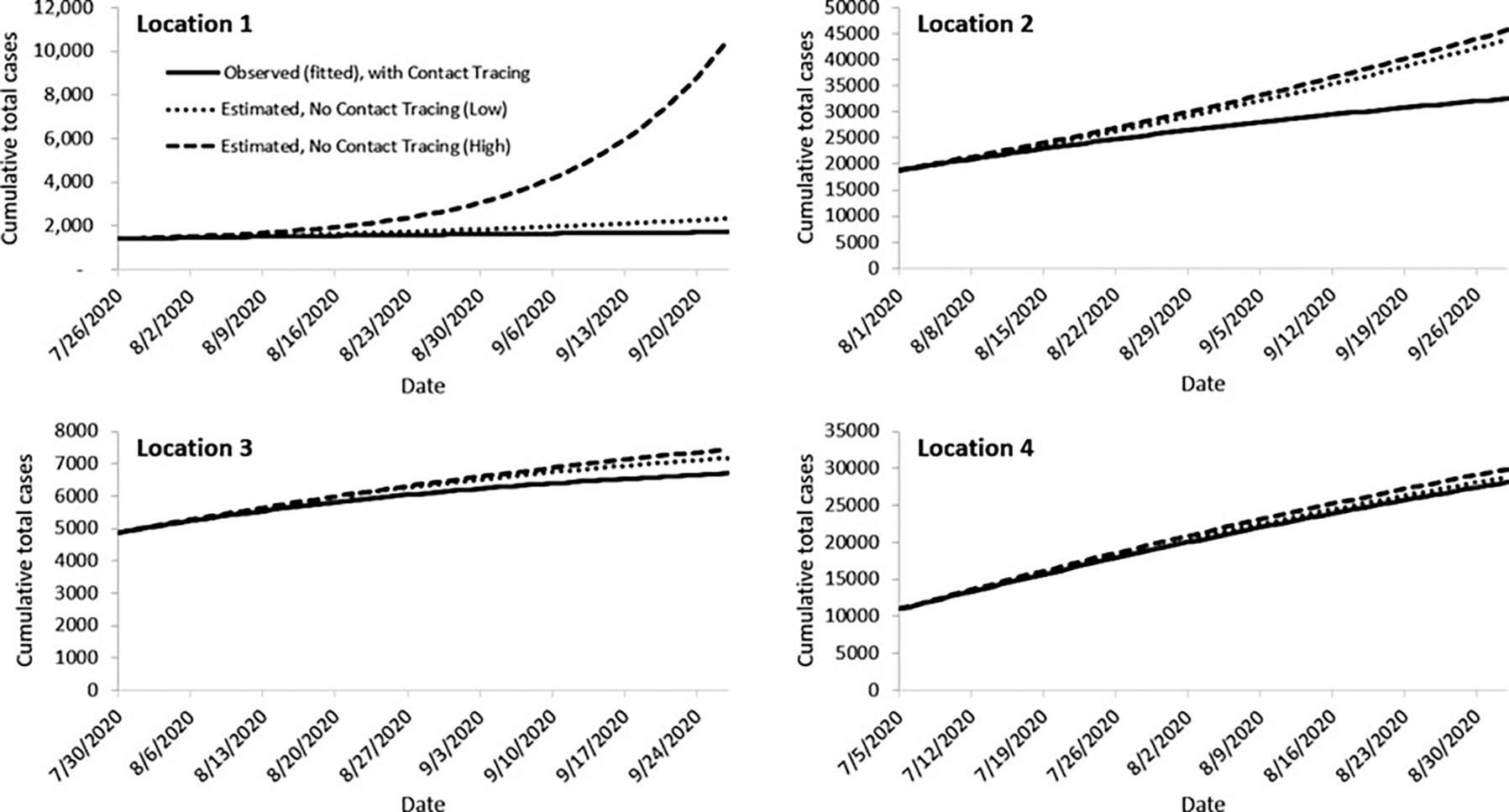
Epidemic Curves Fitted to Observed Case Counts With Case Investigation and Contact Tracing Programs, and Estimated Cases Illustrating What Might Have Occurred Had the Programs Not Been Implementeda
Abbreviations: CICT, case investigation and contact tracing; other NPIs, other nonpharmaceutical interventions.
