Abstract
Urinary leak is one of the most significant complications after partial nephrectomy. In case of persistent urine leaks, placement of a ureteral stent is effective but not always sufficient. This study included 5 patients with persistent urinary leak after partial nephrectomy. The patients underwent flexible ureteroscopy wherein we identified the damaged calyx. Subsequently, we performed percutaneous puncture targeting the distal end of the endoscope at this calyx and installed a nephrostomy tube. Then, the endoscope was removed, and the ureter was drained with a stent. Ureteral stenting ensures elimination of urinary leak in most patients after partial nephrectomy. In patients with persistent urinary leak, retrograde endoscopic percutaneous drainage of the pelvicalyceal system is the method of choice because it allows for rapid and effective treatment of urinary fistulas.
Key words: Complication, Endoscopic treatment, Flexible ureteroscopy, Kidney cancer, Urinary fistula
1. Introduction
The last 3 decades have seen the active introduction of nephron-sparing surgery in the treatment of localized kidney cancer. Stage T1a tumors are an indication for partial nephrectomy (PN)[1] as recommended by various urological associations. The PN provides equivalent oncologic outcomes and better renal function than radical nephrectomy.[2] However, after PN, in contrast to radical nephrectomy, various complications are observed: bleeding, arteriovenous malformations, urinary fistulas (UFs), and delayed ureteral strictures.[3,4] Urinary fistula is a non–life-threatening complication, although urine leaks lead to a poor quality of life and social problems. Frequency of UF after PN ranges from 0.5% to 17.4%,[4,5] with high rates observed after open PN. After the introduction of laparoscopic PN (LPN) and robotic-assisted PN, the number of cases of UF began to decrease gradually.
The main treatment method for these patients is retrograde ureteral stenting or percutaneous drainage of the pelvicalyceal system (PCS) and the perirenal urinoma. In most cases, urinary leak stops with drainage of the upper urinary tract. However, in some patients, urinary leak can persist for a long time. The median and resolution range of UF, according to Kundu et al.,[4] were 64 (29–96) days. If treatment of UF with ureteral stenting is not effective, studies suggest single clinical observations of simultaneous use of 2 stents,[6] retrograde or percutaneous injection of fibrin glue into the PCS,[7] antegrade use of N-butyl-2-cyanoacrilate,[8] and percutaneous cryoablation of the fistulous tract.[9] There is no unified treatment or clear algorithm for the rapid elimination of urinary leak after PN.
2. Materials and methods
After obtaining approval from the institutional review board (No. 8-2020), we retrospectively studied the data of 5 patients (2 men and 3 women) with UF developed after PN from 2018 to 2020 (Table 1). All patients provided informed consent for the use of their clinical information in research studies, and the confidentiality of the data was guaranteed. Of these, 3 patients were previously operated on in other hospitals and 2 patients in our clinic. The mean age of the patients was 55.8 years. The tumor size was 2.5 to 4.8 cm, mean RENAL score was 7.8, and body mass index was 25.0 to 35.5 kg/m2. All patients had earlier undergone minimally invasive PN; the time between surgery and UF development varied between 3 and 10 days. Four of 5 patients had a large amount of discharge from their paranephral drainage system and high creatinine level. One of these patients was hospitalized 10 days after PN because of fever and was diagnosed with urinoma. After drainage, the urine began to flow actively up to 600 mL/d, and ureteral stenting was performed (Table 1).
Table 1.
Patient characteristics.
| Patient | Sex | Age, yr | Body mass index, kg/m2 | Initial surgery | Time to urinary fistula formation, d | Symptoms of urinary fistula | Additional surgeries | Duration of stenting, d |
|---|---|---|---|---|---|---|---|---|
| 1 | Female | 68 | 32.5 | LPN | 5 | Urine leak | Ureteral stenting | 56 |
| 2 | Male | 52 | 28.4 | LPN | 4 | Urine leak | Ureteral stenting | 25 |
| 3 | Female | 57 | 27.5 | LPN | 3 | Urine leak | Ureteral stenting | 21 |
| 4 | Male | 33 | 25 | LPN | 8 | Fever, urinoma | Percutaneous drainage + stenting | 43 |
| 5 | Female | 62 | 35.5 | RAPN | 10 | Fever, urinoma | Percutaneous drainage + stenting | 36 |
LPN = laparoscopic partial nephrectomy; RAPN = robot-assisted partial nephrectomy.
