Abstract
Objectives:
Precision medicine is data-driven healthcare tailored to individual patients based on their unique attributes, including biologic profiles, disease expressions, local environments, and socio-economic conditions. Emergency medicine (EM) has been peripheral to the precision medicine discourse, lacking both a unified definition of precision medicine and a clear research agenda. We convened a national consensus conference to build a shared mental model and develop a research agenda for precision EM.
Methods:
We held a conference to (1) define precision EM, (2) develop an evidence-based research agenda, and (3) identify educational gaps for current and future EM clinicians. Nine preconference workgroups (biomedical ethics, data science, health professions education, healthcare delivery and access, informatics, -omics, population health, sex and gender, and technology and digital tools), comprising 84 individuals, garnered expert opinion, reviewed relevant literature, engaged with patients, and developed key research questions. During the conference, each workgroup shared how they defined precision EM within their domain, presented relevant conceptual frameworks, and engaged a broad set of stakeholders to refine precision EM research questions using a multi-stage consensus-building process.
Results:
217 individuals participated in this initiative, of which 115 were conference day attendees. Consensus-building activities yielded a definition of precision EM and key research questions that comprised a new 10-year precision EM research agenda. The consensus process revealed three themes: (1) preeminence of data, (2) interconnectedness of research questions across domains, and (3) promises and pitfalls of advances in health technology and data science/artificial intelligence. The health professions education workgroup identified educational gaps in precision EM and discussed a training roadmap for the specialty.
Conclusion:
A research agenda for precision EM, developed with extensive stakeholder input, recognizes the potential and challenges of precision EM. Comprehensive clinician training in this field is essential to advance EM in this domain.
Introduction
Medicine is evolving toward personalized treatment of patients and their unique circumstances and illness. However, the data needed to truly individualize patient care has only become widely available in recent decades. Beginning with the Human Genome Project in 1990, there has been an exponential rise in the amount of information available about patients, their medical conditions, and the communities in which they live.1 In 2015, the Precision Medicine Initiative called for an in-depth understanding of patients and their illnesses in order to more precisely tailor treatments to an individual’s genetic, social, and disease features.2–8 More recently, the term precision health has been used to describe the application of precision medicine principles through a broader lens of health, beyond managing illness. Precision health is commonly defined as the use of genomic, biological, environmental, public health, and other data to “predict, prevent, and cure precisely.”9 Specialties such as oncology and cardiology are already deeply engaged in precision medicine, driven by the advancement of gene therapy and other directed treatments.6,10–13 For instance, genetic testing is an important tool in preventive cardiology that can be used to identify patients at high risk of cardiovascular disease and personalize the selection of lipid lowering therapies for them.14 Other specialties such as psychiatry and neurology are earlier in their adoption but advancing rapidly.15–18 The notion of incorporating precision medicine in clinical practice is foreign to most emergency physicians.
Emergency medicine (EM) has not integrated precision medicine to the extent that these other specialties have, in part because precision medicine is often thought of in the context of long-term treatment for patients planned by their outpatient clinicians; for example, targeting a specific tumor receptor as a component of chemotherapy. This has meant EM clinicians have been absent from discussions on how patient care can follow a “precision” paradigm.19–21 However, EM clinicians do recognize the importance of rapidly understanding their patients’ unique disease features and are experts at accounting for patient-specific factors when developing treatment plans for acutely ill and injured patients. Advances within the specialty have allowed for better understanding of how acute care needs of individual patients differ based on the unique manner in which their illnesses manifest and important factors such as social determinants of health.22–24 Thinking boldly about the future, new technologies will afford emergency physicians far more patient-specific data and the tools (e.g. artificial intelligence) necessary to interpret those data to improve our diagnostic accuracy and better tailor our treatment plans. Yet until now, EM has failed to construct a common understanding of precision medicine within the specialty.
Part of the challenge associated with adopting precision EM stems from concerns that providing acute, unscheduled care for undifferentiated, sick, and injured patients does not allow for enough time or information to develop data-driven patient assessments and tailored care plans. While rapidly digesting and responding to detailed data about our patients is a part of EM clinicians’ daily clinical work, our treatments have not been conceptualized as precision medicine. In addition, much of the data needed to tailor care for patients is lost in complex electronic health records, is mired in difficult to grasp social and environmental landscapes, may not be standardized across our specialty, or is unavailable during the emergency department (ED) visit. Furthermore, critics warn of ethical concerns related to data privacy and security, bias and discrimination, and degrading health equity.25 Therefore, there are challenges to address within our specialty, including a need for education regarding precision EM among most clinicians, a lack of usable tools for precision EM implementation, the need for large-scale training to teach clinicians how to access and use data streams needed for the precise care of patients in the ED, and limited research and literature on the topic.
There is no question that the technology needed to further individualize emergency care already exists, and it will advance and become even more powerful in just the next few years. There is a tremendous opportunity to improve acute care if our specialty learns to harness these tools appropriately; those who say this evolution is ‘not for EM’ abdicate the responsibility to do more for our patients if we can. There is an urgent need for the specialty to organize around a shared mental model of precision EM and to develop a research agenda that both conforms to our unique practice environment and is informed by our specific expertise. We organized and led the SAEM 2023 Consensus Conference as a national effort to respond to these needs and to map a path forward for our specialty during this rapid advent of precision EM. We challenged the conference participants to create a compelling and actionable compilation of research questions about precision EM that could be investigated in the coming decade. In this paper, we describe our approach to the definition of precision EM across domains and the development of a policy-relevant consensus research agenda for precision EM to help guide our specialty.
Methods
Study Design, Setting, and Population
We held a national consensus conference to generate a research agenda for precision EM at the Society for Academic Emergency Medicine (SAEM) Annual Meeting on May 16, 2023. Pre-conference participants each contributed to 1 of our 9 workgroups and included content experts in domains related to EM, medical librarians, and patient representatives. We recruited workgroup leads and members based on their scholarship and reputation, and we sought diversity of perspective by seeking pre-conference participants with focused attention to gender, racial, ethnic, generational, and geographic diversity in the identification of workgroup leads and participants. Diversity was reviewed repeatedly by the SAEM Consensus Conference Advisory Board and at the individual workgroup level. Each participant was an expert in the domain of their workgroup and we attempted to limit domain overlap, resulting in an overall cohort of researchers with a myriad of skills and backgrounds. Each workgroup had at least one member who had practical knowledge of precision medicine or relevant training and experiences. Conference day participants included most pre-conference participants, a small number of industry representatives from the technology sector, and interested attendees of the SAEM Annual Meeting. We advertised the conference using EM professional society listservs and SAEM Annual Meeting promotional materials and websites. We identified technology industry partners working in the data science, -omics, and health technology spaces by direct outreach to companies identified through SAEM, the Stanford Emergency Medicine Partnership Program, and recommendations from workgroup members. The industry representatives discussed available and emerging technologies relevant to precision health during the lunch break. They did not participate in pre-conference workgroup efforts. We invited them to join our conference day workgroup discussions to provide insights on technologies that could impact the final research questions, as industry has a unique perspective on regulatory and developmental hurdles regarding health technology. Four companies provided unrestricted educational stipends that we used to offset the cost of the conference. Additional funding was provided by SAEM, the Agency for Healthcare Research and Quality (AHRQ 1R13HS029275-01), Stanford University, and conference registration fees. The conference was open to the public, and we offered AMA Category 1 Continuing Medical Education credits.
