Abstract
Background
In recent decades, early rehabilitation after Achilles tendon rupture (ATR) repair has been proposed. The aim of this prospective cohort study was to compare different immobilisation durations in order to determine the optimal duration after open surgery for ATR repair.
Methods
This study included 1088 patients (mean age, 34.9 ± 5.9 years) who underwent open surgery for acute ATR repair. The patients were categorised into four groups (A, B, C, and D) according to postoperative immobilisation durations of 0, 2, 4, and 6 weeks, respectively. All patients received the same suture technique and a similar rehabilitation protocol after brace removal,; they were clinically examined at 2, 4, 6, 8, 10, 12, 14, and 16 weeks postoperatively, with a final follow-up at a mean of 19.0 months. The primary outcome was the recovery time for the one-leg heel-rise height (OHRH). Secondary outcomes included the time required to return to light exercise (LE) and the recovery times for the range of motion (ROM). Data regarding the surgical duration, complications, the visual analogue scale (VAS) score for pain, the Achilles tendon Total Rupture Score (ATRS), and the American Orthopaedic Foot and Ankle Society (AOFAS) Ankle-Hindfoot Scale score were also collected.
Results
The recovery times for OHRH, LE, and ROM were significantly shorter in groups A and B than in groups C and D (P < 0.001). The VAS scores decreased over time, reaching 0 in all groups by 10 weeks. The mean scores in groups A and B were higher than those in the other groups at 2 and 4 weeks (P < 0.001), whereas the opposite was true at 8 weeks (P < 0.001). ATRS and the AOFAS Ankle-Hindfoot scale score increased across all groups over time, showing significant between-group differences from weeks 6 to 16 (P < 0.001) and weeks 6 to 12 (P < 0.001). The mean scores were better in groups A and B than in groups C and D. Thirty-eight complications (3.5%) were observed, including 20 re-ruptures and 18 superficial infections. All complications were resolved at the last follow-up, with no significant between-group differences.
Conclusions
Immobilisation for 2 weeks after open surgery for ATR repair may be the optimal strategy for early rehabilitation with relatively minimal pain and other complications.
Trial registration
ClinicalTrials.gov (NCT04663542).
Keywords: Achilles tendon rupture, Immobilisation duration, Early functional mobilisation
Background
The Achilles tendon is a common tendon shared between the gastrocnemius and soleus muscles, and it is the strongest and thickest tendon in the human body [1–3]. However, with an increase in awareness regarding fitness, Achilles tendon rupture (ATR) has become a prevalent sports-related injury, particularly among older individuals, individuals with active lifestyles, and boys and men [4–8]. In the general population, ATR affects 8–18 per 100,000 people per year [9]. Patients with ATR may experience symptoms such as severe pain, inability to bear weight, and weakness in the acute phase, which can persist for over 10 years even permanently if left untreated [2, 9, 10]. Therefore, the management of acute ATR is crucial.
Some studies have reported that surgical and nonsurgical treatments for acute ATR have similar clinical outcomes [6, 11, 12]. However, conservative treatment can cause complications such as re-rupture, increased pain, and delayed return to work [13]. Previous meta-analyses [13–17] concluded that the re-rupture rate ranged from 2.3 to 3.7% in the surgical group and from 3.9 to 10.1% in the nonsurgical group. Therefore, surgical treatment has become the mainstay of therapy for acute ATR in recent decades [13].
Following standard surgical treatment, weight-bearing is frequently limited, and immobilisation with a brace for at least 6 weeks is often required [18]. Recent studies [1, 19–22] have reported that an aggressive rehabilitation program can be safely incorporated during the postoperative period and may offer short-term benefits over a more conservative rehabilitation protocol. Early weight-bearing and functional rehabilitation after surgical treatment of ATR have been advocated because they result in better ultimate functional outcomes [1, 19]. However, the optimal treatment and rehabilitation protocols for ATR remain debatable [22].
We believe that a combination of surgical suturing with early rehabilitation training is beneficial for the prognosis of ATR. Therefore, determination of the optimal duration of immobilisation after surgery is necessary. The aim of this study was to compare different immobilisation durations after open surgery for acute ATR.
Materials and methods
The study was reviewed and approved by our institutional review board (Peking University Third Hospital Medical Science Research Ethics Committee; IRB00006761-M2020315), and it has been registered at ClinicalTrials.gov (NCT04663542).
Design and population
This prospective cohort study enrolled 1219 patients who underwent surgical treatment for acute ATR at our university hospital from March 2019 to May 2023, and each patient provided written consent prior to their enrolment in the study. Among these patients, 131 were lost to follow-up, and 1088 patients (89.3%) were included in the final analysis. A radiologist conducted an ultrasound examination of the Achilles tendon preoperatively to confirm the diagnosis and detail the site and extent of the rupture. The inclusion criteria were as follows: (1) age of 18 to 60 years, (2) closed injury, (3) acute ATR (< 7 days since tendon rupture), and (4) ATR at a distance of > 3.5 cm from the tendon insertion point based on the ultrasound. The exclusion criteria were as follows: (1) partial ATR; (2) ATR at a distance of < 3.5 cm from the tendon insertion point based on the ultrasound.; and (3) diseases that may affect functional test results, such as diabetes, neuropathy, and autoimmune disease. The included patients were categorised into four groups (A, B, C, and D) according to the duration of immobilisation (0, 2, 4, and 6 weeks). All patients followed a similar rehabilitation protocol.
