Abstract
Background and Aims:
Caudal block is more frequently used in children for postoperative analgesia. However, its disadvantage is its short duration. Erector spinae plane block (ESPB) at the sacral level can potentially block the pudendal nerve. It may prove an alternative to caudal block for hypospadias repair regarding time to first rescue analgesia.
Methods:
Fifty children of 2–7 years of age were included. After induction of general anaesthesia, Group I (n = 25) was given ultrasound-guided sacral ESPB with 1 ml/kg of 0.25% bupivacaine and Group II (n = 25) was given caudal block with 0.5 ml/kg of 0.25% bupivacaine. Postoperatively at face, leg, activity, cry, consolability (FLACC) score ≥4, rescue analgesia was given using intravenous 15 mg/kg paracetamol. The primary outcome was to compare time to first rescue analgesia, and secondary outcomes were intraoperative haemodynamic parameters, fentanyl consumption, postoperative FLACC score and analgesic consumption in 24 h. Continuous variables were compared using the independent sample t-test or Mann–Whitney test, and categorical variables were compared using the Chi-square test.
Results:
The mean time to first rescue analgesia was 21.30 (standard deviation [SD]: 3.06) h in Group I and 9.36 (SD: 1.71) h in Group II (P < 0.001) (mean difference −11.94 [95% CI: −13.39, −10.48]). The FLACC score was significantly higher (P < 0.05) postoperatively at 8, 10, 12 and 18 h in Group II. Mean postoperative analgesic consumption was 310.5 (SD: 72.69) mg in Group I and 615.6 (SD: 137.51) mg in Group II (P < 0.001) (mean difference 30.5 [95% CI: 236.41, 373.78]).
Conclusion:
Sacral ESPB is better regarding time to first rescue analgesia than caudal block in paediatric patients undergoing hypospadias repair.
Keywords: Caudal block, children, epidural block, hypospadias, paediatric, rescue analgesia, sacral erector spinae block, ultrasound
INTRODUCTION
Caudal block is the most commonly used block for postoperative analgesia in children undergoing hypospadias repair. Though simple, with a high success rate, the duration of action is short, which may result in inadequate postoperative analgesia. This postoperative pain further leads to the administration of analgesics to control pain.[1]
Erector spinae plane block (ESPB) promises to provide visceral and somatic analgesia and has been used at thoracic, lumbar and sacral levels. Sacral ESPB was first performed by Tulgar et al.[2] via a parasagittal approach. Aksu et al.[3] used sacral ESPB with 1 ml/kg of 0.25% bupivacaine via midline approach for hypospadias repair to provide bilateral analgesia. Sacral ESPB is a novel block that is simple, safe and effective for a long duration. In addition, patients remained haemodynamically stable. ESPB at the sacral level can potentially block the pudendal nerve and may prove a better alternative to the caudal block for hypospadias repair.
So, this study was conducted to compare sacral ESPB and caudal block for postoperative analgesia in children undergoing hypospadias repair. We hypothesised that ultrasonography-guided (USG) sacral ESPB may be more effective regarding time to first rescue analgesia in paediatric patients undergoing surgery for hypospadias repair. The primary objective was time to first rescue analgesia in children undergoing hypospadias repair with USG sacral ESPB or caudal epidural block. The secondary objectives were to compare intraoperative haemodynamic parameters (heart rate, systolic and diastolic blood pressure), fentanyl consumption and postoperative face, leg, activity, cry, controllability (FLACC) score and analgesic consumption in 24 h.
METHODS
This study was conducted from April 2023 to September 2023 in a randomised and double-blind manner after obtaining approval from the Institutional Ethics Committee (vide approval number BREC/23/35-37 dated 31 January 2023). The study was registered in the Clinical Trials Registry-India (vide registration number CTRI/2023/03/050959 dated 22 March 2023, https://ctri.nic.in/). Fifty paediatric male patients, aged 2–7 years, with American Society of Anesthesiologists (ASA) physical status I or II, scheduled to undergo elective surgery for hypospadias repair under general anaesthesia were included in the study. Patients with a history of developmental delay, allergic reactions to local anaesthetic, infection at the puncture site and parental refusal were excluded from the study. Written informed consent was obtained from parents for participation in the study and use of the patient data for research and educational purposes. The study was carried out using the principles of the Declaration of Helsinki, 2013, and good clinical practice.
