Abstract
Background
Transforaminal epidural injections (TEI) can alleviate symptoms and help to maintain physical functioning and quality of life in patients with lumbar radicular pain. We aim to develop a prediction model for patient outcome after TEI in patients suffering from unilateral lumbar radicular pain due to lumbar disc herniation (LDH) or single-level spinal stenosis (LSS). The secondary aim is to estimate short-term patient outcome differences between LDH and LSS patients, the association between psychological variables and patient outcome, the rate of additional injections, surgery and complications, and to explore the short-term cost-effectiveness of TEI.
Methods
This study is designed as a multi-centre, observational, prospective cohort study in two large regional hospitals in the Netherlands. Patients diagnosed with unilateral lumbar radicular pain secondary to LDH or LSS and congruent with MRI findings, who are referred for TEI along usual care pathways, are eligible for study participation. A total of 388 patients with LDH or LSS will be included. A pre-defined set of demographic, clinical and radiological variables will be used as the predictors in the model. The primary outcome measure is the Numerical Rating Scale (NRS) for leg pain. Secondary outcome measures include back pain, physical functioning, perceived recovery, pain coping strategies, anxiety and depression and use of analgesics and physical therapy. Patients will be evaluated at baseline, 2 weeks and 6 weeks after treatment. NRS leg pain and Likert perceived recovery data will be used as the dependent variables in a generalized linear mixed model for prediction of TEI outcome, with internal validation of performance (explained variation) by bootstrap resampling. Cost-effectiveness for a period of 6 weeks prior to and after treatment will be performed with decision-analytic modelling.
Discussion
Patients with severe lumbar radicular pain often request additional treatment when conservative care is insufficient. TEI can offer relief of symptoms. Currently, it is not possible to predict responsiveness to this treatment for individual patients. This study is designed to explore predictors that can differentiate between patients that will and will not have a positive outcome after TEI. This information may support treatment strategies for this patient group.
Trial registration
This study is registered at ClinicalTrials.gov database under registry number NCT04540068 on September 1, 2020.
Keywords: Lumbar radicular pain, Spinal stenosis, Lumbar disc herniation, Transforaminal epidural steroid injection, Lumbar spine, Prediction model, Cost-effectiveness
Background
Unilateral lumbar radicular pain is a common symptom of lumbar radiculopathy, a spinal condition with a reported lifetime prevalence of up to 43%, depending on the exact definition of this condition [1]. Generally, lumbar radicular pain is explained as a symptom when the function of one of the exiting lumbosacral nerve roots is affected [2]. The two most common causes are lumbar disc herniation (LDH) and degenerative lumbar spinal stenosis (LSS) due to age-related disc degeneration, hypertrophy of the ligamentum flavum and zygapophyseal joint, and osteophyte formation [3]. Both may result in radiating leg pain, which can be accompanied by back pain, and sensory and motor deficits. Lumbar radicular pain is often insufficiently explained by merely mechanical compression of the nerve root, and, therefore, it is suggested that, additionally, inflammatory and immunological processes are involved in LDH and LSS [4–6]. Disease progression, however, usually differs as patients with LDH are younger on average and have a more acute onset of symptoms which may aggravate when coughing, sneezing or leg-straightening, while patients with LSS often are older and experience gradually increasing symptoms that may exacerbate during standing or walking. Nonetheless, in both patient groups symptoms can severely limit physical functioning, decrease quality of life, and result in absenteeism. Symptoms are expected to spontaneously diminish with time in the majority of LDH patients as this condition is considered to be self-limiting. Hence, guidelines advise conservative treatment for the first weeks to months before opting for non-conservative therapies [7–9]. For LSS there is less general agreement on the most appropriate treatment strategy as symptoms usually follow a more chronic course, although some patients may experience natural resolution of symptoms as well [10–12]. For both patient groups, however, symptoms are frequently insufficiently alleviated with oral pain medication, and, due to the debilitating consequences, medical and socio-economic costs are tremendous in this patient population [13–16].
Transforaminal epidural steroid injections (TEI) have become a growingly popular treatment modality in patients with severe lumbar radicular pain to relieve symptoms. TEI aims to reduce the inflammation around the affected nerve root by limiting nerve root oedema, blocking prostaglandin synthesis and altering the conduction of nociceptive C-fibres [17–20]. The rationale behind this minimally invasive treatment is that it enables the patient to maintain physical functioning, restores quality of life, and, if satisfactorily effective, obviates the need for neurosurgical intervention. However, TEI is considered to have a temporary effect, and it remains unclear in what part of the patients symptoms may reoccur necessitating repeat injections or surgery on the short term nonetheless. Specifically in patients with LSS, which is thought to be more chronic and less self-limiting than LDH, there is debate regarding the efficacy of TEI.
Several systematic reviews and meta-analyses have been conducted on the efficacy of TEI in patients with lumbar radicular pain due to LDH and LSS which demonstrated varying success rates ranging between 19% and 88.4% [21–30]. It is suggested that TEI is likely to be more beneficial in carefully selected subgroups of patients with lumbar radicular pain, explaining the variation and overall modest effect of this treatment in the whole patient group. Therefore, prognostic factors should be identified that could aid in improving patient selection allowing for more tailored treatment strategies in patients with lumbar radicular pain. Numerous demographic, clinical and radiological factors have been assessed for their association with TEI outcome across multiple studies, but few factors have been demonstrated to be consistently significantly associated [31–47] (Table 1). The most consistent prognostic factors for TEI included a shorter duration of symptoms in 3 out of 7 studies (OR 2.6 and 2.5 for VAS ≥ 50% and Roland-Morris disability score ≥ 40% reduction; r -0.48 and -0.36 for VAS and ODI) [38, 43], a positive Slump test in 2 out of 2 studies (Nagelkerke R2 0.10 for VAS leg pain and 0.17 for ODI) [34], degree of nerve root compression in 3 out of 4 studies (R2 0.06 for VAS leg pain and ODI) [35] and radiological etiology of symptoms in 2 out of 5 studies (measure of strength of association not reported). Since there was large methodological variability among studies, strength of association was not always reported and the majority of variables were evaluated in a small number of studies. A reliable predictive model suitable for clinical practice is lacking. Furthermore, psychological variables may affect patient outcome after TEI treatment similarly to spine surgery, but have not been assessed before in relation to this therapy [48, 49].
Table 1.
Variables associated with prediction of TEI outcome in previous studies. Only variables assessed in two studies or more were included. Variables that will be included in the core set of predictors for the model in this study are indicated by an asterisk
| Prediction factor for TEI outcome | Number of studies that found an association | References | Number of studies that did not find an association | References | Core set |
|---|---|---|---|---|---|
| Demographic factors | |||||
| Age | 1 | [38] | 5 | [31, 33, 39, 40, 45] | * |
| BMI | 1 | [38] | 1 | [45] | |
| Duration of symptoms | 3 | [33, 38, 43] | 4 | [31, 39, 40, 45] | * |
| Injection level | 0 | 5 | [31, 39, 41, 45, 47] | ||
| Injection side | 0 | 4 | [31, 38, 39, 47] | ||
| Sex | 1 | [38] | 5 | [31, 39–41, 45] | * |
| Clinical factors | |||||
| Pre-injection pain score | 1 | [38] | 3 | [33, 42, 45] | * |
| Pre-injection functionality score | 1 | [38] | 1 | [42] | |
| Positive Slump test | 2 | [34, 35] | 0 | ||
| Post-injection pain score | 1 | [45] | 1 | [42] | |
| Radiological factors | |||||
| Lesion level | 0 | 2 | [31, 33] | ||
| Lesion severity | 1 | [32] | 2 | [31, 36] | |
| Location of LDH | 2 | [35, 37] | 2 | [33, 47] | * |
| Degree of nerve root compression | 3 | [34, 35, 47] | 1 | [45] | * |
| Presence of transitional vertebrae | 2 | [44, 46] | 1 | [45] | |
| Radiological etiology of symptoms | 2 | [31, 41] | 3 | [33, 34, 40] | * |
| Type of disc degeneration | 1 | [35] | 1 | [47] | |
BMI Body Mass Index, LDH lumbar disc herniation, TEI transforaminal epidural injection
Therefore, a systematic assessment of demographic, clinical and radiological factors and their association with TEI outcome in patients with LDH or LSS is needed in a sufficiently large prospective cohort study. Since the purpose of TEI treatment is to rapidly resolve symptoms, the study’s primary aim is to develop a multivariable prediction model for short-term patient outcome with internal validation of performance. In addition to this prediction model, we aim to determine the association between psychological baseline variables and patient outcome measures as this has not been explored before. Furthermore, as a secondary study objective we intend to explore the short-term cost-effectiveness of TEI. TEI is intended to relief pain symptoms, and, when the effect is satisfactory, may result in reduction of analgesic intake and physical therapy sessions. Moreover, patients with severe symptoms may take a sick-leave from work which has substantial socioeconomic costs. However, this the effect of TEI on these variables has not been studied thoroughly before. We aim to explore the medical expenditures and absence from labour before and after TEI treatment.
