Abstract
The measurement of Hemoglobin (Hb) by the non-invasive method is gaining popularity. The system, consisting of a photodiode is placed in between a Red (630 nm) and an IR (940 nm) LED, along with the signal conditioning circuits. 10 healthy male (8) and female (2) volunteers in the age group between 21 and 24 were recruited for this study. During measurement, the fingertip of a volunteer was placed on the measurement pad. Visible and IR lights are switched ON one after the other. The optical absorbance of the blood component in the arteries was detected by the photodiode using the reflectance method. The current generated was converted into voltage and was processed to remove the noise associated with the signal. From this, the concentration of Hb of the volunteers was determined. On the same day they were taken to the clinical laboratory and Hb values were obtained by the standard invasive method. Hemoglobin values obtained from the two methods were compared and an accuracy of 96.31 % and correlation coefficient value of 0.932405 was achieved. From the Bland -Altman plot, the results obtained are within the confidence interval of 95 %. The error of 3 % can be reduced further by employing sophisticated signal conditioning techniques. The proposed non-invasive method took only a few seconds to find the hemoglobin concentration than the invasive lab test. This method can accelerate the decision-making process in emergency situations.
Keywords: Photoplethysmography, Beer-Lambert law, Hemoglobin (Hb), Non-invasive
1. Introduction
Hemoglobin (Hb) is a protein molecule in red blood cells that carries 98.5 % of oxygen from the lungs to the body's tissues and returns carbon dioxide from the tissues back to the lungs [1]. Hb is a tetramer made of four subunits consisting of two alpha and two beta subunits. Each subunit has a central Heme group that contains iron responsible for its brighter red color and binds an oxygen molecule, which means each Hb molecule binds four oxygen molecules. Hence, the arterial blood, which contains oxygenated Hb, is pure red, and the venous blood, which consists of the deoxygenated Hb, is dark red in colour. The second and third oxygen molecule easily bonds with Hb than the first and fourth oxygen molecule because of its shape-changing behavior.
Hemoglobin has the potential to carry oxygen and the amount of oxygen carried in blood can be measured by calculating the Hb concentration levels [2]. Furthermore, certain diseases and other natural causes may also affect Hb's ability to carry and deliver oxygen. The above condition also holds true for the CO2 levels, pH, and body temperature. The CO2 level in blood and pH have an inverse relationship. When CO2 that exits in blood, acts with water, it produces bicarbonate and hydrogen ions. The increase in CO2 level reduces the pH (to an acidic scale), which in turn reduces the affinity of hemoglobin for the oxygen. Therefore, oxygen detaches. Also, the body temperature will be slightly raised. When pH is high (to the basic scale), more oxygen is needed to attain the same level of hemoglobin saturation level and the body temperature will slightly reduce. Diseases like anemia and thalassemia reduce the oxygen delivery to tissues through hemoglobin. In particular, Thalassemia produces high red blood cells with low hemoglobin concentration resulting in reduced oxygen-carrying capacity. So, the determination of Hb concentration can also be used to analyze such physiological conditions. The normal Hb concentration for men is in the range of 13.5 g/dl to 17.5 g/dl. For women, it is in the range of 12.0 g/dl to 15.5 g/dl. For newborn babies, it ranges from 14 to 24 g/dl [3].
