Abstract
OBJECTIVE:
To explore the differences in Traditional Chinese Medicine (TCM) diagnosis and treatment rules for coronavirus disease 2019 (COVID-19) between Northern and Southern China based on the real-world data from 982 COVID-19 patients.
METHODS:
All consecutive cases of COVID-19 admitted to the TCM department of designated COVID-19 hospitals in eight provinces and cities were retrospectively analyzed. Patients were divided into a Northern and a Southern group according to the location of the admitting hospital. The symptoms, syndrome elements, syndrome distribution and herbal treatments were analyzed. The core prescriptions were extracted using the multiscale backbone-based network comparison algorithm (msbNC).
RESULTS:
The distribution of syndrome elements showed that dampness was common in Northern and Southern China, wind and heat were more often present in the South, while fire toxin and spleen deficiency were more often encountered in the North. The distribution of syndromes showed that the South was dominated by heat dampness accumulating in the lung (55.69%), while the North was dominated by dampness-toxin stagnating in the lung (44.90%).The results of core prescription mining showed that dispelling dampness, dispersing wind, clearing heat and strengthening spleen were the common treatment methods in Northern and Southern China. For mild cases, Jinyinhua (Flos Lonicerae) and Lianqiao (Fructus Forsythiae Suspensae) were often used in the South to clear heat and relieve exterior symptoms, while Chaihu (Radix Bupleuri Chinensis) and Huangqin (Radix Scutellariae Baicalensis) were often used in the North to relieve muscles by expelling heat. For moderate cases, Chaihu (Radix Bupleuri Chinensis), Qinghao (Herba Artemisiae Annuae), and Shigao (Gypsum Fibrosum) were often used to clear heat of Tri-jiao Channel and stomach in the South, while Fuling (Poria), Chenpi (Pericarpium Citri Reticulatae), and Dangshen (Radix Codonopsis) were often used to invigorate spleen and remove dampness in the North. For severe cases, spleen invigoration and dampness removal as well as relaxing the bowels and discharging heat were often used in the North.
CONCLUSION:
There were certain North-South differences in terms of symptoms, syndrome elements and syndrome distribution of COVID-19, as well as differences in core prescriptions during different periods of the disease. The regional differences in the rules of TCM diagnosis and treatment for COVID-19 should be further considered in the process of optimization and revision of relevant treatment guidance.
Keywords: COVID-19; medicine, Chinese traditional; North-South difference; core prescription; syndrome; retrospective studies
1. INTRODUCTION
Traditional Chinese Medicine (TCM) has a long history of use in the treatment of acute epidemic febrile diseases. Indeed, TCM development progressed simultaneously with Western medicine in the fight against epidemics.1 Since the outbreak of severe acute respiratory syndrome (SARS) in 2003,2,3 TCM played a very important role in the control of each epidemic in China such as 2009 H1N1 influenza,4 dengue fever,5 and hand, foot, and mouth disease,6 and its efficacy has been widely recognized. As of 21 July 2022, there were 562 672 324 confirmed cases of coronavirus disease 2019 (COVID-19) and 6 367 793 related deaths worldwide. In China alone, the number of confirmed cases and associated deaths were 5 337 774 and 22 936, respectively.7 The rapid spread of COVID-19 has resulted in a massive threat to the health system and society. Deaths linked indirectly to COVID-19 are attributable to other health conditions for which people were unable to access prevention and treatment because health systems were overburdened by the pandemic. New estimates from the World Health Organization show that the full death toll associated directly or indirectly with the COVID-19 pandemic between 1 January 2020 and 31 December 2021 was approximately 14.9 million.8 The indirect death toll caused by COVID-19 spread was much greater than the direct death toll. Therefore, to deal with the spread of COVID-19, both effective treatment and timely epidemic prevention and control were necessary. TCM has played an important role in the prevention and control of COVID-19 in China from the end of 2019, and has been included and widely promoted as part of the diagnostic and treatment guidelines for COVID-19 published by the National Health Commission. At present, the utilization rate of TCM in designated hospitals of most provinces and cities is more than 80%, reaching up to 100% in some areas.9 With the sustained spread of the epidemic and the emergence of virus variants, patients from different geographical environments and climates were noted to present with different clinical manifestations, and there were certain differences observed in the diagnostic and treatment strategies in different regions. The rules of TCM diagnosis and treatment of COVID-19 need to be further identified and summarized. Therefore, a large multicenter, retrospective cohort study was carried out on 982 confirmed patients in COVID-19 designated hospitals from eight provinces and cities in China, to further clarify the diagnosis and treatment rules of the disease, and to detect potential differences between Northern and Southern China, so as to provide an evidence-based basis for the optimization of relevant diagnostic and treatment guidance.
2. METHODS AND MATERIALS
2.1. Study design and participants
A multicenter, retrospective cohort study design was adopted. All patients diagnosed with COVID-19 and seen in the TCM department of eight COVID-19 designated hospitals in eight provinces of China (Beijing, Shanghai, Shenyang, Dalian, Sichuan, Fujian, Guangzhou and Hubei) were screened for eligibility for enrolment in this study. We retrospectively analyzed all consecutive cases from 14 January 2020 to 16 March 2021. Electronic medical information was collected using the TCM treatment platform for sudden acute infectious diseases. This study was approved by the Ethics Committee of Capital Medical University Beijing Traditional Chinese Medicine Hospital (Ethical Committee approval 2020BL02-041-01, ClinicalTrials. gov ChiCTR2000040765). No informed consent was required in view of established isolation precautions.