Problem Identification
In 2019, we assembled a group of EM faculty members from a single academic medical center who had expertise across different disciplines including education, -omics, artificial intelligence (AI) and data science, population and global health, healthcare delivery and operations, prehospital care, and pediatrics. We convened regularly over a period of three months to examine the engagement of EM in the precision health movement and discuss the role precision medicine may play within the specialty in the coming decade. We identified precision health concepts that apply directly to the current and future practice of EM and concluded that a shared understanding of precision EM did not yet exist in a manner similar to other healthcare specialties. We identified the SAEM Consensus Conference as the best opportunity within EM to organize stakeholders to explore this practice gap and determine a path forward for our specialty.
We formed two subgroups, a precision EM definition development team and a SAEM Consensus Conference Advisory Board. Beginning in 2020, our definition team conducted a series of broad literature reviews and thought exercises to develop an operational definition of precision EM. At the SAEM Western Regional Conference in April 2022, our definition team shared preliminary results with the audience along with key drivers and obstacles to implementation (Figure 1). Following the positive audience response to the presentation at Western SAEM, our advisory board submitted a successful application to conduct the SAEM Consensus Conference in May 2023. The aims for the consensus conference were to (1) Develop a working definition and shared mental model of precision EM; (2) Establish a research agenda for precision EM for the specialty, and (3) Identify educational gaps that must be addressed for EM clinicians.
Figure 1:
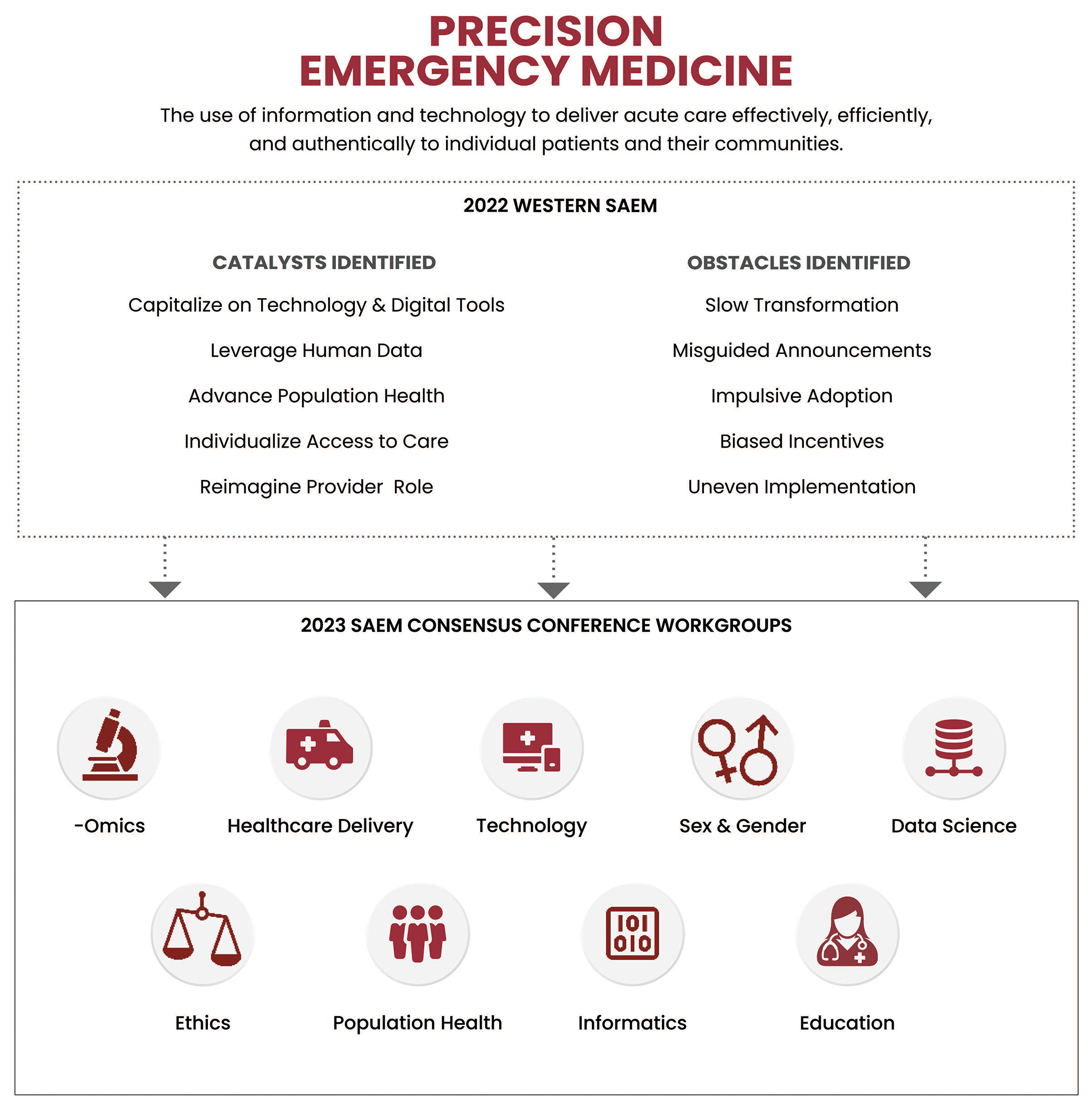
Precision Emergency Medicine Definition and Workgroups
Pre-Conference Workgroups and Literature Reviews
During Summer 2022, we identified nine key domains within precision EM and recruited a diverse group of thought leaders to study them (Figure 1). The workgroup chairs recruited team members from geographically diverse regions of the United States and Canada with input from the advisory board and each other (Supplementary Table 1). Workgroups consisted of six to eleven academic EM physicians with expertise in relevant domains, as evidenced by past publications, professional society presentations, and reputation. We enlisted volunteer library science professionals from six different institutions to support the research of eight workgroups. We also assigned a different member of the Stanford Patient and Family Advocacy Council to each of the workgroups to provide a patient perspective and inform their efforts. In October 2022, we held an in-person meeting of the workgroup leads at the ACEP Scientific Assembly in San Francisco to discuss the literature review process and identify areas of overlap and gaps across the workgroups.
