Abstract
Background
International Medical Graduates (IMG) are an essential part of the international physician workforce, and exploring the predictors of success and failure for IMGs could help inform international and national physician labour workforce selection and planning. The objective of this study was to explore predictors for success for selection of IMGs into high stakes postgraduate training positions and practice and not necessarily for informing IMGs.
Methods
We searched 11 databases, including Medline, Embase and LILACS, from inception to February 2022 for studies that explored the predictors of success and failure in IMGs. We reported baseline probability, effect size in relative risk (RR), odds ratio (OR) or hazard ratio (HR) and absolute probability change for success and failure across six groups of outcomes, including success in qualifying exams, or certificate exams, successful matching into residency, retention in practice, disciplinary actions, and outcomes of IMG clinical practice.
Results
Twenty-five studies (375,549 participants) reported the association of 93 predictors of success and failure for IMGs. Female sex, English fluency, graduation recency, higher scores in USMLE step 2 and participation in a skill assessment program were associated with success in qualifying exams. Female sex, English fluency, previous internship and results of qualifying exams were associated with success in certification exams. Retention to work in Canada was associated with several factors, including male sex, graduating within the past five years, and completing residency over fellowships. In the UK, IMGs and candidates who attempted PLAB part 1, ≥ 4 times vs. first attempters, and candidates who attempted PLAB part 2, ≥ 3 times vs. first attempters were more likely to be censured in future practice. Patients treated by IMGs had significantly lower mortalities than those treated by US graduates, and patients of IMGs had lower mortalities [OR: 0.82 (95% CI: 0.62, 0.99)] than patients of US citizens who trained abroad.
Conclusions
This study informed factors associated with the success and failure of IMGs and is the first systematic review on this topic, which can inform IMG selection and future studies.
Systematic review registration
PROSPERO: CRD42021252678.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12909-024-05837-w.
Keywords: International medical graduates, International trained physicians, Predictors
Background
An increasing number of International Medical Graduates (IMGs), defined as physicians who graduated from medical schools outside the countries where they intend to practice, are migrating to economically advanced countries. IMGs are a vital part of the international physician workforce, and many countries greatly depend on this IMG physician workforce. In the UK in 2018, around 33% of registered doctors graduated outside the UK [1]. IMGs represent 24% of Canadian physicians [2] and 25% in the United States in 2010 [3] and only 47% of medical practitioners in Australia were born in Australia [4]. Employing IMGs comes at tremendous cost savings to the accepting country. In 2013, Australia had saved approximately US$1.7 billion in medical education costs through the arrival of foreign-born medical practitioners over the preceding five years [4].
Competition for IMGs applying to IMG postgraduate training positions is fierce in Western countries, and lawsuits initiated by unsuccessful IMGs have emerged to challenge the system, which have led to the need to be able to legally defend selection decisions [5]. This raises the need for an evidence-based, defensible, and transparent system for selecting and recruiting IMGs to postgraduate training positions. Moreover, postgraduate training of an IMG in their new country is resource intensive and expensive (£485,380 per general practitioner trainee in the UK) [1]. Furthermore, there has been evidence from several countries, including the UK [6], Australia [7–11] and Canada [12, 13], that certain IMGs are more likely to have complaints and suspensions, censure and lawsuits against them. Therefore, it is crucial to identify predictors of success in training, certification exams, and professional practice, as well as the risk of disciplinary actions, during the selection process [14–21]. The leading author (IS) of this review conducted two observational studies [14, 15] to investigate the determinants of success among IMGs in Canada. This exposed the need for an international systematic review to comprehensively understand the factors associated with success.
The main objective of this systematic review is to investigate the predictors of success and failure of IMGs in postgraduate training or practice in their new country.
Methods
We followed the Synthesis without meta-analysis (SWiM) in systematic review reporting guideline [22] and registered our review (PROSPERO Identifier: CRD42021252678). This systematic review did not require ethics approval.
Data sources and searches
An academic librarian (NW) developed and implemented the search strategy by using controlled vocabulary and keywords representing the concepts [International medical graduates], [success and failure] and [predictors and risk factors] on Medline (OvidSP)[1946-present], Cochrane Central Register of Controlled Trials (Cochrane Library, Wiley)[Issue 1 of 12, January 2022], BIOSIS Citation Index (Web of Science)[1969-present], CINAHL (EBSCOHost), Embase (OvidSP), ERIC (EBSCOHost), Global Health (OvidSP), LILACS (https://pesquisa.bvsalud.org/portal/), Science Citation Index (Web of Science)[1900-present], PsycINFO (OvidSP)[1806-present] and Scielo (https://scielo.org/en) from inception to February 28, 2022, without any language or date restriction (eTable 1). We reviewed reference lists of eligible studies and related reviews for additional potentially eligible articles. We have set up an automatic alert for our search strategies to inform us of recent publications.
Eligibility criteria and study selection
We included prospective and retrospective observational studies in any language that: (1) enrolled IMGs who are defined to be physicians working or in postgraduate training in a country other than their country of training, and (2) investigated predictors for success or failure in IMGs during training or practice, utilizing adjusted analyses—comprising any type of regression or the use of ANCOVA or MANCOVA—to demonstrate the association between predictors and outcomes.
Pairs of reviewers independently screened titles and abstracts identified through our literature searches for relevance to the research question. Before the formal screening process, we performed multiple rounds of screening to achieve agreement. For each round, 50 titles and abstracts and 10 full texts were used for pilot screening. Pairs from the same set of reviewers independently assessed the full texts of all potentially eligible articles based on the predetermined selection criteria. All conflicts were resolved through discussion to reach consensus, and if needed, a senior reviewer (IS) was involved. We used online Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia, available at www.covidence.org, to facilitate literature screening.
Outcomes
After data extraction, we decided to enhance our reporting by grouping outcomes into six categories. We defined success as a binary outcome, where a candidate passes a qualifying or certificate exam, matches for residency, and continues to practice in the new country. Conversely, failure was defined as not meeting any of these criteria. Similarly, achieving a higher score on a scale was considered a success for continuous outcomes. Additionally, we classified lawsuits, complaints, suspensions, and censure as types of failure. Regarding clinical outcomes, higher mortality or increased rates of opioid prescriptions were also classified as failures.This refinement will provide a clearer and more organized presentation of the results: (1) success in qualifying exams, e.g. Medical Council of Canada Qualifying Examination (MCCQE); Educational Commission for Foreign Medical Graduates (ECFMG) clinical skill assessment and integrated clinical encounter exams in USA - United States Medical Licensing Examination parts (USMLE); (2) success in matching for residency; (3) success in certification exams for getting licensed and practice medicine e.g., Certification examinations of College of Family Physicians of Canada (CFPC), Royal College of Physicians and Surgeons of Canada (RCPSC), American board of family medicine (ABFM) certificate; (4) retention of IMGs to practice in the new country where the IMG had completed additional postgraduate training, (5) being disciplined or receiving complaints, and (6) clinical outcomes of patients managed by IMGs, e.g. mortality of patients treated by IMGs vs. local medical graduates or quality of practice issues identified as per best practice guidelines (e.g. prescription considerations such as opioid prescription).
Data extraction
We used a modified checklist for critical appraisal and data extraction for systematic reviews of prediction modeling studies (CHARMS-PF) for predictors [23]. The CHARMS checklist provided detailed guidance about the key items across 11 domains grouped into nine main categories: (1) study design, (2) study population features, (3) outcome measurement methods and their validity, (4) predictors and adjusted measures of association with outcomes, (5) sample size, (6) missing data, (7) analysis, (8) results, (9) interpretation and discussion. (eTable 2).
Pairs of reviewers extracted data independently. Reviewers resolved disagreements by discussion or by consultation with an adjudicator when required. When a study reported more than one regression model, we used the model with the largest number of predictors.
Risk of bias assessment
The same pairs of reviewers assessed the risk of bias (RoB) independently and in duplicate using the QUIPS-PF (Quality in prognostic factor studies) tool. We used the following criteria to assess the risk of bias among observational studies (eFigure 1): (1) representativeness of the study population; (2) proportion of missing data (≥ 20% was considered high risk of bias); (3) predictor measurement; (4) validity of outcome assessment; (5) statistical analysis and reporting; (6) whether predictive models optimally adjusted by included, at minimum, age and sex [24].
