Abstract
Background
The Albumin-Bilirubin (ALBI) score, recommended for assessing the prognosis of hepatocellular carcinoma patients, has garnered attention. The efficacy of ALBI score in forecasting the risk of death in sepsis patients remains limited. We designed two cohort studies to assess the association between ALBI score and in-hospital mortality in patients with sepsis.
Methods
A retrospective analysis was conducted utilizing data from the Second Affiliated Hospital of Guangzhou Medical University and the Medical Information Mart for Intensive Care IV(MIMIC-IV). Patients diagnosed with sepsis were included in the analysis. The primary outcome was the in-hospital mortality. Multivariate Cox regression analysis was conducted to assess the independent association between the ALBI score and mortality, with adjustment for potential confounders. Subgroup analysis was conducted to assess the robustness of the findings.
Results
The Guangzhou Sepsis Cohort (GZSC) of the Second Affiliated Hospital of Guangzhou Medical University comprised 2969 participants, while the MIMIC-IV database included 8841 participants. The ALBI score were categorized into < -2.60, −2.60∼-1.39, and >-1.39. After adjusting for confounders, a linear relationship was observed between ALBI score and mortality. Patients with a high ALBI grade were associated with higher in-hospital mortality in both the GZSC (HR: 1.52, 95%CI: 1.24–1.87, p < 0.001) and the MIMIC-IV database (HR: 1.57, 95%CI: 1.46–1.70, p < 0.001).
Conclusions
A high ALBI score is associated with higher in-hospital mortality among sepsis patients in ICU.
Keywords: epsis, Albumin, Bilirubin, In-hospital mortality, Albumin-bilirubin
Highlights
-
•
The Albumin-Bilirubin score has garnered attention recently.
-
•
We designed two large cohort studies to assess the association between Albumin-Bilirubin score and in-hospital mortality in sepsis patients.
-
•
A high Albumin-Bilirubin score is associated with higher in-hospital mortality in ICU patients with sepsis.
1. Introduction
Sepsis, a critical condition in intensive care units (ICUs), arises from an infection that leads to an overactive immune reaction and can lead to the failure of multiple organs [1,2]. It is a widespread and perilous health issue, impacting more than 30 million individuals globally each year and causing nearly 6 million fatalities [3]. Despite medical progress, the survival rate for sepsis remains poor [4,5]. Early identification of patients at high risk and with unfavorable outcomes is essential for providing prompt and suitable medical care [6].
During sepsis, the liver has essential roles, including immune defense and metabolic adaptation to inflammation, as well as nutrient metabolism [7]. Liver failure in sepsis is a significant complication that exacerbates the condition's severity and is associated with poor outcomes [8,9]. It is valuable to access liver function in sepsis patients.
The Albumin-Bilirubin (ALBI) score was recommended to evaluate prognosis of hepatocellular carcinoma patients by Johnson et al. [10]. The ALBI score is a simple index used to evaluate liver function because of including only serum albumin and bilirubin levels. It is also applied to predict the mortality of patients with liver injury [[11], [12], [13]]. However, the efficacy of ALBI score in forecasting the risk of death in critically ill sepsis patients remains to be determined. This study is aimed to investigate the association between ALBI score and in-hospital mortality in patients with sepsis.
2. Methods
2.1. Data sources and setting
A real-world cohort study was initiated, leveraging data from two distinct sources: the Medical Information database of the Intensive Care Unit (ICU) at Guangzhou Medical University's Second Affiliated Hospital, and the Medical Information Mart for Intensive Care (MIMIC-IV). The Guangzhou database encompasses a wealth of information on ICU patients treated from 2017 to 2021 [14]. Guangzhou Medical University's Second Affiliated Hospital functions as a tertiary teaching hospital. This database contains patients with various infection, injury, cancer, etc. Through screening of clinical data by the SOFA score greater than 2 points as a result of a pathological host reaction to infection, We only include sepsis patient's database named GZSC(Guangzhou Sepsis Cohort). The MIMIC-IV database, to which we have secured access, is an extensive repository of more than 70000 clinical individuals in ICU patients from the Beth Israel Deaconess Medical Center, spanning the years 2008–2019 [15,16]. A certificate number 1154503 has been issued to Erya Gou for the utilization of the MIMIC database.
2.2. Study population
Eligibility for inclusion in our study was extended to all individuals from both the Guangzhou Sepsis Cohort (GZSC) and the MIMIC-IV database. We focused on adult patients, aged 18 years and older, who met the sepsis-3 diagnosis criteria. This diagnosis was based on the Sequential Organ Failure Assessment (SOFA) score greater than 2 points as a result of a pathological host reaction to infection [1]. The exclusion criteria is (1) Individuals with ICU stays shorter than 24 h; (2) Lacking data of bilirubin or albumin levels.
2.3. Exposure
The ALBI score was calculated using the following equation: ALBI = [log10bilirubin (μmol/L) × 0.66 − 0.085 × albumin (g/L)] [10]. Patients with sepsis were categorized into three groups based on their ALBI scores: < −2.60, −2.60 to −1.39, and > −1.39 [17].
2.4. Covariates
Data from the database were comprehensively extracted for this study, encompassing a range of demographic details such as age and gender. Additionally, laboratory results from tests performed within the first 24 h following ICU admission were included, like white blood cell counts and serum creatinine levels. The study also accounted for various clinical interventions initiated on the initial ICU day, such as mechanical ventilation and continuous renal replacement therapy (CRRT). Furthermore, the Sequential Organ Failure Assessment (SOFA) scores were documented to assess organ dysfunction.