Surgical procedure
Patients were placed in the prone position and operated on under spinal anaesthesia using a tourniquet. The Achilles tendon resting angle (ATRA) on both sides was measured before disinfection. The ATRA is the angle between the long axis of the fibula and the line from the tip of the fibula to the head of the fifth metatarsal [23]. An incision was made posteromedial to the midline of the Achilles tendon at the level of the rupture in a longitudinal fashion, and the paratenon was divided to identify the rupture. With the ankle placed in a neutral position, the tendon was repaired using the Krackow locking loop technique with two W4843 (ETHIBOND of Johnson & Johnson, US) nonabsorbable sutures and the modified Kessler suture technique with two REF223114 (ORTHOCORD of Depuy Synthes, US) nonabsorbable sutures. The sutures were carefully placed away from the rupture site, and the tendon was sutured to a healthy tendon to enhance the stability of the repair (Fig. 1). Subsequently, six figure-eight sutures (four for the dorsal, two for the ventral) were placed with 2-0-gauge absorbable sutures to reinforce the broken ends. The ATRA on the affected side was measured again to determine whether the repair was suitable, and it was confirmed to be reduced and smaller than that on the contralateral leg. Following tension and strength testing of the ankle, the peritenon and subcutaneous tissues were approximated with 2-0-gauge and 3-0-gauge absorbable sutures, respectively, and the skin was closed with a skin stapler. Following wound binding, a below-knee brace with a wedge was applied with the ankle in 30 degrees plantar flexion position in all patients except those in Group A. All patients underwent surgery performed by the same surgeon using the same operative technique.
Fig. 1.
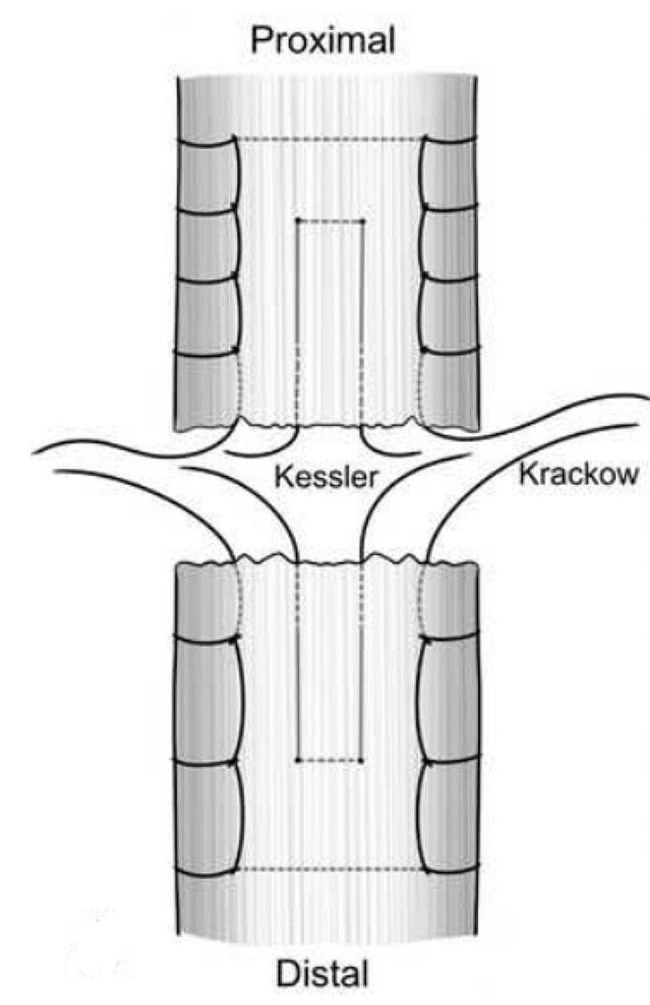
Diagram of our suture technique [24]
Postoperative rehabilitation
Group A included 98 (9.0%) patients without postoperative immobilisation. Group B comprised 439 patients (40.3%) with 2 weeks of postoperative immobilisation, Group C included 443 patients (40.7%) with 4 weeks of immobilisation, and Group D included 108 patients (9.9%) with 6 weeks of immobilisation. Patients in Group D underwent surgery first and were treated using the routine protocol. Subsequently, the duration of immobilisation was gradually reduced, and the patients in Group A were the last to undergo surgery.