In the months leading up to the consensus conference, each workgroup met regularly to prepare a draft set of research questions related to their domain based on literature reviews. The initial intent was for each workgroup to conduct standardized scoping reviews within their domains. However, preliminary efforts identified dramatic differences in the quality and quantity of research relevant to each workgroup. A number of initial reviews yielded sparse returns in both the academic and gray literature, which made full scoping reviews of limited value. Thus, the groups tailored their literature review methods at the workgroup level. For instance, there was insufficient literature about precision medicine to allow for scoping reviews by the population health, informatics, and health professions education workgroups. Thus, they developed numerous search strategies for a variety of different databases reflective of their specific workgroup needs. For example, the EM search strategies included terms specifically related to prehospital care, which was not pertinent to all groups. However, several of the shared strategies remained relatively unchanged among the workgroups, in particular, precision medicine and AI/machine learning. The different methodological approaches to literature reviews employed by each workgroup are summarized in Figure 2.
Figure 2: Workgroups Literature Review Methodologies.
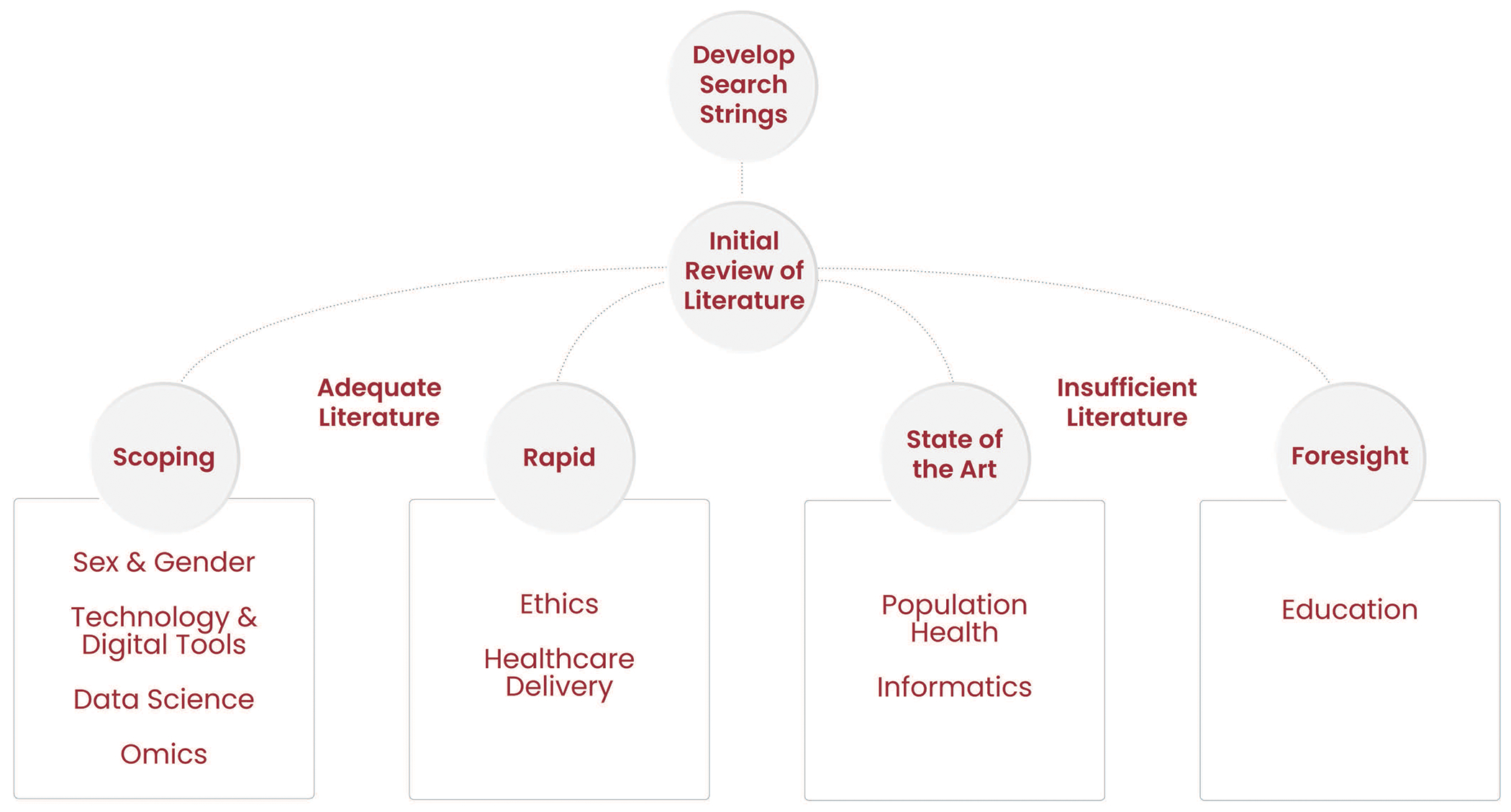
For domains in which the initial literature review produced adequate literature, scoping or rapid reviews were conducted. The purpose of a scoping review is to summarize the body of literature, identify key topics and concepts, and describe existing research efforts and directions. A rapid review uses a simplified but systematic approach to identify, select, and analyze data from the literature. For domains in which the initial review produced insufficient literature, the workgroups conducted a state-of-the-art review, which provides an overall summary of the latest knowledge in the domain, or a foresight review, which focuses on emerging trends and future directions within the domain.
Conference Day Consensus-building Process
We designed the general conference sessions to result in a shared mental model of precision EM for the participants to address Aim 1 of the conference. To accomplish Aim 2 (development of the research agenda), we used three rounds of breakout sessions to discuss, refine, and come to consensus on the final research questions (Figure 3). Participants self-selected which workgroup breakout sessions to attend. In the initial breakout session, the pre-conference workgroups presented results from the literature reviews they completed in the months leading up to the conference, their research question development processes, and a preliminary collection of proposed research questions. The second session brought together disparate workgroups for cross-pollination of expertise and insights from outside the individual workgroups’ domains. We anticipated that these sessions could develop novel research questions and opportunities for academic exploration. We collected newly developed concepts and questions at the intersection of the workgroups in a “parking lot” for further exploration and discussion during the post consensus conference process. In a third breakout session, the workgroups consolidated input on research questions and prioritized them at the individual workgroup level based on importance, urgency, and feasibility. Finally, we reconvened all conference attendees for a closing session, in which each workgroup developed a list of what they decided were the most important research questions, ranked in order of priority. Each workgroup lead presented their lists of prioritized research questions to all conference participants, who then independently provided further prioritization feedback using the upvoting / downvoting feature of Poll Everywhere (San Francisco, CA). After the conference, we collated individual participant input, workgroup discussions, and Poll Everywhere findings to identify the top three research questions developed by each working group. This process yielded the final, prioritized research questions that comprise the precision EM research agenda. Of note, we charged one of the nine workgroups (health professions education) with tailoring their efforts to address Aim 3 of the conference; their contributions to the final research agenda met this final aim.
