1. Background
The importance of physical activity (PA) for health is unequivocal.1 Accordingly, population-based recommendations for exercise, and more recently public health guidelines for PA, have been developed and released by authoritative groups for many decades.2 Such guidelines emerged with leadership from the exercise physiology discipline and were rooted in, and loyal to, the importance of moderate-to-vigorous intensity PA (MVPA) or exercise.1, 2, 3 Until quite recently, PA guidelines around the world focused only on MVPA; and for young to older adults, only MVPA accumulated in bouts of 10 min or more.2,3 While the importance and potency of MVPA for health across all ages is without debate, the singular focus on MVPA with relative disregard for lower intensities of PA may have been unnecessarily exclusionary (or even myopic),4 especially given the relatively arbitrary nature of the thresholds5 delineating each intensity category (e.g., for adults light PA <3.0 metabolic equivalent of task (MET), moderate PA 3.0–<6.0 METs, vigorous PA ≥6.0 METs) and the small portion of the day occupied by MVPA.
Over the past 10–15 years, there has been increased attention on being sedentary as a distinct behavior, clearly distinguishing it from physical inactivity.6,7 This attention led to the development of sedentary-specific public health guidelines for children of all ages in Canada,8,9 and deliberate mention and recognition in guidelines from the United States Department of Health and Human Services10 and the World Health Organization (WHO).11
In 2016, Canada released the world's first “24-hour Movement Guidelines” that integrated all movement behaviors throughout the day—physical activities, sedentary behaviors, and sleep—recognizing that the whole day matters, and that these behaviors interact to affect health, are codependent, and mutually exclusive.12, 13, 14 In Canada, 24-hour movement guidelines now exist for all ages,12,15,16 were adopted by the WHO for children under 5 years,17 and have been adopted or developed in many countries around the world.13 In a very short period of time, traditional MVPA/exercise-centric guidelines have evolved to be more holistic and inclusive of codependent behaviors (i.e., one behavior cannot change without changing the other behaviors)—a new conceptual paradigm for movement behaviors. Research examining the prevalence of populations meeting new 24-hour guidelines and relationships with health indicators and outcomes has proliferated rapidly18,19 and new compositional data analytical procedures20,21 have been used to explore the optimal distributions of 24-hour movement behaviors for health.18,22
With this brief background setting the stage, in this opinion piece we aimed to briefly discuss (i) if the evolution to 24-hour guidelines is justified, (ii) whether integrated 24-hour guidelines stratified only into broad age ranges provide the best movement behavior prescriptions possible, and (iii) whether new computing and analytical capabilities could revolutionize movement behavior guidelines by creating more individualized guidelines.
2. Are 24-hour guidelines justified?
Guidelines related to movement behaviors have evolved rather rapidly over the past 25 years. Whether the “evolution” to 24-hour movement guidelines is considered progress or conversely represents a “devolution” and regression of guidance is debated.4,14,23 Criticisms of the integrated approach include a lack of sufficient evidence to support specific recommendations for sedentary behaviors, light PA, or behavior substitutions;1,11,14,23 the inclusion of screen time as a sub-component of sedentary behavior recommendations;24 and including sleep as a “movement” behavior, among others. Notably, in their most recent guidelines, the United States10 and the WHO (for all ages ≥5 years)11 chose not to employ a 24-hour movement approach. However, there are several lines of thought supporting the use of 24-hour movement guidelines, including:
-
•
an abundance of evidence regarding the relationships between individual movement behaviors (physical activities of all intensities, sedentary behaviors (especially sedentary recreational screen time), and sleep), and a variety of health indicators and outcomes;1,4,6,8, 9, 10, 11, 12,15, 16, 17, 18
-
•
substantive and growing evidence that the combination/composition of movement behaviors making up a 24-hour day are significantly related to a variety of health indicators and outcomes;18,20, 21, 22,25
-
•
dose–response gradient evidence across studies and health indicators showing that meeting more movement behavior recommendations is associated with more favorable health indicators (e.g., increased health benefits of meeting 3>2>1>0 behavioral targets);22,26,27
-
•
increases in intervention possibilities, flexibility, and options when counseling clients or patients;12,15,16,28
-
•
international support, given several countries have produced 24-hour movement guidelines;13,17
-
•
negligible risk associated with making strong recommendations; even if based on low-quality evidence, the benefits of improving each movement behavior far outweigh the risks;12,14, 15, 16, 17
-
•
formative and qualitative research showing that end-users want and appreciate the integration of movement behaviors;29
-
•
alignment of the “energy out” (e.g., movement behaviors) with the “energy in” (diet) approach of the energy balance equation (nutrition guidelines throughout the world consider all food types/groups together, recognizing different combinations can be used to achieve a healthy diet).