All patients started postoperative exercise following the recommended rehabilitation protocol at different times (Table 1). In Group A, postoperative exercise commenced immediately, whereas patients in the other groups underwent rehabilitation exercises after the removal of the immobilisation brace. Professional physical therapy was not implemented during the rehabilitation process.
Table 1.
Rehabilitation Protocol
| After surgery | Postoperative exercise in Group A; Immobilisation with the brace for corresponding time in Group B, C and D |
|---|---|
| Immediately after removing the brace | Ankle mobilisation |
| 0–2 weeks after removing the brace | Standing up for 1 h per day |
| 2–4 weeks after removing the brace | Standing up for 2 h per day |
| Deep squat | |
| 4–6 weeks after removing the brace | Double-legged heel raises |
| Walking less than 1000 steps on flat ground | |
| 6–8 weeks after removing the brace | Single-legged heel raises |
| Walking less than 2000 steps on flat ground | |
| 2 weeks after successfully performing single-leg heel raises | Jogging |
| 4 weeks after successfully performing jogging | More vigorous training |
At 0–2 weeks after brace removal, patients were instructed to perform moderate plantar flexion and dorsiflexion of the ankle and stand up (partial weight-bearing) for 1 h every day. From 2 to 4 weeks after brace removal, ankle exercises remained consistent, with the standing time increased to 2 h per day. Simultaneously, the patients were instructed to perform deep squat exercises. Four to 6 weeks after brace removal, they were instructed to perform double-legged heel raises and walk fewer than 1000 steps on flat ground. Between 6 and 8 weeks after brace removal, the patients were advised to perform single-leg heel raises and limit walking to less than 2000 steps on flat ground. When the patients could successfully perform single-leg heel raises, they were instructed to jog 2 weeks later. Four weeks after successful performing jogging, the patients were allowed to perform more vigorous training. Double crutches were recommended to assist in training during the initial stages of the rehabilitation process.
Data collection
Patients attended follow-up visits at 2, 4, 6, 8, 10, 12, 14, and 16 weeks and at the final follow-up after surgery. During follow-up, all patients were evaluated by the same surgeon. The surgical duration and complications, such as superficial infection, re-rupture, and deep venous thrombosis (DVT), were recorded. The time to return to light exercise (LE), which included rapid walking and jogging, was noted. Dorsiflexion and plantar flexion were measured using a handheld goniometer. The heel-rise height was measured as the distance from the ground to the heel when the patient lifted the heel while keeping the knee straight. The recovery time for the range of motion (ROM) was recorded when it was similar to that for the contralateral leg. The recovery time for the one-leg heel-rise height (OHRH) was recorded when the heel-rise height index (HRHI = involved/uninvolved × 100) reached 50% [9]. The recovery times for OHRH was the primary endpoint, while the recovery times for ROM and the time to return to LE were the secondary outcomes. Clinical scores, including the visual analogue scale (VAS) score for pain, Achilles tendon Total Rupture Score (ATRS) [24], and American Orthopaedic Foot and Ankle Society (AOFAS) Ankle-Hindfoot Scale score [25], were also recorded to evaluate subjective pain and functional status. VAS measures pain on a 10-cm scale, with the status ranging from no pain (extreme left) to the worst possible pain (extreme right). The patients marked their current pain levels on the scale, and the score was accordingly recorded. The ATRS which was recorded after 6 weeks postoperatively was a patient-reported tool designed to measure the outcomes after acute ATR repair. The questionnaire comprises 10 questions to assess symptoms and the level of physical activity, with answers evaluated on an 11-point Likert scale (scores ranging from 0 to 10, with a maximum possible score of 100; higher scores indicate a better health status). The AOFAS Ankle-Hindfoot Scale which was recorded after 6 weeks postoperatively assigned a maximum score of 100 points (90–100 points, excellent; 75–89 points, good; 50–74 points, fair; and < 50 points, poor).
Statistical analysis
Statistical analyses were performed using SPSS version 25.0 (IBM Corp., Armonk, NY, USA). Data are reported as mean ± standard error of the mean unless otherwise noted. Differences in age, sex, body mass index (BMI), the distance from the rupture site to the Achilles tendon insertion site, the gap distance of the rupture site, and the surgical duration among the four groups were determined using one-way analysis of variance. Outcome parameters were examined using the Kruskal–Wallis H test, and complications were analysed using Fisher’s exact test. A P-value of < 0.05 was considered statistically significant.
Results
Group characteristics
In total, 1088 patients with unilateral complete ATR were included (1063 male and 25 female patients; mean age, 35.0 years, range, 18–60 years). Sports injuries, including basketball (479 patients, 44.0%), badminton (386 patients, 35.5%), soccer (95 patients, 8.7%), running (54 patients, 5.0%), and other sports (36 patients, 3.3%) injuries, were the causes of ATR in most patients (96.5%). There were no significant between-group differences in sex, age, BMI, surgical duration, distance from the rupture site to the Achilles tendon insertion site, and gap distance of the rupture site (Table 2).
