Abstract
目的
比较I.D.E.A.L技术与经胫骨隧道(transtibial,TT)技术重建前交叉韧带(anterior cruciate ligament,ACL)的疗效。
方法
回顾分析2020年1月—2022年9月收治且符合选择标准的60例ACL损伤患者临床资料。患者均接受关节镜下自体肌腱重建ACL,术中股骨隧道定位采用I.D.E.A.L技术30例(I.D.E.A.L组)、TT技术30例(TT组)。两组患者年龄、性别、身体质量指数、致伤原因、损伤侧别、受伤至手术时间、合并软骨及半月板损伤构成比以及术前Lysholm评分、国际膝关节文献委员会(IKDC)评分、疼痛视觉模拟评分(VAS)、胫骨前移差值、Blumensaat角等基线资料比较,差异均无统计学意义(P>0.05)。记录住院时间、术后早/远期并发症发生情况,采用Lysholm评分、IKDC评分及VAS评分评价膝关节功能及疼痛程度,测量胫骨前移差值;MRI复查观察移植物愈合情况,并测量移植物股骨端、中段、胫骨端信噪比(signal to noise quotien,SNQ)值,以及膝关节Blumensaat角。计算胫骨前移差值以及Blumensaat角的手术前后差值(变化值)进行组间比较。
结果
术后两组切口均Ⅰ期愈合,住院时间组间差异无统计学意义(P>0.05)。患者均获随访,随访时间12~18个月,平均14.9个月。术后两组膝关节Lysholm评分、IKDC评分均较术前增加,VAS评分降低,其中TT组术后1周VAS评分与术前差异无统计学意义(P>0.05),其余评分两组组内与术前差异均有统计学意义(P<0.05)。术后随时间延长,两组上述评分均呈进一步改善趋势;Lysholm评分、VAS评分术后1周及1、3、6、12个月间差异均有统计学意义(P<0.05),IKDC评分仅术后1个月与术后1周差异有统计学意义(P<0.05)。术后1周I.D.E.A.L组膝关节Lysholm评分、IKDC评分高于TT组、VAS评分更低,差异均有统计学意义(P<0.05);1、3、6、12个月两组间差异均无统计学意义(P>0.05)。术后12个月,两组胫骨前移差值均较术前降低(P<0.05);且I.D.E.A.L组变化值高于TT组,差异有统计学意义(P<0.05)。 I.D.E.A.L组术后早、远期并发症发生率均低于TT组(P<0.05)。术后12个月MRI检查示两组膝关节移植物均生存良好,Blumensaat角均较术前降低(P<0.05),且I.D.E.A.L组Blumensaat角变化值以及移植物股骨端、中段、胫骨端SNQ值均高于TT组(P<0.05)。
结论
采用I.D.E.A.L技术重建ACL术后早期疗效更好,膝关节稳定性更高,术后并发症率更低;但采用TT技术重建术后移植物成熟度更高。
Keywords: 关节镜, 前交叉韧带重建, I.D.E.A.L技术, 经胫骨隧道技术, 移植物
Abstract
Objective
To compare the effectiveness of I.D.E.A.L technique and transtibial (TT) technique in anterior cruciate ligament (ACL) reconstruction.
Methods
A clinical data of 60 patients with ACL injury, who were admitted and met the selection criteria between January 2020 and September 2022, was retrospectively analyzed. All patients underwent arthroscopic ACL reconstruction with autologous tendon. During operation, the femoral tunnel was prepared by using I.D.E.A.L technique in 30 cases (I.D.E.A.L group) and using TT technique in 30 cases (TT group). There was no significant difference in baseline data such as age, gender, body mass index, cause of injury, injured side, interval from injury to operation, constituent ratio of combined cartilage and meniscus injury, and preoperative Lysholm score, International Knee Documentation Committee (IKDC) score, visual analogue scale (VAS) score, anterior tibial translation difference, and Blumensaat angle between the two groups (P>0.05). The length of hospital stay and the occurrence of early and late complications were recorded. During follow-up, the Lysholm score, IKDC score, and VAS score were used to evaluate knee joint function and pain degree, and the anterior tibial translation difference was measured. MRI reexamination was performed to observe the healing of the graft, and the signal to noise quotient (SNQ) values of the femoral end, middle section, and tibial end of the graft, as well as the Blumensaat angle of the knee joint were measured. The differences in tibial anterior translation difference and Blumensaat angle before and after operation (change values) were calculated and compared between the two groups.
Results
The incisions in both groups healed by first intention after operation, and there was no significant difference in the length of hospital stay between the two groups (P>0.05). All patients were followed up 12-18 months, with an average of 14.9 months. The Lysholm score and IKDC score of the knee joint in both groups after operation increased when compared with those before operation, and the VAS score decreased. Compared to preoperative scores, except for the VAS score of the TT group at 1 week after operation (P>0.05), there were significant differences in all scores at different time points postoperatively in the two groups (P<0.05). The above scores in both groups showed a further improvement trend with the prolongation of time after operation. There were significant differences in Lysholm score and VAS score among 1 week, 1 month, 3 months, 6 months, and 12 months after operation in the two groups (P<0.05). The IKDC score of both groups at 1 month after operation was significantly different from that at 1 week after operation (P<0.05). At 1 week after operation, the Lysholm score and IKDC score in the I.D.E.A.L group were significantly higher than those in the TT group (P<0.05), and the VAS score was significantly lower (P<0.05); there was no significant difference between the two groups at 1, 3, 6, and 12 months after operation (P>0.05). At 12 months after operation, the anterior tibial translation differences in both groups were significantly lower than those before operation (P<0.05); and the change value in the I.D.E.A.L group was significantly higher than that in the TT group (P<0.05). The incidences of early and late complications in the I.D.E.A.L group were significantly lower than those in the TT group (P<0.05). At 12 months after operation, MRI examination showed that the grafts of the knee joint in both groups survived well, and the Blumensaat angles of both groups were significantly smaller than those before operation (P<0.05). The change value of the Blumensaat angle in the I.D.E.A.L group was significantly higher than that in the TT group (P<0.05). The SNQ values of the femoral end, middle section, and tibial end of the graft in the I.D.E.A.L group were significantly higher than those in the TT group (P<0.05).