All children were evaluated one day before surgery. Investigations, including haemoglobin, bleeding time, clotting time and complete urine examination, were reviewed. Patients were kept nil per oral, 6 h for solids, 4 h for mother’s milk and 2 h for clear fluids. Oral midazolam 0.5 mg/kg was given 30 min before surgery. After shifting the patient to the operating room, standard ASA monitors were attached, including five lead electrocardiogram, non-invasive blood pressure and oxygen saturation (SpO2). Inhalational induction of anaesthesia was standardised using 6–8% sevoflurane in 100% oxygen. Intravenous (IV) cannulation was done with an appropriate-size cannula. Intravenous (IV) glycopyrrolate 0.005 mg/kg and fentanyl 2 µg/kg were administered. After checking the adequacy of ventilation, IV atracurium 0.5 mg/kg was provided to facilitate the supraglottic airway device placement. Maintenance of anaesthesia was done with of 1% sevoflurane and 50% nitrous oxide in oxygen.
Computer-generated random sequence numbers were used for randomisation. Random allocation into two groups was done with an allocation ratio of 1:1. Allocation concealment was done using sequentially numbered opaque-sealed envelope method, by the operation theatre technician after induction of anaesthesia. An independent observer did the data collection. The enroled participants and independent data-collecting persons were unaware of the patient’s group allocation.
Group I (n = 25) patients were administered a USG-guided sacral ESPB with 1 ml/kg of 0.25% bupivacaine, and Group II (n = 25) was given a USG-guided caudal epidural block with 0.5 ml/kg 0.25% bupivacaine by the investigator who was not involved in data collection.
In Group I, after anaesthesia and before the surgery, the patient was turned to the right lateral position to perform sacral ESPB. After aseptic preparation of the block site, a high-frequency 13-6 MHz linear ultrasound probe was placed longitudinally in the midline just over the sacrum (Sonosite M-Turbo ultrasound machine, Fujifilm Sonosite Inc., USA). Median sacral crests and erector spinae muscles were identified. A 21 gauge, 38 mm needle was inserted using an in-plane technique and was advanced from cranial to caudal direction until its tip touched the top of the fourth median sacral crest [Figure 1]. Following negative aspiration, 1 ml/kg of 0.25% bupivacaine was administered.
Figure 1.
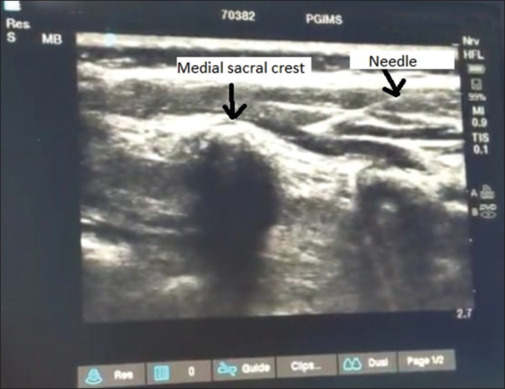
Ultrasound image showing sacral erector spinae block (needle touching median sacral crest)
In Group II, after anaesthesia and before the surgery, the patient was turned to the left lateral position to perform a caudal epidural block. A high-frequency 13-6 MHz linear ultrasound probe was placed transversely over the coccyx to obtain the transverse sonographic view of the sacral hiatus (Sonosite M-Turbo ultrasound machine, Fujifilm Sonosite Inc., USA). Then, the transducer was rotated to 90° to obtain a longitudinal view of the sacral hiatus. A 21 gauge, 38 mm needle was inserted from the probe’s edge using an in-plane technique and then advanced into the sacral canal through the sacrococcygeal membrane [Figure 2]. After negative aspiration, 0.5 ml/kg of 0.25% bupivacaine was administered. After performing the block, patients were turned to supine position in both groups.
Figure 2.