Table 2.
Group characteristics
| Group A | Group B | Group C | Group D | Total | P value | |
|---|---|---|---|---|---|---|
| Number of Patients | 98 | 439 | 443 | 108 | 1088 | |
| Age | 33.9 ± 6.6 | 35.0 ± 5.9 | 35.1 ± 5.9 | 36.4 ± 5.6 | 35.0 ± 5.9 | 0.218 |
| Sex (Male/Female) | 92/6 | 430/9 | 436/7 | 105/3 | 1063/25 | |
| Body Mass Index | 24.7 ± 1.9 | 24.9 ± 1.8 | 24.8 ± 2.0 | 24.9 ± 1.9 | 24.8 ± 1.9 | 0.780 |
| Operation Time | 30.8 ± 3.9 | 31.4 ± 4.2 | 31.6 ± 4.7 | 30.6 ± 3.9 | 31.3 ± 4.3 | 0.121 |
| GDRS | 2.0 ± 0.9 | 2.1 ± 0.9 | 2.1 ± 1.0 | 2.0 ± 1.0 | 2.1 ± 1.0 | 0.425 |
| DRSTI | 4.4 ± 0.5 | 4.4 ± 0.6 | 4.4 ± 0.5 | 4.4 ± 0.5 | 4.4 ± 0.5 | 0.739 |
Data represent the mean [SD];
GDRS, gap distance of the rupture site; DRSTI, distance from the rupture site to the Achilles tendon insertion.
Recovery times
The mean recovery times for ROM were 6.2 ± 1.0, 6.4 ± 1.7, 8.7 ± 1.4, and 10.1 ± 0.5 weeks in groups A, B, C, and D, respectively. The mean recovery time for OHRH was 12.2 ± 1.4 weeks in group A, 12.3 ± 1.8 weeks in group B, 14.2 ± 1.4 weeks in group C, and 14.2 ± 0.8 weeks in group D. The mean time to return to LE was 18.1 ± 1.6, 18.2 ± 1.9, 19.8 ± 1.5, and 20.1 ± 1.2 weeks in groups A to D, respectively. Groups A and B showed significantly shorter recovery times for ROM, OHRH, and LE than did groups C and D (P < 0.001; Table 3).
Table 3.
Recovery Time
| Group A | Group B | Group C | Group D | P value | |
|---|---|---|---|---|---|
| (n = 98) | (n = 439) | (n = 443) | (n = 108) | ||
| ROM | 6.2 ± 1.0 | 6.4 ± 1.7 | 8.7 ± 1.4 | 10.1 ± 0.5 | < 0.001 |
| OHRH | 12.2 ± 1.4 | 12.3 ± 1.8 | 14.2 ± 1.4 | 14.2 ± 0.8 | < 0.001 |
| LE | 18.1 ± 1.6 | 18.2 ± 1.9 | 19.8 ± 1.5 | 20.1 ± 1.2 | < 0.001 |
Data represent the mean [SD];
LE, light exercise; OHRH, one-leg heel-rise height; ROM, range of motion.
Outcome scores
The VAS score for pain significantly decreased from 2 to 8 weeks, especially in Group A, and reached 0 in all four groups after 10 weeks. Significant differences were found among the four groups at 2 (P < 0.001, Group A differed from the other groups), 4 (P < 0.001, Group A differed from the other groups), and 8 (P < 0.001, groups A and B differed from the other groups) weeks. The mean scores in Groups A and B were higher than those in the other groups at 2 and 4 weeks, whereas the opposite was true at 8 weeks (Table 4). The mean ATRS in all groups increased over time. Significant differences were found among the 4 groups from weeks 6 to 16 (P < 0.001, Table 3), with the mean scores in groups A and B being higher than those in the other groups after 6 weeks. The ATRS in Group A significantly differed from the scores in Groups C and D at 6 weeks (P < 0.001); Groups B, C, and D at 8 weeks (P < 0.001); Groups B (P < 0.001), C (P = 0.001), and D (P < 0.001) at 10 weeks; Groups B, C, and D at 12 weeks (P < 0.001); Groups B and D at 14 weeks (P < 0.001); and Groups B, C, and D at 16 weeks (P < 0.001). The ATRS in Group B significantly differed from the scores in Groups C and D at 6 weeks (P < 0.001); and Groups A, B, and C at 8, 10, 12, 14, and 16 weeks (P < 0.001; Table 5). The mean AOFAS Ankle-Hindfoot Scale score increased over time in all groups, with significant differences observed among the four groups from weeks 6 to 12 (P < 0.001, Table 6). The mean scores in Groups A and B were higher than those in the other groups after 6 weeks. Moreover, the score in group A was significantly different from those in groups B, C, and D at 6, and 8 weeks (P < 0.001); groups B and D at 10 weeks (P < 0.001); and groups C and D at 12 weeks (P < 0.001). The score in Group B significantly differed from those in groups A, C, and D at 6, 8, and 10 weeks (P < 0.001); and groups C and D at 12 weeks (P < 0.001; Table 6). At the last follow-up, only the functional recovery of the patients was assessed. No outcome scores were obtained.