Data synthesis
Due to the diverse methods used in assessing success and failure, conducting a meta-analysis was not feasible. Instead, we organized studies based on outcomes, when available, reported the baseline probability for each outcome and a measure of association [relative risk (RR), odds ratio (OR), or hazard ratio (HR)], along with the corresponding 95% confidence interval and absolute probability change for each predictor.
Results
Study selection
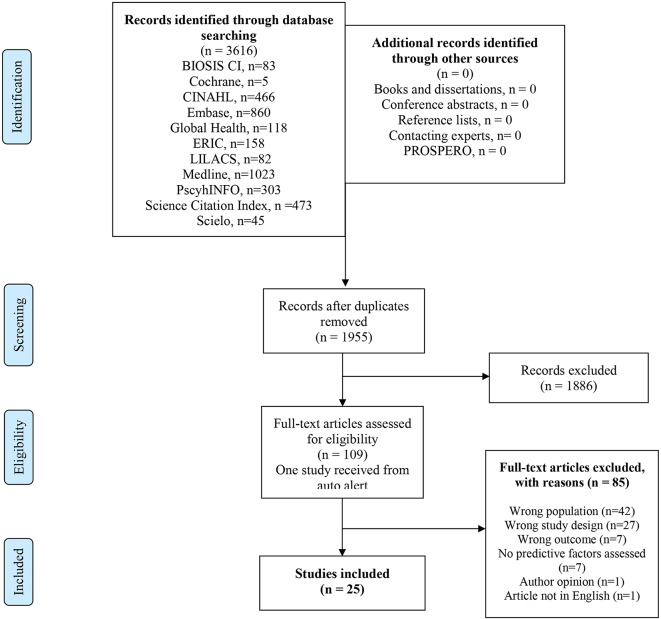
We identified 1,955 unique records, of which a total of 25 studies met our eligibility criteria (Fig. 1). We received one citation [25] from the automatic alert system, designed to notify us of newly published references. We included three studies [12, 26, 27] that reported predictors of success and failure; however, they did not use adjusted analysis. Two eligible studies [14, 15] had population overlap, and we reported the results for predictors supported with larger populations.
Fig. 1.
Flow diagram of study selection
Study characteristics
We included 23 retrospective observational studies, one prospective cohort study [28], and one case-control study for a total of 25 studies included [29] Seven studies were from Canada [12, 14, 15, 27, 30–32], eight from the USA [25, 26, 29, 33–37], seven from the United Kingdom [1, 38–43], and one each from Australia [7], Sweden [28] and Finland [44]. Four were single-institution studies. Wherever funding was acknowledged, it was from an official educational grant or government grant (Table 1).
Table 1.
Baseline characteristics of included studies
| No | Author/ Year | N | Country | Age (median, IQR) | Female Sex% | Outcome |
|---|---|---|---|---|---|---|
| 1 | Kanna, 2009 [1] | 51 | USA | 35 (33, 37) | 43% | (a) annual aggregate graduate PGY-level specific competency-based evaluation (CBE) score above versus below the median score within our program (scoring scale of 1–10), (b) US graduate PGY-level specific resident in-training exam (ITE) score higher versus lower than the median score, and (c) those who succeeded to secure a fellowship within the study period. |
| 2 | Driver, 2014 [2] | 170 | USA | Not reported | Not reported | Successful matching into a US ophthalmology residency) from 2003 to 2008 |
| 3 | Matthews, 2017 [3] | 876 | Canada |
21.6% under 30 78.4% over 30 years |
58.3% | Retention: IMGs who worked and did not work in Canada following family medicine PGME training 2005-9 or specialist PGME training 2005–2006 |
| 4 | Mathews, 2017 [4] | 1214 | Canada |
19.5% Under 30 80.5% over 30 |
55.4% |
Retention: IMG family medicine residents to work in Canada within 2 years after completing GME training IMG residents who passed the MCCQE2 and who passed and obtained a specialty designation among IMGs who entered a family medicine residency program between 2005–2009 |
| 5 | Grierson, 2017 [5] | 900 | Canada | Not reported | Not reported |
Success on Simulated Office orals component of CFPC exam Success on SAMP of CFPC Success on composite certification in College of Family Physicians of Canada examination Success on Royal College of Physicians and Surgeons of Canada certification examination |
| 6 | Tiffin, 2017 [6] | 27,330 | UK | 31 years | 40% | Fitness to practice events (referral or censure) in IMGs registered in UK with GMC (General Medical Council) |
| 7 | Tiffin, 2014 [7] |
53,436 (42017 UK graduates, 11419 IMGs) |
UK |
31.61 UK graduates, 35.89 IMGs |
56% UK graduates, 40% IMGs | Annual review of competence progression (ARCP) performance of doctors who passed professional and Linguistic Assessments Boards (PLAB) tests compared with UK medical graduates |
| 8 | Patterson, 2018 [1] | 1874 | UK | 34 years old | 49.6% |
IMGs who applied for UK GP specialty training 2008–2012 Outcome = performance on the Clinical Skills Assessment (CSA) OSCE component of the MRCGP |
| 9 | Nayer, 2013 [9] | 1382 | Canada |
(grouped into 5-year intervals) Earlier than 1955 = 2.0% 1955–1959 = 8.4% 1960–1964 = 13.2% 1965–1969 = 21.5% 1970–1974 = 24.7% 1975–1979 = 23.1% Later than 1979 = 6.9% |
Not reported | Predictors of CEHPEA CE1 OSCE results Canada |
| 10 | Elkin, 2012 [10] | 39,155 | Australia | Not reported | 35% | Complaints and adverse disciplinary findings against IMGs in Victoria and Western Australia |
| 11 | Alam, 2017 [11] | 264 IMGs and 530 CMGs | Canada | Not reported | 8.7% IMGs, 8.1% CMGs | IMGs disciplined by professional regulatory colleges in Canada 2000–2015 |
| 12 | Haukilahti, 2012 [44] | 746 | Finland | 36 (35, 64) | 58% | Factors associated with good outcome in licensing exams 1994–2009 in Finland for doctors who completed their medical qualifications outside the EEA Criterion for good outcome: all 3 parts of the examination passed on first attempt |
| 13 | Schabort, 2014 [13] | 154 | Canada | Mean not reported | Not reported |
Performance on Canadian Royal College of Physicians and Surgeons of Canada (RCPSC) Certification exam success at first try Performance on CFPC College of Family Physicians) certification examination |
| 14 | Mehdizadeh, 2017 [14] | 1111 | UK | Not reported | Not reported | Performance assessments performed on IMGs in UK by country of qualification as compared to UK graduates controlled for year (UK graduates OR 1) |
| 15 | Sturesson, 2020 [15] | 564 | Sweden | 37 | 51% | Migrant physicians passing the Swedish certification exam for 7 year period categorized by age under and above 45 at completion of exam as well as whether the candidate had participated in a complementary program. |
| 16 | Peterson, 2020 [17] | 6347 | USA | 35.9 | 50.8% | American Board of Family Medicine Certification Examination Score and Failure to obtain certification 2008–2012 |
| 17 | Van Zanten, 2003 [18] | 11,690 | USA | 30.5 | 42% |
ECFMG Clinical Skills Assessment (CSA). Component Integrated Clinical Encounter (ICE) and Doctor-Patient Communication (COM) Passing ICE Passing COM |
| 18 | Norcini, 2014 [19] | 2525 | USA | Not reported | Not reported | Mortality of patient treated by IMG 2003–2009 in Pennsylvania US where principal diagnosis was acute myocardial infarction |
| 19 | Shaw, 2014 [20] | 116 | UK | Not reported | 56.8% | Critical skills assessment (CSA) in general practice specialty training in UK Aug -Dec 2012 |
| 20 | Menzies, 2015 [42] | 2056 | UK | 29 | 72.5% | UK Royal College of Paediatrics and Child Health (MRCPCH) part 1B pass 2007–2011 |
| 21 | Bessant, 2006 [22] | 483 | UK | 30.6 | 42.4% | Independently influencing success in subsequent PACES (Practical Assessment of clinical examination skills) MRCP (UK) Success |
| 22 | Norcini, 2010 [23] | 1497 | USA | Not reported | Not reported | In-hospital mortality of patients treated by IMGs compared to US medical graduates |
| 23 | Tamblyn, 2021 [24] | 7373 | Canada | 43.7 | 39% | Opioid prescribing for chronic pain as indicator for fitness to practice |
| 24 | Khalafallah, 2021 [25] | 243 IMGs compared to 2506 US graduates | USA | Not reported | 9.4% | Securing academic neurosurgical position post residency |
| 25 | Norcini, 2023 [26] |
196,881 hospitalizations, 1,765 clinicians |
USA | Female clinicians 41% | In-Hospital Mortality |
Risk of bias
Eleven of twenty-five (44%) studies were rated as having a low risk of bias. Two (8%) were rated as having a moderate risk of bias. Twelve (48%) were rated as having a high risk of bias. Five studies did not enroll a representative study population, six studies reported high losses to follow-up, seven studies did not measure predictors, five studies did not use valid tools to measure outcomes, the regression model in nine studies did not adjust for one of age and sex and the regression model did not adjust for all predictors (eTable 3).
