Abstract
Background
An mHealth-based school health education platform (EduSaltS) was promoted in real-world China to reduce salt intake among children and their families. This progress evaluation explores its implementation process and influencing factors using mixed methods.
Methods
The mixed-methods process evaluation employed the RE-AIM framework. Quantitative data were collected from a management website monitoring 54,435 third-grade students across two cities. Questionnaire surveys (n = 27,542) assessed pre- and post-education effectiveness. Mixed-effects models were used to control cluster effects. Qualitative interviews (23 individuals and 8 focus groups) identified program performance, facilitators, and barriers. Findings were triangulated using the RE-AIM framework.
Results
The program achieved 100% participation among all the third-grade classes of the 208 invited primary schools, with a 97.7% registration rate among all the 54,435 families, indicating high "Reach." Qualitative interviews revealed positive engagement from children and parents through the "small hands leading big hands" strategy. The high completion rate of 84.9% for each health cloud lesson and the significant improvement in salt reduction knowledge and behaviors scores from 75.0 (95%CI: 74.7–75.3) to 80.9 (95%CI: 80.6–81.2) out of 100 demonstrated the "Effect" of EduSaltS. The program's "Adoption" and "Implementation" were supported by attractive materials, reduced workload via auto-delivered lessons/activities and performance evaluation, and high fidelity to recommended activities, with medians 3.0 (IQR: 2.0–8.0)/class and 9.0 (IQR: 5.0–14.0)/school. Stable course completion rates (79.4%-93.4%) over one year indicated promising "Maintenance." Apart from the facilitating features praised by the interviewees, government support was the basis for the scaling up of EduSaltS. Barriers included the lack of smartphone skills among some parents and competing priorities for schools. Unhealthy off-campus environments, such as excessive use of salt in pre-packaged and restaurant foods, also hindered salt reduction efforts. The program's scalability was evident through its integration into existing health education, engagement of local governments and adaptation across various mobile devices.
Conclusions
The mHealth-based school health education program is scalable and effective for public salt reduction in China. Identified barriers and facilitators can inform future health program scale-ups. The program's successful implementation demonstrates its potential for broader application in public health initiatives aimed at reducing dietary salt intake.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-024-19732-y.
Keywords: RE-AIM model, Mixed qualitative and quantitative methods, Process evaluation, Salt reduction, School health education, Scaling-up program, MHealth
Background
Excessive salt consumption increases the risk of hypertension and is linked to cardiovascular disease, a leading cause of global annual deaths [1]. Reducing population salt intake is one of the most cost-effective measures for mitigating the burden of noncommunicable diseases (NCDs) and is thus a health priority worldwide [2]. Various measures such as reducing salt content in processed food, educating consumers, implementing clear labelling, and imposing salt taxes, have been adopted by many national salt reduction initiatives [3]. High-income countries typically opt for structural or regulatory approaches, whereas low- and middle-income countries focus on changing consumer salt habits or substituting salt with alternatives, particularly for discretionary salt intake from cooking and table salt [4, 5]. These interventions have been implemented in workplaces, fast-food outlets, hospitals, government offices, and various settings, with a significant emphasis on schools and college [6].
In the past four decades, the Chinese salt consumption was nearly twice the World Health Organization’s recommendation [7], with a high-salt diet being the primary dietary contributor to deaths and disability-adjusted life years (DALYs) [8]. Hence, reducing salt consumption is crucial to mitigate salt-related health impacts [9]. China launched a national salt reduction campaign employing traditional strategies like food labelling, salt-restriction spoons, reduced condiment usage in cooking, and decreased intake of pickled foods [9–12]. However, the impact assessment revealed that these measures fell short of China's national target of a 20% salt reduction by 2030 [12].
Innovations in the delivering methods might be needed to further improve the effectiveness and scalability of such approaches. One well-recognized strategy involves school-based health education to enhance children's health behaviors and overall family well-being, as supported by a growing body of research [13, 14]. In China, the School-EduSalt program implemented this strategy through a "small hands leading big hands" approach, successfully decreasing salt intake in children and their families while also lowering blood pressure in adults [15]. A critical consideration is the scalability of such programs and how to expand them in real-world settings to reach a larger and more diverse population. One approach has been the adoption of mobile health (mHealth) technology, offering standardized online health courses for salt reduction. An mHealth-based school health education initiative in China (AppSalt), incorporating both online and offline activities, effectively reduced salt intake among children's parents, as evidenced by a cluster randomized controlled trial (cRCT) study [16, 17].
Based on the successes of School-EduSalt and AppSalt, the aspiration to extend salt reduction efforts to a larger population was explored through a scaling-up initiative known as EduSaltS [18]. The program was implemented in the third-grade students from 2021 in Zhenjiang and Ganzhou cities over the course of one school year (2 school terms), aiming to translate the evidence-based interventions into practical applications on a broader scale to foster overall health enhancements [19]. But due to practical constraints, limited resources and implementation capabilities, challenges in scalability and sustainability are frequently quoted by current evidence body, and the effects of health intervention are usually faded in the scale-up program, if compared with experimental trials [20]. The phenomenon is named as “scale up penalty” mainly attributed to implementation bias [21].
This process evaluation aims to assess the implementation performance of EduSaltS in the real-world and identify the factors that may hinder or facilitate the implementation, thereby offer insights to enhance its implementation in a larger scale.
Methods
Health education activities
EduSaltS is an innovative health education system targeting on primary school student, comprising a WeChat-based education platform (Health Cloud Classroom), a WeChat management terminal (EduSaltS Manager) and a management website (EduSaltS Management Website). The Health Cloud Classroom has 20 auto delivered health cartoon video courses, and other online activities such as knowledge competition and self-learning health materials, and a self-report questionnaire to evaluate knowledge- and behavior-related salt reduction. On-campus offline activities include health lessons, thematic activities, environment building and competition and rewards. The management website tracks real-time data on student performance in activities and the progress of school education activities. For further details on the EduSaltS program, refer to the published proposal [18].