aSolid lines are the epidemic curves at 4 evaluation locations fitted to their observed cumulative case counts with both CICT and other NPIs implemented (see Supplemental Digital Content Appendix Table A4, available at http://links.lww.com/JPHMP/A847). Dashed and dotted lines are the estimated curves illustrating the high (dashed) and low (dotted) estimates of cumulative total cases that might have occurred at these locations if CICT had not been implemented, and only other NPIs were implemented during the 60-day period. The differences between the solid and dashed or dotted lines show the benefits of CICT under low and high assumptions of program effectiveness, with greater divergence between the solid and broken lines indicating greater impact. All results assume that the effects of CICT and other NPIs were constant over the 60 days shown.
This equated to 651 to 9480 CICT-averted cases and 16 to 233 CICT-averted hospitalizations. In contrast, at location 4, 4% to 5% of additional cases and hospitalizations were averted by CICT over 60 days compared with a scenario where only other NPIs were implemented (Table 2 and Figure 1). However, because of location 4’s sizeable population (Table 1), the absolute effects of CICT on transmission were not trivial, with approximately 900 cases averted during the 60-day observation period (Table 2). At location 2, CICT averted 47% to 49% of cases and hospitalizations, and at location 3, 15% to 29% were averted by CICT (Table 2).
Results: Sensitivity analyses
The time from infection of cases to their isolation and contacts’ quarantine had the most substantial impact on the number of cases and hospitalizations averted in all 4 locations (Figure 2; see Supplemental Digital Content Appendix Table A5a–b, available at http://links.lww.com/JPHMP/A847, and Supplemental Digital Content Appendix Figure A3, available at http://links.lww.com/JPHMP/A847). Our results suggest if locations had reduced their baseline times from case exposures to isolation by 1 day, they would have increased the percentage of cases and hospitalizations averted (out of remaining cases after other NPIs had been implemented) by as much as 15 percentage points (location 2). Increasing the percentage of cases interviewed or contacts notified by 20 percentage points would have resulted in at most 3 or 6 percentage points increases in CICT-averted cases and hospitalizations (Figure 2).