2.2. Data collection
Clinical Research Data Platform for Sudden Acute Infectious Diseases was developed for data collection and management. Medical record data collected from patients covered epidemiology, demographics, diagnosis (including TCM syndrome differentiation), clinical symptoms (including tongue image, pulse condition), comorbidities, laboratory tests, illness severity and treatments received during hospitalization (including TCM treatment and conventional treatment). Identification of Chinese medicine syndrome was performed by a Deputy Chief Physician or higher-level clinician, and all data were entered by uniformly trained data entry personnel while another researcher validated the recorded data.
2.3. Definitions
The exposure variable was defined as different areas. Accordingly, all the cases were divided into two groups: a Northern group, composed of patients from the designated hospitals in Northern China, which included Beijing, Shenyang, Dalian, and a Southern group, consisting of patients from the designated hospitals in Southern China, which included Shanghai, Guangzhou, Chengdu, Putian and Huanggang.
2.4. Statistical analysis
SPSS version 24.0 (IBM Corp., Armonk, NY, USA) was used for descriptive and cluster analyses. SPSS Clementine 24.0 (IBM Corp., Armonk, NY, USA) was used to analyze the association rules of the database. Quantitative data were summarized as mean ± standard deviation. Differences between two groups were assessed by analysis of variance (ANOVA). Categorical variables were reported as counts and percentages. Demographic and clinical characteristics at baseline were evaluated using χ 2 tests. In all analyses a significance level of P < 0.05 was deemed statistically significant. The special complex network analysis system for TCM clinical data10 was adopted. The complex network modeling and analysis method were used to build the clinical prescription data into a weighted herbs network with herbs as nodes and herbs compatibility frequency as edges. The msbNC11 was used to mine and analyze the core prescriptions (core herbs and compatibility). This method has been widely used in the core prescription analysis research of famous and old TCM.12
3. RESULTS
3.1. Baseline clinical characteristics of patients
A total of 1178 cases of COVID-19 confirmed patients were collected, and 982 cases from designated hospitals in eight provinces and cities (Beijing, Shanghai, Putian, Guangzhou, Huanggang, Chengdu, Dalian and Shenyang) were included in the final analysis. According to the geographical location of the hospitals, the patients were divided into a Northern group with 211 cases and a Southern group with 771 cases (Figure 1).
Figure 1. Study flowchart.
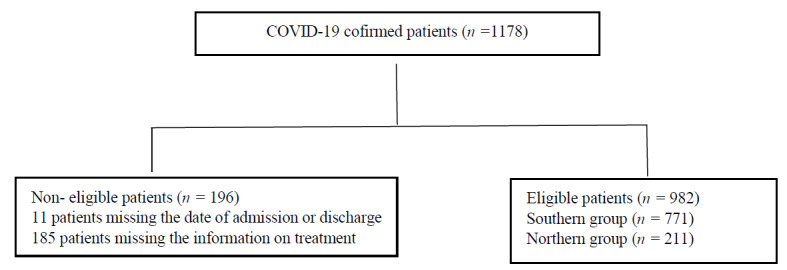
COVID-19: coronavirus disease 2019.
Among the included patients, the proportion of patients in the Northern group with a 14-day contact history was higher than in the Southern group (P < 0.01), while the proportion of patients with recent overseas travel was lower than in the Southern group (P < 0.01). The proportion of asymptomatic infected, severe and critical cases was higher in the Northern group, while the proportion of mild and common cases was higher in the Southern group. The proportion of patients with cardiovascular and cerebrovascular diseases in the Northern group was higher than that in the Southern group (P < 0.01).Comparison of symptoms showed that cough (P < 0.01), expectoration (P < 0.05), chest tightness or shortness of breath (P < 0.01), and dry mouth, bitter mouth or thirst (P < 0.01) were more common in the Northern group than in the Southern group. Comparison of the course of disease between the two groups showed that the hospital length of stay in the Northern group was slightly longer (P < 0.05), and the admission rate in the ICU was higher (P < 0.01), but the ICU length of stay was shorter than Southern group (P < 0.05). Extracorporeal membrane oxygenation (ECMO) use was higher in the Northern group, while there was no significant difference in the proportion of invasive and noninvasive mechanical ventilation between the two groups. Duration of antibiotic treatment in Northern group was significantly shorter than in the Southern group (P < 0.01), and the time of first use of TCM was earlier than in the Southern group (P < 0.05) (Table 1).
Table 1.
