Abstract
Background
Patients living with long-term chronic illnesses often need ongoing medical attention, lifestyle adjustments, and psychosocial support beyond the initial diagnosis and treatment phases. Many experience illness deterioration and subsequently require hospitalisation, especially in the transition period after hospital discharge. A promising strategy for managing long-term conditions is promoting self-management. eHealth interventions involving remote patient monitoring have the potential to promote self-management and offer a more seamless bridge between the hospital and the patient´s home environment. However, such interventions can only significantly impact health and health care if they are effective, accepted and adopted by users, normalised into routine practice and everyday life, and able to be widely implemented. Feasibility studies are used to determine whether an intervention is suitable for the target population and effective in achieving its intended goal. They may also provide critical information about an intervention´s acceptability and usability.
Objectives
We aimed to evaluate the acceptability and usability of a nurse-assisted remote patient monitoring intervention for the post-hospital follow-up of patients with long-term illnesses by use of the core constructs of normalisation process theory.
Design
A descriptive and explanatory qualitative approach was used, with patients observed during training and semi-structured interviews conducted with patients and nurses after study completion.
Settings
Participants were recruited from two university hospitals in Norway between December 2021 and February 2023.
Participants
Ten patients were observed during training, and 27 patients and eight nurses were interviewed after study completion.
Methods
Structured and overt observations were made while the patients received training to operate the remote patient monitoring service, guided by an observation guide. Semi-structured interviews were conducted with patients and nurse navigators about their experiences of remote follow-up care, guided by open ended questions. Data analysis followed a stepwise deductive inductive method.
Results
`Achieving acceptance and usability through digital social interaction´ emerged as a unifying theme that bridged the experiences of patients with long-term illnesses and the nurse navigators. This overarching theme was illustrated by four sub-themes, which all reflected the usability and acceptability of the nurse-assisted remote patient monitoring service in various ways.
Conclusion
Acceptability and usability are critical factors to consider when evaluating remote patient monitoring interventions. In this study, the most important feature for promoting acceptability and usability was the interaction between patients and nurse navigators. Therefore, the intervention´s feasibility and implementation potential rested upon the relationship between its deliverer and receiver.
Keywords: Acceptability, Feasibility, Long-term illness, Normalisation process theory, Nursing research, Qualitative research, Remote patient monitoring, Usability
What is already known about the topic.
-
•
Remote patient monitoring has the potential to support long-term illness patients.
-
•
Remote patient monitoring can impact health and healthcare only if accepted and found usable by the target population.
-
•
Feasibility studies may help determine the acceptability and usability of new technologies.
Alt-text: Unlabelled box
What this paper adds.
-
•
The nurse-assisted remote patient monitoring intervention was found acceptable and usable by patients with heart failure and patients treated for colorectal cancer post-hospitalisation.
-
•
The relationship between acceptability and usability is interconnected and complex.
-
•
The social interaction component in digital technology is essential for acceptability and usability and must be recognised when developing new remote patient monitoring interventions.
Alt-text: Unlabelled box
1. Introduction
Patients living with long-term illness often experience deterioration and subsequently need hospitalisation, especially in the transition period after hospital discharge (Khan et al., 2021; Ang et al., 2015). Consequently, the period can be a critical phase for many (Pollack et al., 2016), during which the focus shifts from acute to long-term illness care, and patients must take responsibility for managing their health condition (Rennke and Ranji, 2015). However, many patients encounter challenges in adhering to post-discharge instructions, managing medications, or recognising potential complications (Mardani et al., 2020; Facchinetti et al., 2020). Therefore, effectively managing their illness during this transition requires continuity of care. Care should be connected and coordinated between patients and healthcare professionals across time and settings (Facchinetti et al., 2020). Digital health interventions could play a role in this transition, offering a more seamless bridge between the hospital and the patient´s home environment (Singh et al., 2022).
We examined the acceptability and usability of a nurse-assisted remote patient monitoring intervention. Acceptability refers to the extent to which an intervention is perceived as appropriate and relevant by the target population, both its receivers and deliverers, based on anticipated or experiential cognitive and emotional responses to the intervention (Sekhon et al., 2017). Acceptability may be acquired prospectively (i.e. before participating in the intervention), concurrently (i.e. whilst participating), and retrospectively (i.e. after participating) (Sekhon et al., 2017). Usability refers to the ease with which an intervention can be navigated and effectively used by the target population (Perski and Short, 2021). This study´s target populations were patients with heart failure and patients surgically treated for colorectal cancer, both of which are long-term illnesses requiring ongoing medical attention, lifestyle adjustments, and psychosocial support beyond the initial diagnosis and treatment phases (Zaharova et al., 2022; Lo et al., 2021; Husebø et al., 2019).
Remote patient monitoring refers to interventions that allow patients to share data using information and communication technologies to improve their care (Farias et al., 2020). Patient-generated data (e.g. vital signs, weight, and blood pressure) are transmitted via telephone, the internet, or videoconferencing from the patient´s home to a healthcare centre, providing clinical review (Malasinghe et al., 2019). One of the key advantages of remote patient monitoring is that it may assist health care professionals in quickly identifying any deviations from the expected recovery trajectory quickly (Stevenson et al., 2023; Farias et al., 2020). However, despite its potential benefits, remote patient monitoring raises some concerns (Thomas et al., 2021). Firstly, such interventions do not have the same possibilities for physical face-to-face interaction. Secondly, investigations into the clinical and cost-effectiveness of remote patient monitoring interventions have reported mixed results (Thomas et al., 2021). Thirdly, remote patient monitoring interventions can only significantly impact health and healthcare if they are shown to be effective, accepted and adopted by users, able to be normalised into routine practice and everyday life, and able to be widely implemented (Stefanicka-Wojtas and Kurpas, 2022).
There is currently a gap between research evidence and practice, especially regarding developing and normalising new health-promoting interventions for the patient groups for which they are intended (Huddlestone et al., 2020). Together with the complex nature of remote patient monitoring interventions, this gap often leads to implementation failure (Murray et al., 2010; May et al., 2007). The target population may accept an intervention, but its potential benefits may remain unrealized if it is unusable within the healthcare context. Conversely, even the most usable intervention may be unsuccessful if it fails to align with the values and preferences of the target population. However, feasibility studies may be used to determine whether an intervention is suitable for the target population and effective in achieving its intended goal (Bowen et al., 2009). They may also provide critical information about an intervention´s acceptability and usability (Meinert et al., 2020). When conducting feasibility studies, normalisation process theory has been shown to provide effective conceptual tools to evaluate the process (Williams et al., 2023). Normalisation process theory offers trialists a consistent framework that can be used to describe, assess, and improve interventions (McNaughton et al., 2020; Heinsch et al., 2021), and to analyze data (Huddlestone et al., 2020; May et al., 2018). Normalisation process theory identifies, characterises, and explains the mechanisms that drive an implementation process. The four key implementation mechanisms of the theory are: coherence (making sense of an intervention), cognitive participation (investing in an intervention), collective action (delivering an intervention), and reflexive monitoring (appraising and modifying an intervention) (Bamford et al., 2014). These mechanisms help explain how individuals and groups work together to make an intervention a routine part of everyday practice. In this study, the four mechanisms will be used to address a gap in the research field, comprehensively evaluating acceptability and usability to determine the feasibility and implementation potential of a nurse-assisted remote patient monitoring intervention.
