Abstract
Background
An increasing number of patients receive ambulance care without being conveyed to a definitive care provider. This process has been described as complex, challenging, and lacking in guideline support by EMS clinicians. The use of quality- and outcome measures among non-conveyed patients is an understudied phenomenon.
Aim
To identify current quality- and outcome measures for the general population of non-conveyed patients in order to describe major trends and knowledge gaps.
Methods
A scoping review of peer-reviewed original articles was conducted to identify quality- and outcome measures for non-conveyance within emergency medical services. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews statement (PRISMA-ScR) was followed. The PROSPERO and OSF database were checked for pending reviews or protocols. PubMed, CINAHL, Scopus, Web of Science and the Cochrane Library database were searched for relevant articles. Searches were performed in November 2023.
Results
Thirty-six studies fulfilled the inclusion criteria and were included in the review. Mortality was the most used outcome measure, reported in 24 (67%) of the articles. Emergency department attendance and hospital admission were the following most used outcome measures. Follow-up durations varied substantially between both measures and studies. Mortality rates were found to have the longest follow-up times, with a median follow-up duration a little bit over one week.
Conclusions
This scoping review shows that studies report a wide range of quality and outcome measures in the ambulance setting to measure non-conveyance. Reported quality and outcome measures were also heterogeneous with regard to their follow-up timeframe. The variety of approaches to evaluate non-conveyance poses challenges for future research and quality improvement. A more uniform approach to reporting and measuring non-conveyance is needed to enable comparisons between contexts and formal meta-analysis.
Introduction
Demand for Emergency Medical Service (EMS) care has increased over the past decade, driven by a patient population with increasingly complex health care needs, limited emergency care resources, and more frequent calls for primary care problems. [1–9]. With this increasing demand for ambulance care, an increasing number of patients receive ambulance care without being conveyed to hospital [10,11]. In this article, non-conveyance is defined as clinician-initiated, definitive on-scene care by an (ambulance) EMS clinician with any level of training and referral to any health care service other than conveyance by an ambulance to a hospital. The definition thus includes the practice of referring patients to the emergency department by alternate means (e.g. a private vehicle or taxi), to primary health care providers, and all other health care facilities and services. For general patient populations, the proportion of non-conveyed patients has been found to range from 3.7–93.7% [12]. The non-conveyed population is characterized by younger patients relative to conveyed patients. Common on-scene diagnoses for non-conveyed patients include abdomen and chest pain, breathing difficulties, trauma, low blood glucose levels, psychiatric problems, as well as a substantial number of patients with non-classifiable symptoms [13,14]. Non-conveyed patients have further been found to often have at least one abnormal vital sign [13–15]. This wide range of potential diagnoses, difficult-to-classify symptoms, abnormal vital signs, and plethora of alternate care pathways all contribute to a difficult decision-making process [13,15,16]. A significant proportion of ambulance patients seek health care following non-conveyance [15,17], though it is not clear what this entails in terms of patient safety [12]. This process has been experienced as complex, challenging, and lacking guideline support by EMS clinicians [12,18,19]. Patients have reported relatively high satisfaction with the care provided during non-conveyance, although it can evoke fear, shame, and a need for reassurance [20,21]. When not conveyed, and instead diagnosed and/or treated on-scene, patients can be referred to a wide range of health care services or left with no follow-up care. Although EMS clinician and patients have a positive attitude towards using alternate care pathways, the safety of the practice of referral to these alternatives remains unclear [22,23].
Historically, the safety of ambulance care has predominantly been measured using non-clinical, often time-related quality measures [24]. There is little to no evidence regarding the clinical benefits of evaluating EMS quality and performance using non-clinical quality measures [25]. The last two decades have seen the increasing use of clinical quality measures, which are most often applicable to specific and rare time-critical conditions (e.g. Out-of-hospital cardiac arrest). Thus, relatively few patients are impacted by their use [26]. Developing meaningful quality measures that holistically measure the quality of EMS care requires a clear definition of quality [27]. The concept of quality is highly contextual, which has resulted in a substantial variety of definitions of quality among clinicians, researchers, and society in general [28,29]. The use of quality measures among non-conveyed patients is an understudied phenomenon with a great variety of different outcome measures, making drawing generalizable conclusions difficult [12,30].
Therefore, to increase our knowledge regarding relevant outcome measures for the general non-conveyed patient population, we conducted a scoping review with the primary objective of identifying current quality and outcome measures for patients non-conveyed by EMS clinicians.
The aim of the study was to identify current quality and outcome measures for the general non-conveyance patient population in order to describe major trends and knowledge gaps.
Methods
Design
A scoping review was chosen since the research question was broad, and prior knowledge suggested that relatively few research papers described quality- or outcome measures for non-conveyed patients in the ambulance setting [31]. The scoping review is reported using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews statement (PRISMA-ScR) [32].
Search strategy
The PROSPERO and OSF database were checked for pending reviews or protocols on the same topic, and none were identified. Systematic literature search strategies were developed for PubMed (National Center for Biotechnology Information, National Institutes of Health; Bethesda, Maryland USA), CINAHL (EBSCO Information Services; Ipswich, Massachusetts USA), Scopus (Elsevier, Amsterdam Netherlands), Web of Science (Clarivate, Philadelphia USA) and the Cochrane Library (The Cochrane Collaboration; Oxford, United Kingdom). All authors and information specialists at the Karolinska University library took part in the development of the search strategy. Searches were performed in November 2023. Full search strategies per database are described in (S1 File).
Selection process
First, search queries for each database were downloaded and imported to BibDesk© v.1.8.11 where all hits were systematically deduplicated [33] and manually reviewed regarding duplication. Second, articles eligible for screening were imported to Rayyan [34]. Two pairs of independent researchers (EH/DS and CM/JL) each screened half of the identified records on title and abstract and decided on inclusion to the next step. The first step was conducted blinded between the two researchers. There were less than five percent conflicts of inclusion between all authors. Conflicts were resolved by consensus in full group discussions. Third, the articles eligible for inclusion were screened, blinded, in full text by the same two researchers. If articles were excluded in the full-text screening phase, the reasons for exclusion are reported in the flow diagram. Fourth, reference lists in all identified systematic reviews and scoping reviews were manually screened, first on title, then abstract and finally full-text articles in the same manner as in steps two and three.