Clinical features and treatment of the two cohorts
| Item | Total cases (n = 982) |
Northern group (n = 211) |
Southern group (n = 771) |
P value |
|---|---|---|---|---|
| Age (years) | 41.30±16.15 | 46.64±17.77 | 39.74±15.31a | <0.001 |
| Female [n (%)] | 533 (54.28) | 97 (45.98) | 436 (56.55) a | <0.001 |
| Male [n (%)] | 449 (45.73) | 114 (54.02) | 335 (43.45)a | <0.001 |
| BMI (kg/m²) | 23.63±3.28 | 23.92±3.69 | 23.55±3.04 | 0.161 |
| Smokers [n (%)] | 81 (8.25) | 22 (10.43) | 59 (7.65) | 0.194 |
| 14-day contact history [n (%)] | 242 (24.64) | 131 (62.09) | 111 (14.40)a | <0.001 |
| Overseas Travel [n (%)] | 455 (46.33) | 17 (8.06) | 438 (56.81)a | <0.001 |
| Asymptomatic [n (%)] | 111 (11.30) | 62 (29.38) | 49 (6.36)a | <0.001 |
| Mild [n (%)] | 112 (11.41) | 11 (5.21) | 101 (13.10)a | <0.001 |
| Moderate [n (%)] | 716 (72.91) | 118 (55.92) | 598 (77.56)a | <0.001 |
| Serious [n (%)] | 40 (4.07) | 17 (8.06) | 23 (2.98)a | <0.001 |
| Critical [n (%)] | 3 (0.31) | 3 (1.42) | 0 (0.0)a | <0.001 |
| Diabetes [n (%)] | 48 (4.89) | 21 (1.00) | 27 (3.50)a | <0.001 |
| Chronic lung disease [n (%)] | 28 (2.85) | 8 (3.79) | 20 (2.59) | 0.295 |
| Cardiovascular disease (including high blood pressure) [n (%)] | 95 (9.67) | 46 (21.80) | 49 (6.46)a | <0.001 |
| Digestive system disease [n (%)] | 8 (0.81) | 0 (0.0) | 8 (1.04) | 0.137 |
| Nervous system disease [n (%)] | 5 (0.51) | 2 (0.95) | 3 (0.39) | 0.312 |
| Chronic liver disease [n (%)] | 16 (1.63) | 2 (0.95) | 14 (1.86) | 0.242 |
| Fever [n (%)] | 122 (12.42) | 31 (14.69) | 91 (11.80) | 0.260 |
| <37.4 ℃[n (%)] | 860 (87.58) | 184 (87.20) | 676 (87.68) | 0.853 |
| 37.4 ℃-38.0 ℃ [n (%)] | 84 (8.56) | 23 (10.90) | 65 (8.43) | 0.266 |
| >38 ℃ [n (%)] | 38 (3.87) | 10 (4.74) | 28 (3.63) | 0.460 |
| Cough [n (%)] | 335 (34.11) | 101 (47.87) | 234 (30.35)a | <0.001 |
| Fatigue [n (%)] | 164 (16.70) | 32 (15.17) | 132 (17.12) | 0.500 |
| Myalgia [n (%)] | 32 (3.26) | 5 (0.24) | 27 (3.50) | 0.412 |
| Irritability [n (%)] | 33 (3.36) | 4 (1.90) | 29 (3.76) | 0.183 |
| Diarrhea [n (%)] | 37 (3.77) | 6 (2.84) | 31 (4.02) | 0.426 |
| Runny nose [n (%)] | 36 (3.67) | 9 (4.27) | 27 (3.50) | 0.601 |
| Expectoration [n (%)] | 216 (22.00) | 59 (27.96) | 157 (20.36)b | 0.018 |
| Sore throat [n (%)] | 81 (8.25) | 12 (5.69) | 69 (8.95) | 0.127 |
| Dyspnea [n (%)] | 95 (9.67) | 41 (19.43) | 54 (7.00)a | <0.001 |
| Abdominal pain [n (%)] | 31 (3.16) | 6 (2.84) | 25 (3.24) | 0.769 |
| Dry mouth [n (%)] | 158 (16.09) | 44 (20.85) | 114 (14.79)b | 0.034 |
| Days from onset to admission (d) | 4.64±5.88 | 4.72±4.58 | 4.62±6.19 | 0.062 |
| Hospital length of stay (d) | 16.98±8.48 | 17.31±6.63 | 16.90±8.90c | 0.014 |
| Course of disease (d) | 20.70±10.19 | 21.26±7.94 | 20.55±10.69 | 0.083 |
| ICU admission [n (%)] | 33(3.36) | 22(10.43) | 11(1.43)a | <0.001 |
| ICU length of stay (d) | 15.57±8.35 | 13.91±6.58 | 33.00±1.41b | 0.022 |
| Viral shedding duration (d) | 12.12±7.74 | 12.38±5.82 | 12.04±8.25 | 0.064 |
| Duration of antibiotic treatment (d) | 9.91±5.12 | 6.89±4.30 | 10.16±5.11b | 0.005 |
| Duration of corticosteroid treatment (d) | 6.40±5.03 | 7.48±7.32 | 6.00±3.86 | 0.609 |
| Duration of oxygenation by nasal cannula or face mask (d) | 2.12±1.69 | 2.05±2.01 | 2.13±1.63 | 0.061 |
| Cases of noninvasive mechanical ventilation [n (%)] | 9(0.92) | 3(1.42) | 6(0.78) | 0.385 |
| Cases of traumatic mechanical ventilation [n (%)] | 6(0.61) | 3(1.42) | 3(0.39) | <0.088 |
| ECMO [n (%)] | 2(0.20) | 2(0.95) | 0(0.0)a | 0.007 |
| Admission days of first TCM use (d) | 2.77±4.18 | 1.78±2.27 | 2.63±1.53b | 0.015 |
Notes: North group: patients from the designated hospitals in Northern China, which included Beijing, Shenyang, Dalian; South group: patients from the designated hospitals in Southern China, which included Shanghai, Guangzhou, Chengdu, Putian Dalian, and Huanggang. BMI: body mass index; ICU: intensive care unit; TCM: Traditional Chinese Medicine; d: days. Categorical variables were reported as counts and percentages. Demographic and clinical characteristics at baseline were evaluated using χ2 tests. Quantitative data were presented as mean ± standard deviation. aP < 0.01, bP < 0.05, Northern vs Southern.