Methods and design
This protocol has been aligned with the Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD) statement and checklist [50].
Design and study setting
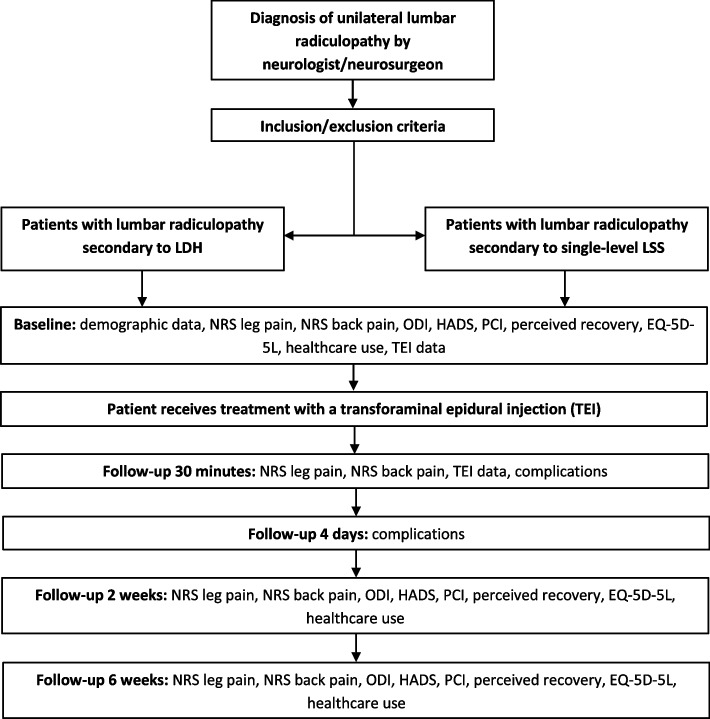
The POTEISS (Prediction of Transforaminal Epidural Injection Success in Sciatica) study is designed as a multicentre, prospective, observational cohort study and is performed in accordance with recommendations by the PROGRESS framework [51]. The study is initiated at the Leiden University Medical Center (LUMC), Leiden, the Netherlands and enrolling patients at the outpatient pain clinic in the Spaarne Hospital (SG), Hoofddorp and Haarlem, the Netherlands and in the Groene Hart Hospital (GHZ), Gouda, the Netherlands since November 2020 with, currently, a total of 115 patients included. Patients that are referred to the pain clinic and that have a scheduled appointment for treatment with TEI as part of standard care are screened for eligibility. When meeting the inclusion criteria, patients are contacted by the study investigator and invited to participate. Follow-up will be performed by completion of a case report form at 30 min follow-up and by sending digital questionnaires through e-mail at baseline, 4 days, 2 and 6 weeks follow-up which are automatically processed in an online secure database once completed. A schematic overview of study procedures is provided in Fig. 1.
Fig. 1.
Flow chart of study procedures
Aims and objectives
The aim of the POTEISS study is to explore patient outcome after TEI in patients with unilateral lumbar radicular pain secondary to lumbar disc herniation or degenerative spinal stenosis and to identify subgroups that benefit more or less from this treatment.
The primary objective is to:
Develop a model based on demographic, clinical and radiological variables for prediction of patient outcome after TEI (outcome defined as ≥ 30% improvement in NRS leg pain; see also Primary analysis section, or defined as a perceived recovery Likert score of 1 or 2; see also Secondary analysis section)
Secondary objectives are to:
Estimate short-term patient outcome after TEI in patients with LDH and LSS
Determine the association between psychological baseline variables and patient outcome measures
Determine the rate of additional injections, surgery and complications after treatment with TEI
Explore the short-term cost-effectiveness with decision-analytic modelling
Eligible study participants and recruitment
The patients are selected from the referral database at the pain clinic. Patients suffering from an episode of unilateral lumbar radicular pain due to LDH or single-level LSS diagnosed by the neurologist or neurosurgeon, congruent with radiological imaging (MRI), and scheduled for treatment with TEI are screened for study participation. The clinical diagnosis of lumbar radicular pain, with or without other symptoms associated with lumbar radiculopathy, by the neurologist or neurosurgeon is based on history taking and physical examination and must be supported with a radiological diagnosis of LDH or LSS on MRI. Lumbar radicular pain is defined as a painful sensation that radiates from the back towards the leg, usually going below the knee and is often described by patients as electric, shooting or cramping. Clinical presentation in case of LDH usually involves a more acute onset with a constant pain which is episodically aggravated and often not dependent on the patient’s position. Patients with clinically suspected LSS usually describe a more gradual onset and progression of with unilateral radicular pain that may be aggravated by walking or standing. In both cases, MRI findings must be congruent with clinical findings, i.e., lumbar level. If MRI results are not congruent with clinical findings, the patient is not eligible for inclusion. TEI treatment appointments are made by a pain clinic nurse as part of standard care. A complete description of inclusion and exclusion criteria can be found in Table 2.
Table 2.
Patient inclusion and exclusion criteria
| Inclusion criteria | Exclusion criteria |
|---|---|
| Clinical diagnosis of unilateral lumbar radicular pain by neurologist or neurosurgeon |
Age under 18 years Severe multisegmental spinal disease |
|
Radiological diagnosis of LDH or LSS on MRI and congruent with clinical findingsa Scheduled appointment for TEI Access to e-mail |
Anatomical abnormalities that may complicate the procedure technically (e.g. severe scoliosis) History of lower back surgery at the same lumbar level and side |
| Signed informed consent |
Previous treatment with TEI for current episode of lumbar radicular pain Active malignancy or infectious disease Use of immunosuppressive drugs Use of systemic corticosteroids in preceding 3 months |
| Circumstances that prevent treatment with TEI (e.g. use of anticoagulants that cannot be temporarily discontinued, allergy against steroids or local anaesthetic) | |
|
Pregnancy Major language barrier |
aDefinitions of LDH and LSS are provided in the Definition of lumbar disc herniation and degenerative spinal stenosis on MRI section. LDH lumbar disc herniation, LSS lumbar spinal stenosis, MRI magnetic resonance imaging, TEI transforaminal epidural injection
Definition of lumbar disc herniation and degenerative spinal stenosis on MRI
For this study, lumbar disc herniation is defined as the presence of protrusion, extrusion or sequestration of an intervertebral disc without other significant degenerative changes that may affect the nerve root at that level. Central lumbar disc herniation will be eligible only if symptoms are unilateral and cauda equina syndrome is absent. Patients with symptoms due to an extraforaminal disc herniation are included as well.
Degenerative spinal stenosis is defined as narrowing of the spinal canal, lateral recess or neuroforamen due to degenerative changes of the bony structures (osteophytes) and surrounding tissues including ligaments, zygapophyseal joints, and a bulging intervertebral disc. Only patients with a stenosis causing unilateral symptoms are eligible. Patients with synovial (facet) cysts, neoplasm or spondylolisthesis resulting in stenosis will be excluded.
Evident physical compression of the nerve root will not be an eligibility criterion, but compression will be graded for analysis of MRI data (see also Secondary study parameters section), since in patients without evident nerve root compression inflammatory processes may be a key contributor that can be treated with a transforaminal epidural steroid injection [52–54].