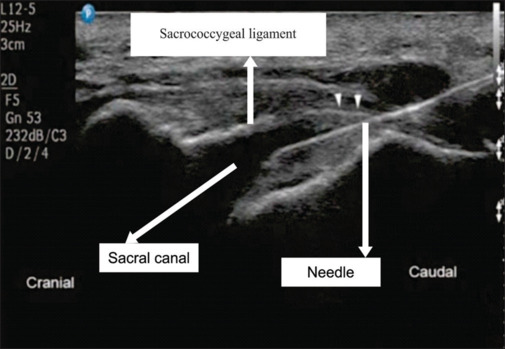
Ultrasound image showing caudal block (needle in sacral canal)
In both groups, an increase in heart rate of more than 20% above the baseline values at any time during the surgery was considered insufficient analgesia and IV fentanyl 1 µg/kg was given. Further maintenance of anaesthesia was done as per the requirement of the case. After the surgery, the residual neuromuscular blockade was reversed by administering IV neostigmine 0.05 mg/kg and glycopyrrolate 0.01 mg/kg, and the supraglottic device was removed. After regaining consciousness, patients were shifted to post anaesthesia care unit. Pain assessment was done postoperatively using FLACC score at 0 h, every 15 min up to 1 h, at 1½, 2, 4, 6, 8, 10, 12 h and then at 18 and 24 h postoperatively. Rescue analgesia was given at a FLACC score of ≥4. The patient was given IV 15 mg/kg of paracetamol infusion as the first rescue analgesia, but it was not given more frequently than 6 h. If pain persisted after paracetamol administration, oral ibuprofen 10 mg/kg was given as a second rescue analgesia but not more frequently than 8 h. At the time of pain assessment, if the child was sleeping comfortably, he was not disturbed and was assumed to be pain free.
Heart rate (HR), systolic blood pressure (SBP) and diastolic blood pressure (DBP) were recorded before induction of general anaesthesia, before the block, after the block, before incision, immediately after the incision and then every 10-min interval till the end of surgery. Intraoperative additional IV fentanyl consumption was also recorded. Postoperatively, the FLACC score, the time required for the first rescue analgesia and the analgesia consumption (paracetamol) in 24 h were recorded.
The sample size was calculated using Epi Info Software (statistical software manufactured by the Centers for Disease Control and Prevention, Atlanta, Georgia (USA). As per the pilot study of 10 cases (five cases in each group), the time to first rescue analgesia was 12.4 (standard deviation [SD]: 4.28) h in the sacral erector spinae block and 6.61 (SD: 0.76) h in the caudal block. We defined a mean difference of 5.79 h for sample size calculation with a 6.5 SD. We calculated the sample size with a 95% confidence interval (CI), 80% power and an alpha level of 0.05. Thus, the sample size was 20 in each group. To balance dropout, the sample size was estimated as 25 in each group.
At the end of the study, all data were compiled and analysed using Statistical Package for the Social Sciences (SPSS) version 25.0 for Windows software program (SPSS Inc., International Business Machines Corporation, Armonk, New York, United States). The data was checked for normality before statistical analysis using the Kolmogorov–Smirnov test. Data on age, weight, duration of surgery, time to first rescue analgesia and total analgesic (paracetamol) consumption in 24 h were normal, and the data on the FLACC score was non-normal. Quantitative variables age, weight, duration of surgery, time to first rescue analgesia and total analgesic (paracetamol) consumption in 24 h were presented as mean (standard deviation). Age, weight and duration of surgery were compared using an independent sample t-test. Mann–Whitney test was used to compare mean FLACC scores. Time to first rescue analgesia and total analgesic (paracetamol) consumption in 24 h were compared using an independent sample t-test. Qualitative variables (number of patients requiring analgesic doses) were presented as frequencies/percentages, and a Chi-square test was used for comparison. A P value < 0.05 was considered statistically significant.
RESULTS
Fifty patients were recruited, and all completed the study [Figure 3]. Both groups were comparable in terms of demographic profile and duration of surgery [Table 1]. The mean time to first rescue analgesia was significantly longer in Group I (P < 0.001) (mean difference: −11.94 [95% CI: −13.39, −10.48]) [Table 2]. Mean HR, SBP and DBP were comparable between the two groups at different timelines. Total intraoperative additional IV fentanyl consumption was nil in both groups. The mean FLACC score for Group I was significantly less (P < 0.05) (mean difference: 0.8 [95% CI: 0.69, 0.9]) [Table 2]. FLACC score was significantly higher (P < 0.05) postoperatively at 8, 10, 12 and 18 h in Group II. The mean postoperative analgesic consumption (paracetamol) in Group I was significantly less (mean difference: 30.5 [95% CI: 236.4, 373.78] mg [Table 2]. In Group I, 5 patients did not require any analgesic and 20 patients required only one dose of analgesic postoperatively. In Group II, 23 patients required two doses of analgesic, and 2 required three doses of analgesic postoperatively (P < 0.001) [Table 2].