The hemoglobin levels can be determined by both invasive and non-invasive methods. The invasive method involves drawing blood sample from the patient's arm and processing it with chemical reagents to find the Hb concentration. It is the most commonly used method in hospitals across the globe and a painful procedure that requires trained staff and is not continuous [[4], [5], [6]]. The non-invasive method doesn't require a painful procedure; it makes use of photoplethysmography and Beer Lambert's law. One such method consists of placing the patient's finger over the light-emitting diode (LED) connected to an electronic circuit. The LED light is made to fall on the finger, part of the incident light gets absorbed and another part gets reflected to the photodiode (PD) in the circuit. The output from the PD is the measure of the concentration of the patient's blood in the finger. Upon eliminating the effect of skin, tissues, and bones, the concentration of blood can be found and used for the measurement of related parameters. The light sources used are Red and IR LED because the oxygenated hemoglobin absorbs more IR and then allows the red light to pass through. On the contrary, the deoxygenated Hemoglobin absorbs more red light and allows the IR light to pass through. Red light's wavelength ranges from 600 to 700 nm and the IR light's wavelength ranges from 850 to 1000 nm [[5], [6], [7]]. Hence, when measuring the Hb concentration using these light sources, the IR's reflectance signal will be greater than the red-light source's reflectance signal. Then, the detected signal from both the light sources will be used for further signal processing and, the filtered voltage signals were used to determine hemoglobin concentration.
2. The proposed methodology
The developed non-invasive system uses the principles of Photo-Plethysmograph (PPG) and Beer-Lambert Law to measure the concentration of hemoglobin. The designed system consists of two light-emitting diodes to obtain PPG signals from Red (630 nm) and IR (940 nm) LED sources [8]. Both LEDs are alternatively turned on for 30 s by the timer designed using IC NE555 connected to the LED driver circuit. This 555-timer IC is used in timing operations to produce accurate delays.
The entire system is shown in the form of a block diagram in Fig. 1. The photodiode placed in between the Red and IR LED receives the diffuse reflected light from the fingertip. The Trans-impedance amplifier (TL084) was used to convert the detected photocurrent into a voltage signal [9].
Fig. 1.
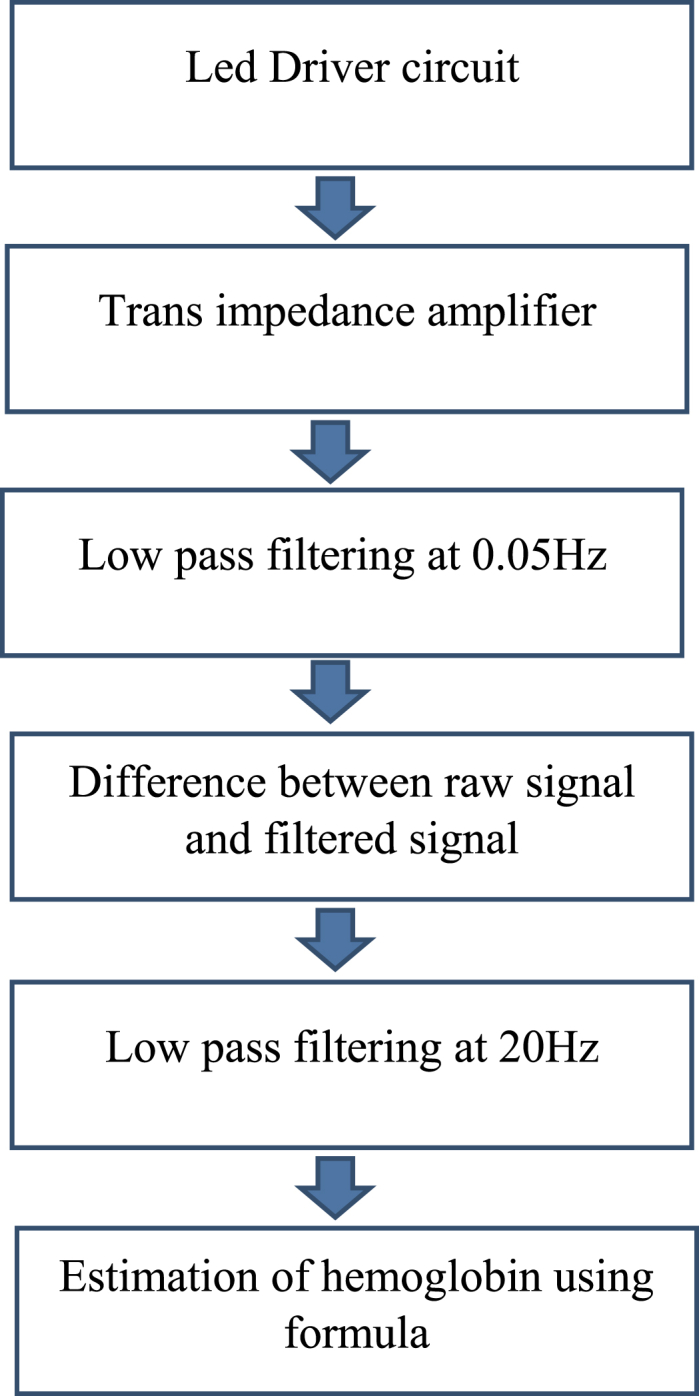
Block diagram.