While the debate regarding segregating or integrating movement behaviors is and should be ongoing, further research is encouraged to help guide the optimal approach for population health.
3. Does “one size fit all”?
Developing public health guidelines for movement behaviors is difficult. It involves many stages to arrive at evidence-informed public-facing recommendations.30 Traditionally these guidelines have been stratified only into broad age groupings for early years (0–4 years),15,17 children (5–11 years),10, 11, 12 youth (12–17 years),10, 11, 12 adults (18–64 years),10,11,16 and older adults (≥65 years).10,11,16 Current guidelines throughout the world take this “one size fits all” approach because such recommendations include evidence from multiple heterogeneous studies with different populations, interventions/exposures, comparators, and health outcomes/indicators.1, 2, 3,8, 9, 10, 11, 12,15, 16, 17 While the evidence is generally of low quality,10, 11, 12,15, 16, 17 it is consistent and when taken together the evidence broadly suggests that recommended movement behavior thresholds promoting health are relevant to apparently healthy populations irrespective of sex, gender, race, ethnicity, or socioeconomic status (SES) of the family.12,15, 16, 17 This approach is pragmatic, providing a universal guideline for all within a broad age group. This also makes it feasible and relatively easy for public health interpretation, messaging, and counseling.
Nevertheless, common sense and research evidence expose inherent limitations to such an approach. First, as a person transitions from one broad age category to the next, suddenly the required cocktail of movement behaviors changes.12,15,16 This convenient categorization approach results in an artifactual stepwise change in surveillance figures of population prevalence meeting guidelines and suggests, for example, that on your 18th birthday the amount of MVPA required for health drops immediately from 420 min per week to 150 min per week!10, 11, 12,16 Second, it stands to reason that a 6-year-old girl of European descent living in a wealthy household in an urban center with 4 siblings may have different optimal movement requirements and circumstances than a 17-year-old male of South Asian heritage living in a rural area with a single parent, no siblings, and on government income support. Socioecological factors such as perceived safety, pollution, and financial strain may modify the associated benefits of time spent in sleep, PA, or sedentary behaviors for these individuals in addition to posing as barriers to accomplishing the “one size fits all” prescription. Third, a “one size fits all” approach results in the crude dichotomization of large age-group population segments into those meeting or not meeting the universal guidelines, thus limiting specific guidance for interventions. More individualized movement behavior recommendations could deliver nuanced guidance better suited to personal and population health promotion and disease prevention, and personal circumstances, while preventing convenient age group-based guidance and prevalence transition artifacts.
We know that the optimal threshold of healthy movement behaviors, whether it be light PA, MVPA, sedentary behaviors, sleep, or their ideal combination(s), varies by age, sex, gender, race, ethnicity, maturation status, underlying health conditions, ability/disability, SES, genetics, and living location; and there are significant interactions and intersections among these characteristics.1,3,8, 9, 10, 11, 12,15, 16, 17, 18,22,25,31, 32, 33 This knowledge was not deliberately ignored by guideline developers in the past, but the amount of such information has been limited (though rapidly expanding), and the possibility of practitioners synthesizing evidence on an individualized basis has been absent from our collective imaginations. Until recently the analytical, computing, and artificial intelligence capacity to take a “precision medicine” and/or “precision health” approach has been unavailable, but this is rapidly changing. The growing ease of access for advanced information technology, automated literature search techniques, plentiful and powerful computational capacity, machine learning, and artificial intelligence now allow for the possibility of a more nuanced approach—precision 24-hour movement behavior recommendations. With multiple lines of evidence, including compositional data analyses, time reallocation studies, and isotemporal substitution investigations supporting an individualized, integrated approach, should we embrace these new opportunities?