3.2. Syndrome element
A total of 17 syndrome elements were extracted from the two groups. The syndrome elements with a frequency ≥10% in the Southern group were heat, wind, lung and dampness. The syndrome elements with a frequency≥10% in the Northern group were toxin, dampness, lung, spleen and deficiency (Table 2).
Table 2.
Frequency distribution of syndrome elements in the Northern and Southern groups
| Northern group (n = 211) | Southern group (n = 771) | ||||
|---|---|---|---|---|---|
| Syndrome elements | Frequency | Proportion (%) | Syndrome elements | Frequency | Proportion (%) |
| Toxin | 86 | 40.76 | Heat | 620 | 80.42 |
| Dampness | 74 | 35.07 | Wind | 349 | 45.27 |
| Lung | 68 | 32.23 | Lung | 81 | 10.51 |
| Spleen | 50 | 23.70 | Dampness | 65 | 8.43 |
| Deficiency | 39 | 18.48 | Phlegm | 48 | 6.23 |
| Heat | 9 | 4.27 | Toxin | 26 | 0.37 |
| Wind | 7 | 3.12 | Cold | 13 | 1.69 |
| Phlegm | 7 | 3.12 | Fire | 11 | 1.43 |
| Exterior | 4 | 1.90 | Spleen | 4 | 0.52 |
| Blood stasis | 4 | 1.90 | Deficiency | 3 | 0.39 |
Notes: North group: patients from the designated hospitals in Northern China, which included Beijing, Shenyang, Dalian; South group: patients from the designated hospitals in Southern China, which included Shanghai, Guangzhou, Chengdu, Putian Dalian, and Huanggang.
3.3. Syndrome pattern
A total of 44 syndromes were extracted from the two groups. The Southern group was dominated by Heat dampness accumulating in the lung pattern, Dampness-toxin stagnating in the lung pattern, Wind heat attacking the lung pattern, and Epidemic toxin blocking the lung pattern. The Northern group was dominated by Dampness-toxin stagnating in the lung pattern, Spleen deficiency and dampness pattern, Heat toxin accumulating in the lung pattern and Epidemic toxin blocking the lung pattern (Table 3).
Table 3.
The top 6 frequencies of syndrome distribution in the Northern and Southern groups
| Northern group (n = 211) | Southern group (n = 771) | ||||
|---|---|---|---|---|---|
| Patterns | Frequency | Proportion (%) | Patterns | Frequency | Proportion (%) |
| Dampness-toxin stagnating in the lung |
94 | 44.55 | Heat dampness accumulating in the lung | 429 | 55.65 |
| Deficiency of lung and spleen Qi | 38 | 18.01 | Dampness-toxin stagnating in the lung |
123 | 15.96 |
| Heat dampness accumulating in the lung | 38 | 18.01 | Wind heat attacking the lung | 41 | 5.32 |
| Qi and Yin deficiency | 21 | 9.52 | Epidemic toxin blocking the lung | 31 | 4.02 |
| Epidemic toxin blocking the lung | 19 | 9.00 | Cold dampness stagnating in the lung |
14 | 1.82 |
| Cold dampness obstructing the lung | 5 | 2.37 | Deficiency of lung and spleen Qi | 14 | 1.82 |
Notes: North group: patients from the designated hospitals in Northern China, which included Beijing, Shenyang, Dalian; South group: patients from the designated hospitals in Southern China, which included Shanghai, Guangzhou, Chengdu, Putian Dalian, and Huanggang.
3.4. Herbals
The most frequently used herbals were Fuling (Poria), Chaihu (Radix Bupleuri Chinensis), Lianqiao (Fructus Forsythiae Suspensae), Huangqin (Radix Scutellariae Baicalensis), Gancao (Radix Glycyrrhizae), Chenpi (Pericarpium Citri Reticulatae), Cangzhu (Rhizoma Atractylodis Lanceae), Jinyinhua (Flos Lonicerae), Huoxiang (Herba Agastaches Rugosa), Huangqi (Radix Astragali Mongolici), Baizhu (Rhizoma Atractylodis Macrocephalae), Dangshen (Radix Codonopsis), Dahuang (Radix Et Rhizoma Rhei Palmati) and Kuxingren (Semen Armeniacae Amarum). The Southern group was dominated by the treatment principle of strengthening spleen and transforming phlegm, clearing heat and releasing the exterior. The Northern group was dominated by the treatment principle of removing wind and heat, transforming dampness and removing toxins (Table 4).
Table 4.
