Abstract
The hemodynamic gain index (HGI), a novel non-invasive hemodynamic marker, represents a promising advancement in cardiovascular risk assessment. Cardiovascular disease and chronic kidney disease (CKD) are closely intertwined and share bidirectional relationships. We aimed to assess the association of HGI with CKD risk in a prospective study. Hemodynamic gain index was calculated using heart rate and systolic blood pressure (SBP) responses measured in 1765 men aged 42–61 years with normal kidney function during exercise testing using the formula: [(Heart ratemax x SBPmax)—(Heart raterest x SBPrest)]/(Heart raterest x SBPrest). Multivariable adjusted hazard ratios (HRs) (95% confidence intervals, CIs) were estimated for CKD. Over a median follow-up duration of 25.9 years, 175 CKD cases occurred. In analysis adjusted for established risk factors, a unit (bpm/mmHg) higher HGI was associated with a decreased risk of CKD (HR 0.78, 95% CI 0.65–0.95). Comparing extreme tertiles of HGI, the corresponding adjusted HR (95% CI) for CKD was 0.53 (0.33–0.85). Addition of HGI to a CKD risk prediction model containing established risk factors improved risk discrimination and reclassification (p-value for difference in -2 log likelihood = .011; net-reclassification-improvement = 59.37%, p = .018; integrated-discrimination-improvement = 0.0064, p = .008). Higher HGI is associated with a lower CKD risk and improves the prediction and classification of CKD beyond common established risk factors.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11357-024-01184-2.
Keywords: Hemodynamic gain index, Chronic kidney disease, Exercise testing, Cohort study
Introduction
Chronic kidney disease (CKD) poses a significant public health burden worldwide, affecting millions of individuals and being associated with substantial morbidity, mortality, and healthcare costs. Major risk factors for CKD encompass hypertension, diabetes, obesity, smoking, and atherosclerotic cardiovascular disease (CVD). Given that CKD is often preventable and manageable when detected early, the search for novel risk indicators becomes paramount. The plentiful health effects of physical activity extend to reducing the risk of CKD as well as delaying its progression [1]. Cardiopulmonary exercise testing (CPX) has emerged as a valuable tool for assessing cardiorespiratory fitness (CRF), a modifiable risk factor that is principally determined through increased aerobic physical activity[2] and shown to be a robust predictor of CVD and overall health [3]. Moreover, emerging evidence indicates a significant relationship between CRF and CKD risk [4]. During CPX, heart rate and blood pressure responses in addition to CRF are core parameters routinely measured. The hemodynamic responses during exercise hold promise as potential markers of cardiovascular health and are gaining attention as valuable prognostic indicators. One such novel hemodynamic marker is the hemodynamic gain index (HGI), which is derived from the combination of exercise heart rate and systolic blood pressure (SBP) responses during CPX [5]. HGI has demonstrated its ability to predict adverse cardiovascular outcomes [6–8], representing a promising advancement in cardiovascular risk assessment. Despite the well-established link between CVD and CKD [9], the association between HGI and CKD risk has yet to be evaluated. Therefore, the primary aim of the current study is to investigate the potential association between HGI and the risk of CKD. We also assessed the extent to which HGI measurements could improve the prediction of CKD using measures of risk discrimination and reclassification.
Materials and methods
The Kuopio Ischemic Heart Disease (KIHD) population-based prospective cohort study which comprises a representative sample of 2682 men, aged 42–61 yr, drawn from eastern Finland[4] was used for the analysis. Baseline assessments and physical examinations occurred between March 1984 and December 1989. Ethical approval for the study protocol was obtained from the Research Ethics Committee of the University of Eastern Finland, and all participants provided written informed consent. To estimate CRF, peak oxygen uptake was directly assessed using a respiratory gas analyzer (Medical Graphics) during a maximal symptom-limited exercise-tolerance test performed on an electrically braked cycle ergometer [4]. Additionally, electrocardiographic indices, blood pressure (BP), and heart rate were measured both at rest and during the exercise testing phase [7, 8]. The HGI was derived using the following formula: ([Heart ratemax x SBPmax]—[Heart raterest x SBPrest])/(Heart raterest x SBPrest) [5], obtained from the heart rate and SBP responses during the exercise tests. Chronic kidney disease was defined based on the National Kidney Foundation Kidney Disease Outcomes Quality Initiative (KDOQI) guideline, encompassing kidney damage (e.g., albuminuria) or an estimated glomerular filtration rate (eGFR) lower than 60 mL/min per 1.73 m2 (or both) for a duration of 3 months or longer [10]. Incident CKD cases that occurred from the commencement of the study until 2014 were included in the analysis. To estimate the hazard ratios (HRs) with 95% CI for CKD, multivariable Cox proportional hazards models were employed. To investigate whether adding information on HGI to established risk factors for CKD is associated with improvement in the prediction of CKD risk, we calculated measures of discrimination (e.g., Harrell’s C-index[11] and difference in -2 log likelihood) and reclassification (net-reclassification-improvement (NRI) and integrated-discrimination-improvement (IDI)) [12, 13]. All statistical analyses were performed using Stata version MP 18 (Stata Corp).