4. What might precision 24-Hour Movement Guidelines look like?
Moving to an individualized approach for movement behavior guidelines will require significant adaptation by health practitioners, educators, epidemiologists, policy makers, and the general public. As the saying goes, it will require a paradigm shift. Below we imagine an approach that could be employed, and briefly discuss the strengths and limitations of such an approach.
Using the integrated 24-hour movement paradigm as a conceptual platform, an individualized “Movement Index” could be developed. This would be a single, integrated, personalized metric that takes into account daily PA, sedentary behavior, and sleep, as well as related correlates (e.g., age, sex, gender, race, ethnicity, SES, health status). Imagine the Movement Index as a score from 1 to 100, where a higher score represents a better movement composition for promoting and preserving health, specific to the individual. This movement from an isolationist conceptualization (e.g., the importance of sleep, exercise, or digital screen exposure) to a complex, integrated, and individual model (the whole day and each person matters) could inherently overcome persistent disregard for issues of equity, diversity and inclusion, and recognize the reality that optimal movement behavior compositions vary by age, sex, race, ethnicity, and underlying health conditions among others. Imagine evolving from the default of generic sex-merged and broad age-range blended recommendations that are adequate for all and optimal for none. Such an index would challenge our “line(s) in the sand” approach (e.g., 60 min per day of MVPA for children), where an individual is routinely dichotomized as meeting or not meeting a particular movement behavior recommendation, and opt for a more organic understanding that the health impact of integrated movement behaviors exist on a continuum and any “line in the sand” is inherently artificial, suboptimal for many, and disregards the opportunity to maximize health promotion guidance at any/all level(s).
While the concept of a more individualized approach would be new to the movement behavior field, other health behaviors have moved towards this direction with at least more nuanced guidance. For instance, dietary guidelines are consistently a subject of debate, and the health status of the client/patient often acts as a determinant in establishing specific guidelines.34 While “precision nutrition” is not included in the WHO's guidelines for a healthy diet,35 numerous scholars within this domain vigorously discuss the issue, providing, at minimum, promising pathways and perspectives for the field.36,37 A group of experts has suggested that “precision nutrition” might be a promising strategy to solve some nutritional issues in low- and middle-income countries by focusing on more detailed local data to refine nutritional recommendations.36 Another example of this precision approach is related to alcohol consumption. Many countries diverge (often based on national evidence) regarding the safe dose and/or the dose with minimal health risk of alcoholic beverage intake for an adult. These dosages can vary by sex, age, and often differ from one country to another.38, 39, 40 Without debating the merit of the quality of each country's evidence, this may indicate that the metric for a specific behavior can vary also according to cultural aspects. In addition, health behaviors (e.g., diet, PA, sleep) challenge and change the integration of the body's metabolic and inflammatory responses, inherently affecting biological strategies, or “precision health”, for better management of symptoms of certain diseases, such as some types of cancer.41
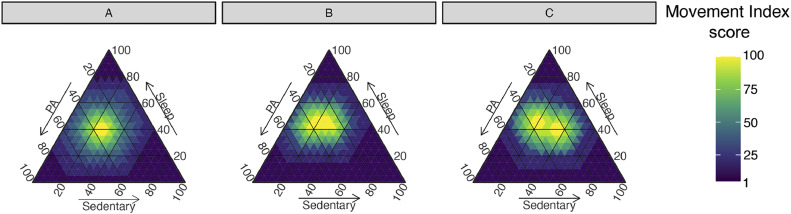
Fig. 1 provides a visual representation of how a 24-hour movement behavior integrated, individualized Movement Index could work. The figure provides a hypothetical example of an individual across 3 scenarios where their underlying characteristics (e.g., age, sex, gender, race, ethnicity, underlying health conditions, ability/disability, SES) vary and the Goldilocks zone—the movement behavior composition associated with the best health outcome25,28—drifts according to the best available research evidence. The illustration also shows that wherever an individual may reside in the heat map, there are multiple avenues to move towards the Goldilocks zone by readjusting combinations of movement behaviors. There are many routes to healthier movement behaviors, which can be customized to individual preferences, and the potency of any such nudges differ among individuals. One approach and one size does not fit all. Ultimately, with sufficient data feeding the Movement Index scoring mechanism, this precision health approach could be extended to be disease or health condition specific (e.g., what is the optimal movement behavior composition for promoting bone health in a 14-year-old Brazilian boy?). With population use over time, and artificial intelligence and machine learning capabilities, the precision possibilities of a personalized Movement Index would only improve.
