ABSTRACT
Patients with frontal fibrosing alopecia (FFA) can present with facial micropapules which histologically represent vellus hair lichen planopilaris (LPP). Noninflammatory vellus hair LPP in the absence of FFA is rarely reported. The report describes noninflammatory vellus hair LPP presenting as symmetrical facial micropapules in the absence of clinical signs of FFA.
Keywords: Facial eruption, facial micropapules, frontal fibrosing alopecia, lichen plano pilaris, vellus hair
INTRODUCTION
Certain facial eruptions can be challenging to diagnose and manage. Classification of some such eruptions may be difficult despite meticulous clinicopathological correlation. Lichen planopilaris (LPP) can involve both terminal and vellus hair. Facial papular rash resulting from vellus hair LPP in patients with frontal fibrosing alopecia (FFA) has been described.[1] The author has studied clinical and histopathological characteristics of the facial rash of five female patients who presented to his practice with a progressively worsening, curious facial eruption between 2011 and 2013.[2] There was a striking clinical similarity in the morphology of the rash in all patients. None of the patients displayed clinical signs of FFA or any evidence of body hair loss despite a 9-year follow-up. The author presents the clinical and demographic details of patients [Table 1] and the histopathological characteristics of the rash.
Table 1.
Demographics and clinical features
| Age at presentation (years) | Onset of symptoms (years) at initial presentation | Initial histological suggestion | Scalp and eyebrow involvement | Body vellus hair involvement |
|---|---|---|---|---|
| Mid 30’s | 7 | LPP | - | - |
| Late 30’s | 20 | Sebaceous gland hyperplasia | - | - |
| Mid 40’s | 6 | Fibrofolliculomas | - | - |
| Mid 20’s | 1 | Rosacea | - | - |
| Mid 40’s | 3 | Rosacea | - | - |
LPP – Lichen planopilaris
CASE SERIES
Case 1
A woman in her mid-30s was referred with a 7-year history of an asymptomatic facial eruption. She gave a history of “sensitive skin” but denied previous rashes, excessive sun exposure, or any significant medical history. She was not on any medications although had taken antidepressant citalopram in the past. Examination revealed a symmetrical micropapular eruption affecting the temples, upper neck, and cheeks, though with some sparing laterally over the cheeks [Figure 1a]. There was no evidence of eyebrow, scalp, or body hair loss. A skin biopsy from the affected site on the cheek showed features of follicular loss characterized by follicular streamers and follicular stelae within the dermis. Relative expansion of sebaceous units was also present. Perifollicular inflammation centered at the level of infundibulum was seen along with perifollicular fibrosis [Figure 2a].
Figure 1.
Clinical presentation in. (a) Case 1-micropapular eruption with sparing over the mid to lateral cheeks, (b) Case 2-coalescing skin-colored papules on the cheeks with sparing of the mid-cheeks, (c) Case 3-skin-colored micropapules on the chin, (d) Case 4-micropapular eruption on the cheeks with evidence lack of involvement of lateral cheeks, (e) Case 5-Skin-colored papules scattered on the cheeks
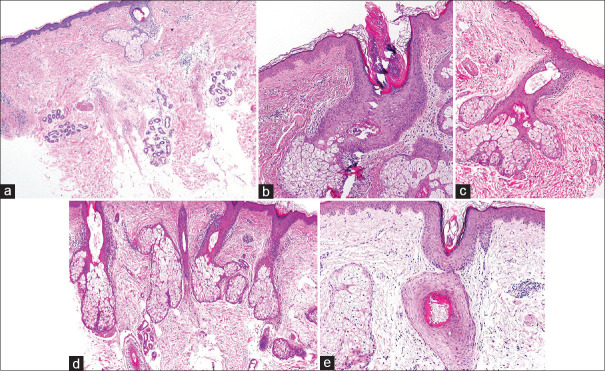
Figure 2.
