ABSTRACT
Lower leg hair removal is the method of reducing unwanted lower leg hair. Various technologies for lower leg hair removal include Intense Pulsed Light (IPL), alexandrite laser, and neodymium-doped yttrium aluminum garnet (Nd: YAG) laser. Conventional techniques are abandoned because effectiveness of the latest technological therapies has a longer period with minimal side effects. The comparison of successful treatment among IPL, alexandrite laser, and Nd: YAG laser for lower leg hair removal. Two patients, male and female, 28 years old, Fitzpatrick IV skin type. Three areas in the lower legs are marked for IPL 695 nm, fluence 15 J/cm2, pulse duration 60 ms; alexandrite 755 nm, fluence 3 J/cm2, pulse duration 2 ms, long-pulsed Nd: YAG 1064 nm, fluence 32 J/cm2, pulse duration 60 ms. IPL for 3 sessions at 2-week intervals. The alexandrite and Nd: YAG lasers for 3 sessions at 4-week intervals. Successful parameters with hair reduction and Visual Analog Scale (VAS) can be seen from photography and dermoscopy before and after therapy. In the first case, the most effective reduction terminal hair after IPL (95,1%), alexandrite (91,02%) and Nd: YAG (79,69%), respectively. In the second case, the most effective reduction of terminal hair after alexandrite (91,02%), Nd: YAG (79,69%), and IPL (20%), respectively. Hyperpigmentation and the highest VAS score (6–7) are found in the area treated with alexandrite lasers of two patients. Two patients have decreased Dermatology Life Quality Index scores. Nd: YAG laser may be better suitable for both sexes with minimal side effects. The limitation of this study is the smaller subject group and limited session.
Keywords: Alexandrite, intense pulse light, lower leg hair removal, neodymium-doped yttrium aluminum garnet
INTRODUCTION
The excessive hair growth or unwanted hair in women and men is a problem that is quite often encountered. Around 81% of males and 11% of females in the world have problems with unwanted hair.[1,2] Research in New Zealand (2013) reported that 13% of males and 93% of females wanted to eliminate unwanted hair in the lower leg. Unwanted hair can cause emotional stress and disturbances in the quality of life.[1,2] Unwanted hair is one of the problems in cosmetic dermatology. Various methods are used to remove unwanted hair. However, there is no optimal result yet.[3,4]
Method hair removal such as shaving, waxing, and removing is a cheap and easy method, but temporary and requires repeated actions.[1,5,6] Therapy modalities for hair removal are expected to last longer and even permanently.[4,5,7] Currently, the use of lasers for hair removal is growing and main options for handling unwanted hair.[6,7]
The effectiveness of hair removal is determined by a reduction in the number of terminal hairs, color changes, and the terminal hair become finer and lighter. In 1995, the Food and Drug Administration (FDA) has legalized the use of laser and light technology for hair removal. Some lasers that give improvement for hair removal such as ruby laser (694 nm), alexandrite (755 nm), diode (800–1000 nm), intense pulsed light (IPL) (550–1200 nm), and neodymium-doped yttrium aluminum garnet (Nd: YAG) laser (1064 nm). These lasers have their advantages and disadvantages.[1]
We report a case series of two patients with unwanted hair in both lower limbs. The alexandrite (755 nm), IPL (695 nm), and Nd: YAG (1064 nm) laser were performed. This case report aims to compare the three treatment modalities by assessing the decrease in the number of lower limb hairs, Visual Analog Scale (VAS), Dermatology Life Quality Index (DLQI), as well as side effects.[2]
CASE SERIES
Case 1
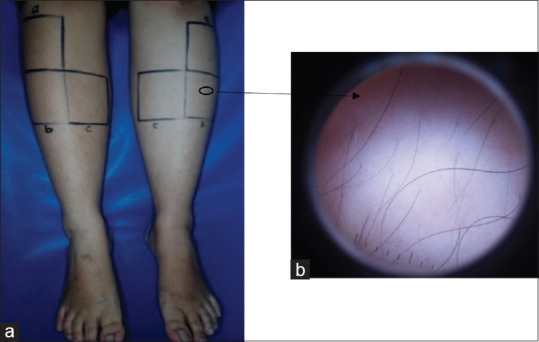
A 28-year-old male, went to the Dermatology and Venereology Polyclinic of Dr. Mohammad Hoesin General Hospital Palembang for lower leg hair removal. The patient complains that the lower leg hair is too long and disturbing appearance. The patient has never shaved his lower leg hair with a razor and has never taken any action to hair removal lower limbs before, like waxing, or lasers. The patient has no contraindications for laser surgery. General physical examination status was within the normal limits. Dermatological status in the bilateral tibial region contains terminal hairs, black, curly, medium thickness coarse, discrete. Dermoscopy examination revealed terminal and vellus hairs in the number of 1–2 per follicle, black in color and uniform in shape, depicting normal hair [Figure 1a and b]. Mapping of hair distribution was assessed manually using transparent mica plastic and tabulated, and a DLQI assessment was carried out. Patients’ consent forms haave been obtained for all patients.
