Highlights
-
•
Using nationwide Danish health register data, associations between fluoroquinolone use and elevated hazard rates of Achilles tendon rupture were found.
-
•
Associations were most pronounced with increasing dosage and within 30 days following fluoroquinolone use.
-
•
Despite recent findings calling the previously suggested associations between fluoroquinolones and aortic and valvular diseases into question, advised caution in relation to tendinopathies still seems relevant.
Fluoroquinolones (FQs) are a class of antibiotics used to treat bacterial infections, such as lower respiratory, gastrointestinal, and urinary tract infections. Due to its broad-spectrum action and wide availability, it is a commonly prescribed group of antibiotics worldwide.1
However, FQs have been described as exerting collagen degrading effects, which has led to warnings pertaining to increased risks of tendinitis, Achilles tendon rupture, as well as potentially life-threatening aortic and valvular diseases.2, 3, 4, 5, 6 Even so, the data on which these warnings are based have limitations, and several recent notable publications using high quality data did not find the described associations with aortic or valvular disease.7, 8, 9 As such, these recent investigations could call into question the clinical relevance of the described collagen-degrading FQ effects altogether. Hence, using Danish nationwide registers and clinical databases, we sought to revisit and investigate the potential relationship between FQ exposure and Achilles tendon lesions.
We conducted a nationwide nested case-control study including subjects aged 30–100 years during 2003–2021. Cases were defined as incident Achilles tendon lesion/rupture as indicated by hospital diagnostic codes (International Classification of Diseases, 10th edition, code S860). For all analyses, cases were matched according to sex, age, and year of index in a 1:30 ratio to controls. The exposure of interest was claimed prescriptions for oral formulations of FQ (ciprofloxacin or moxifloxacin) within given exposure windows. We considered 60-day, 90-day, and 1-year exposure windows to scrutinize short-, intermediate-, and long-term associations between FQ exposure and Achilles tendon rupture. We used an active comparator design, comparing subjects exposed to FQ only with subjects exposed to amoxicillin. A potentially harmful effect of FQ could be exacerbated with increasing FQ exposure; as such, we also calculated cumulative defined daily doses (cDDDs) of FQ to compare higher cumulative doses with lower doses. Any association between FQ exposure and Achilles tendon rupture was evaluated using multivariable Cox proportional hazards regression models adjusted for relevant confounders. From these models, conditional logistic regression software was used to obtain hazard ratios (HR) with 95% confidence intervals (95%CIs). Further details pertaining to the statistical methodology and data used have been provided previously.7
A total of 28,806 cases were identified with 864,090 sampled controls. The median age was 38 (interquartile range:= 30–50 years), and the majority were males (76%). In general, comorbidity and concomitant medical treatment were very well balanced between cases and controls. Of note, the prevalence of both trigger finger and Dupuytren's contracture were low among both cases and controls (<1%) and cases were more frequently treated with oral glucocorticoids than controls (6% vs. 2%).
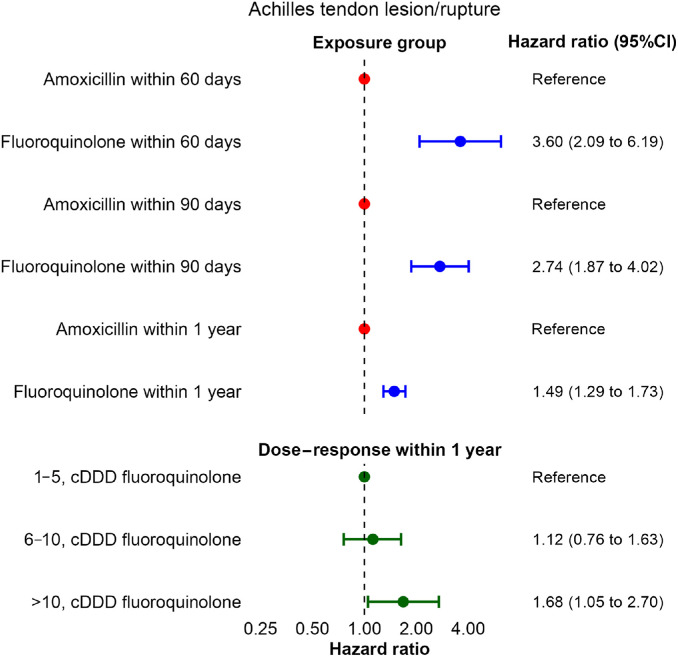
Overall, we saw a clear signal of increased rates of Achilles tendon lesions in individuals exposed to FQ as compared to amoxicillin, with the effects being attenuated by broader exposure window (60-day: HR = 3.60 (95%CI: 2.09–6.19); 90-day HR = 2.74 (95%CI: 1.87–4.02), 1-year HR = 1.49 (95%CI: 1.29–1.73)) (Fig. 1).
Fig. 1.
The Forest plot depicts the association between fluoroquinolone use and Achilles tendon rupture with amoxicillin as reference. The bottom panel depicts the cDDD of fluoroquinolones and the rates of Achilles tendon rupture. The x axis depicts the hazard ratios with 95%CI, and the y axis depicts exposure groups of claimed fluoroquinolone prescriptions. 95%CI = 95% confidence intervals; cDDD = cumulative defined daily doses.