Inclusion criteria: (1) Peer-reviewed research written in English, (2) All countries with no time constraints and including all study designs, (3) Research concerning non-conveyance within the ambulance service (e.g., not evaluations of emergency departments, primary health care, and dispatch centers.), (4) Articles reporting on the use or development of a quality- or outcome measures, (5) All provider levels were included, but had to be dispatched via the 9-1-1/1-1-2 system (e.g. not including community paramedicine interventions).
Exclusion criteria: (1) Articles reporting on clinical subgroups, for example; hypoglycemia and opioid overdose, (2) Articles clearly and only reporting on patient-initiated refusal of care, (3) Review articles.
All included articles were then divided between, and reviewed by one of the authors, who extracted all relevant information, including all identifiable quality and outcome measures. No evaluation of the quality of the included articles was performed since the main interest was the prevalence of reported quality and outcome measures in the literature rather than the findings of the studies.
Analysis
The analysis was guided by the methodological framework described by Arksey and O’Malley (2005) [31]. The extracted measures were recorded in a Google Sheets document and then reviewed by the authors collaboratively. In this process, similar measures which had been written in different ways were combined (e.g., “EMS recontact” and “recontact with EMS” or “death” and “mortality”) and categorized into overarching types of measures. These data were then exported and processed using R (v 4.2.0) to generate descriptive statistics. The prevalence of each measure was described using absolute values and percentages. The follow-up time used in the studies for each measure was described in aggregate using box plots. The complete R code used to produce the analysis and generate tables and figures is available as (S2 File).
Results
From the database searches, 2,515 hits were identified. After deduplication, a total of 1,622 titles and abstracts were included for screening. In the first step, articles were included based on title and abstract. Of all screened articles, a total of 62 were retrieved to be read in full text, 32 of which were excluded. Of these, 15 articles were excluded due to the evaluation of sub-populations (e.g., hypoglycemia, falls, or opioid overdose). Twelve articles were not based on original research (i.e., review articles). Four articles evaluated only patient-initiated refusals, and one article concerned the evaluation of the theoretical ability of providers to predict patient outcomes. Thirty articles from the database searches fulfilled the inclusion criteria and were included in the review. The 12 excluded review articles were read in full text, and 274 references were extracted. These references were screened in the same way as the articles for the database searches. Of all review article references, six original articles were included after deduplication, abstract screening and full-text review. In total 36 studies fulfilled the inclusion criteria and were included in the review. The selection process is described in Fig 1.
Fig 1. Flow diagram for the inclusion process.
Included articles were produced in the Sweden (7), USA (9), UK (5), Finland (4), Australia (4), Netherlands (1), Canada (3), Iran (1), and New Zealand (2). The ambulances were most commonly staffed by paramedics. A variety of study designs, Observational (n = 30), Mixed methods (n = 3), Qualitative (n = 1), Cluster-randomized (n = 1), Case-control (n = 1), and data collection approaches (Prospective (n = 14), Retrospective (n = 16) was used. Patients were of all ages, and various cut-off thresholds between 15–21 years were used to define adulthood. Fourteen studies included only adult patients, four studies included only children, one study included only elderly (>60 years) patients, and one study included only adult non-elderly patients (18–65 years). The remainder reported results for patients of all ages (Table 1).
Table 1. Description of included articles.
| Title | Context | Study design | Population | Quality- or outcome measures used |
|---|---|---|---|---|
| Blodgett, (2020) [35] | UK (Paramedic) | Prospective observational | Age > = 17, n = 4540 | Emergency department attendance, Hospital admission, Mortality, Emergency department interventions, Number of ward transfers |
| Bosson, (2023) [36] | USA (Paramedic) | Prospective observational | Age > = 18, n = 3330 | Primary care, EMS recontact, Emergency department attendance, Mortality, Symptom progression, Any follow-up care after recommendation of no care, Patient satisfaction |
| Breeman, (2018) [37] | Netherlands (Nurse-based) | Prospective observational | Age > = 18, n = 1095 | Primary care, Mobile care unit, EMS recontact, Emergency department attendance, Mortality, Any follow-up care after recommendation of no care, Referral to tertiary care, Patient satisfaction, Agreement about transport decision with physician |
| Carrigan, (2022) [38] | Canada (Paramedic) | Retrospective observational | All ages, n = 14072 | EMS recontact, Mortality |
| Cooper, (2004) [39] | UK (Paramedic & ECP) | Mixed methods | All ages, n = 501 | EMS conveyance rates |
| Coster, (2019) [40] | UK (EMT & Paramedic) | Retrospective observational | All ages, n = 42796 | EMS recontact, Emergency department attendance, Hospital admission, Mortality |
| Forsell, (2021) [41] | Sweden (Nurse based) | Prospective observational | Age > = 18, n = 1048 | Primary care visit, EMS recontact, Emergency department attendance, Hospital admission, Any follow-up care after recommendation of no care |
| Haines, (2006) [42] | USA (Paramedic) | Prospective observational | Age > = 21, n = 5336 | Primary care visit, Emergency department attendance, Hospital admission, Mortality, Patient satisfaction |
| Heinonen, (2022) [43] | Finland (Mixed) | Retrospective observational | Age >16, n = 76233 | Mortality |
| Höglund, (2022) [44] | Sweden (Nurse) | Prospective observational | All ages, n = 2691 | Emergency department attendance, Hospital admission, ICU, Mortality |
| Jensen, (2013) [45] | Canada (Paramedic & ECP) | Retrospective observational | All ages, n = 238 | EMS recontact |
| Kahalé, (2009) [46] | Canada (Paramedic) | Retrospective observational |
Age < = 15, n = 345 |
Any follow-up care after recommendation of no care |
| Keene, (2015) [47] | Australia (Paramedic) | Qualitative | Age > = 18, n = 20 | Referral to tertiary care, Primary care visit, Emergency department attendance |