2. Methods
2.1. Study design
This study is part of a larger research project, eHealth@Hospital-2-Home, which has three phases: (i) developing a nurse-assisted remote patient monitoring intervention, (ii) assessing the feasibility of the intervention, and (iii) conducting a randomised controlled trial (Husebø et al., 2019). This study pertains to the main project´s second phase, in which the feasibility of the nurse-assisted remote patient monitoring intervention is assessed. The intervention uses an existing platform (Dignio Connected Care), which patients can access through the My Dignio platform and nurse navigators can access through the Dignio Prevent platform (Grisot et al., 2019). The feasibility study used a descriptive and explanatory qualitative approach involving the triangulation of observation and semi-structured interviews. A study protocol for this feasibility study has been previously published (Morken et al., 2023).
2.2. Study intervention and participants
The remote patient monitoring intervention is a non-acute, 30-day post-hospitalisation intervention facilitated by nurse navigators. The nurse navigators are experienced hospital nurses with the clinical skills required to identify and monitor the healthcare requirements of patients with heart failure and colorectal cancer (Morken et al., 2023). The intervention includes a wireless, portable personal computer system (Apple iPad) with the My Dignio or Dignio Prevent application installed. The application is linked to monitoring devices by Bluetooth to register clinical measures such as blood pressure, pulse, weight, and temperature. The My Dignio application allows the patient to send self-reported symptoms and well-being, as well as clinical measurements, to the nurse navigators. The Dignio Prevent application allows the nurse navigators to see the measurements and symptoms and provide feedback to the patients. The application is generically designed to ensure full adoption of the eHealth service (i.e., the user interface is similar regardless of patient group). However, its features and content are carefully selected to fit the various patient populations.
2.3. Study population and recruitment
The study`s populations were patients with heart failure or colorectal cancer. The patients were a convenience sample, and the selection criteria were age ≥18 years, able to understand and speak the Norwegian language, and hospitalised due to symptomatic heart failure with an ejection fraction of ≥40 % or surgical treatment for colorectal cancer with curative intent. The patients with heart failure were recruited from cardiology bedside wards at two hospitals (A and B) in the southern part of Norway. Patients with colorectal cancer were recruited from a gastro-surgical bedside ward at hospital A. One of the nurse navigators contacted the patients about participation in this study before their discharge from the hospital. Before consenting to participate, the patients were shown an informational video, (https://www.youtube.com/watch?v=pT2NhK_jAAU), in which the intervention was thoroughly illustrated, and they received an information and consent letter from the nurse navigator. After providing consent, the patients were shown how to use the iPad, My Dignio platform, and the home monitoring devices before hospital discharge.
The study sample also comprised the nurse navigators involved in this study. They were consecutively recruited from hospitals A and B after the feasibility study had ended. The nurse navigators received training in the Dignio Prevent platform from a representative from Dignio either in person or through the Microsoft Teams platform (version 1.0.1). Table 1 provides a summary of the of the participants’ demographics.
Table 1.
Overview on demographic information.
| Patients | N = 27 |
|---|---|
| Age in years, Md (min-max) | 69 (48–85) |
| Sex, female | 8 |
| Diagnosis | |
| Heart failure | 17 |
| Colorectal cancer | 10 |
| Nurse navigators | n = 8 |
| Age in years, Md (min-max) | 31 (25–39) |
| Sex, female | 7 |
*N = count.
*Md = median.
2.4. Data collection
Data were collected by first observing 10 patients during their training in the application. The observations were structured and overt. The first author passively observed patients with heart failure (n = 4) while they received training from a nurse navigator. In contrast, the first author actively observed patients with colorectal cancer (n = 6) while providing their training. An observation guide was followed during the observations, and the field notes were recorded in an observation log immediately after each observation. Please see Supplementary materials, file 1, Table 1, Table 2, for an overview of the observation logs.
Table 2.
Core questions in the interview guide.
| Patient topic guide – questions about design and user-friendliness |
|
|
|
| Patient topic guide – questions about relevance and usefulness |
|
|
|
| Patient topic guide – questions about improvements |
|
|
|
| Nurse navigator topic guide – questions about design and user-friendliness |
|
|
|
| Nurse navigator topic guide – questions about relevance and usefulness |
|
|
|
| Nurse navigator topic guide – questions about improvements |
|
|
|
Data were also collected using semi-structured interviews with 27 patients after er their 30-day follow-up period. The nurse navigators (n = 8) who delivered the remote patient monitoring intervention were also interviewed. A semi-structured interview guide developed by the research team was followed during the interviews. It was arranged according to topics, with open-ended questions and sub-probes. Each interview was initiated with the question: ‘What is your overall experience with digital follow-up care and home monitoring?’ The interviews, which lasted from 40 to 60 min, continued with questions about design, content, ease of use, personal relevance, and interactions between patients and nurse navigators. A more detailed overview of the questions from the interview guides is presented in Table 2.
The first author performed all of the interviews. They were conducted either face-to-face or, when travel distances were long, digitally through the communication platform Microsoft Teams (version 1.0.1.) or by phone. The patient interviews (N = 27) were conducted individually. However, only two nurse navigators were interviewed individually (n = 2), with the other six interviewed in dyads (n = 3).
2.5. Data analysis
The observation data were organised in an observation log. The interviews were audio-taped and transcribed ad verbum, and the transcripts were then triangulated and analysed using stepwise-deductive induction, to identify issues and themes across the empirical material (Tjora, 2018; Lofthus et al., 2018; Gilstad et al., 2022). In the stepwise-deductive induction approach, the qualitative analysis aims to explore issues developed from the detailed processing of empirical data in an ‘upwards’ inductive process (inductive theory development). However, throughout the data analysis process, the researcher also works ‘downwards’ and deductively by constantly comparing from a more theoretical and conceptual understanding (deductive validation) (Tjora, 2018). The stepwise-deductive inductive approach is outlined in Fig. 1.
Fig. 1.
The stepwise-deductive induction coding method.
*NPT = normalization process theory.
The first author led the interpretation process, which was followed by discussions with the co-authors. All of the female co-authors (I.M.M, M.S, A.M.L.H) are professors with backgrounds as registered nurses. The male co-author (C.M) is a sociology professor who co-founded the normalization process theory. The analysis resulted in 952 preliminary inductively derived codes regarding patients’ and nurse navigators’ user experiences with the eHealth service. Based on coherence within each group, the codes were manually sorted into 12 groups (Tjora, 2018). Some of these groupings were thematically linked. Therefore, a higher degree of sorting was made, yielding eight categories and four subthemes. During categorization and thematization, all female authors collaborated to establish labels that best illustrated the findings. There were few debates on the codes and categories. However, some codes needed to be re-grouped after discussions among the co-authors. Several alternatives were considered before reaching a consensus on categories and sub-themes. Once the inductive coding was complete, the data extracts, codes and categories were translated from Norwegian to English, and the constructs from the normalization process theory were used as a theoretical lens through which to interrogate the findings and to help maximise the explanatory potential. Therefore, the constructs of the normalisation process theory were retrospectively ‘mapped’ to the four sub-themes that emerged from the inductive analysis, as higher-order concepts (McNaughton et al., 2020). During this deductive mapping process, an unexpected condition, or underlying pattern surfaced, leading to the construction of an overarching theme that bridged the sub-themes and constructs. This ‘abductive leap’ resulted from the combination or synthesis of induction and deduction (Karlsen et al., 2021), enabling a more comprehensive understanding of remote patient monitoring and the conditions necessary for accepting and using such technology. During the process of ‘mapping’ the constructs of normalization process theory to the sub-themes, the male co-author was engaged to ensure that the descriptions of the themes were consistent with the constructs of normalization process theory. For a detailed outline of the analysis process and alignment of sub-themes and categories with the constructs of normalisation process theory, please see Supplementary materials, file 2, Tables 3–6.