The data from the Trans-impedance amplifier was collected and stored in storage devices through a digital oscilloscope as a ‘.CSV’ file. Then the data file was converted to a ‘.txt’ file for processing the signal. The voltage signal was filtered by the low-pass filter with a cutoff frequency of 0.05 Hz. Then the difference between the filtered signal and the unfiltered signal was obtained. This signal was further amplified and filtered by a low pass filter with a cutoff frequency of 20 Hz. This signal and used to calculate the Hemoglobin concentration by Beer-lambert's law, which depends upon the extinction coefficient and optical path length [10]. This was performed by the code developed in MATLAB software.
2.1. Calculation of Hb concentration
The determination of Hemoglobin concentration is based on the light absorbance and reflectance characteristics of the skin. The PPG signal from both LED sources has the optical absorbance characteristics of the blood components [11].
According to Beer-Lambert's law, the amount of absorbance of a substance is directly proportional to the product of path length traveled by light (Tf), the extinction coefficient values (∈x), and the concentration of the substance (Cx). The extinction coefficient is the measure of absorbance or reflectance of a substance and it varies for different wavelengths. These values can be calculated using molar concentration [12]. The amount of light absorbance of a substance can be expressed as in equation (1).
| (1) |
The equation of absorbance was obtained by the reflectance method for the signals obtained from red and IR sources as given by equation (2) and equation (3).
| (2) |
| (3) |
where ∈ red, ∈ir-Extinction coefficients for Red and IR.
Cred, Cir-concentration of Hb for Red and IR.
Tf-pathway length traveled by light expressed in equation (4).
| (4) |
d = geometric distance, n = refractive index.
The hemoglobin carries oxygen from the lungs to the tissues it becomes oxygenated hemoglobin (oxy-Hb) and when it releases the oxygen it becomes de-oxygenated hemoglobin (deoxy-Hb). The oxy-Hb absorbs more IR light than red light and this condition is reversed for deoxy-Hb where it absorbs more red light. Therefore, the amount of Red and IR absorbance can be expressed as in equations (5), (6).
| (5) |
| (6) |
The concentration of Hemoglobin in the blood (g/dl) can be expressed in an equation as the sum of oxyhemoglobin (Cℎbo) and deoxy-hemoglobin (Cℎb) concentrations [9] as in equation (7).
| (7) |
D-Density of blood, 1.05 g/dl.
The oxygen saturation levels are the ratio of the concentration of oxygenated Hemoglobin and the total Hemoglobin concentration in blood and are expressed as in equations (8), (9).
| (8) |
From the equations of (4) & (5), we get
| (9) |
The hemoglobin concentration cannot be determined directly from the measured SpO2 levels, because SpO2 values can change with variations in respiratory patterns [13] while the hemoglobin level remains unaltered. To minimize this effect, the standard SpO2 formula is used as given in equation (10). The resulting hemoglobin values depend only on the absorbance and extinction coefficients of the hemoglobin in the blood by substituting equation (8) in equation (9)
| (10) |
The concentration of deoxyhemoglobin was calculated by converting equation (8) as in equation (11)
| (11) |
Substituting equation (10) in equation (5) we get equation (12).
| (12) |
Comparing equations (7), (9), (11) we get equation (13)
| (13) |
Equation (13) is used to determine the concentration of hemoglobin from the coefficient values obtained with respect to the wavelength of the light spectrum. To analyze the accuracy of the proposed device, the obtained results were compared with the results of hemoglobin concentration determined by the invasive method.