Figure 1.

(a) Hair in the bilateral tibial region of the first patient when baseline (b) result dermoscopy examination in the left tibial region
Case 2
A 28-year-old female, went to the Dermatology and Venereology Polyclinic of Dr. Mohammad Hoesin General Hospital Palembang for lower leg hair removal. The patient complains of lower leg hair that interferes with appearance. History of shaving 10 years ago. The patient has never done waxing or previous laser action. The patient has no contraindications for laser surgery. General physical examination status was within the normal limits. Dermatological status in the bilateral tibial region contains terminal hairs, black, straight, smooth, and discrete thickness. Dermoscopy examination revealed terminal and vellus hairs in the number of 1–2 per follicle, black in color and uniform in shape, depicting normal hair; [Figure 2a and b]. Mapping of hair distribution was assessed manually using transparent mica plastic and tabulated, and DLQI assessment was carried out.
Figure 2.
(a) Hair in the bilateral tibial region of the second patient when baseline (b) results of dermoscopy examination in the left tibial region
Procedure
We diagnosed two patients with bilateral tibial unwanted hair (L68.2). Management with counseling, education, and information regarding the physiological state of hair on both lower limbs, treatment plans, side effects, and results after therapy. Getting informed consent before the action of treatment.
The patient was planned for IPL at 2-week intervals, alexandrite laser, and Nd: YAG laser at 4 weeks interval for 3 sessions. Evaluation of follow-up observations in the form of an assessment of the decrease in the number of hairs, side effects, and quality of life after the current procedure baseline, 1st week, 2nd, 3rd, 4th, and 6th month after the last session [Tables 1-3].
Table 1.
Observation clinical feature and dermoscopic of two patients in baseline, and 4th week
| Time | Case 1 | Case 2 |
|---|---|---|
| Baseline |
 After shaving lower leg hair |
 After shaving lower leg hair |
 Dermoscopic |
 Dermoscopic |
|
| 10 min after IPL, alexandrite laser, and Nd: YAG laser in first session |

|

|
| 4th week |

|

|
 Dermoscopic after IPL |
 Dermoscopic after IPL |
|

|
 Dermoscopic after alexandrite laser |
|
 Dermoscopic after Nd: YAG laser |
 Dermoscopic after Nd: YAG laser |
|
| 10 min after IPL, alexandrite laser, and Nd: YAG laser in second session |

|

|
IPL: Intense pulsed light, Nd: YAG: Neodymium-doped yttrium aluminum garnet
Table 3.
The number of terminal hair in baseline, 1st week, 2nd week, 3rd week, 4th week (case 2)
| Area | The number of terminal hair | ||||
|---|---|---|---|---|---|
|
| |||||
| Baseline | 1st week | 2nd week | 3rd week | 4th week | |
| Tibialis dekstra (A) | 61 | 57 | 50 | 42 | 40 |
| Tibialis dekstra (B) | 56 | 45 | 20 | 16 | 12 |
| Tibialis dextra (C) | 66 | 64 | 24 | 18 | 15 |
| Tibialis sinistra (A) | 90 | 84 | 59 | 48 | 31 |
| Tibialis sinistra (B) | 79 | 43 | 26 | 20 | 16 |
| Tibialis sinistra (C) | 67 | 34 | 26 | 21 | 18 |
| Total | 419 | 327 | 205 | 165 | 132 |
Table 2.