2.6. Trustworthiness
We used credibility, dependability, transferability, and confirmability to establish trustworthiness and assure that our findings reflect the participants’ perspectives (Graneheim et al., 2017). Credibility was assured by presenting the findings to other researchers, with both positive and negative aspects of remote patient monitoring documented. Dependability was assured by having the first author conduct all the interviews and transcribing them verbatim, making this aspect consistent. Transferability was ensured by providing detailed descriptions of the themes and presenting them so that others could relate to them. Additionally, readers can evaluate the quotations in the article and the appendix and determine if the results are transferable to similar contexts. Moreover, the participants were recruited from two hospitals and different wards, further strengthening transferability. Confirmability was established by following the recommended steps in the stepwise-deductive induction approach (Tjora, 2018).
2.7. Ethical considerations
We conducted this study according to the principles of the Helsinki Declaration (World Medical Association, 2013). All participants received verbal and written information about its aim. All participation was voluntary, and participants could withdraw from the study at any time. All participants gave their written consent to participate, and the findings have been anonymised. This study was approved by the Norwegian Center for Research Data (ID.NO: 523386) and the participating hospitals’ Privacy Appeals Board. The Regional Ethics Committee deemed the current feasibility study exempt (ID.NO: 242405).
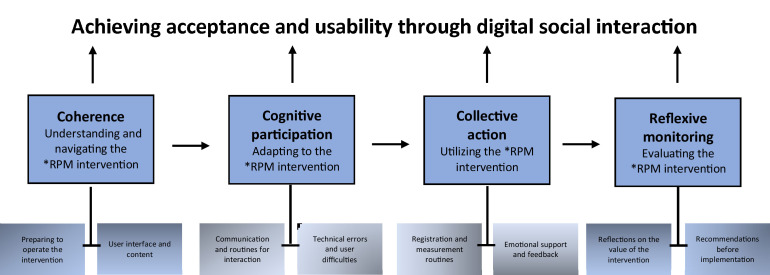
3. Findings
The overarching theme, `Achieving acceptance and usability through digital social interaction´, was a multidimensional concept that embodied the participants’ efforts to accept and use the remote patient monitoring intervention, with the digital social interaction between patient and nurse manifesting as the driving force. The overarching theme was informed by four interrelated subthemes, which were further broken down into eight categories, as shown in Fig. 2. The findings will be presented in turn, headlined with each subtheme and category. The findings from the patients will be presented first, followed by the nurse navigators.
Fig. 2.
The main findings from the study presented as the overarching concept, sub-themes, and categories.
*RPM = remote patient monitoring.
3.1. Coherence: understanding and navigating the remote patient monitoring intervention
The first sub-theme is supported by two categories: ‘preparing to operate the intervention’and ‘service interface and content’. It represents the patients’ and nurse navigators’ perception of the scope and nature of the nurse-assisted remote patient monitoring intervention, its practical functions and technicalities, and how remote patient monitoring facilitates patient-nurse interaction. This subtheme also describes the effort made by the participants to understand their responsibilities and specific tasks connected to participation in the intervention.
3.1.1. Preparing to operate the intervention
3.1.1.1. Patients
The patients had their first practical review of the digital platform and its associated medical devices during hospitalisation. This review became an initial ‘sense-making’ phase, in which the patients were introduced to the technical and practical aspects of the digital platform. Some patients described this first encounter as overwhelming, and the observational field notes showed that some were skeptical during the introduction. However, as the nurse navigators explained the intervention and the patient´s specific tasks, this skepticism was replaced with a more positive ‘I-can-do-this’ attitude. Moreover, the patients were introduced to the intervention individually, which represented the first step of the patient-nurse relationship – a relation that was described as particularly important and one that seemed to foster trust in remote patient monitoring:
‘I knew her. She treated me when I was hospitalised. It wasn´t a stranger that asked me questions. That was important. Had it been more general…one that didn´t know what I´d gone through … that would have been different.’ [Patient with colorectal cancer 6]
The importance of knowing your care provider was confirmed by patients who were not introduced to the intervention by their nurse navigator, and thus did not know who provided the digital follow-up. They described a different experience, wanting to have known the nurse navigator in forehand.
3.1.1.2. Nurse navigators
Preparing the patients also represented a sense-making phase for the nurse navigators. However, for them, the technology was familiar. It was more important for the nurse-navigators to ‘make sense’ of the patients and their needs. Therefore, nurse navigators described sitting down and reviewing the intervention and tasks connected to participation, as particularly beneficial since they got to know and form a bond with the patients during this phase. The nurse navigators also felt a greater personal ownership of the patients they recruited and trained themselves:
‘I think it´s easier to provide follow-up to patients whose history I know. Only a 10-minute talk make me provide them with better care. The patients felt safe, and I knew their problems. Everything was easier when I had seen them in advance.’ [Nurse navigator 8]
Nevertheless, due to the complex nature of the intervention, the nurse navigators described conducting the review with the patients as a time-consuming task.
3.1.2. Service interface and content
3.1.2.1. Patients
The observation data showed that the patients had few questions during the review. When they tested and applied the medical devices, they all managed to complete the task on their own. All the technical and practical aspects related to the patient platform were described as intuitive and easy. During the review of the daily and weekly questionnaires, few patients had remarks or comments. Furthermore, the patients were introduced to a disease-specific information page, in addition to the possibility of getting graphical overviews and trends. This latter feature was particularly acknowledged and found useful by the more ‘digital curious’ patients, as described by this patient with heart failure:
‘I managed to get a graphic overview of all my measurements, and before I returned the medical equipment, I took a picture of it. I will bring this picture with me to my next check-up at the out-patient clinic … they might not be so interested, but I am going to show it to them anyway.’ [Patient with heart failure 7]
Furthermore, all the patients managed to set up and perform the various tasks connected to the intervention on their own immediately after discharge. Therefore, the patient preparation seemed to provide the patients with the necessary understanding and skills to ‘take on’ the intervention.
3.1.2.2. Nurse navigators
The nurse navigators described the technical and operational aspects of the remote patient monitoring intervention as easy and found the system to have all the necessary features. However, surprisingly the nurse navigators reported that they were reluctant to offer participation in the intervention to patients if they thought the digital technology or the interventions’ everyday tasks would be too difficult or add too much to the patient's workload. Therefore, a few nurse navigators reported being selective as to whom they offered remote patient monitoring to, as expressed by this nurse navigator:
‘I wouldn’t say picky, but we were particular about who we recruited. Some patients were extremely multimorbid and, even though not diagnosed, also cognitively challenged. I wanted to feel safe about the patients we monitored, so I didn´t have to constantly pay attention in case they became acutely ill.’ [Nurse navigator 1]
3.2. Cognitive participation: adapting to the remote patient monitoring intervention
The second subtheme is supported by two categories: ‘digital communication and routines for interaction’and ‘technical errors and user difficulties’. It describes how the patients and nurse navigators established their roles, contributed to the intervention, and organised themselves to undertake the new technology, including remote interaction.
