Abstract
Navigational bronchoscopy is increasingly used to target peripheral pulmonary nodules using electromagnetic navigational platforms (ENB), fluoroscopic navigation, or robotic-assisted bronchoscopy. The selection of equipment largely depends on the availability of technology, expertise, and the characteristics of the nodule and patient. Radial EBUS (r-EBUS) is often combined with these techniques for real-time confirmation of the nodule location. A bronchus sign is considered to have a higher diagnostic yield when biopsy tools can directly reach the nodule. We describe a case series of creating a false airway into the nodule when an eccentric r-EBUS signal is seen to subsequently obtain a concentric signal.
Keywords: peripheral pulmonary nodule, radial EBUS, diagnosis
Introduction
Pulmonary nodules are common, with the prevalence being 8 to 51% in large lung cancer screening trials, and can pose challenges in terms of the diagnostic approach.1,2 While the prevalence of malignancy increases with nodule size, even smaller nodules (size 5 mm to 10 mm) may have a malignancy rate from 6% to 28%, as published in a systematic review.2 In general, computed tomography (CT) guided transthoracic needle aspiration (TTNA) or bronchoscopic biopsies are the preferred techniques, depending on the location, size, and proximity to an airway or vascular structure of the nodule, and especially when risk of surgical complications is high. The American College of Chest Physicians recommends using electromagnetic navigational bronchoscopy (ENB) over conventional bronchoscopy to obtain tissue from peripheral pulmonary nodules when available (Grade IC recommendation) and radial EBUS (r-EBUS) is recommended as an adjunct to confirm the location of the nodule in real time (Grade IC recommendation).3 The diagnostic yield for a peripheral nodule is higher when the r-EBUS probe is within the lesion as opposed to being adjacent to it.4 We present two cases in which a false airway was created into the nodule to improve the r-EBUS signal from eccentric to concentric during ENB.
Case Reports
These cases were reviewed and presented in accordance with the Institutional Review Board at the University of Minnesota, Minneapolis, MN, USA. Informed consent prior to the procedures allows de-identifiable information related to patient care to be used for publication. Written consents for the procedures and publication of this manuscript were obtained.
Case 1
An 84-year-old woman was referred to pulmonary clinic for further evaluation of an incidentally discovered pulmonary nodule. The patient had a medical history of moderate COPD (FEV1 of 1.2 L, 65% of predicted) requiring maintenance treatment with a long-acting B agonist and an inhaled steroid. In addition, she carried a diagnosis of rheumatoid arthritis, which was treated with methotrexate and low-dose prednisone. She was a former smoker, with a 25 pack-year smoking history. The pulmonary nodule was first visualized in 2016 on a low-dose lung cancer screening chest CT, measuring 5 mm in the anterior segment of the right upper lobe. A 6-month follow CT scan did not reveal any changes in the size or appearance of the nodule. The patient was lost to follow-up until she had COVID-19 infection and chest CT performed in April 2021 showed that the nodule measured 14 × 12 mm with lobulation. She had a long recovery from the COVID infection and underwent a follow-up chest CT in February 2022 when the nodule measured 14 mm × 17 mm and preserved its lobulated shape (Figure 1). When the patient was examined in pulmonary clinic, different diagnostic options were discussed. Owing to its central location and proximity to an airway of the nodule, the bronchoscopic approach was determined to be the best option over CT-guided biopsy or surgical biopsy. The procedure was performed in the operating room under general anesthesia for mediastinal staging with linear endobronchial ultrasound (L-EBUS) and electromagnetic navigational bronchoscopy (Veran Medical Technologies Inc., St Louis, MO, USA) for nodule biopsy. L-EBUS examination of lymph node stations did not reveal any nodes >5 mm (short diameter); therefore, nodal biopsies were not performed. After reaching the nodule with ENB, the ultrasonographic image from r-EBUS showed an eccentric view (Figure 2). Thus, we retracted the r-EBUS and created a hole and path with a PeriView FLEX needle (Olympus Medical Systems Corp., Tokyo, Japan) into the nodule (Figure 3). The needle was advanced three times to a depth of 1cm based on CT measurement. Subsequently, we advanced the r-EBUS through the false airway (Figure 4) and obtained a concentric view of the nodule (Figure 5). Mini forceps (CoreDx, Boston Scientific Corporation, Marlborough, MA, USA) were advanced and used to perform multiple biopsies of the nodule through the false airway. Rapid evaluation of the forceps biopsies (touch prep) revealed the presence of fatty material and mesenchymal tissue. The final cytology report confirmed the diagnosis of hamartoma.
Figure 1.