Figure 3:
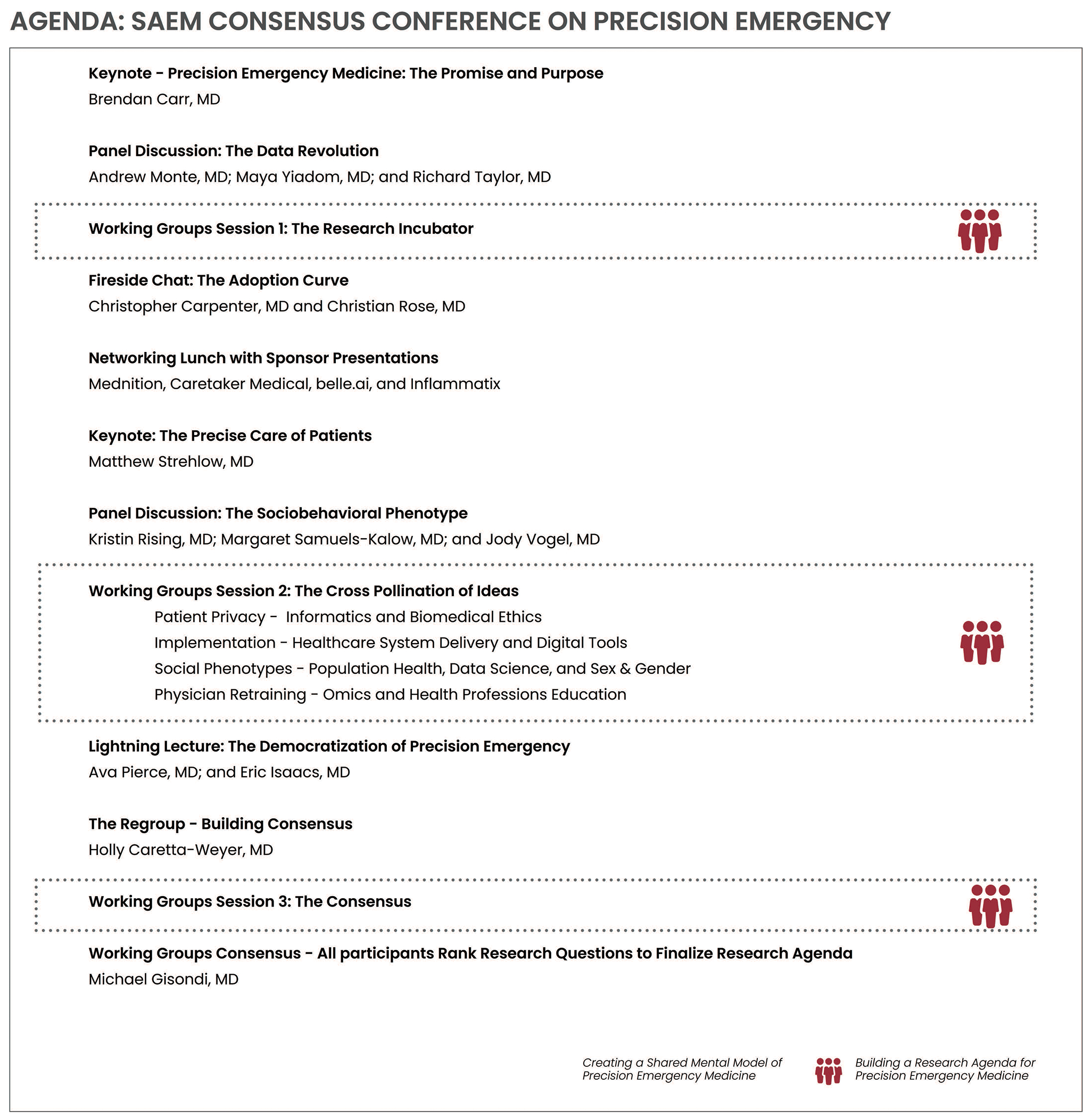
Consensus Conference Agenda
Primary Outcome
The primary conference outcome was a 10-year research agenda for precision EM developed and adopted through consensus among our participants. To build the research agenda, workgroups developed a preliminary list of questions to answer in the coming decade to advance a collective understanding and implementation of precision EM. The conference attendees then refined and agreed upon a final list of research questions, yielding the research agenda.
Results
Demographics
In total, 217 people contributed to this 4-year project. The consensus conference had 115 same-day participants from 53 academic institutions in the United States and Canada; most were emergency physicians who conduct research in a relevant domain. Participants involved in conference planning, pre-conference workgroups, and/or facilitation of the meeting included: 17 members of the definition team (16 academic emergency physicians and 1 PhD researcher who focuses on education,) 4 members of the consensus conference advisory board (all emergency physician researchers; 3 analyze large data sets routinely in their work), 14 workgroup leads (all emergency physician researchers with expertise in their respective workgroup domains,) 61 additional workgroup members that were academic emergency physicians with expertise in their respective workgroup domains, 7 research librarians, 7 patient representatives (most were retirees with college degrees or higher, none were physicians,) 5 technology industry representatives, 2 administrative staff, and 11 conference day student volunteers. Most but not all workgroup leads and members attended the consensus conference; none of the patient volunteers or research librarians attended. We did not solicit other demographic data from the participants.
Aim 1: Definition
A “Definitions Team” composed of academic emergency physicians from a single institution met monthly for 1 year to create a definition of precision EM.26 The definition was then presented at a Western Regional SAEM conference in Spring 2022. The definition was then further reviewed and discussed with workgroup leads and team members early in the consensus conference planning process. We introduced this draft definition of precision EM for consideration by all participants during a general session at the consensus conference. In the absence of negative feedback or suggested edits from the attendees, we adopted the working definition without changes. We define Precision Emergency Medicine as the use of information and technology to deliver acute care effectively, efficiently, and authentically to individual patients and their communities.