Process evaluation
RE-AIM model using mixed methods
As EduSaltS was implemented across various cities with comprehensive online and offline educational strategies, a process evaluation solely employing quantitative or qualitative methods may not fully achieve the desired breadth and depth of understanding and corroboration. Therefore, mixed methods were used to evaluate the EduSaltS [22]. This study utilized the RE-AIM framework as the theoretical model for evaluation, which is widely accepted and offers comprehensive insights for the process evaluation [23–26]. Based on the five dimensions of the RE-AIM model—Reach, Effectiveness, Adoption, Implementation, and Maintenance—the evaluation diagram and contents were developed (Table 1). The StaRI checklist for implementation research [27] and GRAMMS checklist for mixed methods study [28] were used to secure scientific rigor and reporting.
Table 1.
Mixed methods RE-AIM evaluation framework
| RE-AIM domains | Themes | Quantitative methods | Qualitative methods |
|---|---|---|---|
| Reach | Extent to which individuals accepted the program | Proportion and Characteristics of the students participated in the program |
Approach of recruitment and registration; Factors that facilitate or hinder the enrolment |
| Effectiveness | Health outcomes | Positive and negative health outcomes before and after the education |
Improvement of students’ and salt-reduction behavior; Change of families’ salt consumption; Factors affect the students’ behavior change |
| Adoption | Organization adopting the program | Proportion of schools adopting EduSaltS; |
Adoption strategies; Launching activities; Needs and requirements of adopting the school salt reduction; Reasons for not adopting EduSaltS |
| Implementation | Degree to which the intervention activities were carried out as planned | Extent to which the students attended and/or completed online and offline activities |
How students completed the health activities on schedule; Roles of family and school during implementation; How Efficient the mHealth measures were; Influential issues in individual, family, school, and wider community for students to achieve the expected implementation; |
| Maintenance | Likelihood of sustained program implementation at both the individual and organizational levels |
Trends of completion rates from the first lesson to the final one; Extent to which the efforts were made by governmental administration |
Factors may hinder students’ capability to maintain the health effects after the completion of EduSaltS; Opportunity and challenging issues for possibly scaling-up the program to larger population and settings |
Participants
The quantitative analyses were based on the 54,435 third-grade students who participated in the education course as well as the27,542 students who completed the pre- and post-education self-report questionnaires. For the qualitative study, twenty-three informants were interviewed, comprising 4 health experts from the CDC, 6 government officials, 6 principals, and 7 headteachers. Eight focus groups were held involving 40 students and 40 parents, with 10 participants in each group. Table 2 shows the specific characteristics of the participants. During the real-world implementation of the EduSaltS, no demographic information was collected for the students and their families including the gender of the students.
Table 2.
Participant characteristics in the mixed methods evaluation
| Quantitative methods | Qualitative methods | |||
|---|---|---|---|---|
| Participants in education activities | Self-report questionnaire investigation | Individual interview | Focus group | |
| Sample size | 54435 | 27542 | 23 | 80 |
| Gender | ||||
| Female | Not collected | Not collected | 16 | 40 |
| Male | 7 | 40 | ||
| Province, City | ||||
| Jiangxi, Ganzhou | 34662 | 15928 | 11 | 40 |
| Jiangsu, Zhenjiang | 19773 | 11614 | 12 | 40 |
| Role | ||||
| CDC health expert | - | - | 4 | - |
| Government official | - | - | 6 | - |
| Principal | - | - | 6 | - |
| Headteacher | - | - | 7 | - |
| Parent | - | - | 40, 4 groups | |
| Student | 54435 | 27542 | 40, 4 groups | |
| Program period | Nov 2021 to Jul 2022 and Oct 2022 to Jul 2023 | Oct 2022 to Jul 2023 | Nov 2021 to Jul 2022 and Oct 2022 to Jul 2023 | Oct 2022 to Jul 2023 |
Quantitative data collection and analysis
To quantitatively analyze the participation, program adoption, implementation and maintenance, quantitative data (retrieved date 09/Jul/2023) were collected from the EduSaltS Management Website. Additionally, a self-report questionnaire embedded in the "Health Cloud Classroom" was employed to evaluate educational effects before and after the program (Supplementary material, additional file 1). Standard knowledge and practice scores out of 100 were used to measure overall knowledge and practice enhancement. The relevant statistical indicators were calculated as the following equations:
, where the score for a single choice question was assigned 100 for correct answer and 0 for the incorrect, while the score for a multi-choice practice question was assigned 100 for the best behavior and 0 for the poorest, and an interval score
Activity score: automatically calculated by and retrieved from the management website.
N of governmental administration activities: automatically summarized by the management website.
Numeric data, including activity scores and the number of activities, were presented using frequency, median and Interquartile Range, or mean and 95% confidence intervals. Analysis of variance was employed to assess statistical differences in the data. Categorical data were described in terms of frequency and percentage, with statistical differences tested using chi-squared tests. The before-after effects were estimated via mixed-effects models with adjustment for clusters, i.e. class nested within school, and school within district. SAS Enterprise Guide 8.3 was utilized for data cleaning, management, and quantitative analysis.
Qualitative data collection and analysis
Qualitative research was carried out through individual face-to-face interviews and focus groups from May to Jun of 2023 right after the completion of the education courses delivered via the EduSaltS platform. Purposive sampling was employed to select CDC health experts, government officials, school principals, and headteachers for individual interviews (n = 23), while students and parents were targeted for focus group discussions (n = 80, divided into eight groups).
Individual interviews primarily delved into the facilitators and barriers encountered during project implementation, as well as elicited suggestions for addressing them. The group interviews aimed to gather insights on participants' experiences, health benefits gained, and challenges faced throughout the project. The semi structured interview outlines have been presented in the published proposal [18].
The interviews took place before the project ends in each city. Individual face-to-face interviews were conducted with one researcher leading the session, while another researcher recorded key points shared by the participants. On average, individual interviews lasted 30 min (ranging from 25 to 40 min).
Focus groups were facilitated by one researcher leading the discussion, with another researcher recording key points and overseeing the process. These focus group sessions lasted an average of 50 min (ranging from 45 to 60 min). All interviews were audio-recorded and transcribed into text for analysis.