| Knapp, (2009) [48] | USA (Paramedic) | Prospective observational | Age 18–65, n = 93 | Emergency department attendance, Hospital admission, Adverse event |
| Langabeer, (2016) [49] | United States (EMT & Paramedic) | Case-control | All ages, n = 5570 | EMS recontact, Mortality, EMS conveyance rates, Patient satisfaction |
| Larsson, (2017) [50] | Sweden (Nurse) | Prospective observational | Age > = 18, n = 3018 | Hospital admission, Mortality, Any follow-up care after recommendation of no care |
| Laukkanen, (2022) [51] | Finland (Mixed) | Retrospective observational | All ages, n = 12530 | Emergency department attendance, Hospital admission, ICU, Mortality, Physician consultation |
| Lederman, (2021) [52] | Sweden (Nurse) | Retrospective observational | Age >18, n = 17809 | Emergency department attendance, Hospital admission, Mortality |
| Magnusson, (2016) [53] | Sweden (Nurse) | Retrospective observational | All ages, n = 529 | Emergency department attendance, Hospital admission, Specific intervention |
| Magnusson, (2018) [54] | Sweden (Nurse) | Prospective observational | Age 0–15, n = 197 | Emergency department attendance, Hospital admission, Mortality, Full triage, Specific intervention |
| Magnusson, (2020) [55] | Sweden (Nurse) | Prospective observational | Age > = 16, n = 6652 | Emergency department attendance, Hospital admission, "Time sensitive condition", Adverse event |
| Mason, (2007) [56] | UK (Paramedic practitioners) | Cluster-randomized trial | Age >60, n = 394 | EMS recontact, Emergency department attendance, Hospital admission, Mortality, Patient satisfaction, Quality of life, Specific intervention, Any follow-up care after recommendation of no care, Adverse event |
| Nehme, (2023) [57] | Australia (Paramedic) | Retrospective observational | Age < = 17, n = 62975 | EMS recontact, Emergency department attendance, Hospital admission, Adverse event |
| Oulasvirta, (2019) [58] | Finland (EMT & Paramedic) | Retrospective observational | Age < = 15, n = 3579 | Emergency department attendance, ICU, Mortality |
| Paulin, (2021) [59] | Finland (Nurse) | Prospective observational | All ages, n = 11861 | Primary care visit, EMS recontact, Emergency department attendance, Hospital admission, Mortality |
| Peyravi, (2015) [60] | Iran (Paramedic) | Mixed methods | All ages, n = 3019 | Mortality, Any follow-up care after recommendation of no care, Recovery |
| Pringle Jr, (2005) [61] | USA (Mixed) | Prospective observational | All ages, n = 310 | Emergency department attendance, Hospital admission, Mortality, Any follow-up care after recommendation of no care |
| Schmidt, (2001) [62] | USA (EMT & Paramedic) | Prospective observational | All ages, n = 1433 | Hospital admission, ICU, Specific intervention |
| Schmidt, (2006) [63] | USA (Paramedic) | Retrospective observational | All ages, n = 1581 | Mortality |
| Snooks, (2004) [64] | UK (EMT & Paramedic) | Mixed methods | Age Not specified, n = 788 | EMS recontact |
| Supples, (2022) [65] | USA (Mixed) | Retrospective observational | All ages, n = 3927 | EMS recontact |
| Todd, (2021) [66] | New Zealand (EMT & Paramedic) | Retrospective observational | Age > = 15, n = 83171 | Mortality, EMS conveyance rates, Any follow-up care after recommendation of no care, Recurrence of symptoms |
| Todd, (2021) [67] | New Zealand (EMT & Paramedic) | Retrospective observational | Age > = 15, n = 41406 | EMS recontact, Mortality |
| Tohira, (2016) [68] | Australia (Paramedic & ECP) | Prospective observational | All ages, n = 67387 | EMS recontact, Hospital admission, Mortality |
| Tohira, (2016) [69] | Australia (Paramedic) | Retrospective observational | All ages, n = 38293 | EMS recontacts, Emergency department attendance, Hospital admission, Mortality |
| Zachariah, (1992) [70] | USA (Paramedic) | Retrospective observational | All ages, n = 158 | Emergency department attendance, Hospital admission, ICU, Mortality |
Several different quality and outcome measures were described in the included articles (Table 2). Most commonly reported quality or outcome measure involved an event or health care contact. Mortality was the most used measure, reported in 24 of 36 articles. Emergency department attendance and hospital admission were the following most used outcome measures.
Table 2. Description of identified quality and outcome measures.
| Measure type | Measure name | Number of times each measure was reported | Most common timeframe or statistic (% of total) |
|---|---|---|---|
| Event/health care contact | Mortality | 24 (67%) | 1 week (29%) |
| Event/health care contact | Emergency department attendance | 21 (58%) | 3 days (38%) |
| Event/health care contact | Hospital admission | 20 (56%) | 3 days (40%) |
| Event/health care contact | EMS recontact | 15 (42%) | 2 days (40%) |
| Event/health care contact | Any follow-up care after recommendation of no care | 9 (25%) | 1 day (22%) |
| Event/health care contact | Primary care | 6 (17%) | 1 day (33%) / 3 days (33%) |
| Event/health care contact | ICU | 5 (14%) | Not specified (60%) |
| Patient reported | Patient satisfaction | 5 (14%) | Not specified (60%) |
| Event/health care contact | Specific intervention | 4 (11%) | 3 days (50%) |
| Event/health care contact | Adverse event | 4 (11%) | 1 month (25%) / 2 days (25%) / 48 hours (25%) / Not specified (25%) |
| Event/health care contact | EMS conveyance rates | 3 (8%) | Immediate (33%) / 1 day (33%) / 2 days (33%) |
| Care duration | EMS | 2 (6%) | Average 27min-35min (50%), Median 39min (50%) |
| Care duration | Hospital admission | 2 (6%) | Median 3 days (50%) / not clearly stated (50%) |
| Event/health care contact | Referral to tertiary care | 2 (6%) | Not specified (100%) |
| Care duration | Emergency department | 1 (3%) | Not clearly stated (100%) |
| Time to care | Time from non-conveyance to Emergency department | 1 (3%) | Average 43 min (100%) |
| Event/health care contact | "Time sensitive condition" | 1 (3%) | 3 days (100%) |
| Event/health care contact | ED Interventions | 1 (3%) | 1 month (100%) |
| Event/health care contact | Mobile care unit | 1 (3%) | 1 day (100%) |
| Event/health care contact | Number of ward transfers | 1 (3%) | 1 month (100%) |
| Event/health care contact | Recurrence of symptoms | 1 (3%) | 2 days (100%) |
| Expert evaluation | Agreement about transport decision with physician | 1 (3%) | Not applicable (100%) |
| Guideline/protocol adherence | Full triage | 1 (3%) | Not applicable (100%) |