2.2. Data acquisition
To acquire the signal, a volunteer is asked to place his finger on the led sources. The red source is switched on and data is viewed on the digital CRO for 30s and it is stored as a CSV file. Then the IR source is switched on and data is acquired again for 30 s. The diffuse reflectance signal received by the photodiode was converted into voltage by the trans-impedance amplifier. The data were then stored on a USB drive with the digital oscilloscope [14]. The signal is converted from a ‘.csv’ file to a text file. Then this text file was used as input signal for processing in MATLAB software. Similarly, data were acquired from all the volunteers. The age group of the volunteers is 21–24 years. Then they were taken to the university health center and their Hb was measured invasively in the clinical laboratory.
The data exported to MATLAB was initially displayed as signal. Then the acquired signals were filtered and processed to get the targeted voltage signal. This voltage signal from both Red and IR LED sources was used as variables in the calculations for the determination of hemoglobin concentration. The extinction coefficients were taken from the literature [12,[15], [16], [17]].
3. Evaluation metrics
The evaluation metrics used to analyze the results include accuracy, RMSE, correlation, and Bland Altman plots.
3.1. Accuracy and error
The accuracy is calculated by taking the absolute difference between the Hb values estimated by invasive lab test (Hbi) and optical method (HbN) as in equation (14) and the error is calculated by calculating the difference between accuracy and 100 % as in equation (15).
| (14) |
| (15) |
3.2. Root mean square error (RMSE)
The RMSE value is one of the most common evaluation metrics used to observe the quality of the results obtained. It is calculated by the sum of the square of the difference between the reference and proposed method and dividing it by the number of observations as in equation (16).
| (16) |
3.3. Correlation
Correlation is an evaluation metric that establishes the relationship between two variables here invasive and non-invasive Hb values. It can be positive, negative or zero. The formula for the correlation (r) is given by equation (17).
| (17) |
where x = Hb values obtained by invasive method, y = Hb values obtained by non-invasive method and , represents mean of the Hb values respectively.
3.4. Bland Altman plot
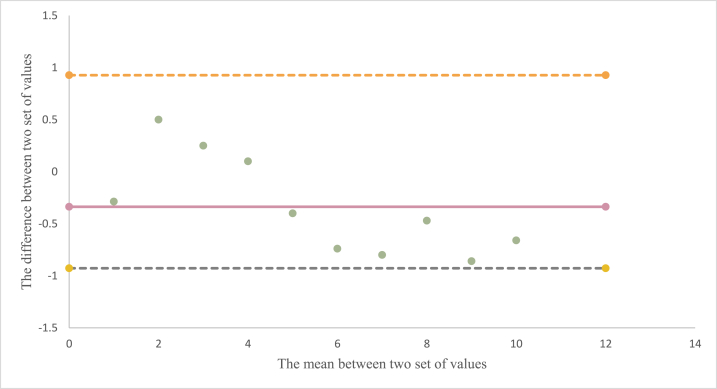
Bland Altman plot is the most used evaluation method to find the agreement between two methods of measurement or variables. Here, it is obtained by plotting the difference between the Hb values obtained by the invasive and optical methods against the average of the Hb values between the two methods. The measures like bias, upper and lower limit of agreement (LOA) were calculated by finding the mean of difference, and LOA was calculated by multiplying the standard deviation with 1.96 and −1.96 respectively and plotted along.