Researchers employed thematic analysis to code crucial information from the transcripts based on the five domains of the RE-AIM framework [29]. Key points and relevant perceptions related to the research questions were coded and organized within the analysis framework. The coded key information was then summarized to develop research themes, which were examined as research findings [30]. The analysis process and results were deliberated and reviewed by an expert panel to secure research quality. Qualitative data analysis was carried out using NVivo Release 1.7.1.
Integration of qualitative and quantitative data analysis
The integration of qualitative and quantitative data used a triangulation protocol for mixed methods research [31]. Initially, the data were analyzed separately as described above and then integrated to identify similarities, inconsistencies or mutual remedies in the findings. The triangulation of the results was presented at the theme level by cross-referencing the qualitative and quantitative results [32]. Eventually, comprehensive arguments were presented according to RE-AIM domains, which not only showed program implementation performance, but also demonstrated the facilitators and barriers.
Results
Reach - student enrolment
A total of 54,435 students registered in this health education program, representing 97.7% of all third-grade students (55,715) across all the 1,260 classes of 208 schools selected by region from the participating cites. Parents demonstrated a willingness to participate in school-organized health activities, expressing trust in schools' ability to enhance their children's health. They also acknowledged successful registration in the "Health Cloud Classroom" under the supervision of headteachers (Parent, Mingzhu Primary School): “Because this is a school project, we were glad to participate in. The headteachers contacted me through a WeChat group. They guided us to register a mobile application.” During the registration, a small number of students encountered challenges due to (Principal, Henshun Primary School, Zhenjiang): “parents’ lack of primary skills to operate applications on mobiles,” which potentially hindered the program from reaching all the students and their families through the mHealth approach.
Effectiveness - knowledge and practice improvement
As depicted in Table 3, the questionnaire results revealed a pre-post rise in awareness of salt reduction knowledge and the adoption of healthy behaviors. The standard scores for all knowledge and practice inquiries increased from 75.0 (95% CI: 74.7–75.3) to 80.9 (95% CI: 80.6–81.2).
Table 3.
Salt-reduction knowledge awareness, practice, and standard scores before and after education by the self-report questionnaire investigation
| Before* | After* | |
|---|---|---|
| Awareness rate of health knowledge (%, 95%CI) | ||
| Recommendation of salt for adults less than 5 g/day | 35.0 (34.3–35.8) | 48.6 (47.8–49.4) |
| The primary component of salt is sodium chloride | 84.5 (83.0–85.9) | 89.8 (88.7–90.8) |
| Significant cause of hypertension is salt | 86.6 (86.0–87.1) | 89.6 (89.2–90.1) |
| Sichuan pepper contains the lowest sodium than soy sauce, bean sauce, monosodium glutamate | 85.4 (84.5–86.2) | 93.2 (92.7–93.6) |
| Even if blood pressure is normal, it is necessary to reduce salt intake | 84.5 (83.5–85.5) | 91.2 (90.5–91.8) |
| Sodium content on nutrition label shows the salt content in food | 82.9 (81.3–84.4) | 89.5 (88.4–90.5) |
| Choose the lowest salt food among four options by analyzing the sodium content in 100 g food | 53.5 (52.5–54.6) | 58.4 (57.3–59.4) |
| Adoption rate of health behavior (%, 95%CI) | ||
| Choose low or reduced-salt meals | 34.9 (34.2–35.6) | 45.2 (44.5–45.9) |
| Consume salty snacks less than once a week | 71.0 (69.7–72.3) | 72.5 (71.2–73.7) |
| Choose healthy snacks after checking nutrition board | 88.8 (87.5–90) | 93.4 (92.5–94.2) |
| Standard scores of knowledge and practice (Mean, 95%CI) | ||
| In total | 75.0 (74.7–75.3) | 80.9 (80.6–81.2) |
| Knowledge awareness | 72.5 (72.1–72.9) | 79.4 (78.9–79.8) |
| Health practice adoption | 79.4 (79.1–79.7) | 83.5 (83.3–83.8) |
*Results have been adjusted because of the clusters, class level, which is nested within school, which in turn is nested within district
Parents shared insights on their children's enhanced health behaviors, noting that they were more attentive to nutrition labels when purchasing food and beverages, opting for healthier choices. Some students also disseminated health information from EduSaltS to their family members, including elderly relatives who typically contend with noncommunicable diseases, to promote salt reduction (Parent, Mingzhu Primary School, Zhenjiang): “My son frequently checks nutrition labels and informs me about salt content. My child consistently reminds his grandmother to use less salt while cooking."
Parents affirmed the health benefits because of this program in their family. They developed cooking skills aimed at reducing salt and progressively reduced their intake of salted vegetables, a common dietary practice in their communities (Parent, Tianzhushan Primary School, Zhenjiang): “Before this project, I used to put much salt and soy sauce while stir-frying vegetables, but now I put just a little when cooking almost done. I use garlic instead of salt to increase taste.”
Furthermore, the entire family changed their dietary practices to reduce salt intake (Parent, Mingzhu Primary School): “We used to eat out often on Sundays, but now we eat out less frequently and order takeaway less."
The barrier to achieving greater salt reduction effects was the adverse influence of unhealthy off-campus environments. Convenience stores and restaurants around schools are major sources of salt intake for students (Principal, Henshun primary school, Zhenjiang): “In accordance with certain regulations, our schools no longer host on-campus stores, although such stores still operate in the surrounding areas. Furthermore, advertisements in the broader community entice students to consume heavily processed foods, particularly during their commute between home and school.”
School adoption and participation
Totally, 100% invited schools (208) agreed to participate in the health education program after a formal introduction meeting convened by local education bureaus, which was essential for program adoption. Furthermore, the informant emphasized that health needs pushed invited school adopted the education (Official, Danyang Education Bureau, Zhenjiang): “the accumulation of health issues among students exerted considerable pressure on school health, urging schools to actively take health actions.” Meanwhile, School health education was highlighted by national health policies (Health expert, Zhenjiang CDC, Zhenjiang): “The Opinions on Comprehensive Improvement of School Health and Health Education in the New Era, issued by Department of Education, advocated widening channels and innovatively integrating Internet technologies into health education.” This policy perfectly resonated with the intervention measures employed by the EduSaltS.