3. Outcomes
3.1. The primary outcome was in-hospital mortality
3.1.1. Statistical analysis
Continuous variables exhibiting normal distribution were reported as the mean accompanied by the standard deviation (SD). Conversely, those with a skewed distribution were depicted through the median along with the interquartile range (IQR). Categorical data were represented in terms of frequencies and their respective percentages. To ascertain the normalcy of continuous variables, either the Student's t-test or the Wilcoxon rank-sum test was employed, depending on the distribution. For the analysis of categorical variables, the Pearson's chi-squared test was the primary method, with Fisher's exact test used when appropriate.
Curve fitting techniques were employed to explore the correlation between the ALBI score and the likelihood of in-hospital mortality. The relationship was further assessed using multivariable Cox regression models, which were utilized to determine the ALBI score's independent effect on mortality and to compute the corresponding hazard ratios (HR) along with their 95 % confidence intervals (CI). Kaplan–Meier methodology was applied to create survival curves, which were subsequently analyzed using the log-rank test to identify significant differences. To address potential survival bias, subgroup analyses were conducted, categorizing the data based on pertinent covariates.
All analyses were conducted using R version 4.2.2, available from The R Foundation (http://www.R-project.org), and Free Statistics software, version 1.9 (Beijing, China, http://www.clinicalscientists.cn/freestatistics). A two-tailed p-value threshold of <0.05 was applied to determine statistical significance [18].
3.2. Sensitivity analysis
Receiver operator characteristic (ROC) curve was used to evaluate the predictive value. Gender, age(categorized as 65 years) and sepsis-associated liver injury (SALI) were included in the subgroup analysis. SALI was defined by total bilirubin (TBIL) > 2 mg/dL and the occurrence of an international normalized ratio (INR) > 1.5 in the presence of sepsis [7,19].
4. Results
4.1. Population and baseline characteristics
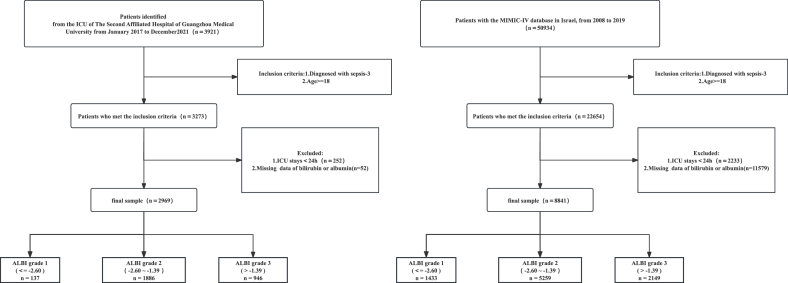
Following the application of inclusion and exclusion criteria, our study enrolled a total of 2969 patients from the Guangzhou Sepsis Cohort (GZSC) and 8841 patients from the MIMIC-IV database, as illustrated in Fig. 1. The detailed baseline characteristics of these patients are presented in Table 1. Patients with higher ALBI grades, as opposed to those with grade 1, were typically older, predominantly male, and exhibited elevated Mean Arterial Pressure (MAP), Blood Urea Nitrogen (BUN), bilirubin levels, and SOFA scores. Additionally, there was a higher incidence of vasoactive medication use and continuous renal replacement therapy (CRRT) among the higher-grade patients, contrasted with lower serum total calcium and albumin levels. Discrepancies in other characteristics between the two databases were observed, including variations in respiratory rate, white blood cell count, and length of ICU stay.
Fig. 1.
The flow chart of the study.
Table 1.
Baseline characteristics of the study participants.