Intervention procedures
Transforaminal epidural injection (TEI)
Administration of the transforaminal epidural injection (TEI) will be performed by multiple experienced anaesthesiologists from the participating hospitals. The treating anaesthesiologist determines the treatment level based on clinical findings and radiological imaging (diagnosed by neurologist or neurosurgeon). The patient will lie in a prone position on the table with a support underneath to reduce the natural lordosis. The skin is sterilized with chlorhexidine and locally anaesthetized with 1 mL 1% lidocaine. Under fluoroscopic image guidance the needle is placed via a transforaminal approach in close proximity of the nerve root. This is achieved by advancing the needle subpedicularly towards the safe triangle which is confined by the inferior border of the pedicle, the exiting nerve root and inferiorly from the anterior margin of the pedicle [55] (Fig. 2).
Fig. 2.
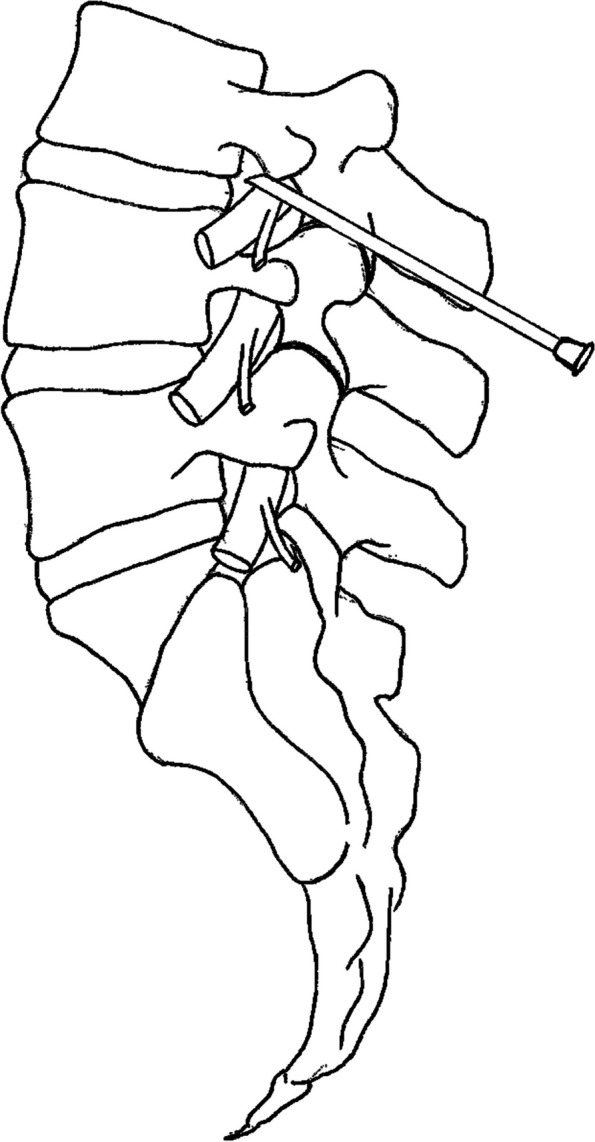
Transforaminal approach into the safe triangle space. This space is confined by the inferior border of the pedicle, the exiting nerve root and inferiorly from the anterior margin of the pedicle
Contrast agent is injected to confirm correct positioning of the needle. In case of incorrect positioning, the needle is retracted and repositioned towards the correct location. In accordance with current Dutch anaesthesiologic guidelines, injections at L3 and below will contain 1,5 ml lidocaine 2% and 40 mg methylprednisolone acetate and injections above L3 will contain 1,5 ml lidocaine 1% and 10 mg dexamethasone to prevent possible vascular occlusion of the artery of Adamkiewicz [56]. After the procedure, the patient will stay for 30 min at the recovery room for monitoring.
Adjuvant care
Since this is an observational cohort study, patients are allowed to use any type of adjuvant care as they require. This may include, but is not limited to, analgesic usage and physical therapy. To compare the use of concomitant therapy between groups, the patients are requested to register their use of oral pain medication and physical (rehabilitation) therapy during follow-up.
Data collection and protection
Data will be collected using Castor EDC, a web-based data capture platform (Ciwit B.V., Amsterdam, The Netherlands). After study participation has been confirmed and informed consent has been provided, the patient will complete baseline questionnaires the day before TEI treatment. For all follow-up moments the patient will receive an e-mail with a hyperlink to the questionnaires to fill in at home. When the questionnaires are completed, they will be automatically processed anonymously in Castor EDC. All data will be safeguarded and stored for 15 years after end of study. In the database each patient is given an untraceable ID that can only be linked to the patient’s personal details with a key file. Access to this key file and the final dataset will only be granted to members of the research team, an independent monitor and the Inspection for Healthcare Inspection and Youth (IGJ).
Study parameters and follow-up
Demographic data are assessed at baseline by an independent researcher and outcome measurements are self-reported by the patient. Follow-up starts on the day of treatment and patients fill in questionnaires at 4 days, 2 and 6 weeks after treatment. Patients are not entitled to see results from previous follow-up moments. A summary of all outcome measurements for each follow-up moment can be found in Table 3.
Table 3.
Data collection schedule
| Baseline | Follow-up | ||||
|---|---|---|---|---|---|
| 30 min | Day 4 | Week 2 | Week 6 | ||
| Demographic data | ✓ | ||||
| NRS leg pain | ✓ | ✓ | ✓ | ✓ | |
| NRS back pain | ✓ | ✓ | ✓ | ✓ | |
| ODI | ✓ | ✓ | ✓ | ||
| HADS | ✓ | ✓ | ✓ | ||
| PCI | ✓ | ✓ | ✓ | ||
| Perceived recovery | ✓ | ✓ | |||
| EQ-5D-5L | ✓ | ✓ | ✓ | ||
| Health care usea | ✓ | ✓ | ✓ | ||
| TEI dataa | ✓ | ✓ | |||
| Complications | ✓ | ✓ | |||
aSpecifics on the collected data are provided in the Secondary study parameters section. HADS Hospital Anxiety and Depression Scale, NRS numerical rating scale, ODI Oswestry Disability Index, PCI pain coping inventory, TEI transforaminal epidural injection, VAS visual analogue scale
Primary study parameter
The primary study outcome measure, the Numerical Rating Scale (NRS) for leg pain, will be assessed at baseline, 30 min, 2 weeks and 6 weeks after treatment. NRS for leg pain will be scored on a 0 (no pain) to 10-point (worst imaginable pain) scale with increments of 1 point. Each patient will give an average score for the previous 7 days and the highest score during those same 7 days. Leg pain from lumbar radiculopathy may vary during the week and, therefore, an average score of the past 7 days will be more representative with sufficient reliability [57, 58].
Secondary study parameters
In order to assess back pain, physical functioning, anxiety and depression-related complaints, pain coping strategies and perceived recovery secondary study outcome measures will be measured. In addition, other study parameters will be collected for development of a prediction model.
NRS for back pain will be scored at baseline, 30 min, 2 weeks and 6 weeks after treatment. NRS for back pain will be scored on a 0 (no pain) to 10-point (worst imaginable pain) scale with increments of 1 point. Each patient will give an average score for the previous 7 days and the highest score during those same 7 days. Similarly to leg pain, back pain intensity may change during the week and, therefore, an average score of the past 7 days will be more representative with sufficient reliability [57, 58].
The Oswestry Disability Index (ODI) will be recorded to assess physical functioning. The ODI will be scored on a 0 (no disability) to 50-point (worst disability possible) scale at baseline, 2 and 6 weeks after treatment and multiplied by a factor of 2 to provide a score on a 0 to 100 percentage scale.
The Hospital Anxiety and Depression Scale (HADS) will be measured to evaluate complaints of anxiety and depression at baseline, 2 weeks and 6 weeks after treatment. Both are scored with 7 items on a Likert scale that ranges from 0 to 3. For each dimension a maximum score of 21 points is possible. A score between 0 and 7 implies the absence of anxiety or depression, between 8 and 10 indicates a possible anxiety or depression disorder, and 11 or higher indicates the presence of anxiety or depression.
The Pain Coping Inventory (PCI) will be recorded to measure how the patient copes with pain symptoms. This scale assesses 6 different coping styles using 33 items which can be answered with scores from 1 (never or rarely used) to 4 (very often used) to determine how often the patient practices a certain coping strategy. The PCI will be obtained at baseline, 2 weeks and 6 weeks after treatment.
