Highlights
-
•
Running/training characteristics and health and lifestyle factors, along with morphological and biomechanical aspects, show large effect sizes in increasing the risk for running-related injuries (RRIs).
-
•
The review highlights methodological issues in the design, conduction, and reporting of the included systematic reviews, indicating the need for higher quality studies.
-
•
Most primary studies and systematic reviews did not focus on specific injuries, complicating the identification of distinct risk factors associated with each injury type.
-
•
Biomechanical factors were the main focus of existing meta-analyses, but evidence remains insufficient to conclusively identify biomechanical risk factors.
Keywords: Umbrella review, Runners, Injury, Risk factor
Abstract
Purpose
This umbrella systematic review (SR) of SRs and meta-analysis seeks to comprehensively synthesize existing literature to identify and consolidate the diverse range of risk factors contributing to running-related injuries (RRIs).
Methods
Systematic searches were conducted on June 28, 2023, across Web of Science, SPORTDiscus, Scopus, PubMed, and Cochrane Library. We included SRs, whether accompanied by meta-analyses or not, that focused on investigating risk factors for RRIs within observational studies. The methodological quality of the SRs was evaluated using the Assessing the Methodological Quality of Systematic Reviews II. To assess the extent of overlap across reviews, the corrected covered area metric was calculated.
Results
From 1509 records retrieved, 13 SRs were included. The degree of overlap between SRs was low (4%), and quality varied from critically low (n = 8) to low (n = 5). Two hundred seven outcomes assessed in 148 primary studies were identified as being associated with the occurrence of RRIs. The effect sizes of the associations for which risk measures were reported (n = 131) were classified as large (n = 30, 23%), medium (n = 38, 29%), small (n = 48, 37%) or no effect (n = 15, 11%). Running/training characteristics, health and lifestyle factors, along with morphological and biomechanical aspects, exhibit large effect sizes in increasing the risk for RRIs.
Conclusion
Drawing from the outcomes of the low-quality SRs and associations with large effect sizes, our findings indicate that running/training characteristics and health and lifestyle factors, as well as morphological and biomechanical aspects, are all implicated in elevating the risk of RRIs, emphasizing the multifactorial basis of injury incidence in running. Given the low quality and heterogeneity of SR, individual findings warrant cautious interpretation.
Graphical Abstract
1. Introduction
Running is one of the most popular and practiced sport activities.1 It is an accessible, low-cost sport with well-known health benefits that has attracted many individuals that choose running as their main sport activity.1,2 Running-related injuries (RRIs), however, are common among runners3, 4, 5 with an incidence rate that varies from 4.26 (recreational runners) to 33.07 (novice runners) per 1000 h of running exposure. The knee, lower leg, and foot are the most affected sites,3 whereas patellofemoral pain syndrome, medial tibial stress, plantar fasciitis, iliotibial band syndrome, and Achilles tendinopathy are the most frequent diagnoses.3,4 RRIs lead to excessive health costs that often include visiting a general practitioner and medical specialist, surgical treatment, physiotherapy, and medication.8,9 Time loss to recovery10 and absences from work8,9 also have an important impact on the individual quality of life and productivity.
RRIs are multifactorial and result from the complex interaction between individual attributes (e.g., age, gender, body mass index),4,11,12 morphological risk factors (e.g., navicular drop, Q-angle, and arch index),12, 13, 14 biomechanics (e.g., running kinematics and kinetics),15, 16, 17 and running/training features (e.g., training frequency, volume, experience),4,12 as well as health and lifestyle factors (e.g., medical history, alcohol consumption and participation in other sports).4,11,14 These 5 domains have received great attention but despite extensive research, risk factors for RRIs remain unclear.14,18
A comprehensive analysis integrating previously published systematic reviews (SRs) or meta-analyses is missing.6,11,13,14,16, 17, 18, 19, 20 In the last 3 years, 7 SRs and meta-analyses were published, including 155 observational prospective studies.11,13,17,19, 20, 21, 22 To identify and consolidate the diverse range of risk factors contributing to RRIs, an umbrella review, and analysis of the current state of knowledge in this field is necessary. Current knowledge on this topic will support evidence-based practice and guide future studies.23,24 In this study, we aimed to examine risk factors for RRIs through an umbrella SR of SRs and meta-analysis.
2. Methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines25 and recommendations for Umbrella Reviews23 were followed to conduct this study. The protocol of this study was registered in the International Prospective Register of Systematic Reviews (PROSPERO) (registration number CRD42021286241).
2.1. Search strategy
Five electronic bibliographic databases were searched: Web of Science, SPORTDiscus, Scopus, PubMed, and Cochrane Library. We limited searches to peer-reviewed journal articles published in English language from database inception to June 28, 2023. The search strategy used keywords related to injury, running, and reviews. Full description of search strategy used in each database is presented in Supplementary File 1.
The search strategy was implemented in the fields of title, abstract, and keywords of each database. The articles resulting from the search were inserted into Endnote (Version 21; Clarivate, Philadelphia, PA, USA), and duplicates were removed. Articles were then exported to Rayyan platform26 and 2 independent researchers (CKC and JMM) conducted the study selection. A third researcher (CR) resolved any discrepancies.
2.2. Eligibility criteria
We used PECOS (Population, Exposure, Comparator, Outcomes, and Study design) strategy for eligibility criteria (Table 1).
Table 1.
PECOS strategy.
| PECOS strategy | Inclusion criteria | Exclusion criteria |
|---|---|---|
| Population | Healthy adults ≥18 years old | − |
| Exposure | Running | Other sports that involve running (i.e., soccer, handball, basketball, jogging, walking, etc.) |
| Comparator | No comparisons were made. | − |
| Outcomes | Risk factors for lower limb and/or lower back and/or trunk injury | − |
| Study design | Systematic reviews with or without meta-analysis that included observational studies (prospective, retrospective and case-control) | Case reports, comments, narrative reviews and not published in peer-reviewed journals |
Abbreviation: PECOS = Population, Exposure, Comparator, Outcomes, and Study design.