| Variables | GZSC |
MIMIC-IV |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total (n = 2969) | ALBI ≤ −2.60 (n = 137) | −2.60 <ALBI ≤ −1.39 (n = 1886) | ALBI > -1.39 (n = 946) | P value | Total (n = 8841) | ALBI ≤ −2.60 (n = 1433) | −2.60 <ALBI ≤ −1.39 (n = 5259) | ALBI > -1.39 (n = 2149) | P value | |
| Demographics | ||||||||||
| Sex, n (%) | 0.455 | 0.071 | ||||||||
| Male | 1884 (63.5) | 93 (67.9) | 1200 (63.6) | 591 (62.5) | 5053 (57.2) | 855 (59.7) | 2962 (56.3) | 1236 (57.5) | ||
| Female | 1085 (36.5) | 44 (32.1) | 686 (36.4) | 355 (37.5) | 3788 (42.8) | 578 (40.3) | 2297 (43.7) | 913 (42.5) | ||
| Age (years) | 66.6 ± 16.7 | 60.8 ± 17.9 | 66.8 ± 17.0 | 67.0 ± 15.9 | <0.001 | 63.4 ± 16.8 | 61.6 ± 17.6 | 64.8 ± 16.7 | 60.9 ± 16.0 | <0.001 |
| Vital signs | ||||||||||
| MAP(mmHg) | 88.1 ± 27.0 | 102.0 ± 24.2 | 90.3 ± 28.1 | 81.6 ± 23.5 | <0.001 | 77.0 ± 10.8 | 81.1 ± 11.3 | 77.1 ± 10.8 | 74.0 ± 9.6 | <0.001 |
| Heart rate(bpm) | 102.1 ± 27.4 | 103.3 ± 27.4 | 99.9 ± 28.0 | 106.3 ± 25.7 | <0.001 | 89.3 ± 17.4 | 85.0 ± 16.0 | 88.6 ± 17.3 | 93.6 ± 17.7 | <0.001 |
| Respiratory rate(bpm) | 23.1 ± 8.1 | 23.8 ± 8.2 | 23.1 ± 8.4 | 23.0 ± 7.6 | 0.723 | 20.3 ± 4.3 | 19.5 ± 3.7 | 20.5 ± 4.2 | 20.6 ± 4.7 | <0.001 |
| Temperature(°C) | 36.9 ± 0.9 | 37.0 ± 0.9 | 36.9 ± 0.9 | 36.8 ± 1.0 | 0.063 | 36.9 ± 0.7 | 37.0 ± 0.6 | 36.9 ± 0.7 | 36.8 ± 0.7 | <0.001 |
| SPO2(%) | 92.7 ± 50.6 | 97.6 ± 35.9 | 90.2 ± 52.1 | 96.9 ± 50.6 | 0.605 | 96.8 ± 2.3 | 97.2 ± 1.9 | 96.8 ± 2.2 | 96.7 ± 2.7 | <0.001 |
| Laboratory findings | ||||||||||
| White blood cell( × 109) | 11.7 (7.5, 17.1) | 12.0 (8.7, 16.2) | 11.7 (7.8, 17.0) | 11.5 (6.3, 17.7) | 0.433 | 14.1 (9.6, 19.8) | 13.7 (10.2, 18.1) | 13.8 (9.5, 19.5) | 14.9 (9.6, 21.7) | <0.001 |
| Creatinine (mg/dL) | 1.3(0.9, 2.6) | 1.1 (0.8, 2.3) | 1.3 (0.9, 2.8) | 1.3 (0.9, 2.5) | 0.175 | 1.3 (0.9, 2.2) | 1.2 (0.9, 1.8) | 1.3 (0.9, 2.2) | 1.4 (0.9, 2.4) | <0.001 |
| BUN (mg/dL) | 25.7 (16.3,46.6) | 19.7(13.4,36.6) | 25.4(16.3,46.3) | 27.7(17.1,48.3) | <0.001 | 27.0 (17.0, 45.0) | 22.0 (15.0, 34.0) | 28.0 (17.0, 46.0) | 30.0 (18.0, 50.0) | <0.001 |
| Potassium (mmol/L) | 3.9 ± 1.6 | 4.0 ± 0.9 | 3.9 ± 1.4 | 3.9 ± 2.0 | 0.882 | 4.7 ± 1.0 | 4.8 ± 1.1 | 4.7 ± 1.0 | 4.7 ± 0.9 | <0.001 |
| Sodium (mmol/L) | 139.2 ± 8.8 | 140.4 ± 7.3 | 139.5 ± 8.7 | 138.4 ± 9.1 | 0.002 | 140.2 ± 6.0 | 141.3 ± 5.4 | 140.4 ± 6.0 | 138.9 ± 6.1 | <0.001 |
| Chlorine (mmol/L) | 104.4 ± 9.3 | 102.7 ± 9.5 | 103.9 ± 9.2 | 105.5 ± 9.4 | <0.001 | 106.3 ± 7.2 | 106.3 ± 6.7 | 106.3 ± 7.2 | 106.3 ± 7.6 | 0.997 |
| Calcium (mmol/L) | 2.0 ± 0.2 | 2.2 ± 0.2 | 2.1 ± 0.2 | 1.9 ± 0.2 | <0.001 | 2.1 ± 0.2 | 2.3 ± 0.2 | 2.1 ± 0.2 | 2.0 ± 0.3 | <0.001 |
| Bilirubin,mg/dl | 0.5 (0.3, 1.0) | 0.4 (0.3, 0.8) | 0.5(0.3, 1.0) | 0.6(0.4, 1.0) | <0.001 | 0.8 (0.5, 2.0) | 0.5 (0.3, 0.7) | 0.7 (0.4, 1.4) | 2.6 (1.1, 6.3) | <0.001 |
| Albumin,g/dl | 28.5 ± 6.5 | 40.7 ± 2.9 | 31.1 ± 3.9 | 21.7 ± 4.3 | <0.001 | 3.2 ± 0.7 | 4.2 ± 0.4 | 3.2 ± 0.4 | 2.4 ± 0.4 | <0.001 |
| Scoring system | ||||||||||
| SOFA score | 9.0 (7.0, 12.0) | 9.0 (7.0, 10.0) | 9.0 (7.0, 11.0) | 10.0 (8.0, 13.0) | <0.001 | 3.0 (2.0, 5.0) | 3.0 (2.0, 4.0) | 3.0 (2.0, 5.0) | 4.0 (3.0, 6.0) | <0.001 |
| In-hospital management | ||||||||||
| CRRT | 550 (18.5) | 22 (16.1) | 334 (17.7) | 194 (20.5) | 0.146 | 609 (7.2) | 75 (5.5) | 327 (6.5) | 207 (10.2) | <0.001 |
| Mechanical ventilation | 2016 (67.9) | 87 (63.5) | 1239 (65.7) | 690 (72.9) | <0.001 | 4904 (58.4) | 814 (59.9) | 2832 (56.5) | 1258 (61.9) | <0.001 |
MAP, mean arterial pressure; BUN, blood urea nitrogen; CRRT, continuous renal replacement therapy.