4. Results and discussion
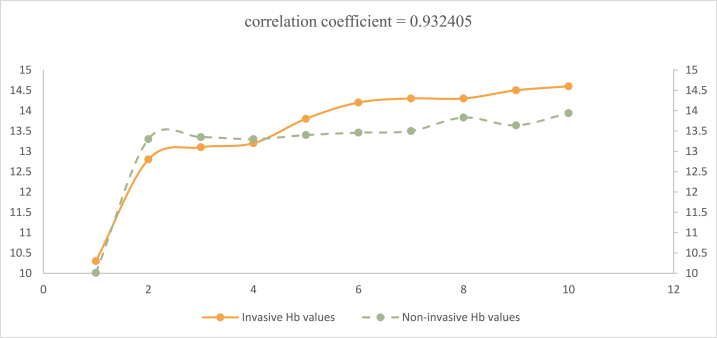
Table 1 shows the gender and age of volunteers who participated in the experiment along with Hb values obtained through the invasive method and proposed non-invasive method. It can be observed that the range of Hb values are from 12.8 to 14. In addition to that, the accuracy and error percentage values are tabulated for all the readings. The average accuracy and error percentages obtained are 96.31 and 3.675 respectively. RMSE is found to be 0.561121 g/dl. This indicates that our model can predict the data with good accuracy. The obtained r value is 0.932405, which is closer to 1. It indicates that the Hb values calculated by the proposed method is highly positively correlated to the reference method. Fig. 2 is the scatter plot between the Hb values obtained by both methods and it is evident that our proposed method is closely following the standard method. The Bland Altman plot is shown in Fig. 3. The upper and lower limits of agreement and bias are −0.92739, 0.927388, and −0.3367 respectively and are plotted. The limits were fixed by keeping the confidence level at 95 percent and a critical score value of 1.96. It is noted that the standard deviation between the two sets of measurements was as less as 0.473157.
Table 1.
Experimental results on volunteers.
| Subject | Gender | Age | Non-invasive Hb value (g/dl) | Invasive Hb value (g/dl) | Accuracy (%) | Error (%) |
|---|---|---|---|---|---|---|
| 1 | Female | 22 | 10.013 | 10.3 | 97.21 | 2.78 |
| 2 | Male | 22 | 13.83 | 14.3 | 96.71 | 3.28 |
| 3 | Male | 22 | 13.94 | 14.6 | 95.47 | 4.52 |
| 4 | Male | 24 | 13.46 | 14.2 | 94.78 | 5.21 |
| 5 | Male | 22 | 13.3 | 13.2 | 99.24 | 0.75 |
| 6 | Male | 21 | 13.35 | 13.1 | 98.09 | 1.90 |
| 7 | Male | 22 | 13.64 | 14.5 | 94.06 | 5.93 |
| 8 | Male | 23 | 13.4 | 13.8 | 97.10 | 2.89 |
| 9 | Female | 22 | 13.3 | 12.8 | 96.09 | 3.90 |
| 10 | Male | 23 | 13.5 | 14.3 | 94.40 | 5.59 |
| Average | 96.31 | 3.675 | ||||
Fig. 2.
Correlation plot between Hb values obtained by both invasive and non-invasive values.
Fig. 3.
Bland Altman plot between non-invasively and invasively obtained Hb values.
5. Conclusion
The determination of hemoglobin concentration not only indicates the physiological condition of the patients, but it also helps healthcare professionals to decide the course of treatment for many diseases. Worldwide many healthcare institutions follow the invasive method of taking blood from the arm of the patient to determine Hb concentration. In this work, a non-invasive method of Hb-level determination was proposed. Many non-invasive methods of Hb level determination have error because of improper removal of optical reflectance of blood components other than Hb but the proposed methodology reduced the error percentage by minimizing those interferences, since the equations derived depends upon the path length and existence coefficient values. The path length was determined by the refractive index and the physical distance between sensor systems. The Hb concentration was determined for 10 volunteers using the non-invasive method and the results were compared with clinically measured Hb concentration through the invasive method and found to have an accuracy of 96.31 % with RMSE of 0.56 %, R-value of 0.93 % and there is good agreement between the proposed and reference method as per Bland Altman plot. The correlation values obtained are higher than [[18], [19], [20]], comparable to Refs. [21,22] but lesser than [23] In the future, the proposed method can be improved by including the adaptive filters and involving more numbers of volunteers.