Conclusion
The early effectiveness of ACL reconstruction by using the I.D.E.A.L technique is better, the knee joint is more stable, and the incidence of postoperative complication is lower. However, the maturity of the graft after reconstruction using the TT technique is higher.
Keywords: Arthroscopy, anterior cruciate ligament reconstruction, I.D.E.A.L technique, transtibial technique, graft
前交叉韧带(anterior cruciate ligament,ACL)是维持膝关节稳定性的重要韧带之一,具有限制胫骨前移及维持旋转的功能[1]。跑步、跳跃等运动过程中如突然减速或改变方向,身体惯性会对膝关节施加较大剪切应力,常导致ACL损伤[2]。而损伤后如不及时治疗,会引起膝关节不稳、慢性关节疾病及软组织损伤等问题[3-4]。关节镜下重建是目前治疗ACL损伤的主要方法[5],但对于重建移植物类型及固定方式、骨隧道定位点以及术后康复方案等方面,均未达成共识[6-8]。其中,ACL重建术中股骨隧道定位点是目前研究热点。经胫骨隧道(transtibial,TT)技术是采用“过顶点”进行股骨隧道定位,由于手术操作简便、手术时间短等优势,在临床获得广泛应用[9-10],但因移植物不能放置于股骨侧ACL解剖中心附近,存在术后膝关节不稳风险,是其最大不足[11-13]。I.D.E.A.L技术是近年来提出的新理念,基于ACL股骨止点解剖学、组织学、等距性、生物力学和临床数据,提出股骨隧道位点应具有等距性(Isometric)、覆盖ACL股骨直接止点(Direct insertion)、偏离中心定位于足印区的前(高)和近(深)区(Eccentrically located),从而使股骨止点位于解剖(Anatomical)足印区内并保证屈伸过程中的低张力性(Low tension),简称“I.D.E.A.L”;采用该技术可将股骨隧道内口定位于原生ACL足印区内[14-15],弥补了TT技术上述不足。但目前两种技术用于ACL重建的疗效比较研究较少。为此,我们进行了一项回顾性研究,以期为临床术式选择提供参考。报告如下。
1. 临床资料
1.1. 一般资料
患者纳入标准:① 有明显外伤史;② 单侧膝关节ACL损伤,且经MRI检查示ACL损伤、断裂信号;③ 以自体半腱肌与股薄肌腱作为移植物行ACL重建;④ 临床资料完整。排除标准:① 年龄<18岁、>50岁;② 合并同侧膝关节其余韧带损伤;③ 合并Ⅰ度以上软骨损伤、Ⅱ度以上半月板损伤;④ 患侧有ACL重建手术史;⑤ 患有精神类疾病或依从性较低、不配合随访。
2020年1月—2022年9月,共60例患者符合选择标准纳入研究。关节镜下ACL重建术中股骨隧道定位采用I.D.E.A.L技术30例(I.D.E.A.L组)、TT技术30例(TT组)。两组患者年龄、性别、身体质量指数、致伤原因、损伤侧别、受伤至手术时间、合并软骨及半月板损伤构成比以及术前Lysholm评分、国际膝关节文献委员会(IKDC)评分、疼痛视觉模拟评分(VAS)、胫骨前移差值、Blumensaat角等基线资料比较,差异均无统计学意义(P>0.05)。见表1。
表 1.