2.3. Data extraction
Two authors (CKC and JMM) extracted data from 13 SRs. The results were similar and therefore, only 1 author (CKC) continued with data extraction. The following information was extracted from each SRs:
-
a)
Publication year;
-
b)
Geographic region: Country of first author's affiliation;
-
c)
Review type: SR or SR with a meta-analysis;
-
d)
Number of studies: Number of articles included under each review;
-
e)
Publication period: Search period;
-
f)
Search strategy: Databases searched;
-
g)
Primary study type: Prospective, retrospective, or case-control;
-
h)
Participants characteristics: Number of participants, age, gender, body mass index, running experience (novice, recreational, competitive, cross-country, short or long distance);
-
i)
Follow-up period: Duration of participants’ follow-up;
-
j)
Injury definition: Whether the review reported the definition of injury of each primary;
-
k)
Main anatomical injury site: Lower extremity, groin, knee, ankle, and/or other sites; 27
-
l)
Main diagnosis/injury: Patellofemoral pain syndrome, medial tibial stress syndrome, plantar fasciitis, Achilles tendinopathy, stress fracture, ankle sprain, and/or other diagnosis;3
-
m)
Risk factors: Any outcome that was significantly associated (p < 0.05) with RRIs in a bivariate analysis; or that presented odds ratio (OR), relative risk (RR), or hazard ratio (HR) values greater than 1.0 in a regression analysis;
-
n)
Measures of risk: OR, RR, or HR values; and 95% confidence interval (95%CI);
-
o)
PRISMA: Whether the review followed the PRISMA statement;
-
p)
Risk of bias: Methods used to assess risk of bias and the results of this analysis;
-
q)
Level of evidence: Whether the review reported the level of evidence for each risk factor, which tool was used, and the interpretation of the result;
-
r)
Meta-analysis: Estimates, effect size, and heterogeneity (I², as %).
Based on the extracted values of OR, RR, and HR, effect sizes of the measures were interpreted as follow28: no effect: RR or HR < 1.21 or OR < 1.31; small effect: RR or HR: 1.22–1.85 or OR: 1.32–2.37; medium effect: RR or HR: 1.86–2.99 or OR: 2.38–4.69; large effect: RR or HR > 3.00 or OR > 4.70.
A narrative synthesis of the included SRs was carried out according to the domains previously established in the literature4,11,12: (a) individual attributes, (b) running/training, (c) health and lifestyle, (d) morphological, and (e) biomechanical factors. For each domain, risk factors were identified based on the outcomes reported in the SRs.
2.4. Overlap
In umbrella reviews, overlap indicates the degree of primary studies were included in more than 1 SRs.29,30 To identify the overlap 1 author (CKC) elaborated a citation matrix,30 which is schematically shown in Fig. 1. The corrected covered area (CCA) was calculated using the following equation:30
| (1) |
where N is the total number of included publications (total number of ticked boxes in the citation matrix); r is the number of primary studies (rows); and c is the number of SRs (columns).
Fig 1.
Example of matrix and corrected covered area (CCA) formula. c = number of systematic reviews (columns); N = Total number of included publications (total number of ticked boxes in the citation matrix); r = number of primary studies (rows).
The CCA results were expressed in percentage (%) and interpreted as follows: 0–5 as slight/low; 6–10 as moderate; 11–15 as high; and >15 as very high overlap.30 A CCA of 100% means that every review included in this umbrella SR comprised the same studies. On the other hand, a CCA of 0% indicates that every review included was composed by unique studies.
2.5. Quality assessment
The quality assessment of the included SRs was performed using the Assessing the Methodological Quality of Systematic Reviews II (AMSTAR 2).31,32 The checklist consists of 16 different items with 3 answering options: yes, partial yes, or no. Compared to the original checklist, the AMSTAR 2 was modified to cover studies of risk factors.33 The items that refer to interventions were replaced by exposures.33 The final rating was interpreted as follows: (a) high: no or 1 non-critical weakness; (b) moderate: more than 1 non-critical weakness; (c) low: 1 critical flaw with or without non-critical weaknesses; or (d) critically low: more than 1 critical flaw with or without non-critical weaknesses.31,32 Two researchers (CKC and JMM) performed the quality assessment independently. Discrepancies were solved by discussion and consensus or by a third researcher (CR).
3. Results
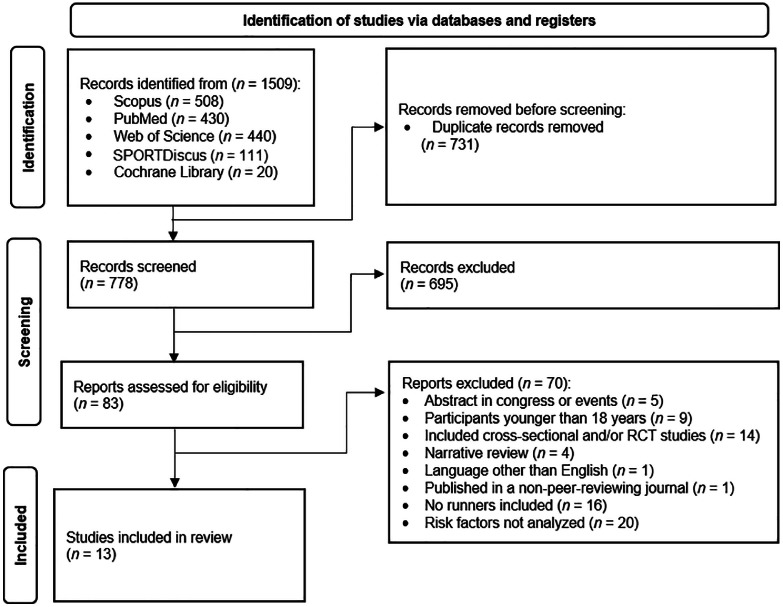
The search identified 1509 records. After removing 731 duplicates and screening titles and abstracts, 83 SRs were considered for inclusion. Of the 83 studies selected for full reading, 43 studies had discrepancies. After the authors discussed the inclusion and exclusion criteria, the conflict between the 43 studies was resolved. Finally, 13 SRs were included after full-text assessment (Fig. 2). The reasons for exclusions are reported in Supplementary File 2.