Data availability
Data used in this research is available with the authors. It will be shared upon request.
CRediT authorship contribution statement
Ranjith R: Writing – original draft, Software, Methodology, Investigation. Priya S: Software, Methodology, Investigation. Kaviya Dharshini A S: Validation, Formal analysis. Jeeva J.B: Writing – review & editing, Supervision, Conceptualization.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
The authors thank IECH, VIT-Vellore for approval of ethical clearance for taking blood samples from volunteers. The authors are grateful to the volunteers for their participation in this experiment.
Contributor Information
Ranjith R, Email: ranjith.r2013@vit.ac.in.
Priya S, Email: priyas.2013@vit.ac.in.
Kaviya Dharshini A S, Email: kaviyadharshinias@vit.ac.in.
Jeeva J.B, Email: jbjeeva@vit.ac.in.
References
- 1.Timm U., Kraitl J., Schnurstein K., Ewald H. Photometric sensor system for a non-invasive real-time hemoglobin monitoring. Proc. SPIE. March 2013;8572 [Google Scholar]
- 2.Timm U., Lewis E., McGrath D., Kraitl J., Ewald H. LED based sensor system for non-invasive measurement of the hemoglobin concentration in human blood. IFMBE Proceedings. 2008;23 [Google Scholar]
- 3.Desai Brinda, Chaskar Uttam. International Conference on Electrical, Electronics, and Optimization Techniques (ICEEOT) –. 2016. Comparison of optical sensors for non-invasive hemoglobin measurement. [Google Scholar]
- 4.Kumar Abhishek, Saxena A.K. IEEE International Conference on Signal Processing, Informatics, Communication, and Energy Systems (SPICES) 2015. Ramesh Kumar sonkar, “Non-invasive measurement of heart rate and hemoglobin concentration level through fingertip”. [Google Scholar]
- 5.Gayat E., Aulagnier J., Matthieu E., Boisson M., Fischler M. Non-invasive measurement of hemoglobin: assessment of two different point-of-care technologies. PLoS One. Jan. 2012;7(1) doi: 10.1371/journal.pone.0030065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shabaninejad Hosein, Ghadimi N., Sayehmiri Kourosh, Hosseinifard Hossein, Azarfarin Rasoul, Gorji Hasan Abolghasem. Comparison of invasive and noninvasive blood hemoglobin measurement in the operating room: a systematic review and meta-analysis. Mar. 2019;33(3):441–453. doi: 10.1007/s00540-019-02629-1. [DOI] [PubMed] [Google Scholar]
- 7.Timm U., Lewis E., Leen G., McGrath D., Kraitl J., Ewald H. 2010 IEEE Sensors Applications Symposium (SAS), Limerick, Ireland. 2010. Non-invasive continuous online hemoglobin monitoring system; pp. 131–134. doi: 10.1109/SAS.2010.5439415. [Google Scholar]
- 8.Daimiwal N., Sundhararajan M., Shriram R. 2014 International Conference on Communication and Signal Processing, Melmaruvathur, India. 2014. Comparative analysis of LDR and OPT 101 detectors in reflectance type PPG sensor; pp. 1078–1081. doi: 10.1109/ICCSP.2014.6950013. [Google Scholar]
- 9.Chugh S., Kaur J. 2015 International Conference on Control Communication & Computing India (ICCC), Trivandrum, India. 2015. Non-invasive hemoglobin monitoring device; pp. 380–383. doi: 10.1109/ICCC.2015.7432925. [Google Scholar]