Fig. 1.
Ternary plot illustrations of a personalized “Movement Index” as a function of movement behavior composition. Axes are the percentage of the 24-hour period in each movement behavior. In this illustration, the movement behavior composition is simplified to include just physical activity, sedentary behavior, and sleep to facilitate communication of a Movement Index score in a 2-dimensional diagram. Further disaggregation between intensities of physical activity (e.g., light, moderate, or vigorous), types of sedentary behavior (e.g., active vs. passive, screen time vs. non-screen), and/or sleep (e.g., sleep quality; naps/short bouts vs. nighttime/long bouts) is, however, possible. The heat map in each diagram represents the distribution of behaviors associated with Movement Index scores that could range from 1 to 100. Movement Index scores are determined as yellow/lighter for better scores and purple/dark for worse scores. The depicted Movement Index scores are hypothetical and not based on real data. (A–C) Examples of persons with a different combination of hypothetical traits (e.g., age, sex, gender, race, ethnicity, underlying health conditions, ability/disability, socioeconomic status), which modify the association between movement behavior combinations and Movement Index score (see how the Goldilocks zone drifts with different underlying characteristics—making it individualized). Plots similar to this illustration, with real data, could be developed for several health indicators and subsequently aggregated to a composite or master plot that would provide the basis for an individualized “precision health” scoring framework for a personalized “Movement Index”. PA = physical activity.
Using a personalized Movement Index approach would require a new surveillance approach. For example, rather than reporting population or sample proportions meeting or not meeting isolated or combined movement recommendations, public health assessments would report the average Movement Index for the whole population and/or specific age, sex, ethnic, or disease groups. Progress would be assessed based on whether personalized Movement Index scores improved (i.e., movement behavior compositions were healthier for the population under study). The new “line in the sand” might be the proportion of the population at or beyond a certain Movement Index score (e.g., 60/100) or a relative improvement in Movement Index scores (e.g., 10%).
A precision health approach using a personalized Movement Index to assess, monitor and surveil integrated movement behaviors has many advantages over existing approaches, including recognizing that one size does not fit all and providing more personalized guidance; embracing the totality of underlying research evidence that shows different health impacts of different movement behaviors among individuals with different characteristics; moving more authentically to a truly integrated approach to movement behaviors; avoiding step-wise changes in guidelines during transitions between age-group categories; being more inclusive by recognizing and accounting for differing characteristics among individuals; and providing greater flexibility in approaches to improve movement behaviors.
A paradigm shift to a precision health approach would also come with several possible limitations, some of which no doubt are unknown or not easily predicted. Some anticipated limitations include: resistance to leaving the existing guidelines approach behind; retraining requirements for practitioners/gate-keepers/end-users; changes required for surveillance and lack of continuity of measurement indices for temporal comparisons; potential risks of bias in calculation algorithms including inequities in underlying research (e.g., less resolution of understanding of certain mediators/moderators, less evidence from low- and middle-income countries leading to less precise Movement Index estimations and advice); loss of simpler public health recommendations (or efforts needed to find ways to retain simple messaging); loss of tangible secondary diffusion (e.g., recommendation for 60 min MVPA on a poster may be read and internalized in an unplanned way, whereas interacting with website or app to determine individualized composition may take more planning and intention); difficulties in engaging hard to reach groups (e.g., people without access to the internet); privacy concerns; and the difficulty of conveying an integrated, personalized approach.