Figure 3.
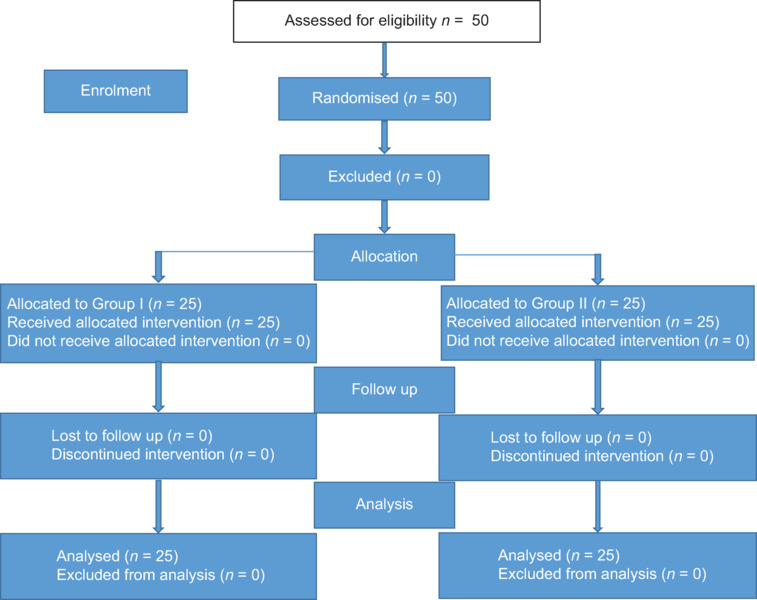
Consolidated standards of reporting trials flow diagram
Table 1:
Demographic variables and duration of surgery of the participants
| Parameter | Group I (n=25) | Group II (n=25) |
|---|---|---|
| Age (years), Mean (SD) | 4.76 (1.69) | 4.96 (1.59) |
| Weight (kg), Mean (SD) | 20.68 (4.96) | 19.84 (4.31) |
| Duration of surgery (min), Mean (SD) | 57.0 (3.23) | 55.8 (4.25) |
Data expressed as mean (standard deviation). SD=standard deviation, n=number of patients
Table 2:
Comparison of postoperative parameters between the two groups
| Parameter | Group I (n=25) | Group II (n=25) | Mean difference (95% CI) | P |
|---|---|---|---|---|
| FLACC score, Mean (SD) | 0.314 (0.81) | 1.14 (1.54) | 0.8 (0.69, 0.9) | 0.040 |
| Time to first rescue analgesia, Mean (SD) (h) | 21.30 (3.06) | 9.36 (1.71) | −11.94 (−13.39, −10.48) | <0.001 |
| Postoperative analgesic (paracetamol) consumption in 24 h (mg), Mean (SD) | 310.5 (72.69) | 615.6 (137.51) | 30.5 (236.41, 373.78) | <0.001 |
| Number of doses of rescue analgesia – 0/1/2/3, n | 5/20/0/0 | 0/0/23/2 | – | <0.001 |
Data expressed as mean (standard deviation) or number of patients. CI=confidence interval, n=number of patients, FLACC score=face, leg, activity, cry, controllability score
DISCUSSION
This study demonstrated that the time of first rescue analgesia was longer and that the FLACC score and postoperative analgesic (paracetamol) consumption were lesser with sacral ESPB.
ESPB has been effective at thoracic and lumbar levels in various studies.[4,5,6] Sacral ESPB is an interfascial plane block that provides somatic and visceral analgesia, blocking spinal nerves’ dorsal and ventral rami. ESPB at the sacral level can potentially block the pudendal nerve.[7] Bilateral effect can be produced with a single injection using the midline approach.[3] Oksuz et al.[8] observed the duration of sacral ESPB to be 24 h in a 7-month-old boy scheduled for anoplasty. Few case reports mentioned sacral ESPB for postoperative analgesia and radicular pain treatment.[7,9,10,11] Kaya et al.[12] used it as a sole anaesthetic technique in two adult patients scheduled for anal fistulectomy.