4.2. Primary outcome
The mortality rates of patients within the cohort were 22.1 % (657/2969) in GZSC and 20.5 % (1725/8841) in MIMIC-IV, respectively. Meanwhile, in the GZSC database, the mortality rates of patients in ALBI group 1, 2 and 3 were 17.5 % (24/2969), 19.5 % (367/2969), 28.1 % (266/2969), respectively(Table 2).
Table 2.
Primary outcome of total patients.
| Variables | GZSC |
MIMIC-IV |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total (n = 2969) | ALBI ≤ −2.60 (n = 137) | −2.60 <ALBI ≤ −1.39 (n = 1886) | ALBI > -1.39 (n = 946) | P value | Total (n = 8841) | ALBI ≤ −2.60 (n = 1433) | −2.60 <ALBI ≤ −1.39 (n = 5259) | ALBI > -1.39 (n = 2149) | P value | |
| Los ICU (days) | 14.4 (8.0, 25.0) | 15.6 (8.5, 27.8) | 15.0 (8.2, 25.8) | 13.5 (7.1, 22.2) | <0.001 | 6.1 ± 6.8 | 6.2 ± 7.3 | 5.9 ± 6.6 | 6.4 ± 7.0 | 0.004 |
| In-hospital mortality,n,% | 657 (22.1) | 24 (17.5) | 367 (19.5) | 266 (28.1) | <0.001 | 1725 (20.5) | 195 (14.4) | 925 (18.4) | 605 (29.8) | <0.001 |
4.3. Relationship between ALBI and in-hospital mortality in patients with sepsis in ICU
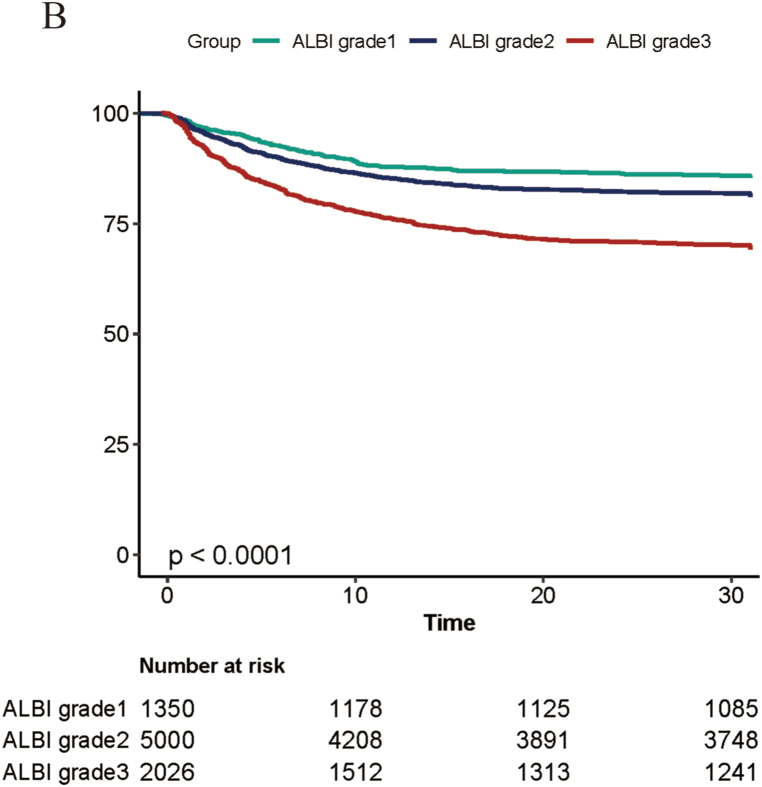
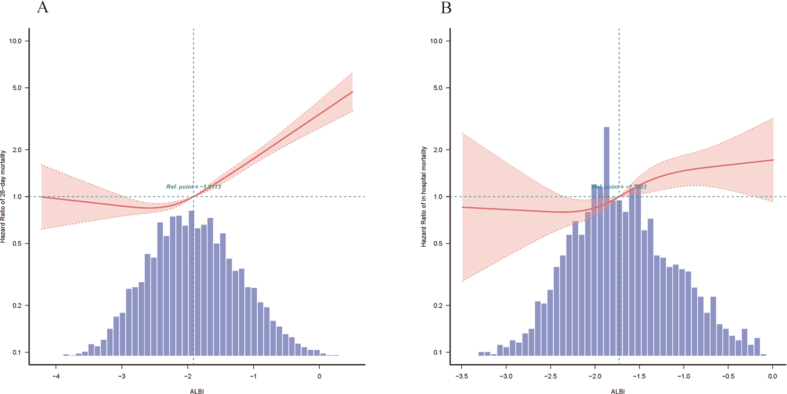
The curve fitting analysis showed a linear trend between the ALBI score and in-hospital mortality both two databases(eFig. 1A and B). The Kaplan-Meier curve showed a higher mortality rate in patients of grade 3 (ALBI -2.60∼ −1.39) (p < 0.0001, in GZSC (Fig. 2A)) (p < 0.0001, in MIMIC-IV (Fig. 2B)).