The number of terminal hair in baseline, 1st week, 2nd week, 3rd week, 4th week (case 1)
| Area | The number of terminal hair | ||||
|---|---|---|---|---|---|
|
| |||||
| Baseline | 1st week | 2nd week | 3rd week | 4th week | |
| Tibialis dekstra (A) | 238 | 50 | 41 | 6 | 2 |
| Tibialis dekstra (B) | 156 | 62 | 24 | 17 | 14 |
| Tibialis dextra (C) | 133 | 75 | 59 | 30 | 27 |
| Tibialis sinistra (A) | 174 | 89 | 46 | 9 | 3 |
| Tibialis sinistra (B) | 163 | 66 | 29 | 16 | 15 |
| Tibialis sinistra (C) | 141 | 85 | 46 | 25 | 22 |
| Total | 1005 | 472 | 245 | 103 | 83 |
For preparing the treatment, shave the hair of both lower limbs 3 days before the procedure. In the bilateral tibial region is divided into three squares, starting 2 cm below the patella to the inferior medial tibial region with a length of 7 cm on each side. Each box marked with the letters a, b, c, indicates the laser and IPL used, including IPL with single pulse mode, filter 695 nm, influence 15 J/cm2, pulse duration 60 ms (a); alexandrite laser filter 755 nm, influence 3 J/cm2, pulse duration 2 ms (b), Nd: YAG laser filter 1064 nm, influence 32 J/cm2, pulse duration 60 ms (c). The area to be treated is cleaned with alcohol swabs. Given lidocaine cream 2.5% + prilocaine 2.5% occlusion 60 min on the lesion. After topical anesthesia, the area to be treated is cleaned using gauze. The patient’s eyes are covered with special laser light protection glasses. Performed IPL, alexandrite laser, and Nd: YAG laser. After the treatment, compressing use an ice pack on the laser-treated area for 15 min. Mometasone furoate 0.1% cream every 12 h on the skin for 3 days.
In the first patient, after the first and second sessions of IPL, the side effects were pain and heat with a VAS score of 5. After the first session of alexandrite laser treatment, side effects such as erythema and perifollicular edema were found which disappeared 3 days later with a VAS score of 7. One week posttreatment alexandrite laser, hyperpigmentation, and itching were found. Four weeks after the alexandrite laser treatment, the hyperpigmentation was partially reduced. After the Nd: YAG laser treatment, side effects were found in the form of pain with a VAS score of 3. Before the procedure, the patient’s DLQI score was 5. After 4 weeks of treatment, the patient’s DLQI score was 1.
In the second patient, after the first and second sessions of IPL, side effects were pain and heat with VAS score of 4. After the first session of alexandrite laser treatment, side effects were erythema with a VAS score of 6. One week after alexandrite laser treatment, hyperpigmentation was found. Three weeks after the alexandrite laser procedure, the hyperpigmentation was partially covered with crusts. Four weeks after the alexandrite laser treatment, the crusting was reduced, the hyperpigmentation was partially reduced. After the Nd: YAG laser treatment, side effects were pain with a VAS score of 3. Before the procedure, the patient’s DLQI score was 6. After 4 weeks of treatment, the patient’s DLQI score was 1.
DISCUSSION
Unwanted hair is excess hair growth that is triggered by various causes. Commonly, unwanted hair is caused by normal conditions, such as puberty, pregnancy, and menopause.[1] Terminal hair growth in males and females is influenced by androgen hormones released through the ovaries and adrenal glands. Several diseases can cause excess hair growth, such as polycystic ovary syndrome, Cushing’s syndrome, and adrenal tumors. Unwanted hair is more experienced by males than females in the armpit and leg area.[2,7,8] Two patients, a 28-year-old male and female went to the Cosmetic Dermatology Polyclinic of Dr. Mohammad Hoesin general hospital Palembang with complaints to remove unwanted hair on both lower limbs. Both patients had Fitzpatrick IV skin type. The first patient had curly hair texture, black color, and medium thickness. The second patient has straight hair texture, black color, and smooth.