Predictors and outcomes
Twenty-five studies (375,549 participants) reported the association between 93 independent variables with six outcome groups in IMGs. To optimize the reporting and interpretation of the results of this systematic review, the authors identified six groups of outcomes based on their similarity.
Success in qualifying exams
We identified two studies [30, 34] that explored predictors of success in qualifying exams in the USA and Canada. One study [34] showed that female candidates were more likely to pass the Integrated Clinical Encounter (ICE) [OR: 2.64 (95%CI: 2.31, 3.03)] and Doctor-Patient Communication (COM) components of the clinical skills assessment (CSA) [OR: 2 (95%CI: 1.71, 2.39)] for ECFMG certification.
Mathews (2017) [30] demonstrated that sex was not associated with success in the MCCQE2 in Canada (Table 2) (eFigure 2). Van Zanten (2003) [33] showed that candidates with higher TOEFL scores were more likely to pass the ICE and COM. Additionally, native English language-speaking candidates had a very high likelihood of passing COM [OR: 6.85 (95%CI: 3.81, 12.29)].
Table 2.
Predictors of success and failure in certification exams
| Author/ year/ sample size/country/RoB | Predictor | OR (95% CI) | P Value | Outcome | Baseline risk for outcome | Predictor/absolute success or failure change |
|---|---|---|---|---|---|---|
| Age | ||||||
|
Grierson, 2017 [15] N = 469 Canada |
Age 10 years decrement | 1.68 (1.15, 2.44) | 0.007 | Success on Simulated Office Orals component of the Certification in The College of Family Physicians examination | 91.5% | Each 10 years decrement in age increase success rate by 3.3% (95%CI: 1–4.8% more) |
|
Grierson, 2017 [15] N = 469 Canada |
1.86 (1.33, 2.60) | 0.001 | Success on Short Answer Management Problems component of the Certification in The College of Family Physicians examination | 85.5% | Each 10 years decrement in age increase success rate by 6.1% (95%CI: 3.2–8.4% more) | |
|
Grierson, 2017 [15] N = 469 Canada |
1.76 (1.32, 2.33) | 0.001 | Success on composite Certification in The College of Family Physicians examination | 79.3% | Each 10 years decrement in age increase success rate by 7.8% (95%CI: 4.2–10.6% more) | |
|
Grierson, 2017 [15] N = 431 Canada |
1.54 (1.08, 2.18) | 0.02 | Success on Royal College of Physicians and Surgeons of Canada certification examination | 84.4% | Each 10 years decrement in age increase success rate by 4.9% (95%CI: 1–7.8% more) | |
|
Menzies, 2015 [42] N = 2,056 UK |
Age 10 years decrement | 0.71 (0.53, 0.97) | 0.029 | Membership of the Royal College of Paediatrics and Child Health (MRCPCH) part 1B examination outcome | 41% | Each 10 years decrement in age decrease success rate by 8% (95%CI: 0.7% less to 14.1% less) |
|
Tiffin, 2014 [39] N = 52,871 doctors UK |
Age 10 years decrement | 1 (0.86, 1.16) | 0.39 |
Less satisfactory Annual Review of Competence Progression (ARCP) outcome for international medical graduates (IMG) versus UK graduates (Ordinal outcome) |
NR | |
|
Sturesson, 2020 [28] N = 564, Sweden |
NR | NR | Failing Licensing Exam | Older candidates were more likely to fail | ||
|
Haukilahti, 2012 [44] N = 383 Finland |
Age < 35 vs. ≥ 35 | 1.02 (0.44, 2.38) | 0.96 | Success in licensing examinations of IMG doctors in Finland | 51.3% | IMG doctors < 35 vs. ≥ 35 was 0.5% more (20% less to 20.2% more) likely to pass the licensing exams |
| Sex: Female vs. Male | ||||||
|
Grierson, 2017 [15] N = 469 Canada |
Female vs. Male | 1.96 (1.15, 3.33) | < 0.01 | Success on Short Answer Management Problems component of the Certification in The College of Family Physicians examination | 85.5% | Female were more likely to be successful 6.5% more (95%CI: 1.7 to 9.7% more) |
|
Menzies, 2015 [42] N = 2,056 UK |
Female vs. Male | 0.95 (0.77, 1.18) | 0.63 | Membership of the Royal College of Paediatrics and Child Health (MRCPCH) part 1B examination outcome | 41% | Female were less likely to be successful 1.2% less (95%CI: 6.1 less to 4% more) |
|
Haukilahti, 2012 [44] N = 383, Finland |
Female vs. Male | 1.80 (1.02, 3.16) | 0.041 | Success in licensing examinations of IMG doctors in Finland | 51.3% | Female were more likely to pass the exam 14.2% more (95%CI: 0.5–25.6% more) |
|
Shaw, 2014 [41] N = 116 UK |
Female vs. Male | 3.33 (1.01, 11.11) | 0.048 |
Passing Clinical skill assessment In trainees who completed ST3 year General Practice Speciality in UK |
68% | Female were more likely to pass the exam 19.6% more (95%CI: 0.2–28% more) |
|
Tiffin, 2014 [39] N = 52,871 doctors UK |
Female vs. Male | 1.29 (1.23, 1.34) | NR | Obtaining more satisfactory Annual Review of Competence Progression (ARCP) outcome (outcome is ordinary variable) to assess all doctors in UK postgraduate training | Females were more likely to obtain more satisfactory Annual Review of Competence Progression (ARCP) | |
|
Mathews, 2017 [31] N = 876 Canada |
Sex (Female vs. Male) | 1.67 (1.20, 2.33) | 0.002 | Obtain Speciality Designation in family medicine |
Female IMG were more likely obtain speciality designation. 8% (95%CI: 3%,11%) |
|
| Fluency in English | ||||||
|
Grierson, 2017 [15] N = 469 Canada |
Fluency in English | 2.14 (1.25, 3.65) | < 0.01 | Success on Short Answer Management Problems component of the Certification in The College of Family Physicians examination | 85.5% | Fluent candidates were 7.16% (95%CI: 2.55–10.06%) more likely to be successful. |
|
Grierson, 2017 [15] N = 469, Canada |
Fluency in English | 1.89 (1.18, 3.0) | 0.008 | Success on composite Certification in The College of Family Physicians examination | 79.3% |
Fluent candidates were more likely to be successful. 8.6% more (95%CI: 2.6%, 12.7% more) |
|
Grierson, 2017 [15] N = 431 Canada |
Fluency in English | 1.87 (1.04, 3.38) | 0.04 | Success on Royal College of Physicians and Surgeons of Canada certification examination | 84.4% |
Fluent candidates were more likely to be successful. 6.6% more (95%CI: 0.5%, 10.4% more) |
|
Patterson, 2018 [1] N = 1,874 UK |
English fluency 1 score IELTS test |
Coefficient (95%CI) Linear regression 4.21 (3.18, 5.25) | < 0.001 | Clinical Skills Assessment (CSA) component of Membership of the Royal College of General Practitioners (MRCGP) | One score increase in IELTS (ranging 1–9) was associated with 4 (95%CI: 3–5) score increase in CSA | |
| Race and Ethnicity | ||||||
|
Bessant, 2006 [43] N = 483 UK |
White ethnic origin | 2.04 (1.42, 2.94) | 0.023 | success of candidates taking a revision course in preparation for the MRCP (UK) PACES (practical assessment of clinical examination skills) examination. | 45.3% |
White ethnicity graduates were more likely pass PACES 17.5% (95%CI: 8.7%, 25.6%) |
|
Tiffin, 2014 [39] N = 52,871 doctors UK |
White vs. Non-white ethnicity | 1.39 (0.94, 2.04) | NR | Obtaining less satisfactory Annual Review of Competence Progression (ARCP) outcome (outcome is ordinary variable) to assess all doctors in UK postgraduate training | NA (outcome is an ordinary variable) | |
| Nationality | ||||||
|
Haukilahti, 2012 [44] N = 383, Finland |
Nationality Other vs. Russian | 1.35 (0.81, 2.27) | 0.247 | Success in licensing examinations of IMG doctors in Finland | 51.3% | 7% (95%CI: -5%,19%) |
|
Schabort, 2014 [14] CFPC, N = 69; RCPSC, N = 85 Canada |
Country of birth (Other vs. Canada) | 1.54 (0.49, 4.87) | 0.46 | Success in Certification examination–College of Family Physicians of Canada, simulated office oral (SOO) and short-answer management problem (SAMP) | 71% | 8% (95%CI: -16%, 21%) |
|
Schabort, 2014 [14] CFPC, N = 69; RCPSC, N = 85 Canada |
Country of birth (Other vs. Canada) | 1.53 (0.50, 4.73) | 0.46 | Success on first try of Royal College of Physicians and Surgeons of Canada (RCPSC) examination. | 78% | 6% (95%CI: -14%, 16%) |