Fig. 2A.
K-M analysis of in patients with sepsis of GZSC.
Fig. 2B.
K-M analysis of in patients with sepsis of MIMIC-IV.
The results of multivariate COX regression model are shown in Table 3. In the adjusted model, each point increase in ALBI was associated with a 52 % or 57 % increase in mortality risk(GZSC: HR:1.52,95%CI:1.24–1.87, p < 0.001 vs. MIMIC-IV: HR:1.57, 95%CI:1.46–1.70, p < 0.001). Patients with high ALBI level had a significantly higher risk of in-hospital mortality (HR: 2.00, 95 % CI:1.08–3.71, p = 0.027), compared to those with low ALBI levels. Similar results were also found in MIMIC IV database(HR: 2.00, 95%CI:1.68–2.39, p < 0.001).
Table 3.
Association between ALBI score and in-hospital motality in multiple regression model.
| GZSC |
MIMIC-IV |
|||||||
|---|---|---|---|---|---|---|---|---|
| Crude Model |
Adjusted Model |
Crude Model |
Adjusted Model |
|||||
| HR (95 % CI) | P value | HR (95 % CI) | P value | HR (95 % CI) | P value | HR (95 % CI) | P value | |
| Continuous variable | ||||||||
| ALBI | 1.42 (1.26–1.60) | <0.001 | 1.52 (1.24–1.87) | <0.001 | 1.63 (1.52–1.74) | <0.001 | 1.57 (1.46–1.70) | <0.001 |
| Categorical variables | ||||||||
| ALBI ≤ −2.60 | Ref | Ref | Ref | Ref | ||||
| −2.60 <ALBI ≤ −1.39 | 1.11 (0.77–1.58) | 0.581 | 1.25 (0.7–2.22) | 0.457 | 1.32 (1.13–1.54) | <0.001 | 1.16 (0.98–1.36) | 0.080 |
| ALBI > -1.39 | 1.81 (1.26–2.6) | 0.001 | 2.00 (1.08–3.71) | 0.027 | 2.32 (1.98–2.73) | <0.001 | 2.00 (1.68–2.39) | <0.001 |
| Trend for test | <0.001 | <0.001 | <0.001 | <0.001 | ||||
Adjusted Model: adjusted for Age, Gender, Heart rate, Respiratory rate, SPO2, Temperature,WBC, Potassium, Sodium, Chlorine, Calcium, Creatinine, BUN, CRRT, Mechanical ventilation.
4.4. Sensitivity analysis
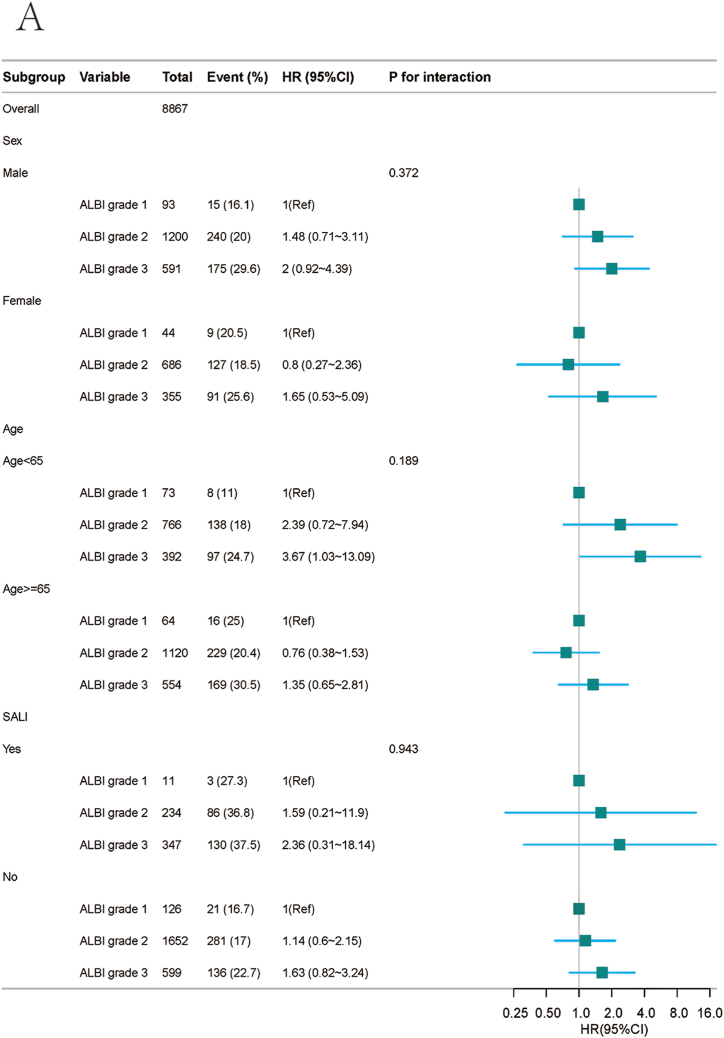
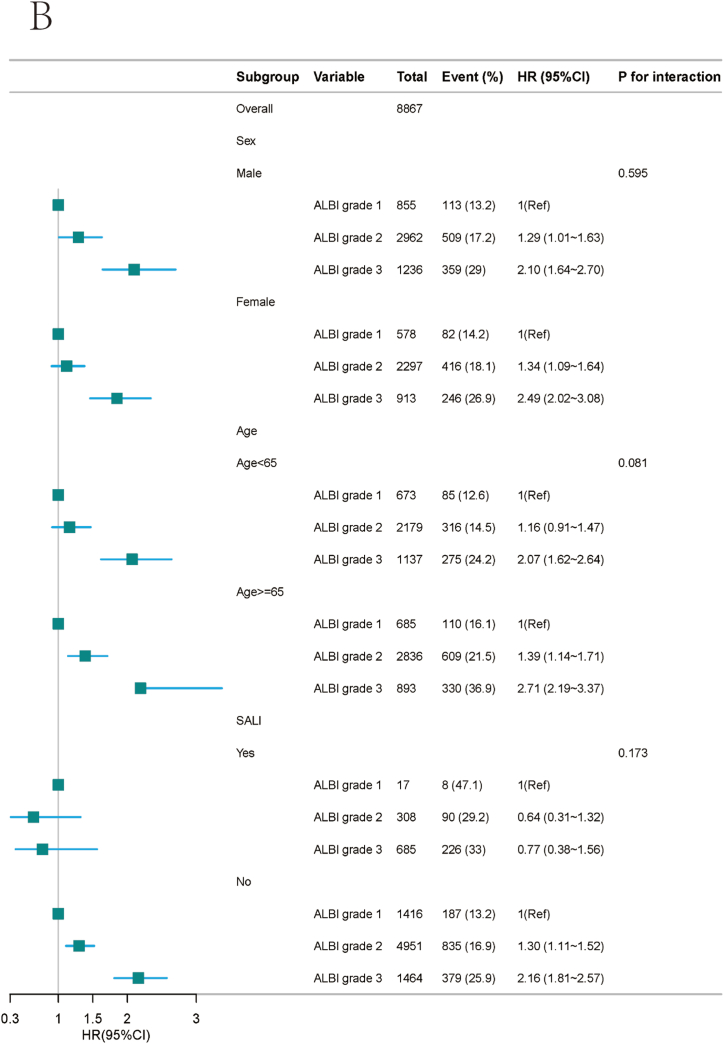
The area under the curves for ALBI was 0.570 in the GZSC database and 0.598 in the MIMIC-IV database (eFig. 2A, Fig. 2BA and B). Meanwhile we incorporated the SOFA score for comparative analysis. Subgroup analysis showed that patients with high ALBI had a significantly higher risk of in-hospital mortality in GZSC and MIMIC-IV, compared to low ALBI, except patients with SAIL(Fig. 3A, Fig. 3BA and B). In patients with SAIL, the risk of in-hospital mortality is not statistically significant regardless of the ALBI score's height.
Fig. 3A.
Stratified analyses of the association between ALBI grade and in-hospital mortality status according to sex, age and SAIL in GZSC.
Fig. 3B.
Stratified analyses of the association between ALBI grade and in-hospital mortality status according to sex, age and SAIL in MIMIC-IV.