FDA legalizes the use of laser and light technology for hair removal in 1995, tools that can be used such as the ruby laser (694 nm), the alexandrite laser (755 nm), diode laser (800–1000 nm), laser Q-switched, long-pulsed Nd: YAG (1064 nm), and IPL (500–1200 nm).[1,9,10] Laser working mechanism hair removal, namely photothermal, photomechanical, and photochemical. The photothermal energy of the laser causes an increasing temperature of the hair bulb so thermal destruction of the hair follicle happened. Photothermal destroys hair follicles through a selective photothermal process, which is a mechanism that damages the pigmented target structure of melanin in the hair shaft, which absorbs energy from certain wavelengths. Photomechanical energy initiates the shock waves and photochemical energy is generated by free radicals.[11]
The ideal patient for laser surgery hair removal has dark terminal hair, fair skin, and normal hormonal status. This affects the response to therapy. Fitzpatrick IV-VI skin types have an increase in epidermal melanin that affects the melanin chromophore of the bulb and hair shaft, so side effects are more common. Straight and fine hair has less pigment, so it is less responsive to laser hair removal.[11]
The Nd: YAG (1064 nm) laser is the safest laser for Fitzpatrick IV-VI type dark skin patients with black hair, because of its higher wavelength, resulting in less absorption of melanin. This laser has a high wavelength so that it can penetrate deeper into the dermis and reduce the risk of damage to melanin in the epidermis. The shorter wavelength, the higher absorption by melanin causing the risk of side effects to occur in dark-skinned patients. Alexandrite laser (755 nm) is the choice for patients with Fitzpatrick skin types I to IV, also the best choice for thin and fine hair. IPL (400–1200 nm) is polychromatic, incoherent, can be used on Fitzpatrick skin types I-VI with large spot sizes so that the action on large areas can be done more quickly but require more therapy sessions than lasers to achieve the therapeutic target.[12,13]
Before the treatment of hair removal, the hair is shaved. Lower leg hair is shaved 2–3 days before the procedure hair removal is performed so that the visible size of 1–2 mm above the skin during the procedure.[9,12] Mustafa assessed that hair shaved before laser hair removal causes a higher laser power to be absorbed into the skin layer than unshaven ones.[14] Both patients had their lower leg hair shaved 3 days before the procedure so the laser power could be optimized.
Karaca et al. assessed the IPL ratio (650–950 nm), spot size 3 mm × 1 mm, pulse 30s, influence 1–7 J/cm2; alexandrite laser (755 nm), spot size 5 mm, pulse 2 ms, influence 1–32 J/cm2; and Nd: YAG (1064 nm) laser, spot size 6 mm, pulse 45–60 ms, influence 30–150 J/cm2 for unwanted hair treatment of bilateral tibialis in 25 women, performed in 3 sessions at 6-week intervals.[15] The effectiveness of alexandrite laser (755 nm) and long-pulsed Nd: YAG (1064 nm) at 4–6 week intervals, and IPL (695 nm) at 2–12 week intervals gave significant therapeutic results.[12,16,17]
Both patients were treated by comparing the three treatment modalities using an area 7 cm × 7 cm square in the bilateral tibial region. Each box marked with the letters a, b, and c indicates the laser and IPL used. IPL measures 695 nm (box a), spot size 3 mm × 1 mm pulse 60 s, influence 15 J/cm2; alexandrite laser 755 nm (box b), spot size 5 mm, pulse 2 ms, influence 3 J/cm2; and Nd: YAG 1064 nm (box c), spot size 6 mm, pulse 60 ms, influence 32 J/cm2. The IPL procedure in 3 sessions with an interval of 2 weeks, alexandrite laser, and Nd: YAG 3 sessions with an interval of 4 weeks.