Results
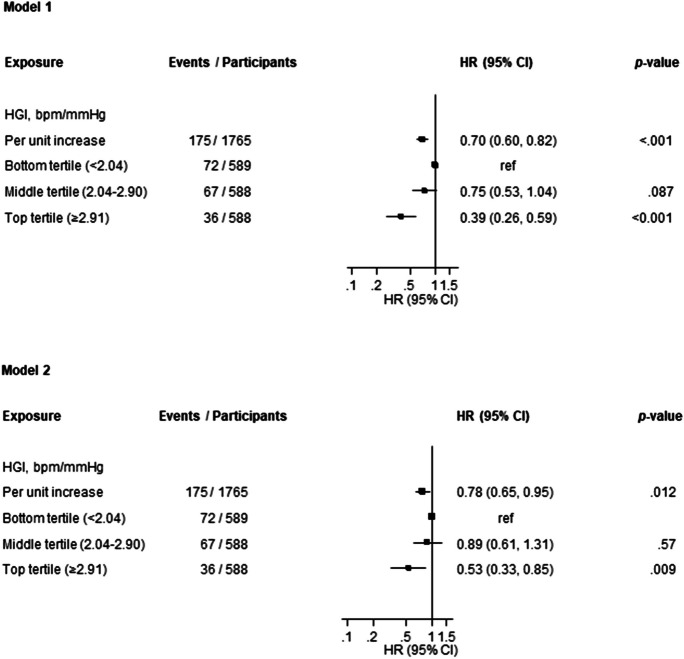
Among the participants included in the analysis, a total of 1765 men provided complete information on HGI, potential confounding variables, and CKD events (Electronic Supplementary Material 1). At baseline, their mean ± SD age was 53 ± 5 yr, while the mean ± SD HGI was 2.53 ± 1.05 bpm/mmHg (Table 1). Over a median (IQR) follow-up duration of 25.9 (18.0, 28.0) yr, a total of 175 CKD cases were observed. In the age-adjusted analysis, each 1 unit increase in HGI was associated with a significantly lower risk of CKD (HR 0.70, 95% CI 0.60–0.82) (Fig. 1-Model 1), which was attenuated to (HR 0.78, 95% CI 0.65–0.95) on further adjustment for body mass index, total cholesterol, smoking, prevalent type 2 diabetes, hypertension and coronary heart disease, alcohol consumption, socioeconomic status, eGFR and physical activity (Fig. 1-Model 2). Alternatively, comparing individuals in the top tertile of HGI to those in the bottom tertile, the corresponding adjusted HRs (95% CIs) for CKD were 0.39 (0.26–0.59) and 0.53 (0.33–0.85), respectively. A CKD risk prediction model containing traditional risk factors yielded a C-index of 0.6500 (95% CI: 0.6022 to 0.6978). After addition of information on HGI, the C-index was 0.6615 (95% CI: 0.6143 to 0.7088), representing a modest increase of 0.0115 (95% CI: -0.0042 to 0.0273; p = 0.15). The -2 log likelihood was significantly improved on addition of HGI to the risk model (p for comparison = 0.011). The continuous NRI and IDI were 59.37% (95% CI: 10.29 to 108.45; p = 0.018) and 0.0064 (0.0016 to 0.0111; p = 0.008), respectively.
Table 1.