Frequency of use of Chinese Herbal Medicine (top 10) in the Northern and Southern groups
| Northern group (n = 211) | Southern group (n = 771) | ||||
|---|---|---|---|---|---|
| Herbal | Frequency | Proportion (%) | Herbal | Frequency | Proportion (%) |
| Chaihu (Radix Bupleuri Chinensis) |
122 | 57.82 | Fuling (Poria) | 187 | 24.25 |
| Huangqin (Radix Scutellariae Baicalensis) |
121 | 57.35 | Lianqiao (Fructus Forsythiae Suspensae) |
174 | 22.56 |
| Gancao (Radix Glycyrrhizae) | 120 | 56.87 | Gancao (Radix Glycyrrhizae) | 168 | 21.79 |
| Cangzhu (Rhizoma Atractylodis Lanceae) |
110 | 52.13 | Chenpi (Pericarpium Citri Reticulatae) |
165 | 21.40 |
| Huoxiang (Herba Agastaches Rugosa) |
107 | 50.71 | Jinyinhua (Flos Lonicerae) | 131 | 16.99 |
| Jinyinhua (Flos Lonicerae) |
100 | 47.39 | Huangqi (Radix Astragali Mongolici) |
120 | 15.56 |
| Fuling (Poria) |
100 | 47.39 | Huangqin (Radix Scutellariae Baicalensis) |
119 | 15.43 |
| Chenpi (Pericarpium Citri Reticulatae) |
94 | 44.55 | Baizhu (Rhizoma Atractylodis Macrocephalae) |
112 | 14.53 |
| Baizhu (Rhizoma Atractylodis Macrocephalae) |
89 | 42.18 | Dangshen (Radix Codonopsis) | 92 | 11.94 |
| Kuxingren (Semen Armeniacae Amarum) |
85 | 40.28 | Dahuang (Radix Et Rhizoma Rhei Palmati) |
87 | 11.28 |
Notes: North group: patients from the designated hospitals in Northern China, which included Beijing, Shenyang, Dalian; South group: patients from the designated hospitals in Southern China, which included Shanghai, Guangzhou, Chengdu, Putian Dalian, and Huanggang.
3.5. Compatibility rules for asymptomatic cases
Core prescriptions for asymptomatic patients were Jinyinhua (Flos Lonicerae), Gancao (Radix Glycyrrhizae), Jiegeng (Radix Platycodi), Huangqi (Radix Astragali Mongolici), Chenpi (Pericarpium Citri Reticulatae), Fuling (Poria), Lianqiao (Fructus Forsythiae Suspensae), Huangqin (Radix Scutellariae Baicalensis), and Huoxiang (Herba Agastaches Rugosa). Releasing the exterior, transforming dampness and reinforcing healthy Qi were mostly used in Southern group. The common compatibilities in Southern group were: Huoxiang (Herba Agastaches Rugosa), Huangqi (Radix Astragali Mongolici), Jinyinhua (Flos Lonicerae) and Gancao (Radix Glycyrrhizae). Releasing the exterior, transforming dampness, and transforming phlegm were mostly used in the Northern group. The common compatibilities in the Northern group were: Huoxiang (Herba Agastaches Rugosa), Jiegeng (Radix Platycodi), Fuling (Poria), Chenpi (Pericarpium Citri Reticulatae), Gancao (Radix Glycyrrhizae) and Jinyinhua (Flos Lonicerae).
3.6. Compatibility rules for mild cases
Core prescriptions for mild cases were: Fuling (Poria), Chenpi (Pericarpium Citri Reticulatae), Jiegeng (Radix Platycodi), Jinyinhua (Flos Lonicerae), Gancao (Radix Glycyrrhizae), Lianqiao (Fructus Forsythiae Suspensae), Dangshen (Radix Codonopsis), Baizhu (Rhizoma Atractylodis Macrocephalae), Huangqin (Radix Scutellariae Baicalensis), Huanglian (Rhizoma Coptidis), Huoxiang (Herba Agastaches Rugosa) and Kuxingren (Semen Armeniacae Amarum). The Southern group frequently used eliminating dampness and transforming phlegm, clearing heat and dispelling wind to improve patients' symptoms and the most common compatibilities in southern group were: Huoxiang (Herba Agastaches Rugosa), Chenpi (Pericarpium Citri Reticulatae), Fuling (Poria), Chaihu (Radix Bupleuri Chinensis), Banxia (Rhizoma Pinelliae), Cangzhu (Rhizoma Atractylodis Lanceae) and Gancao (Radix Glycyrrhizae). The Northern group often used to release the exterior and clearing heat. The most common com-patibilities were: Jinyinhua (Flos Lonicerae), Lianqiao (Fructus Forsythiae Suspensae), Huangqin (Radix Scutellariae Baicalensis) and Gancao (Radix Glycyrrhizae).
3.7. Compatibility rules for moderate cases
Core prescriptions for moderate cases were: Jinyinhua (Flos Lonicerae), Gancao (Radix Glycyrrhizae), Fuling (Poria), Huoxiang (Herba Agastaches Rugosa), Chenpi (Pericarpium Citri Reticulatae), Huangqin (Radix Scutellariae Baicalensis), Dangshen (Radix Codonopsis), Huangqi (Radix Astragali Mongolici), Jiegeng (Radix Platycodi), Lianqiao (Fructus Forsythiae Suspensae). The Southern group mostly used clearing heat, drying dampness and dispersing the lung as a treatment principle. The common compatibilities in Southern group were: Shigao (Gypsum Fibrosum), Kuxingren (Semen Armeniacae Amarum), Huangqin (Radix Scutellariae Baicalensis), Chaihu (Radix Bupleuri Chinensis), Cangzhu (Rhizoma Atractylodis Lanceae), Lugen (Rhizoma Phragmitis) and Qinghao (Herba Artemisiae Annuae). The Northern group used dispelling wind, clearing heat and removing toxins in most cases. The common compatibilities in Northern group were: Jiegeng (Radix Platycodi), Chenpi (Pericarpium Citri Reticulatae), Fuling (Poria), Lianqiao (Fructus Forsythiae Suspensae), Jinyinhua (Flos Lonicerae) and Huangqin (Radix Scutellariae Baicalensis).