Table 4.
Visual analogue scale (VAS) for Pain
| Time (weeks) | Group A | Group B | Group C | Group D | P value |
|---|---|---|---|---|---|
| (n = 98) | (n = 439) | (n = 443) | (n = 108) | ||
| 2 | 5.0 ± 0.5 | 2.1 ± 1.0 | 1.7 ± 0.9 | 1.9 ± 0.6 | < 0.001 |
| 4 | 1.9 ± 0.8 | 0.9 ± 1.1 | 0.8 ± 0.6 | 0.9 ± 0.6 | < 0.001 |
| 6 | 0.2 ± 0.4 | 0.4 ± 0.9 | 0.3 ± 0.7 | 0.2 ± 0.6 | 0.531 |
| 8 | 0 | 0 | 0.2 ± 0.4 | 0.1 ± 0.3 | < 0.001 |
Data represent the mean [SD].
Table 5.
Achilles tendon total rupture score (ATRS)
| Time (weeks) | Group A | Group B | Group C | Group D | P value |
|---|---|---|---|---|---|
| (n = 98) | (n = 439) | (n = 443) | (n = 108) | ||
| 6 | 52.5 ± 1.8 | 50.5 ± 7.7 | 40.4 ± 4.0 | 18.9 ± 1.3 | < 0.001 |
| 8 | 66.7 ± 1.7 | 61.4 ± 5.9 | 51.5 ± 2.7 | 38.0 ± 2.3 | < 0.001 |
| 10 | 69.7 ± 1.5 | 73.0 ± 5.5 | 69.9 ± 5.9 | 61.1 ± 3.0 | < 0.001 |
| 12 | 75.6 ± 1.8 | 81.9 ± 5.0 | 77.4 ± 4.6 | 71.5 ± 2.6 | < 0.001 |
| 14 | 82.7 ± 1.6 | 85.9 ± 2.4 | 82.3 ± 2.8 | 78.4 ± 2.1 | < 0.001 |
| 16 | 87.3 ± 0.9 | 87.7 ± 1.1 | 85.8 ± 1.8 | 84.2 ± 1.4 | < 0.001 |
Data represent the mean [SD].
Table 6.
American Orthopaedic Foot and Ankle Society (AOFAS) hindfoot scores
| Time (weeks) | Group A | Group B | Group C | Group D | P value |
|---|---|---|---|---|---|
| (n = 98) | (n = 439) | (n = 443) | (n = 108) | ||
| 6 | 94.0 ± 1.5 | 90.9 ± 10.2 | 82.5 ± 5.8 | 72.9 ± 3.1 | < 0.001 |
| 8 | 94.3 ± 2.2 | 97.8 ± 4.8 | 89.2 ± 7.6 | 83.1 ± 1.3 | < 0.001 |
| 10 | 97.7 ± 1.8 | 99.3 ± 1.6 | 96.2 ± 5.5 | 96.0 ± 1.5 | < 0.001 |
| 12 | 99.6 ± 1.0 | 99.3 ± 1.6 | 98.1 ± 3.4 | 98.7 ± 1.0 | < 0.001 |
| 14 | 99.8 ± 1.0 | 99.3 ± 1.6 | 99.5 ± 1.4 | 99.7 ± 0.7 | 0.116 |
| 16 | 99.9 ± 0.4 | 99.7 ± 0.7 | 99.5 ± 1.4 | 99.7 ± 0.7 | 0.170 |
Data represent the mean [SD].
Complications
A total of 38 complications (38/1088, 3.5%) were observed in the study, including five (5/98, 5.1%) in Group A, 15 (15/439, 3.4%) in Group B, 15 (15/443, 3.4%) in Group C, and three (3/108, 2.8%) in Group D. Re-rupture (20 cases, 1.8%) occurred at 8 weeks after surgery (four in group A, eight in group B, and eight in group C; P = 0.190) and was diagnosed through clinical examination and a positive Thompson’s test. Superficial infections (18 cases, 1.7%) were observed across all groups (one in Group A, seven in Group B, seven in Group C, and three in Group D; P = 776). No significant differences in complications were found among the four groups (P = 0.816). At the last follow-up, all patients had recovered without complications (Table 7).
Table 7.