| Time from Graduation/ Graduation Recency | ||||||
|
Haukilahti, 2012 [44] N = 383 Finland |
Time from graduation < 10vs ≥ 10 | 1.20 (0.52, 2.86) | 0.658 | Success in licensing examinations of IMG doctors in Finland | 51.3% | 5% (95%CI: -15%, 24%) |
|
Schabort, 2014 [14] CFPC, N = 69; RCPSC, N = 85 Canada |
Years since graduation | 1.05 (0.87, 1.25) | 0.63 | Success in Certification examination–College of Family Physicians of Canada, simulated office oral (SOO) and short-answer management problem (SAMP) | 71% | 1% (95%CI: -3%, 4.4%) |
| Place of Qualification/Graduation | ||||||
|
Menzies, 2015 [42] N = 2,056 UK |
Place of qualification (UK graduates vs. IMG) | 3.17 (2.41, 4.17) | < 0.001 | Membership of the Royal College of Paediatrics and Child Health (MRCPCH) part 1B examination outcome | 41% |
UK graduates were more likely to pass MRCPCH exam 28% more (95%CI: 22–33% more) |
|
Bessant, 2006 [43] N = 483 UK |
Graduated from UK medical school. N = 483 |
4.87(3.86, 5.72) | 0.003 | Success of candidates taking a revision course in preparation for the MRCP (UK) PACES (practical assessment of clinical examination skills) examination | 45% |
Graduates from UK vs. overseas medical schools were more likely pass PACES 35% more (95%CI: 31–37% more) |
|
UK graduates with White ethnic origin N = 227 |
2.15 (1.21, 3.81) | 0.012 |
White vs. non-white ethnic UK graduates were more likely pass PACES 19% (95%CI: 5%, 31%) |
|||
|
Shaw, 2014 [41] N = 116 UK |
European vs. non-European university | 21.3 (5.6, 91.3) | < 0.001 |
Passing Clinical skill assessment in trainees who completed ST3 year in UK |
50% | Candidates graduated from European universities were 45.5% more (95%CI: 34.9 to 48.9% more) likely to pass CSA |
| Previous Experience | ||||||
|
Schabort, 2014 [14] CFPC, N = 69; Canada |
Previous Internship | 2.34 (0.61, 8.92) | 0.22 | Success in Certification examination–College of Family Physicians of Canada, simulated office oral (SOO) and short-answer management problem (SAMP) | 71% | Previous internship associated with 14% more (95%CI: 11% less to 25% more) success |
| Previous residency | 0.92 (0.29, 2.89) | 0.88 | Previous residency associated with 2% less (95%CI: 29% less to 17% more) success | |||
| Professional experience | 0.39 (0.098, 1.54) | 0.18 | Previous residency associated with 22% less (95%CI: 52% less to 8% more) success | |||
| Research experience | 1.18 (0.40, 3.54) | 0.76 | Previous residency associated with 3% more (95%CI: 22% less to 19% more) success | |||
|
Schabort, 2014 [14] RCPSC, N = 85 Canada |
Previous Internship | 4.09 (1.24, 13.5) | 0.02 | Success on first try of Royal College of Physicians and Surgeons of Canada (RCPSC) examination. | 78% |
IMG residents who previously completed internship were more likely to pass RCPSC exam on first try 16% (95%CI: 3%, 20%) |
| Previous residency | 1.48 (0.46, 4.76) | 0.51 | 6% (95%CI: -15%, 16%) | |||
| Professional experience | 0.49 (0.14, 1.66) | 0.25 | -15% (95%CI: -45%, 7%) | |||
| Research experience | 0.67 (0.20, 2.26) | 0.52 | -8% (95%CI: -37%, 11%) | |||
|
Sturesson, 2020 [28] N = 564 Sweden |
Participating in Complementary Program for physician (CPP) | NR | NR | Failing licensing exam | NR | Participants in CPP were less likely failing licensing exam |
|
Schabort, 2014 [14] CFPC, N = 69; Canada |
Human Development Index value (HDI) | 0.49 (0.002, 97.7) | 0.79 | Success in Certification examination–College of Family Physicians of Canada, simulated office oral (SOO) and short-answer management problem (SAMP) | 71% | -43% (95%CI: -78%, 21%) |
|
Schabort, 2014 [14] CFPC, N = 69; RCPSC, N = 85 Canada |
Human Development Index value (HDI) | 0.15 (0.001, 37.9) | 0.50 | Success on first try of Royal College of Physicians and Surgeons of Canada (RCPSC) examination | 78% | -43% (95%CI: -78%, 21%) |
|
Grierson, 2017 [15] N = 431 Canada |
Human Development Index value (HDI) | 41.75 (4.29, 406.05) | 0.001 | 84% |
Candidates from countries with higher HDI are more likely to succeed. 15% (95%CI: 11%, 16%) |
|
| Previous exam and qualifications | ||||||
| USA | ||||||
|
Peterson, 2020 [33] N = 3,255 USA |
USMLE Step1 | 0.99 (0.99, 1.01) | NR | Failing to obtain American board of family medicine (ABFM) certificate by IMGs | 8% failed | Each higher score in USMLE step 1 reduce probability of failing by 0.07% (95%CI: 0.07%less to 0.07% more) |
| USMLE Step 2 Communication and interpersonal skills | 1.00 (0.98, 1.02) | NR | Each higher score in USMLE step 2 do not change probability of failing (95%CI: 0.15%less to 0.15% more) | |||
|
USMLE Step 2 Spoken English proficiency |
1.04 (1.02, 1.06) | NR | Each higher score in USMLE step 2 Spoken English proficiency increase probability of probability of failing by 0.3% (95%CI: 0.15–0.44% more) | |||
|
USMLE Step 2 Integrated clinical encounter |
0.99 (0.97, 1.01) | NR | Each higher score in USMLE step 2 Integrated clinical encounter reduce probability of failing by 0.07% (95%CI: 0.22%less to 0.07% more) | |||
| USMLE Step 2 CK | 0.99 (0.98, 0.99) | NR | Each higher score in USMLE step 2 CK reduce probability of failing by 0.07% (95%CI: 0.07–0.15% less | |||
| USMLE Step 3 | 0.99 (0.98, 1.00) | NR | Each higher score in USMLE step 3 reduce probability of failing by 0.07% (95%CI: 0.00–0.15% less | |||
| ABFM in-training examination (ITE) PGY-1 | 0.99 (0.99, 0.99) | NR | IMGs who got higher score on ITE PGY1 were less likely to fail in ABFM certificate. -0.07% | |||
| ABFM ITE PGY-2 | 0.99 (0.99, 0.99) | NR | IMGs who got higher score on ITE PGY2 were less likely to fail in ABFM certificate. -0.07% | |||
| ABFM ITE PGY-3 | 0.99 (0.99, 0.99) | NR | IMGs who got higher score on ITE PGY3 were less likely to fail in ABFM certificate. -0.07% | |||
| Exam in UK | ||||||
|
Menzies, 2015 [42] N = 2,056 UK |
Part 1 A concurrently undertaken | 1.21 (0.81, 1.83) | 0.36 | Membership of the Royal College of Paediatrics and Child Health (MRCPCH) part 1B examination outcome | 41% | 4.7% more (5% less to 15% more) |
|
Patterson, 2018 [1] N = 1,874 UK |
Clinical Problem-Solving Test CPST | Coefficient (95%CI) Linear regression 0.05 (0.04, 0.07) | < 0.001 | Clinical Skills Assessment (CSA) component of Membership of the Royal College of General Practitioners (MRCGP) | NR | One score increase in CPST was associated with 0.05 (95%CI: 0.04, 0.07) score increase in CSA |
| Situational Judgment Test SJT | Coefficient (95%CI) Linear regression 0.07 (0.05, 0.09) | < 0.001 |
IMG with higher SJT score were more likely pass the CSA One score increase in SJT was associated with 0.07 (95%CI: 0.05, 0.09) score increase in CSA |
|||
|
Bessant, 2006 [43] N = 483 UK |
Passed part 2 written paper first time in all candidates. | 3.64 (2.31, 5.73) | 0.002 | success of candidates taking a revision course in preparation for the MRCP (UK) PACES (practical assessment of clinical examination skills) examination | 45% |
Candidates who passed part 2 written paper first time were more likely to pass PACES 30% (95%CI: 20%, 37%) |
| Exam in Canada | ||||||
|
Mathews, 2017 [31] N = 876 Canada |
Had skill assessment (Yes vs. No) | NR | NS | Obtain Speciality Designation in family medicine | 78.1% | |
| Years between MD and PGME ≥ 6 years vs. ≤ 5 years | NR | NS | ||||
Green: Low risk of bias, Yellow: moderate risk of bias, Red: high risk of bias
NS = Not-significant, NR = Not reported, Bold font = Significant;
Van Zanten (2003) [34] showed that candidates with higher scores on the USMLE step 2 were more likely to pass the CSA. Mathews (2017) [30] showed that IMGs who participated in a skills assessment program had a very high likelihood with high variability of passing the MCCQE2 [OR:9.60 (95%CI: 1.29, 71.63)] (Table 2).