Baseline characteristics of study participants overall and by chronic kidney disease
| Characteristics | Overall (n = 1765) Mean ± SD or median (IQR) |
With CKD (n = 175) Mean ± SD or median (IQR) |
Without CKD (n = 1590) Mean ± SD or median (IQR) |
|---|---|---|---|
| Hemodynamic gain index, bpm/mmHg | 2.53 ± 1.05 | 2.29 ± 0.94 | 2.56 ± 1.06 |
| Resting heart rate on bicycle, bpm | 62 ± 11 | 62 ± 11 | 62 ± 11 |
| Peak heart rate on bicycle, bpm | 155 ± 25 | 148 ± 28 | 156 ± 24 |
| Resting SBP on bicycle, mmHg | 150 ± 22 | 154 ± 24 | 150 ± 22 |
| Peak SBP on bicycle, mmHg | 204 ± 27 | 205 ± 30 | 204 ± 27 |
| Age, yr | 53 ± 5 | 54 ± 5 | 53 ± 5 |
| Socioeconomic status | 8.4 ± 4.3 | 9.4 ± 4.3 | 8.3 ± 4.2 |
| Body mass index, kg/m2 | 26.9 ± 3.4 | 27.8 ± 3.8 | 26.8 ± 3.4 |
| Alcohol consumption, g/week | 32.9 (6.4, 95.6) | 32.0 (6.3, 96.0) | 33.0 (6.4, 95.6) |
| Physical activity, KJ/day | 1163 (620, 1914) | 1215 (565, 1826) | 1162 (622, 1938) |
| Current smoking | 568 (32.2%) | 49 (28.0) | 519 (32.6%) |
| History of type 2 diabetes | 63 (3.6%) | 8 (4.6%) | 55 (3.5%) |
| History of hypertension | 526 (29.8%) | 60 (34.3%) | 466 (29.3%) |
| History of coronary heart disease | 415 (23.5%) | 54 (30.9%) | 361 (22.7%) |
| Total cholesterol, mmol/l | 5.93 ± 1.09 | 6.04 ± 1.15 | 5.92 ± 1.09 |
| Estimated GFR, ml/min/1.73 m2 | 88.2 ± 17.0 | 87.1 ± 15.7 | 88.3 ± 17.2 |
BMI, body mass index; CKD, chronic kidney disease; GFR, glomerular filtration rate; IQR, interquartile range; SD, standard deviation; SBP, systolic blood pressure
Socioeconomic status was generated as a summary index that combined factors such as income, education, occupational prestige, material standard of living and housing conditions. The composite index ranged from 0 to 25, with higher values indicating lower socioeconomic status
Fig. 1.
Association of hemodynamic gain index with chronic kidney disease
Discussion
Higher HGI demonstrated a strong association with a lower risk of CKD, even after accounting for several well-established risk factors. Furthermore, addition of information on HGI to a model containing traditional risk factors for CKD was associated with significant improvements in the discrimination and reclassification of long-term CKD. The significance of the association of HGI with CKD risk lies in the fact that hemodynamic responses to exercise, such as heart rate and blood pressure, have been recognized as independent predictors of vascular disease and essential determinants of prognosis [14]. The index reflects the compliance of the vasculature and the cardiovascular system's ability to generate sufficient blood flow to meet physiological demands during maximal aerobic exercise [5]. Higher HGI levels during exercise have been associated with better cardiac function and predict adverse cardiovascular outcomes [6–8]. Since CVD and CKD are closely intertwined and share complex and bidirectional relationships, a more robust cardiovascular system, represented by higher HGI, may confer protection against CKD development. The implications of these findings are significant in the context of CKD prevention and management. The identification of HGI as a strong and independent risk indicator and predictor of CKD provides a promising easily accessible and valuable tool for long-term risk stratification. Early identification of individuals at increased CKD risk using HGI could facilitate targeted interventions, potentially reducing the burden of CKD and its associated complications. Further research and validation studies are warranted to establish HGI's clinical value in risk stratification and its potential implications for CKD prevention.
The strengths of this study include its robust cohort design, a relatively large sample size, long-term follow-up with zero loss to follow-up, comprehensive adjustment for multiple confounding factors and assessment of risk prediction using established methods and measures. However, certain limitations should be acknowledged. Firstly, the study population consisted of middle-aged and older Finnish men, limiting the generalizability of the findings to women and other populations. Furthermore, the observational design poses potential concerns regarding reverse causation and regression dilution, necessitating cautious interpretation of the results.
Conclusion
The current study contributes valuable insights into the relationship between HGI and CKD risk. HGI is a strong risk indicator and predictor of CKD and represents a simple and non-invasive marker for assessing CKD risk.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We thank the staff of the Kuopio Research Institute of Exercise Medicine and the Research Institute of Public Health and University of Eastern Finland, Kuopio, Finland for the data collection in the study.
Authors’ contributions
Study design SKK and JAL. Study conduct: SKK and JAL. Data collection: SKK and JAL. Data analyses: SKK. Data interpretation: SKK and JAL. Drafting manuscript: SKK. Revising manuscript content: SKK and JAL. Approving final version of manuscript. SKK and JAL. SKK takes responsibility for the integrity of the data analysis.
Funding
JAL acknowledges support from The Finnish Foundation for Cardiovascular Research, Helsinki, Finland. SKK is funded by the National Institute for Health and Care Research (NIHR) Applied Research Collaboration East Midlands (ARC EM) and Leicester NIHR Biomedical Research Centre (BRC). The views expressed are those of the author and not necessarily those of the NIHR or the Department of Health and Social Care.