14 x 17mm right upper lobe nodule.
Figure 2.
Eccentric radial EBUS view of right upper lobe nodule.
Figure 3.

Creation of false airway with needle.
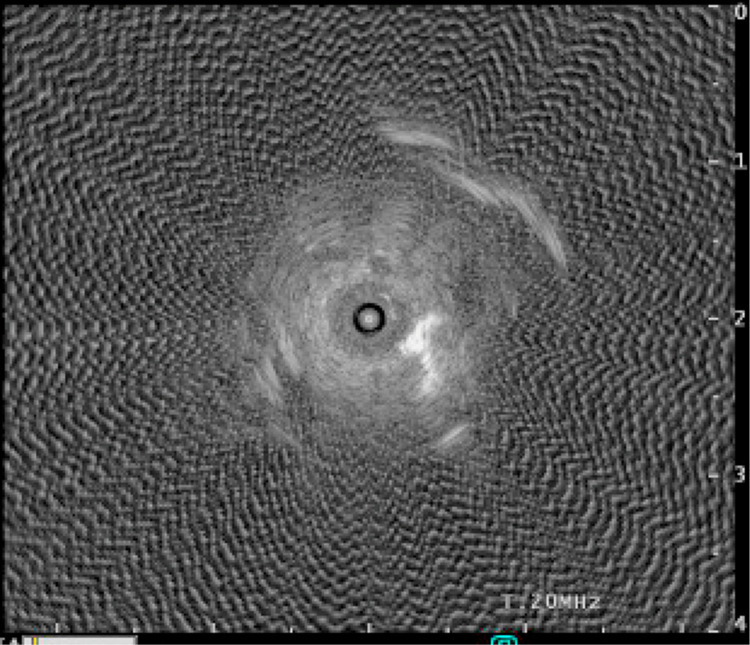
Figure 4.

Radial EBUS advanced through false airway.
Figure 5.
Concentric radial EBUS view of right upper lobe nodule through false airway.
Case 2
A 63-year-old man with a history of stage 4 chronic kidney disease was being evaluated for kidney transplantation. As part of the pre-transplant workup, the patient underwent a chest CT scan to evaluate existing pulmonary nodules. The patient was a former smoker (40 pack-year). The patient had normal spirometry results and diffusion capacity on pulmonary function testing. His medical history included coronary artery disease, gout, and hypertension. His pulmonary nodule, which was round and non-calcified and located in the right middle lobe, initially measured 5 mm in March 2021 but had increased in size to 7 mm (Figure 6) on repeat chest CT in March 2022. Given the need to rule out malignancy before kidney transplantation and his risk factors for lung cancer, the patient was discussed in a multidisciplinary thoracic oncology meeting to determine the diagnostic approach. The patient underwent L-EBUS for mediastinal staging and navigational bronchoscopy of the lung nodule. Two mediastinal nodes (stations 7 and 11L) were negative for malignancy by the on-site cytology evaluation. After navigation was performed to the lung nodule, an eccentric r-EBUS view was obtained (Figure 7). A false airway was created using the PeriView FLEX needle (Olympus Medical Systems Corp., Tokyo, Japan). The needle was advanced three times to a depth of 5mm based on CT measurement. Insertion of the r-EBUS through the false airway showed a concentric view (Figure 8). Mini forceps (CoreDx, Boston Scientific Corporation, Marlborough, MA, USA) were advanced through the false airway and multiple biopsies were performed. On-site touch prep evaluation revealed lesional tissue, which was subsequently reported to be a neuroendocrine tumor.
Figure 6.

7mm right middle lobe nodule.
Figure 7.
Eccentric radial EBUS view of right middle lobe nodule.
Figure 8.
Concentric radial EBUS view of right middle lobe nodule through false airway.