Fig 2.
PRISMA 2020 flow diagram. PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses. RCT = randomized controlled trial.
The first SR was published in 2007.4 The primary studies were mostly prospective, and the number of primary studies ranged from 1 study19 to 66 studies.21 Most SRs used Downs and Black Quality Index17,19, 20, 21,34 to assess the risk of bias. Further methodological information from each SR is presented in Table 2.
Table 2.
Methodological information from each SR.
| Study | Geographic region | Review type | PRISMA | Databases searched | Search period | Primary studies | Number of primary studies | Risk of bias assessment tools | Level of evidence assessment tools |
|---|---|---|---|---|---|---|---|---|---|
| Van Gent et al (2007)4 | Netherlands | SR | NR | PubMed | Databases inception until January 2006 | Prospective and retrospective | 17 | Quality scoring tool elaborated by authors | Guidelines of van Tulder et al. (2003)40 |
| Van Poppel et al. (2021)11 | Netherlands | SR | Yes | PubMed, CINAHL, Cochrane Library | Databases inception until February 2019 | Prospective | 29 | Quality in prognosis studies and Prediction model risk of Bias Assessment Tool | GRADE |
| Van der Worp et al. (2015)12 | Netherlands | SR | No | CINAHL, Embase, PubMed and PsycInfo | CINAHL (1982 to December 26, 2012), Embase (1947 to January 1, 2013), PubMed (1940 to December 26, 2012), and PsycInfo (1806 to January 1, 2013) | Prospective and retrospective | 15 | Modified assessment tools of the Cochrane Collaboration and previous systematic reviews of risk factors for musculoskeletal disorders | Guidelines of van Tulder et al. (2003)40 |
| Peterson et al. (2022)13 | Australia | SR and meta-analysis | Yes | MEDLINE, Embase, CINAHL, SPORTDiscus, AMED and Cochrane library | Database inception until January 13, 2021 | Prospective | 30 | Health Evidence Bulletins | NA |
| Saragiotto et al. (2014)14 | Brazil | SR | NR | Embase, PubMed, CINAHL, SPORTDiscus, Latin American and Caribbean Centre on Health Sciences Information and Scientific Electronic Library Online | Embase (1980 to December 2012), PubMed (1946 to December 2012), CINAHL (1988 to December 2012) SPORTDiscus (1977 to December 2012), Latin American and Caribbean Centre on Health Sciences Information (1985 to December 2012) and Scientific Electronic Library Online (1998 to December 2012) | Prospective | 11 | Modified Newcastle Ottawa Scale | NA |
| Vannatta et al. (2020)17 | USA | SR and meta-analysis | NR | MEDLINE, CINAHAL and PubMed | Databases inception to January 2019 | Prospective | 13 | Downs and Black Quality Index | Modified version of guidelines of van Tulder et al. (2003)40 |
| Anderson et al. (2020)19 | Australia | SR | Yes | Medline, Embase, CINAHL and SPORT Discus | Databases inception to the 4th week of April 2019 | Prospectivea | 53 (1) | Downs and Black Quality Index | Modified version of guidelines of van Tulder et al. (2003)40 |
| Burke et al. (2021)20 | Ireland | SR | Yes | MEDLINE, PubMed, SPORTDiscus and Web of Science | January 1960 to Nov 2020 | Retrospective and prospective | 13 | Downs and Black Quality Index | GRADE |
| Willwacher et al. (2022)21 | Germany | SR | Yes | PubMed | Databases inception to February 5, 2021 | Prospective and retrospective | 66 | Downs and Black Quality Index | Guidelines of van Tulder et al. (2003)40 |
| Ross et al. (2023)22 | USA | SR | PubMed, Embase, CINAHL, Ovid MEDLINE | Database inception until November 30, 2020 | Prospective and retrospective | 10 (3) | Joanna-Briggs Institute Critical Appraisal Tool | NA | |
| Neal et al. (2016)34 | United Kingdom | SR and meta-analysis | Yes | Web of Science, MEDLINE and CINAHL | Database inception until April 2015 | Case control and prospective | 28 (2) | Downs and Black Quality Index | Guidelines of van Tulder et al. (2003)40 |
| Louw and Dreary (2014)35 | United Kingdom | SR | Yes | 34 databases (main: CINAHL, PsycInfo, Embase, PubMed, ScienceDirect and Web of Science) | Databases inception to July 2011 | Prospective and retrospective case control | 12 | Quality assessment tool for quantitative studies | Guidelines of Reid and Rivett (2005)41 |
| Mann et al. (2016)36 | Luxembourg | SR | Yes | PubMed, Embase, CINAHL, ScienceDirect and Scopus | Database inception until March 2015 | Prospective and retrospective | 8 | Modified version of assessment tool prepared by other authors | NA |
Note: Numbers in brackets represent the number of only observational studies included in systematic review.
Abbreviations: GRADE = Grading of Recommendations Assessment, Development, and Evaluation; NA = not applied; NR = not reported; PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses; SR = systematic review.