3.2.1. Digital communication and routines for interaction
3.2.1.1. Patients
Most of the patients adapted to digital communication and quickly found their preferred way to interact with the nurse navigator. The majority found messages to be the easiest and fastest way to communicate, whereas video was viewed as excessive and troublesome. Some patients had daily contact with the nurse navigators, while for others, the contact was more sporadic. However, the feedback from the nurse navigators was described as swift and effective and the patients reported that they provided them with individually adjusted care and practical solutions to their problems. Furthermore, most of the patients found it reassuring that the nurse navigator ‘checked-up’ on them regularly since the transition home could be challenging. Therefore, to be offered remote patient monitoring immediately after hospital discharge seemed to be particularly valued, as this patient described:
‘During hospitalisation you wear these electrodes. And then comes the day they remove them and just – ok, you can go. It´s like cutting the umbilical cord … you´re completely on your own. The fact that I could reach out to the nurse if something was up … that was important … at least to me.’ [Patient with heart failure 16]
3.2.1.2. Nurse navigators
The nurse navigators quickly adopted a routine for interacting with each patient, and like the patients, they also preferred messaging. However, the patients’ messages did not always provide the nurse navigators with a ‘complete picture’. Therefore, to resolve ambiguities or to elaborate on the content off the messages, the nurse navigators often contacted the patients by telephone.
‘It was cumbersome both for us and the patients to write messages back and forth. You often need more distinctions to assess of the situation. When they report that their breathing is heavier, you need to hear them breathe. And older people, they often responded with short messages, so it wasn´t always easy to understand their situation.’ [Nurse dyad 1]
While the telephone was not a part of the service, it was found to be the most appropriate tool for communication when the interventions’ message function fell short. It was described as more cumbersome to schedule face-to-face contact (i.e., a video call) than telephoning. However, the nurse navigators initiated a video call if it better met the patients’ needs.
3.2.2. Technical errors and user difficulties
3.2.2.1. Patients
When adapting to the remote patient monitoring intervention, some of the patients found it challenging to interpret the questions on the daily and weekly questionnaires. They were not always sure if they provided the correct answers to the questions and often had to ask the nurse navigator to clarify. However, all the patients adapted to the technical aspects of remote patient monitoring, and few technical problems were reported. The difficulties were usually related to usernames and passwords, charging or battery capacity, and the touchscreen. Additionally, the Bluetooth communication between the tablet and the medical devices was interrupted on some occasions, and the patients had to manually enter the digits. Nevertheless, when faced with these challenges, the patients `stayed on case´. They seemed committed to the intervention and made valuable contributions to driving it forward.
3.2.2.2. Nurse navigators
There were a few technical challenges related to the nurse navigators’ platform. However, nurse navigating placed new demands on the nurses. The most frequently mentioned challenge was the feeling of being needed and having to be available, also outside regular working hours. The nurse navigators reported that they usually adjusted the follow-up to the patient´s’ needs, but not being able to control the patient´s response time was described as frustrating. Additionally, some of the nurse navigators found it challenging to balance being a ‘regular’ nurse and being a nurse navigator. Therefore, having other nurse navigators to interact and cooperate with was highlighted as particularly valuable:
‘It was less vulnerable when we worked together and cooperated on the patients … it eased the burden of conscience. Having complete responsibility for one person … no, it was better to make decisions together.’[Nurse dyad 2]
3.3. Collective action: utilizing the remote patient monitoring intervention
The third subtheme is supported by the following two categories: ‘registrations and measurement routines’ and ‘emotional support and feedback’. It describes the effort made by the participants to operationalise and integrate the remote patient monitoring intervention into their everyday lives and work practice. In addition, the patient-nurse commitment was an integral part of how the participants’ maintained confidence and trust in the new technology.
3.3.1. Registrations and measurement routines
3.3.1.1. Patients
All the patients established a regular routine from day one and performed their tasks in the same order and at the same time throughout the 30-day follow-up period. The daily measurements were usually performed in the morning and completed within a short period. The patients described that keeping a regular schedule made it easier for them to register if their condition changed. Some also reported that the graphical overview of their measurements provided them with a good overview of any progress and deterioration and, thus, a better sense of control. Interestingly, a few patients also ‘experimented’ and took their measurements at various times to explore. One patient said the following:
‘It was interesting to pay attention to my blood pressure and pulse. Sometimes, I took the measurements before I went for a walk … and then half an hour after I returned … and then I was like: How is it? … Is there much difference? It was interesting.’[Patient with heart failure 4]
3.3.1.2. Nurse navigators
The nurse navigators attempted to establish regular routines for follow-up. However, they described combining their role as a regular nurse with the role of navigating the intervention as particularly difficult. All the nurse navigators worked shifts, which made it even harder to establish stable routines. Additionally, it was particularly demanding to set aside time to log on, evaluate the patients, and provide them with answers during working hours. Understandably, navigating nursing tasks were set aside in favour of regular nursing tasks. Moreover, it was also stressful for the nurse navigators to log on during a shift and see red alerts or messages in which the patients’ described signs of deterioration. If the nurse navigators were unable to handle these notifications immediately, it became a source of worry and made them feel guilty, which further interfered with their regular tasks at the ward.
3.3.2. Emotional support and feedback
3.3.2.1. Patients
All the patients reported that the nurse navigators provided them with support and an overall sense of security and trust. In fact, most referred to the nurse navigators as ‘my nurse’ or by their first name. The patients highly valued the feedback from the nurse navigators. They described it as comforting to have someone to discuss symptoms and complications with, such as variations in blood pressure or weight, surgical wounds, or pain. The patients described it as particularly supportive that specialised healthcare personnel evaluated their questionnaires and measurements on a daily basis, and they all trusted the feedback they received from the nurse navigators. It also seemed that some patients avoided hospitalisation due to the digital follow-up, as this patient noted:
‘It was very comforting to talk to the nurses … I was so afraid that my lungs would fill with water again … so when my weight increased, they talked to the doctor about increasing my diuretics. That felt so reassuring … I think I´ve avoided one admittance to hospital, maybe two.’ [Patient with heart failure 6]
3.3.2.2. Nurse navigators
The nurse navigators quickly realised that digital follow-up served an unmet healthcare need, and that they had become important to many patients. Consequently, the nurse navigators made an effort to be available for the patients and provide them with feedback as fast as possible. The nurse navigators did not take their nursing tasks lightly, and many described the importance of `delivering what they had promised´. A consistent theme throughout the interviews was that being a nurse navigator was more demanding responsibility-wise than time-wise. Some of the nurse navigators described that the patients were constantly on their minds, as expressed by two of the nurse navigators:
‘Thinking about the patients became a part of our daily routine …. every day. It sounds dramatic, but they [the patients] could be the first thing that entered our mind when we got out of bed … we thought of them … also subconsciously. We were very aware of our responsibility.’ [Nurse dyad 1]
All the nurse navigators described a strong sense of responsibility for the patients. However, they highlighted the positive feedback from the patients as a reward, and like the patients, the nurse navigators often referred to the patients as ‘my patient’. Providing patients with digital follow-up was described as meaningful and seemed to give the nurse navigators an overall burst of confidence.
3.4. Reflexive monitoring: evaluating the remote patient monitoring intervention
The fourth subtheme is supported by the following two categories: ‘reflections on the value of the intervention’and ‘recommendations before implementation´. It represents the participants’ appraisal and evaluation of the remote patient monitoring intervention, and their judgement on its utility and effectiveness. It also includes the participants’ reflections on the follow-up time and their thoughts on improving the intervention.