Comparison of baseline data between the two groups (n=30)
两组基线资料比较(n=30)
| 基线资料 Baseline data |
I.D.E.A.L组 I.D.E.A.L group |
TT组 TT group |
统计值 Statistical value |
P值 P value |
| 性别(男/女,例) | 20/10 | 22/8 | χ2=0.317 | 0.573 |
| 年龄(x±s,岁) | 29.06±7.12 | 27.84±7.46 | t=0.648 | 0.520 |
| 身体质量指数(x±s,kg/m²) | 20.44±1.31 | 20.73±1.36 | t=−0.816 | 0.418 |
| 致伤原因(运动伤/其他,例) | 19/11 | 23/7 | χ2=1.270 | 0.260 |
| 损伤侧别(左侧/右侧,例) | 12/18 | 16/14 | χ2=1.071 | 0.301 |
| 受伤至手术时间(x±s,d) | 10.06±2.80 | 9.93±3.05 | t=0.176 | 0.861 |
| 合并软骨及半月板损伤 [例(%)] | 7(23.33) | 5(16.17) | χ2=0.417 | 0.519 |
| 术前Lysholm评分(x±s,分) | 42.2±10.3 | 43.3±10.4 | t=−0.399 | 0.691 |
| 术前IKDC评分(x±s,分) | 35.9±9.4 | 35.5±8.2 | t=0.183 | 0.855 |
| 术前VAS评分(x±s,分) | 5.3±1.5 | 5.5±1.7 | t=−0.328 | 0.744 |
| 术前胫骨前移差值(x±s,mm) | 4.88±0.59 | 4.91±0.74 | t=−0.180 | 0.858 |
| 术前Blumensaat角(x±s,°) | 18.77±2.40 | 18.27±2.29 | t=0.825 | 0.413 |
1.2. 手术方法
两组手术均由同一外科团队完成。全身麻醉或蛛网膜下腔阻滞麻醉下,患者取仰卧位,患肢大腿根部束气压止血带,设定压力45 kPa、时间90 min,常规消毒、铺巾。
① 取前内侧、前外侧入路放置关节镜,行关节镜下检查,通过刨削系统和等离子射频刀清理滑膜、血凝块和部分髌下脂肪垫,进一步明确诊断;清理ACL胫骨及股骨止点,暴露股骨隧道定位点。
② 取腱方法:于患肢胫前内侧3.0 cm作斜形切口,逐层分离皮下组织,显露半腱肌、股薄肌腱,取腱器取出肌腱后用爱惜邦缝线编织处理成6股单束结构,放置生理盐水中备用。
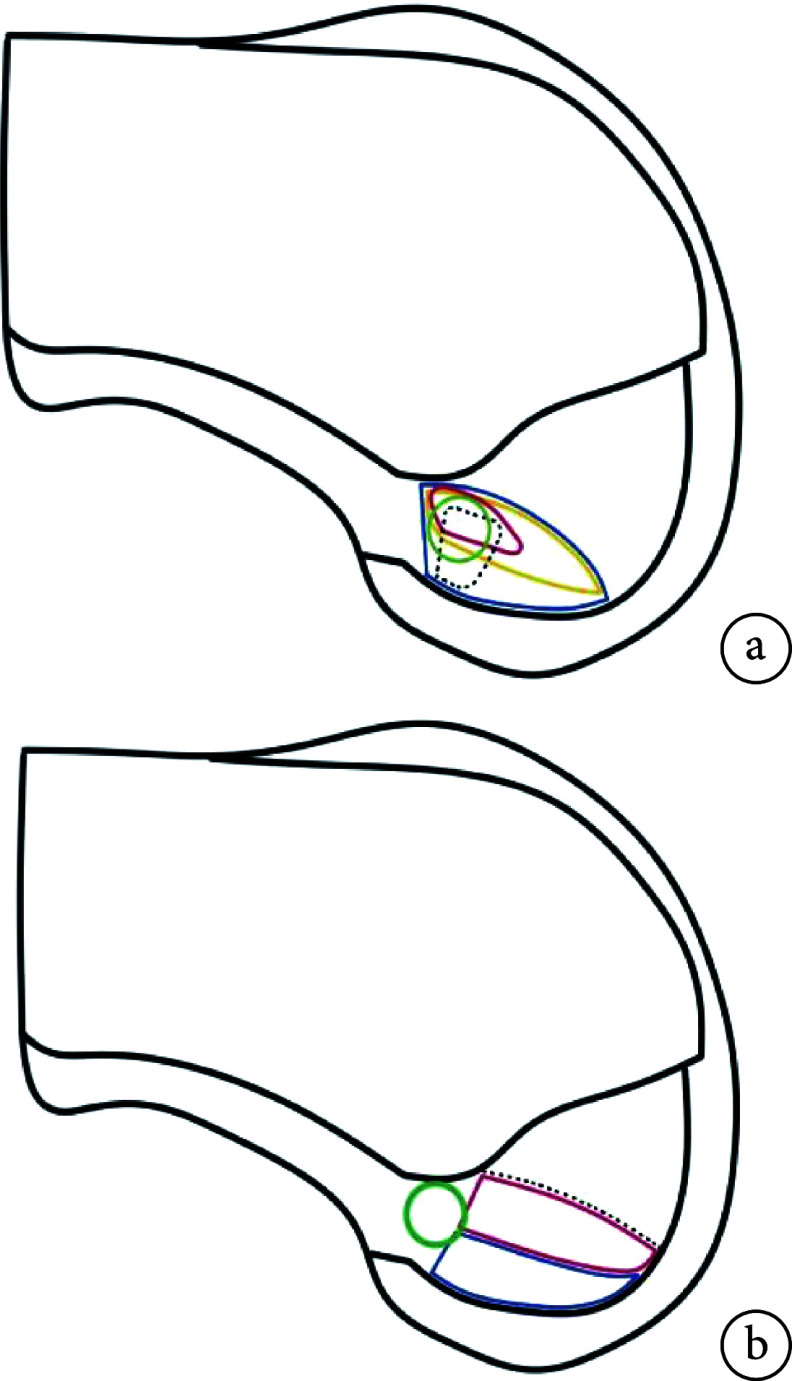
③ 骨隧道制备:两组胫骨隧道制备方法一致。屈膝90°,胫骨定位器调至55°,定位至胫骨止点残端,用钻头沿导针钻通胫骨侧形成胫骨隧道。股骨隧道制备:I.D.E.A.L组“4”字位放置膝关节,股骨定位器穿过前内侧入路。屈曲膝关节至130°,将引导器置于股骨髁间切迹后缘前方6 mm处。通过钻头构建“骨窝”结构股骨隧道。TT组首先将股骨定位器穿过胫骨隧道放置,膝关节屈曲90° 时定位至股骨髁间窝“过顶点”位置;通过钻头构建“骨窝”结构股骨隧道。定位示意图见图1。
图 1.