| Guideline/protocol adherence | Physician consultation | 1 (3%) | Not applicable (100%) |
| Patient reported | Quality of Life | 1 (3%) | 1 month (100%) / 3 days (100%) |
| Patient reported | Recovery | 1 (3%) | Not specified (100%) |
| Patient reported | Symptom progression | 1 (3%) | Not specified (100%) |
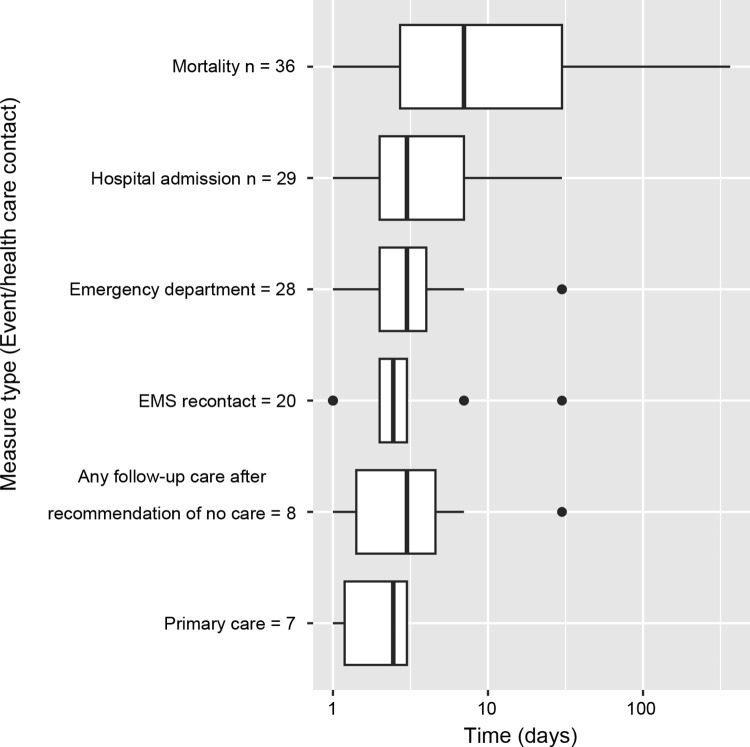
Follow-up durations varied substantially between both measures and studies, as described in Fig 2 below. Mortality rates were found to have the longest follow-up times, with a median follow-up duration of slightly over one week. Other measures had shorter follow-up durations, with all other measures with more than five occurrences in the literature having a median follow-up time of 72 hours or less.
Fig 2. Box plot of follow-up durations of quality measures with >5 occurrences, log scaled.
Note that n values are larger than in Table 2 due to studies reporting quality measures at multiple follow-up durations.
Discussion
This study found that patient mortality was the most commonly investigated quality or outcome measure following non-conveyance, reported in 24 (67%) of included studies. Measures of subsequent patient contact with the emergency department were found in 21 (58%) of all included studies, and hospital admission was reported in 20 (56%). The median follow-up duration for mortality was about one week, while emergency department visits and hospital admission measures were most commonly measured at three days. Outcome measures were often based on retrospectively gathered data. At the same time, only a few studies investigated patient-reported measures or measures based on expert review.
The interpretation of the identified measures varies substantially depending on the type of care pathway a patient is referred to following a non-conveyance decision (e.g., primary care or alternate transport to an emergency department). To increase the clinical relevance of the reported outcome measures concerning subsequent contacts, outcomes should be reported and stratified by non-conveyance destination.
The vast majority of the identified measures were based on all-cause data, and as argued by Ebben et al., health care re-contact rates are most relevant when they are related to the initial non-conveyance decision [12]. The validity and clinical relevance of the quality measures may thus be questionable. In an emergency department setting for instance, about 6 percent of repeated contacts within 72 hours were unrelated to the initial contact [71] while in a dispatching context, a 15% rate of unrelated contacts within 72 hours has been found [72]. Determining the relationship between two health care contacts can however be time-consuming, based on retrospective data, and such determinations have been found to have low interrater reliability [72]. The development of a standardized definition of whether two health care contacts are related could aid in promoting more valid and reproducible results. Many of the reported quality and outcome measures can only be obtained if data between different care providers (for instance, emergency dispatcher, primary care, EMS and emergency department) is linked, which is a barrier to data collection in some contexts [73].
We argue that the extent to which subsequent health care contacts, such as emergency department visits or hospital admissions, should be considered adverse events is questionable. The relevance of mortality over the long follow-up durations found in this study in measuring the quality of ambulance care is also open to question. The proportion of related contacts among subsequent health care contacts has been shown to decrease substantially over time [72]. Shorter-term mortality rates are arguably sufficient to capture situations where an adverse event might have occurred while minimizing sources of bias and random noise. Survival curves may offer a more nuanced alternative to reporting patient mortality rates over fixed durations [74–76]. It may furthermore be appropriate to exclude, or at least separately report, patients in end-of-life palliative care with short life expectancy from mortality statistics.
We found only one study evaluating the agreement between EMS clinicians and hospital clinicians, though additional studies evaluating such agreement rates were identified but excluded as they evaluated agreement only theoretically, e.g., whether a transported patient could have been left at home [77]. Performing expert reviews of medical records to identify triage errors has been found to be useful in similar contexts. Performing manual expert reviews of non-conveyance decisions determined to be “high risk” based on an automatically extracted quality measures may offer a fruitful approach to improving quality and limiting patient risks in the context of non-conveyance decisions in the EMS [72].
Not all articles stated who initiated the non-conveyance decision. Since the current study focused on describing quality and outcome measures relevant to clinician-initiated non-conveyance decisions, articles that clearly and only described patient-initiated refusals were excluded. Articles that did not clearly state who made the non-conveyance decision were still included to describe as many quality and outcome measures for the general non-conveyance population as possible.
This scoping review provides a high-level overview of how non-conveyance for the general non-conveyance population is measured and reported. How the described quality and outcome measures relate to patient safety remains unclear.
Limitations
Scoping reviews have a significant limitation compared to systematic reviews in the generally broad nature of the research question, resulting most often in similarly broad and heterogeneous findings. This makes it more difficult to synthesize the findings comprehensively. Articles that fulfill the inclusion criteria could also be missed. Nonetheless, scoping reviews are appropriate for the aim of describing a body of research and identifying major patterns. The results of this review showed significant heterogeneity; therefore, results had to be abstracted to a high level. Although two to three authors reviewed each article and agreement between authors during the inclusion and exclusion process was high, no formal quality assessment of included articles was performed. This decision was made since the research question involved describing the quality and outcome measures used in the literature, rather than drawing conclusions regarding their findings.