5. Summary—Time for the next new paradigm
In the past decade a new paradigm integrating all movement behaviors (physical activities, sedentary behaviors, and sleep) recommendations into a single 24-hour movement behavior guideline has been adopted by many. Despite this advancement in holistic thinking, universal guidelines across broad age groups lack the specificity (e.g., by age, sex, gender, race, ethnicity, underlying health conditions, ability/disability, SES) of guidance contained in the underlying evidence. The new paradigm can provide advancements in the holistic understanding of the correlates and determinants of 24-hour movement behaviors and their relationships with health outcomes. For even broader reach and greater impact of this approach, there is a need to connect decision-makers, healthcare professionals, researchers, marginalized groups, and other stakeholders so that comprehensive information, insight, and perspectives contribute to the construction of future movement behavior guidelines.
Advancements in research techniques now provide a platform for individualized precision 24-hour movement behavior guidelines that customize recommendations to individual characteristics and circumstances making them more tailored and equitable. We can, so should, do better with our public health guidance. With this opinion piece we challenge 24-hour movement behavior researchers and guideline developers to venture into the next new paradigm and work to inform and develop precision 24-hour movement behavior guidelines, optimized for every individual, leading to precision insights and interventions, management and manipulations for improved population health and wellness. We encourage more and better research to further support or refute the premise of this opinion piece.
Acknowledgments
Acknowledgments
This project was supported in part by an anonymous donation to develop the Precision Child and Youth Mental Health Initiative. The funder had no role in in the writing, editing, or publishing of this manuscript.
Authors’ contributions
MST conceived and wrote the manuscript; MJD designed the figure. All authors reviewed the manuscript several times and helped with editing and rewriting. All authors have read and approved the final version of the manuscript, and agree with the order of presentations of the authors.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Peer review under responsibility of Shanghai University of Sport.
References
- 1.U.S. Department of Health and Human Services . U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion; Atlanta, GA: 1996. Physical activity and health: A report of the surgeon general. [Google Scholar]
- 2.Rahl RL. Human Kinetics Publishers; Champaign, IL: 2010. Physical activity and health guidelines: Recommendations for various ages, fitness levels, and conditions from 57 authoritative sources. [Google Scholar]
- 3.Tremblay MS, Warburton DER, Janssen I, et al. New Canadian physical activity guidelines. Appl Physiol Nutr Metab. 2011;36:36–46. doi: 10.1139/H11-009. [DOI] [PubMed] [Google Scholar]
- 4.Ross R, Janssen I, Tremblay MS. Public health importance of light intensity physical activity. J Sport Health Sci. 2024;13:674–675. doi: 10.1016/j.jshs.2024.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mendes MdA, da Silva I, Ramires V, et al. Metabolic equivalent of task (METs) thresholds as an indicator of physical activity intensity. PLoS One. 2018;13 doi: 10.1371/journal.pone.0200701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tremblay MS, Colley R, Saunders TJ, Healy GN, Owen N. Physiological and health implications of a sedentary lifestyle. Appl Physiol Nutr Metab. 2010;35:725–740. doi: 10.1139/H10-079. [DOI] [PubMed] [Google Scholar]
- 7.Tremblay MS, Aubert S, Barnes JD, et al. Sedentary Behavior Research Network (SBRN) – Terminology Consensus Project process and outcome. Int J Beh Nutr Phys Act. 2017;14:75. doi: 10.1186/s12966-017-0525-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tremblay MS, LeBlanc AG, Janssen I, et al. Canadian sedentary behaviour guidelines for children and youth. Appl Physiol Nutr Metab. 2011;36:59–64. doi: 10.1139/H11-012. [DOI] [PubMed] [Google Scholar]