Schematic diagram of femoral tunnel positioning
股骨隧道定位示意图
a. I.D.E.A.L组 蓝线区域:“Anatomical” 黄线区域:“Direct insertion” 红线区域:“Isometric” 黑色虚线区域:“Low tension” 绿色圆圈:“I.D.E.A.L”定位点;b. TT组 红线区域:直接止点 蓝线区域:间接止点 绿色圆圈:“过顶点”定位点
a. I.D.E.A.L group Blue line area: “Anatomical” Yellow line area: “Direct insertion” Red line area: “Isometric” Dashed black line area: “Low tension” Green circle: “I.D.E.A.L.” positioning point; b. TT group Red line area: Direct insertion Blue line area: Indirect insertion Green circle: the “over the top” positioning point
④ 移植物填充:将移植物拉入骨隧道,股骨端采用可调式带袢钢板固定于股骨皮质外,胫骨端采用挤压螺旋钉固定。关节镜下观察其是否存在翻转、与骨隧道撞击、缝线断裂,探钩探查其紧张程度;反复屈伸膝关节以及行Lachman试验,确保移植物稳定性。最后冲洗关节腔,切口缝合、加压包扎。
1.3. 术后处理
两组术后处理方法一致。术后第2天切口换药,并行膝关节MRI检查观察胫骨、股骨隧道及移植物状态;常规消肿、止痛、抗感染以及预防下肢深静脉血栓形成处理。术后患膝佩戴可调节支具固定于伸直位,2周内行踝泵练习、直腿抬高以及主、被动屈伸膝关节练习达0°~60°;2~4周膝关节屈伸达0°~90°,行推髌活动,开始负重行走训练并逐步增至体质量的50%;5~12周负重行走逐步增至体质量100%;3个月后拆除支具,恢复正常膝关节活动。
1.4. 疗效评价指标
记录住院时间以及并发症发生情况,包括术后早期(<1个月;膝关节水肿、麻木、下肢深静脉血栓形成)及远期(>1个月;膝关节僵硬、活动后僵硬、骨关节炎)并发症。术前以及术后1周及1、3、6、12个月定期随访,采用Lysholm评分、IKDC评分及VAS评分评价膝关节功能及疼痛程度。术前及术后12个月,使用Ligs关节韧带数字体查仪(上海逸动医学科技有限公司)测量双膝关节120 N应力下胫骨相对于股骨向前位移差值(胫骨前移差值)。术后12个月MRI观察移植物愈合情况,测量信噪比(signal to noise quotien,SNQ)值以反映其成熟度。SNQ值测量时选取移植物股骨端、中段、胫骨端为关注区域,关注区域面积均为0.2 cm2,背景信号选取髌腱前2 cm背景噪声区域。SNQ值计算公式如下:SNQ值=移植物信号强度/背景信号强度−股四头肌腱信号强度/背景信号强度[9]。同时测量膝关节Blumensaat角,即ACL远端前缘与髁间窝顶部连线之间的夹角。计算胫骨前移差值以及Blumensaat角的手术前后差值(变化值)进行组间比较。
1.5. 统计学方法
采用SPSS27.0统计软件进行分析。计量资料采用Shapiro-Wilk检验进行正态性检验,均符合正态分布,数据以均数±标准差表示,组间比较采用独立样本t检验;两组Lysholm评分、IKDC评分及VAS评分多时间点比较采用重复测量方差分析,若不满足球形检验,采用Greenhouse-Geisser法进行校正,同一组别不同时间点间比较采用 Bonferroni 法,同一时间点不同组别间比较采用多因素方差分析。计数资料以率表示,组间比较采用四格表卡方检验。检验水准α=0.05。
2. 结果
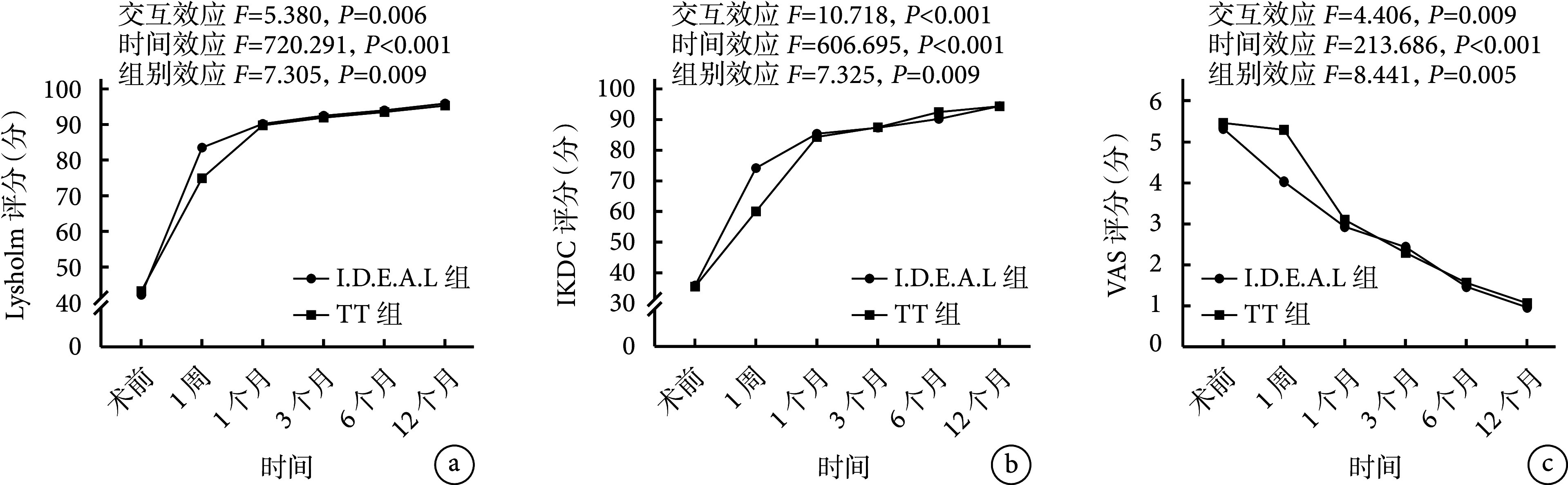
术后两组切口均Ⅰ期愈合,住院时间组间差异无统计学意义(P>0.05)。患者均获随访,随访时间12~18个月,平均14.9个月。术后两组膝关节Lysholm评分、IKDC评分均较术前增加,VAS评分降低。除TT组VAS评分术后1周与术前差异无统计学意义(P>0.05)外,其余各评分组内各时间点与术前差异均有统计学意义(P<0.05)。术后随时间延长,两组上述指标均呈进一步改善趋势,其中Lysholm评分及VAS评分各时间点间差异均有统计学意义(P<0.05);IKDC评分术后1个月与1周差异有统计学意义(P<0.05),其余时间点间差异均无统计学意义(P>0.05)。组间比较:术后1周I.D.E.A.L组膝关节Lysholm评分、IKDC评分高于TT组,VAS评分更低,差异均有统计学意义(P<0.05);其余时间点两组间各评分差异均无统计学意义(P>0.05)。见图2。术后12个月,两组胫骨前移差值均较术前减小,差异有统计学意义(P<0.05);I.D.E.A.L组胫骨前移差值变化值高于TT组,差异有统计学意义(P<0.05)。
图 2.