After the diagnosis of UF, a 7F ureteral stent was installed and the patients were discharged. However, during the observation period (on average, 25 ± 12 days postoperatively), urine leak through the drainage persisted with no decrease in urine volume.
Two patients had severe stent-associated symptoms that were not corrected by сonservative management. All patients insisted on more active treatment, noting a poor quality of life and reluctance to walk with a stent to close the fistula for a long, unpredictable time.
Before the operation, computed tomography urogram was performed to clarify renal function and to determine the localization of urine leak. In 2 patients, the fistulous tract was located in the lower calyx, in 2 other patients, in the middle calyx, and in 1 in the upper calyx. All patients underwent retrograde endoscopic-assisted percutaneous treatment of persistent UF example of a clinical case given hereinafter.
3. Case presentation
A 33-year-old man was diagnosed with left renal carcinoma T1a and treated with an LPN on July 6, 2020, at another clinic. The RENAL Nephrometry Score was 7×. The retroperitoneal drain was removed on the third day, and the patient was discharged. However, 7 days after the operation, he returned to the clinic with pain in the operated kidney and fever. The ultrasound revealed urinoma, and its percutaneous drainage was performed on July 14, 2020. The next day, because of abundant urine flow through the drainage, stenting of the left ureter was performed. The patient was admitted to our clinic on August 17, 2020, with complaints of drainage and urine leak (300–400 mL/d). Computed tomography urogram showed that the kidneys were of normal shape and size and secreted a contrast media in a timely manner, the PCS was not dilated, no stones were visualized, and the perinephric tissue was not changed. The urine leak was seen in the upper pole calyceal group (Fig. 1). The patient underwent retrograde endoscopic-assisted percutaneous treatment of UF on August 18, 2020, 43 days after LPN. After patient positioning and removing the stent, a rigid ureteroscopy was performed. The ureter and the pelvis were in place. Damage was noted in the upper pole calyceal group, the neck of which was not narrowed (Fig. 2A). The retrograde pyelography showed UF and contrast media leak (Fig. 2B). Thereafter, flexible ureteroscopy was performed to identify damaged calyx (Fig. 2C). Then, under ultrasound and endoscopic control, focusing on the distal end of the flexible ureteroscope, percutaneous puncture of the PCS was performed through the damaged calix (Fig. 3). After that, a nephrostomy tube was installed (Fig. 4). The flexible ureteroscope was removed, and a 6F ureteral stent was placed. There were no complications, and after 2 days, the patient was discharged. After 10 days, the ureteral stent was removed. Computed tomography with antegrade pyelography was performed showing good patency of the upper urinary tract and no contrast media leak (Fig. 5A). The next day, the nephrostomy tube was removed. A 12F Nelaton catheter was inserted into the UF by 2 cm, and fistulography was performed. There was no contrast media leak, it freely enters the PCS of the left kidney, then the ureter (Fig. 5B). After removal of the nephrostomy tube, the UF closed. At control ultrasound, there was no urinoma, and the PCS of the left kidney was not dilated.
Figure 1.

Computed tomography urogram: the arrow shows urine leak.
Figure 2.
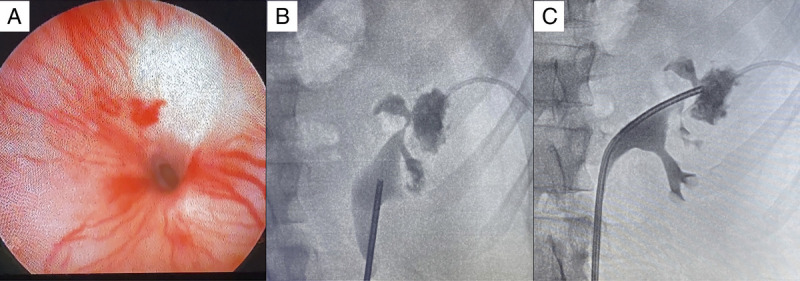
Intraoperative visualization of the damaged calyx. (A) Retrograde rigid ureteroscopy. (B) Retrograde pyelography: contrast agent extravasation. (C) Flexible ureteroscopy with retrograde pyelography.