FIGURE 2.
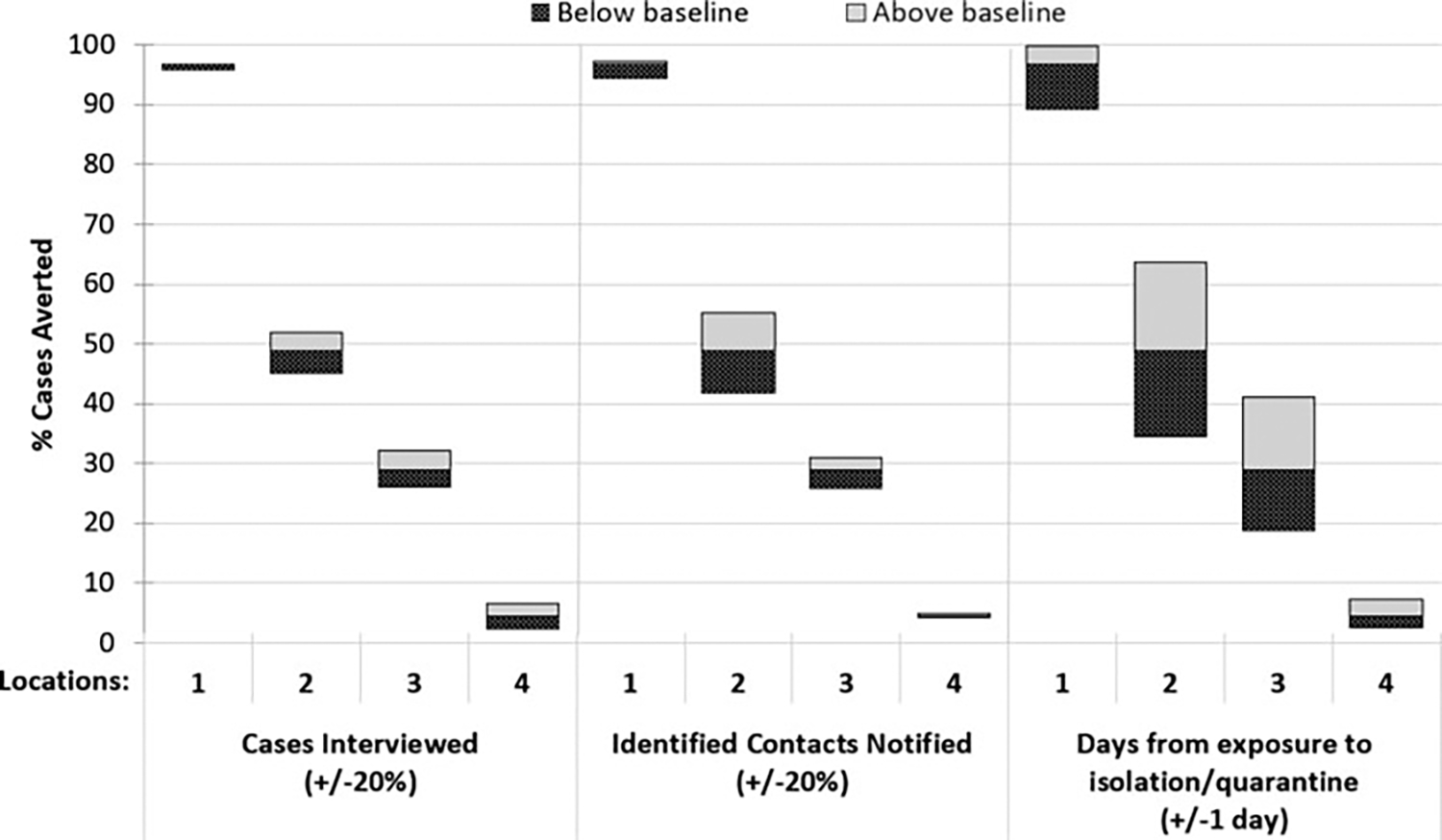
Effects of Improvements and Constraints to Case Investigation and Contact Tracing Performance Measures Compared With the Baseline Percent Cases Averted by the Programsa,b
Abbreviations: CICT, case investigation and contact tracing; other NPIs, other nonpharmaceutical interventions.
aPercent cases averted by CICT calculated as percentage of total cases averted out of remaining cases after other NPIs were implemented.
bResults shown assume notification is a sufficient trigger for contacts to quarantine (high effectiveness CICT). Results for our low CICT effectiveness scenario (ie, monitoring contacts is necessary for effective quarantine) are provided in Supplemental Digital Content Appendix Figure A3 (available at http://links.lww.com/JPHMP/A847). Baseline results are shown in Table 2. The proportion of Cases Interviewed and Contacts Notified were capped at 100% and 0% when the baseline percentage interviewed was greater than 80% or less than 20%. See Supplemental Digital Content Appendix Table A5a–b (available at http://links.lww.com/JPHMP/A847) for more detailed results.
We found that locations with a longer baseline number of days between case exposures and their isolation experienced greater impact from reducing this time. For example, location 2 could have increased the proportion of cases averted by 15 percentage points simply by speeding up isolation from 9 to 8 days. In contrast, if location 1 reduced its time to case isolation from 6 to 5 days, cases averted would have improved by only 0.3% (see Supplemental Digital Content Appendix Table A5a, available at http://links.lww.com/JPHMP/A847).
For the sensitivity analysis examining the impact of under-reported and under-detected cases (where we increased reported cases by a factor of two), we found that such adjustment leads to decreased reductions in transmission and estimates of cases averted due to CICT (see Supplemental Digital Content Appendix Table A7, available at http://links.lww.com/JPHMP/A847).
