Abstract
Background
Intramuscular (IM) injection of penicillin G Benzathine (PGB) is widely recognized as the primary treatment for patients at all stages of syphilis. However, the discomfort and induration associated with PGB injections are often a challenge for patients. While lidocaine is already known to reduce injection pain and is standard practice in some countries, the added value of combining lidocaine with the z-track technique has not been thoroughly investigated. This study aims to observe the use of combining lidocaine with the Z-track technique in the treatment of syphilis, and to explore less painful methods of administering IM PGB for the treatment of syphilis in adult patients.
Methods
32 syphilis patients requiring penicillin treatment were injected with 1.2 million units of penicillin on both sides of the buttocks. The left side was injected using the traditional method with 0.9% saline as the solvent (control Group), while the right side was injected using a “z” injection method with 0.2% lidocaine as the solvent (experimental Group). The success rate of the single injection, the intensity and duration of the post-injection pain and the induration reaction were observed and recorded.
Results
There was no statistically significant difference in single injection success rate and immediate post injection pain score between the two sides (P>0.05). However, the right side had a lower pain score at 30 minutes post injection and fewer induration reactions, showing a statistically significant difference between the two sides (P<0.05). Chi-squared analysis showed that age, gender and BMI had no significant effect on pain scores 30 minutes after injection in either the control or intervention groups. (P>0.05).
Conclusion
The lidocaine + Z-track penicillin method can reduce delayed pain and induration reactions in patients with syphilis, and provides an additional approach to improving patient comfort beyond the standard use of lidocaine alone. This method merits clinical promotion.
Keywords: syphilis, penicillin G benzathine, PGB, intramuscular injection
Introduction
Syphilis is a sexually and vertically transmitted bacterial infection caused by Treponema pallidum.1 According to the World Health Organization (WHO)’s 2021 Global Progress Report on HIV, Viral Hepatitis, and Sexually Transmitted Infections, approximately 17.7 million adults aged 15–49 years were living with syphilis worldwide in 2012, with an estimated 6.3 million new cases reported in 2016.2 For the treatment of early syphilis, the WHO, Centers for Disease Control and Prevention (CDC), and European guidelines recommend benzathine penicillin G (BPG) as the preferred treatment option, typically given as a single dose by intramuscular injection.3 However, the severe pain associated with the administration and injection site of these treatments can sometimes be of considerable intensity.
Lidocaine is a local anaesthetic that significantly reduces pain immediately after intramuscular injection of any drug. Lidocaine hydrochloride as a diluent for PGB has been shown to significantly reduce injection pain without affecting the penicillin concentration, and research has also shown that using wider and longer needles for PGB administration can reduce pain.4 The Z-track technique has been used in a variety of various conditions to improve injection pain and drug leakage during intramuscular injections, reduce skin irritation and improve patient compliance.5 However, research into this specific approach is limited, which is a key reason for our clinical trial. In this study, a 0.2% lidocaine solution was used as a solvent, and the “Z” track injection method was used to modify intramuscular injections with the aim of improving the overall injection quality of PGB, reducing patient discomfort and minimising induration reactions.
Materials and Methods
Patients
From January 2021 to August 2022, a total of 32 patients requiring treatment for syphilis with a dose of 2.4 million units (MU) of intramuscular PGB were randomly selected for the study. Exclusion criteria included: (1) positive penicillin allergy test; (2) age≤18 years; (3) cognitive impairment preventing effective communication with medical staff or accurate expression of feelings, thus preventing completion of clinical questionnaires; (4) patients with sensory impairments such as tactile or pain perception abnormalities (dullness, sensitivity); (5) recent use of anaesthetics, history of psychiatric medication or history of medication affecting pain perception; (6) allergy to amide-type local anaesthetics or any other components of this drug; (7) pregnant women with syphilis. This study was approved by the medical ethics committee of our hospital.
Study Design
The study was conducted in the injection room of the Dermatology Department of the Second Affiliated Hospital of Wannan Medical College. The study used a self-matched design, with each patient acting as their own control. Specifically, 32 patients received injections of 1.2 million units of penicillin G benzathine on both sides of the buttocks - one side using the traditional method with 0.9% saline (control group) and the other side using the “Z” track injection method with 0.2% lidocaine (experimental group). This design allows a direct comparison of the two methods within the same patient. This study used a single-blind design, where the patients were unaware of the specific injection technique used, while the study operators were aware of the technique administered.