3.8. Compatibility rules for serious and critical cases
Core prescriptions for serious and critical cases were: Huangqin (Radix Scutellariae Baicalensis), Gancao (Radix Glycyrrhizae), Kuxingren (Semen Armeniacae Amarum), Baizhu (Rhizoma Atractylodis Macroce-phalae), Lianqiao (Fructus Forsythiae Suspensae), Chenpi (Pericarpium Citri Reticulatae), Fuling (Poria), Chaihu (Radix Bupleuri Chinensis), Bohe (Herba Menthae Haplocalycis), Yiyiren (Semen Coicis), Huoxiang (Herba Agastaches Rugosa), Lugen (Rhizoma Phragmitis ) and Huzhanggen (Radix Polygoni Cuspidati). The Southern group mostly used clearing heat, dispersing the lung, drying dampness and transforming phlegm. The common compatibilities in Southern group were: Huangqin (Radix Scutellariae Baicalensis), Gancao (Radix Glycyrrhizae), Huoxiang (Herba Agastaches Rugosa), Jinyinhua (Flos Lonicerae), Lianqiao (Fructus Forsythiae Suspensae), Kuxingren (Semen Armeniacae Amarum), Huzhanggen (Radix Polygoni Cuspidati), Chaihu (Radix Bupleuri Chinensis), Fuling (Poria) and Chenpi (Pericarpium Citri Reticulatae). The Northern group mostly used clearing heat, transforming phlegm, removing toxins and transforming stasis, and the common compatibilities were: Huangqin (Radix Scutellariae Baicalensis), Gancao (Radix Glycyrrhizae), Baizhu (Rhizoma Atractylodis Macrocephalae), Huoxiang (Herba Agastaches Rugosa), Maidong (Radix Ophiopogonis Japonici), Tinglizi (Semen Lepidii Apetali), Gualou (Fructus et Semen Trichosanthis), Dahuang (Radix Et Rhizoma Rhei Palmati), Mabiancao (Herba Verbenae Officinalis), Qinghao (Herba Artemisiae Annuae) and Huzhanggen (Radix Polygoni Cuspidati).
4. DISCUSSION
COVID-19 can be considered as “cold and damp pestilence ” in TCM, which is caused by a pestilential pathogen, having the clinical features of fever, dry cough, and fatigue.13 The core pathogenesis of the disease is dampness and toxic pestilential pathogen invading the lung, Sanjiao and spleen, dampness and heat stagnating and obstructing, which leads to epidemic toxin blocking the lung. The treatment principle is to eliminate turbidity and detoxify, which is expected to persist throughout the whole disease course. For epidemic disease treatment, TCM has applied the concept of "Tongzhi prescription" (Adopting a method or prescription for treating the core pathogenesis) since ancient times, such as Wen Yi Lun: “How do you know it is an epidemic? The syndrome and pulse are the same among people in the year of prevalence, and there is no difference in medication and effect.”14 “There is only one effective medicine for each disease, which doesn't need to consider the prescription compatibility of monarch, minister, assistant and guide.” Therefore, it was very important to detect and extract the ” core prescriptions” for the prevention and treatment of sudden acute infectious diseases such as COVID-19. In addition, the ancients also believed in the concept of treating epidemic diseases according to three factors (treatment according to time, place and person), such as Wen Yi Lun: “The plagues are different in different years, regions and seasons.” 14 Dampness plague in different climates or regions can be mixed up with the characteristics of wind, cold, heat and dryness. Dampness plague damages Tri-jiao channel, lung and spleen which is the core pathogenesis. There were two main forms of TCM intervention in response to COVID-19 outbreaks in China. In cases where the epidemic broke out on a very large scale and the health system was too overburdened to adopt the "one person, one policy," the general prescription could be used as soon as possible to improve patients’ prognosis. When under the normal prevention and control measures against COVID-19, health resources could meet the TCM requirement "one person, one policy," it was suggested to comprehensively consider the region, climate and personal constitution, and adopt and make syndrome differentiation for each stage of the disease according to three factors: time, place and person. Currently, 23 provinces and regions in China have released modified treatment guidance according to geographical, weather conditions, and people’s physique and constitution, and TCM practitioners have already participated throughout the treatment process for COVID-19 in designated hospitals. 15
In this retrospective study, 982 real-world cases were included, and were analyzed before the emergence of COVID-19 variants in China. For example, the Delta and Omicron virus strains appeared in China in June 2021 and October 2022, respectively, while this study included COVID-19 cases from January 2020 to March 2021. Hence, the different TCM treatments and diagnoses were mainly due to differences in patients’ physique and geographical and weather conditions but not due to different virus strains. It was found that there were certain differences in the clinical profiles, syndrome differentiation and treatments of the disease in different regions. Similar to other studies,16 common clinical symptoms of confirmed COVID-19 were cough, expectoration, fatigue, thirst and fever. Symptoms such as cough (P < 0.01), expectoration (P < 0.05), chest tightness, shortness of breath (P < 0.01), dry mouth and bitter mouth (P < 0.05) were more common among patients in the Northern group, which showed that the “heat” symptoms in the Northern group were more obvious than in the Southern group. The comparison of syndrome element distribution shows that the five most common syndrome elements overall were: "wind," "lung," "dampness," "spleen" and "deficiency." Dampness was the most common syndrome element in both the North and the South. Fire toxin and spleen deficiency were the common denominator in the Northern group, while wind and heat were the common denominator in the Southern group. The distribution of syndrome pattern was mainly Dampness-toxin stagnating in the lung in the Northern group (44.90%) and Heat dampness accumulating in the lung in the Southern group (55.69%). In the South, which has a humid and hot climate, the pathogenic characteristics would reflect heat dampness stagnation and obstruction more, so treatment of all stages of the disease should focus on inducing urination and promoting bowel movement to eliminate pathogenic factors and disperse Qi movement. In the North’ which has a cold and dry climate, people had a body constitution of spleen deficiency with dampness accumulation caused by high fat and salt diets that lead to internal turbidity. When the dampness plague combines the turbidity inside with each other, lead orifices are blocked and dryness injures Yin. Therefore, the treatment is mainly used to remove dampness and detoxify, and reinforce healthy Qi to strengthen the body.