Corresponding skin biopsies (All H and E, ×100, vertical sectioning) showing. (a) Case1 - Perifollicular inflammation and perifollicular fibrosis with follicular loss and relative expansion of sebaceous units, (b) Case 2 - Mild perivascular perifollicular lymphocytic inflammation and fibrosis with a reduction in the number of hair follicles giving a ‘pseudo sebaceous gland hyperplasia’appearance, (c) Case 3 - Subtle lichenoid inflammation is present at the level of the infundibulum with associated dilatation of the hair follicle, (d) Case 4 - Lichenoid inflammation affecting the vellus hair follicles at the level of the infundibulum, (e) Case 5 - Vellus hair follicular distortion with subtle inflammation and perifollicular fibrosis
Case 2
A woman in her late 30s gave a 20-year history of a symmetrical papular eruption on the face associated with mild pruritus. A short trial of topical Retin A cream had been ineffective. Other than childhood asthma and eczema, there was no contributory medical history. Clinical examination revealed coalescing skin-colored papules affecting the temples and lateral cheeks with sparing of the mid-cheeks though involving the chin and upper neck [Figure 1b]. Eyebrows, scalp, and body hair involvement were not seen. Punch biopsy from the left cheek showed slight prominence of sebaceous units and mild perivascular superficial chronic inflammation and although the features were subtle, overall they were felt to most suggestive of sebaceous gland hyperplasia. This, however, did not correspond to the clinical presentation. A review of the skin biopsy showed mild perivascular perifollicular lymphocytic inflammation and fibrosis with an overall reduction in the number of hair follicles giving a “pseudo-sebaceous gland hyperplasia” appearance [Figure 2b].
Case 3
A woman in her mid-40s presented with a 6-year history of a symmetrical micropapular eruption affecting the paranasal, periorbital, and chin predominantly, with sparing over the mid to lateral cheeks [Figure 1c]. No relevant past medical history was forthcoming. Skin and hair examination was otherwise unremarkable. A clinical diagnosis of multiple fibrofolliculomas was considered at the time of presentation. Histology from a submental papule showed several follicular units with some mild superficial inflammation, though in deeper sections, there were some well-defined granulomas and EVG staining raised the possibility of elastolytic granuloma though this did not fit with the clinical features. Review of histology showed subtle lichenoid inflammation at the level of the infundibulum with associated dilatation of the hair follicle and evidence of follicular loss with vascular stelae at the site of a previous vellus hair follicle [Figure 2c].
Case 4
This patient presented in her mid-20s with a 13-month history of a mildly pruritic micropapular facial eruption affecting predominantly the cheeks and chin with evidence of sparing over the lateral cheeks [Figure 1d]. There were no clinical signs of FFA, and no loss of eyebrow or body hair was present. There was no history of flushing or inflammatory papules. A clinical diagnosis of colloid milia was considered. Biopsy of the left cheek revealed perifollicular chronic inflammation, solar elastosis, Demodex species, and superficial vascular ectasia raising the possibility of rosacea. Histology review showed lichenoid inflammation affecting the vellus hair follicles at the level of the infundibulum in the adjacent follicular units [Figure 2d].
Case 5
This woman presented in her mid-40s with a 3-year history of an asymptomatic widespread micropapular eruption over the temples, cheeks, and neck [Figure 1e]. A clinical diagnosis of multiple syringomas or eruptive vellus hair cysts was considered. Biopsy showed a minor change with superficial dermal telangiectasia and a minor nonspecific upper dermal lymphocytic infiltrate and was thought possibly to represent rosacea. On review of the skin biopsy, vellus hair follicular distortion consisting of subtle inflammation, perifollicular fibrosis, and squamatization of the follicular epithelium was apparent [Figure 2e].
COMMENT
The strikingly similar, symmetrically distributed facial micropapules in our patients had been a diagnostic dilemma with clinical and histological diagnoses of fibrofolliculomas, rosacea, sebaceous gland hyperplasia, and colloid milium being considered but not confirmed due to discordance in clinical and histopathological findings. Detailed histopathological review of all cases and interpretation of these results in light of similar clinical findings point to a unifying diagnosis of vellus hair LPP.
Vellus hair LPP has been reported in association with FFA.[1] However, none of the patients in this series displayed any clinical signs of FFA. The author has followed up on these patients for 9 years and none of them have thus far developed FFA nor demonstrated any visible changes of LPP in their eyebrows, eyelashes, axillary, or body pubic hair, which are commonly affected in patients with FFA.[3,4]
The duration of the micropapules in our patients ranged from 1 to 20 years, with a median of 6 years. None of the patients developed additional scalp, eyebrow, or extrafacial papules or alopecia suggestive of LPP. It is likely, therefore, that these patients have a pure vellus hair variant of LPP, with sparing of the terminal scalp or eyebrow hair that may remain uninvolved throughout the course of the disease. In addition, this pure-vellus hair variant of LPP may have a predilection for facial vellus hair and may not affect body vellus hair.