Figure 3.

Percutaneous puncture of the damaged calyx. (A) The puncture needle is visualized paranephral in the area of tumor resection performed earlier: needle (indicated by blue arrow) and clip (indicated by green arrow). (B) The needle is inserted into the renal pelvis through the calyx. (C) The wire guide is installed antegrade.
Figure 4.
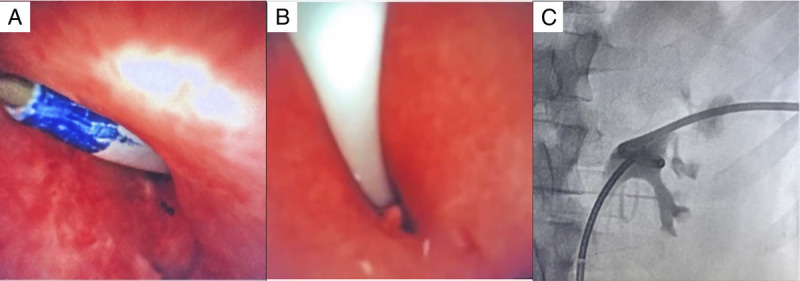
Nephrostomy tube installation. (A) Dilation of the puncture site. (B) Nephrostomy tube installation under flexible endoscope control. (C) Antegrade pyelography after installation of the nephrostomy tube and ureteral stent.
Figure 5.
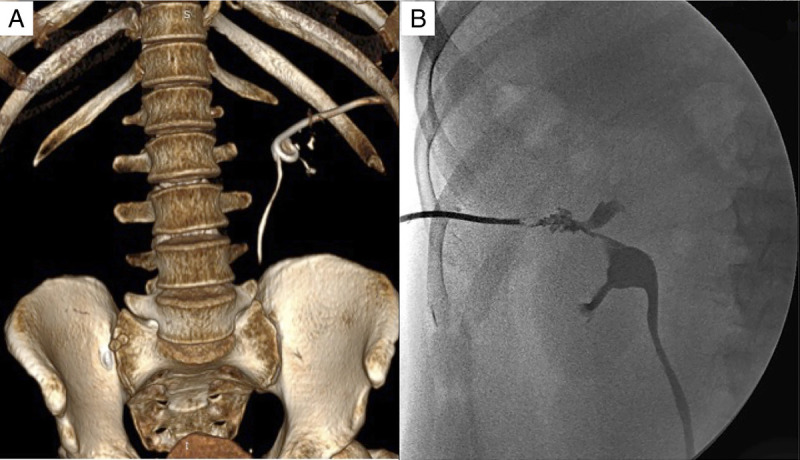
Postoperative computed tomography scan with 3D reconstruction and X-ray scan. (A) Computed tomography with antegrade pyelography. (B) Fistulography after nephrostomy tube removal: good patency of the upper urinary tract.
All patients with UF resulting from PN were successfully operated on with no complications. The mean surgery time was 45.0 ± 20.5 minutes (range, 40–65 minutes). Only 2 patients had some discharge from the fistula within 1 day after nephrostomy tube removal, which stopped without any additional interventions. Three patients had their fistula healed immediately. The treatment efficacy during the whole follow-up period of 18 ± 4 months (range, 6–26 months) was 100%.
4. Discussion
UF is a non–life-threatening complication and more often observed in open surgery for renal cancer. Studies have shown the preoperative predictors of the possible development of UF in PN.[3–5] Kundu et al.[4] found that 3 factors are reliably associated with the development of UF based on the results of 1118 PN: tumor size, volume of blood loss, and time of warm ischemia.
The most common treatment for patients with UF is ureteral stenting or percutaneous drainage of the PCS. In most cases, it leads to the elimination of UF; however, in a certain group of patients, UF did not close leading to delayed treatment.