Discussion
The diagnosis of peripheral pulmonary nodules remains a significant challenge, despite advancements in bronchoscopic technologies. In a review by DiBardino et al, CT-guided TTNA had a diagnostic accuracy of 92.1% and pneumothorax rate of 20.5%.5 In contrast, a recent meta-analysis done of different navigational bronchoscopy techniques showed a diagnostic yield of 70.3% of ENB and 76.5% with the newer technology of robotic bronchoscopy with an overall pneumothorax rate of 2.5%.6 A positive bronchus sign on chest CT, where a bronchus is visualized going into the nodule, is shown to increase the diagnostic yield in the bronchoscopic approach in a study using ENB technology from 78.3% to 88%.7 Although the diagnostic yield is lower with bronchoscopic biopsy, mediastinal staging for malignant pulmonary nodules can be completed during the same procedure, and the pneumothorax rate is much lower. R-EBUS has been used as an adjunct and confirmatory tool in navigational and robotic bronchoscopies. Two single-center studies showed that the diagnostic yield was increased with the addition of r-EBUS to ENB compared with ENB alone.8,9 A meta-analysis of r-EBUS showed that the position of the radial probe with regard to the lesion affected the diagnostic yield, with an increased yield when the r-EBUS probe was within the lesion compared to when it was adjacent to it.4 The creation of a false airway has not been well adopted by interventional pulmonologists. Hearth et al studied a navigational system that does not have an electromagnetic navigation component, but instead reconstructs the airways and major vessels from the CT images. The user is guided to within 3 mm of the nodule and creates a tunnel using a core needle, followed by the insertion of a sheath through the lung parenchyma in 10 of 12 patients, reaching the lesion with a 100% diagnostic yield.10 Although this study did not utilize r-EBUS confirmation of the lesion, all patients with successful tunneling were diagnosed under fluoroscopic guidance. With these studies in mind, we combined r-EBUS with ENB and presented a novel and easy technique to improve the position of the radial probe to improve diagnostic yield. We did not encounter any complications such as bleeding or pneumothorax. There was no visible blood vessel present between the nodule and airway on CT images in either of these cases.
Conclusion
The creation of a false airway leading to a higher diagnosis with r-EBUS confirmation is feasible, but further randomized trials would help to identify the limitations of this technique and compare its diagnostic value to other available technologies, as well as bleeding and pneumothorax risk.
Disclosure
The authors report no conflict of interest in this work.
References
- 1.Khan T, Usman Y, Abdo T, Chaudry F, Keddissi JI, Youness HA. Diagnosis and management of peripheral lung nodule. Ann Transl Med. 2019;8(15):348–363. doi: 10.21037/atm.2019.03.59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wahidi MM, Govert JA, Goudar RK, Gould MK, McCrory DC. American College of Chest Physicians. Evidence for the treatment of patients with pulmonary nodules: when is it lung cancer?: ACCP evidence-based clinical practice guidelines. Chest. 2007;1323 Suppl:94S–107S. doi: 10.1378/chest.07-1352 [DOI] [PubMed] [Google Scholar]
- 3.Detterbeck FC, Lewis SZ, Diekemper R, et al. Executive summary: diagnosis and management of lung cancer, 3rd ed: American college of chest physicians evidence-based clinical practice guidelines. Chest. 2013;143:7S–37S. doi: 10.1378/chest.12-2377 [DOI] [PubMed] [Google Scholar]
- 4.Ali MS, Trick W, Mba BI, Mohananey D, Sethi J, Musani AI. Radial endobronchial ultrasound for the diagnosis of peripheral pulmonary lesions: a systematic review and meta-analysis. Respirology. 2017;22(3):443–453. doi: 10.1111/resp.12980 [DOI] [PubMed] [Google Scholar]
- 5.DiBardino D, Yarmus LB, Semaan R. Transthoracic needle biopsy of the lung. J Thorac Dis. 2015;7(4):S304–S316. doi: 10.3978/j.issn.2072-1439.2015.12.16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kops SEP, Heus P, Korevaar DA, et al. Diagnostic yield and safety of navigation bronchoscopy: a systematic review and meta-analysis. Lung Cancer. 2023;180:107196. doi: 10.1016/j.lungcan.2023.107196 [DOI] [PubMed] [Google Scholar]
- 7.Raval AA, Amir L. Community hospital experience using electromagnetic navigation bronchoscopy system integrating tidal volume computed tomography mapping. Lung Cancer Manag. 2016;5:9–19. doi: 10.2217/lmt-2015-0007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ozgul G, Cetinkaya E, Ozgul MA, et al. Efficacy and safety of electromagnetic navigation bronchoscopy with or without radial endobronchial ultrasound for peripheral lung lesions. Endosc Ultrasound. 2016;5(3):189–195. doi: 10.4103/2303-9027.183979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Song JY, Shin SH, Yoo H, et al. Efficacy of combining multiple electromagnetic navigation bronchoscopy modalities for diagnosing lung nodules. J Clin Med. 2022;11(24):7341. doi: 10.3390/jcm11247341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Herth FJ, Eberhardt R, Sterman D, Silvestri GA, Hoffman H, Shah PL. Bronchoscopy transparenchymal nodule access: first in human trial of a novel procedure for sampling solitary pulmonary nodules. Thorax. 2015;70:326–332. doi: 10.1136/thoraxjnl-2014-206211 [DOI] [PubMed] [Google Scholar]