5. Discussion
In this cohort study, we reported that the ALBI grade was a predictor of patients with sepsis. Our findings revealed that among high ALBI grade was associated with higher in-hospital mortality in both the GZSC(HR:1.52,95%CI:1.24–1.87, p < 0.001) and the MIMIC-IV database(HR:1.57, 95%CI:1.46–1.70, p < 0.001). The results remained stable in subgroup analysis.
The ALBI score, which includes serum bilirubin and albumin levels, was developed as a new model to assess liver function and predict the survival of patients with liver disease [10]. The ALBI score originated for HCC patients to estimate the extent of liver dysfunction. Meanwhile, it has also been widely used in patients without HCC [[20], [21], [22]]. A meta-analysis indicates a strong association between elevated preoperative ALBI scores and the risk of postoperative liver failure and mortality following hepatectomy [13]. In our study, we use ALBI score to assess liver function and prognosis of patients with sepsis. We found that a high ALBI grade was associated with higher in-hospital mortality in these patients.
Besides its application in predicting liver diseases [[11], [12], [13]], the ALBI score has been used to predict survival in patients with heart failure [23,24]. Su Han et al.(n = 9749) conducted the in-hospital mortality rate for heart failure patients(HF) escalated by 8.2 % per 0.1-point rise in the ALBI score (OR 1.082; 95 % CI:1.052–1.114; p < 0.001) [24]. Similaly, Luo et al.(n = 3381) reached the same conclusions in HF patients. Compared with the low ALBI group, the odds ratio (OR) for the short-term all-cause mortality of high group was 2.41 (95 % CI: 1.85–3.15, P < 0.001) [23]. In our study, we extented the use of ALBI in patients with sepsis. It was found that it could evaluate the prognosis of patients with sepsis.
Liver failure is a common complications of sepsis [7]. Therefore, we included SALI as a variable in subgroup analyses. In patients with SAIL, risk of in-hospital mortality is not statistically significant no matter ALBI score height. The reason maybe the sample size of SALI in the ALBI grade 1, the reference group was small(n = 11 and n = 17). Rendering the results in this part were biased(Fig. 3A, Fig. 3BA and B).
Interestingly, the relationship between ALBI and mortality was also observed in non-SALI patients(HR: 2.16; 95 % CI:1.81–2.57; Fig. 3A, Fig. 3BB). This means that in patients without sepsis-related liver injury, a higher ALBI score is associated with an increased risk of death. The specific mechanisms need further exploration.