Aim 2: Research Agenda
Our teams and conference participants successfully developed a 10-year research agenda for precision EM composed of 27 consensus-derived questions across a broad set of domains (Table 1). This deliverable was the primary outcome of this project and met Aim 2 of the conference.
Table 1:
Research Agenda for Precision Emergency Medicine
| Workgroup Domain | Research Questions |
|---|---|
| Biomedical Ethics | 1. How should precision medicine be used to maximize patient benefit and continue medical progress without overburdening clinicians or putting institutional needs first? 2. How can data be used to provide the greatest societal benefit while allowing individuals to retain ongoing control of selected private information? 3. How do we minimize or prevent subsequent harm resulting from algorithms influenced by implicit bias and structural disparities for marginalized groups (homeless, drug addiction, people with mental illness, geographic, financial, technology access, other identities, clinician acceptance in certain areas or specialties)? |
| Data Science | 1. What precision EM care delivery problems are best addressed with machine learning and data sciences techniques? What needs to be considered to translate these solutions to bedside? 2. How can we reduce barriers to privacy and legal restrictions that make the initiation of single institution, and particularly multi-centered research, difficult? How can we use medical education and governance to work through these restrictions and build both clinician and patient trust? What processes are needed both in EM and in health systems to have successful implementation and maintenance? 3. What is limiting our ability to validate and generalize findings and methodologies to advance data sciences for precision EM care? How can we evolve best practice for data quality: Data standardization? Managing missing data? Monitoring practice and data shift? |
| Healthcare Delivery and Access to Care | 1. How should EDs and health systems integrate into the communities they serve (e.g., use of health information exchanges [HIEs]) and use prediction tools to better deliver care and optimize care transitions across care delivery spaces? a. What are best practices for identifying and engaging stakeholders and conducting research on and implementation of personalized medicine within emergency care delivery systems? 2. How do we integrate other clinicians and use bidirectional data transfer to optimize this system (e.g., prehospital providers, primary care offices, rehab facilities, etc.)? 3. What measures can be used to evaluate equity in the implementation of precision medicine within systems of emergency care? |
| Health Professions Education | 1. What is the future role of humans in medicine, and what skills do those clinicians need when using AI algorithms? What technologies will they need to practice precision emergency medicine? How do we teach trainees to act, reason, or think in the absence of precision medicine tools? 2. How do we incorporate the patient voice in clinician training in precision medicine? For example, which skills and clinician role (understander, explainer, collaborator, advocate, skeptic) will patients deem most important for learners to master? 3. What techniques are best for teaching interdisciplinary leadership skills, or so-called ‘fusion skills,’29 in undergraduate and graduate medical education settings to best prepare our trainees for the future AI workplace? Is there a developmental framework for trainees at different levels of medical and computer training? How will they find and convey information, and how will those skills enhance decision science? Which role will clinicians assume in their adoption of precision medicine: trainers, explainers, or sustainers? |
| Informatics | 1. What informatics systems can we employ to overcome the barriers of fragmented systems and improve acute unscheduled care? 2. How can we optimize information delivery and clinical summarization to improve safety and reduce cognitive overload for patients and clinicians? 3. How do we build collaborative data, information, and knowledge ecosystems to support dynamic, scalable solutions for emergency care? |
| Omics | 1. How can we best translate the findings of -omics research to the bedside to improve emergency medical care? 2. How can we construct the needed network/platform for emergency departments conducting multi-center -omics research? 3. How do we grow and develop the EM -omics research and implementation workforce? |
| Population Health and Social EM | 1. What are the best practices for precision social EM to ensure accountability and equity and prevent stigmatization, discrimination, and criminalization? 2. What are meaningful outcomes for precision social EM from the perspective of patients, the health system, and communities? 3. How do we leverage precision medicine to most effectively develop interventions to improve individual and population health? |
| Sex and Gender | 1. How can we translate relevant scientific research regarding sex and gender-specific care from other fields into EM in a timely manner? 2. How do changing sex hormone profiles (endogenous and exogenous) affect the presentation, diagnosis, treatment, and prognosis for emergency department patients across the lifespan? 3. How do patient and clinician gender identity (or other attributes) affect clinical decision making and implementation in EM? |
| Technology and Digital Tools | 1. Through the lens of precision EM, what are the greatest unmet needs that technologies and digital tools can enable EM to more quickly diagnose patients and identify the best therapeutic and disposition pathways? 2. How do we increase academic EM leading emerging technology research in collaboration with current and emergent technology companies focused on improving precision EM care? How do we create an innovations network that leverages institutional experience and economies of scale to allow academic clinicians and technology companies low barriers to collaborate on focus areas, study, and scale new technologies and tools? 3. How can we achieve consensus on a national framework for evaluating, adopting, and implementing precision EM tools and technologies, and what is the threshold of evidence needed to validate the usefulness of new technologies for their target populations? |
Aim 3: Educational Gaps
The Health Professions Education workgroup identified educational gaps for clinicians and formulated a set of relevant research questions to meet Aim 3 of the conference. These are included in Table 1. A separate manuscript describes the unique methodology employed by this workgroup, a detailed review of their research questions and other findings, and recommendations for how to move forward with large-scale clinician training.27
Discussion
Participants in the 2023 SAEM Consensus Conference built a shared mental model of precision EM and developed a 10-year precision EM research agenda. The consensus conference process — from conceptualization to post conference research agenda consolidation — benefited from strong stakeholder engagement, broad participation from across academic EM, and partnerships with patients and industry stakeholders. Data scientists, health services researchers, and other thought and research leaders in our field conceptualized a compelling path forward for the next decade and drafted a research agenda consisting of the most important, foundational questions that must be addressed for precision EM to take root.
Within the workgroups and conference sessions, participants agreed that precision medicine is accelerating rapidly, and for EM to grow in a way that maximally benefits patients and communities, the specialty now needs to be intentional and thoughtful in adapting and applying precision medicine’s core concepts and tenets. EM has made tremendous progress over recent decades in establishing itself as a core component of the modern healthcare system.28–30 It is imperative that the unique, foundational aspects of EM — those core to the specialty such as access to care, timely diagnosis and treatment, and social EM — be included in how precision EM is defined. As we advance into a new era of healthcare defined by AI and the use of deep troves of information about individual patients and their communities, EM must demonstrate the importance of its unique practice environment, knowledge base, and role in stewarding the health of the population by leading precision medicine efforts, not just for EM but for the entire house of medicine.