Change trends of the knee joint function and pain scores in the two groups
两组膝关节功能及疼痛评分变化趋势
a. Lysholm评分;b. IKDC评分;c. VAS评分
a. Lysholm score; b. IKDC score; c. VAS score
术后早期,I.D.E.A.L组发生水肿3例,TT组发生水肿3例、麻木4例、下肢深静脉血栓形成3例;术后远期,I.D.E.A.L组发生膝关节僵硬、骨关节炎各1例,TT组发生膝关节僵硬4例、活动后疼痛2例、骨关节炎5例。I.D.E.A.L组术后早、远期并发症发生率均低于TT组,差异有统计学意义(P<0.05)。见表2。
表 2.
Comparison of outcome indicators between the two groups (n=30)
两组结局指标比较(n=30)
| 结局指标 Outcome indicator |
I.D.E.A.L组 I.D.E.A.L. group |
TT组 TT group |
效应值(95%CI) Effect value (95%CI) |
P值 P value |
| 住院时间(x±s,d) | 5.50±0.76 | 5.65±0.85 | MD=–0.153(–0.569,0.262) | 0.463 |
| 胫骨前移差值变化值(x±s,mm) | 3.48±0.74 | 2.92±0.93 | MD=0.526(0.128,0.997) | 0.012 |
| Blumensaat角变化值(x±s,°) | 9.40±2.53 | 2.33±2.37 | MD=7.067(5.800,8.330) | <0.001 |
| 移植物SNQ值(x±s) | ||||
| 股骨端 | 15.84±4.57 | 13.30±4.36 | MD=2.532(0.223,4.840) | 0.032 |
| 中段 | 13.39±5.81 | 10.52±4.53 | MD=2.870(0.175,5.564) | 0.037 |
| 胫骨端 | 11.37±3.50 | 7.35±2.28 | MD=4.020(2.487,5.552) | <0.001 |
| 术后并发症 [例(%)] | ||||
| 早期 | 3(10.00) | 10(33.33) | OR=0.222(0.054,0.914) | 0.041 |
| 远期 | 2(6.67) | 11(36.67) | OR=0.123(0.025,0.621) | 0.044 |
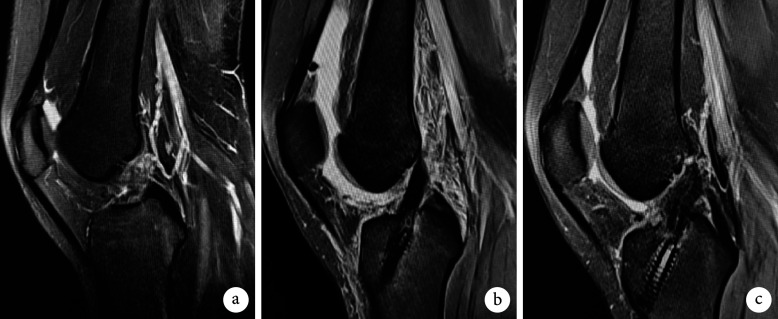
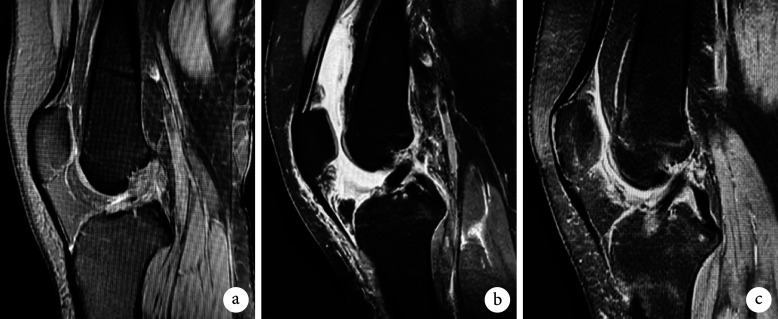
术后12个月MRI检查示两组膝关节移植物均生存良好,走行及张力无异常,未出现移植物断裂、从骨隧道滑脱等情况。两组Blumensaat角均较术前减小,差异有统计学意义(P<0.05),I.D.E.A.L组Blumensaat角变化值高于TT组,差异有统计学意义(P<0.05)。I.D.E.A.L组移植物股骨端、中段、胫骨端SNQ值均高于TT组,差异有统计学意义(P<0.05)。见表2及图3、4。
图 3.