3.4.1. Reflections on the value of the intervention
3.4.1.1. Patients
Most patients valued remote patient monitoring and would have participated again had they been offered. However, for some, the overall usefulness of remote patient monitoring first became apparent some way into the intervention, as described by this patient:
`I wasn`t aware how useful the follow-up would be. I was very insecure in the beginning, so it was really good to have a connection to where I had been treated … but initially I didn`t quite see how this could benefit me´. [Patient with colorectal cancer 9]
Many patients expressed worry about ending the relationship with their nurse navigator, and a recurrent phrase during the interviews was: ‘Who would look after me now?’, suggesting that remote patient monitoring promoted patients with a sense of security. However, a few expressed ambivalence towards remote patient monitoring. These patients used the intervention as intended. They expressed appreciation for it and described the benefits of using it. However, they also revealed that the intervention generated emotions they did not want to engage with. Their participation ‘forced’ them to think about and act on their illness, when in reality, they wanted to forget about it, as expressed by this patient:
‘I couldn’t distance myself … I had to live with it throughout the research project … but at the same time, had you asked me again, I would participate because it is such a positive project … I would have said yes. It provided me with security, but the disease stayed with me, and I wanted to get rid of it.» [Patient with colorectal cancer 7]
3.4.1.2. Nurse navigators
All the nurse navigators viewed the remote patient monitoring intervention as a supplemental service, in which the patients were provided with an extra set of tools to manage their illness. Additionally, most of the nurse navigators valued the opportunity to follow-up on patients outside of a hospital setting and learn more about their challenges in their home environment. Positively, the nurse navigators took some of the things they learned while providing digital follow-up, back into their regular jobs at the ward. Two of the nurse navigators said:
«We talk differently about nutrition. Now we make a point of the importance of eating enough…worry less about having a few kilos extra. Our focus before was more on optimal heart nutrition, but now…I think we have gained a broader understanding for patients with heart failure…what they have to live with and what they are going through…we do meet them in a different way now than before.» [Nurse dyad 1]
3.4.2. Recommendations before implementation
3.4.2.1. Patients
The patients found the 30-day follow-up period to be adequate and proposed few specific changes to the technological aspects of the intervention. However, several proposed that remote patient monitoring should be a permanent offer and made available to as many patients as possible after hospital discharge. Others felt it would be more helpful if the nurse navigators had more room to initiate actions. Some went even further and advocated for giving the nurse navigators authority to help patients ‘skip’ some of the cumbersome steps in the healthcare system should their condition deteriorate.
3.4.2.2. Nurse navigators
The nurse navigators’ platform was also easy to operate. However, compared to the patient platform, the nurse navigators had to ‘click through’ more steps to complete their everyday tasks. Steps, such as evaluating notifications and signing them out, could benefit from being simplified. Additionally, some nurse navigators described that the smart-phone version had a poor layout. Consequently, they depended on a computer to get a good visual overview of each patient or reply to their messages. They highlighted this as cumbersome and inconvenient, in addition to interfering with their other work tasks.
4. Discussion
Using the lens of normalisation process theory, this study aimed to comprehensively evaluate the acceptability and usability of a nurse-assisted remote patient monitoring intervention and determine its feasibility and implementability. The interconnectedness of acceptability and usability became apparent in this intervention. The overarching theme ‘Achieving acceptance and usability through digital social interaction’ emerged as a continuous and stepwise process. It proposes that the social relationship and digital interaction between the patient and nurse navigator is the driving force of the remote patient monitoring intervention, and a precondition for the participant´s willingness to accept and use it. The process, which involved active involvement from both patients and nurse navigators, started with ‘coherence’: understanding and navigating the remote patient monitoring intervention». This step, which represented the practical review of the intervention, laid the first foundation for the patient-nurse relationship, and formed the basis for how the participants made sense of the intervention, and each other. During the next step, ‘cognitive participation’: adapting to the remote patient monitoring intervention», the patient-nurse relationship developed further as they began establishing their roles and use the different features of the service, with the most prominent feature being the communication between them. During the third step, ‘collective action: utilising the remote patient monitoring intervention’, the patients and nurse navigators became more committed to the intervention and each other. Many patients and nurse navigators formed a close relationship, which seemed to drive the intervention forward. The last step, ‘reflexive monitoring: evaluating the remote patient monitoring intervention’, represented an appraisal phase, in which the ‘digital relationship’ between patients and nurse navigators was highlighted as especially valuable and one that mutually benefitted them.
In this study, the constructs of the normalisation process theory followed sequentially from each other: coherence seemed like a necessary precursor to participation, a degree of cognitive participation was required before collective action, and reflexive monitoring represented the final stage before normalisation (May et al., 2018). However, the steps in which the participants achieved acceptability and usability also appeared interrelated and overlapping, and it proved somewhat difficult to separate the transition between them. Nevertheless, in this study, the construct of coherence seems to align with prospective acceptability, in that the participants accepted the remote patient monitoring intervention before delivery (Sekhon et al., 2017). The pre-intervention review provided the participants with the necessary sense-making to understand the nature and purpose of remote patient monitoring before participating in the intervention. It also provided them with the practical skills to interact with it effectively and efficiently (i.e., usability). The patient's prospective acceptance and basic skills related to the technical aspects of the intervention, were expressed through their immediate integration of the intervention into their normal everyday activities after hospital discharge. The fact that the participants found the intervention usable and coherent and managed to engage cognitively with it also laid the necessary foundation for the next steps in the process, cognitive participation, and collective action.
For the nurse navigators, prospective acceptability, together with their role as training facilitators, led to an eagerness to incorporate the intervention into their everyday routine. While they sometimes struggled to align the intervention to existing practices, their initial sense-making made them undertake an administrative role in which they worked actively to meet the patient´s needs and make the intervention fit each patient. This finding is consistent with previous research showing that providing a patient-centric and personalised approach is crucial when determining the success of a remote patient monitoring intervention (Srivastava et al., 2019).
The normalisation process theory constructs of cognitive participation and collective action seem closely related to the concept of concurrent acceptability (Sekhon et al., 2017). In the nurse-assisted remote patient monitoring intervention, the participants clearly used the necessary actions and skills to enact and commit to the intervention. Its accessible and ‘ready-to-use’ technology provided a basic and necessary foundation for their ability to establish routines and to utilize the intervention in everyday life. Moreover, the participants also engaged with the intervention on a more cognitive level, suggesting that they found the intervention trustworthy and dependable, and that it delivered what it promised (Pang and Liu, 2023). Furthermore, in this study, the relationship between patients and nurse navigators was based on trust. The patients trusted that the nurse navigators performed daily digital checkups, made accurate interpretations of their measurements and messages, reached out to them if something was irregular, and provided accurate advice. Similarly, the nurse navigators, trusted that the patients performed daily measurements, answered the questionnaire, communicated to them if their condition deteriorated, and used the advice they received. Therefore, both high usability skills and the trust-based relationship seemed to be a precursor to, and a promoter of acceptability. This study also found evidence that the nurse navigators’ independent and administrative role in the intervention was key to the patients’ acceptability and usability experiences. The way they executed their navigating role laid the foundation for high usability, in addition to contributing to both prospective and concurrent acceptance for patients.