The research questions presented in Table 1 highlight the breadth of research avenues to be explored. Notably, there is little direct overlap among each workgroup’s research questions, likely resulting from the consensus-building methodology used and the fact that we defined precision EM somewhat broadly in order for it to be applicable to our specialty. However, we did identify three overarching themes that were consistent across the workgroups: (1) the preeminence of data, (2) the interconnectedness of research questions across the subdomains, and (3) the promises and pitfalls of advances in health technology and data science/AI.
Most pronounced among the themes, which was discussed by all workgroups and influenced many of the consensus-derived research questions, is the preeminence of data: including how to acquire, manage, utilize, and apply data within EM. Data that once was mostly unquantified and described as clinician “intuition” or “gestalt” is now being measured and formatted into billions of discrete data points.31 The scale of this individual patient-level data far outstrips our current clinicians’ and systems’ abilities to safely and effectively integrate routine data, as well as our ability to competently turn data analyses into actionable information for use at the bedside by EM clinicians when caring for individual patients.32 While there is a depth of data in certain EM domains, it is often not accessible in other key areas, for example, data on social drivers of health and learner performance. Existing data sources include local and externally accessible electronic health records; direct-to-consumer health companies like those offering genetic testing, activity tracking, and dietary support; public health records that range from local community data to large national datasets; environmental and climate data such as air quality, precipitation, and heat index; as well as data on risk-taking behaviors collected by insurance companies and found in legal records. These data are rarely shared across institutions due to privacy and ethical concerns.
AI and current data science tools could review the massive amounts of structured and unstructured data from these many sources and generate semi-cohesive stories. Data is not organized for existing AI tools however, and if AI is launched haphazardly, it will likely produce unintended, serious adverse consequences; we must refine these patient-relevant data for our purpose and amass meaningfully large datasets from these existing sources. Moreover, consistent safeguards are lacking to ensure that data is rigorously and ethically derived, high-quality, relevant, and trustworthy. As such, datasets used for AI or machine learning may be poor or incomplete, risking biased decision-making or errors.33 Consensus conference participants concluded that AI will fundamentally alter healthcare including EM, in a way that no advancement has since the advent of antibiotics. The research agenda constructed through the consensus conference process is an important step in guiding this data revolution in EM to improve the health of our patients as individuals, the wellness of our clinicians, and the equity of “health” within our communities.
A second theme identified from review of the research agenda is the interconnected nature of the research questions across the workgroup domains. While they may not overlap directly, answers from different workgroups will need to be integrated when considering how to best conduct research on and implement precision EM. For instance, to apply precision EM in a manner that limits biases and reduces disparities (Healthcare Delivery workgroup), we need clinicians who are trained to live at the intersection of clinical medicine and AI (Technology and Informatics workgroups). Correspondingly, any technologies or data underlying precision EM need to be developed and disseminated with a commitment to affordability, equity, and inclusion, so that specific clinician groups, areas of the country, and patients are not excluded from its benefit. The realization of the promise of -omics research will depend on new healthcare technology and delivery systems at the bedside. The interconnectedness and intersection of the workgroups’ research questions holds tremendous opportunity for further exploration as we move towards precision EM.
Finally, it was evident in the consensus process and resultant research agenda that both enthusiasm and caution are evoked by the idea of precision EM. Participants engaged in the consensus conference in high numbers — requiring us to close same-day conference registration — and participants vigorously debated how to best define and further research the field of precision EM through multiple lenses. Enthusiasm was reflected in many of the research questions, such as, “Through the lens of precision EM, what are the greatest unmet needs that technologies and digital tools can enable EM to more quickly diagnose patients and identify their best therapeutic and disposition pathways?” However, other questions reflected participants’ caution. For example, the Biomedical Ethics and Social and Population Health workgroups’ outcomes included questions such as “How will you teach trainees to be able to still act, reason, or think in the absence of precision medicine tools? and What is the ROLE of HUMANS in medicine and what skills do those humans need in the setting of AI algorithms?” A balance of these somewhat competing attitudes/views will allow our specialty to best leverage this energy on behalf of our patients and future practitioners to advance the specialty to unimagined heights. However, EM clinicians will need to lead and engage in the process of deploying precision EM to avoid negative outcomes.
With this work, we introduced the relatively new concept of precision EM to our specialty and identified the scope of research efforts that lie ahead in the next decade. The research agenda was derived through the consensus of many thought leaders and productive investigators in our field, and as such, should be viewed as authoritative and contemporary. Now, there is an urgency to disseminate these research questions to relevant funding agencies so the work of researching how to best integrate precision EM into our daily practice can begin in earnest. Therefore, we will strategically disseminate our new precision EM research agenda to potential funding agencies who support EM investigators in the various domains represented by our working groups (e.g., health services research, biomedical ethics, health professions education.) These will include the Society for Academic Emergency Medicine, Emergency Medicine Foundation, AHRQ, the NIH All of Us initiative along with other relevant NIH sections, and other EM professional societies. It is likely that precision EM has not been considered previously among their funding priorities. We will also leverage dissemination strategies for new research findings offered by AHRQ to its funded investigators. Our goal is to educate key decision-makers at these agencies about our precision EM research agenda and inspire them to offer new lines of funding for this transformative work.
Big data and machine learning are slowly and somewhat inconspicuously being inserted into the practice of EM already. Implementation science to apply data to patient care was discussed across workgroups; without integration of implementation science principles into our future efforts, it is unlikely that we will achieve the full promise of precision EM. Implementation scientists will be key partners to ensure the systematic uptake of future research findings into the routine practice of all emergency physicians. Their dissemination of best practices, once derived by translational and health services researchers, will promote the execution of precision EM in acceptable ways and improve quality of acute care. However, without the involvement and engagement of EM leaders, these tools will not be fully adopted, or will be adopted in maladaptive fashion. We must conduct the necessary research outlined in the newly derived agenda soon to expand the capabilities precision medicine offers into the emergency department to benefit patients with urgent and emergent health needs.
Finally, precision EM is a novel approach to the care of the acutely ill and injured. While it builds directly on EM fundamentals, it demands adoption of new technology — likely including AI — and alternative models of acute care delivery. We envision a future in which emergency physicians skillfully leverage AI to analyze complex, voluminous patient data in order to personalize diagnostic testing, risk stratification, therapeutics, and care plans (Box 1). However, without evidence-based implementation strategies, we will fail to realize the promise of precision EM and instead be stymied by misused technologies, bias, error and inequity. We believe our consensus-driven research agenda will help us keep the wellbeing of our patients and our clinicians at the forefront of these paradigm shifts.
Box 1: The Promise of Precision Emergency Medicine.