A 20-year-old female patient in the TT group, MRI before and after ACL reconstruction of right knee
TT组患者,女,20岁,右膝关节ACL重建手术前后MRI
a. 术前;b. 术后1周;c. 术后12个月
a. Before operation; b. At 1 week after operation; c. At 12 months after operation
图 4.
A 25-year-old female patient in the I.D.E.A.L group, MRI before and after ACL reconstruction of right knee
I.D.E.A.L组患者,女,25岁,右膝关节ACL重建手术前后MRI
a. 术前;b. 术后1周;c. 术后12个月
a. Before operation; b. At 1 week after operation; c. At 12 months after operation
3. 讨论
TT技术是ACL等长重建经典术式,重建后的移植物纤维可以获得更好等长性[16-17]。其股骨隧道定位相对固定,在膝关节屈伸过程中由于采用“过顶点”定位方式[18-19],可最大限度减少胫骨、股骨对移植物的牵引,避免“雨刷效应”、“蹦极效应”导致的骨隧道扩大[20]。同时胫骨平台所受压力较小,不依赖韧带周围特有解剖标志,手术中股骨止点定位较为容易。但该技术弊端在于股骨定位由胫骨隧道决定,股骨侧定位点位置相对过高(朝向髁间切迹的顶部)及过深(Blumensaat线后),移植物过于垂直,难以维持正常膝关节控制前后位移和旋转位移的功能,限制了膝关节部分活动[21-24]。近年来,Pearle等[14]提出一种名为“I.D.E.A.L”(等距性、股骨直接止点、足印高深区、股骨隧道定位于解剖足印区、低张力)理论,即ACL重建股骨隧道最佳定位理论。该理论中的股骨隧道位置再现原ACL等距,在组织学上,其股骨隧道内口位于ACL纤维股骨直接止点组织结构;在解剖学上,其还原膝关节整个屈伸范围内原ACL的低张力屈曲模式。相对于TT技术,I.D.E.A.L技术更符合组织学、生物力学及解剖学特点。但在实际钻取股骨隧道过程中很难定位至I.D.E.A.L理论所要求的最佳定位内口位置,是由于该位置周围缺乏标志物,且内口较小。
本研究中,两组术后膝关节功能评分均较术前增加,术后1周I.D.E.A.L组评分均高于TT组,表明两种技术均能明显改善膝关节功能,但I.D.E.A.L技术术后早期膝关节功能恢复更好,分析原因可能是I.D.E.A.L技术重建的ACL相对于TT技术更符合原生ACL解剖学与生物力学,术后患者适应性好,膝关节周围肌肉力量可以达到更好训练要求,膝关节功能恢复更好。术后1周两组VAS评分均较术前降低,但TT组组内差异无统计学意义(P>0.05),且I.D.E.A.L组VAS评分明显低于TT组(P<0.05);结果显示术后早期TT组疼痛程度无明显缓解,I.D.E.A.L组疼痛程度低于TT组,分析原因可能是TT技术制备的股骨隧道内口定位更高,股骨隧道更垂直,所造成的骨质缺损更多,患者疼痛相对明显。
传统膝关节稳定性查体试验(如Lachman试验、前抽屉试验等)结果依赖于查体者经验,对于膝关节胫骨向前位移程度难以精准检测。为此,本研究采用Ligs关节韧带数字体查仪测量胫骨前移差值,使检测结果更精准[25-26]。研究结果显示术后12个月两组胫骨前移差值均较术前减小(P<0.05),I.D.E.A.L组胫骨前移差值变化值大于TT组(P<0.05),提示术后两组膝关节稳定性均较术前提升,I.D.E.A.L组膝关节稳定性高于TT组。
Blumensaat角是ACL重建术后膝关节稳定性的影响因素,与术后膝关节稳定性成负相关[27-28]。本研究中,术后12个月两组Blumensaat角均较术前减小(P<0.05),I.D.E.A.L组Blumensaat角变化值大于TT组(P<0.05),间接提示术后I.D.E.A.L组较TT组具有更好的膝关节稳定性,结合上述相关评价指标结果, 进一步明确采用I.D.E.A.L技术行ACL重建在膝关节稳定性恢复方面具有优势。分析原因,TT技术的股骨隧道定位方式通常形成较为垂直的股骨隧道,重建ACL也因此相对垂直,股骨侧足印区位于原生ACL之上[29]。而I.D.E.A.L技术重建ACL股骨侧足印区位于原生ACL之内,解剖学上优于TT技术,能更好地复刻原生ACL控制膝关节前后位移和旋转位移的功能。
目前,国际上通过影像学评估ACL重建术后移植物成熟度,常用方法是通过MRI计算移植物SNQ值,且二者成负相关[30-31],移植物的血管化、韧带化和强度与MRI信号相关[32]。恢复移植物结构完整性是安全恢复运动的基础[33],故基于移植物成熟度评估患者重返运动时重建ACL二次断裂风险具有一定意义。本研究中,术后12个月I.D.E.A.L组移植物股骨端、中段、胫骨端SNQ值大于TT组(P<0.05),提示成熟度低于TT组;分析原因,I.D.E.A.L组股骨隧道较TT组平直,移植物与股骨隧道内口应力较大,导致其“韧带化”过程相对缓慢。
此外,本研究还发现,术后早、远期I.D.E.A.L组并发症发生率均低于TT组(P<0.05),分析原因可能是I.D.E.A.L技术股骨端定位,早期在膝关节功能恢复、疼痛缓解方面效果更好,能更早达到康复锻炼的要求,从而减少了并发症的发生。
综上述,采用两种技术ACL重建均能取得较好疗效;但I.D.E.A.L技术重建术后早期疗效更好,膝关节稳定性更高,并发症发生率更低;而采用TT技术重建术后移植物成熟度更高,患者重返运动时ACL发生二次断裂风险更低。然而,本研究为回顾性研究,样本量较小,有待大样本前瞻性、多中心研究来进一步验证上述结论。
利益冲突 在课题研究和文章撰写过程中不存在利益冲突;经费支持没有影响文章观点和对研究数据客观结果的统计分析及其报道
伦理声明 研究方案经昆明医科大学第一附属医院伦理委员会批准[(2022)伦审L第224号]
作者贡献声明 王凡:文章撰写、研究设计与数据统计分析;李彦林、王国梁:研究指导、手术操作、文章内容审阅及修改;李骅、施青吕、李黎:患者随访,数据收集与研究实施
Funding Statement
云南省科技厅技术创新人才培养对象项目(202205AD160007)
Innovative Talents Training Object of Yunnan Science and Technology Department (202205AD160007)
References