Goh assessed the ratio of long-pulsed Nd: YAG laser to IPL as much as 1 session to the patient unwanted hair on the face, armpits, and lower limbs with skin types IV-VI. In the 6th-week follow-up, there was a reduction in terminal hair after IPL (64%) and Nd: YAG (73%). A randomised clinical trials assessed the comparison of alexandrite and IPL lasers in 232 patients with unwanted hair skin types II IV. In the 6th month follow up, there was a reduction in terminal hair after alexandrite laser (68.8%) and after IPL (67%).[18] In the first patient, at the end of the IPL session, there was a decrease in the number of terminal hairs on the right and left legs, by 95.1% and 93.47%, respectively; alexandrite lasers are 91.02% and 90.79%, respectively; and Nd: YAG lasers 79.69% and 84.39%, respectively. In the second patient, at the end of the IPL session, there was a decrease in the number of terminal hairs on the right and left limbs, respectively, 20% and 47.45%; alexandrite lasers 78.57% and 79.74%, respectively; and Nd: YAG lasers at 77.27% and 73.13%, respectively.
Dermoscopy is one of the supporting examinations to assess the effectiveness of hair removal. Toossi et al. assessed 50 dermoscopy images of hair reduction compared to counting using the multi-resolution staining method and found that the dermoscopy examination has high accuracy with few errors.[19] In observation, dermoscopy examination post-IPL and laser patients’ hair removal found a reduction in the pigment of melanin.[20] Subjectively, both patients stated that they experienced hair loss. Objectively, the dermoscopy image also found a reduction in the number of terminal hairs, the hair looked finer, and the color was lighter than the normal baseline.
Based on the mechanism of action of the laser, postlaser action can be found in inflammation, erythema, and perifollicular edema. This is a normal response to the hair follicle by heating from the laser. Perifollicular erythema and edema may disappear within 2 days to a week, administration of cold water compresses and topical corticosteroids can accelerate healing. Analgesics are generally not required.[5] Both patients showed perifollicular erythema and edema a few minutes after alexandrite laser therapy which was reported to disappear after 3 days. Cold compresses of 0.9% NaCl and 0.1% mometasone furoate topical cream was applied to the therapeutic area to reduce postoperative erythema.
The most common side effects include pain and discomfort which can be treated with oral analgesics. Other side effects that are often encountered are the appearance of purpura, vesicles, and crusts.[21,22] If found can be treated with topical antibiotics, topical corticosteroids, and emollients. Pigmentation disorders such as hyperpigmentation or hypopigmentation can occur. Hyperpigmentation disorders are usually temporary and will improve with time, occurs because the laser light stimulates the melanocytes to produce more melanin, similar to what happens when people spend a long time sunbathing.[5] Ismail compared the level of comfort, safety, and effectiveness of the measures of hair removal with long-pulsed Nd: YAG and IPL in 50 females with skin types IV-VI. The patient complained of pain and posttreatment inflammation with the Nd: YAG laser.[23] Al-Dhalimi compared long-pulse alexandrite and IPL for facial hair removal. During 6 sessions, hyperpigmentation complications were found in 10% of patients treated with alexandrite laser.[15] The Nd: YAG laser is considered the safest in dark-skinned patients because it has a higher wavelength, thereby reducing epidermal damage.[21] Both patients experienced hyperpigmentation up to 4 weeks posttreatment with alexandrite laser. Meanwhile, after IPL and Nd: YAG, no significant side effects were found.
Assessment of posttreatment pain was measured by the VAS with pain ranging from 0 (no pain) to 10 (unbearable pain). Karaca et al. assessed VAS in 21 patients after IPL, alexandrite laser, and Nd: YAG laser and found the lowest VAS after alexandrite laser (3.90), followed by IPL (5.71), and Nd: YAG (6.95).[15] Inversely proportional to the VAS assessed in both cases posttreatment. Both patients were measured for VAS after alexandrite laser with the highest score (6–7), followed by IPL (4–5), and Nd: YAG with the value of 3.