The msbNC can be used as a promising approach to discover effective herb interactions from large-scale clinical data,11 which was used in this research to detect the core prescriptions in Northern and Southern China. The comparison of common herbals distribution shows that most of the commonly used herbals in the North and South were the same, such as Fuling (Poria), Chenpi (Pericarpium Citri Reticulatae), Jinyinhua (Flos Lonicerae), Lianqiao (Fructus Forsythiae Suspensae), Huangqin (Radix Scutellariae Baicalensis) and Baizhu (Rhizoma Atractylodis Macrocephalae), etc. Hence, removing dampness, dispersing wind, clearing heat and strengthening the spleen were common treatment methods. There were certain differences in the treatment at different stages of disease progression between the North and South. For mild cases, Jinyinhua (Flos Lonicerae), Lianqiao (Fructus Forsythiae Suspensae) and other herbals for releasing the exterior with pungent-cool were used in the South, while Chaihu (Radix Bupleuri Chinensis) and Huangqin (Radix Scutellariae Baicalensis) were used in the North to relieve muscle heat and harmonize and release Shaoyang. For moderate cases, Chaihu (Radix Bupleuri Chinensis), Qinghao (Herba Artemisiae Annuae) and Shigao (Gypsum Fibrosum) were often used in the South to clear away the heat evil of Shaoyang Yang and Yang Ming (lung and stomach), while Chenpi (Pericarpium Citri Reticulatae), Fuling (Poria) and Dangshen (Radix Codonopsis), etc. were often used in the North to strengthen the spleen and remove dampness. For severe and critical cases, Gualou (Fructus et Semen Trichosanthis), Dahuang (Radix Et Rhizoma Rhei Palmati) and Tinglizi (Semen Lepidii Apetali) were often used in the North to unblock the bowel and clear heat. The differences in treatment might be due to differences in body constitution in the North and South. The Southern people had thin and sparse striae of the skin and muscle, and herbals of releasing the exterior with pungent-cool could be used to remove pathogenic factors and release the exterior. When the disease progresses to the stage of pneumonia, the Sanjiao and lung obstruction were obvious, so Chaihu (Radix Bupleuri Chinensis), Qinghao (Herba Artemisiae Annuae) and Shigao (Gypsum Fibrosum) were used to clear the heat of Shaoyang and Yangming. The people in Northern China had dense striae of the skin and muscle, so in the early stage of the disease, the epidemic toxin and Wei-defensive Qi compete with each other in the muscle, and it is difficult to remove epidemic toxin by the herbal releasing the exterior. In the early stage of the disease, Chaihu (Radix Bupleuri Chinensis) and Huangqin (Radix Scutellariae Baicalensis) were often used to relieve muscle and clear heat. In the later stage of the disease, dryness and heat injure Qi and Yin, so spleen invigoration, dampness removal and bowel movement promotion were often used in the North.
The present study has some notable strength. First, it summarized the symptoms, syndrome elements and syndrome types of patients at the initial stage of COVID-19. Second, we preliminarily explored the similarities and differences of the pathological mechanism of patients in the North and South, and further clarified the main pathogenesis of the disease caused by the damp pestilence. Third, by comparing the differences in the diagnosis and treatment rules between the North and the South, we provided an evidence base for the concept of treating epidemic diseases according to three factors. However, there are still some limitations of this study. Due to the recognition and response to the original virus strain and the strict prevention and control measures being carried out in China in the early stage of the COVID-19 pandemic, there were no outbreaks of such a wide geographical range involving Southern and Northern China simultaneously. As a result, there are no data on the diagnosis and treatment of patients in Southern and Northern China at the same time point, making it impossible to prove the differences in TCM diagnosis and treatment rules between the South and the North caused by differences in temperature, region and human body constitution, or caused by a single factor.