Conclusions
This scoping review shows that studies reported a wide range of measures in the ambulance setting to measure the quality- and outcomes of non-conveyance. The majority of included studies however included subsequent mortality, emergency department visits, and hospital admission. Studies were heterogeneous with regard to their follow-up timeframe, ranging from one day to one year. The most commonly reported outcome measures were in the form of mortality rates or subsequent contacts with the health care system following non-conveyance. There was a lack of patient-reported quality and outcome measures. The variety of approaches to evaluating non-conveyance poses challenges for future research.
A uniform approach to measuring and reporting non-conveyance is needed to enable comparisons between contexts and formal meta-analysis.
These findings can be used by researchers seeking to use standardized quality measures, outcome measures and follow-up durations in future studies to maximize the comparability of prehospital research. We furthermore identify a substantial reliance on outcome measures that can be easily extracted retrospectively from hospital records. Such measures are useful in terms of comparative evaluations and performing an initial selection for patients experiencing a potential adverse event. EMS organizations should consider various quality and outcome measures to capture multiple aspects of the phenomenon. The relevance of each quality and outcome measure needs further investigation. New quality and outcome measures may need to be developed to capture additional important aspects.
The current study revealed knowledge gaps related to uniformity in reporting strategies and the need for future studies to evaluate the clinical relevance of the used quality and outcome measures. The development of more sophisticated methods to more precisely identify adverse events resulting from non-conveyance should be sought. Our findings may be useful for EMS providers seeking to measure the complex phenomenon of non-conveyance.
Supporting information
(DOCX)
(DOCX)
(XLSX)
(R)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Edwards MJ, Bassett G, Sinden L, Fothergill RT. Frequent callers to the ambulance service: patient profiling and impact of case management on patient utilisation of the ambulance service. Emerg Med J. 2015;32(5):392–6. doi: 10.1136/emermed-2013-203496 [DOI] [PubMed] [Google Scholar]
- 2.Søvsø MB, Kløjgaard TA, Hansen PA, Christensen EF. Repeated ambulance use is associated with chronic diseases—a population-based historic cohort study of patients’ symptoms and diagnoses. Scand J Trauma Resusc Emerg Med. 2019;27(1):46. doi: 10.1186/s13049-019-0624-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jones CMC, Wasserman EB, Li T, Amidon A, Abbott M, Shah MN. The Effect of Older Age on EMS Use for Transportation to an Emergency Department. Prehosp Disaster Med. 2017;32(3):261–8. doi: 10.1017/S1049023X17000036 [DOI] [PubMed] [Google Scholar]
- 4.Booker MJ, Purdy S, Shaw ARG. Seeking ambulance treatment for ’primary care’ problems: a qualitative systematic review of patient, carer and professional perspectives. BMJ open. 2017;7(8):e016832. doi: 10.1136/bmjopen-2017-016832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Christensen EF, Larsen TM, Jensen FB, Bendtsen MD, Hansen PA, Johnsen SP, et al. Diagnosis and mortality in prehospital emergency patients transported to hospital: a population-based and registry-based cohort study. BMJ open. 2016;6(7):e011558. doi: 10.1136/bmjopen-2016-011558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Snooks HA, Khanom A, Cole R, Edwards A, Edwards BM, Evans BA, et al. What are emergency ambulance services doing to meet the needs of people who call frequently? A national survey of current practice in the United Kingdom. BMC Emerg Med. 2019;19(1):82. doi: 10.1186/s12873-019-0297-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sangkharat K, Fisher P, Thomas GN, Thornes J, Pope FD. The impact of air pollutants on ambulance dispatches: A systematic review and meta-analysis of acute effects. Environ Pollut. 2019;254(Pt A):112769. doi: 10.1016/j.envpol.2019.06.065 [DOI] [PubMed] [Google Scholar]
- 8.Sangkharat K, Mahmood MA, Thornes JE, Fisher PA, Pope FD. Impact of extreme temperatures on ambulance dispatches in London, UK. Environ Res. 2020;182:109100. doi: 10.1016/j.envres.2019.109100 [DOI] [PubMed] [Google Scholar]
- 9.Courtemanche C, Friedson AI, Rees DI. Association of Ambulance Use in New York City With the Implementation of the Patient Protection and Affordable Care Act. JAMA Netw Open. 2019;2(6):e196419. doi: 10.1001/jamanetworkopen.2019.6419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Andrew E., Nehme Z., Cameron P., & Smith K. (2020). Drivers of Increasing Emergency Ambulance Demand. Prehospital Emergency Care, 24(3), 385–393. doi: 10.1080/10903127.2019.1635670 [DOI] [PubMed] [Google Scholar]
- 11.Larsen T, Bendtsen M, Søvsø M, Lindskou T, Hansen P, Jensen F, et al. Treat-and-release EMS patients in the north denmark region: identification and vital signs. BMJ open. 2017;7:A13–A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ebben RHA, Vloet LCM, Speijers RF, Tonjes NW, Loef J, Pelgrim T, et al. A patient-safety and professional perspective on non-conveyance in ambulance care: a systematic review. Scand J Trauma Resusc Emerg Med. 2017;25(1):71. doi: 10.1186/s13049-017-0409-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lederman J, Lindström V, Elmqvist C, Löfvenmark C, Djärv T. Non-conveyance in the ambulance service: a population-based cohort study in Stockholm, Sweden. BMJ open. 2020;10(7):e036659. doi: 10.1136/bmjopen-2019-036659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hoglund E, Andersson-Hagiwara M, Schroder A, Moller M, Ohlsson-Nevo E. Characteristics of non-conveyed patients in emergency medical services (EMS): a