Handjani (2013) assessed the quality of life of 42 patients who underwent surgery hair removal using laser treatments, including alexandrite and Nd: YAG lasers. Four months after the procedure for 3 sessions, the mean DLQI score decreased by 10 points, indicating an improvement in the patient’s quality of life.[24] At 4 weeks post-treatment, both patients had a decrease in their DLQI score to 1.
Effective assessment of actions hair removal seen in the observations until the 6th month of the last session. This is due to the telogen phase of lower leg hair up to 6 months, which is longer than the hair of other body parts.[6] The target of therapy is for the hair become smooth and light in color so that there is no more melanin which is the target of the three modalities.[1] Both patients experienced a reduction in the number of terminal hairs and the hair appeared finer after a 4-week evaluation. The next evaluation will be carried out in the 3rd session and 6th month after the last session.
CONCLUSION
Two cases have been reported hair removal of lower leg hair in skin type patients IV used IPL (695 nm), the alexandrite laser (755 nm), and Nd: YAG laser (1064 nm). Both cases experienced improvement after 4 weeks of action in terms of decreasing the number of terminal hairs. The highest side effects of hyperpigmentation and VAS (6–7) were found in areas treated with alexandrite laser. Both patients’ DLQI scores decreased. Nd: YAG laser may be better suitable for both sexes with minimal side effects, but the limitation of this study is the smaller subject group and limited session. The treatment modality in these two cases is currently under observation.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank their colleagues from the Department of Dermatology and Venereology, Faculty of Medicine, Sriwijaya University, Dr. Mohammad Hoesin Hospital, Palembang, Indonesia, that greatly accommodated and assisted in sampling.
REFERENCES
- 1.Wheat A, Radborne M. Hair removal: A summary of techniques with a particular emphasis on the importance and versatility of electrolysis. PMFA News. 2015;2:1–3. [Google Scholar]
- 2.Terry G, Braun V. To let hair be, or to not let hair be?Gender and body hair removal practices in Aotearoa/New Zealand. Body Image. 2013;10:599–606. doi: 10.1016/j.bodyim.2013.07.001. [DOI] [PubMed] [Google Scholar]
- 3.Thacker P, Kumar P. Near infrared pulsed light for permanent hair reduction in fitzpatrick skin types IV and V. J Cutan Aesthet Surg. 2016;9:249–53. doi: 10.4103/0974-2077.197078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agarwal M, Velaskar S, Gold MH. Efficacy of a low fluence, high repetition rate 810 nm diode laser for permanent hair reduction in Indian patients with skin types IV-VI. J Clin Aesthet Dermatol. 2016;9:29–33. [PMC free article] [PubMed] [Google Scholar]
- 5.Ibrahimi OA, Avram MM, Hanke CW, Kilmer SL, Anderson RR. Laser hair removal. Dermatol Ther. 2011;24:94–107. doi: 10.1111/j.1529-8019.2010.01382.x. [DOI] [PubMed] [Google Scholar]
- 6.Kaufman J. Laser and light therapy. In: Baumann L, editor. Cosmetic Dermatology Principles and Practices. 2nd ed. New York: The McGraw-Hill Companies, Inc; 2016. pp. 212–21. [Google Scholar]
- 7.Gan SD, Graber EM. Laser hair removal: A review. Dermatol Surg. 2013;39:823–38. doi: 10.1111/dsu.12116. [DOI] [PubMed] [Google Scholar]
- 8.Koch D, Pratsou P, Szczecinska W. The diverse application of laser hair removal therapy: A tertiary laser unit experience with less common indication and literature overview. Lasers Med Sci. 2015;30:453–67. doi: 10.1007/s10103-013-1464-5. [DOI] [PubMed] [Google Scholar]