There was a need to introduce a simple, affordable for most clinics, effective method of treating persistent UF after PN. This technique is clear with no technical difficulties. The endoscopic assessment of the PCS allows a detailed assessment of the structure of the PCS and of the urine leak. It also allows to assess the condition of the neck of the injured calyx, to exclude its stricture. After the installation of a nephrostomy tube through the damaged calyx, a straight, stable UF of a small diameter is formed for 10 to 12 days, allowing faster rehabilitation.
5. Conclusions
Ureteral stenting ensures elimination of UF in most patients after PN. In single cases of persistent UF, fibrin glue and cyanoacrylate-based sealant, simultaneous installation of 2 stents, and percutaneous cryoablation of the fistulous tract were used. An alternative that is a rapid and effective treatment of UF is the retrograde endoscopic-assisted percutaneous treatment.
Acknowledgments
None.
Statement of ethics
This study has obtained approval from the institutional review board (No. 8-2020). All patients provided informed consent for the use of their clinical information in research studies, and the confidentiality of the data was guaranteed. All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding source
None.
Author contributions
BG: Conceptualization, methodology, writing – original draft;
BK: Supervision, validation;
MS: Writing – review & editing;
MA: Investigation, visualization;
AT: Writing – original draft, investigation.
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
Footnotes
How to cite this article: Guliev B, Komyakov B, Shevnin M, Agagyulov M, Talyshinskii A. Management of persistent urine leak after partial nephrectomy: a case series. Curr Urol 2024;18(2):155–158. doi: 10.1097/CU9.0000000000000136
Contributor Information
Bakhman Guliev, Email: gulievbg@mail.ru.
Boris Komyakov, Email: komyakovbk@mail.ru.
Murad Agagyulov, Email: murad1311@bk.ru.
Ali Talyshinskii, Email: ali-ma@mail.ru.
Conflict of interest statement
No conflict of interest has been declared by the authors.
References
- 1.Ljungberg B Albiges L Abu-Ghanem Y, et al. European Association of Urology guidelines on renal cell carcinoma: The 2019 update. Eur Urol 2019;75(5):799–810. [DOI] [PubMed] [Google Scholar]
- 2.Scosyrev E, Messing EM, Sylvester R, Campbell S, Van Poppel H. Renal function after nephron-sparing surgery versus radical nephrectomy: Results from EORTC randomized trial 30904. Eur Urol 2014;65(2):372–377. [DOI] [PubMed] [Google Scholar]
- 3.Ryan J, MacCraith E, Davis NF, McLornan L. A systematic management algorithm for perioperative complications after robotic assisted partial nephrectomy. Can Urol Assoc J 2019;13(11):E371–E376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kundu SD, Thompson RH, Kallingal GJ, Cambareri G, Russo P. Urinary fistulae after partial nephrectomy. BJU Int 2010;106(7):1042–1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peyton CC Hajiran A Morgan K, et al. Urinary leak following partial nephrectomy: A contemporary review of 975 cases. Can J Urol 2020;27(1):10118–10124. [PubMed] [Google Scholar]
- 6.Alsikafi NF, Steinberg GD, Gerber GS. Dual stent placement for the treatment of a persistent urine leak after partial nephrectomy. Urology 2001;57(2):355–357. [DOI] [PubMed] [Google Scholar]
- 7.Bradford TJ, Wolf JS, Jr. Percutaneous injection of fibrin glue for persistent nephrocutaneous fistula after partial nephrectomy. Urology 2005;65(4):799. [DOI] [PubMed] [Google Scholar]
- 8.Selli C, De Maria M, Manica M, Turri FM, Manassero F. Minimally invasive treatment of urinary fistulas using N-butyl-2-cyanoacrylate: A valid first line option. BMC Urol 2013;13:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ward TJ, Ahmed O, Chung BI, Sze DY, Hwang GL. Percutaneous cryoablation for successful treatment of a persistent urine leak after robotic-assisted partial nephrectomy. J Vasc Interv Radiol 2015;26(12):1867–1870. [DOI] [PubMed] [Google Scholar]