one-year prospective descriptive and comparative study in a region of Sweden. BMC Emerg Med. 2020;20(1):61. doi: 10.1186/s12873-020-00353-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vloet LCM, de Kreek A, van der Linden EMC, van Spijk JJA, Theunissen VAH, van Wanrooij M, et al. A retrospective comparison between non-conveyed and conveyed patients in ambulance care. Scand J Trauma Resusc Emerg Med. 2018;26(1):91. doi: 10.1186/s13049-018-0557-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Höglund E, Schröder A, Möller M, Andersson-Hagiwara M, Ohlsson-Nevo E. The ambulance nurse experiences of non-conveying patients. J Clin Nurs. 2019; 28: 235–244. doi: 10.1111/jocn.14626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mikolaizak AS, Simpson PM, Tiedemann A, Lord SR, Close JC. Systematic review of non-transportation rates and outcomes for older people who have fallen after ambulance service call-out. Australasian journal on ageing. 2013;32(3):147–57. doi: 10.1111/ajag.12023 [DOI] [PubMed] [Google Scholar]
- 18.Lederman J, Lofvenmark C, Djarv T, Lindstrom V, Elmqvist C. Assessing non-conveyed patients in the ambulance service: a phenomenological interview study with Swedish ambulance clinicians. BMJ open. 2019;9(9):e030203. doi: 10.1136/bmjopen-2019-030203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Oosterwold J, Sagel D, Berben S, Roodbol P, Broekhuis M. Factors influencing the decision to convey or not to convey elderly people to the emergency department after emergency ambulance attendance: a systematic mixed studies review. BMJ Open. 2018. Aug 30;8(8):e021732. doi: 10.1136/bmjopen-2018-021732 ; PMCID: PMC6119414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.van Doorn SCM, Verhalle RC, Ebben RHA, Frost DM, Vloet LCM, de Brouwer CPM. The experience of non-conveyance following emergency medical service triage from the perspective of patients and their relatives: A qualitative study. Int Emerg Nurs. 2021;54:100952. doi: 10.1016/j.ienj.2020.100952 [DOI] [PubMed] [Google Scholar]
- 21.King R, Oprescu F, Lord B, Flanagan B. Patient experience of non-conveyance following emergency ambulance service response: A scoping review of the literature. Australas Emerg Care. 2021;24(3):210–23. doi: 10.1016/j.auec.2020.08.006 [DOI] [PubMed] [Google Scholar]
- 22.Blodgett JM, Robertson DJ, Pennington E, Ratcliffe D, Rockwood K. Alternatives to direct emergency department conveyance of ambulance patients: a scoping review of the evidence. Scand J Trauma Resusc Emerg Med. 2021;29(1):4. doi: 10.1186/s13049-020-00821-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ebben RHA, Castelijns M, Frenken J, Vloet LCM. Characteristics of non-conveyance ambulance runs: A retrospective study in the Netherlands. World J Emerg Med. 2019;10(4):239–43. doi: 10.5847/wjem.j.1920-8642.2019.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Price L. Treating the clock and not the patient: ambulance response times and risk. Qual Saf Health Care. 2006;15(2):127–30. doi: 10.1136/qshc.2005.015651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Myers JB, Slovis CM, Eckstein M, Goodloe JM, Isaacs SM, Loflin JR, et al. Evidence-based performance measures for emergency medical services systems: a model for expanded EMS benchmarking. Prehosp Emerg Care. 2008;12(2):141–51. doi: 10.1080/10903120801903793 [DOI] [PubMed] [Google Scholar]
- 26.Howard I, Cameron P, Wallis L, Castren M, Lindstrom V. Quality Indicators for Evaluating Prehospital Emergency Care: A Scoping Review. Prehosp Disaster Med. 2018;33(1):43–52. doi: 10.1017/S1049023X17007014 [DOI] [PubMed] [Google Scholar]
- 27.Pap R, Lockwood C, Stephenson M, Simpson P. Indicators to measure prehospital care quality: a scoping review. JBI Database System Rev Implement Rep. 2018;16(11):2192–223. doi: 10.11124/JBISRIR-2017-003742 [DOI] [PubMed] [Google Scholar]
- 28.Cooperberg MR, Birkmeyer JD, Litwin MS. Defining high quality health care. Urol Oncol. 2009;27(4):411–6. doi: 10.1016/j.urolonc.2009.01.015 [DOI] [PubMed] [Google Scholar]
- 29.Donabedian A. The quality of care. How can it be assessed? JAMA. 1988;260(12):1743–8. doi: 10.1001/jama.260.12.1743 [DOI] [PubMed] [Google Scholar]
- 30.Yeung T., Shannon B., Perillo S., Nehme Z., Jennings P. and Olaussen A. (2019), Review article: Outcomes of patients who are not transported following ambulance attendance: A systematic review and meta-analysis. Emergency Medicine Australasia, 31: 321–331. https://doi-org.db.ub.oru.se/10.1111/1742-6723.13288. [DOI] [PubMed] [Google Scholar]
- 31.Arksey H. and O’Malley L. (2005) ‘Scoping studies: towards a methodological framework’, International Journal of Social Research Methodology, 8(1), pp. 19–32. doi: 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 32.Tricco Andrea C., Lillie Erin, Zarin Wasifa, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med.2018;169:467–473. [Epub 4 September 2018]. doi: 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 33.Bramer WM, Giustini D, de Jonge GB, Holland L, Bekhuis T. De-duplication of database search results for systematic reviews in EndNote. J Med Libr Assoc. 2016. Jul;104(3):240–3. doi: 10.3163/1536-5050.104.3.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016. Dec 5;5(1):210. doi: 10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.*Blodgett JM, Robertson DJ, Ratcliffe D, Rockwood K. Piloting data linkage in a prospective cohort study of a GP referral scheme to avoid unnecessary emergency department conveyance. BMC Emerg Med. 2020. Jun 12;20(1):48. doi: 10.1186/s12873-020-00343-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.*Bosson N, Toy J, Chang A, Haase D, Kipust A, Korotzer L, Warren J, Kim YS, Kazan C, Gausche-Hill M. Short-Term Outcomes and Patient Perceptions after Paramedic Non-Transport during the COVID-19 Pandemic. Prehosp Emerg Care. 2023. May 3:1–7. doi: 10.1080/10903127.2023.2205512 [DOI] [PubMed] [Google Scholar]