- 9.Small R, editor. A Practical Guide to Laser Procedures. Philadelphia: Wolters Kluwers; 2016. Hair removal; pp. 55–82. [Google Scholar]
- 10.Zachary CB, Kelly KM. Laser and energy-based therapies. In: Bolognia JL, Achaffer JV, Cerroni L, editors. Dermatology. 4th ed. New York: Elsevier; 2018. pp. 2364–86. [Google Scholar]
- 11.Arsiwala SZ, Majid IM. Methods to overcome poor responses and challenges of laser hair removal in dark skin. Indian J Dermatol Venereol Leprol. 2019;85:3–9. doi: 10.4103/ijdvl.IJDVL_1103_16. [DOI] [PubMed] [Google Scholar]
- 12.Ullman Y, Naftali YB. IPL for hair removal. In: Fodor L, Ullmann Y, editors. Aesthetic Applications of Intensed Pulsed Light. 2nd. Switzerland: Springer; 2020. pp. 75–91. [Google Scholar]
- 13.Shirkavand A, Ataie-Fashtami L, Sarkar S, Alinaghizadeh MR, Fateh M, Zand N, et al. Thermal damage patterns of diode hair-removal lasers according to various skin types and hair densities and colors: A simulation study. Photomed Laser Surg. 2012;30:374–80. doi: 10.1089/pho.2011.3152. [DOI] [PubMed] [Google Scholar]
- 14.Mustafa FH, Jaafar MS. Shaving area of unwanted hair before laser operation is useful in cosmetic procedure: A simulation study. J dermatol Dermatol Surg. 2015;19:36–42. [Google Scholar]
- 15.Karaca S, Kaçar SD, Ozuğuz P. Comparison of SHR Mode IPL System with Alexandrite and Nd: YAG Lasers For Leg Hair Reduction. Balkan Med J. 2012;29:401–5. doi: 10.5152/balkanmedj.2012.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yanghuabian B, Hajerbrahimi S, Pashazadek H, Pascazadek F. Technology assesment of long pulsed alexandrite laser device for hair removal: A systematic review. J Discov. 2019;23:821–8. [Google Scholar]
- 17.Gold MH, Biron JA, Thompson B. Clincal evaluation of novel intensed pulsed light source for facial skin hair removal for home use. J Clin Aesthet Dermatol. 2015;8:30–5. [PMC free article] [PubMed] [Google Scholar]
- 18.Haedersdal M, Faurschou A. Photoepilation of unwanted hair growth. In: Raulin C, Karsai S, editors. Laser and IPL Technology in Dermatology and Aesthetic Medicine. 1st Ed. Berlin: Springer; 2011. pp. 125–45. [Google Scholar]
- 19.Toossi MT, Pourreza HR, Zare H, Sigari MH, Layegh P, Azimi A. An effective hair removal algorithm for dermoscopy images. Skin Res Technol. 2013;19:230–5. doi: 10.1111/srt.12015. [DOI] [PubMed] [Google Scholar]
- 20.Sillard L, Mantoux F, Larrouy JC, Hofman V, Passeron T, Lacour JP, et al. Dermoscopic changes of melanocytic nevi after laser hair removal. Eur J Dermatol. 2013;23:121–3. doi: 10.1684/ejd.2012.1907. [DOI] [PubMed] [Google Scholar]
- 21.Husain Z, Alster TS. The role of lasers and intense pulsed light technology in dermatology. Clin Cosmet Investig Dermatol. 2016;9:29–40. doi: 10.2147/CCID.S69106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Al-Hargan A, Ghobara YA, Al-Issa A. Purpura induced by laser hair removal: A case report. J Med Case Rep. 2018;12:60. doi: 10.1186/s13256-018-1604-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ismail SA. Long-pulsed Nd: YAG laser versus. Intense pulsed light for hair removal in dark skin: A randomized controlled trial. Br J Dermatol. 2012;166:317–21. doi: 10.1111/j.1365-2133.2011.10695.x. [DOI] [PubMed] [Google Scholar]
- 24.Handjani F, Saki N, Kardeh B, Maghsoodi M. Assessment of laser therapy on the quality of life in patients with hirsutism using the dermatology life quality index. Iran J Dermatol. 2013;16:6–8. [Google Scholar]