In the transition from the hospital to home, many patients encounter challenges in managing their illness and recognising complications or deterioration. However, with support from a remote patient monitoring intervention, more patients could effectively self-manage their long-term illnesses at home (Hanlon et al., 2017). Nonetheless, when providing digital follow-up, it is crucial to provide feedback to patients in a way that strengthens them to take control of their health (Koehler et al., 2018). In this study, the nurse navigators seemed to provide timely and appropriate care via the response system, which relieved patients’ symptoms and offered them solutions to their various complications. Through their navigating role, the patients also provided them with valuable knowledge on the consequences of living with long-term illnesses. The fact that this newly acquired knowledge could be used in their work as regular nurses seemed to contribute to their acceptance of the intervention. Furthermore, research show that remote patient monitoring interventions are offered more frequently to patients with better prognosis and with less risk of deteriorating (Geller et al., 2019), affecting overall acceptability. Clinical frailty is related to a lower level of self-care (Munkhaugen et al., 2023). Frail patients may find it difficult to accept the everyday tasks connected to participation in remote patient monitoring interventions. Due to `gatekeeping´, the patients in this study may have been less frail and therefore also highly compliant and mostly provided the nurse navigators with positive feedback. This feedback is likely to have generated positive emotions in the nurse navigators which may have made it easier for them to accept their navigating responsibilities.
The normalisation process theory construct of reflexive monitoring seems to align well with the concept of retrospective acceptability (Sekhon et al., 2017). We found that the interaction between the patients and nurse navigators in the nurse-assisted remote patient monitoring intervention was rewarding and contributed to overall high acceptability by both patients and nurse navigators throughout the intervention. It is also likely that the system´s high usability contributed to the participants acceptance. However, while usability was high among all the participants, some features of the intervention would benefit from improvement. The nurse navigators mainly highlighted changes to technical aspects of their platform that would make the system´s operation more effective and thus lead to more timely and appropriate responses from them. The patients’ judgements on the intervention seemed less related to technical features. Instead, they promoted a more independent nurse navigator role, in which remote patient monitoring form a more direct and straight line back into the hospital should the patients need it. The desire for ‘fast track’ access to healthcare services has been described in previous studies (Srivastava et al., 2019; Pedone et al., 2015).
Behavioural interventions can often be complex and challenging for participants to fully comprehend before experiencing them (Ortblad et al., 2023). Additionally, participants’ perceptions of acceptability may change throughout an intervention (Manne and Andrykowski, 2006). When retrospectively evaluating this study, we found that high usability and high overall usefulness were not necessarily synonymous with fully accepting the intervention. For some patients, participation instead created mixed emotions. After hospital discharge, many patients want to ‘return to normal’, which can sometimes conflict with the healthcare system´s expectations of ‘living with’ and embracing the tasks connected to self-managing their illness. Previous research indicates that a recursive relationship seems to exist between illnesses and the technologies that monitor them, which does not necessarily reduce anxiety but makes prominent the unpredictable existence of the illness (Lehoux, 2008). Therefore, patients can associate monitoring of their illness with enthusiasm, engagement, and pride, but also with increased awareness of their illness, limitation, and differentness (Salmela et al., 2019). In this study, the ambivalence expressed towards remote patient monitoring, result from a contradictory relationship between ill and normal, which was made even more apparent by participating in the nurse-assisted remote patient monitoring intervention. However, the results from this study may suggest that the social interaction between the patient and nurse navigator moderated or outweighed the ambivalence or negative emotions that participation in the intervention generated.
5. Implications
Based on the results from this study, it seems particularly important to consider the significance of social interaction when developing future remote patient monitoring interventions. The social interaction component in digital healthcare interventions should not be underestimated. Additionally, the risk of creating ambivalence is always present when patients are ‘forced’ to confront their illness. Therefore, future remote patient monitoring interventions should be even more tailored to meet patients’ need to report symptoms and their ability to address their long-term illnesses. Furthermore, such interventions may also benefit from a tighter fit to nurses’ work schedule. Additionally, future research may focus on testing remote patient monitoring interventions in larger randomized control trials’. Remote patient monitoring could also be beneficial for other chronic illness populations.
6. Limitations
This study had some limitations. First, it appeared that a few of the nurse navigator regarded recruitment as a discretionary activity, since they seemed more inclined to offer digital follow-up to more robust patients. This approach may have affected overall acceptability. It may also imply that we have interviewed a subset of participants who held particularly positive views of remote patient monitoring. Second, some nurse navigators described digital follow-up as time-consuming and increasing their workload. This illustrates that nurses involved in remote patient monitoring require efficient workflows and support to manage the additional responsibilities associated with digital follow-up. Consequently, when remote patient monitoring is implemented, nurse navigators should be provided time in their work schedule to conduct follow-up. Third, the dissimilar interview methods (i.e., digital versus face-to-face and individual versus dyadic interviews), may have caused different dynamics during the interviews. However, similar issues were explored during the interviews, and data saturation was achieved. Last, the considerably smaller number of nurse navigators interviewed compared to patients may not provide an adequate representation of their perceptions.
7. Conclusion
In this study, the interaction between patients and nurse navigators was the most essential feature of the nurse-assisted remote patient monitoring intervention in terms of acceptability and usability. As a result, the feasibility and implementability of the intervention rested upon the relationship between receiver and deliverer. Furthermore, the study's findings emphasise the significance of digital follow-up care following hospital discharge. Remote patient monitoring helps ensure that the support and guidance provided during hospitalisation extend into the post-discharge period. Moreover, the study demonstrates that remote patient monitoring is more than just a technological innovation for the benefit of the intervention recipients. The nurse-assisted remote patient monitoring intervention also improved the knowledge of the nurse navigators who delivered it. Increasing healthcare professionals’ knowledge about living with a long-term illness may improve their ability to prepare patients for life at home after hospital discharge. Therefore, the nurse-assisted remote patient monitoring intervention has the potential to improve patient trajectories in the long term. However, additional research is needed to determine how remote patient monitoring affects nurses’ workflow, which remote patient monitoring solutions will be most beneficial in nurses’ work practices, and how to integrate remote patient monitoring into existing healthcare systems.
CRediT authorship contribution statement
Hege Wathne: Writing – review & editing, Writing – original draft, Visualization, Validation, Methodology, Formal analysis, Conceptualization. Carl May: Writing – review & editing, Visualization, Methodology, Conceptualization. Ingvild Margreta Morken: Writing – review & editing, Supervision, Methodology, Conceptualization. Marianne Storm: Writing – review & editing, Supervision, Methodology, Conceptualization. Anne Marie Lunde Husebø: Writing – review & editing, Supervision, Methodology, Formal analysis, Conceptualization.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors would like to thank all the patients and nurse navigators who shared their experiences of participating in a remote patient monitoring intervention.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.ijnsa.2024.100229.