Participants’ characteristics, follow-up periods, and injury information are presented in Table 3. The number of included participants in each SR ranged from 52 participants19 to 16,836 participants.11 Seven SRs reported participant age, ranging from 1835 to 50 years.35 Participants’ running experiences varied across categories such as novice,12, 13, 14,25,36 recreational,4,12, 13, 14,17,20,22,36 competitive4,12, 13, 14,20 or experienced;22,36 engaging in activities including cross-country,12,14,17,19,20 track and field,4 and short or long distances.11 The follow-up periods, as reported in 7 SRs, ranged from 1 day4 to 7 years.20 The most prevalent diagnoses included overall RRIs,11,12,14,17,20,36 Achilles tendinopathy,11, 12, 13,17,21,36 patellofemoral pain,11, 12, 13,17,21,36 iliotibial band syndrome,13,17,21,35,36 and stress fractures.11,19,36
Table 3.
Participant's characteristics, follow-up period and injury information.
| Review | Participants characteristics |
Follow-up period (min–max) | Injury |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total participants | Average age (min–max) |
Gender | Mean BMI (min–max) | Running experience | Other characteristics | Definition | Anatomical area | Main diagnosis | ||
| Van Gent et al (2007)4 | 13,662 | NR | M/F | NR | Track and field, recreational and competitive | – | 1 day–18 months | Yes | Ankle, lower leg, knee, upper leg, hip/pelvis and lower extremity | Skin lesions, pain/stiffness, overuse, cramps, ankle sprain, joint problems, tendonitis and other injuries |
| Van Poppel et al. (2021)11 | 16,836 | 36.6–43.3 | M/F | 24.6–26.3 | Short and long distance | – | 6 weeks–1 year | Yes | NR | Overall RRIs, PFP, Achilles tendinopathy, stress fractures |
| Van der Worp et al. (2015)12 | 9643 | 36–44 | M/F | 23.0–25.9 | Novice, recreational, competitive and cross-country | – | 8 weeks–1 year | Yes | NA | Overall RRIs, Achilles tendinopathy, and PFP |
| Peterson et al. (2022)13 | 3404 | NR | M/F | NR | Novice, recreational and competitive | – | 8 weeks–2 years | NR | NA | Lower leg pain, PFP, iliotibial band syndrome and Achilles tendinopathy |
| Saragiotto et al. (2014)14 | 4671 | NR | NR | NR | Novice, recreational, competitive and cross-country | – | NR | NR | NR | Overall RRIs |
| Vannatta et al. (2020)17 | 932 | 19.2–45.0 | M/F | 19.9–24.5 | Recreational and cross-country | – | 1 season–2 years | Yes | NA | Overall RRIs, PFP, iliotibial band syndrome, Achilles tendinopathy |
| Anderson et al. (2020)19 | 52 | 20 | M/F | 20–21 | Cross-country | Foot strike patterns: rearfoot and forefoot | 5 years | NR | NA | Repetitive stress injuries |
| Burke et al. (2021)20 | 2564 | 19–42 | M/F | 20.3–24.6 | Cross-country, recreational and competitive | Foot strike patterns: rearfoot, midfoot and forefoot | 4 months–7 years | Yes | NR | Overall RRIs |
| Willwacher et al. (2022)21 | 16,370 | NR | M/F | NR | NR | – | NR | NR | NA | Achilles tendinopathy, medial tibial stress syndrome, tibial stress fractures, plantar fasciitis, iliotibial band syndrome, PFP, patellar tendinopathy, hamstring tendinopathy |
| Ross et al. (2023)22 | 7353 | 37.3–46.5 | M/F | NR | Novice, recreational and experienced | – | NR | Yes | Hip/Groin | Hip/groin RRIs |
| Louw and Dreary (2014)35 | 530 | NR (age range: 18–50) | M/F | NR | Only runners | – | NR | Yes | NA | Iliotibial band syndrome |
| Mann et al. (2016)36 | 669 | NR | M/F | NR | Novice, recreational and experienced | – | NR | NR | NA | PFP, lower leg injuries, Achilles tendinopathy, iliotibial band syndrome, second metatarsal stress fracture, plantar fasciitis and RRIs |
Abbreviations: BMI = body mass index; F = female; M = male; NA = not applicable; NR = not reported; PFP = patellofemoral pain; RRIs = running-related injuries.
The 13 SRs included a total of 148 different primary studies that investigated risk factors for RRIs. The degree of overlap between SRs was considered low (CCA = 0.04; 4%). Findings are grouped and presented in detail in Supplementary Files according to the following domains: individual attributes (Supplementary File 3), running/training factors (Supplementary File 4), health and lifestyle factors (Supplementary File 5), morphological factors (Supplementary File 6), and biomechanical factors (Supplementary Files 7 and 8).
The quality appraisal of the 13 SRs is presented in Table 4. In general, the quality of the SRs was classified as being critically low (8 reviews)4,14,17,19,21,34, 35, 36 and low (5 reviews).11, 12, 13,20,21
Table 4.
Quality appraisal of the systematic reviews included on this umbrella review.