The patients were in their mid-20s to mid-40s at presentation, with the youngest being 19 years old at disease onset. This is in contrast to the age of onset of FFA which usually affects middle-aged or postmenopausal women.[1,5] This observation also lends support to the hypothesis that pure vellus hair LPP may be a distinct condition which may not progress to FFA.
Four years after the first description of our case series, Van de Maele et al. published a case series of five female patients with very similar clinical features of facial micropapules without any evidence of FFA.[6] In addition, like our patients, all patients were premenopausal, with an age range from 30 to 44 years old.
Patients in this study were referred with papular lesions on the face which had been progressively worsening. Before the diagnosis of vellus hair, LPP was made case 2 underwent a patch test with the carbon dioxide laser, but this did not bring about any discernible improvement. Two patients were commenced on hydroxychloroquine 200 mg bd which stabilized their condition but did not result in reversal of the facial papules.
The patients discussed here have a distinct dermatological condition that affects young women and presents as symmetric facial micropapules. While histology favors a diagnosis of vellus hair LPP in all patients, the absence of other skin findings and especially a lack of association with FFA supports this view. This condition may not be uncommon but underdiagnosed especially as the clinical signs can be subtle and patients may either not present to their physicians or may dismiss the signs as textural changes. Furthermore, as was the case in these patients, histopathological signs are usually very subtle and a high index of clinical suspicion and good collaboration between the dermatologists and histopathologists is necessary to arrive at the correct diagnosis.
In summary, five female patients with an asymptomatic to mildly pruritic, progressively worsening, strikingly similar facial rash comprising of small, closely grouped, skin-colored to yellowish papules, and presenting on both cheeks with symmetric islands of sparing have been described. None of the patients had any clinical features of FFA at presentation nor have they developed any such features despite 9-year follow-up. Review of skin biopsies in all patients showed lichenoid inflammation of varying severity at the level of the infundibulum and in some cases, destruction of vellus hair follicles-confirming the diagnosis of vellus hair LPP.
Given the strikingly similarity in the morphology of the facial eruption in all our patients and the characteristic histological features of vellus hair LPP, the author proposes the term Symmetrical Idiopathic MicroPapular faciaL Eruption or SIMPLE which may be used to describe this distinct facial rash in patients in the absence of clinical features of FFA.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient (s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initial s will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The author is indebted to Drs. L Jamieson and L Motta for their help in the histological interpretation of biopsies.
REFERENCES
- 1.Donati A, Molina L, Doche I, Valente NS, Romiti R. Facial papules in frontal fibrosing alopecia: Evidence of vellus follicle involvement. Arch Dermatol. 2011;147:1424–7. doi: 10.1001/archdermatol.2011.321. [DOI] [PubMed] [Google Scholar]
- 2.Newsham J, Motta L, Jamieson LA, Madan V. CPC05 symmetrical idiopathic micropapular facial eruption or SIMPLE: A case series describing a new, distinct clinical entity characterized by lichen planopilaris affecting vellus hairs in the absence of frontal fibrosing alopecia. Br J Dermatol. 2014;171(Suppl 1):13–4. [Google Scholar]
- 3.Moreno-Ramírez D, Camacho Martínez F. Frontal fibrosing alopecia: A survey in 16 patients. J Eur Acad Dermatol Venereol. 2005;19:700–5. doi: 10.1111/j.1468-3083.2005.01291.x. [DOI] [PubMed] [Google Scholar]
- 4.Samrao A, Chew AL, Price V. Frontal fibrosing alopecia: A clinical review of 36 patients. Br J Dermatol. 2010;163:1296–300. doi: 10.1111/j.1365-2133.2010.09965.x. [DOI] [PubMed] [Google Scholar]
- 5.Kossard S, Lee MS, Wilkinson B. Postmenopausal frontal fibrosing alopecia: A frontal variant of lichen planopilaris. J Am Acad Dermatol. 1997;36:59–66. doi: 10.1016/s0190-9622(97)70326-8. [DOI] [PubMed] [Google Scholar]
- 6.Van de Maele B, Vossaert K, Lanssens S, Haspeslagh M, De Schepper S. Facial lichen planopilaris: A separate entity or not?A case series. Int J Trichology. 2018;10:183–5. doi: 10.4103/ijt.ijt_5_18. [DOI] [PMC free article] [PubMed] [Google Scholar]