Perceived recovery will be measured to determine how the patient perceived his or her recovery. A 7-point Likert scale is used: ‘completely recovered’ = 1, ‘significantly recovered’ = 2, ‘somewhat recovered’ = 3, ‘no recovery’ = 4, ‘somewhat worsened’ = 5, ‘significantly worsened’ = 6 and ‘worse than ever’ = 7. Perceived recovery will be assessed at 2 weeks and 6 weeks after treatment.
EQ-5D-5L questionnaire: will be used for the cost-effectiveness analysis. This questionnaire consists of both the EQ-5D-5L descriptive systems which measures five dimensions of health-related Quality of Life (mobility, self-care, daily activities, pain/discomfort, and anxiety/depression with 5 severity levels) and the EQ-VAS, a visual analogue scale rating the overall current health-related Quality of Life ranging from 0 (as bad as death) to 100 (perfect health). The EQ-5D scores will be assessed at baseline and at 2, and 6 weeks follow-up.
Health care use: pain medication use, physical therapy use and number of appointments with GP (at GP’s practice, at home or via telephone/e-mail) are recorded at 2 weeks and 6 weeks after treatment. At baseline patients are asked about these variables for the 6-week period preceding study participation.
Radiological variables: lumbar level and location of disc herniation (central, paramedian, foraminal or extraforaminal) or stenosis (central, lateral recess, foraminal), type of disc degeneration (bulging, protrusion, extrusion, sequestration) and Pfirrmann classification [59], degree of stenosis (Miskin scale [60]), disc height loss (0%, 1–25%, 26–50%, 51–75%, > 75%), vertebral end plate changes (Modic scale [61]), facet degeneration (Weishaupt scale [62]), epidural lipomatosis grading (Borré scale [63]) and degree of nerve root impingement (Pfirrmann grading [64]) will be evaluated by two independent researchers, blinded to clinical data including patient outcome, on T1 and T2 weighted sagittal and transversal MRI data.
Other parameters
TEI data: data on administration of TEI is collected by the anaesthesiologist or by a nurse. This includes the date of injection, lumbar level, side and the occurrence of any complication during the procedure or within 30 min afterwards.
Data regarding the need for additional injections or surgery after TEI will be obtained from the patient’s medical record.
Complications: data will be collected on complications occurring periprocedural by the anaesthesiologist or nurse. At the fourth day after treatment the patient is requested to fill in a questionnaire about the occurrence of any complication since the procedure. Information on other adverse events that require a visit to the hospital or hospitalization will be obtained from the patient’s medical record.
Sample size calculation
The sample size was calculated for a multivariable prediction model with a binary outcome in R (version 3.6.3) [65] using the ‘pmsampsize’ package [66] to ensure ample patients for this analysis. The criteria used to calculate the sample size aim to minimize overfitting and ensure accurate estimation of pivotal variables in the model [67]. For the calculation we used a dichotomized NRS for leg pain as the binary outcome variable based on a minimal reduction of 30% in leg pain intensity compared to baseline (further elaborated in the ‘Analysis’ section). We hypothesized that 60% of the patients will be considered a ‘success’ (for definition see Primary analysis section) after two weeks based on estimations in previous literature [25]. We assumed an R2 (percentage of variation in outcome explained by the model) of 0.25, based on the strength of association of individual predictors as reported by a limited number of previous studies. Furthermore, we assumed an expected number of predictor variables of 10 and a desired level of shrinkage (measure of overfitting) at internal validation of 0.9. With an assumed margin of error of 0.05 in the estimation of the intercept a total of 369 patients is needed. A sample size of 369 patients will suffice for a range of R2 (0.22–0.73). With a loss to follow-up of 5% we aim to include a total of 388 patients. The ratio of patients with LDH and LSS to be included will not be predefined but will result from the ratio in clinical practice. We estimated that the ratio LDH: LSS patients will be between 2:1 and 3:1 based on clinical experience.
Data analysis
Demographic data will be reported using descriptive statistics. Continuous variables (age, BMI, duration of symptoms) will be presented by median and interquartile range. Categorical variables (sex, cause of symptoms, smoking status, alcohol use, side of radicular symptoms, use of pain medication, use of physical therapy, living situation and daily occupation) will be presented using numbers and percentages. For comparisons of demographic data between patients with LDH and LSS, appropriate statistical tests will be performed, depending on scale of measurement: for continuous outcomes the Mann–Whitney U test will be used, whereas for categorical data the χ2 test will be employed.
Primary analysis
The primary study outcome measure, the average score on the NRS leg pain scale, will be determined 30 min after the procedure and at the 2 and 6-week follow-up moments. Linear mixed models will be used with a radiological diagnosis (LDH or LSS) by time (as a main effect) and random effect for repeated measures within-subjects to assess differences between patient groups across all time points while correcting for potential confounders.
Furthermore, for each patient the change in NRS leg pain score at follow-up will be dichotomized using a predefined cut-off of 30% or more pain reduction compared to baseline. This is based on the minimally clinical important difference (MCID) of 30% as recommended by an international consensus group [68]. Patients with pain reduction of 30% or more compared to baseline will be considered ‘success’ and patients with less pain reduction, an increase in pain, repeat injections or surgery within the follow-up period will be considered ‘non-success’. Proportions of ‘success’ and ‘non-success’ will be compared between groups across all time-points. A generalized linear mixed model analysis for this dichotomized outcome measure at 6 weeks follow-up will be performed to predict a positive outcome after TEI. The model will include different sets of predictors using demographic, clinical and radiological variables:
Core predictors: age, sex, duration of symptoms, pre-injection NRS for leg pain, HADS and PCI scores, radiological diagnosis (LDH or single-level LSS), location of disc degeneration, degree of nerve root compression (Pfirrmann grading) and vertebral endplate changes (Modic scale).
Extended set of predictors: body mass index (BMI), injection level, injection side, pre-injection ODI score, presence of neurologic deficit (sensory and motor deficits observed during physical examination), post-procedural NRS for leg pain score at 30 min, NRS for leg pain at 2 weeks, perceived recovery at 2 weeks, type of disc degeneration, MRI signal intensity of the nerve root, lesion level and presence of transitional vertebrae
Exploration of MRI: radiological variables not included in the core or extended predictor set will be assessed as categorical variables using different scales (see Secondary study parameters section) for their association with TEI outcome
The core predictor set includes variables that were relatively consistently associated with TEI outcome based on a literature review and variables that were hypothetically auspicious.
Performance measures will include the area under the receiver operating characteristic curve (AUC) to indicate discriminative ability, and R2 for overall performance. Internal validation will be performed by bootstrap resampling with 500 iterations.
Secondary analysis
The mean NRS for back pain and ODI will be determined postprocedural and for the 2 and 6-week follow-up moments. Similarly to NRS for leg pain, linear mixed models will be used with a radiological diagnosis (LDH or LSS) by time (as a main effect) and random effect for repeated measures within-subjects to assess differences between patient groups across all time points while correcting for potential confounders. For assessment of the number of ‘success’ and ‘non-success’ for back pain (NRS) and disability (ODI) scores, a predefined cut-off of 30% or more reduction compared to baseline will be used [68].
Likert data for perceived recovery will be dichotomized (a score of 1 or 2 will be considered a ‘successful recovery’ and patients with this score, therefore, ‘success’, 3–7 will be considered ‘no successful recovery’ and patients with this score, therefore, ‘non-success’) and compared between LDH and LSS groups using Chi-square tests for the 2- and 6-week follow-up time points. A generalized linear mixed model analysis for dichotomized perceived recovery data at 6-weeks follow-up will be performed. The same sets of predictors will be used as for the prediction model based on dichotomized NRS leg pain data.
An exploratory cost-effectiveness analysis of TEI versus usual care will be performed by comparing the observed costs and effects the six weeks before treatment to the six weeks after treatment, assuming the period before treatment to be representative for usual care. The analysis will be performed from a healthcare perspective. Patients will provide data for this analysis through the EQ-5D-5L and healthcare use questionnaires at baseline, 2 and 6 weeks follow-up. Healthcare use will be valued using standard prices as published in the Dutch costing guideline [69]. Effects will be expressed in quality adjusted life years (QALYs). QALYs will be estimated by first calculating the utilities using the Dutch tariff [70]. Subsequently, the QALYs for the 6 week period before treatment will be based on the utility at baseline, and the QALYs in the 6 weeks after treatment will be obtained from utilities measured at baseline, 2 and 6 weeks follow-up using the area under the curve method.