Treatment Regimen for Syphilis Patients
PGB was administered at a total dose of 2.4 million units (MU), with 1.2 MU injected intramuscularly into each buttock. The injections were administered by nurses with at least one year’s experience in dermatology who had received standardized training. In a self-matched parallel design, the left buttock was injected with 0.9% sodium chloride as a solvent for conventional intramuscular injection (control group), while the right buttock was injected with 0.2% lidocaine as a solvent for modified intramuscular injection (experimental group). The skin was disinfected with povidone-iodine solution. Disinfection consisted of two applications covering an area of at least 5 cm in diameter. Injections were made using a 5mL disposable syringe and a 7-gauge needle with a solvent volume of 4 mL.
Conventional Intramuscular Injection
Dissolve 1.2 MU of PGB in 4 mL of 0.9% sodium chloride injection solution. The injection site for PGB is located on the outer third of the line connecting the anterior superior iliac spine to the coccyx. The operator uses the left thumb and forefinger to pull the patient’s skin away from the injection site. The right hand holds the syringe with the needle at a 90° angle to the injection site. The needle is quickly inserted to a depth of approximately 2.5 cm (two-thirds of the needle length). After aspirating the syringe to ensure there is no blood reflux, the medication is injected slowly. After the injection, the site is covered with a sterile dry cotton swab and the needle is withdrawn quickly. The injection site is then covered with sterile gauze.
Modified Intramuscular Injection
Dissolve 1.2 MU of PGB in 3.5mL of 0.2% lidocaine solvent. Slowly inject the 0.2% lidocaine along the wall of the vial during preparation. After thorough dissolution, disinfect the patient’s skin and inject the drug using the ”Z-track technique:6 the operator uses the index, middle and ring fingers of the left hand to displace the patient’s skin and subcutaneous tissue in a single direction, with a displacement of approximately 2.0 to 3.0 cm. This manoeuvre is maintained until needle insertion is complete. The right hand then quickly inserts the needle to a depth of approximately two-thirds of its length (approximately 2.5 cm). After aspirating the syringe to confirm that there is no blood reflux, the drug is slowly injected. When the injection is complete, the syringe is withdrawn and the left hand releases the skin and subcutaneous tissue, allowing them to return to their original position. This manoeuvre facilitates closure of the injection channel and prevents drug leakage. Finally, sterile gauze is applied to cover the injection site.
Assessment of Efficacy
Pain is assessed using a visual analogue scale (VAS) ranging from 0 to 10. Nurses draw a 10 cm line on paper with 0 and 10 at each end, with 0 representing no pain and 10 representing severe pain. Immediately after the injection and 30 minutes later, patients were asked to correctly rate the pain at both injection sites using the VAS. Patients were observed for 30 minutes after injection to ensure there are no adverse reactions before being allowed to leave. During the 30-minute observation period, patients were informed about possible adverse reactions after injection (such as nodules, swelling, etc.) and how to manage them. A follow-up telephone call is made to the patient on the third day after the injection to inquire about any adverse reactions, such as nodules, and to record the findings.
Statistical Analysis
Measurement data following a normal distribution are expressed as mean ± standard deviation ( ), and group comparisons are made using paired t-tests. Where data did not follow a normal distribution, non-parametric tests were used for group comparisons. Count data are described using frequencies and rates, and group comparisons are made using the chi-squared test or Fisher’s exact test. Statistical analysis was performed using GraphPad Prism 9.5.0 software. A P-value <0.05 indicates statistical significance.
), and group comparisons are made using paired t-tests. Where data did not follow a normal distribution, non-parametric tests were used for group comparisons. Count data are described using frequencies and rates, and group comparisons are made using the chi-squared test or Fisher’s exact test. Statistical analysis was performed using GraphPad Prism 9.5.0 software. A P-value <0.05 indicates statistical significance.