- 1.Hassebrock JD, Gulbrandsen MT, Asprey WL, et al Knee ligament anatomy and biomechanics. Sports Med Arthrosc Rev. 2020;28(3):80–86. doi: 10.1097/JSA.0000000000000279. [DOI] [PubMed] [Google Scholar]
- 2.Beaulieu ML, Ashton-Miller JA, Wojtys EM Loading mechanisms of the anterior cruciate ligament. Sports Biomech. 2023;22(1):1–29. doi: 10.1080/14763141.2021.1916578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reijman M, Eggerding V, van Es E, et al Early surgical reconstruction versus rehabilitation with elective delayed reconstruction for patients with anterior cruciate ligament rupture: COMPARE randomised controlled trial. BMJ. 2021;372:n375. doi: 10.1136/bmj.n375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang LJ, Zeng N, Yan ZP, et al Post-traumatic osteoarthritis following ACL injury. Arthritis Res Ther. 2020;22(1):57. doi: 10.1186/s13075-020-02156-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Diermeier TA, Rothrauff BB, Engebretsen L, et al Treatment after ACL injury: Panther symposium ACL treatment consensus group. Br J Sports Med. 2021;55(1):14–22. doi: 10.1136/bjsports-2020-102200. [DOI] [PubMed] [Google Scholar]
- 6.Jin JX, Fang PZ, Hu ZW, et al Comparison of the effectiveness of autologous grafts for anterior cruciate ligament reconstruction: A protocol for an overview of systematic review and network meta-analysis. Medicine (Baltimore) 2020;99(43):e22832. doi: 10.1097/MD.0000000000022832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mayr R, Smekal V, Koidl C, et al ACL reconstruction with adjustable-length loop cortical button fixation results in less tibial tunnel widening compared with interference screw fixation. Knee Surg Sports Traumatol Arthrosc. 2020;28(4):1036–1044. doi: 10.1007/s00167-019-05642-9. [DOI] [PubMed] [Google Scholar]
- 8.Metso L, Nyrhinen KM, Bister V, et al Comparison of clinical results of anteromedial and transtibial femoral tunnel drilling in ACL reconstruction. BMC Musculoskelet Disord. 2020;21(1):341. doi: 10.1186/s12891-020-03351-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Matthewson G, Macdonald P Techniques for femoral socket creation in ACL reconstruction. Sports Med Arthrosc Rev. 2020;28(2):56–65. doi: 10.1097/JSA.0000000000000281. [DOI] [PubMed] [Google Scholar]
- 10.Bowman EN, Freeman TH, Limpisvasti O, et al Anterior cruciate ligament reconstruction femoral tunnel drilling preference among orthopaedic surgeons. Knee. 2021;29:564–570. doi: 10.1016/j.knee.2021.02.030. [DOI] [PubMed] [Google Scholar]
- 11.Cuzzolin M, Previtali D, Delcogliano M, et al. Independent versus transtibial drilling in anterior cruciate ligament reconstruction: a meta-analysis with meta-regression. Orthop J Sports Med, 2021, 9(7): 23259671211015616.
- 12.Loucas M, Loucas R, D’Ambrosi R, et al. Clinical and radiological outcomes of anteromedial portal versus transtibial technique in ACL reconstruction: a systematic review. Orthop J Sports Med, 2021, 9(7): 23259671211024591.