Complications
| Group A | Group B | Group C | Group D | Total | P value | |
|---|---|---|---|---|---|---|
| (n = 98) | (n = 439) | (n = 443) | (n = 108) | |||
| Superficial infection | 1(1.0%) | 7(1.6%) | 7(1.6%) | 3(2.8%) | 18(1.7%) | 0.776 |
| Re-rupture | 4(4.1%) | 8(1.8%) | 8(1.8%) | 0 | 20(1.8%) | 0.190 |
| Total | 5(5.1%) | 15(3.4%) | 15(3.4%) | 3(2.8%) | 38(3.5%) | 0.816 |
Discussion
ATR is an injury closely associated with sports-related activities, with 96.5% of patients in our study sustaining injuries during different sports activities. The most common activities, in decreasing order of frequency, included basketball (44.0%), badminton (35.5%), soccer (8.7%), running (5.0%), and others (3.3%), consistent with the findings from other studies [1, 26–28]. In the present study, there were 25 female patients (male-to-female ratio, 42.5:1); this sex distribution could be attributed to the preference for sports involving non-high-intensity physical activity, which are associated with lower ATR rates among girls and women. Sex could also independently contribute to the ATR pathogenesis [1]. Therefore, a large proportion of the patients in our study were young, active sportsmen; more research is needed to focus on patients with ATR who are not injured in sports.
Differences in surgical methods and surgeon experience result in varying immobilisation durations and early functional exercise schedules following open surgery for acute ATR. Traditional postoperative rehabilitation programs usually require a strict, non-weight-bearing plantar flexion cast for 6 weeks. In China, there are no professional physical therapists to guide postoperative rehabilitation exercises. Therefore, the surgeon’s rehabilitation protocol tends to be more conservative (e.g., immobilisation for 8–12 weeks). However, recent studies indicated that appropriately shortening the immobilisation duration and early functional exercise can enhance postoperative rehabilitation. Multiple studies [10, 29, 30] have compared early functional rehabilitation with immobilisation. Okoroha et al. [29] reported that a shortened immobilisation duration after open surgery for acute ATR can improve the ankle joint range of motion, reduce complications, and enhance postoperative recovery without causing increased tension or excessive elongation of the Achilles tendon tissue. Groetelaers et al. [30] performed minimally invasive ATR repair and demonstrated that early mobilisation appears to be as safe as traditional postoperative immobilisation, with equal patient satisfaction and fewer major complications.
In the present study, although patients received the same protocols after the removal of the immobilisation brace, the timing of successful single-legged heel raises varied. Therefore, some patients may experience faster or slower recovery. In group A, patients were instructed to perform moderate plantar flexion and dorsiflexion of the ankle and partial weight-bearing while standing immediately after surgery. In the early stage, ankle function recovered more rapidly in Group A than in the other groups. However, Group A had a higher VAS score for pain and Achilles tendon re-rupture rate than did the other groups. In contrast, patients in Group B recovered faster and experienced less pain than those in the other groups. These results indicated that a 2-week immobilisation period was the best choice after open surgery for ATR.
The complication rate was the highest in group A (5/98, 5.1%). However, there were no significant differences in complications among the four groups. A possible reason for this is the insufficient sample size for Group A. Given the higher incidence of complications and more pain in Group A, we no longer recommend immediate postoperative brace removal.
One of the most important aspects of ATR treatment is the incidence of re-rupture. A review investigating surgical interventions for acute ATR reported re-rupture rates of 0–12% [31]. Comparatively, our study reported a relatively low re-rupture rate of 1.8% (20/1088). Strong fixation for ATR using the Krackow locking loop technique combined with modified Kessler sutures is the premise for early postoperative rehabilitation exercises. Patients can perform adequate early weight-bearing and functional exercises after surgery. Consequently, the possibility of re-rupture also increases. Re-rupture in all 20 patients in the present study occurred during a fall or a similar sudden trauma rather than during regular rehabilitation exercises. The patients experienced re-rupture because of uncontrolled dorsiflexion without brace protection. Therefore, we recommend wearing walking boots if patients want to walk long distances after brace removal.
This study had certain limitations. First, most patients were boys or men, and this may have resulted in a potential sex-related bias. Second, this was a large, single-centre cohort study, and the immobilisation duration for each patient was selected in chronological order rather than random order. Therefore, multicentre, prospective randomised controlled trials are required to verify our conclusions. Third, the clinical scores in this study, such as the VAS score, ATRS, and AOFAS Ankle-Hindfoot Scale score, have subjective components that may lead to errors. Thus, more objective and high-quality questionnaires are required to evaluate patient recovery after open surgery for ATR repair. Fourth, we lacked information about the long-term status of patients after surgery, and studies with extended follow-up periods are required. Finally, our study did not focus much on the elongation of the Achilles tendon during the follow-up, which needs more attention in future studies.
Conclusion
Immobilisation for 2 weeks after open surgery for ATR may be the optimal strategy for early rehabilitation with relatively minimal pain and other complications.
Acknowledgements
Not applicable.
Abbreviations
- ATR
Achilles tendon rupture
- ATRS
Achilles tendon Total Rupture Score
- AOFAS
American Orthopaedic Foot and Ankle Society
- BMI
Body mass index
- DVT
Deep venous thrombosis
- LE
Light exercise
- OHRH
One-leg heel-rise height
- ROM
Range of motion
- ATRA
Achilles tendon resting angle
- OHRH
One-leg heel-rise height
- VAS
Visual analogue pain scale
- VAS
Visual analogue scale
Author contributions
YC, SG, ZC, YF, LB, GS, JF, YL and FZ were all involved with the conception and design of the study, acquisition of data, analysis and interpretation of data, and drafting and revision of the article. All authors read and approved the final manuscript.