Results
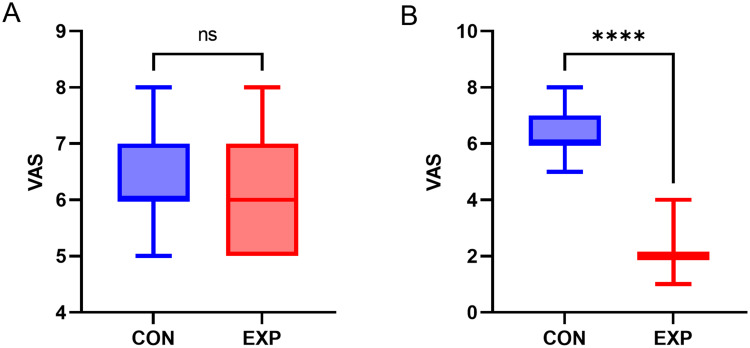
A total of 32 patients participated in the study, including 12 males (37.7%) and 20 females (62.5%), ranging in age from 18 to 70 years, with a mean age of 49 years. Table 1 provides demographic information and detailed clinical data. There was no statistically significant difference in pain scores immediately after injection (Figure 1A). However, the intervention group had significantly lower pain scores than the control group 30 minutes after injection (P < 0.0001) (Figure 1B). When comparing the incidence of induration reactions between the two groups, the intervention group had a lower incidence of nodules (6.25%) than the control group (31.25%), which was statistically significant (P < 0.05). Chi-squared analysis showed that age, gender and BMI did not significantly affect pain scores 30 minutes after injection in either the control or experimental groups, with p-values ranging from 0.078 to 0.553. No patients in our study experienced allergic or Jarisch-Herxheimer reactions, confirming that lidocaine solvent does not increase the incidence of adverse reactions.
Table 1.
Demographic and Clinical Data of the 32 Patients
| Characteristics | Number of Patients (%) n=32 |
|---|---|
| Age | |
| <40 | 7(21.875) |
| ≥40 | 25(78.125) |
| Gender | |
| Males | 12(37.5) |
| Females | 20(62.5) |
| BMI | |
| <18.5 | 1(3.125) |
| >24 | 15(46.875) |
| 18.5–24 | 16(50) |
| Comorbidities (Yes/No) | |
| No | 23(71.875) |
| Yes | 9(28.125) |
Figure 1.
The scale of the visual analogue scale (VAS): (A) shows the immediate pain scores (red is the experimental buttock, the blue is the controls), and (B) shows the 30-minute pain scores (ed is the experimental buttock, the blue is the controls). ****P < 0.001.
Discussion
The severity of pain after a PGB injection can reduce adherence to treatment,7 so improving tolerability could potentially improve adherence. Other studies have shown that combining local anaesthetics with other drugs for different indications, such as lidocaine with kanamycin, can significantly reduce pain immediately after injection without compromising treatment efficacy.8 The Z-track technique has been used in various conditions to improve pain and drug leakage during intramuscular injections.9,10
In our study, we combined these two techniques to improve the pain associated with penicillin injections. Our results showed that the pain scores 30 minutes after injection in the intervention group were lower than those in the control group, with a statistically significant difference (P < 0.0001), indicating that the modified intramuscular injection method of PGB can reduce injection pain. Studies have shown that lidocaine can inhibit cell depolarization, block nerve impulse conduction and pain transmission pathways, which is beneficial for relieving the pain caused by PGB injections. There was no significant statistical difference in pain scores immediately after injection between the two groups, but there was a statistically significant difference in pain scores 30 minutes after injection. The statistical results of the incidence rate of local nodules showed that the intervention group had a lower incidence rate of nodules (6.25%) compared to the control group (31.25%), which was statistically significant (P < 0.05), indicating that the modified intramuscular injection method of PGB can reduce the incidence rate of local nodules after injection.
Studies have shown that after suspension injection, the dispersed medium is absorbed by the tissue and the active agent, penicillin G, forms a drug reservoir at the injection site, slowly releasing the drug. However, such drugs are not readily absorbed into the capillaries of muscle tissue, leading to muscle fiber degeneration, local tissue edema, poor drug absorption and nodule formation.11 In addition to its significant analgesic effect, lidocaine injection solution also has a local muscle relaxant effect. In addition, as a membrane stabilizer, lidocaine can inhibit the adhesion of neutrophil aggregates, reduce the release of inflammatory factors and alleviate inflammatory reactions.12 The Z-track injection technique can seal the liquid in the deep layers of the muscle, facilitating the dispersion and absorption of suspended particles and reducing the incidence of nodules. It is conceivable that our method may improve the overall injection experience and possibly enhance drug absorption, although further research is needed to confirm these effects.
A major strength of this study is its demonstration that the combination of PGB with anaesthetics and the use of the Z-track injection technique not only reduces delayed pain in syphilis patients, but also reduces induration reactions. However, a limitation of our study is that the majority of our patients were not pregnant women with syphilis or congenital syphilis patients, and the sex ratio was not balanced. This may affect the generalisability of the results to women or patients of different ages. In addition, it remains unclear whether the reduction in pain is due to the Z-track technique, the use of lidocaine, or a combination of both. Our study does not provide enough evidence to distinguish the individual effects of each technique. Future research should focus on isolating and evaluating the contributions of each technique to better understand their specific roles in pain management.