- 13.Saltzman BM, Wang S, Habet NA, et al The Hybrid transtibial technique for femoral tunnel drilling in anterior cruciate ligament reconstruction: a finite element analysis model of graft bending angles and peak graft stresses in comparison with transtibial and anteromedial portal techniques. J Am Acad Orthop Surg. 2022;30(18):e1195–e1206. doi: 10.5435/JAAOS-D-21-00883. [DOI] [PubMed] [Google Scholar]
- 14.Pearle AD, McAllister D, Howell SM Rationale for strategic graft placement in anterior cruciate ligament reconstruction: I.D.E.A.L. femoral tunnel position. Am J Orthop (Belle Mead NJ) 2015;44(6):253–258. [PubMed] [Google Scholar]
- 15.Li X, Lu J, Su J, et al High flexion femoral side remnant preservation positioning technique: a new method for positioning the femoral tunnel in anterior cruciate ligament reconstruction. J Orthop Surg Res. 2024;19(1):189. doi: 10.1186/s13018-024-04670-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.樊嵘, 何智超, 马传雨, 等 经胫骨入路与经辅助内侧入路制备股骨隧道类等长重建前交叉韧带的疗效比较. 中华创伤骨科杂志. 2022;24(03):267–271. doi: 10.3760/cma.j.cn115530-20210622-00295. [DOI] [Google Scholar]
- 17.Zhao J Anatomical single-bundle transtibial anterior cruciate ligament reconstruction. Arthrosc Tech. 2020;9(9):e1275–e1282. doi: 10.1016/j.eats.2020.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.赵青松, 李欢, 徐鹏, 等 单束前交叉韧带重建股骨侧定位点的选择进展. 生物骨科材料与临床研究. 2022;19(1):80–83, 88. [Google Scholar]
- 19.汤义民, 徐斌, 王高远, 等 前交叉韧带解剖单束重建中股骨止点的临床应用研究. 安徽医科大学学报. 2019;54(10):1642–1646. [Google Scholar]
- 20.郑维蓬, 刘治军, 魏合伟, 等 单束类等长重建前交叉韧带术后骨道位置及直径变化. 中国中医骨伤科杂志. 2021;29(9):40–45. [Google Scholar]
- 21.Fox MA, Zsidai B, Dadoo S, et al Anatomic anterior cruciate ligament reconstruction. Arthroscopy. 2023;39(9):1968–1970. doi: 10.1016/j.arthro.2023.03.004. [DOI] [PubMed] [Google Scholar]
- 22.Manderle BJ, Beletsky A, Gorodischer T, et al Transtibial anterior cruciate ligament reconstruction: tips for a successful anatomic reconstruction. Arthrosc Tech. 2021;10(12):e2783–e2788. doi: 10.1016/j.eats.2021.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schwartzberg R Editorial Commentary: Anteromedial portal drilling of the ACL femoral socket avoids transtibial constraint results in anatomic reconstruction and superior outcomes. Arthroscopy. 2023;39(6):1526–1528. doi: 10.1016/j.arthro.2022.12.023. [DOI] [PubMed] [Google Scholar]
- 24.Kilinc BE, Kara A, Oc Y, et al Transtibial vs anatomical single bundle technique for anterior cruciate ligament reconstruction: A retrospective cohort study. Int J Surg. 2016;29:62–69. doi: 10.1016/j.ijsu.2016.03.025. [DOI] [PubMed] [Google Scholar]
- 25.Wu D, Wang D, Han Y, et al A novel digital arthrometer to measure anterior tibial translation. J Orthop Surg Res. 2023;18(1):101. doi: 10.1186/s13018-022-03497-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.刘佳, 高娟, 李嫚, 等 Ligs关节韧带数字体查仪与KT-1000测量前交叉韧带损伤后膝关节前向不稳定的对比研究. 中国运动医学杂志. 2023;42(1):14–18. doi: 10.16038/j.1000-6710.2023.01.004. [DOI] [Google Scholar]
- 27.靳莉丹, 申瑞田 三维CT联合MRI分析膝关节ACL损伤重建术后移植物、周围结构与膝关节稳定性关系. 影像科学与光化学. 2022;40(2):418–423. doi: 10.7517/issn.1674-0475.210916. [DOI] [Google Scholar]
- 28.张壮岱, 金社辉, 冯志军, 等 解剖型前交叉韧带重建术前、术后MRI与正常膝关节MRI比较分析. 解放军医药杂志. 2016;28(8):39–43. doi: 10.3969/j.issn.2095-140X.2016.08.010. [DOI] [Google Scholar]
- 29.Feng H, Wang N, Xie D, et al Anteromedial portal technique, but not outside-in technique, is superior to standard transtibial technique in knee stability and functional recovery after anterior cruciate ligament reconstruction: a network meta-analysis. Arthroscopy. 2023;39(6):1515–1525. doi: 10.1016/j.arthro.2022.11.026. [DOI] [PubMed] [Google Scholar]
- 30.Zhang Y, Liu S, Chen Q, et al Maturity progression of the entire anterior cruciate ligament graft of insertion-preserved hamstring tendons by 5 years: a prospective randomized controlled study based on magnetic resonance imaging evaluation. Am J Sports Med. 2020;48(12):2970–2977. doi: 10.1177/0363546520951507. [DOI] [PubMed] [Google Scholar]
- 31.Ye Z, Xu J, Chen J, et al Effect of anterolateral structure augmentation on graft maturity after anterior cruciate ligament reconstruction: a clinical and MRI follow-up of 2 years. Am J Sports Med. 2022;50(7):1805–1814. doi: 10.1177/03635465221092768. [DOI] [PubMed] [Google Scholar]
- 32.Shimodaira H, Tensho K, Koyama S, et al Effect of a new remnant-preserving technique with anatomical double-bundle anterior cruciate ligament reconstruction on MRI-based graft maturity: a comparison cohort study. Knee Surg Sports Traumatol Arthrosc. 2023;31(6):2394–2405. doi: 10.1007/s00167-022-07180-3. [DOI] [PubMed] [Google Scholar]
- 33.Malahias MA, Capece FM, Ballarati C, et al Sufficient MRI graft structural integrity at 9 months after anterior cruciate ligament reconstruction with hamstring tendon autograft. Knee Surg Sports Traumatol Arthrosc. 2022;30(6):1893–1900. doi: 10.1007/s00167-021-06830-2. [DOI] [PubMed] [Google Scholar]