- 37.*Breeman W, Poublon NA, Verhofstad MHJ, Van Lieshout EMM. Safety of on-scene medical care by EMS nurses in non-transported patients: a prospective, observational study. Scand J Trauma Resusc Emerg Med. 2018. Sep 14;26(1):79. doi: 10.1186/s13049-018-0540-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.*Carrigan S, Goldstein J, Carter A, Asada Y, Travers A. The Prevalence and Characteristics of Non-Transports in a Provincial Emergency Medical Services System: A Population-Based Study. J Emerg Med. 2022. Apr;62(4):534–544. doi: 10.1016/j.jemermed.2021.12.009 [DOI] [PubMed] [Google Scholar]
- 39.*Cooper S, Barrett B, Black S, Evans C, Real C, Williams S, Wright B. The emerging role of the emergency care practitioner. Emerg Med J. 2004. Sep;21(5):614–8. doi: 10.1136/emj.2003.011247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.*Coster J, O’Cathain A, Jacques R, Crum A, Siriwardena AN, Turner J. Outcomes for Patients Who Contact the Emergency Ambulance Service and Are Not Transported to the Emergency Department: A Data Linkage Study. Prehosp Emerg Care. 2019. Jul-Aug;23(4):566–577. doi: 10.1080/10903127.2018.1549628 [DOI] [PubMed] [Google Scholar]
- 41.*Forsell L, Forsberg A, Kisch A, Rantala A. Inequalities and short-term outcome among patients assessed as non-urgent in a Swedish ambulance service setting. Int Emerg Nurs. 2021. Jul;57:101018. doi: 10.1016/j.ienj.2021.101018 [DOI] [PubMed] [Google Scholar]
- 42.*Haines CJ, Lutes RE, Blaser M, Christopher NC. Paramedic initiated non-transport of pediatric patients. Prehosp Emerg Care. 2006. Apr-Jun;10(2):213–9. doi: 10.1080/10903120500541308 [DOI] [PubMed] [Google Scholar]
- 43.*Heinonen K, Puolakka T, Salmi H, Boyd J, Laiho M, Porthan K, et al. Ambulance crew-initiated non-conveyance in the Helsinki EMS system-A retrospective cohort study. Acta Anaesthesiol Scand. 2022. May;66(5):625–633. doi: 10.1111/aas.14049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.*Höglund E, Schröder A, Andersson-Hagiwara M, Möller M, Ohlsson-Nevo E. Outcomes in patients not conveyed by emergency medical services (EMS): a one-year prospective study. Scand J Trauma Resusc Emerg Med. 2022. Jun 13;30(1):40. doi: 10.1186/s13049-022-01023-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.*Jensen JL, Travers AH, Bardua DJ, Dobson T, Cox B, McVey J, et al. Transport outcomes and dispatch determinants in a paramedic long-term care program: a pilot study. CJEM. 2013. Jul;15(4):206–13. doi: 10.2310/8000.2012.120965 [DOI] [PubMed] [Google Scholar]
- 46.*Kahalé J, Osmond MH, Nesbitt L, Stiell IG. What are the characteristics and outcomes of nontransported pediatric patients? Prehosp Emerg Care. 2006. Jan-Mar;10(1):28–34. doi: 10.1080/10903120500373322 [DOI] [PubMed] [Google Scholar]
- 47.*Keene T, Davis M, Brook C. Characteristics and Outcomes of Patients Assessed by Paramedics and Not Transported to Hospital: A Pilot Study. Australasian Journal of Paramedicine. 2015;12:1–8. doi: 10.33151/ajp.12.2.231 [DOI] [Google Scholar]
- 48.*Knapp BJ, Tsuchitani SN, Sheele JM, Prince J, Powers J. Prospective evaluation of an emergency medical services-administered alternative transport protocol. Prehosp Emerg Care. 2009. Oct-Dec;13(4):432–6. doi: 10.1080/10903120902935256 . [DOI] [PubMed] [Google Scholar]
- 49.*Langabeer JR 2nd, Gonzalez M, Alqusairi D, Champagne-Langabeer T, Jackson A, Mikhail J, et al. Telehealth-Enabled Emergency Medical Services Program Reduces Ambulance Transport to Urban Emergency Departments. West J Emerg Med. 2016. Nov;17(6):713–720. doi: 10.5811/westjem.2016.8.30660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.*Larsson G, Holmén A, Ziegert K. Early prehospital assessment of non-urgent patients and outcomes at the appropriate level of care: A prospective exploratory study. Int Emerg Nurs. 2017. May;32:45–49. doi: 10.1016/j.ienj.2017.02.003 [DOI] [PubMed] [Google Scholar]
- 51.*Laukkanen L, Lahtinen S, Raatiniemi L, Ehrola A, Kaakinen T, Liisanantti J. Emergency department admission and mortality of the non-transported emergency medical service patients: a cohort study from Northern Finland. Emerg Med J. 2022. Jun;39(6):443–450. doi: 10.1136/emermed-2020-209914 [DOI] [PubMed] [Google Scholar]
- 52.*Lederman J, Lindström V, Elmqvist C, Löfvenmark C, Ljunggren G, Djärv T. Non-conveyance of older adult patients and association with subsequent clinical and adverse events after initial assessment by ambulance clinicians: a cohort analysis. BMC Emerg Med. 2021. Dec 11;21(1):154. doi: 10.1186/s12873-021-00548-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.*Magnusson C, Källenius C, Knutsson S, Herlitz J, Axelsson C. Pre-hospital assessment by a single responder: The Swedish ambulance nurse in a new role: A pilot study. Int Emerg Nurs. 2016. May;26:32–7. doi: 10.1016/j.ienj.2015.09.001 [DOI] [PubMed] [Google Scholar]
- 54.*Magnusson C, Herlitz J, Karlsson T, Axelsson C. Initial assessment, level of care and outcome among children who were seen by emergency medical services: a prospective observational study. Scand J Trauma Resusc Emerg Med. 2018. Oct 19;26(1):88. doi: 10.1186/s13049-018-0560-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.*Magnusson C, Herlitz J, Axelsson C. Patient characteristics, triage utilisation, level of care, and outcomes in an unselected adult patient population seen by the emergency medical services: a prospective observational study. BMC Emerg Med. 2020. Jan 30;20(1):7. doi: 10.1186/s12873-020-0302-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.*Mason S, Knowles E, Colwell B, Dixon S, Wardrope J, Gorringe R, et al. Effectiveness of paramedic practitioners in attending 999 calls from elderly people in the community: cluster randomised controlled trial. BMJ. 2007. Nov 3;335(7626):919. doi: 10.1136/bmj.39343.649097.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.*Nehme E, Nehme Z, Cox S, Smith K. Outcomes of paediatric patients who are not transported to hospital by Emergency Medical Services: a data linkage study. Emerg Med J. 2023. Jan;40(1):12–19. doi: 10.1136/emermed-2022-212350 [DOI] [PubMed] [Google Scholar]