In conclusion, the character of TCM treatment of epidemic disease was “Tongzhi prescription” combined with treatment according to three etiological factors. This retrospective study showed that the core pathogenesis of COVID-19 was dampness and epidemic pathogen invading the lung. The main treatment methods were transforming dampness, removing wind, clearing heat and strengthening the spleen. Due to differences in body constitution between Northern and Southern China patients, there were differences in clinical symptoms, syndrome pattern, and treatment methods for different stages of the disease. The optimization and revision of the COVID-19 treatment guidance needs to further consider the differences in diagnosis and treatment among different climates and regions.
Footnotes
Supported by National Key Research and Development Plan: Study on TCM Syndrome Regularity and Optimization of Coronavirus Disease 2019 Diagnosis and Treatment Plan (No. 2021YFC1712901)
Contributor Information
Qingquan LIU, Email: liuqingquan2003@126.com.
Mifeng LIU, Email: liumifeng@bjzhongyi.com.
References
- 1. Wang WY, Xie Y, Zhou H, Liu L. Contribution of Traditional Chinese Medicine to the treatment of COVID-19. Phytomedicine 2021; 85: 153279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Jia W, Gao W. Is Traditional Chinese Medicine useful in the treatment of SARS? Phytother Res 2003; 17: 840-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chen Z, Nakamura T. Statistical evidence for the usefulness of Chinese medicine in the treatment of SARS. Phytother Res 2004; 18: 592-4. [DOI] [PubMed] [Google Scholar]
- 4. Li JH, Wang RQ, Guo WJ, Li JS. Efficacy and safety of Traditional Chinese Medicine for the treatment of influenza A (H1N1): a Meta-analysis. J Chin Med Assoc 2016; 79: 281-1. [DOI] [PubMed] [Google Scholar]
- 5. Liu LD, Liu J, Lin LP, Ai XY, Tan XH, Yuan LX. Analysis of TCM syndrome characteristics and pathogenesis of 345 cases of dengue. Zhong Guo Zhong Yi Ji Zheng Za Zhi 2016; 25: 1316-8. [Google Scholar]
- 6. Li X, Zhang X, Ding J, et al. Comparison between Chinese herbal medicines and conventional therapy in the treatment of severe hand, foot, and mouth disease: a randomized controlled trial. Evid Based Complement Alternat Med 2014; 2014: 140764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. World Health Organization . WHO Coronavirus (COVID-19) Dashboard, 2022-12-02, cited 2022-12-05; Available from URL: https://covid19.who.int/. https://covid19.who.int/ [Google Scholar]
- 8. World Health Organization . 14.9 million excess deaths associated with the COVID-19 pandemic in 2020 and 2021, 2022-05-05. cited 2022-12-05; Available from URL: https://www.who.int/zh/news/item/05-05-2022-14.9-million-excess-deaths-were-associated-with-the-covid-19-pandemic-in-2020-and-2021. https://www.who.int/zh/news/item/05-05-2022-14.9-million-excess-deaths-were-associated-with-the-covid-19-pandemic-in-2020-and-2021 [Google Scholar]
- 9. State Administration of Traditional Chinese Medicine . The use rate of Traditional Chinese Medicine in treating COVID-19 in Dalian reached 100%, 2020-07-28; cited 2022-12-05; Available from URL: http://www.satcm.gov.cn/xinxifabu/gedidongtai/2020-08-12/16390.html.http://www.satcm.gov.cn/xinxifabu/gedidongtai/2020-08-12/16390.html [Google Scholar]
- 10. Zhou X, Liu B. Network analysis system for Traditional Chinese Medicine clinical data. 2009 2nd International Conference on Biomedical Engineering and Informatics; 2009 Oct 17-19. Tianjin, China. New York: IEEE, 2009: 1-5. [Google Scholar]
- 11. Du N, Zhou X, Zhang R, Jia C, Yu J, Liu B. Multiscale backbone based network comparison algorithm for effective herbal interaction analysis. 2011 4th International Conference on Biomedical Engineering and Informatics; 2011 Oct 15-17. Shanghai, China. New York: IEEE, 2011: 1757-62. [Google Scholar]
- 12. Xing GL, Liu JJ, Yu ZC, Zhou XZ, Yang Y. Analysis of the rule of Chinese medicine Master ShenBaofan in the treatment of coronary heart disease based on complex network. Hunan Zhong Yi Yao Da Xue Xue Bao 2021; 41: 986-91. [Google Scholar]
- 13. Tong XL, Li XY, Zhao LH, Li WQ, Yang YY, Lin YQ. Explore the TCM prevention and treatment strategies of new coronavirus pneumonia (COVID-19) from the perspective of cold and damp pestilence. Zhong Yi Za Zhi 2020; 61: 465-70, 553. [Google Scholar]
- 14. Wu YK (Ming dynasty) . Wen Yi Lun. Beijing: People's Medical Publishing House, 1990: 2- 3. [Google Scholar]
- 15. Wang W, Wang Y, Ma S, Li R. Analysis on strategy, participation rate and cure effect of traditional Chinese medicine in treating COVID-19 in 23 provinces (municipalities and autonomous regions). Shi Jie Zhong Yi Yao Za Zhi 2020; 15: 813-8. [Google Scholar]
- 16. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020; 382: 1708-20. [DOI] [PMC free article] [PubMed] [Google Scholar]