Funding
This work was supported by the Capital Health Development Research Project (No. 2022-2-4096).
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
This study was reviewed and approved by the institutional review board of Peking University Third Hospital Medical Science Research Ethics Committee (IRB00006761-M2020315), and it has been registered at ClinicalTrials.gov (NCT04663542).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Yang Lv, Email: lvyang42@126.com.
Fang Zhou, Email: zhouf@bjmu.edu.cn.
References
- 1.Tarantino D, Palermi S, Sirico F, et al. Achilles Tendon rupture: mechanisms of Injury, principles of Rehabilitation and Return to play. J Funct Morphol Kinesiol. 2020;5(4):95. 10.3390/jfmk5040095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dams OC, van den Akker-Scheek I, Diercks RL, et al. The recovery after Achilles tendon rupture: a protocol for a multicenter prospective cohort study. BMC Musculoskelet Disord. 2019;20(1):69. 10.1186/s12891-019-2437-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maffulli N. Current concepts in the management of subcutaneous tears of the Achilles tendon. Bull Hosp Jt Dis. 1998;57(3):152–8. [PubMed] [Google Scholar]
- 4.Maffulli N, Irwin AS, Kenward MG, et al. Achilles tendon rupture and sciatica: a possible correlation. Br J Sports Med. 1998;32(2):174–7. 10.1136/bjsm.32.2.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Noback PC, Jang ES, Cuellar DO, et al. Risk factors for achilles tendon rupture: a matched case control study. Injury. 2017;48(10):2342–7. 10.1016/j.injury.2017.08.050. [DOI] [PubMed] [Google Scholar]
- 6.Myhrvold SB, Brouwer EF, Andresen TKM, et al. Nonoperative or Surgical Treatment of Acute Achilles’ Tendon rupture. N Engl J Med. 2022;386(15):1409–20. 10.1056/NEJMoa2108447. [DOI] [PubMed] [Google Scholar]
- 7.Glazebrook M, Rubinger D. Functional Rehabilitation for Nonsurgical Treatment of Acute Achilles Tendon rupture. Foot Ankle Clin. 2019;24(3):387–98. 10.1016/j.fcl.2019.05.001. [DOI] [PubMed] [Google Scholar]
- 8.Gajhede-Knudsen M, Ekstrand J, Magnusson H, et al. Recurrence of Achilles tendon injuries in elite male football players is more common after early return to play: an 11-year follow-up of the UEFA Champions League injury study. Br J Sports Med. 2013;47(12):763–8. 10.1136/bjsports-2013-092271. [DOI] [PubMed] [Google Scholar]
- 9.Mansfield K, Dopke K, Koroneos Z, et al. Achilles Tendon Ruptures and repair in Athletes-a review of sports-related Achilles injuries and return to play. Curr Rev Musculoskelet Med. 2022;15(5):353–61. 10.1007/s12178-022-09774-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lantto I, Heikkinen J, Flinkkila T, et al. Early functional treatment versus cast immobilization in tension after achilles rupture repair: results of a prospective randomized trial with 10 or more years of follow-up. Am J Sports Med. 2015;43(9):2302–9. 10.1177/0363546515591267. [DOI] [PubMed] [Google Scholar]
- 11.Lantto I, Heikkinen J, Flinkkila T, et al. A prospective randomized trial comparing Surgical and nonsurgical treatments of Acute Achilles Tendon ruptures. Am J Sports Med. 2016;44(9):2406–14. 10.1177/0363546516651060. [DOI] [PubMed] [Google Scholar]
- 12.Renninger CH, Kuhn K, Fellars T, et al. Operative and Nonoperative Management of Achilles Tendon Ruptures in active Duty Military Population. Foot Ankle Int. 2016;37(3):269–73. 10.1177/1071100715615322. [DOI] [PubMed] [Google Scholar]
- 13.Deng S, Sun Z, Zhang C, et al. Surgical Treatment Versus Conservative Management for Acute Achilles T Endon rupture: a systematic review and Meta-analysis of Randomized controlled trials. J Foot Ankle Surg. 2017;56(6):1236–43. 10.1053/j.jfas.2017.05.036. [DOI] [PubMed] [Google Scholar]
- 14.Zhao JG, Meng XH, Liu L, et al. Early functional rehabilitation versus traditional immobilization for surgical Achilles tendon repair after acute rupture: a systematic review of overlapping meta-analyses. Sci Rep. 2017;7:39871. 10.1038/srep39871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ochen Y, Beks RB, van Heijl M, et al. Operative treatment versus nonoperative treatment of Achilles tendon ruptures: systematic review and meta-analysis. BMJ. 2019;364:k5120. 10.1136/bmj.k5120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reda Y, Farouk A, Abdelmonem I, et al. Surgical versus non-surgical treatment for acute Achilles’ tendon rupture. A systematic review of literature and meta-analysis. Foot Ankle Surg. 2020;26(3):280–8. 10.1016/j.fas.2019.03.010. [DOI] [PubMed] [Google Scholar]