| Study | AMSTAR tool |
Total | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | ||
| Anderson et al. (2020)19 | No | Partial yes | No | Partial yes | Yes | No | No | No | Yes | No | Yes | No | No | No | No | Yes | Critically low-quality review |
| Burke et al. (2021)20 | Yes | Yes | Yes | Partial yes | Yes | No | No | Yes | Yes | No | 0 | 0 | Yes | Yes | 0 | Yes | Low-quality review |
| Louw and Dreary (2014)35 | Yes | No | Yes | Partial yes | No | No | No | Partial yes | Yes | No | 0 | 0 | Yes | No | 0 | Yes | Critically low-quality review |
| Neal et al. (2016)34 | Yes | No | Yes | No | Yes | No | No | Yes | Yes | No | No | No | No | No | No | Yes | Critically low-quality review |
| Saragiotto et al. (2014)14 | Yes | No | Yes | Partial yes | Yes | Yes | No | Partial yes | Yes | No | 0 | 0 | Yes | Yes | 0 | Yes | Critically low-quality review |
| Van der Worp et al. (2015)12 | Yes | Partial yes | Yes | Partial yes | Yes | No | No | Yes | Yes | No | 0 | 0 | Yes | Yes | 0 | Yes | Low-quality review |
| Van Gent et al. (2007)4 | Yes | No | Yes | No | No | No | No | Yes | Yes | No | 0 | 0 | Yes | No | 0 | No | Critically low-quality review |
| Van Poppel et al. (2021)11 | Yes | Yes | Yes | Partial yes | Yes | No | No | Yes | Yes | No | 0 | 0 | Yes | No | 0 | Yes | Low-quality review |
| Vanatta et al. (2020)17 | Yes | Partial yes | Yes | Partial yes | Yes | No | No | Yes | Yes | No | Yes | Yes | Yes | No | No | Yes | Critically low-quality review |
| Willwacher et al. (2022)21 | Yes | Partial yes | Yes | No | Yes | Yes | No | Yes | Yes | No | 0 | 0 | No | No | 0 | Yes | Critically low-quality review |
| Mann et al. (2016)36 | No | No | Yes | Partial yes | Yes | No | No | Partial yes | Yes | No | 0 | 0 | Yes | No | 0 | Yes | Critically low-quality review |
| Peterson et al. (2022)13 | Yes | Partial yes | Yes | Partial yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | No | Yes | Low-quality review |
| Ross et al (2023)22 | Yes | Partial yes | Yes | Partial yes | Yes | Yes | No | Yes | Yes | No | 0 | 0 | Yes | No | 0 | Yes | Low-quality review |
Notes: (1) Did the research questions and inclusion criteria for the review include the components of PICO? (2) Did the report of the review contain an explicit statement that the review methods were established prior to the conduct of the review and did the report justify any significant deviations from the protocol? (3) Did the review authors explain their selection of the study designs for inclusion in the review? (4) Did the review authors use a comprehensive literature search strategy? (5) Did the review authors perform study selection in duplicate? (6) Did the review authors perform data extraction in duplicate? (7) Did the review authors provide a list of excluded studies and justify the exclusions? (8) Did the review authors describe the included studies in adequate detail? (9) Did the review authors use a satisfactory technique for assessing the risk of bias (RoB) in individual studies that were included in the review? (10) Did the review authors report on the sources of funding for the studies included in the review? (11) If meta-analysis was performed, did the review authors use appropriate methods for statistical combination of results? (12) If meta-analysis was performed, did the review authors assess the potential impact of RoB in individual studies on the results of the meta-analysis or other evidence synthesis? (13) Did the review authors account for RoB in primary studies when interpreting/discussing the results of the review? (14) Did the review authors provide a satisfactory explanation for, and discussion of, any heterogeneity observed in the results of the review? (15) If they performed quantitative synthesis did the review authors carry out an adequate investigation of publication bias (small study bias) and discuss its likely impact on the results of the review? (16) Did the review authors report any potential sources of conflict of interest, including any funding they received for conducting the review?
Abbreviations: AMSTAR = A MeaSurement Tool to Assess systematic Reviews; PICO = Population, Intervention, Comparation, and Outcome.
Fifty-nine different factors across all domains were identified based on the outcomes reported in the SRs. Of these, 5 factors are from the individual attribute domain, 6 factors from the health and lifestyle domain, 17 factors from the running/training domain, 5 factors from the morphological domain and 26 factors from the biomechanical domain. These factors are listed in the first column of the respective Supplementary Files 3–8. The effect size of each outcome was reported, being classified as large (23% of the outcomes, n = 30), medium (29%, n = 38), small (37%, n = 48), and as no effect (11%, n = 15). For the remaining 38% (n = 81) of the outcomes reported in the SR, the value of the risk measure was not reported.
In Fig. 3, we summarize the risk factors for RRI. In this summary, we exclude outcomes associated with a RR or HR < 1.21 or OR < 1.31 (indicative of no effect) and also findings reported from critically low-quality SRs.
Fig 3.
Overview of risk factors for RRIs considering only the systematic reviews with low quality, according to the classification of the effect size of the measures of risk (large, medium, and small effect sizes). Results are shown for studies that showed low quality (n = 5). RPE = rating of perceived exercise; RRIs = running-related injuries.
Four SRs performed meta-analysis.13,17,19,34 Only biomechanical risk factors were investigated. During the stance phase of running, slower hip adduction velocity (mean difference = −12,8 °/s; p = 0.04),13 higher peak force under 2nd metatarsal (standardized mean difference = 0.65; p = 0.02),34 and under 3rd metatarsal (standardized mean difference = 0.60; p = 0.03);34 and lower time to peak force underneath the lateral heel (standardized mean difference = −0.56; p = 0.04)34 are shown to increase the risk for RRIs. Less knee extension strength (standardized mean difference = −0.19; p = 0.03)13 was also considered to increase the risk for RRIs. Regarding the level of evidence available in each SRs, the results of the meta-analyses indicated limited and conflicting evidence for all these risk factors (Supplementary File 9).
4. Discussion
This umbrella SR of SRs and meta-analysis synthesizes the existing literature regarding the diverse range of risk factors contributing to RRIs, providing a comprehensive overview and analysis of the current state of knowledge in this field. This is the first umbrella review to systematically summarize risk factors for RRIs. Our results highlight the significant interest of researchers in this topic and corroborate the assumption of a multivariate etiology for RRIs.
Our analysis showed unsatisfactory quality for all the included SRs, ranging between critically low and low quality. This indicates the presence of methodological issues in their design, conduction and/or reporting, based on the critical domains assessed by AMSTAR 2 tool. Most SRs did not provide a list of excluded studies, failed to present a comprehensive literature search strategy, and did not provide a proper description of an explicit statement that the review methods were established prior (PROSPERO database registration and significant deviations from the protocol were stated). The registration of SRs minimizes the occurrence of duplicate reviews or reviews with similar objectives, promotes transparency, and reduces the potential risk of bias.37 In agreement with tool recommendations,31 reviews that were classified as critically low quality should not be used, and low quality SRs should be used with caution.31 More high-quality SRs are necessary and will strengthen the evidence about RRIs to guide training and injury prevention programs.