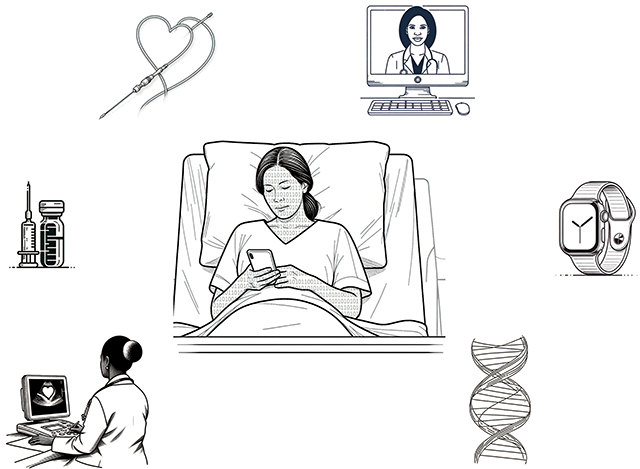
A 47-year-old woman from South Asia has a video visit with an EM provider for severe, general fatigue. She grew up in a household with open stove cooking and lives with a smoker. Her step counter shows reduced steps and pace over the past week. The ambient temperature is over 40 degrees Celsius. The AI-enabled, real-time transcription and decision support flags an elevated cardiac risk based on her genetic profile, rhythm strip and social and environmental drivers of health - the physician counsels her to be brought immediately to the ED. Initial ECG and triage troponin are non-diagcardiac but within five minutes the ED’s continuous cardiac monitor AI algorithm detects early indicators of ST elevation. Bedside echo by the ED provider simultaneously interpreted by the physician and AI detect regional wall motion abnormality. Tele-cardiology is notified. Dual antiplatelet therapy is selected based on her pharmacogenetic profile and the patient is quickly transferred to the interventional cardiology lab.
Limitations
While the consensus process met our intended aims, the time constraints of a single-day conference allowed for a relatively brief discussion of the intersections between workgroups (45 min); more time would have afforded a deeper exploration of key research questions that may arise at these points of intersection. We allowed flexibility in the approach to literature reviews and question derivation, leveraging group expertise to define appropriate review methods most suited to the topic and available evidence. This approach may have limited the consistency of rigor in the literature review process across workgroups and may make consolidation and reporting of the research agenda development more challenging.
We discussed domains within precision EM extensively and our deliberations formed the framework for the workgroups. Identifying the correct breadth and specificity when constructing the workgroups was naturally an imperfect task and potentially created areas of overlap among workgroups (e.g., informatics and data science) and left out important subfields. For instance, age was identified as an important subfield during the initial in-person planning but was not added as a tenth workgroup. It was agreed upon by workgroup leads that they would consider age within their specific domains. Despite this approach, there likely remains significant opportunity within the precision EM research agenda to build questions centered on aging. A similar discussion took place with regard to social determinants of health, health disparities, and population health, with these topics being addressed within each workgroup rather than as its own domain given the topic’s cross-cutting nature. Of note, the results of the 2022 SAEM Consensus Conferences focused on race and population health were not available at the time we formed our nine working groups. We determined that a specific workgroup to examine racism through the lens of precision EM would be premature and did not, therefore, include a separate workgroup on racism and instructed all workgroups to consider racism within their specific subfield. An important outcome of the workgroups, which was not presented in this paper, is an analysis of how precision EM applies to each domain. We anticipate this work will be presented in future publications by each workgroup.
Conclusions
Precision Emergency Medicine is the use of information and technology to deliver acute care effectively, efficiently, and authentically to individual patients and their communities. The 2023 SAEM Consensus Conference on precision emergency medicine resulted in a 10-year research agenda to guide the adoption of this practice paradigm, built through broad stakeholder engagement. Emergency medicine must thoughtfully engage in the precision medicine movement in order to optimize the inevitable practice changes ahead of us and thus redefine acute care for our specialty once more.
Supplementary Material
Acknowledgements
We wish to acknowledge administrative support of the Society of Academic Emergency Medicine (SAEM) in organizing and hosting the SAEM Consensus Conference on “Precision Emergency Medicine: Building a Research Agenda” on May 16, 2023. We also thank the volunteer scribes who gave their time to record the proceedings at the conference day and the patient advisory committee for their guidance and help throughout the process. We also acknowledge and thank Melissa McMillian CAE, CNP, for her expertise, guidance and grace, commitment to excellence and work in preparing the conference and obtaining grant funding for the final conference. The authors wish to acknowledge the invaluable participation of all the attendees of the 2023 SAEM Consensus Conference, without whom this work would not be possible. Lastly, a special thanks to all workgroup members (Supplementary Table 1).
Financial support:
Funding for this conference was made possible [in part] by the Society for Academic Emergency Medicine (SAEM) and by grant R13HS029275 from the Agency for Healthcare Research and Quality (AHRQ). The views expressed in written conference materials or publications and by speakers and moderators do not necessarily reflect the official policies of the Department of Health and Human Services; nor does mention of trade names, commercial practices, or organizations imply endorsement by the U.S. Government. Funding was also provided by Stanford University Department of Emergency Medicine, industry sponsors, and conference registration fees. Industry sponsors had no role in planning the conference or in determining the final outputs of the consensus process. Conference registration fees were managed by SAEM.
Conflicts of Interest:
MS, MAG, and MCH are Consensus Conference co-chairs and received 2% FTE salary from the SAEM conference budget. There were no financial incentives based on conference registrations or evaluations.
MG is supported by grant funding to Stanford from The Agency for Healthcare Quality and Research (AHRQ 1R13HS029275-01).
TMC reports grant support to McMaster University from the PSI Foundation and Medical Council of Canada, and received payment from the Association of American Medical Colleges for writing part of the manuscript.
AJ reports grant funding to University of California, Davis, from NIH for investigator-initiated research.
DK has received money from Cook Medical for providing staff educational materials and from Brainbox, Rebion, Philips, and Veralox for investigator-initiated research. He also serves on the scientific advisory boards of Brainbox and Rebion, and receives stock options as compensation.
ATL reports grant funding to Duke University for investigator-initiated research from Roche Diagnostics, Inc., Abbott Laboratories, Quidel Inc., Brainbox Inc., Forest Devices, Inc., Becton Dickenson, SENSE Neuro Diagnostics, Ophirex, Inc., and Jiaxing Wisetest Biotech, Co.
AP is a SAEM Board of Directors Member at Large and receives support from the SAEM Foundation/Academy for Diversity and Inclusion in Emergency Medicine and the National Heart, Lung and Blood Institute.
All other authors declare no conflicts of interest.