Our study suggests that early assessment of the ALBI score can identify patients with a high risk of death, even patients without SAIL. Further research is needed to determine whether early liver-protective therapy in patients with high sepsis severity scores can improve their prognosis.
This study also has some limitations. Firstly, all laboratory data represent initial values at ICU admission. Causal relationship between ALBI and in-hospital mortality is unknown. Marginal structural models, a new class of causal models that allowed for improved adjustment of confounding affected by previous treatment [25]. We plan to research this relationship in the context of causal inference used marginal structural models in the future. Secondly, the baseline characteristics varied significantly across the three database groups. To address these disparities, we utilized a multivariable Cox proportional hazards regression model, enhancing the reliability of our results. While we acknowledge that some estimation bias may remain, our methodological approach aims to minimize its impact. Finally, bilirubin and albumin levels, recorded within the first 24 h of ICU admission, were available for only about 50 % of the patients in the MIMIC-IV database. However, the results of GZSC is similar to those of the MIMIC IV database. In conclusion, despite these limitations, our study provides valuable evidence on the association between ALBI and in-hospital mortality in sepsis patients. The large sample size, long follow-up period, and adjustment for confounding factors contribute to the strength of our findings. Further research is warranted to confirm and expand upon our results.
6. Conclusion
A high ALBI score is associated with higher in-hospital mortality among sepsis patients in ICU. These findings have significant implications for risk stratification and management of sepsis patients.
Ethics approval and consent to participate
The Clinical Research and Applied Ethics Committee of the Second Affiliated Hospital of Guangzhou Medical University approved the ethical review of this study(2023-hg-ks-22). The MIMIC-IV database has already received approval from the institutional review boards at Beth Israel Deaconess Medical Center and the Massachusetts Institute of Technology. Our research adhered to local legislation and institutional guidelines. Furthermore, the need for written informed consent was waived by the same ethics committee, given that the database does not contain protected health information.
Consent for publication
All authors have reviewed and approved the manuscript for publication.
Availability of data and materials
Datasets can be obtained by contacting the corresponding author upon a reasonable request.
Funding
This research was supported by The National Natural Science Foundation of China(82202371) and The Second Affiliated Hospital of Guangzhou Medical University New Technology Clinical Research Project(2022-LCYJ-YY-03).
CRediT authorship contribution statement
Erya Gou: Writing – review & editing, Writing – original draft, Methodology, Formal analysis, Data curation, Conceptualization. Qilin Yang: Writing – review & editing, Writing – original draft, Validation, Supervision, Software, Resources, Data curation. Jieru Chen: Methodology, Investigation, Formal analysis. Tianyu Kong: Supervision, Software, Investigation. Zhiwei Tang: Visualization, Validation, Software, Data curation. Qirui Wen: Formal analysis, Data curation, Conceptualization. Wenxing Huang: Project administration, Methodology, Investigation. Guangqian Yang: Investigation, Data curation. Wenling Li: Formal analysis, Data curation. Deliang Wen: Supervision, Software, Resources, Investigation. Zhenhui Zhang: Writing – review & editing, Writing – original draft, Supervision, Conceptualization.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
Not applicable.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2024.e34697.
Contributor Information
Erya Gou, Email: gouerya623@163.com.
Qilin Yang, Email: yangqilin@gzhmu.edu.cn.
Jieru Chen, Email: chenjieru77@163.com.
Tianyu Kong, Email: ktyfancy@126.com.
Zhiwei Tang, Email: tzwicu@126.com.
Qirui Wen, Email: wen.qirui@163.com.
Wenxing Huang, Email: huangwenxingicu@163.com.
Guangqian Yang, Email: 2009682038@gzhmu.edu.cn.
Wenling Li, Email: 18130906778@163.com.
Deliang Wen, Email: deliangw@163.com.
Zhenhui Zhang, Email: zhzhhicu@126.com.
Abbreviations
- ALBI:
Albumin-Bilirubin
- MIMIC-IV:
Medical Information Mart for Intensive Care-IV
- GZSC:
Guangzhou Sepsis Cohort
- ICU:
Iintensive Care Unit
- SOFA score:
sequential organ failure assessment score
- CRRT:
continuous renal replacement therapy
- SD:
standard deviation
- IQR:
interquartile range
- HR:
hazard ratios
- CI:
confidence intervals
- ROC:
Receiver operator characteristic
- MAP:
mean arterial pressure
- WBC:
white blood cell
- PaO2:
partial pressure of oxygen in arterial blood
- BUN:
blood urea nitrogen
- Los ICU days:
days of ICU stay
- SALI:
sepsis-associated liver injury
Appendix A. Supplementary data
The following are the Supplementary data to this article:
figs1.
figs2.