Methodological differences between primary studies were found, which contributes to the heterogeneity of SRs and meta-analyses. This lack of consistency results in insufficient information to confirm the robustness and generalizability of the data. Several considerations should guide the design of future observational studies, including clarity in defining injuries,38 specifying follow-up length, describing the studied population and outcomes, and thoroughly reporting confounding factors.39 High-quality observational studies that address these aspects are necessary for advancing knowledge in this field.
The heterogeneity of SRs poses a challenge for comprehending the risk factors for injuries in running. Differences in the population investigated, injury definition, length of follow-up, and sample size across studies are some of the sources of heterogeneity. Most SRs studied mixed population, such as novice, recreational, competitive, and/or cross-country runners with very little attention given to running experience separately. Some SRs focused on a specific injury, such as patellofemoral pain,34 iliotibial syndrome35 or repetitive stress injuries,19 but most reported on overall RRIs.4,11,12,14,17 Five SRs did not report the length of follow-up.14,21,22,35,36 Of those that report, the length of follow-up varied considerably among the SRs, ranging from 1 day4 to 7 years.20 Additionally, the definition of RRIs is different across individual studies and, consequently, in each SR. To address these issues, we suggest that future SRs should consider narrowing the scope and focusing on a single question, such as a specific injury or running experience.
It seems extremely important to have a clear definition for injury in future studies,38 given that different definitions can lead to different estimates of effect for injury (OR, HR, or RR, for example), and incidence estimates. Lack of clarity in the description and definition of the outcomes is also an issue. Previous injury, for example, corresponds with “an injury 12 months before a new injury” in some studies, while others assess it as the history of injury, regardless of time.
RRIs seem to share common risk factors, particularly those associated with running/training characteristics and health-related lifestyle factors. These factors likely play a significant role in various types of RRIs. Conversely, biomechanical and morphological factors might be more specific to certain types of injuries, such as iliotibial band syndrome, patellofemoral pain syndrome, medial tibial stress syndrome, and Achilles tendinopathy. However, this remains speculative as, most primary studies and SRs did not address a specific injury (i.e. Achilles tendinopathy, patellofemoral pain, iliotibial band syndrome, and stress fractures). Instead, they grouped these injuries under the term “overall RRIs”, which complicates the identification of specific risk factors associated with each distinct injury.
Despite the efforts of researchers in the field, the main risk factors, or the set of risk factors for RRIs, remain unclear. The existing meta-analyses focus only on biomechanical factors. However, despite the large volume of information, the current evidence remains insufficient to conclusively identify biomechanical risk factors. Subsequent research efforts could contribute to future meta-analyses incorporating individual attributes, such as running/training patterns, health and lifestyle indicators, and morphological risk factors.
The main strength of this work is to provide an overview of the current state of research on risk factors for RRIs. The comprehensiveness of the search and the qualitative approach used to report the current evidence must be acknowledged. We found a low overlap degree among the SRs, which reveals that few SRs concluded on the same available data. To the best of our knowledge, this was the first review to analyze the magnitude of effect sizes of the outcomes. This allows the best available evidence on injury prevention and aids readers in comprehending the associations magnitude and interpretating their practical significance. Interpreting the effect size for each available risk factor can significantly contribute to improved decision-making by professionals working with runners.
The comprehensive review allows the reader to explore diverse factors associated with running injuries. Interestingly, BMI11,14 lacked a clear association, whereas heightened stature4,14 exhibited a positive correlation with elevated injury risks. Examining lifestyle aspects unveiled alcohol consumption,4 participation in other sports,4 and certain medical histories,4,22 including prior injuries, as contributory factors. Within the realm of running practices, increased race participation,12 marathon running,4 and initiation into running4,11,14 demonstrated heightened injury risks. Weekly running distance4,11,14 and volume11 revealed medium to large associations, stressing the need for tailored exercise regimens. Biomechanical aspects, particularly focusing on hip11,13,21,35 and pelvic21 stability, as well as specific foot patterns,11,13,17,20,21,36 emerged as significant in injury prevention. Finally, incorporating comprehensive functional movement screening,11,13 particularly paying attention to a drop squat and the ability to lift one leg while lying and keeping the knee straight (active straight leg raise), can potentially aid in identifying individuals at a higher risk of overall RRIs. While these findings offer valuable insights, the need for further research is evident to establish conclusive relationships and inform targeted training strategies for injury risk reduction.
Of note, the quality assessment conducted in this umbrella review revealed an unsatisfactory scenario, with 8 out of the 13 SRs characterized by critically low-quality ratings. Fig. 3 excludes the findings from the 8 SRs with critically low quality. The supplementary materials present all the information extracted from the SRs, including that which was classified as critically low quality.
Some limitations must be considered in relation to our umbrella review. Our inclusion criteria resulted in a limited number of SRs included to compose this study. However, to summarize the available evidence and reach conclusive results regarding the risk factors for RRIs, a comprehensive and consistent research approach regarding RRIs definition, outcome variables, participants, and study design was required.
5. Conclusion
This umbrella SR provides a comprehensive overview about the risk factors for RRIs. Drawing from the outcomes of the low-quality SRs and associations with large effect sizes, our findings indicate that running/training characteristics and health and lifestyle factors, as well as morphological and biomechanical aspects, are all implicated in elevating the risk of RRIs, emphasizing the multifactorial basis of injury incidence in running. The results of this umbrella review should be approached cautiously in clinical practice because none of the SRs included presented a rating of moderate or high confidence in quality.
Acknowledgments
Acknowledgments
This work was supported by the Programa de Bolsas Universitárias de Santa Catarina – Brasil (Uniedu) (Grant No. 14786 and Grant No. 16479) and the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES).