Regarding graduation recency, candidates who graduated ≤ 5 years had more success on the COM exam in the USA [OR: 1.54 (95%CI:1.32, 1.81)] [34]. Conversely, candidates who graduated ≥ 6 years ago were more likely to pass the MCCQE2 in Canada [OR:3.45 (95%CI: 1.52, 7.69)] [30].
Matching into residency (postgraduate training position)
We identified one study [29] that investigated predictors of IMGs matching into an ophthalmology residency, which showed that having three letters of recommendation from US ophthalmologists [OR: 6.2 (95%CI:2.54, 15.16)], a USMLE step 1 score ≥ 236 [OR: 3.22 (95%CI: 1.38, 7.49)], having received an academic award [OR:1.12 (95%CI:1.03, 1.22)], having high-impact journal publications [OR: 2.99 (95%CI:1.51, 5.72)], and having US research experience [OR: 2.95 (95%CI:1.31, 6.67)] were associated with successful matching into ophthalmology residency in the USA. Furthermore, the results showed that doing postgraduate clinical training, including a surgical internship for ≥ 3 years in the USA, reduced the success rate for matching into an ophthalmology residency in the USA [OR: 0.26 (95%CI: 0.12, 0.58)] [29] (eTable 3).
Success/failure in certification exams
Nine studies informed predictors of success/failure in certification exams.
Age
Five studies reported conflicting evidence on the association between age and success in certification exams. While one study demonstrated that a decrease in age (younger age) was associated with greater success in the College of Family Physicians of Canada [OR = 1.76 (1.32, 2.33)] and the Royal College of Physicians and Surgeons of Canada certification exams [OR = 1.54 (1.08, 2.18)] in Canada [15] a similar study indicated that younger candidates were more successful in the licensing exam in Sweden [28]. However, another study showed that age increment was associated with more success in Membership of the Royal College of Pediatrics and Child Health part 1B examination outcome [OR = 0.71 (0.53, 0.97)] in the UK [41] (Table 3) (eFigure 3). The remaining two studies [39, 44] showed a statistically non-significant association between age and success in certification exams.
Table 3.
Predictors of success and failure in qualifying exams
| Author/ year/ sample size/country/RoB | Predictor | OR (95% CI) | pValue | Outcome | Baseline risk for outcome | Predictor/absolute success or failure change | |
|---|---|---|---|---|---|---|---|
| Outcome: success in qualifying exam | |||||||
|
Van Zanten 2003 [34] N = 11,690 USA |
Female vs. Male | 2.64 (2.31, 3.03) | NR | Integrated Clinical Encounter (ICE) component of ECFMG Clinical Skill assessment (CSA) | NR | Females were more likely to pass ICE | |
| Female vs. Male | 2 (1.71, 2.39) | NR |
Doctor-Patient Communication (COM) ECFMG Clinical Skill assessment (CSA) |
NR | Females were more likely to pass COM | ||
|
Mathews, 2017 [30] N = 876 Canada |
Sex (Female vs. Male) | NR | NS | Passing MCCQE2 | NR | There is no association between sex and success in MCCQE2 | |
| Language fluency | |||||||
|
Van Zanten 2003 [34] N = 11,690 USA |
TOEFL, every 10-unit increase | 1.2 (NR) | NR | Integrated Clinical Encounter (ICE) | NR | Candidates with higher score on TOEFL exam were more likely to pass ICE | |
|
Native language (English versus other) |
6.85 (3.81, 12.29) | NR |
Doctor-Patient Communication (COM) |
NR | English native language IMGs were more likely to pass COM | ||
| TOEFL, every 10-unit increase | 1.62 (NR) | NR |
Doctor-Patient Communication (COM) |
NR | Candidates with higher score on TOEFL exam were more likely to pass COM | ||
| Graduation recency | |||||||
|
Van Zanten 2003 [34] N = 11,690 USA |
Recent graduation (≤ 5 years) | 1.54 (1.32, 1.81) | NR |
Doctor-Patient Communication (COM) |
NR | IMGs who graduated less than 5 years were more likely to pass COM | |
|
Mathews, 2017 [30] N = 876 Canada |
Years between MD and PGME ≥ 6 years vs. ≤ 5 years |
3.45 (1.52, 7.69) | 0.003 | Passing MCCQE2 | 96.1% |
IMGs graduated ≥ 6 years were more likely to pass MCCQ2. 2.8% (95%CI: 1.3%, 3.5%) more |
|
| Previous qualification exams | |||||||
|
Van Zanten 2003 [34] N = 11,690 USA |
Step2, every 10-unit increase | 1.08 (NR) | NR |
Doctor-Patient Communication (COM) |
NR | Candidates with higher score on Step 2 exam were more likely to pass COM | |
| Step2, every 10-unit increase | 1.2 (NR) | NR | Integrated Clinical Encounter (ICE) | NR | Candidates with higher score on Step 2 exam were more likely to pass ICE | ||
|
Mathews, 2017 [30] N = 876 Canada |
Participation in a skill assessment program (Yes vs. No) | 9.60 (1.29, 71.63) | 0.027 | Passing MCCQE2 | 96.1% |
IMGs who have skill assessment were more likely to pass MCCQE2. 3.5% (95%CI: 0.9%, 3.9%) more |
|
NR = Not reported, Bold font = Significant; Green = Low Risk of Bias (RoB), Red = High RoB
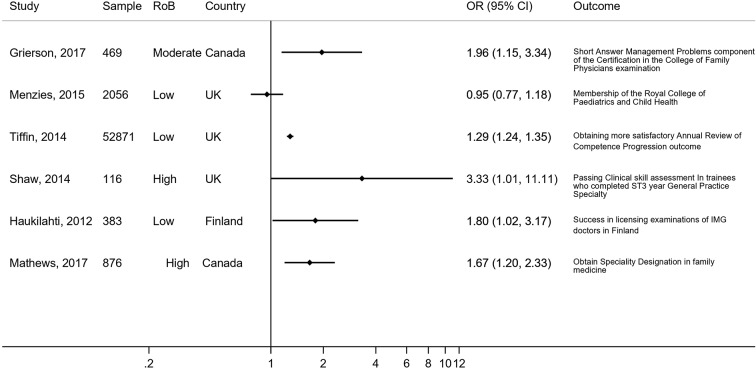
Female gender
Six studies [15, 30, 39, 41, 42, 44] explored the associations between female gender and success in certification exams, with five studies [15, 30, 39, 41, 44] indicating that female candidates were more likely to succeed in various certification exams [1] (Table 3)(Fig. 2).
Fig. 2.
Association of female gender and success in certificate exams
English fluency
Two studies showed that English fluency was associated with more success in both components of the College of Family Physicians examination, the Royal College of Physicians and Surgeons certification examination in Canada and the Clinical Skills Assessment (CSA) component of the Royal College of General Practitioners Membership in the UK [1, 15] (eTable 5).