Appendix. Supplementary materials
References
- Ang C.W., Seretis C., Wanigasooriya K., Mahadik Y., Singh J., Chapman M.A.S. The most frequent cause of 90-day unplanned hospital readmission following colorectal cancer resection is chemotherapy complications. Colorectal Dis. 2015;17(9):779–786. doi: 10.1111/codi.12945. [DOI] [PubMed] [Google Scholar]
- Bamford Claire, Poole Marie, Brittain Katie, Chew-Graham Carolyn, Fox Chris, Iliffe Steve, Manthorpe Jill, Robinson Louise, CAREDEM team Understanding the challenges to implementing case management for people with dementia in primary care in England: a qualitative study using normalization process theory. BMC Health Serv. Res. 2014;14:1–12. doi: 10.1186/s12913-014-0549-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen Deborah J, Kreuter Matthew, Spring Bonnie, Cofta-Woerpel Ludmila, Linnan Laura, Weiner Diane, Bakken Suzanne, Kaplan Cecilia Patrick, Squiers Linda, Fabrizio Cecilia. How we design feasibility studies. Am. J. Prev. Med. 2009;36(5):452–457. doi: 10.1016/j.amepre.2009.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Facchinetti Gabriella, D'Angelo Daniela, Piredda Michela, Petitti Tommasangelo, Matarese Maria, Oliveti Alice, Marinis Maria Grazia De. Continuity of care interventions for preventing hospital readmission of older people with chronic diseases: a meta-analysis. Int. J. Nurs. Stud. 2020;101 doi: 10.1016/j.ijnurstu.2019.103396. [DOI] [PubMed] [Google Scholar]
- Farias Frederico Arriaga Criscuoli de, Dagostini Carolina Matté, Bicca Yan de Assunção, Falavigna Vincenzo Fin, Falavigna Asdrubal. Remote patient monitoring: a systematic review. Telemed. e-Health. 2020;26(5):576–583. doi: 10.1089/tmj.2019.0066. [DOI] [PubMed] [Google Scholar]
- Geller J.C., Lewalter T., Bruun N.E., Taborsky M., Bode F., Nielsen J.C., Stellbrink C., Schon S., Muhling H., Oswald H., Reif S., Kaab S., Illes P., Proff J., Dagres N., Hindricks G., In-Time Study Group Implant-based multi-parameter telemonitoring of patients with heart failure and a defibrillator with vs. without cardiac resynchronization therapy option: a subanalysis of the IN-TIME trial. Clin. Res. Cardiol. 2019;108(10):1117–1127. doi: 10.1007/s00392-019-01447-5. https://www.ncbi.nlm.nih.gov/pubmed/30874886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilstad Heidi, Sand Kari, Solbjør Marit, Melby Line. Deconstructing (e) health literacy: aspects that promote and inhibit understanding of health information in breast cancer patient pathways. Int. J. Qual. Stud. Health Well-being. 2022;17(1) doi: 10.1080/17482631.2022.2137961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graneheim Ulla H, Lindgren Britt-Marie, Lundman Berit. Methodological challenges in qualitative content analysis: a discussion paper. Nurse Educ. Today. 2017;56:29–34. doi: 10.1016/j.nedt.2017.06.002. [DOI] [PubMed] [Google Scholar]
- Grisot M., Moltubakk Kempton A., Hagen L., Aanestad M. Data-work for personalized care: examining nurses' practices in remote monitoring of chronic patients. Health Inform. J. 2019;25(3):608–616. doi: 10.1177/1460458219833110. https://www.ncbi.nlm.nih.gov/pubmed/30880551 [DOI] [PubMed] [Google Scholar]
- Hanlon P., Daines L., Campbell C., McKinstry B., Weller D., Pinnock H. Telehealth interventions to support self-management of long-term conditions: a systematic metareview of diabetes, heart failure, asthma, chronic obstructive pulmonary disease, and cancer. J. Med. Internet. Res. 2017;19(5):e172. doi: 10.2196/jmir.6688. https://www.ncbi.nlm.nih.gov/pubmed/28526671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinsch Milena, Wyllie Jessica, Carlson Jamie, Wells Hannah, Tickner Campbell, Kay-Lambkin Frances. Theories informing eHealth implementation: systematic review and typology classification. J. Med. Internet Res. 2021;23(5):e18500. doi: 10.2196/18500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huddlestone Lisa, Turner Jessica, Eborall Helen, Hudson Nicky, Davies Melanie, Martin Graham. Application of normalisation process theory in understanding implementation processes in primary care settings in the UK: a systematic review. BMC Fam. Pract. 2020;21:1–16. doi: 10.1186/s12875-020-01107-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Husebø, Anne Marie Lunde, Marianne Storm, Ingvild Margreta Morken, Jens Espeland, Laila Garberg Hagen, et Bjørg Karlsen. 2019. Discussing a nurse assisted ehealth service from hospital to home. 2019 International Conference on Wireless and Mobile Computing, Networking and Communications (WiMob).
- Karlsen Bjørg, Martin Hillestad Torgeir, Dysvik Elin. Abductive reasoning in nursing: challenges and possibilities. Nurs. Inq. 2021;28(1):e12374. doi: 10.1111/nin.12374. [DOI] [PubMed] [Google Scholar]
- Khan Muhammad Shahzeb, Sreenivasan Jayakumar, Lateef Noman, Abougergi Marwan S, Greene Stephen J, Ahmad Tariq, Anker Stefan D, Fonarow Gregg C, Butler Javed. Trends in 30-and 90-day readmission rates for heart failure. Circul. Heart Fail. 2021;14(4) doi: 10.1161/CIRCHEARTFAILURE.121.008335. [DOI] [PubMed] [Google Scholar]
- Koehler Friedrich, Koehler Kerstin, Deckwart Oliver, Prescher Sandra, Wegscheider Karl, Kirwan Bridget-Anne, Winkler Sebastian, Vettorazzi Eik, Bruch Leonhard, Oeff Michael. Efficacy of telemedical interventional management in patients with heart failure (TIM-HF2): a randomised, controlled, parallel-group, unmasked trial. Lancet. 2018;392(10152):1047–1057. doi: 10.1016/S0140-6736(18)31880-4. [DOI] [PubMed] [Google Scholar]
- Lehoux Pascale. The duality of health technology in chronic illness: how designers envision our future. Chronic Illn. 2008;4(2):85–97. doi: 10.1177/1742395308092475. [DOI] [PubMed] [Google Scholar]
- Lo P.S., Lin Y.P., Hsu H.H., Chang S.C., Yang S.P., Huang W.C., Wang T.J. Health self-management experiences of colorectal cancer patients in postoperative recovery: a qualitative study. Eur. J. Oncol. Nurs. 2021;51 doi: 10.1016/j.ejon.2021.101906. https://www.ncbi.nlm.nih.gov/pubmed/33601194 [DOI] [PubMed] [Google Scholar]
- Lofthus Ann-Mari, Weimand Bente M, Ruud Torleif, Rose Diana, Heiervang Kristin S. “This is not a life anyone would want”—A qualitative study of norwegian ACT service users' experience with mental health treatment. Issues Ment. Health Nurs. 2018;39(6):519–526. doi: 10.1080/01612840.2017.1413459. [DOI] [PubMed] [Google Scholar]
- Malasinghe Lakmini P, Ramzan Naeem, Dahal Keshav. Remote patient monitoring: a comprehensive study. J. Ambient Intell. Humaniz. Comput. 2019;10:57–76. [Google Scholar]
- Manne S.L., Andrykowski M.A. Are psychological interventions effective and accepted by cancer patients? II. Using empirically supported therapy guidelines to decide. Ann. Behav. Med. 2006;32(2):98–103. doi: 10.1207/s15324796abm3202_4. https://www.ncbi.nlm.nih.gov/pubmed/16972804 [DOI] [PubMed] [Google Scholar]