Authors’ contributions
CKC conceived and designed the study, carried out the data collection, analysis and interpretation, and participated in writing (original draft, review, and editing); JMM carried out the data collection, analysis and interpretation, and participated in writing (original draft, review, and editing); FHD, MPdC, and HdBF provided critical feedback, and participated in writing (review and editing); CR conceived and designed the study, provided critical feedback, and participated in writing (review and editing). All authors have read and approved the final version of the manuscript, and agree with the order of presentation of the authors.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Peer review under responsibility of Shanghai University of Sport.
Supplementary materials associated with this article can be found in the online version at doi:10.1016/j.jshs.2024.04.011.
Supplementary materials
References
- 1.Lee DC, Pate RR, Lavie CJ, Sui X, Church TS, Blair SN. Leisure-time running reduces all-cause and cardiovascular mortality risk. J Am Coll Cardiol. 2014;64:472–481. doi: 10.1016/j.jacc.2014.04.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pedisic Z, Shrestha N, Kovalchik S, et al. Is running associated with a lower risk of all-cause, cardiovascular and cancer mortality, and is the more the better? A systematic review and meta-analysis. Br J Sports Med. 2020;54:898–905. doi: 10.1136/bjsports-2018-100493. [DOI] [PubMed] [Google Scholar]
- 3.Kakouris N, Yener N, Fong DTP. A systematic review of running-related musculoskeletal injuries in runners. J Sport Health Sci. 2021;10:513–522. doi: 10.1016/j.jshs.2021.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Van Gent RN, Siem D, Van Middeloop M, Van Os AG, Bierma-Zeinstra SMA, Koes BW. Incidence and determinants of lower extremity running injuries in long distance runners: A systematic review. Br J Sports Med. 2007;41:469–480. doi: 10.1136/bjsm.2006.033548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Franke TPC, Backx FJG, Huisstede BMA. Running themselves into the ground? Incidence, prevalence, and impact of injury and illness in runners preparing for a half or full marathon. J Orthop Sports Phys Ther. 2019;49:518–528. doi: 10.2519/jospt.2019.8473. [DOI] [PubMed] [Google Scholar]
- 6.Kemler E, Blokland D, Backx F, Huisstede B. Differences in injury risk and characteristics of injuries between novice and experienced runners over a 4-year period. Phys Sportsmed. 2018;46:485–491. doi: 10.1080/00913847.2018.1507410. [DOI] [PubMed] [Google Scholar]
- 7.Buist I, Bredeweg SW, Van Mechelen W, Lemmink KAPM, Pepping GJ, Diercks RL. No effect of a graded training program on the number of running-related injuries in novice runners: A randomized controlled trial. Am J Sports Med. 2008;36:33–39. doi: 10.1177/0363546507307505. [DOI] [PubMed] [Google Scholar]
- 8.Hespanhol Jr LC, van Mechelen W, Postuma E, Verhagen E. Health and economic burden of running-related injuries in runners training for an event: A prospective cohort study. Scand J Med Sci Sports. 2016;26:1091–1099. doi: 10.1111/sms.12541. [DOI] [PubMed] [Google Scholar]
- 9.Hespanhol Junior LC, Huisstede BMA, Smits DW, et al. The NLstart2run study: Economic burden of running-related injuries in novice runners participating in a novice running program. J Sci Med Sport. 2016;19:800–804. doi: 10.1016/j.jsams.2015.12.004. [DOI] [PubMed] [Google Scholar]
- 10.Nielsen RO, Rønnow L, Rasmussen S, Lind M. A prospective study on time to recovery in 254 injured novice runners. PLoS One. 2014;9:e99877. doi: 10.1371/journal.pone.0099877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Van Poppel D, van der Worp M, Slabbekoorn A, et al. Risk factors for overuse injuries in short- and long-distance running: A systematic review. J Sport Health Sci. 2021;10:14–28. doi: 10.1016/j.jshs.2020.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Van der Worp MP, Ten Haaf DSM, Van Cingel R, de Wijer A, Nijhuis-van der Sanden MW, Bart Staal J. Injuries in runners; A systematic review on risk factors and sex differences. PLoS One. 2015;10 doi: 10.1371/journal.pone.0114937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Peterson B, Hawke F, Spink M, et al. Biomechanical and musculoskeletal measurements as risk factors for running-related injury in non-elite runners: A systematic review and meta-analysis of prospective studies. Sports Med Open. 2022;8:38. doi: 10.1186/s40798-022-00416-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Saragiotto BT, Yamato TP, Hespanhol Junior LC, Rainbow MJ, Davis IS, Lopes AD. What are the main risk factors for running-related injuries? Sports Med. 2014;44:1153–1163. doi: 10.1007/s40279-014-0194-6. [DOI] [PubMed] [Google Scholar]
- 15.Ceyssens L, Vanelderen R, Barton C, Malliaras P, Dingenen B. Biomechanical risk factors associated with running-related injuries: A systematic review. Sports Med. 2019;49:1095–1115. doi: 10.1007/s40279-019-01110-z. [DOI] [PubMed] [Google Scholar]
- 16.Mousavi SH, Hijmans JM, Rajabi R, Diercks R, Zwerver J, van der Worp H. Kinematic risk factors for lower limb tendinopathy in distance runners: A systematic review and meta-analysis. Gait Posture. 2019;69:13–24. doi: 10.1016/j.gaitpost.2019.01.011. [DOI] [PubMed] [Google Scholar]
- 17.Vannatta CN, Heinert BL, Kernozek TW. Biomechanical risk factors for running-related injury differ by sample population: A systematic review and meta-analysis. Clin Biomech. 2020;75 doi: 10.1016/j.clinbiomech.2020.104991. [DOI] [PubMed] [Google Scholar]