Schools need to improve students’ health, but the challenge is prioritizing health issues among students. Notably, during the COVID-19 pandemic, schools experienced lockdowns, and more attention was given to mitigating infection risks (Principal, Hengshun Primary School, Zhenjiang): “Schools hesitated to adopt EduSaltS to reduce salt intake at the initiative period, which seems not directly relevant to the pandemic response.”
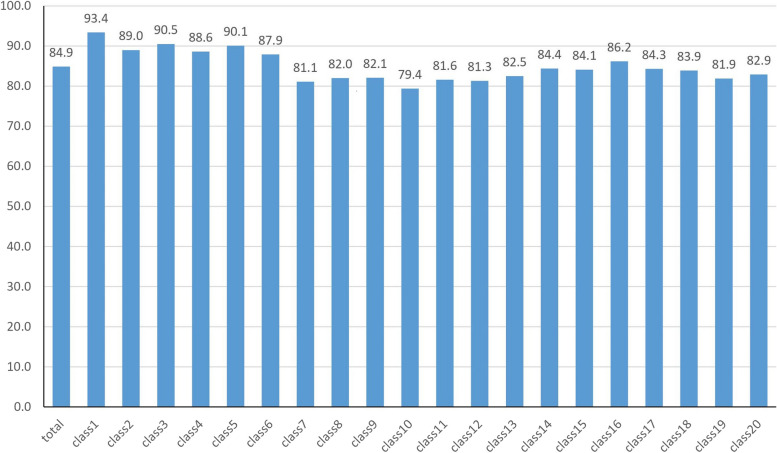
Implementation
The school effectively executed a variety of health activities proposed by the EduSaltS with a high degree of fidelity. For students, average completion rate of the 20 health cloud courses was 84.9%, and the rates fluctuated between 79.4% and 93.4% (Fig. 1). The participation rate for optional online activities, such as knowledge competition was 57.6%, and that for health materials self-learning was 81.1% (Table 4).
Fig. 1.
Completion rate of health cloud classes
Table 4.
Individual online activities
| Completion rate of each health cloud course (%) | 79.4 to 93.4 |
| Completion rate of 20 per course per student (%) | 84.9 |
| Completion rate of at least one salt-reduction course (%) | 99.4 |
| Completion rate of at least 4 salt-reduction courses (%) | 93.4 |
| Completion rate of all 8 salt-reduction courses (%) | 55.0 |
| Utilization rate of knowledge competition (%) | 57.6 |
| Adoption rate of health materials self-learning (%) | 81.1 |
| Activity score (mean, 95%CI) | 2353.6 (2343.5–2363.7) |
| Online activity score (mean, 95%CI) | 1790.5 (1784.9–1796.0) |
The average health activity score was 2353.6 (95% CI: 2343.5–2373.7). Online health activities played a predominant role, and the average score was 1790.5 (95% CI: 1784.9–1796.0).
In total, 1800 school activities were conducted by 162 schools, with a median of 9.0, and 3999 class activities were conducted, with a median of 3.0 (Table 5). The results show that the required activities were more than optional activities at either the school or class level.
Table 5.
Offline health activities
| N of schools or classes | N of Activities | Median | Interquartile Range | |
|---|---|---|---|---|
| School level activity | 162 | 1800 | 9.0 | 5.0–14.0 |
| Health theme activities (Required) | 155 | 417 | 2.0 | 1.0–3.0 |
| Putting up posters (Required) | 151 | 724 | 5.0 | 3.0–6.0 |
| Canteen chef health education (Required) | 91 | 113 | 1.0 | 1.0–1.0 |
| Health video playing (Optional) | 66 | 228 | 3.0 | 2.0–4.0 |
| Health audio broadcasting (Optional) | 59 | 212 | 3.0 | 2.0–4.0 |
| Evaluation and reward (Optional) | 62 | 93 | 1.0 | 1.0–2.0 |
| Class level activity | 612 | 3999 | 3.0 | 2.0–8.0 |
| Health theme activities (Required) | 544 | 1212 | 2.0 | 1.0–2.0 |
| Putting up posters (Optional) | 286 | 532 | 1.0 | 1.0–2.0 |
| Health lessons (Optional) | 380 | 1736 | 3.0 | 1.0–6.0 |
| Evaluation and reward (Optional) | 264 | 519 | 1.0 | 1.0–2.0 |
The informants attributed successful implementation to the attractiveness of health activities (Health expert, Danyang CDC, Zhenjiang): "Health education activities are enjoyable for both parents and children." The parents also expressed that both the students and family members were happy to perform the health activities together (Parent, Tianzhushan Primary School, Ganzhou): "My child and his father like doing knowledge competition together, finding it quite interesting, a valuable parent‒child interactive experience.”
Moreover, to reduce the workload for all the relevant individuals, the health cloud courses were issued automatically by “EduSaltS Manager” on Monday. Meanwhile, EduSaltS provided the teachers with ready-to-use health materials which were developed by health professionals with input from health education experts and can be downloaded from management websites. This approach gave teachers the flexibility to choose topics of interest for regular health education classes (Health expert, Danyang CDC, Ganzhou): “I looked through the health education materials in the app, and they're quite interesting and professional. …. I can choose lecture content according to own education needs.”
Another robust measure for implementation was real-time monitoring and evaluation. A school principal appraised the efficiency of the management application (Principal, Mincheng Primary School, Zhenjiang): “Through ‘EduSaltS Manager’ and ‘Management Website’, we can promptly check completion rates, rank health activities, and compare the progress between schools. The delay and incompletion were timely identified by headteachers and shared with parents.” Efficient information sharing between schools and families was frequently cited by the parents (Parent, Shahe Primary School, Ganzhou): “Appreciated the headteachers’ timely reminder for consistent engagement in the salt reduction activities.”