Race and ethnicity
We identified two studies [39, 43] with conflicting results regarding the relationship between ethnicity and success in certification exams. Bessant (2006) [42] reported White graduates were more likely to pass the practical assessment of clinical examination skills examination of the MRCP in the UK [OR:2.04 (95%CI: 1.42, 2.94)], while Tiffin (2014) [39] demonstrated that being White was not associated with Annual Review of Competence Progression in the UK (eTable 5).
Country of graduation
Our search identified three studies that explored the association between the place of graduation and success in certification exams. Two studies showed that graduates from the UK vs. IMGs were more likely to pass the Membership of the Royal College of Paediatrics and Child Health MRCPCH [OR: 3.17 (95%CI: 2.41, 4.17)] and PACES (practical assessment of clinical examination skills) examination of the MRCP (Royal College of Pediatrics, UK) [42] [OR: 4.87(95%CI:3.86, 5.72)]. We also identified a study that showed graduates from European vs. non-European universities were very likely to pass the Clinical Skills assessment in 3rd-year residency in the UK [41] [OR: 21.3 (95%CI: 5.6, 91.3)] (Table 3).
Previous experience
In terms of previous experience, Schabort (2014) demonstrated that candidates with a prior internship were more likely to pass the Royal College of Physicians and Surgeons of Canada (RCPSC) examination on their first attempt [14] [OR:4.09 (95%CI: 1.24, 13.5)] (Table 3).
Result of qualifying exams
To explore the association between qualification exams and success in licensing exams in the USA, we identified one study which showed that lower USMLE Step 2 CK [OR:0.99 (95%CI: 0.98, 0.99)] and in training examination scores through years 1–3 of residency [OR:0.99 (95%CI: 0.99, 0.99)] were marginally associated with failing to obtain ABFM certification in the USA. Conversely, higher scores on the spoken English proficiency component of the USMLE Step 2 was associated with failing ABFM certification [OR:1.04 (95%CI: 1.02, 1.06)] [33] (Table 3).
Explaining the association between qualification exams and success in certificate exams in the UK, results of one study revealed that higher scores in the clinical problem-solving test [Coefficient for Linear regression 0.05 (95%CI: 0.04, 0.07)] and Situational Judgment Test [Coefficient Linear regression 0.07 (95%CI: 0.05, 0.09)] were associated with higher scores in the clinical skills assessment component of the Membership of the Royal College of General Practitioners (MRCGP) exam in the UK [1]. Bessant (2006) also showed that candidates who passed the part 2 written test on the first attempt were more likely to pass the PACES (Practical Assessment and Clinical Skills Examination) component of the MRCP in the UK [OR:3.64 (95%CI:2.31, 5.73)] [43] (Table 3).
Predictors of IMG retention for practice and academic career pursuits in a new country
We identified a study that showed that recent graduates who received their MD degree ≤ 5 years ago were more likely to work in Canada within two years after Postgraduate training [OR: 1.36 (95%CI: 1.03, 1.79)], and IMGs who were eligible for full licensure were more likely to work in Canada [OR:3.72 (95%CI:2.30, 5.99)] [30] Furthermore, residency vs. fellowship candidates were more likely to work in Canada [OR: 2.63 (95%CI: 1.59, 4.35)] [31] (eTable 5).
One study showed that when comparing family medicine and specialty IMGs, family medicine candidates were more likely to work in rural communities [OR: 2.32 (95%CI: 1.33, 4.17)], and male IMGs were more likely to work in rural communities [OR: 1.77 (95%CI: 1.16, 2.70)] [30].
One study showed that completing a post-residency clinical fellowship was associated with following an academic career amongst IMGs [OR: 1.73 (95%CI: 1.01, 2.96)] [37] (eTable 5).
Being disciplined and receiving complaints from the medical board
One study demonstrated that males [HR: 2.73 (95%CI: 1.90, 3.93)], IMGs with higher International English Language Testing System (IELTS) speaking scores [HR: 1.39 (95%CI: 1.13, 1.72)] and IMGs who attempted to pass the Professional and Linguistic Assessment of the General Medical Council in the UK (PLAB 1) after ≥ 4th attempts [HR: 2.30 (95%CI: 1.26, 3.59)] and PLAB 2 at ≥ 3rd attempts [HR: 2.45 (95%CI:1.44, 4.18)] were more likely to be censured by the General Medical Council (GMC) in the UK [38]. Furthermore, one study conducted in Australia showed that being an IMG was associated with attracting complaints [OR:1.24 (95%CI: 1.13, 1.36)] and being adversely disciplined [7] [OR: 1.41 (95%CI: 1.07, 1.85)] (eTable 6).
We identified a study with unadjusted results showing that IMGs had a higher risk of being disciplined than North American medical graduates [12] [OR = 1.58 (95%CI: 1.38, 1.82)] (eTable 8).
Clinical outcomes of patients managed by IMGs
One study showed that mortality rates in patients were lower when treated by non-US trained IMGs vs. US medical graduates or US citizens trained abroad [OR: 0.91 (95%CI: 0.86, 0.96)] [36]. Each additional score of the physician’s USMLE Step 2 CK examination decreased the likelihood of mortality in patients treated by that physician [OR: 0.998 (95%CI: 0.996, 0.999)] [35]; and patients of non-US trained IMGs had a 20% lower likelihood of mortality [OR: 0.82 (95%CI: 0.62, 0.99)] than patients treated by US citizens trained abroad [35] (eTable 7).
Another study [32] showed that male IMG physicians in the US were more likely to prescribe opioids [31] [OR:1.11 (95%CI: 1.03, 1.19)] (eTable 9) and US IMG specialists, including internists, medical specialists, surgeons, and emergency medicine specialists, were less likely to prescribe opioids vs. primary care physicians. IMG physicians practicing in the north [OR: 0.63 (95%CI: 0.58, 0.69)] and west regions [OR: 0.88 (95%CI: 0.80, 0.96)] were less likely to prescribe opioids vs. physicians from the southern US [31] (eTable 7).
Discussion
It is imperative to recognize that IMGs apply in large numbers for postgraduate training in their new country, competing for a limited number of positions. For example, in the 2023 Canadian Residency Service Match, 2105 IMGs registered, of which 555 (26.3%) were matched into a postgraduate residency position [45]. Furthermore, Canadian and US citizens who are unsuccessful at securing a medical school position in their country, are leaving their country of citizenship to complete medical school training elsewhere and then return to have to compete as an IMG with immigrant IMGs for postgraduate training positions in their country [46]. Medical schools often have less background information about IMG applicants compared to local graduates, where the Medical School Performance Record (MSPR) or other customary variables are available to aid in the file review, selection to interviews, and ranking process. This clearly demonstrates the importance of identifying predictors for IMG success and failure in residency and practice employment from the data available at the application; and highlights the need for a transparent, evidence-based, and defensible selection process for IMGs.
Although a pooled association measure would be more informative for decision-makers, we were unable to pool data statistically for a single pooled result due to diversity in outcome assessment methods. Yet, we identified six groups of outcomes. We have summarized the evidence in a narrative format, highlighting the association between various predictors and each outcome while acknowledging the uncertainty inherent in this evidence. Despite these limitations, it remains the most comprehensive evidence available to inform decisions regarding the selection of IMGs.
We found that female sex, English fluency and higher scores in previous qualification exams were associated with more success in the CSA components of the Educational Commission for Foreign Medical Graduates (ECFMG) exams [34]. Given that females demonstrate higher exam success compared to males in our systematic review, this trend may be attributed to their superior performance in topics like Ob/Gyn and stronger skills in data gathering, communication skills, clinical skills and note-writing [34, 47]. Additionally, factors such as cultural integration, exemplified by Finnish immigrants [44] and the global imbalance in healthcare opportunities for women, provide more opportunities for highly qualified female IMGs to succeed [15]. However, conflicting findings suggest a need for further study to clarify these associations conclusively. Qualitative evidence synthesis is increasingly prioritized in decision-making processes for complex areas like this.