Conclusions
This study shows that the combined use of penicillin G benzathine (PGB) with a local anaesthetic and the “Z” track injection technique not only reduces the delayed pain of intramuscular injection in syphilis patients, but also reduces the incidence of induration reactions. We recommend the use of this method for the treatment of primary syphilis. Further research is needed to confirm the long-term efficacy and safety of this method, to assess its applicability to different patient populations, and to evaluate its impact on overall treatment outcomes. Future studies should also explore its potential benefits in combination with other treatments.
Acknowledgments
The authors thank all the patients who participated in the study.
Funding Statement
There is no funding to report.
Data Sharing Statement
The data supporting the results of this study are available on reasonable request from the corresponding author.
Ethical statements
This study was conducted in accordance with the tenets of the Declaration of Helsinki of 1964 and its subsequent amendments or equivalent ethical standards. Written informed consent was obtained from each participant.
Author Contributions
All authors have made a substantial contribution to the work reported, be it conception, design, execution, acquisition of data, analysis and interpretation, or all of these; have been involved in drafting, revising, or critically reviewing the article; have given final approval of the version to be published; have agreed on the journal to which the article will be submitted; and agree to accept responsibility for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Peeling RW, Mabey D, Chen X-S, et al. Syphilis. Lancet. 2023;402(10398):336–346. doi: 10.1016/S0140-6736(22)02348-0 [DOI] [PubMed] [Google Scholar]
- 2.Rowley J, Vander Hoorn S, Korenromp E, et al. Chlamydia, gonorrhoea, trichomoniasis and syphilis: global prevalence and incidence estimates, 2016. Bull World Health Organ. 2019;97(8):548–562. doi: 10.2471/BLT.18.228486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hazra A, Collison MW, Davis AM. CDC sexually transmitted infections treatment guidelines, 2021. JAMA. 2022;327(9):870–871. doi: 10.1001/jama.2022.1246 [DOI] [PubMed] [Google Scholar]
- 4.Estrada V, Santiago E, Cabezas I, et al. Tolerability of IM penicillin G benzathine diluted or not with local anesthetics, or different gauge needles for syphilis treatment: a randomized clinical trial. BMC Infect Dis. 2019;19(1):883. doi: 10.1186/s12879-019-4490-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sanlialp Zeyrek A, Takmak Ş, Kurban NK, et al. Systematic review and meta-analysis: physical-procedural interventions used to reduce pain during intramuscular injections in adults. J Adv Nurs. 2019;75(12):3346–3361. doi: 10.1111/jan.14183 [DOI] [PubMed] [Google Scholar]
- 6.Pullen RL Jr. Administering medication by the Z-track method. Nursing. 2005;35(7):24. doi: 10.1097/00152193-200506000-00016 [DOI] [PubMed] [Google Scholar]
- 7.Nir Y, Sabo E, Paz A, et al. Fear of injections in young adults: prevalence and associations. Am J Trop Med Hyg. 2003;68(3):341–344. doi: 10.4269/ajtmh.2003.68.341 [DOI] [PubMed] [Google Scholar]
- 8.Clement ME, Okeke NL, Hicks CB. Treatment of syphilis: a systematic review. JAMA. 2014;312(18):1905–1917. doi: 10.1001/jama.2014.13259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Altun I. May the Z-tracking technique to prevent any leakage in insulin injection be an alternative to the 10-second waiting technique? J Diabetes Sci Technol. 2018;12(2):537–538. doi: 10.1177/1932296817730378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yilmaz D, Khorshid L, Dedeoglu Y. The effect of the z-track technique on pain and drug leakage in intramuscular injections. Clin Nurse Spec. 2016;30(6):E7–E12. doi: 10.1097/NUR.0000000000000245 [DOI] [PubMed] [Google Scholar]
- 11.Greenblatt DJ, Allen MD. Intramuscular injection-site complications. JAMA. 1978;240(6):542–544. doi: 10.1001/jama.1978.03290060044011 [DOI] [PubMed] [Google Scholar]
- 12.Amir J, Ginat S, Cohen YH, et al. Lidocaine as a diluent for administration of benzathine penicillin G. Pediatr Infect Dis J. 1998;17(10):890–893. doi: 10.1097/00006454-199810000-00008 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data supporting the results of this study are available on reasonable request from the corresponding author.