Missing data
Patterns of missing data will be explored and visualized. Imputation will be considered using multiple imputation based on correlation with covariates and the outcomes using the ‘mice’ package in R [71].
Reporting
Study results will be reported in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) and Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis or Diagnosis (TRIPOD) guidelines [50, 72].
Study limitations
This study is limited by the absence of a formal control group. It is possible that a subgroup of patients with lumbar radicular pain can be satisfactorily treated with an inert substance or other types of treatment [27]. As such, it is possible that prognostic factors found through this study may also be associated with outcome after other treatments. Ideally, this would require a randomized controlled trial and the sample size would have to be smaller for feasibility reasons precluding the development of a prediction model for treatment outcome. The exploratory cost-effectiveness assumes the 6-week period before treatment to be representative of usual care. Additionally, the study may be limited by selection bias since most patients will be suffering from chronic symptoms. Patients with (sub)acute symptoms are usually treated conservatively. At the time they are referred to the pain clinic for TEI, symptoms will have a more chronic character. Furthermore, at baseline patients are asked about their health care utilization in the six weeks prior to participation. This may possibly lead to recall bias.
Discussion
Patients with severe lumbar radicular pain often request further treatment when conservative care with oral pain medication is inadequate. TEI is a minimally invasive treatment that could provide sufficient symptom reduction and obviate the need for surgery in part of those patients for whom conservative care have failed. To offer each patient the most appropriate treatment strategy it is necessary that clinicians can differentiate between patients whose symptoms can be sufficiently alleviated with TEI and patients that may need to be subjected to surgery nonetheless. Therefore, this study aims to explore prognostic factors and develop a prediction model for assessment of the likely outcomes with TEI.
A considerable number of studies has previously assessed prognostic factors for TEI success in patients with lumbar radicular pain. However, only few variables have been evaluated across multiple studies and for these factors the results are inconsistent. Among demographic variables, duration of symptoms has been demonstrated to be associated with pain reduction across multiple studies. A prolonged duration of symptoms was associated with worse outcome in three studies [33, 38, 43]. Yet, in the majority of studies duration of symptoms along with age, BMI, sex, injection level and side were not significantly associated with outcomes. Additionally, among clinical variables a positive Slump test was shown to be associated with patient outcome in two studies [34, 35]. Pre-injection pain and physical functioning scores, and post-injection pain scores were not associated with TEI outcome in multiple studies. Furthermore, several radiological characteristics were correlated with treatment outcome. Two studies showed an association between superior TEI outcome and LSS rather than LDH [31, 41], although three studies reported no association [33, 34, 40], and two studies reported that patients with transitional vertebrae fared worse after TEI compared to patients without this spinal deformity [44, 46]. Four studies that assessed the association between the location of disc herniation and treatment outcome showed inconsistent results [33, 34, 37, 47]. In addition, three out of four studies demonstrated better outcome after TEI in patients with a higher degree of nerve root impingement [34, 35, 47]. This appears paradoxical as it is hypothesized that in patients without high-grade nerve root compression inflammation plays a more crucial role and, expectingly, would fare better after TEI treatment. Therefore, the degree of nerve root compression will be thoroughly evaluated in the current study and included as a covariate in the prediction model. Additionally, the HADS and PCI scores will be included in the prediction model. The PCI has not been correlated with outcome after TEI before, while the HADS has been investigated before only once, but that study included patients undergoing multiple injections [73]. However, both have been demonstrated to correlate with outcome after surgery predicting residual pain and disability and a passive pain coping strategy may aid in the transition from acute to chronic pain [74–77]. Furthermore, among radiological variables the presence of Modic changes will be included as it is hypothesized that this feature represents the effects of inflammatory processes which may respond better to treatment with steroids [78–80].
The large discrepancies between findings from previous studies most likely relate to the variety of patient populations, methodological designs and treatment techniques. For this reason, it is imperative to provide a clear definition of patients with lumbar disc herniation, but particularly of stenosis patients. Patients with central disc herniation or spinal stenosis and radicular pain in both legs may require treatment with bilateral transforaminal injections. Moreover, in patients with symptomatic multi-level spinal stenosis a corticosteroid injection at a single level may not be sufficient and, therefore, outcome measures will not accurately present the effect of the injection. Hence, in the current study only patients are included with unilateral radicular pain congruent with radiological imaging and without clinically relevant multi-level degenerative changes. Although TEI may be effective for patients suffering from unilateral lumbar radicular pain due to LDH as well as single-level LSS, some variables could predict treatment outcome in one group but not the other. A number of previous studies has evaluated both aetiologies as a single population and possibly this obscured the true predictive value of certain factors. Therefore, in this study these patient groups will be assessed separately.
Additionally, variation in methodological design may have affected the reported effect sizes of TEI in previous studies. The sample sizes of some studies were small, which may have led to a lack of statistical power to draw appropriate conclusions. For this prospective study, the sample size calculation was specifically aimed at the development of a prediction model to ensure sufficient power for detection of significant differences. Moreover, treatment outcome after TEI is often presented in terms of success rates based on a predefined percentual or absolute decline in pain or disability scores. However, various definitions of success were employed which reduces comparability between studies. We will use a standardized threshold of 30% pain reduction compared to baseline as recommended by an international consensus group [68], although, statistically, we recognize a number of limitations of dichotomization, such as debate on whether to use an absolute of relative scale, the arbitrary point of dichotomization and a loss of statistical power.
Finally, treatment procedures were different among previous studies. The diversity of corticosteroids, injection dose and number of injections may have affected treatment results. In the current study, standardized doses of corticosteroids will be used according to national anesthesiologic guidelines and patients will only receive one injection. In patients receiving a second injection within six weeks after the first injection, initial treatment will be considered to have failed [48].
This observational cohort study will provide insights in the outcome after a single TEI in patients with unilateral lumbar radicular pain secondary to LDH or single-level LSS in clinical practice. In addition, this study is expected to provide data for the development of a prediction model of patient outcome after TEI. Prediction of patient outcome after TEI could be an important step towards a tailored and personalized treatment strategy for patients with lumbar radicular pain.
Ethics and dissemination
Informed consent is obtained from every patient. POTEISS is registered at ClinicalTrials.gov (NCT04540068). Results for LDH and LSS patients will be offered to peer-reviewed journals. The study is expected to be completed on 31 December 2026. Data will be available from the authors on reasonable request.
Acknowledgements
Not applicable.
Authors’ information
Not applicable.
Abbreviations
- AUC
Area under the curve
- BMI
Body mass index
- EQ-VAS
EuroQoL visual analogue scale
- GHZ
Groene Hart Hospital
- GP
General practitioner
- HADS
Hospital anxiety and depression scale
- IGJ
Inspection for Healthcare and Youth
- LDH
Lumbar disc herniation
- LSS
Single-level lumbar spinal stenosis
- LUMC
Leiden University Medical Center
- MCID
Minimally clinical important difference
- MRI
Magnetic resonance imaging
- NRS
Numerical rating scale
- ODI
Oswestry disability index
- OR
Odds ratio
- PCI
Pain coping inventory
- POTEISS
Prediction of Transforaminal Epidural Injection Success in Sciatica
- QALY
Quality-adjusted life year
- SG
Spaarne Hospital
- TEI
Transforaminal epidural injection
- VAS
Visual analogue scale
Authors’ contributions
EV wrote the manuscript and study protocol and is responsible for the design of the study, the sample size calculation, design of the analysis and organisation of the study at SG and GHZ. OH and EB contributed to TEI methodology, designed the study, revised the protocol and are responsible for organisation of the study at SG. KS contributed to TEI methodology and is responsible for organisation of the study at GHZ. ES contributed to the proposed statistical analyses. EvdA-vM contributed to the proposed exploratory cost-effectiveness analysis. CV is the principal investigator and initiator and responsible for the design of the study, design of the analysis, organisation of the study at SG and GHZ, and wrote the study protocol. All authors reviewed and approved the final version of the manuscript.
Funding
The POTEISS study did not receive any form of funding before or after commencement of the study.