Three letters of reference from US ophthalmologists, a USMLE step 1 score > 236, high-impact journal publications, and US research experience were associated with more success in Ophthalmology residency matching [29]. The association between the number of recommendation letters from US ophthalmologists suggests a preference over non-US letters for several reasons: Residency committees may value letters from US physicians with whom they have professional relationships; these letters demonstrate the applicant’s ability to make productive mentoring relationships; they signify approval from a physician trained in the US system; and letters from non-US physicians unfamiliar with the US match process may lack sufficient commentary on valued applicant characteristics. It should be noted that the number of letters of support as a predictor of matching in residency reflects several complex factors, such as work ethics, professional collaboration, and interpersonal relationships [29].
The evidence also showed that age decrement was associated with more success in certification exams in Canada [15] The findings of European studies showed notable inconsistencies regarding the association between age and success in certification exams [28, 39, 42, 44]. All studies [15, 39, 41, 44] except one [42] showed that females were more successful in passing licensing exams or had more satisfactory progress in competence. We found inconsistent results on the relationship between White ethnicity and certification assessment success [39, 43]. The results showed that candidates who graduated from UK and European medical schools were more likely to pass the MRCPCH writing test [42] and clinical skills assessment (CSA) [41, 43] in the UK. Possible reasons for these findings include familiarity with the culture and reduced language barriers. However, none of these factors can conclusively explain the findings [43]. Further investigation is needed to determine if these differences show real differences in skills.
Among all previous experiences of internship, residency and research, Schabort [14] showed that previous internship was associated with success in the RCPSC certification exams in Canada.
Considering previous exams and qualifications, the USMLE step 2 CK scores, in-training exams performance in 1st − 3rd-year residency were associated with residents’ performance in the ABFM certification exam [33]. Higher scores in the Clinical problem-solving and situational judgment tests were associated with success in the Royal College of General Practitioners (MRCGP) exam in the UK [1].
One study showed that male candidates who graduated ≤ 5 years ago, were eligible for a full license, and completed residency vs. fellowships were more likely to remain and work in Canada [31].
We identified a study that reported being male, higher scores in the speaking module of the IELTS and attempting to pass the PLAB1 ≥ 4 times and PLAB2 ≥ 3 times were more likely to be disciplined by the GMC in the UK [38]. The authors of this study suggested that making the PLAB or replacement assessment more stringent and raising the required standards of language reading and listening and clinical skills competency, as well as capping the number of PLAB resits permitted, may result in fewer fitness to practice events in IMGs.
Regarding clinical performance, one study showed that relative mortality risks were 20% lower when non-US trained IMGs treated patients than US citizens trained abroad [35].
Since the current evidence is derived from observational studies, the certainty of evidence is low. The observed association between predictors and outcomes indicates a significant relationship, yet it does not establish causation. Given the multifactorial nature of each association, it is important to note that these findings are indicative. Caution should be exercised when interpreting this evidence.
Strength and limitations
This review is the first and only systematic review on this topic using rigorous Cochrane-endorsed methodological tools (CHARMS, CHARMS-PF) to explore the predictors for success and failure in IMGs using variables available at the time of selection. Strengths of our review include explicit eligibility criteria and a comprehensive search without language restriction that identified 25 studies exploring predictors of success and failure for IMGs through adjusted analysis. We also assessed the risk of bias for each study using the QUIPS tool [24]. Whenever possible, we reported baseline probability for the outcome and presented the association as both relative and absolute measures transparently and explicitly to optimize interpretation.
The main limitation was excessive diversity in measuring outcomes, which made meta-analysis impossible to perform, and it provided more limited information for decision-makers. The results of this review are limited by the quality of primary studies available for inclusion, as more than half of the studies have a moderate to high risk of bias.
Conclusions
The main objective of this systematic review was to investigate the predictors of success and failure of IMGs in postgraduate training or practice in their new country. The studies encompassed in this systematic review span across Australia, Canada, Finland, the United Kingdom, the United States of America, and Sweden—making it the only study of its kind internationally. These studies identified predictors for success in qualifying or certification examinations, success in matching to a postgraduate residency position, or retention of an IMG to practice in their new country after the country had invested in training them. Moreover, these studies identified predictive factors for instances where IMGs were disciplined or faced complaints at medical boards in three countries. These findings are notably serious and warrant close attention. Another significant finding was predictors for mortality of patients treated by IMGs and predictors for clinical competence of IMGs in practice.
These predictors are worthy of the attention of all organizations and international policymakers involved in IMG selection, and the result of this review could assist in exploring predictors for success for IMG selection into postgraduate training or employment.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors thank Dr. Farid Foroutan, PhD, for guidance on methodology and reporting results.
Author contributions
IS, CH and VA conceived the study. RC and NR performed the literature search in consultation with IS and CH. MA, VA, IS and NA assisted with study organization and performed data analysis and critical revision of the manuscript. MA, VA, and IS provided writing and manuscript revision. All authors read and approved the final manuscript.
Funding
None.
Data availability
The datasets supporting the conclusions of this article are included within the article and its additional files.
Declarations
Ethical approval
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Patterson F, Tiffin PA, Lopes S, Zibarras L. Unpacking the dark variance of differential attainment on examinations in overseas graduates. Med Educ. 2018;52(7):736–46. 10.1111/medu.13605 [DOI] [PubMed] [Google Scholar]
- 2.CIHI. Canadian Institute of Health Information. Physicians in Canada, 2016: Summary Report. Ottawa, ON: CIHI; 2017. [Google Scholar]
- 3.Huijskens EGW, Hooshiaran A, Scherpbier A, Van Der Horst F. Barriers and facilitating factors in the professional careers of international medical graduates. Med Educ. 2010;44(8):795–804. 10.1111/j.1365-2923.2010.03706.x [DOI] [PubMed] [Google Scholar]
- 4.Negin J, Rozea A, Cloyd B, Martiniuk ALC. Foreign-born health workers in Australia: an analysis of census data. Hum Resour Health. 2013;11(1):1–9. 10.1186/1478-4491-11-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fayerman P. Canadian doctors educated abroad file lawsuit, say limits on B.C. residency training are unfair. Vancouver Sun. 2018.
- 6.Dyer C. Rate of serious complaints against UK doctors is higher for those qualifying outside Europe. BMJ: Br Med J (Online). 2009;338. [DOI] [PubMed]
- 7.Elkin K, Spittal MJ, Studdert DM. Risks of complaints and adverse disciplinary findings against international medical graduates in Victoria and Western Australia. Med J Australia 2012;197(8):448–52. [DOI] [PubMed]
- 8.Studdert DM, Spittal MJ, Elkin K. Risks of complaints and adverse disciplinary findings against international medical graduates in Victoria and Western Australia. Med J Australia. 2013;198(5):258–258. 10.5694/mja12.11624 [DOI] [PubMed] [Google Scholar]
- 9.Elkin KJ, Spittal MJ, Elkin DJ, Studdert DM. Doctors disciplined for professional misconduct in Australia and New Zealand, 2000–2009. Med J Aust. 2011;194(9):452–6. 10.5694/j.1326-5377.2011.tb03058.x [DOI] [PubMed] [Google Scholar]
- 10.Breen KJ. Risks of complaints and adverse disciplinary findings against international medical graduates in Victoria and Western Australia. Med J Aust. 2013;198(5):257–8. 10.5694/mja12.11572 [DOI] [PubMed] [Google Scholar]