- 58.*Oulasvirta J, Salmi H, Kuisma M, Rahiala E, Lääperi M, Harve-Rytsälä H. Outcomes in children evaluated but not transported by ambulance personnel: retrospective cohort study. BMJ Paediatr Open. 2019. Oct 23;3(1):e000523. doi: 10.1136/bmjpo-2019-000523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.*Paulin J, Kurola J, Koivisto M, Iirola T. EMS non-conveyance: A safe practice to decrease ED crowding or a threat to patient safety? BMC Emerg Med. 2021. Oct 9;21(1):115. doi: 10.1186/s12873-021-00508-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.*Peyravi M, Örtenwall P, Khorram-Manesh A. Can Medical Decision-making at the Scene by EMS Staff Reduce the Number of Unnecessary Ambulance Transportations, but Still Be Safe? PLoS Curr. 2015. Jun 30;7. doi: 10.1371/currents.dis.f426e7108516af698c8debf18810aa0a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.*Pringle RP Jr, Carden DL, Xiao F, Graham DD Jr. Outcomes of patients not transported after calling 911. J Emerg Med. 2005. May;28(4):449–54. doi: 10.1016/j.jemermed.2004.11.025 [DOI] [PubMed] [Google Scholar]
- 62.*Schmidt TA, Atcheson R, Federiuk C, Mann NC, Pinney T, Fuller D, Colbry K. Hospital follow-up of patients categorized as not needing an ambulance using a set of emergency medical technician protocols. Prehosp Emerg Care. 2001. Oct-Dec;5(4):366–70. doi: 10.1080/10903120190939526 [DOI] [PubMed] [Google Scholar]
- 63.*Schmidt MJ, Handel D, Lindsell CJ, Collett L, Gallo P, Locasto D. Evaluating an emergency medical services-initiated nontransport system. Prehosp Emerg Care. 2006. Jul-Sep;10(3):390–3. doi: 10.1080/10903120600725918 [DOI] [PubMed] [Google Scholar]
- 64.*Snooks H, Kearsley N, Dale J, Halter M, Redhead J, Cheung WY. Towards primary care for non-serious 999 callers: results of a controlled study of "Treat and Refer" protocols for ambulance crews. Qual Saf Health Care. 2004. Dec;13(6):435–43. doi: 10.1136/qhc.13.6.435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.*Supples MW, Liao M, O’Donnell DP, Duszynski TJ, Glober NK. Descriptive analysis of emergency medical services 72-hour repeat patient encounters in a single, Urban Agency. Am J Emerg Med. 2023. Mar;65:113–117. doi: 10.1016/j.ajem.2022.12.025 [DOI] [PubMed] [Google Scholar]
- 66.*Todd VF, Swain A, Howie G, Tunnage B, Smith T, Dicker B. Factors Associated with Emergency Medical Service Reattendance in Low Acuity Patients Not Transported by Ambulance. Prehosp Emerg Care. 2021. Jan 25:1–17. doi: 10.1080/10903127.2020.1862943 [DOI] [PubMed] [Google Scholar]
- 67.*Todd VF, Moylan M, Howie G, Swain A, Brett A, Smith T, et al. Predictive value of the New Zealand Early Warning Score for early mortality in low-acuity patients discharged at scene by paramedics: an observational study. BMJ Open. 2022. Jul 14;12(7):e058462. doi: 10.1136/bmjopen-2021-058462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.*Tohira H, Fatovich D, Williams TA, Bremner A, Arendts G, Rogers IR, et al. Which patients should be transported to the emergency department? A perpetual prehospital dilemma. Emerg Med Australas. 2016. Dec;28(6):647–653. doi: 10.1111/1742-6723.12662 [DOI] [PubMed] [Google Scholar]
- 69.*Tohira H, Fatovich D, Williams TA, Bremner AP, Arendts G, Rogers IR, et al. Is it Appropriate for Patients to be Discharged at the Scene by Paramedics? Prehospital emergency care. 2016;20(4):539–49. doi: 10.3109/10903127.2015.1128028 [DOI] [PubMed] [Google Scholar]
- 70.*Zachariah BS, Bryan D, Pepe PE, Griffin M. Follow-up and Outcome of Patients Who Decline or Are Denied Transport by EMS. Prehospital and Disaster Medicine. 1992;7(4):359–64. doi: 10.1017/S1049023X00039777 [DOI] [Google Scholar]
- 71.Cheng SY, Wang HT, Lee CW, Tsai TC, Hung CW, Wu KH. The characteristics and prognostic predictors of unplanned hospital admission within 72 hours after ED discharge. The American journal of emergency medicine. 2013;31(10):1490–4. doi: 10.1016/j.ajem.2013.08.004 [DOI] [PubMed] [Google Scholar]
- 72.Spangler D, Edmark L, Winblad U, Colldén-Benneck J, Borg H, Blomberg H. Using trigger tools to identify triage errors by ambulance dispatch nurses in Sweden: an observational study. BMJ open. 2020;10(3):e035004. doi: 10.1136/bmjopen-2019-035004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bradley CJ, Penberthy L, Devers KJ, Holden DJ. Health services research and data linkages: issues, methods, and directions for the future. Health Serv Res. 2010. Oct;45(5 Pt 2):1468–88. doi: 10.1111/j.1475-6773.2010.01142.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Goel MK, Khanna P, Kishore J. Understanding survival analysis: Kaplan-Meier estimate. Int J Ayurveda Res. 2010;1(4):274–8. doi: 10.4103/0974-7788.76794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Miles J, Jacques R, Turner J, Mason S. The Safety INdEx of Prehospital On Scene Triage (SINEPOST) study: the development and validation of a risk prediction model to support ambulance clinical transport decisions on-scene-a protocol. Diagn Progn Res. 2021;5(1):18. doi: 10.1186/s41512-021-00108-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bjorkman J, Laukkanen-Nevala P, Olkinuora A, Pulkkinen I, Nurmi J. Short-term and long-term survival in critical patients treated by helicopter emergency medical services in Finland: a registry study of 36 715 patients. BMJ open. 2021;11(2):e045642. doi: 10.1136/bmjopen-2020-045642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hauswald M. Can paramedics safely decide which patients do not need ambulance transport or emergency department care? Prehosp Emerg Care. 2002;6(4):383–6. doi: 10.1080/10903120290937978 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(XLSX)
(R)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.