Footnotes
Previous presentations: None
References
- 1.Wilson B, Nicholls SG. The Human Genome Project, and recent advances in personalized genomics. RMHP 2015;9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Research Council (US) Committee on A Framework for Developing a New Taxonomy of Disease. Toward Precision Medicine: Building a Knowledge Network for Biomedical Research and a New Taxonomy of Disease [Internet]. Washington (DC): National Academies Press (US); 2011. [cited 2019 Oct 14]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK91503/ [PubMed] [Google Scholar]
- 3.Collins FS, Varmus H. A New Initiative on Precision Medicine. N Engl J Med 2015;372(9):793–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dzau VJ, Ginsburg GS. Realizing the Full Potential of Precision Medicine in Health and Health Care. JAMA 2016;316(16):1659. [DOI] [PubMed] [Google Scholar]
- 5.Feero WG, Wicklund CA, Veenstra D. Precision Medicine, Genome Sequencing, and Improved Population Health. JAMA 2018;319(19):1979. [DOI] [PubMed] [Google Scholar]
- 6.Kass-Hout TA, Stevens LM, Hall JL. American Heart Association Precision Medicine Platform. Circulation 2018;137(7):647–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gilard V, Derrey S, Marret S, Bekri S, Tebani A. Precision Neurosurgery: A Path Forward. JPM 2021;11(10):1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Introduction – Precision Surgery. European Journal of Surgical Oncology (EJSO) 2017;43(5):iii. [Google Scholar]
- 9.Minor L. Discovering Precision Health: Predict, Prevent and Cure to Advance Health and Wellbeing. 1st ed. Hoboken, NJ, USA: Wiley-Blackwell; 2020. [Google Scholar]
- 10.Kikano S. Precision Medicine in Pediatric Cardiology. Pediatric Annals 2022;51(10):e390–5. [DOI] [PubMed] [Google Scholar]
- 11.Weldy CS, Ashley EA. Towards precision medicine in heart failure. Nat Rev Cardiol 2021;18(11):745–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tsimberidou AM, Fountzilas E, Nikanjam M, Kurzrock R. Review of precision cancer medicine: Evolution of the treatment paradigm. Cancer Treatment Reviews 2020;86:102019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mateo J, Steuten L, Aftimos P, et al. Delivering precision oncology to patients with cancer. Nat Med 2022;28(4):658–65. [DOI] [PubMed] [Google Scholar]
- 14.Lee S-H. Role of Genetics in Preventive Cardiology: Focused on Dyslipidemia. Korean Circ J 2021;51(11):899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ashina M, Terwindt GM, Al-Karagholi MA-M, et al. Migraine: disease characterisation, biomarkers, and precision medicine. The Lancet 2021;397(10283):1496–504. [DOI] [PubMed] [Google Scholar]
- 16.Keshavan MS, Clementz BA. Precision medicine for psychosis: a revolution at the interface of psychiatry and neurology. Nat Rev Neurol [Internet] 2023. [cited 2023 Jul 6];Available from: https://www.nature.com/articles/s41582-023-00788-0 [DOI] [PubMed]
- 17.Hampel H, Gao P, Cummings J, et al. The foundation and architecture of precision medicine in neurology and psychiatry. Trends in Neurosciences 2023;46(3):176–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Williams LM, Hack LM. A precision medicine–based, ‘fast-fail’ approach for psychiatry. Nat Med 2020;26(5):653–4. [DOI] [PubMed] [Google Scholar]
- 19.Limkakeng AT, Monte AA, Kabrhel C, et al. Systematic Molecular Phenotyping: A Path Toward Precision Emergency Medicine? Acad Emerg Med 2016;23(10):1097–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schultebraucks K, Shalev AY, Michopoulos V, et al. A validated predictive algorithm of post-traumatic stress course following emergency department admission after a traumatic stressor. Nat Med 2020;26(7):1084–8. [DOI] [PubMed] [Google Scholar]
- 21.Taylor RA, Pare JR, Venkatesh AK, et al. Prediction of In-hospital Mortality in Emergency Department Patients With Sepsis: A Local Big Data–Driven, Machine Learning Approach. Acad Emerg Med 2016;23(3):269–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stopyra JP, Riley RF, Hiestand BC, et al. The HEART Pathway Randomized Controlled Trial One-year Outcomes. Academic Emergency Medicine 2019;26(1):41–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wolf SJ, McCubbin TR, Feldhaus KM, Faragher JP, Adcock DM. Prospective validation of wells criteria in the evaluation of patients with suspected pulmonary embolism. Annals of Emergency Medicine 2004;44(5):503–10. [DOI] [PubMed] [Google Scholar]
- 24.Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the Early Management of Patients With Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke [Internet] 2019. [cited 2023 Oct 9];50(12). Available from: https://www.ahajournals.org/doi/10.1161/STR.0000000000000211 [Google Scholar]
- 25.Ahmed L, Constantinidou A, Chatzittofis A. Patients’ perspectives related to ethical issues and risks in precision medicine: a systematic review. Front Med 2023;10:1215663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Strehlow M, Alvarez A, Blomkalns AL, et al. Precision Emergency Medicine. Academic Emergency Medicine In Review. [DOI] [PubMed] [Google Scholar]
- 27.Chan T, Thoma B, Finnell J, et al. Precision Medicine within Health Professions Education: Defining a Research Agenda for Emergency Medicine using a Foresight and Strategy Technique (FaST) Review. AEM Education and Training Accepted 2/11/24:In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tadesse Gebremedhin L, Nsanzimana S, Lamin Samateh A, et al. A call to invest in emergency, critical and operative care for universal health coverage. Nat Med 2023;29(7):1591–2. [DOI] [PubMed] [Google Scholar]
- 29.Jamison DT, Gelband H, Horton S, et al. Disease Control Priorities, Third Edition (Volume 9): Improving Health and Reducing Poverty [Internet]. Washington, DC: World Bank; 2017. [cited 2024 Apr 1]. Available from: http://hdl.handle.net/10986/28877 [Google Scholar]
- 30.Zink BJ. Anyone, Anything, Anytime: A History of Emergency Medicine. 2nd ed. American College of Emergency Physicians; 2018. [Google Scholar]
- 31.Vigilante K, Escaravage S, McConnell M. Big Data and the Intelligence Community — Lessons for Health Care. N Engl J Med 2019;380(20):1888–90. [DOI] [PubMed] [Google Scholar]
- 32.Davenport T, Kalakota R. The potential for artificial intelligence in healthcare. Future Healthc J 2019;6(2):94–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rose C, Barber R, Preiksaitis C, et al. A Conference (Missingness in Action) to Address Missingness in Data and AI in Health Care: Qualitative Thematic Analysis. J Med Internet Res 2023;25:e49314. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