In this circumstance, headteachers played the pivotal role of intermediaries between the program and the target population. One example of the importance of headteachers was that a school with a newly transferred headteacher who missed program training experienced a sudden decrease in the completion rate of cloud health courses. To motivate headteachers in the implementation of health activities, schools developed incentive measures (Principal, Wenqinglu Primary School, Ganzhou): “The headteachers who successfully completed health activities were evaluated with higher teaching performance and priority of year reward or promotion.”
However, despite the boosters advancing the program, barriers from family may adversely affect the implementation. One common issue was (Teacher, Xincheng Primary School, Zhenjiang): “parents migrated from their poor hometown to affluent cities for better job opportunities.” Another barrier stems from the demanding schedule of parents, who are occupied by heavy workloads and constraints on the time available for their children (Parent, Shahe Primary School, Ganzhou): “We have our own jobs and responsibilities and might be overwhelmed by those school activities.” As a result (Teacher, Xincheng Primary School, Zhenjiang): “the children encountered difficulties in fulfilling health activities due to lack inspiration and support, typically provided by the parents.”
Maintenance and sustainability
As the health education program spans a school year, maintenance was acknowledged to be a challenge. The completion rates of health cloud courses experienced a decline, starting at a peak of 93.4% at the beginning of the first semester and reaching a lower rate of 79.4% by the end of the semester. Notably, nine completion rates of courses in the second school term remained below the average completion rate of whole program period (84.9%), only one was 86.2%.
To avoid a drop of completion rate and maintain fidelity implementation, considerable governmental efforts were made. This includes 17 government directive and 10 capability training events delivered by provincial or city education and health authorities. The local managers conducted 57 field supervisions and 60 online monitoring activities, particularly to target poorly performing schools and address implementing difficulties (Table 6).
Table 6.
Governmental activities
| Total | provincial | Ganzhou | Zhenjiang | |
|---|---|---|---|---|
| Government issued directive | 17 | 2 | 4 | 11 |
| field supervision | 57 | 19 | 16 | 22 |
| Online monitoring and management | 60 | 23 | 9 | 28 |
| capability training for health education | 10 | 4 | 2 | 4 |
| support school's offline activities | 5 | 0 | 1 | 4 |
Those governmental activities were smoothly conducted because of bolstered intersectoral collaboration between local governments, as the informant expressed (Official, Zhanggong Health Committee, Ganzhou): “Establishment of clear responsibilities in conjunction with health authorities, wherein health sectors provided professional and technological support, while the education sector took responsibility for motivating, organizing, and monitoring the schools to achieve project goals.” This articulated management mechanism holds promise for the scalable implementation of EduSaltS.
Along with governmental measures, the informants recognized that family active engagement and therefore positive feedback from schools, such as commendations for their children's performance in the EduSaltS, significantly motivated their participation in future school health programs (Parent, Heyang Primary School, Zhenjiang): “My child received praise and recognition from teacher. As parents, we are very happy and motivated to continue doing well.”
Despite those potential facilitators for maintenance, the completion rate still shown a drop according to quantitative results, that means scaling-up salt reduction in schools also face challenges. The informants claimed that lack of essential policy environment may be one attribution (Official, Danyang Education Bureau, Zhenjiang): “Government should issue policy to require school cafeteria chefs to accept mandatory training for salt reduction.” Another informant mentioned (Health expert, Jiangxi CDC, Ganzhou): “a lack of guidelines will cause difficulties in the adoption and implementation of school salt reduction in the future.” Along with the policy support, another issue, financial support after the program officially end, were mentioned by the informants. Mainly, affordable maintenance should be made to keep this mHealth-based school health education system accessible (Health expert, Danyang CDC, Zhenjiang): “The applications should be freely downloadable from mobile and website not only for the program participants but also for larger populations.” This further triggered another financial issue to update education materials to cater to other grades of students.
Discussion
This research evaluated the implementation process of the mHealth-based school salt reduction program and examined the factors for its implementation. The quantitative results show that the program achieved a high registration rate and completion rate of online health lessons. Through online and offline activities, the students improved their knowledge and practices related to salt reduction. Factors that promote individual and school participation include parents' trust and students’ willingness to participate in school-organized health activities [33]. The schools themselves have an urgent need to improve students’ health [34]. The use of an online platform allows flexible student participation [35], and schools can organize and manage activities without additional resources. However, participating in the program required primary skills to operate smartphones and register in the Health Cloud Classroom, which increased the difficulty of participation for some caregivers, especially grandparents [16].
This evaluation illustrated the determinants that facilitate successful implementation: the attractiveness of health activities, deep parental engagement, effective communication between schools and families, teachers' dedication, a healthy school environment, and government coordination [36].
Remarkably, EduSaltS was carried out and implemented during the COVID-19 pandemic. The intervention measures utilized mHealth technology, allowing the project's main activities to be completed online even in strict lockdown areas [37, 38]. Furthermore, education materials have been provided to schools through mHealth based application, which has reduced teachers’ workload and led to additional efforts to develop education materials. This approach made it scalable for most schools, especially in situations where resources and manpower were diverted to acute infectious disease control.
Several factors should be highlighted from the study findings to implicate scaling-up health programs. First, the high-salt dietary environment outside schools compromises the effects of salt reduction on students, as their taste preferences remain high due to continuous exposure to high-salt food from convenience stores and restaurants around school districts [39]. The food from off-campus sources made it challenging to achieve the expected reduction in salt intake [40, 41]. Therefore, expanding salt reduction to school surroundings and wider communities is crucial for the success of implementing school salt reduction projects [42]. Meanwhile, the school is a relatively closed environment, and any promotional intervention through the school must first obtain the consent and support of the local education commission, which is a prerequisite. So, notices from the local education commission were formally issued to all the schools in the selected regions to help them understand the project and make decision for the participation. However, we did not ask the local government to provide any other additional monetary or in-kind support. Moreover, legislative and regulatory measures developed by government can encourage commercial sectors, who were determinantal for health environment, to reduce sodium content in the products and prioritize positive health among children [43, 44].
Second, there was a contradiction in the allocation of resources between salt reduction activities and other health activities in school [45]. High salt intake as a daily dietary habit has not received as much attention as other issues, such as myopia prevention and obesity, which are prevalent among Chinese students. The balance between salt reduction and other student health problems is a challenge for schools, given their limited resources and time commitment [46]. Therefore, utilizing existing school resources is crucial for implementing the innovative EduSaltS project, which leverages school staff, facilities, and materials and avoids significant additional resource requirements [47].