Discussion and Conclusions
Our modeled estimates of cases and hospitalizations averted illustrate that CICT can be effective in containing the impact of COVID-19. Impacts due to CICT varied widely across the locations studied, averting 4% of cases and hospitalizations in one locale to 97% in another, from among the remaining cases and hospitalizations after other NPIs were implemented. These estimated reductions were also substantial on an absolute basis, ranging from 859 averted cases (0.1% of location 4’s population) to 9480 (1.5% of location 1’s population) over a 60-day period. Such sizeable estimates of averted cases are partially due to the success of CICT programs at suppressing the exponential growth in cases associated with uncontrolled transmission (2.5 new infections per case without interventions and almost all the population susceptible to infection [see Supplemental Digital Content Table A2, available at http://links.lww.com/JPHMP/A847]), compounded over approximately 10 generations of infection that occur in our 60-day observation period. For example, at location 1 where our estimates of CICT impacts were greatest, our low estimate of the effects of other NPIs on transmission (a 36.6% reduction) caused transmission to drop from 2.5 infections per infectious case to 1.6. When we add our estimated effect of CICT to the transmission reductions already afforded by other NPIs (a further 26.2% reduction in transmission), the effective number of new infections per infectious case drops to below 1 (0.93). An epidemic is waning any time that the number of new infections per infectious case drops below 1.0. We found large percentage reductions in cases (90%+) at locations where the combined effects of CICT and other NPIs approached (or dropped below) 1 new infection generated per case (locations 1, 5, and 6; see Supplemental Digital Content Table A4, available at http://links.lww.com/JPHMP/A847).
Our modeled estimates indicate that reducing the time from infection to case isolation and contact quarantine (even by just 1 day) provides the biggest gain in improving the impact of CICT. We found this to be true even when compared with the potential impact of a 20% increase in percentage of cases interviewed or contacts notified and monitored. For example, even if locations 2 and 3 had interviewed 100% of their cases and notified 100% of the identified contacts, they would not have achieved the same gains in cases and hospitalizations averted as if they had reduced the time to case isolation by a single day. Our results are consistent with previous studies that found that minimizing testing delay or onset-to-isolation delay had the largest impact on reducing onward transmissions.6,16,17 The benefits from doing so are most pronounced (ie, will yield the greatest impact on cases averted) among jurisdictions with longer delays (8 days or longer after case infection) to notify and isolate contacts.
It should be noted that we do not attribute to any single factor the potential impacts of reductions in time from exposure to isolation and quarantine. Our estimates of additional averted cases could have been achieved from any combination of many factors, such as earlier testing of cases, less time between patient testing and test results reported to the health department, shorter time from test results received to contact notification, or from contacts choosing to quarantine more quickly. While these and other process metrics can be improved by increasing the number of case investigators and contact tracers or with automated systems and technology upgrades, options exist that may not require many additional resources. For example, health departments can prioritize interviewing cases or notifying contacts of COVID-19 cases most recently tested, or those experiencing fewer days of symptomatic illness. In addition, when contact tracers’ caseloads are high, devoting less time to cases and contacts that are unreachable or do not respond to messages may reduce effective time from infection to isolation and quarantine.
This study has several strengths. First, this work can be replicated by other jurisdictions that are interested in estimating direct health impact of CICT activities. The tool we used, COVIDTracer Advanced, is publicly available and designed for use by practicing public health officials, although its use for this analysis required advanced familiarity of features.10 In addition, by aggregating and presenting systematically collected data from multiple anonymized jurisdictions, we were able to show the range of potential effects, from health departments experiencing resource constraints to those with ample support.
A primary limitation of this study is that we did not directly measure the proportions of cases that effectively isolated and contacts that correctly quarantined. In addition, there is a lack of data on the levels of compliance among the population for whom we sought to model CICT’s impacts: individuals who directly interacted with their health departments and provided quarantine guidance (see Supplemental Digital Content Appendix, available at http://links.lww.com/JPHMP/A847, section, titled Compliance With Quarantine and Isolation Guidance). In the absence of clear data suggesting otherwise, we assumed cases and contacts comply with isolation and quarantine guidance upon completing case interviews, being notified of their exposures, or when they agree to undergo daily monitoring for COVID-19–like symptoms. While our assumed compliance among individuals notified of their exposures but not monitored may be overly optimistic, our associated high estimates of cases averted offer insight into the potential benefits from galvanizing high public compliance with quarantine guidance. Similarly, our low-impact estimates, based on the assumption that active monitoring is necessary for individuals to adhere to isolation/quarantine guidance, likely underestimates overall compliance levels. This is because, under this scenario, we assume no compliance (0%) among individuals notified of their exposure but not actively monitored. Notably, our conclusions regarding the relative influence of CICT measures are not affected by this limitation, with single-day changes in time to contact notification being more important than 20 percentage point changes (or less) in compliance (Figure 2; see Supplemental Digital Content Appendix Figure A3, available at http://links.lww.com/JPHMP/A847, and Supplemental Digital Content Appendix Table A5a–b, available at http://links.lww.com/JPHMP/A847). Finally, we do not know whether Exposure Notification (EN) Apps (ie, smartphone-enabled contact tracing apps) were utilized by locations during the observation period we analyzed, and if so, how their use would have affected compliance with isolation.