Availability of data and materials
Data will be available upon reasonable request. Requests can be made with the corresponding author.
Declarations
Ethics approval and consent to participate
Approval from the Scientific Research Committee and Board of Directors from Leiden University Medical Center, the Spaarne Hospital and the Groene Hart Hospital have been granted. Informed consent will be obtained from all participants. Significant protocol modifications will have to be approved by the Committee and communicated through the study registry. All study procedures will be performed in accordance with the Declaration of Helsinki 2013 and other relevant national and international guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Konstantinou K, Dunn KM. Sciatica: review of epidemiological studies and prevalence estimates. Spine (Phila Pa 1976). 2008;33(22):2464–72. 10.1097/BRS.0b013e318183a4a2 [DOI] [PubMed] [Google Scholar]
- 2.Tarulli AW, Raynor EM. Lumbosacral radiculopathy. Neurol Clin. 2007;25(2):387–405. 10.1016/j.ncl.2007.01.008 [DOI] [PubMed] [Google Scholar]
- 3.Waldman SD. 84 - Spinal Stenosis. In: Waldman SD, editor. Atlas of Common Pain Syndromes. 4th ed. Philadelphia: Elsevier; 2019. p. 324–7. [Google Scholar]
- 4.Kobayashi S, Yoshizawa H, Yamada S. Pathology of lumbar nerve root compression Part 1: Intraradicular inflammatory changes induced by mechanical compression. J Orthop Res. 2004;22(1):170–9. 10.1016/S0736-0266(03)00131-1 [DOI] [PubMed] [Google Scholar]
- 5.Robinson JP, Brown PB, Fisk JD. Pathophysiology Of Lumbar Radiculopathies and The Pharmacology Of Epidural Corticosteroids and Local Anesthetics. Phys Med Rehabil Clin N Am. 1995;6(4):671–90. 10.1016/S1047-9651(18)30429-7 [DOI] [Google Scholar]
- 6.Stafford MA, Peng P, Hill DA. Sciatica: a review of history, epidemiology, pathogenesis, and the role of epidural steroid injection in management. Br J Anaesth. 2007;99(4):461–73. 10.1093/bja/aem238 [DOI] [PubMed] [Google Scholar]
- 7.Chiu CC, Chuang TY, Chang KH, Wu CH, Lin PW, Hsu WY. The probability of spontaneous regression of lumbar herniated disc: a systematic review. Clin Rehabil. 2015;29(2):184–95. 10.1177/0269215514540919 [DOI] [PubMed] [Google Scholar]
- 8.Kreiner DS, Hwang SW, Easa JE, Resnick DK, Baisden JL, Bess S, et al. An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J. 2014;14(1):180–91. 10.1016/j.spinee.2013.08.003 [DOI] [PubMed] [Google Scholar]
- 9.Lorio M, Kim C, Araghi A, Inzana J, Yue JJ. International Society for the Advancement of Spine Surgery Policy 2019-Surgical Treatment of Lumbar Disc Herniation with Radiculopathy. Int J Spine Surg. 2020;14(1):1–17. 10.14444/7001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kreiner DS, Shaffer WO, Baisden JL, Gilbert TJ, Summers JT, Toton JF, et al. An evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spinal stenosis (update). Spine J. 2013;13(7):734–43. 10.1016/j.spinee.2012.11.059 [DOI] [PubMed] [Google Scholar]
- 11.Anderson DB, Luca K, Jensen RK, Eyles JP, Van Gelder JM, Friedly JL, et al. A critical appraisal of clinical practice guidelines for the treatment of lumbar spinal stenosis. Spine J. 2021;21(3):455–64. 10.1016/j.spinee.2020.10.022 [DOI] [PubMed] [Google Scholar]
- 12.Katz JN, Zimmerman ZE, Mass H, Makhni MC. Diagnosis and Management of Lumbar Spinal Stenosis: A Review. JAMA. 2022;327(17):1688–99. 10.1001/jama.2022.5921 [DOI] [PubMed] [Google Scholar]
- 13.Geurts JW, Willems PC, Kallewaard JW, van Kleef M, Dirksen C. The Impact of Chronic Discogenic Low Back Pain: Costs and Patients’ Burden. Pain Res Manag. 2018;2018:4696180. 10.1155/2018/4696180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dagenais S, Caro J, Haldeman S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J. 2008;8(1):8–20. 10.1016/j.spinee.2007.10.005 [DOI] [PubMed] [Google Scholar]
- 15.Lambeek LC, van Tulder MW, Swinkels IC, Koppes LL, Anema JR, van Mechelen W. The trend in total cost of back pain in The Netherlands in the period 2002 to 2007. Spine (Phila Pa 1976). 2011;36(13):1050–8. 10.1097/BRS.0b013e3181e70488 [DOI] [PubMed] [Google Scholar]
- 16.Gore M, Sadosky A, Stacey BR, Tai KS, Leslie D. The burden of chronic low back pain: clinical comorbidities, treatment patterns, and health care costs in usual care settings. Spine (Phila Pa 1976). 2012;37(11):E668-77. 10.1097/BRS.0b013e318241e5de [DOI] [PubMed] [Google Scholar]
- 17.McLain RF, Kapural L, Mekhail NA. Epidural steroid therapy for back and leg pain: mechanisms of action and efficacy. Spine J. 2005;5(2):191–201. 10.1016/j.spinee.2004.10.046 [DOI] [PubMed] [Google Scholar]
- 18.Collighan N, Gupta S. Epidural steroids. Continuing Education in Anaesthesia Critical Care & Pain. 2009;10(1):1–5. 10.1093/bjaceaccp/mkp043 [DOI] [Google Scholar]
- 19.Johansson A, Hao J, Sjölund B. Local corticosteroid application blocks transmission in normal nociceptive C-fibres. Acta Anaesthesiol Scand. 1990;34(5):335–8. 10.1111/j.1399-6576.1990.tb03097.x [DOI] [PubMed] [Google Scholar]
- 20.Kantrowitz F, Robinson DR, McGuire MB, Levine L. Corticosteroids inhibit prostaglandin production by rheumatiod synovia. Nature. 1975;258(5537):737–9. 10.1038/258737a0 [DOI] [PubMed] [Google Scholar]
- 21.Manchikanti L, Buenaventura RM, Manchikanti KN, Ruan X, Gupta S, Smith HS, et al. Effectiveness of therapeutic lumbar transforaminal epidural steroid injections in managing lumbar spinal pain. Pain Physician. 2012;15(3):E199-245. 10.36076/ppj.2012/15/E199 [DOI] [PubMed] [Google Scholar]
- 22.Buenaventura RM, Datta S, Abdi S, Smith HS. Systematic review of therapeutic lumbar transforaminal epidural steroid injections. Pain Physician. 2009;12(1):233–51. 10.36076/ppj.2009/12/233 [DOI] [PubMed] [Google Scholar]
- 23.Benny B, Azari P. The efficacy of lumbosacral transforaminal epidural steroid injections: a comprehensive literature review. J Back Musculoskelet Rehabil. 2011;24(2):67–76. 10.3233/BMR-2011-0279 [DOI] [PubMed] [Google Scholar]
- 24.Bhatia A, Flamer D, Shah PS, Cohen SP. Transforaminal Epidural Steroid Injections for Treating Lumbosacral Radicular Pain from Herniated Intervertebral Discs: A Systematic Review and Meta-Analysis. Anesth Analg. 2016;122(3):857–70. 10.1213/ANE.0000000000001155 [DOI] [PubMed] [Google Scholar]
- 25.MacVicar J, King W, Landers MH, Bogduk N. The effectiveness of lumbar transforaminal injection of steroids: a comprehensive review with systematic analysis of the published data. Pain Med. 2013;14(1):14–28. 10.1111/j.1526-4637.2012.01508.x [DOI] [PubMed] [Google Scholar]
- 26.Oliveira CB, Maher CG, Ferreira ML, Hancock MJ, Oliveira VC, McLachlan AJ, et al. Epidural Corticosteroid Injections for Sciatica: An Abridged Cochrane Systematic Review and Meta-Analysis. Spine (Phila Pa 1976). 2020;45(21):E1405-e15. 10.1097/BRS.0000000000003651 [DOI] [PubMed] [Google Scholar]