Third, the project utilized WeChat on smartphones as a platform for health education and primary online health activities. WeChat is the most widely used mobile application in China, providing a solid foundation for increasing the possibility of reaching. This platform does not require extra payment, which increases the acceptability of scaling-up. The continued accessibility of WeChat-based education and management functions was perceived as a premise for scaling-up. Moreover, real-time evaluation through management websites is essential for continually identifying and addressing off-track issues that may arise during project maintenance [48, 49].
Finally, this study found that the stability of the management structure is crucial for smooth implementation and long-term continuation. As a complex promotion project, excessive reliance on respected individuals to maintain operations was risky because changes in leadership positions hindered the high-quality completion of school health activities. For schools, staff turnover was inevitable. Timely training of headteachers who just joined the project to qualify them for health education knowledge and skills was vital to prevent sudden drops in the completion rate of health activities [50, 51].
Strengths and limitations
Based on the RE-AIM theoretical model, the mixed methods process evaluation offered a comprehensive framework to evaluate the facilitators and barriers encountered during the implementation of EduSaltS. Across five model dimensions, this study not only highlighted individual-level engagement and health benefits derived from school salt reduction initiatives but also examined factors influencing project implementation and sustainability at both school and societal levels. By gaining a deeper understanding of the determinantal factors in the implementation process, successful strategies from this program can be extrapolated to guide future health scaling-up programs.
In terms of limitations, this study did not delve into the detailed demographics of participants nor compare the characteristics of participants with non-participants. Particularly, the lack of gender-specific data limits the ability to understand differential impacts and adoption issues between male and female participants, which could affect program efficacy and implementation strategies. However, as a scaling-up program aimed at translating experimental evidence into real-world benefits for larger populations, the focus was on recruiting as many attendees as possible rather than rigorously selecting participants. A specially designed sampling survey targeting 799 students and their parents from 30 schools will make up for its shortcomings, but the results will be reported in a separate article.
Conclusions
The process evaluation revealed that the EduSaltS program attained high acceptability among participants and was widely adopted at the organizational level. Health activities were implemented with high fidelity, leading to improved health knowledge and practices in students and their families, particularly in reducing salt intake and enhancing overall well-being. These results offer evidence of initial scalability due to practical educational tools, strong family involvement, effective institutional management, and a supportive policy environment. The program holds significant promise in curbing excessive salt consumption among broader populations in various settings, potentially delaying the onset of related diseases.
Supplementary Information
Additional file 1. Health Knowledge and Behavior Assessment: Self-report questionnaire.
Additional file 2. Results of process evaluation on EduSaltS based on RE-AIM model with mixed methods.
Additional file 3. Qualitative quotation, source, code and theme.
Acknowledgements
We thank the original data creators, depositors, copyright holders, the funders. We appreciate the contribution from the local education bureaus, health committees and agencies.
Abbreviations
- CDC
Centre for Diseases Control and Prevention
- NCDs
Non-communicable diseases
- DALYs
Disability adjusted life year
- cRCT
Cluster randomized controlled trial
Authors’ contributions
YINGHUA LI and PUHONG ZHANG conducted the research design, all research management, and findings interpretation. HAIJUN GUO. YUAN LI and LI LI conducted the research design, organized the fieldwork, data collection, data analysis, theoretical interpretation of the mixed methods findings and manuscript drafting. RONG LUO and GUANGMING YI conducted the program progress monitoring, fieldwork organization and interview data collection. LANLAN WANG and GANG ZHANG contributed to program management, the education material development, fieldworks organization and interview data collection. FENG J HE and CHANGQIONG WANG conducted research design, fieldworks and manuscript drafting. NAIBO WANG. LIHUANG LI. TAO MAO and JIAJIN LIN conducted program management, organized fieldworks, and data collection. All authors were involved in preparing the manuscript and approved the final version to be published.
Funding
This independent research was supported by the Medical Research Council [MR/T024399/1], under the Global Alliance for Chronic Disease (GACD) Scale-up Research Programme. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR, or the Department of Health.
Availability of data and materials
The qualitative transcripts generated and/or analyzed during the current study are not publicly available due to protecting participants’ anonymity. The quantitative datasets are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The study was approved by the Ethic Committee of Chinese Center for Health Education (IERC2023001). Participants had consented to accept the education by agreeing e-consent before the registration in EduSaltS. Written informed consent for the interview and focus group were obtained from all interviewees.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Yinghua Li, Email: liyinghua729@sina.com.
Puhong Zhang, Email: zpuhong@georgeinstitute.org.cn.
References
- 1.Al Jawaldeh A, Rafii B, Nasreddine L. Salt intake reduction strategies in the eastern mediterranean region. East Mediterr Health J. 2019;24(12):1172–80. 10.26719/emhj.18.006 [DOI] [PubMed] [Google Scholar]
- 2.WHO global report on sodium intake reduction https://iris.who.int/bitstream/handle/10665/366393/9789240069985-eng.pdf?sequence=1.