Our study has other limitations. We assumed that the effectiveness of CICT and other NPIs remained constant over a 60-day period. Since we were able to approximate the observed cumulative epidemic curves for most locations we studied, this assumption appears reasonable for our observation period (see Supplemental Digital Content Figure A1, available at http://links.lww.com/JPHMP/A847). Another limitation is that, in using the COVIDTracer Advanced age-based default values for risks of hospitalizations for all 14 jurisdictions, we do not account for the potential that age-based admissions of COVID-19 patients may differ from one location to another. As such, we may over- or underestimate the hospitalizations prevented. We believe, however, that it is unlikely that incorporating location-specific precision on hospitalizations would yield any different policy choices. Finally, we do not quantify or account for the resources and effort necessary to achieve the gains possible by focusing on notification speed over increasing the proportions of cases interviewed or contacts notified.
Our analysis combined primary implementation data with modeling to assess the health impact of COVID-19 CICT in the United States. While we illustrated that CICT can be effective at reducing onward transmission in some jurisdictions, other jurisdictions saw limited effectiveness. The exact reasons for, and the relative importance of, the potential factors causing such reduced levels of impact remain to be investigated. This work provides public health decision makers with an understanding of the benefits that CICT programs can produce as well as ideas for prioritizing potential improvements of such programs.
Supplementary Material
Implications for Policy & Practice.
Case investigation and contact tracing can be effective in preventing COVID-19 infections and hospitalizations.
Greatest improvements in the impact of COVID-19 case investigation and contact tracing can be achieved by reducing the time to notify cases and contacts (even by just 1 day, presuming subsequent isolation and quarantine). The benefits from reducing time to notification will be most pronounced among jurisdictions with longer delays between when patients provide a sample for testing and when cases and contacts are notified and requested to isolate or quarantine.
Jurisdictions can potentially improve the speed of notification without additional resources by (1) prioritizing cases and their contacts that are most recently tested (or those experiencing fewer days of symptomatic illness); (2) devoting less time to cases and contacts that are unreachable or do not respond to messages; (3) limiting the duration of calls (eg, using less questions or a shorter script) during periods of high caseloads.
Acknowledgments
This work was performed as part of the official duties of all participants in support of the US CDC’s COVID-19 Response.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
No conflicts of interest to report.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (http://www.JPHMP.com).
Written work prepared by employees of the Federal Government as part of their official duties is, under the U.S. Copyright Act, a “work of the United States Government” for which copyright protection under Title 17 of the United States Code is not available. As such, copyright does not extend to the contributions of employees of the Federal Government.
Contact Tracing Impact Group (alphabetically listed): Greta Anschuetz, Robert Bonacci, Brittany Byers, Joshua Clayton, Nickolas DeLuca, Matthew Donahue, Catherine Donovan, Veronica Fialkowski, Aaron Fleischauer, Heather Forbes, Clay Goddard, Heather Grome, Gibbie Harris, Susan Hayes, Blake Hendrickson, Julia Janssen, Sara Johnson, Amanda Jones, Catherine J. Knott, Reed Magleby, Stephen A. McCurdy, Alana McGrath, Heather McLaughlin, James Miller, Zack Moore, Michelle Morris, Jill Moses, Allison Newman, Sai Paritala, Caroline Q. Pratt, Lauren Prinzing, Pratima Raghunathan, Jonathan Steinberg, Alana Sulka, Christina G. Tan, Melanie Taylor, Puthiery Va, Kate Varela, Andee Weisbeck, and Matthew Willis.
See, for example, 45 CFR part 46, 21 CFR part 56; 42 USC §241(d); 5 USC §552a; 44 USC §3501 et seq.