- 9.Tremblay MS, LeBlanc AG, Carson V, et al. Canadian sedentary behavior guidelines for the early years (aged 0–4 years) Appl Physiol Nutr Metab. 2012;37:370–391. doi: 10.1139/h2012-019. [DOI] [PubMed] [Google Scholar]
- 10.2018 Physical Activity Guidelines Advisory Committee . U.S. Department of Health and Human Services; Washington, DC: 2018. 2018 Physical Activity Guidelines Advisory Committee Scientific Report. [Google Scholar]
- 11.Bull FC, Al-Ansari SS, Biddle S, et al. World Health Organization 2020 guidelines on physical activity and sedentary behavior. Br J Sports Med. 2020;54:1451–1462. doi: 10.1136/bjsports-2020-102955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tremblay MS, Carson V, Chaput J-P, et al. Canadian 24-Hour Movement Guidelines for children and youth: An integration of physical activity, sedentary Behavior, and sleep. Appl Physiol Nutr Metab. 2016;41(Suppl. 3):S311–S327. doi: 10.1139/apnm-2016-0151. [DOI] [PubMed] [Google Scholar]
- 13.Tremblay MS. Introducing 24-hour movement guidelines for the early years: A new paradigm gaining momentum. J Phys Act Health. 2020;17:92–95. doi: 10.1123/jpah.2019-0401. [DOI] [PubMed] [Google Scholar]
- 14.Tremblay MS, Ross R. How should we move for health? The case for the 24-hour movement paradigm. CMAJ. 2020;192:E17298–E17299. doi: 10.1503/cmaj.202345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tremblay MS, Chaput J-P, Adamo KB, et al. Canadian 24-Hour Movement Guidelines for the early years (0–4 years): An integration of physical activity, sedentary behavior, and sleep. BMC Public Health. 2017;17(Suppl. 5):874. doi: 10.1186/s12889-017-4859-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ross R, Chaput J-P, Giangregorio L, et al. Canadian 24-Hour Movement Guidelines for adults aged 18–64 years and adults aged 65 years or older: An integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab. 2020;45(Suppl. 2):S57–102. doi: 10.1139/apnm-2020-0467. [DOI] [PubMed] [Google Scholar]
- 17.World Health Organization . World Health Organization; Geneva: 2019. WHO guidelines on physical activity, sedentary behavior and sleep for children under 5 years of age. [PubMed] [Google Scholar]
- 18.Rollo S, Antsygina O, Tremblay MS. The whole day matters: Understanding 24-hour movement guideline adherence and relationships with health indicators across the lifespan. J Sport Health Sci. 2020;9:493–510. doi: 10.1016/j.jshs.2020.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tapia-Serrano MA, Sevil-Serrano J, Sánchez-Miguel PA, López-Gil JF, Tremblay MS, García-Hermoso A. Prevalence of meeting 24-Hour Movement Guidelines from pre-school to adolescence: A systematic-review and meta-analysis including 387,437 participants and 23 countries. J Sport Health Sci. 2022;11:427–437. doi: 10.1016/j.jshs.2022.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pedisic Z. Measurement issues and poor adjustments for physical activity and sleep undermine sedentary behavior research – The focus should shift to the balance between sleep, sedentary behavior, standing and activity. Kinesiology. 2014;46:135–146. [Google Scholar]
- 21.Chastin SFM, Palarea-Albaladejo J, Dontje ML, Skelton DA. Combined effects of time spent in physical activity, sedentary behaviors and sleep on obesity and cardio-metabolic health markers: A novel compositional data analysis approach. PLoS One. 2015;10 doi: 10.1371/journal.pone.0139984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Carson V, Tremblay MS, Chaput J-P, Chastin SFM. Associations between sleep duration, sedentary time, physical activity and health indicators among Canadian children and youth using compositional analyses. Appl Physiol Nutr Metab. 2016;41(Suppl. 3):S294–S302. doi: 10.1139/apnm-2016-0026. [DOI] [PubMed] [Google Scholar]
- 23.Tremblay MS, Rollo S, Saunders TJ. Sedentary Behavior Research Network members support new Canadian 24-Hour Movement Guideline recommendations. J Sport Health Sci. 2020;9:479–481. doi: 10.1016/j.jshs.2020.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Straker L, Zabatiero J, Danby S, Thorpe K, Edwards S. Conflicting guidelines on young children's screen time and use of digital technology create policy and practice dilemmas. J Pediatr. 2018;202:300–303. doi: 10.1016/j.jpeds.2018.07.019. [DOI] [PubMed] [Google Scholar]