- 3.Santos JA, Tekle D, Rosewarne E, Flexner N, Cobb L, Al-Jawaldeh A, Kim WJ, Breda J, Whiting S, Campbell N, et al. A systematic review of salt reduction initiatives around the world: a midterm evaluation of progress towards the 2025 global non-communicable diseases salt reduction target. Adv Nutr. 2021;12(5):1768–80. 10.1093/advances/nmab008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zandstra EH, Lion R, Newson RSJFQ. Preference: Salt reduction: moving from consumer awareness to action. Food Qual Prefer. 2016;48:376–81. 10.1016/j.foodqual.2015.03.005 [DOI] [Google Scholar]
- 5.Wang L, Zhang P, Li Y, Li Y, Zhang B, Wang H, Wu J, Han J, Li C, Li N, et al. Deepening the action on salt reduction in China-suggestions on strategy and implementation plan. Chin J Prev Med. 2023;57(7):10. [DOI] [PubMed] [Google Scholar]
- 6.Trumbo PR, Kirkpatrick KM, Roberts J, Smith P, Zecca P. Perspective: challenges and strategies to reduce the sodium content of foods by the food service industry. Adv Nutr. 2023;14(4):592–8. 10.1016/j.advnut.2023.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tan M, He FJ, Wang C, MacGregor GA. Twenty-four-hour urinary sodium and potassium excretion in China: a systematic review and meta-analysis. J American Heart Assoc. 2019;8(14):e012923. 10.1161/JAHA.119.012923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, Li X, Wang L, Wang L, Liu Y, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the Global burden of disease study 2017. Lancet. 2019;394(10204):1145–58. 10.1016/S0140-6736(19)30427-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wu F, Zhang L, Guo W, Wang M, Gao Y, Liu D, Bai Y, Zhao Y, Mi S, Zhao W, et al. Evaluation of China healthy lifestyle for all interventions based on RE-AIM framework - China, 2007–2020. China CDC Weekly. 2022;4:403–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fan F, Li Y. Salt reduction in the world – intervention strategies and measures: a progress review. Chin J Public Health. 2022;38(8):1070–8. [Google Scholar]
- 11.Healthy China Action Plan (2019–2030) https://www.gov.cn/xinwen/2019-07/15/content_5409694.htm.
- 12.National nutrition plan (2017–2030) https://www.gov.cn/zhengce/content/2017-07/13/content_5210134.htm.
- 13.Fornari LS, Giuliano I, Azevedo F, Pastana A, Vieira C, Caramelli B. Children first study: how an educational program in cardiovascular prevention at school can improve parents’ cardiovascular risk. Eur J Prev Cardiol. 2012;20(2):301–9. 10.1177/2047487312437617 [DOI] [PubMed] [Google Scholar]
- 14.Gunawardena N, Kurotani K, Indrawansa S, Nonaka D, Mizoue T, Samarasinghe D: School-based intervention to enable school children to act as change agents on weight, physical activity and diet of their mothers: a cluster randomized controlled trial. International Journal of Behavioral Nutrition and Physical Activity 2016, 13(1). [DOI] [PMC free article] [PubMed]
- 15.He FJ, Wu Y, Feng XX, Ma J, Ma Y, Wang H, Zhang J, Yuan J, Lin CP, Nowson C, et al. School based education programme to reduce salt intake in children and their families (School-EduSalt): cluster randomised controlled trial. BMJ. 2015;350:h770. 10.1136/bmj.h770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sun Y, Li Y, He FJ, Liu H, Sun J, Luo R, Guo C, Zhang P. Process evaluation of an application-based salt reduction intervention in school children and their families (AppSalt) in China: a mixed-methods study. Front Public Health. 2022;10:744881. 10.3389/fpubh.2022.744881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.He FJ, Zhang P, Luo R, Li Y, Sun Y, Chen F, Zhao Y, Zhao W, Li D, Chen H, et al. App based education programme to reduce salt intake (AppSalt) in schoolchildren and their families in China: parallel, cluster randomised controlled trial. BMJ. 2022;376:e066982. 10.1136/bmj-2021-066982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang P, Sun J, Li Y, Li Y, Sun Y, Luo R, Nie X, Li L, Liu Y, He FJ. An mHealth-based school health education system designed to scale up salt reduction in China (EduSaltS): A development and preliminary implementation study. Front Nutr. 2023;10:1161282. 10.3389/fnut.2023.1161282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nine step for developing a scale-up strategy https://apps.who.int/iris/handle/10665/44432.
- 20.Sanchez-Flack JC, Herman A, Buscemi J, Kong A, Bains A, Fitzgibbon ML. A systematic review of the implementation of obesity prevention interventions in early childcare and education settings using the RE-AIM framework. Transl Behav Med. 2020;10(5):1168–76. 10.1093/tbm/ibz179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sutherland RL, Jackson JK, Lane C, McCrabb S, Nathan NK, Yoong SL, Lum M, Byaruhanga J, McLaughlin M, Brown A, et al. A systematic review of adaptations and effectiveness of scaled-up nutrition interventions. Nutr Rev. 2022;80(4):962–79. 10.1093/nutrit/nuab096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee SYD, Iott B, Banaszak-Holl J, Shih SF, Raj M, Johnson KE, Kiessling K, Moore-Petinak ND. Application of mixed methods in health services management research: a systematic review. Medical Care Res Rev. 2021;79(3):331–44. 10.1177/10775587211030393 [DOI] [PubMed] [Google Scholar]
- 23.Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999;89(9):1322–7. 10.2105/AJPH.89.9.1322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yoshida Y, Patil SJ, Brownson RC, Boren SA, Kim M, Dobson R, Waki K, Greenwood DA, Torbjornsen A, Ramachandran A, et al. Using the RE-AIM framework to evaluate internal and external validity of mobile phone-based interventions in diabetes self-management education and support. J Am Med Inform Assoc. 2020;27(6):946–56. 10.1093/jamia/ocaa041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nhim K, Gruss SM, Porterfield DS, Jacobs S, Elkins W, Luman ET, Van Aacken S, Schumacher P, Albright A. Using a RE-AIM framework to identify promising practices in National Diabetes Prevention Program implementation. Implement Sci. 2019;14(1):81. 10.1186/s13012-019-0928-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li H. Using RE-AIM framework to evaluate health intervention programs. Chinese J Health Educ. 2013;29(05):466–8+473. [Google Scholar]
- 27.Hilary P, Melanie B, Christopher RC, Sandra E, Gonzalo G, Chris JG, Jo R-M, Paul M, Elizabeth M, Anita P, et al. Standards for reporting implementation studies (StaRI) statement. BMJ. 2017;356:i6795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.O’Cathain A, Murphy E, Nicholl J. The quality of mixed methods studies in health services research. J Health Serv Res Policy. 2008;13(2):92–8. 10.1258/jhsrp.2007.007074 [DOI] [PubMed] [Google Scholar]