References
- 1.Singer M., et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3) JAMA. 2016;315:801–810. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zou R., et al. DNA-PKcs promotes sepsis-induced multiple organ failure by triggering mitochondrial dysfunction. J. Adv. Res. 2022;41:39–48. doi: 10.1016/j.jare.2022.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bauer M., et al. Mortality in sepsis and septic shock in Europe, North America and Australia between 2009 and 2019- results from a systematic review and meta-analysis. Crit. Care Lond. Engl. 2020;24:239. doi: 10.1186/s13054-020-02950-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Szilágyi B., Fejes Z., Pócsi M., Kappelmayer J., Nagy B. Role of sepsis modulated circulating microRNAs. EJIFCC. 2019;30:128–145. [PMC free article] [PubMed] [Google Scholar]
- 5.Yang L., Wang H., Shen Q., Feng L., Jin H. Long non-coding RNAs involved in autophagy regulation. Cell Death Dis. 2017;8:e3073. doi: 10.1038/cddis.2017.464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hird C. Early diagnosis and effective management of sepsis. Nurs. Stand. R. Coll. Nurs. G. B. 1987;35:59–66. doi: 10.7748/ns.2020.e11507. 2020. [DOI] [PubMed] [Google Scholar]
- 7.Ea W., M I., Rk W., L Ł. Liver dysfunction in sepsis. Adv. Clin. Exp. Med. Off. Organ Wroclaw Med. Univ. 2018;27 doi: 10.17219/acem/68363. [DOI] [PubMed] [Google Scholar]
- 8.Savio L.E.B., et al. CD39 limits P2X7 receptor inflammatory signaling and attenuates sepsis-induced liver injury. J. Hepatol. 2017;67:716–726. doi: 10.1016/j.jhep.2017.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sun J., et al. Gut-liver crosstalk in sepsis-induced liver injury. Crit. Care Lond. Engl. 2020;24:614. doi: 10.1186/s13054-020-03327-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Johnson P.J., et al. Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the ALBI grade. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2015;33:550–558. doi: 10.1200/JCO.2014.57.9151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mai R.-Y., et al. Combination of ALBI and APRI to predict post-hepatectomy liver failure after liver resection for HBV-related HCC patients. Cancer Manag. Res. 2019;11:8799–8806. doi: 10.2147/CMAR.S213432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fidan E., Fidan S., Merev E., Kazaz N. The Relationship between albumin-Bilirubin grade and survival in hepatocelluler carcinoma patients treated with sorefanib. Niger. J. Clin. Pract. 2022;25:173–177. doi: 10.4103/njcp.njcp_525_20. [DOI] [PubMed] [Google Scholar]
- 13.Pang Q., Zhou S., Liu S., Liu H., Lu Z. Prognostic role of preoperative albumin-bilirubin score in posthepatectomy liver failure and mortality: a systematic review and meta-analysis. Updat. Surg. 2022;74:821–831. doi: 10.1007/s13304-021-01080-w. [DOI] [PubMed] [Google Scholar]
- 14.Zhang Z., et al. Exploring disease axes as an alternative to distinct clusters for characterizing sepsis heterogeneity. Intensive Care Med. 2023;49:1349–1359. doi: 10.1007/s00134-023-07226-1. [DOI] [PubMed] [Google Scholar]
- 15.Yang Q., et al. Association between wait time of central venous pressure measurement and outcomes in critical patients with acute kidney injury: a retrospective cohort study. Front. Public Health. 2022;10 doi: 10.3389/fpubh.2022.893683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yang Q., et al. Association between the β-blocker use and patients with sepsis: a cohort study. Front. Med. 2023;10 doi: 10.3389/fmed.2023.1272871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marasco G., et al. Prognostic value of the albumin-bilirubin grade for the prediction of post-hepatectomy liver failure: a systematic review and meta-analysis. J. Clin. Med. 2021;10:2011. doi: 10.3390/jcm10092011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yang Q., et al. Relationship between driving pressure and mortality in ventilated patients with heart failure: a cohort study. Cancer Res. J. 2021;2021 doi: 10.1155/2021/5574963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pruinelli L., et al. Delay within the 3-hour surviving sepsis campaign guideline on mortality for patients with severe sepsis and septic shock. Crit. Care Med. 2018;46:500–505. doi: 10.1097/CCM.0000000000002949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fidan E., Yildirim A., Kazaz N., Fidan S., Cekic A.B. The relationship between albumin-bilirubin score and survival in patients operated for pancreatic cancer. JPMA J. Pak. Med. Assoc. 2022;72:1340–1344. doi: 10.47391/JPMA.2413. [DOI] [PubMed] [Google Scholar]
- 21.Duman Z.M., Timur B. Albumin-bilirubin score: a novel mortality predictor in valvular surgery. Braz. J. Cardiovasc. Surg. 2023;38:271–277. doi: 10.21470/1678-9741-2022-0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Takada K., et al. Assessment of the albumin-bilirubin grade as a prognostic factor in patients with non-small-cell lung cancer receiving anti-PD-1-based therapy. ESMO Open. 2022;7 doi: 10.1016/j.esmoop.2021.100348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Luo Y., Li Z., Liu J., Chong Y., Wu B. Prognostic value of the albumin-bilirubin score in critically ill patients with heart failure. Ann. Palliat. Med. 2021;10:12727–12741. doi: 10.21037/apm-21-3424. [DOI] [PubMed] [Google Scholar]
- 24.Han S., et al. Prognostic impact of albumin-bilirubin score on the prediction of in-hospital mortality in patients with heart failure: a retrospective cohort study. BMJ Open. 2022;12 doi: 10.1136/bmjopen-2021-049325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang Z., et al. Causal inference with marginal structural modeling for longitudinal data in laparoscopic surgery: a technical note. Laparosc. Endosc. Robot. Surg. 2022;5:146–152. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Datasets can be obtained by contacting the corresponding author upon a reasonable request.