References
- 1.Center for Health Security, Johns Hopkins Bloomberg School of Public Health. A national plan to enable comprehensive COVID-19 case finding and contact tracing in the US. https://www.centerforhealthsecurity.org/our-work/pubs_archive/pubs-pdfs/2020/200410-national-plan-to-contact-tracing.pdf. Published 2020. Accessed May 1, 2021. [Google Scholar]
- 2.Lash RR, Moonan PK, Byers BL, et al. COVID-19 contact tracing in the United States, 2020. JAMA Netw Open. 2021;4(6):e2115850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ruebush E, Fraser MR, Poulin A, Allen M, Lane JT, Blumenstock JS. COVID-19 case investigation and contact tracing: early lessons learned and future opportunities. J Public Health Manag Pract. 2021;27(suppl 1):S87–S97. [DOI] [PubMed] [Google Scholar]
- 4.Lash RR, Donovan CV, Fleischauer AT, et al. COVID-19 contact tracing in two counties—North Carolina, June-July 2020. MMWR Morb Mortal Wkly Rep. 2020;69(38):1360–1363. https://www.cdc.gov/mmwr/volumes/69/wr/mm6938e3.htm. Accessed May 1, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Megnin-Viggars O, Carter P, Melendez-Torres GJ, Weston D, Rubin GJ. Facilitators and barriers to engagement with contact tracing during infectious disease outbreaks: a rapid review of the evidence. PLoS One. 2020;15(10):e0241473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hellewell J, Abbott S, Gimma A, et al. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Global Health. 2020;8(4):e488–e496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Keeling MJ, Hollingsworth TD, Read JM. Efficacy of contact tracing for the containment of the 2019 novel coronavirus (COVID-19). J Epidemiol Community Health. 2020;74(10):861–866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sachdev DD, Brosnan HK, Reid MJA, et al. Outcomes of contact tracing in San Francisco, California—test and trace during shelter-in-place. JAMA Intern Med. 2021;181(3):381–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spencer KD, Chung CL, Stargel A, et al. COVID-19 case investigation and contact tracing efforts from health departments—United States, June 25-July 24, 2020. MMWR Morb Mortal Wkly Rep. 2021;70(3):83–87. https://www.cdc.gov/mmwr/volumes/70/wr/mm7003a3.htm. Accessed May 1, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. COVIDTracer Advanced: a planning tool to illustrate the resources needed to conduct contact tracing and monitoring of coronavirus disease 2019 (COVID-19) cases and the potential impact of community interventions and contact tracing efforts on the spread of COVID-19 2020. https://www.cdc.gov/coronavirus/2019-ncov/php/contact-tracing/COVIDTracerTools.html. Accessed May 1, 2021.
- 11.He X, Lau EHY, Wu P, et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med. 2020;26(5):672–675. [DOI] [PubMed] [Google Scholar]
- 12.He X, Lau EHY, Wu P, et al. Author correction: temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med. 2020; 26(9):1491–1493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. COVID Data Tracker. https://covid.cdc.gov/covid-data-tracker. Accessed May 1, 2021.
- 14.Centers for Disease Control and Prevention. COVID-19 pandemic planning scenarios. https://www.cdc.gov/coronavirus/2019-ncov/hcp/planning-scenarios.html. Updated February 14, 2021. Accessed May 1, 2021.
- 15.Angulo FJ, Finelli L, Swerdlow DL. Estimation of US SARS-CoV-2 infections, symptomatic infections, hospitalizations, and deaths using seroprevalence surveys. JAMA Netw Open. 2021;4(1): e2033706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kretzschmar ME, Rozhnova G, Bootsma MCJ, van Boven M, van de Wijgert JHHM, Bonten MJM. Impact of delays on effectiveness of contact tracing strategies for COVID-19: a modelling study. Lancet Public Health. 2020;5(8):e452–e459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention. Prioritizing COVID-19 contact tracing mathematical modeling methods and findings. https://www.cdc.gov/coronavirus/2019-ncov/php/contact-tracing/contact-tracing-plan/prioritization/mathematicalmodeling.html. Published March 24, 2021. Accessed May 1, 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