- 25.Duncan MJ, Kuzik N, Silva DAS, et al. “Goldilocks days” for adolescent mental health: Movement behavior combinations for well-being, anxiety and depression by gender. Mental Health Phys Act. 2024;26 doi: 10.1016/j.mhpa.2023.100572. [DOI] [Google Scholar]
- 26.Sampasa-Kanyinga H, Lien A, Hamilton HA, Chaput JP. The Canadian 24-Hour Movement Guidelines and self-rated physical and mental health among adolescents. Can J Public Health. 2022;113:312–321. doi: 10.17269/s41997-021-00568-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Roman-Viñas B, Chaput J-P, Katzmarzyk PT, et al. Proportion of children meeting recommendations for 24-hour movement guidelines and associations with adiposity in a 12-country study. Int J Behav Nutr Phys Act. 2016;13:123. doi: 10.1186/s12966-016-0449-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dumuid D, Olds T, Wake M, et al. Your best day: An interactive app to translate how time reallocations within a 24-hour day are associated with health measures. PLoS One. 2022;17 doi: 10.1371/journal.pone.0272343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Faulkner G, White L, Raizi N, Latimer-Cheung AE, Tremblay MS. Canadian 24-Hour Movement Guidelines for children and youth: Exploring the perceptions of stakeholders regarding their acceptability, barriers to uptake, and dissemination. Appl Physiol Nutr Metab. 2016;41(Suppl. 3):S303–S310. doi: 10.1139/apnm-2016-0100. [DOI] [PubMed] [Google Scholar]
- 30.Tremblay MS, Haskell WL. In: Physical activity and health. 2nd ed. Bouchard C, Blair SN, Haskell WL, editors. Human Kinetics Publishers; Champaign, IL: 2012. From science to physical activity guidelines; pp. 359–378. [Google Scholar]
- 31.Silva DAS, Duncan MJ, Kuzik N, Tremblay MS. Associations between anxiety disorders and depression symptoms are related to 24-hour movement behaviors among Brazilian adolescents. J Affective Disorders. 2023;339:280–292. doi: 10.1016/j.jad.2023.07.004. [DOI] [PubMed] [Google Scholar]
- 32.Silva DAS, Duncan MJ, Kuzik N, Tremblay MS. Race/ethnicity inequities in the association between movement behaviors and suicidal thoughts/ideation among adolescents. J Pediatr Psychol. 2024;49:166–174. doi: 10.1093/jpepsy/jsad085. [DOI] [PubMed] [Google Scholar]
- 33.Kong C, Chen A, Ludyga S, et al. Associations between meeting 24-hour movement guidelines and quality of life among children and adolescents with autism spectrum disorder. J Sport Health Sci. 2023;12:73–86. doi: 10.1016/j.jshs.2022.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hong BV, Agus JK, Tang X, et al. Precision nutrition and cardiovascular disease risk reduction: The promise of high-density lipoproteins. Curr Atheroscler Rep. 2023;25:663–677. doi: 10.1007/s11883-023-01148-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.World Health Organization. Carbohydrate intake for adults and children: WHO guideline summary. Available at: https://iris.who.int/handle/10665/374925. [accessed 23.03.2024]. [PubMed]
- 36.Bedsaul-Fryer JR, van Zutphen-Küffer KG, Monroy-Gomez J, et al. Precision nutrition opportunities to help mitigate nutrition and health challenges in low- and middle-income countries: An expert opinion survey. Nutrients. 2023;15:3247. doi: 10.3390/nu15143247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bailey RL, Stover PJ. Precision nutrition: The hype is exceeding the science and evidentiary standards needed to inform public health recommendations for prevention of chronic disease. Annu Rev Nutr. 2023;43:385–407. doi: 10.1146/annurev-nutr-061021-025153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Paradis C, Butt P, Shield K, et al. Canadian Centre on Substance Use and Addiction; Ottawa, ON: 2023. Canada's guidance on alcohol and health: Final report. [Google Scholar]
- 39.AustralianGovernment . National Health and Medical Research Council. Commonwealth of Australia; Canberra: 2020. Australian guidelines to reduce health risks from drinking alcohol. [Google Scholar]
- 40.European Commission . European Commission; 2023. National low-risk drinking recommendations (or drinking guidelines) and standard units. [Google Scholar]
- 41.Sleight AG, Crowder SL, Skarbinski J, et al. A new approach to understanding cancer-related fatigue: Leveraging the 3P Model to facilitate risk prediction and clinical care. Cancers (Basel) 2022;14:1982. doi: 10.3390/cancers14081982. [DOI] [PMC free article] [PubMed] [Google Scholar]