- 10.Raid Saleem Al-Baradie, Anandh Sam Chandra Bose . 10th International Multi-Conferences on Systems, Signals & Devices. 2013. Portable smart non-invasive hemoglobin measurement system. (SSD13) [Google Scholar]
- 11.Nirupa L.A., Kumar V. International Symposium on Medical Measurements and Applications. June 2014. Non-invasive measurement of hemoglobin content in blood; pp. 1–5. [Google Scholar]
- 12.Meng F., Alayash A.I. Determination of extinction coefficients of human hemoglobin in various redox states. Anal. Biochem. 2017;521:11–19. doi: 10.1016/j.ab.2017.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pintavirooj C., Ni B., Chatkobkool C, Pinijkij K. Noninvasive portable hemoglobin concentration monitoring system using optical sensor for anemia disease. Healthcare (Basel) 2021 May 29;9(6):647. doi: 10.3390/healthcare9060647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kraitl J., Timm U., Ewald H., Lewis E. SENSORS, 2011 IEEE, Limerick, Ireland. 2011. Non-invasive sensor for an in vivo hemoglobin measurement; pp. 276–279. doi: 10.1109/ICSENS.2011.6126982. [Google Scholar]
- 15.Kim Jae G., Liu Hanli. Extinction coefficients of hemoglobin for near infrared spectroscopy of tissue. Engineering in Genomics, IEEE Engineering in Medicine and Biology Magazine. March 2005;24(2):118–121. doi: 10.1109/memb.2005.1411359. [DOI] [PubMed] [Google Scholar]
- 16.Rochmanto R.A., Zakaria H., Alviana R.D., Shahib N. 2017 4th International Conference on Electrical Engineering, Computer Science and Informatics (EECSI) 2017. Non-invasive hemoglobin measurement for Anemia diagnosis; pp. 1–5. (new-setup) [DOI] [Google Scholar]
- 17.Feng Ximeng, Li Gang, Yu Haixia, Wang Shaohui, Yi Xiaoqing, Lin Ling. Wavelength selection for portable noninvasive blood component measurement system based on spectral difference coefficient and dynamic spectrum. Spectrochim. Acta Mol. Biomol. Spectrosc. 2018;(193):40–46. doi: 10.1016/j.saa.2017.10.063. [DOI] [PubMed] [Google Scholar]
- 18.John B., Jamal A. Efficacy of noninvasive hemoglobin measurement by pulse co-oximetry in neonates. Journal of Clinical Neonatology. 2020;9(1):57. doi: 10.4103/jcn.jcn_89_19. [DOI] [Google Scholar]
- 19.Arai Y., et al. Evaluation of the use of non-invasive hemoglobin measurement in early childhood. Pediatr. Res. 2022;93(4):1036–1040. doi: 10.1038/s41390-022-02204-7. [DOI] [PubMed] [Google Scholar]
- 20.Kumar R.D., et al. "A novel noninvasive hemoglobin sensing device for anemia screening,". IEEE Sensor. J. 2021;21(13):15318–15329. doi: 10.1109/JSEN.2021.3070971. 1 July1. [DOI] [Google Scholar]
- 21.Pinto Caje, Parab Jivan, Naik Gourish. Non-invasive hemoglobin measurement using embedded platform. Sensing and Bio-Sensing Research. 2020;29 [Google Scholar]
- 22.Nandanwar Rutuja, et al. "Non-Invasive sensor technology for hemoglobin measurement in blood.". Methodology. 2021;5:8. [Google Scholar]
- 23.Panda Santosh Kumar, Mishra Alpana, Kumar Jena Pratap. "Agreement between noninvasive hemoglobin and laboratory hemoglobin measurements in neonates: a systematic review and meta-analysis.". Neonatology. 2023;120(1):24–32. doi: 10.1159/000526100. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data used in this research is available with the authors. It will be shared upon request.