- 29.Nowell LS, Norris JM, White DE, Moules NJ. Thematic analysis. Int J Qual Methods. 2017;16(1):160940691773384. 10.1177/1609406917733847 [DOI] [Google Scholar]
- 30.Morton K, Dennison L, Band R, Stuart B, Wilde L, Cheetham-Blake T, Heber E, Slodkowska-Barabasz J, Little P, McManus RJ, et al. Implementing a digital intervention for managing uncontrolled hypertension in primary care: a mixed methods process evaluation. Implement Sci. 2021;16(1):57. 10.1186/s13012-021-01123-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Trieu K, Jan S, Woodward M, Grimes C, Bolam B, Nowson C, Reimers J, Davidson C, Webster J. Protocol for the process evaluation of a complex, statewide intervention to reduce salt intake in Victoria, Australia. Nutrients. 2018;10(8):998. 10.3390/nu10080998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jong ST, Brown HE, Croxson CHD, Wilkinson P, Corder KL, van Sluijs EMF. GoActive: a protocol for the mixed methods process evaluation of a school-based physical activity promotion programme for 13–14year old adolescents. Trials. 2018;19(1):282. 10.1186/s13063-018-2661-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Åvitsland A, Ohna SE, Dyrstad SM, Tjomsland HE, Lerum Ø, Leibinger E. The process evaluation of a school-based physical activity intervention: influencing factors and potential consequences of implementation. Health Educ. 2020;120(2):121–39. 10.1108/HE-01-2020-0004 [DOI] [Google Scholar]
- 34.Yang J, Jiao W, Yang J, Gao Q. The current situation of school health in China. Int J Trop Dis Health. 2022;43:14–8. [Google Scholar]
- 35.Noorbhai H, Ojo TA. mHealth and e-Learning in health sciences curricula: a South African study of health sciences staff perspectives on utilisation, constraints and future possibilities. BMC Med Educ. 2023;23(1):189. 10.1186/s12909-023-04132-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ismail MR, Seabrook JA, Gilliland JA. Process evaluation of fruit and vegetables distribution interventions in school-based settings: a systematic review. Prev Med Rep. 2021;21:101281. 10.1016/j.pmedr.2020.101281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kumar S, Misra R, Chakraborty D, Chhabra PK, Upadhyaya P. A study of perceptions of students and teachers towards e-learning and its effectiveness - a cross-sectional study during COVID-19 lockdown in JNUIMSRC. Int J Curr Res Rev. 2020;12:195–8. 10.31782/IJCRR.2020.122336 [DOI] [Google Scholar]
- 38.Naciri A, Radid M, Kharbach A, Chemsi G. E-learning in health professions education during the COVID-19 pandemic: a systematic review. J Educ Eval Health Profess. 2021;18:27. 10.3352/jeehp.2021.18.27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Trieu K, Webster J, Jan S, Hope S, Naseri T, Ieremia M, Bell C, Snowdon W, Moodie M. Process evaluation of Samoa’s national salt reduction strategy (MASIMA): what interventions can be successfully replicated in lower-income countries? Implement Sci. 2018;13(1):107. 10.1186/s13012-018-0802-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.França FCOD. Andrade IdS, Zandonadi RP, Sávio KE, Akutsu RdCCdA: Food environment around schools: a systematic scope review. Nutrients. 2022;14(23):5090. 10.3390/nu14235090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bassi S, Bahl D, Arora M, Tullu FT, Dudeja S, Gupta R. Food environment in and around schools and colleges of Delhi and National Capital Region (NCR) in India. BMC Public Health. 2021;21(1):1767. 10.1186/s12889-021-11778-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Healthy food environment and school food https://www.fao.org/school-food/overview/en/.
- 43.Hoe C, Weiger C, Minosa MKR, Alonso F, Koon AD, Cohen JE. Strategies to expand corporate autonomy by the tobacco, alcohol and sugar-sweetened beverage industry: a scoping review of reviews. Global Health. 2022;18(1):17. 10.1186/s12992-022-00811-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.The L. Unravelling the commercial determinants of health. Lancet. 2023;401(10383):1131. 10.1016/S0140-6736(23)00590-1 [DOI] [PubMed] [Google Scholar]
- 45.Sawyer SM, Raniti M, Aston R. Making every school a health-promoting school. Lancet Child Adolesc Health. 2021;5(8):539–40. 10.1016/S2352-4642(21)00190-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shoesmith A, Hall A, Wolfenden L, Shelton RC, Powell BJ, Brown H, McCrabb S, Sutherland R, Yoong S, Lane C, et al. Barriers and facilitators influencing the sustainment of health behaviour interventions in schools and childcare services: a systematic review. Implement Sci. 2021;16(1):100. 10.1186/s13012-021-01134-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Palinkas L, Christian DL, Todd C, Rance J, Stratton G, Mackintosh KA, Rapport F, Brophy S. Involving the headteacher in the development of school-based health interventions: A mixed-methods outcome and process evaluation using the RE-AIM framework. Plos One. 2020;15(4):e0230745. 10.1371/journal.pone.0230745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.World Health Organization. Practical guidance for scaling up health service innovations. Geneva: World Health Organization; 2009. [Google Scholar]
- 49.Guide for monitoring scale-up of health practices and interventions http://cquin.icap.columbia.edu/wp-content/uploads/2018/07/MEASURE_Monitoring-scale-up.pdf.
- 50.Centers for Disease Control and Prevention. School health guidelines to promote healthy eating and physical activity. Atlanta: Centers for Disease Control and Prevention (CDC), U.S; 2011. [PubMed] [Google Scholar]
- 51.Nubani Husseini M, Zwas DR, Donchin M. Teacher training and engagement in health promotion mediates health behavior outcomes. Int J Environ Res Public Health. 2022;19(5):3128. 10.3390/ijerph19053128 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Health Knowledge and Behavior Assessment: Self-report questionnaire.
Additional file 2. Results of process evaluation on EduSaltS based on RE-AIM model with mixed methods.
Additional file 3. Qualitative quotation, source, code and theme.
Data Availability Statement
The qualitative transcripts generated and/or analyzed during the current study are not publicly available due to protecting participants’ anonymity. The quantitative datasets are available from the corresponding author on reasonable request.