- 18.Sanfilippo D, Beaudart C, Gaillard A, Bornheim S, Bruyere O, Kaux JF. What are the main risk factors for lower extremity running-related injuries? A retrospective survey based on 3669 respondents. Orthop J Sports Med. 2021;9 doi: 10.1177/23259671211043444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anderson LM, Bonanno DR, Hart HF, Barton CJ. What are the benefits and risks associated with changing foot strike pattern during running? A systematic review and meta-analysis of injury, running economy, and biomechanics. Sports Med. 2020;50:885–917. doi: 10.1007/s40279-019-01238-y. [DOI] [PubMed] [Google Scholar]
- 20.Burke A, Dillon S, O'Connor S, Whyte EF, Gore S, Moran KA. Risk factors for injuries in runners: A systematic review of foot strike technique and its classification at impact. Orthop J Sports Med. 2021;9 doi: 10.1177/23259671211020283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Willwacher S, Kurz M, Robbin J, et al. Running-related biomechanical risk factors for overuse injuries in distance runners: A systematic review considering injury specificity and the potentials for future research. Sports Med. 2022;52:1863–1877. doi: 10.1007/s40279-022-01666-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ross BJ, Lupica GM, Dymock ZR, Miskimin C, Mulcahey MK. Sex-related differences in hip and groin injuries in adult runners: A systematic review. Phys Sportsmed. 2023;51:107–120. doi: 10.1080/00913847.2021.2016355. [DOI] [PubMed] [Google Scholar]
- 23.Aromataris E, Fernandez R, Godfrey CM, Holly C, Khalil H, Tungpunkom P. Summarizing systematic reviews: Methodological development, conduct and reporting of an umbrella review approach. Int J Evid Based Healthc. 2015;13:132–140. doi: 10.1097/XEB.0000000000000055. [DOI] [PubMed] [Google Scholar]
- 24.Fusar-Poli P, Radua J. Ten simple rules for conducting umbrella reviews. Evid Based Ment Health. 2018;21:95–100. doi: 10.1136/ebmental-2018-300014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5:210. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brunner R, Friesenbichler B, Casartelli NC, Bizzini M, Maffiuletti NA, Niedermann K. Effectiveness of multicomponent lower extremity injury prevention programmes in team-sport athletes: An umbrella review. Br J Sports Med. 2019;53:282–288. doi: 10.1136/bjsports-2017-098944. [DOI] [PubMed] [Google Scholar]
- 28.Olivier J, May WL, Bell ML. Relative effect sizes for measures of risk. Commun Stat Theory Methods. 2017;46:6774–6781. [Google Scholar]
- 29.Lunny C, Pieper D, Thabet P, Kanji S. Managing overlap of primary study results across systematic reviews: Practical considerations for authors of overviews of reviews. BMC Med Res Methodol. 2021;21:140. doi: 10.1186/s12874-021-01269-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pieper D, Antoine SL, Mathes T, Neugebauer EAM, Eikermann M. Systematic review finds overlapping reviews were not mentioned in every other overview. J Clin Epidemiol. 2014;67:368–375. doi: 10.1016/j.jclinepi.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 31.Shea BJ, Reeves BC, Wells G, et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomized or non-randomized studies of healthcare interventions, or both. BMJ. 2017;358:j4008. doi: 10.1136/bmj.j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gates A, Gates M, Duarte G, et al. Evaluation of the reliability, usability, and applicability of AMSTAR, AMSTAR 2, and ROBIS: Protocol for a descriptive analytic study. Syst Rev. 2018;7:85. doi: 10.1186/s13643-018-0746-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Harrison SL, Buckley BJR, Rivera-Caravaca JM, Zhang J, Lip GYH. Cardiovascular risk factors, cardiovascular disease, and COVID-19: An umbrella review of systematic reviews. Eur Heart J Qual Care Clin Outcomes. 2021;7:330–339. doi: 10.1093/ehjqcco/qcab029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Neal BS, Barton CJ, Gallie R, O'Halloran P, Morrissey D. Runners with patellofemoral pain have altered biomechanics which targeted interventions can modify: A systematic review and meta-analysis. Gait Posture. 2016;45:69–82. doi: 10.1016/j.gaitpost.2015.11.018. [DOI] [PubMed] [Google Scholar]
- 35.Louw M, Deary C. The biomechanical variables involved in the aetiology of iliotibial band syndrome in distance runners—A systematic review of the literature. Phys Ther Sport. 2014;15:64–75. doi: 10.1016/j.ptsp.2013.07.002. [DOI] [PubMed] [Google Scholar]
- 36.Mann R, Malisoux L, Urhausen A, Meijer K, Theisen D. Plantar pressure measurements and running-related injury: A systematic review of methods and possible associations. Gait Posture. 2016;47:1–9. doi: 10.1016/j.gaitpost.2016.03.016. [DOI] [PubMed] [Google Scholar]
- 37.Schiavo JH. PROSPERO: An international register of systematic review protocols. Med Ref Serv Q. 2019;38:171–180. doi: 10.1080/02763869.2019.1588072. [DOI] [PubMed] [Google Scholar]
- 38.Yamato TP, Saragiotto BT, Lopes AD. A consensus definition of running-related injury in recreational runners: A modified Delphi approach. J Orthop Sports Phys Ther. 2015;45:375–380. doi: 10.2519/jospt.2015.5741. [DOI] [PubMed] [Google Scholar]
- 39.Mann B, Wood E. Confounding in observational studies explained. Open Epidemiol J. 2012;5:18–20. [Google Scholar]
- 40.van Tulder M, Furlan A, Bombardier C, Bouter L, Editorial Board of the Cochrane Collaboration Back Review Group Updated method guidelines for systematic reviews in the Cochrane collaboration back review group. Spine. 2003;28:1290–1299. doi: 10.1097/01.BRS.0000065484.95996.AF. [DOI] [PubMed] [Google Scholar]
- 41.Reid SA, Rivett DA. Manual therapy treatment of cervicogenic dizziness: A systematic review. Man Ther. 2005;10:4–13. doi: 10.1016/j.math.2004.03.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.