Moreover, examining cumulative exposure to FQ (cDDD), increasing cDDD was associated with increased rates of Achilles-tendon rupture in a dose–response manner (cDDD: 1–5 as reference; cDDD: 6–10, HR = 1.12 (95%CI = 0.76–1.63); cDDD >10, HR–1.68 (95%CI: 1.05–2.70)) (Fig. 1).
Hence, the high-quality epidemiological data presented in this letter underline the finding that FQ seems to exert acute effects on tendons, leading to high rates of tendinitis and Achilles tendon injuries. The association was exacerbated by a short exposure window, indicating a clear signal toward acute effects. Moreover, the described dose-response relationship between cumulative doses of FQ and the rates of tendon injuries support an overall credible association. This is in line with previous findings in the literature and constitutes an important message as a series of recent investigations have questioned the pathogenicity and clinical relevance of the described collagen-degrading effects of FQ in relation to aortopathies and valvular disease.7, 8, 9 Thus, the overall clinical relevance of the described collagen degradation could be dubious with regard to tendinopathies as well.
FQs have been shown to up-regulate matrix metalloproteinases, which in turn leads to degeneration of collagen fibrils (especially type I collagen) believed to be the mechanism behind the increased rates of tendon lesions as well as the cardiovascular adverse events previously associated with FQ use.10 The contrast between the clear and robust association with tendinopathies and the lack of association with aortic and valvular diseases could be perceived as puzzling because the proposed mechanism is the same. Further research in both clinical and laboratory settings is needed to elucidate this conundrum.
Our data are based on patients in the Danish health care system, in which ciprofloxacin and moxifloxacin are available in oral formulations. To what degree our results can be extrapolated to other generations of FQs is unknown. Moreover, we did not have clinical or imaging data regarding lesion sites of the Achilles tendon.
Although concerns regarding FQs and cardiovascular disease, which have led to warnings issued by regulatory bodies, have been deemed questionable, our data clearly indicate that physicians using FQs should be aware of the increased risk for Achilles tendon injuries related to treatment. As such, other treatment options are preferred in patients considered to be at high risk (e.g., patients with previous or prevalent tendinopathies).
Author contributions
AH and JES conducted the initial analyses and accessed and verified the data. PVR drafted the manuscript. All authors conceived the idea, revised the manuscript for important intellectual content. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication. All authors have read and approved the final version of the manuscript, and agree with the order of presentation of the authors.
Competing Interest
The authors declare that they have no competing interests.
Footnotes
Peer review under responsibility of Shanghai University of Sport.
References
- 1.Hicks LA, Bartoces MG, Roberts RM, et al. US outpatient antibiotic prescribing variation according to geography, patient population, and provider specialty in 2011. Clin Infect Dis Off Publ Infect Dis Soc Am. 2015;60:1308–1316. doi: 10.1093/cid/civ076. [DOI] [PubMed] [Google Scholar]
- 2.Daneman N, Lu H, Redelmeier DA. Fluoroquinolones and collagen associated severe adverse events: A longitudinal cohort study. BMJ Open. 2015;5 doi: 10.1136/bmjopen-2015-010077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Etminan M, Sodhi M, Ganjizadeh-Zavareh S, Carleton B, Kezouh A, Brophy JM. Oral fluoroquinolones and risk of mitral and aortic regurgitation. J Am Coll Cardiol. 2019;74:1444–1450. doi: 10.1016/j.jacc.2019.07.035. [DOI] [PubMed] [Google Scholar]
- 4.van der Linden PD, Sturkenboom MCJM, Herings RMC, Leufkens HMG, Rowlands S, Stricker BHCh. Increased risk of Achilles tendon rupture with quinolone antibacterial use, especially in elderly patients taking oral corticosteroids. Arch Intern Med. 2003;163:1801–1807. doi: 10.1001/archinte.163.15.1801. [DOI] [PubMed] [Google Scholar]
- 5.Khaliq Y, Zhanel GG. Fluoroquinolone-associated tendinopathy: A critical review of the literature. Clin Infect Dis. 2003;36:1404–1410. doi: 10.1086/375078. [DOI] [PubMed] [Google Scholar]
- 6.Alves C, Mendes D, Marques FB. Fluoroquinolones and the risk of tendon injury: A systematic review and meta-analysis. Eur J Clin Pharmacol. 2019;75:1431–1443. doi: 10.1007/s00228-019-02713-1. [DOI] [PubMed] [Google Scholar]
- 7.Strange JE, Holt A, Blanche P, et al. Oral fluoroquinolones and risk of aortic or mitral regurgitation: A nationwide nested case-control study. Eur Heart J. 2021;42:2899–2908. doi: 10.1093/eurheartj/ehab374. [DOI] [PubMed] [Google Scholar]
- 8.Huh K, Kang M, Jung J. Lack of association between fluoroquinolone and aortic aneurysm or dissection. Eur Heart J. 2023;44:4476–4484. doi: 10.1093/eurheartj/ehad627. [DOI] [PubMed] [Google Scholar]
- 9.Brown JP, Wing K, Leyrat C, et al. Association between fluoroquinolone use and hospitalization with aortic aneurysm or aortic dissection. JAMA Cardiol. 2023;8:865–870. doi: 10.1001/jamacardio.2023.2418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tsai W-C, Hsu C-C, Chen CPC, et al. Ciprofloxacin up-regulates tendon cells to express matrix metalloproteinase-2 with degradation of type I collagen. J Orthop Res Off Publ Orthop Res Soc. 2011;29:67–73. doi: 10.1002/jor.21196. [DOI] [PubMed] [Google Scholar]