- 11.Zubaran C. Risks of complaints and adverse disciplinary findings against international medical graduates in Victoria and Western Australia. Med J Aust. 2013;198(5):256–7. 10.5694/mja12.11809 [DOI] [PubMed] [Google Scholar]
- 12.Alam A, Matelski JJ, Goldberg HR, Liu JJ, Klemensberg J, Bell CM. The characteristics of international medical graduates who have been disciplined by professional regulatory colleges in Canada: a retrospective cohort study. Acad Med. 2017;92(2):244–9. [DOI] [PubMed]
- 13.Jeyalingam T, Matelski JJ, Alam AQ, Liu JJ, Goldberg H, Klemensberg J, et al. The characteristics of physicians who are re-disciplined by medical boards: a retrospective cohort study. Joint Comm J Qual Patient Saf. 2018;44(6):361–5. [DOI] [PubMed] [Google Scholar]
- 14.Schabort I, Mercuri M, Grierson LE. Predicting international medical graduate success on college certification examinations: responding to the thomson and cohl judicial report on IMG selection. Can Fam Physician. 2014;60(10):e478-e84. [PMC free article] [PubMed]
- 15.Grierson LE, Mercuri M, Brailovsky C, Cole G, Abrahams C, Archibald D, et al. Admission factors associated with international medical graduate certification success: a collaborative retrospective review of postgraduate medical education programs in Ontario. Can Med Association Open Access J. 2017;5(4):E785–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tamblyn R, Abrahamowicz M, Dauphinee WD, Hanley JA, Norcini J, Girard N, et al. Association between licensure examination scores and practice in primary care. JAMA. 2002;288(23):3019–26. 10.1001/jama.288.23.3019 [DOI] [PubMed] [Google Scholar]
- 17.Tamblyn R, Abrahamowicz M, Dauphinee D, Wenghofer E, Jacques A, Klass D, et al. Physician scores on a national clinical skills examination as predictors of complaints to medical regulatory authorities. JAMA. 2007;298(9):993–1001. 10.1001/jama.298.9.993 [DOI] [PubMed] [Google Scholar]
- 18.Carlson ML, Archibald DJ, Sorom AJ, Moore EJ. Under the microscope: assessing surgical aptitude of otolaryngology residency applicants. Laryngoscope. 2010;120(6):1109–13. 10.1002/lary.20914 [DOI] [PubMed] [Google Scholar]
- 19.Garrud P. Who applies and who gets admitted to UK graduate entry medicine?-an analysis of UK admission statistics. BMC Med Educ. 2011;11(1):71. 10.1186/1472-6920-11-71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.MacLellan A-M, Brailovsky C, Miller F, Leboeuf S. Clerkship pathway: a factor in certification success for international medical graduates. Can Fam Physician. 2012;58(6):662–7. [PMC free article] [PubMed] [Google Scholar]
- 21.Grumbach K, Commentary. Adopting postbaccalaureate premedical programs to enhance physician workforce diversity. Acad Med. 2011;86(2):154–7. 10.1097/ACM.0b013e3182045a68 [DOI] [PubMed] [Google Scholar]
- 22.Campbell M, McKenzie JE, Sowden A, Katikireddi SV, Brennan SE, Ellis S et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ. 2020;368. [DOI] [PMC free article] [PubMed]
- 23.Moons KGM, de Groot JAH, Bouwmeester W, Vergouwe Y, Mallett S, Altman DG, et al. Critical appraisal and data extraction for systematic reviews of prediction modelling studies: the CHARMS checklist. PLoS Med. 2014;11(10):e1001744. 10.1371/journal.pmed.1001744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Grooten WJA, Tseli E, Äng BO, Boersma K, Stålnacke B-M, Gerdle B, et al. Elaborating on the assessment of the risk of bias in prognostic studies in pain rehabilitation using QUIPS—aspects of interrater agreement. Diagn Prognostic Res. 2019;3(1):1–11. 10.1186/s41512-019-0050-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Norcini J, Grabovsky I, Barone MA, Anderson MB, Pandian RS, Mechaber AJ. The associations between United States Medical Licensing Examination Performance and outcomes of Patient Care. Acad Med. 2023:101097. [DOI] [PubMed]
- 26.Kanna B, Gu Y, Akhuetie J, Dimitrov V. Predicting performance using background characteristics of international medical graduates in an inner-city university-affiliated internal medicine residency training program. BMC Med Ed. 2009;9(1):1–8. [DOI] [PMC free article] [PubMed]
- 27.Nayer M, Rothman A. IMG candidates’ demographic characteristics as predictors of CEHPEA CE1 results. Can Fam Physician. 2013;59(2):170–6. [PMC free article] [PubMed]
- 28.Sturesson L, Heiding A, Olsson D, Stenfors, T. ‘Did I pass the licensing exam?’Aspects influencing migrant physicians’ results: a mixed methods study. BMJ Open. 2020;10(7):e038670. [DOI] [PMC free article] [PubMed]
- 29.Driver TH, Loh AR, Joseph D, Keenan JD, Naseri A. Predictors of matching in ophthalmology residency for international medical graduates. Ophthalmology. 2014;121(4):974–5. e2. 10.1016/j.ophtha.2013.11.024 [DOI] [PubMed] [Google Scholar]
- 30.Mathews M, Kandar R, Slade S, Yi Y, Beardall S, Bourgeault I. Examination outcomes and work locations of international medical graduate family medicine residents in Canada. Can Fam Physician. 2017;63(10):776–83. [PMC free article] [PubMed] [Google Scholar]
- 31.Mathews M, Kandar R, Slade S, Yi Y, Beardall S, Bourgeault IL. Retention patterns of canadians who studied medicine abroad and other international medical graduates. Healthc Policy. 2017;12(4):33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tamblyn R, Girard N, Boulet J, Dauphinee D. Habib B. Association of clinical competence, specialty and physician country of origin with opioid prescribing for chronic pain: a cohort study. BMJ Qual & Safety. 2022;31(5):340–52. [DOI] [PMC free article] [PubMed]
- 33.Peterson LE, Boulet JR, Clauser B. Associations between medical education assessments and American board of family medicine certification examination score and failure to obtain certification. Acad Med. 2020;95(9):1396–403. [DOI] [PubMed]
- 34.Van Zanten M, Boulet JR, McKinley DW. Correlates of performance of the ECFMG Clinical skills assessment: influences of candidate characteristics on performance. Acad Med. 2003;78(10):S72–4. [DOI] [PubMed]
- 35.Norcini JJ, Boulet JR, Opalek A, Dauphinee WD. The relationship between licensing examination performance and the outcomes of care by international medical school graduates. Acad Med. 2014;89(8):1157–62. [DOI] [PubMed]
- 36.Norcini JJ, Boulet JR, Dauphinee WD, Opalek A, Krantz ID, Anderson ST. Evaluating Qual care Provided Graduates Int Med Schools. Health Affairs. 2010;29(8):1461–8. [DOI] [PubMed] [Google Scholar]
- 37.Khalafallah AM, Jimenez AE, Camp S, Horowitz MA, Chiu I, Ryu D et al. Predictors of academic neurosurgical career trajectory among international medical graduates training within the United States. Neurosurgery. 2021;89(3):478–85. [DOI] [PubMed]
- 38.Tiffin PA, Paton LW, Mwandigha LM, McLachlan JC, Illing J. Predicting fitness to practise events in international medical graduates who registered as UK doctors via the Professional and Linguistic Assessments Board (PLAB) system: a national cohort study. BMC Med. 2017;15(1):1–15. 10.1186/s12916-017-0829-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tiffin PA, Illing J, Kasim AS, McLachlan JC. Annual Review of competence progression (ARCP) performance of doctors who passed Professional and Linguistic Assessments Board (PLAB) tests compared with UK medical graduates: national data linkage study. BMJ. 2014;348. [DOI] [PMC free article] [PubMed]
- 40.Mehdizadeh L, Potts H, Sturrock A, Dacre, J. Prevalence of GMC performance assessments in the United Kingdom: a retrospective cohort analysis by country of medical qualification. BMC Med Ed. 2017;17(1):1–12. [DOI] [PMC free article] [PubMed]
- 41.Shaw B, Fox J, Brown J, Hart A, Mamelok J. An investigation of factors affecting the outcome of the clinical skills assessment (CSA) in general practice specialty training. Educ Primary Care. 2014;25(2):91–5. [DOI] [PubMed]
- 42.Menzies L, Minson S, Brightwell A, Davies-Muir A, Long A, Fertleman C. An evaluation of demographic factors affecting performance in a paediatric membership multiple-choice examination. Postgrad Med J. 2015;91(1072):72–6. [DOI] [PubMed]
- 43.Bessant R, Bessant D, Chesser A, Coakley G. Analysis of predictors of success in the MRCP (UK) PACES examination in candidates attending a revision course. Postgrad Med J. 2006;82(964):145–9. [DOI] [PMC free article] [PubMed]
- 44.Haukilahti RL, Virjo I, Mattila K. Success in licensing examinations of doctors from outside the European economic area: experiences from Finland 1994–2009. Educ Primary Care. 2012;23(5):342–9. [DOI] [PubMed]
- 45.2023 CaRMS Forum. 2023 [cited 2023 2023]. https://www.carms.ca/pdfs/carms-forum-2023.pdf
- 46.Bartman I, Boulet JR, Qin S, Bowmer MI. Canadians studying medicine abroad and their journey to secure postgraduate training in Canada or the United States. Can Med Educ J. 2020;11(3):e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Unwin E, Potts HW, Dacre J, Elder A, Woolf K. Passing MRCP (UK) PACES: a cross-sectional study examining the performance of doctors by sex and country. BMC Med Educ. 2018;18:1–9. 10.1186/s12909-018-1178-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets supporting the conclusions of this article are included within the article and its additional files.