- 17.McCormack R, Bovard J. Early functional rehabilitation or cast immobilisation for the postoperative management of acute Achilles tendon rupture? A systematic review and meta-analysis of randomised controlled trials. Br J Sports Med. 2015;49(20):1329–35. 10.1136/bjsports-2015-094935. [DOI] [PubMed] [Google Scholar]
- 18.Carter TR, Fowler PJ, Blokker C. Functional postoperative treatment of Achilles tendon repair. Am J Sports Med. 1992;20(4):459–62. 10.1177/036354659202000417. [DOI] [PubMed] [Google Scholar]
- 19.Kim U, Choi YS, Jang GC, et al. Early rehabilitation after open repair for patients with a rupture of the Achilles tendon. Injury. 2017;48(7):1710–3. 10.1016/j.injury.2017.04.050. [DOI] [PubMed] [Google Scholar]
- 20.Gould HP, Bano JM, Akman JL, et al. Postoperative Rehabilitation following Achilles Tendon Repair: a systematic review. Sports Med Arthrosc Rev. 2021;29(2):130–45. 10.1097/JSA.0000000000000309. [DOI] [PubMed] [Google Scholar]
- 21.Lu J, Liang X, Ma Q. Early functional Rehabilitation for Acute Achilles Tendon ruptures: an Update Meta-Analysis of Randomized controlled trials. J Foot Ankle Surg. 2019;58(5):938–45. 10.1053/j.jfas.2018.12.014. [DOI] [PubMed] [Google Scholar]
- 22.Saxena A, Giai Via A, Grävare Silbernagel K, et al. Current Consensus for Rehabilitation Protocols of the surgically repaired Acute Mid-substance Achilles rupture: a systematic review and recommendations from the GAIT Study Group. J Foot Ankle Surg. 2022;61(4):855–61. 10.1053/j.jfas.2021.12.008. [DOI] [PubMed] [Google Scholar]
- 23.Carmont MR, Grävare Silbernagel K, Brorsson A, et al. The Achilles tendon resting angle as an indirect measure of Achilles tendon length following rupture, repair, and rehabilitation. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2015;2(2):49–55. 10.1016/j.asmart.2014.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nilsson-Helander K, Thomeé R, Silbernagel KG, et al. The Achilles tendon total rupture score (ATRS): development and validation. Am J Sports Med. 2007;35(3):421–6. 10.1177/0363546506294856. [DOI] [PubMed] [Google Scholar]
- 25.Kitaoka HB, Alexander IJ, Adelaar RS, et al. Clinical Rating systems for the Ankle-Hindfoot, midfoot, Hallux, and lesser toes. Foot Ankle Int. 1997;18(3):187–8. 10.1177/107110079701800315. [DOI] [PubMed] [Google Scholar]
- 26.Campillo-Recio D, Comas-Aguilar M, Ibáñez M, et al. Percutaneous Achilles tendon repair with absorbable suture: outcomes and complications. Rev Esp Cir Ortop Traumatol. 2023;67(1):T56–61. 10.1016/j.recot.2022.10.014. [DOI] [PubMed] [Google Scholar]
- 27.Xu XY, Gao S, Lv Y, et al. Duration of immobilisation after Achilles tendon rupture repair by open surgery: a retrospective cohort study. J Orthop Surg Res. 2021;16(1):196. 10.1186/s13018-021-02342-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Godoy-Santos AL, Bruschini H, Cury J, et al. Fluoroquinolones and the risk of Achilles Tendon disorders: Update on a neglected complication. Urology. 2018;113:20–5. 10.1016/j.urology.2017.10.017. [DOI] [PubMed] [Google Scholar]
- 29.Okoroha KR, Ussef N, Jildeh TR, et al. Comparison of tendon lengthening with traditional versus accelerated rehabilitation after achilles tendon repair: a prospective randomized controlled trial. Am J Sports Med. 2020;48(7):1720–6. 10.1177/0363546520909389. [DOI] [PubMed] [Google Scholar]
- 30.Groetelaers RP, Janssen L, van der Velden J, et al. Functional treatment or cast immobilization after minimally invasive repair of an Acute Achilles Tendon rupture: prospective, randomized trial. Foot Ankle Int. 2014;35(8):771–8. 10.1177/1071100714536167. [DOI] [PubMed] [Google Scholar]
- 31.Khan RJ, Carey Smith RL. Surgical interventions for treating acute Achilles tendon ruptures. Cochrane Database Syst Rev. 2010;9CD003674. 10.1002/14651858.CD003674.pub4. Published 2010 Sep 8. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.