Data availability
Restrictions apply to the availability of the outcome data due to recent Finnish legislation concerning the use of national social and health registers in research.
Declarations
The KIHD study was conducted in accordance with the ethical standards set forth in the Helsinki Declaration (1983). Participants in the study were included after obtaining their written and informed consent for the study. The institutional review board of the University of Kuopio and Kuopio University Hospital, Kuopio, Finland (License number 143/97) approved the study protocol.
Conflict of interest
The authors declare that they have no conflicts of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wilund KR, Thompson S, Viana JL, Wang AY. Physical Activity and Health in Chronic Kidney Disease. Contrib Nephrol. 2021;199:43–55. 10.1159/000517696 [DOI] [PubMed] [Google Scholar]
- 2.Ross R, Blair SN, Arena R, Church TS, Despres JP, Franklin BA, et al. Importance of Assessing Cardiorespiratory Fitness in Clinical Practice: A Case for Fitness as a Clinical Vital Sign: A Scientific Statement From the American Heart Association. Circulation. 2016;134(24):e653–99. 10.1161/CIR.0000000000000461 [DOI] [PubMed] [Google Scholar]
- 3.Kunutsor SK, Jae SY, Kurl S, Laukkanen JA. The interplay between systolic blood pressure, cardiorespiratory fitness, and mortality risk: a prospective cohort study. J Cardiopulm Rehabil Prev. 2023;43(3):222–24. [DOI] [PubMed]
- 4.Kunutsor SK, Isiozor NM, Myers J, Seidu S, Khunti K, Laukkanen JA. Baseline and usual cardiorespiratory fitness and the risk of chronic kidney disease: a prospective study and meta-analysis of published observational cohort studies. Geroscience. 2023;45(3):1761–74. [DOI] [PMC free article] [PubMed]
- 5.Vainshelboim B, Kokkinos P, Myers J. Prognostic Value and Clinical Usefulness of the Hemodynamic Gain Index in Men. Am J Cardiol. 2019;124(4):644–9. 10.1016/j.amjcard.2019.05.015 [DOI] [PubMed] [Google Scholar]
- 6.Vainshelboim B, Kokkinos P, Myers J. Hemodynamic gain index in women: A validation study. Int J Cardiol. 2020;1(308):15–9. 10.1016/j.ijcard.2020.03.066 [DOI] [PubMed] [Google Scholar]
- 7.Laukkanen JA, Isiozor NM, Willeit P, Kunutsor SK. Hemodynamic gain index is associated with cardiovascular mortality and improves risk prediction: A PROSPECTIVE COHORT STUDY. J Cardiopulm Rehabil Prev. 2023;43(5):368–76. [DOI] [PMC free article] [PubMed]
- 8.Laukkanen JA, Isiozor NM, Willeit P, Kunutsor SK. Haemodynamic Gain Index Is Associated with Risk of Sudden Cardiac Death and Improves Risk Prediction: A Cohort Study. Cardiology. 2023;148(3):246–56. 10.1159/000530637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Couser WG, Remuzzi G, Mendis S, Tonelli M. The contribution of chronic kidney disease to the global burden of major noncommunicable diseases. Kidney Int. 2011;80(12):1258–70. 10.1038/ki.2011.368 [DOI] [PubMed] [Google Scholar]
- 10.National KF. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39(2 Suppl 1):S1-266. [PubMed] [Google Scholar]
- 11.Harrell FE Jr, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15(4):361–87. [DOI] [PubMed] [Google Scholar]
- 12.Pencina MJ, D’Agostino RB Sr, D’Agostino RB Jr, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008;27(2):157–72. 10.1002/sim.2929 [DOI] [PubMed] [Google Scholar]
- 13.Pencina MJ, D'Agostino RB Sr, Steyerberg EW. Extensions of net reclassification improvement calculations to measure usefulness of new biomarkers. Statistics in Medicine. [Research Support, American Recovery and Reinvestment Act Research Support, N.I.H., Extramural]. 2011;30(1):11–21. [DOI] [PMC free article] [PubMed]
- 14.Guazzi M, Arena R, Halle M, Piepoli MF, Myers J, Lavie CJ. 2016 Focused Update: Clinical Recommendations for Cardiopulmonary Exercise Testing Data Assessment in Specific Patient Populations. Circulation. 2016;133(24):e694-711. 10.1161/CIR.0000000000000406 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Restrictions apply to the availability of the outcome data due to recent Finnish legislation concerning the use of national social and health registers in research.