- 27.Verheijen EJA, Bonke CA, Amorij EMJ, Vleggeert-Lankamp CLA. Epidural steroid compared to placebo injection in sciatica: a systematic review and meta-analysis. Eur Spine J. 2021;30:3255–64. 10.1007/s00586-021-06854-9 [DOI] [PubMed] [Google Scholar]
- 28.Chou R, Hashimoto R, Friedly J, Fu R, Bougatsos C, Dana T, et al. Epidural Corticosteroid Injections for Radiculopathy and Spinal Stenosis: A Systematic Review and Meta-analysis. Ann Intern Med. 2015;163(5):373–81. 10.7326/M15-0934 [DOI] [PubMed] [Google Scholar]
- 29.Manchikanti L, Knezevic NN, Boswell MV, Kaye AD, Hirsch JA. Epidural Injections for Lumbar Radiculopathy and Spinal Stenosis: A Comparative Systematic Review and Meta-Analysis. Pain Physician. 2016;19(3):E365-410. 10.36076/ppj/2016.19.E365 [DOI] [PubMed] [Google Scholar]
- 30.Manchikanti L, Knezevic E, Latchaw RE, Knezevic NN, Abdi S, Sanapati MR, et al. Comparative Systematic Review and Meta-Analysis of Cochrane Review of Epidural Injections for Lumbar Radiculopathy or Sciatica. Pain Physician. 2022;25(7):E889-e916. [PubMed] [Google Scholar]
- 31.Bang YJ, Park HJ, Sim WS, Lee DW, Lee JY. Correlation between paravertebral spread of injectate and clinical efficacy in lumbar transforaminal block. Sci Rep. 2020;10(1):11508. 10.1038/s41598-020-68474-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chang MC, Lee DG. Outcome of Transforaminal Epidural Steroid Injection According to the Severity of Lumbar Foraminal Spinal Stenosis. Pain Physician. 2018;21(1):67–72. 10.36076/ppj.1.2018.67 [DOI] [PubMed] [Google Scholar]
- 33.Cyteval C, Fescquet N, Thomas E, Decoux E, Blotman F, Taourel P. Predictive factors of efficacy of periradicular corticosteroid injections for lumbar radiculopathy. AJNR Am J Neuroradiol. 2006;27(5):978–82. [PMC free article] [PubMed] [Google Scholar]
- 34.Ekedahl H, Jönsson B, Annertz M, Frobell RB. Three week results of transforaminal epidural steroid injection in patients with chronic unilateral low back related leg pain: The relation to MRI findings and clinical features. J Back Musculoskelet Rehabil. 2016;29(4):693–702. 10.3233/BMR-160671 [DOI] [PubMed] [Google Scholar]
- 35.Ekedahl H, Jönsson B, Annertz M, Frobell RB. The 1-Year Results of Lumbar Transforaminal Epidural Steroid Injection in Patients with Chronic Unilateral Radicular Pain: The Relation to MRI Findings and Clinical Features. Am J Phys Med Rehabil. 2017;96(9):654–62. 10.1097/PHM.0000000000000730 [DOI] [PubMed] [Google Scholar]
- 36.Elsayad E, Mortada M, Elhawala TAES, Hady EAE, Hijab A. Annals of the Rheumatic Diseases. 2017;76(Suppl 2):1000. [Google Scholar]
- 37.Guclu B, Deniz L, Yuce Y, Adilay U, Aytar H, Turkoglu M, et al. Transforaminal Epidural Steroid Injection in the Treatment of Pain in Foraminal and Paramedian Lumbar Disc Herniations. Turk Neurosurg. 2020;30(3):394–9. [DOI] [PubMed] [Google Scholar]
- 38.Kaufmann TJ, Geske JR, Murthy NS, Thielen KR, Morris JM, Wald JT, et al. Clinical effectiveness of single lumbar transforaminal epidural steroid injections. Pain Med. 2013;14(8):1126–33. 10.1111/pme.12122 [DOI] [PubMed] [Google Scholar]
- 39.Kim YH, Kim HJ, Seo J, Chai JW, Song HG, Choi YH, et al. Spinal nerve signal intensity on Dixon T2-weighted water-only sequence: an important outcome predictor after lumbar transforaminal epidural injection. Eur Radiol. 2021;31(12):9459–67. 10.1007/s00330-021-08119-x [DOI] [PubMed] [Google Scholar]
- 40.Lee JW, Kim SH, Lee IS, Choi JA, Choi JY, Hong SH, et al. Therapeutic effect and outcome predictors of sciatica treated using transforaminal epidural steroid injection. AJR Am J Roentgenol. 2006;187(6):1427–31. 10.2214/AJR.05.1727 [DOI] [PubMed] [Google Scholar]
- 41.Olguner SK, Celiktas M, Oktay K, Arslan A, Bilgin E, Gezercan Y, et al. Comparison of 1-year results of single transforaminal epidural steroid injection among patients with different spinal pathologies-related radicular pain. Niger J Clin Pract. 2020;23(6):835–41. 10.4103/njcp.njcp_24_19 [DOI] [PubMed] [Google Scholar]
- 42.Ploumis A, Christodoulou P, Wood KB, Varvarousis D, Sarni JL, Beris A. Caudal vs transforaminal epidural steroid injections as short-term (6 months) pain relief in lumbar spinal stenosis patients with sciatica. Pain Med. 2014;15(3):379–85. 10.1111/pme.12318 [DOI] [PubMed] [Google Scholar]
- 43.Sariyildiz MA, Batmaz İ, Yazmalar L, Güneş M, Turan Y. The effectiveness of transforaminal epidural steroid injections on radicular pain, functionality, psychological status and sleep quality in patients with lumbar disc herniation. J Back Musculoskelet Rehabil. 2017;30(2):265–70. 10.3233/BMR-150438 [DOI] [PubMed] [Google Scholar]
- 44.Sencan S, Azizov S, Celenlioglu AE, Bilim S, Gunduz OH. Effect of sacralization on the success of lumbar transforaminal epidural steroid injection treatment: prospective clinical trial. Skeletal Radiol. 2023;52(10):1949–57. 10.1007/s00256-022-04089-3 [DOI] [PubMed] [Google Scholar]
- 45.Şencan S, Çelenlioğlu AE, Asadov R, Gündüz OH. Predictive factors for treatment success of transforaminal epidural steroid injection in lumbar disc herniation-induced sciatica. Turk J Med Sci. 2020;50(1):126–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Son KM, Lee SM, Lee GW, Ahn MH, Son JH. The Impact of Lumbosacral Transitional Vertebrae on Therapeutic Outcomes of Transforaminal Epidural Injection in Patients with Lumbar Disc Herniation. Pain Pract. 2016;16(6):688–95. 10.1111/papr.12315 [DOI] [PubMed] [Google Scholar]
- 47.Tecer D, Adiguzel E, Tan AK, Taskaynatan MA. Role of Magnetic Resonance Imaging in Ascertaining the Success of Transforaminal Epidural Steroid Injection for Lumbar Radicular Pain. Pain Med. 2017;18(4):645–50. [DOI] [PubMed] [Google Scholar]
- 48.Johansson AC, Linton SJ, Rosenblad A, Bergkvist L, Nilsson O. A prospective study of cognitive behavioural factors as predictors of pain, disability and quality of life one year after lumbar disc surgery. Disabil Rehabil. 2010;32(7):521–9. 10.3109/09638280903177243 [DOI] [PubMed] [Google Scholar]
- 49.Ionescu D, Iacob CI, Brehar FM, Avram E. The role of catastrophizing and basic psychological needs satisfaction on health-related quality of life and pain in patients with lumbar disc herniation. Front Psychol. 2023;14:1147254. 10.3389/fpsyg.2023.1147254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Collins GS, Reitsma JB, Altman DG, Moons KG. Transparent Reporting of a multivariable prediction model for Individual Prognosis or Diagnosis (TRIPOD): the TRIPOD statement. Ann Intern Med. 2015;162(1):55–63. 10.7326/M14-0697 [DOI] [PubMed] [Google Scholar]