- Mardani A., Griffiths P., Vaismoradi M. The role of the nurse in the management of medicines during transitional care: a systematic review. J. Multidiscip. Healthc. 2020;13:1347–1361. doi: 10.2147/JMDH.S276061. https://www.ncbi.nlm.nih.gov/pubmed/33154651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- May C., Finch T., Mair F., Ballini L., Dowrick C., Eccles M., Gask L., MacFarlane A., Murray E., Rapley T., Rogers A., Treweek S., Wallace P., Anderson G., Burns J., Heaven B. Understanding the implementation of complex interventions in health care: the normalization process model. BMC. Health Serv. Res. 2007;7:148. doi: 10.1186/1472-6963-7-148. https://www.ncbi.nlm.nih.gov/pubmed/17880693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- May C.R., Cummings A., Girling M., Bracher M., Mair F.S., May C.M., Murray E., Myall M., Rapley T., Finch T. Using normalization process theory in feasibility studies and process evaluations of complex healthcare interventions: a systematic review. Implement. Sci. 2018;13(1):80. doi: 10.1186/s13012-018-0758-1. https://www.ncbi.nlm.nih.gov/pubmed/29879986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNaughton R.J., Steven A., Shucksmith J. Using normalization process theory as a practical tool across the life course of a qualitative research project. Qual. Health Res. 2020;30(2):217–227. doi: 10.1177/1049732319863420. https://www.ncbi.nlm.nih.gov/pubmed/31347440 [DOI] [PubMed] [Google Scholar]
- Meinert E., Rahman E., Potter A., Lawrence W., Van Velthoven M. Acceptability and usability of the mobile digital health app noobesity for families and health care professionals: protocol for a feasibility study. JMIR. Res. Protoc. 2020;9(7):e18068. doi: 10.2196/18068. https://www.ncbi.nlm.nih.gov/pubmed/32706703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morken Ingvild Margreta, Wathne Hege Bjøkne, Karlsen Bjørg, Storm Marianne, Nordfonn Oda Karin, Gjeilo Kari Hanne, Urstad Kristin Hjorthaug, Søreide Jon Arne, Husebø Anne Marie. Assessing a nurse-assisted eHealth intervention posthospital discharge in adult patients with non-communicable diseases: a protocol for a feasibility study. BMJ Open. 2023;13(8) doi: 10.1136/bmjopen-2022-069599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munkhaugen J., Sverre E., Dammen T., Husebye E., Gjertsen E., Kristiansen O., Aune E. Frailty, health literacy and self-care in patients admitted with acute heart failure. Tidsskr. Nor. Laegeforen. 2023;143(17) doi: 10.4045/tidsskr.23.0297. https://www.ncbi.nlm.nih.gov/pubmed/37987080 [DOI] [PubMed] [Google Scholar]
- Murray E., Treweek S., Pope C., MacFarlane A., Ballini L., Dowrick C., Finch T., Kennedy A., Mair F., O'Donnell C., Ong B.N., Rapley T., Rogers A., May C. Normalisation process theory: a framework for developing, evaluating and implementing complex interventions. BMC. Med. 2010;8:63. doi: 10.1186/1741-7015-8-63. https://www.ncbi.nlm.nih.gov/pubmed/20961442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortblad K.F., Sekhon M., Wang L., Roth S., van der Straten A., Simoni J.M., Velloza J. Acceptability assessment in HIV prevention and treatment intervention and service delivery research: a systematic review and qualitative analysis. AIDS Behav. 2023;27(2):600–617. doi: 10.1007/s10461-022-03796-1. https://www.ncbi.nlm.nih.gov/pubmed/35870025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pang Hua, Liu Yanxinyue. Untangling the effect of cognitive trust and perceived value on health-related information seeking, sharing and psychological well-being: motivations sought perspective. Telemat. Inform. 2023;79 [Google Scholar]
- Pedone C., Rossi F.F., Cecere A., Costanzo L., Antonelli Incalzi R. Efficacy of a physician-led multiparametric telemonitoring system in very old adults with heart failure. J. Am. Geriatr. Soc. 2015;63(6):1175–1180. doi: 10.1111/jgs.13432. https://www.ncbi.nlm.nih.gov/pubmed/26031737 [DOI] [PubMed] [Google Scholar]
- Perski O., Short C.E. Acceptability of digital health interventions: embracing the complexity. Transl. Behav. Med. 2021;11(7):1473–1480. doi: 10.1093/tbm/ibab048. https://www.ncbi.nlm.nih.gov/pubmed/33963864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollack A.H., Backonja U., Miller A.D., Mishra S.R., Khelifi M., Kendall L., Pratt W. Closing the gap: supporting patients' transition to self-management after hospitalization. Proc. SIGCHI Conf. Hum. Factor Comput. Syst. 2016. 2016:5324–5336. doi: 10.1145/2858036.2858240. https://www.ncbi.nlm.nih.gov/pubmed/27500285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rennke Stephanie, Ranji Sumant R. Transitional care strategies from hospital to home: a review for the neurohospitalist. Neurohospitalist. 2015;5(1):35–42. doi: 10.1177/1941874414540683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salmela Tarja, Valtonen Anu, Lupton Deborah. The affective circle of harassment and enchantment: reflections on the ŌURA ring as an intimate research device. Qual. Inq. 2019;25(3):260–270. [Google Scholar]
- Sekhon M., Cartwright M., Francis J.J. Acceptability of healthcare interventions: an overview of reviews and development of a theoretical framework. BMC. Health Serv. Res. 2017;17(1):88. doi: 10.1186/s12913-017-2031-8. https://www.ncbi.nlm.nih.gov/pubmed/28126032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh H., Tang T., Steele Gray C., Kokorelias K., Thombs R., Plett D., Heffernan M., Jarach C.M., Armas A., Law S., Cunningham H.V., Nie J.X., Ellen M.E., Thavorn K., Nelson M. Recommendations for the design and delivery of transitions-focused digital health interventions: rapid review. JMIR. Aging. 2022;5(2):e35929. doi: 10.2196/35929. https://www.ncbi.nlm.nih.gov/pubmed/35587874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srivastava Anshul, Do Jacquelyn-My, Sales Virna L, Ly Samantha, Joseph Jacob. Impact of patient-centred home telehealth programme on outcomes in heart failure. J. Telemed. Telecare. 2019;25(7):425–430. doi: 10.1177/1357633X18775852. [DOI] [PubMed] [Google Scholar]
- Stefanicka-Wojtas Dorota, Kurpas Donata. eHealth and mHealth in chronic diseases—identification of barriers, existing solutions, and promoters based on a survey of EU stakeholders involved in REGIONS4PERMED (H2020) J. Pers. Med. 2022;12(3):467. doi: 10.3390/jpm12030467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevenson Lynne Warner, Ross Heather J, Rathman Lisa D, Boehmer John P. Remote monitoring for heart failure management at home. J. Am. Coll. Cardiol. 2023;81(23):2272–2291. doi: 10.1016/j.jacc.2023.04.010. [DOI] [PubMed] [Google Scholar]
- Thomas Emma E, Taylor Monica L, Banbury Annie, Snoswell Centaine L, Haydon Helen M, Rejas Victor M Gallegos, Smith Anthony C, Caffery Liam J. Factors influencing the effectiveness of remote patient monitoring interventions: a realist review. BMJ Open. 2021;11(8) doi: 10.1136/bmjopen-2021-051844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tjora Aksel. Routledge; 2018. Qualitative Research As Stepwise-Deductive Induction. [Google Scholar]
- Williams A., Lennox L., Harris M., Antonacci G. Supporting translation of research evidence into practice-the use of Normalisation Process Theory to assess and inform implementation within randomised controlled trials: a systematic review. Implement. Sci. 2023;18(1):55. doi: 10.1186/s13012-023-01311-1. https://www.ncbi.nlm.nih.gov/pubmed/37891671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Medical Association World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–2194. doi: 10.1001/jama.2013.281053. https://www.ncbi.nlm.nih.gov/pubmed/24141714 [DOI] [PubMed] [Google Scholar]
- Zaharova S., Litwack K., Gopalakrishnan S., Ellis J., Saltzberg M.T. Self-management in heart failure: the importance of self-regulation but not complexity of condition. West J. Nurs. Res. 2022;44(4):375–382. doi: 10.1177/0193945921997428. https://www.ncbi.nlm.nih.gov/pubmed/33709833 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.