- 51.Hingorani AD, Windt DA, Riley RD, Abrams K, Moons KG, Steyerberg EW, et al. Prognosis research strategy (PROGRESS) 4: stratified medicine research. BMJ. 2013;346: e5793. 10.1136/bmj.e5793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.el Barzouhi A, Vleggeert-Lankamp CL, Lycklama à Nijeholt GJ, Van der Kallen BF, van den Hout WB, Jacobs WC, et al. Magnetic resonance imaging in follow-up assessment of sciatica. N Engl J Med. 2013;368(11):999–1007. 10.1056/NEJMoa1209250 [DOI] [PubMed] [Google Scholar]
- 53.Janardhana AP, Rajagopal, Rao S, Kamath A. Correlation between clinical features and magnetic resonance imaging findings in lumbar disc prolapse. Indian J Orthop. 2010;44(3):263–9. 10.4103/0019-5413.65148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.van Rijn JC, Klemetso N, Reitsma JB, Majoie CB, Hulsmans FJ, Peul WC, et al. Symptomatic and asymptomatic abnormalities in patients with lumbosacral radicular syndrome: Clinical examination compared with MRI. Clin Neurol Neurosurg. 2006;108(6):553–7. 10.1016/j.clineuro.2005.10.003 [DOI] [PubMed] [Google Scholar]
- 55.Mandell JC, Czuczman GJ, Gaviola GC, Ghazikhanian V, Cho CH. The Lumbar Neural Foramen and Transforaminal Epidural Steroid Injections: An Anatomic Review With Key Safety Considerations in Planning the Percutaneous Approach. AJR Am J Roentgenol. 2017;209(1):W26-w35. 10.2214/AJR.16.17471 [DOI] [PubMed] [Google Scholar]
- 56.Dietrich TJ, Sutter R, Froehlich JM, Pfirrmann CW. Particulate versus non-particulate steroids for lumbar transforaminal or interlaminar epidural steroid injections: an update. Skeletal Radiol. 2015;44(2):149–55. 10.1007/s00256-014-2048-6 [DOI] [PubMed] [Google Scholar]
- 57.Bolton JE, Humphreys BK, van Hedel HJ. Validity of weekly recall ratings of average pain intensity in neck pain patients. J Manipulative Physiol Ther. 2010;33(8):612–7. 10.1016/j.jmpt.2010.08.009 [DOI] [PubMed] [Google Scholar]
- 58.Jamison RN, Raymond SA, Slawsby EA, McHugo GJ, Baird JC. Pain assessment in patients with low back pain: comparison of weekly recall and momentary electronic data. J Pain. 2006;7(3):192–9. 10.1016/j.jpain.2005.10.006 [DOI] [PubMed] [Google Scholar]
- 59.Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976). 2001;26(17):1873–8. 10.1097/00007632-200109010-00011 [DOI] [PubMed] [Google Scholar]
- 60.Miskin N, Isaac Z, Lu Y, Makhni MC, Sarno DL, Smith TR, et al. Simplified Universal Grading of Lumbar Spine MRI Degenerative Findings: Inter-Reader Agreement of Non-Radiologist Spine Experts. Pain Med. 2021;22(7):1485–95. 10.1093/pm/pnab098 [DOI] [PubMed] [Google Scholar]
- 61.Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR. Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology. 1988;166(1 Pt 1):193–9. 10.1148/radiology.166.1.3336678 [DOI] [PubMed] [Google Scholar]
- 62.Weishaupt D, Zanetti M, Boos N, Hodler J. MR imaging and CT in osteoarthritis of the lumbar facet joints. Skeletal Radiol. 1999;28(4):215–9. 10.1007/s002560050503 [DOI] [PubMed] [Google Scholar]
- 63.Borré DG, Borré GE, Aude F, Palmieri GN. Lumbosacral epidural lipomatosis: MRI grading. Eur Radiol. 2003;13(7):1709–21. 10.1007/s00330-002-1716-4 [DOI] [PubMed] [Google Scholar]
- 64.Pfirrmann CW, Dora C, Schmid MR, Zanetti M, Hodler J, Boos N. MR image-based grading of lumbar nerve root compromise due to disk herniation: reliability study with surgical correlation. Radiology. 2004;230(2):583–8. 10.1148/radiol.2302021289 [DOI] [PubMed] [Google Scholar]
- 65.R Core Team. R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2021. https://www.R-project.org/.
- 66.Ensor JR. Pmsampsize: Sample Size for Development of a Prediction Model. R package version 1.1.0. 2020. https://cran.r-project.org/package=pmsampsize.
- 67.Riley RD, Snell KIE, Ensor J, Burke DL, Harrell FE Jr, Moons KGM, et al. Minimum sample size for developing a multivariable prediction model: Part I - Continuous outcomes. Stat Med. 2019;38(7):1262–75. 10.1002/sim.7993 [DOI] [PubMed] [Google Scholar]
- 68.Ostelo RW, Deyo RA, Stratford P, Waddell G, Croft P, Von Korff M, et al. Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine (Phila Pa 1976). 2008;33(1):90–4. 10.1097/BRS.0b013e31815e3a10 [DOI] [PubMed] [Google Scholar]
- 69.Kanters TA, Bouwmans CAM, van der Linden N, Tan SS, Hakkaart-van RL. Update of the Dutch manual for costing studies in health care. PLoS ONE. 2017;12(11):e0187477. 10.1371/journal.pone.0187477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Versteegh MM, Vermeulen KM, Evers SMAA, de Wit GA, Prenger R, Stolk EA. Dutch Tariff for the Five-Level Version of EQ-5D. Value Health. 2016;19(4):343–52. 10.1016/j.jval.2016.01.003 [DOI] [PubMed] [Google Scholar]
- 71.van Buuren S, Groothuis-Oudshoorn K. mice: Multivariate Imputation by Chained Equations in R. J Stat Softw. 2011;45(3):1–67. 10.18637/jss.v045.i03 [DOI] [Google Scholar]
- 72.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–9. 10.1016/j.jclinepi.2007.11.008 [DOI] [PubMed] [Google Scholar]
- 73.Bahar-Ozdemir Y, Sencan S, Ercalik T, Kokar S, Gunduz OH. The Effect of Pre-Treatment Depression, Anxiety and Somatization Levels on Transforaminal Epidural Steroid Injection: A Prospective Observational Study. Pain Physician. 2020;23(3):E273–80. [PubMed] [Google Scholar]
- 74.McGreevy K, Bottros MM, Raja SN. Preventing Chronic Pain following Acute Pain: Risk Factors, Preventive Strategies, and their Efficacy. Eur J Pain Suppl. 2011;5(2):365–72. 10.1016/j.eujps.2011.08.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Leeuw M, Goossens ME, Linton SJ, Crombez G, Boersma K, Vlaeyen JW. The fear-avoidance model of musculoskeletal pain: current state of scientific evidence. J Behav Med. 2007;30(1):77–94. 10.1007/s10865-006-9085-0 [DOI] [PubMed] [Google Scholar]
- 76.Linton SJ. Early identification and intervention in the prevention of musculoskeletal pain. Am J Ind Med. 2002;41(5):433–42. 10.1002/ajim.10052 [DOI] [PubMed] [Google Scholar]
- 77.den Boer JJ, Oostendorp RA, Beems T, Munneke M, Evers AW. Continued disability and pain after lumbar disc surgery: the role of cognitive-behavioral factors. Pain. 2006;123(1–2):45–52. 10.1016/j.pain.2006.02.008 [DOI] [PubMed] [Google Scholar]
- 78.Dudli S, Fields AJ, Samartzis D, Karppinen J, Lotz JC. Pathobiology of Modic changes. Eur Spine J. 2016;25(11):3723–34. 10.1007/s00586-016-4459-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Crockett MT, Kelly BS, van Baarsel S, Kavanagh EC. Modic Type 1 Vertebral Endplate Changes: Injury, Inflammation, or Infection? AJR Am J Roentgenol. 2017;209(1):167–70. 10.2214/AJR.16.17403 [DOI] [PubMed] [Google Scholar]
- 80.Peterson CK, Pfirrmann CW, Hodler J. Are Modic changes related to outcomes in lumbar disc herniation patients treated with imaging-guided lumbar nerve root blocks? Eur J Radiol. 2014;83(10):1786–92. 10.1016/j.ejrad.2014.06.008 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be available upon reasonable request. Requests can be made with the corresponding author.