Bansal et al.[13] evaluated USG sacral ESPB for postoperative analgesia in paediatric patients undergoing hypospadias repair. They observed that postoperative analgesic consumption was significantly less in the sacral ESPB group than in the control group. In a recent study, Mermer et al.,[14] evaluated the analgesic effect of sacral ESPB on post-hemorrhoidectomy pain in adult patients. They observed significantly low pain scores and decreased tramadol consumption in sacral ESPB up to 24 h.
The results of this study are in contrast to those of a study conducted by Elbadry et al.,[15] who observed no significant difference in time to first rescue analgesia between the caudal group and the sacral ESPB in children undergoing hypospadias repair. It may be due to the reason that these authors used fentanyl in a dose of 1 µg/kg at the time of induction of anaesthesia. In contrast, 2 µg/kg was used in this study. Other factors contributing to this difference may be the differences in the experience of anaesthesiologists and different approaches (bilateral approach vs midline approach in this study). Similar to this study, Raghove et al.[16] observed the duration of the caudal block to be 8 h. Mohamed et al.[17] used dexamethasone as an additive for caudal block, and the duration of analgesia was observed to be 9.2 (SD: 0.9) h despite using the additive. In the current study, the duration of the sacral ESPB was observed to be longer compared to various studies in which additives were even added to the caudal block.
Additionally, FLACC score and postoperative analgesic (paracetamol) consumption were lower in the sacral ESPB group. In contrast, Elbadry et al.[15] observed comparable pain scores and pethidine consumption between sacral ESPB and caudal blocks. Hassan et al.[1] compared a combination of dexamethasone and dexmedetomidine as adjuvants to bupivacaine versus dexamethasone or dexmedetomidine to bupivacaine in paediatric caudal block. They observed that the pain score increased at 12 h in all the groups. In this study, the FLACC score increased at 18 h in Group I and 8 h in Group II. FLACC score has been observed to be comparatively less even at 18 h in sacral ESPB group, which further signifies the superior analgesic efficacy of sacral ESPB compared to caudal block.
No bradycardia or hypotension was observed in the sacral ESPB group and caudal group, and patients remained haemodynamically stable intraoperatively. Elbadry et al.[15] observed significantly higher hypotension in the caudal group than in the sacral ESPB. A dose of 1 ml/kg of 0.25% bupivacaine for the caudal block is most likely the reason for this hypotension in their study, whereas 0.5 ml/kg of 0.25% bupivacaine was used in the current study.
The strength of this study is the non-inferiority of sacral ESPB as compared to caudal block, including various advantages of sacral ESPB. It is easy to perform under USG guidance because it is applied relatively superficially, and the injection site is not close to major vascular and neural structures. It can widely spread under the muscle depending on the volume and allows long-term analgesia without motor block. In addition, it provides coverage of multiple dermatomal levels by a longitudinal midline technique, and the patient remains haemodynamically stable.[15] The study’s limitations are that it is a single-centre study, has a relatively small sample size and lacks long-term follow-up to assess outcomes beyond 24 h postoperatively. Limited literature is available on the use of sacral ESPB in children. Therefore, further trials enroling more patients are needed in this direction in the future.
CONCLUSION
USG-guided sacral ESPB using the midline approach significantly prolongs the duration of postoperative analgesia when compared to USG-guided caudal block in children undergoing hypospadias repair.
Study data availability
De-identified data may be requested with reasonable justification from the authors (email to the corresponding author) and shall be shared upon request.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Hassan PF, Hassan AS, Elmetwally SA. Caudal analgesia for hypospadias in pediatrics: Comparative Evaluation of adjuvants dexamethasone and dexmedetomidine combination versus dexamethasone or dexmedetomidine to bupivacaine: A prospective, double-blinded, randomized comparative study. Anesth Essays Res. 2018;12:644–50. doi: 10.4103/aer.AER_77_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tulgar S, Senturk O, Thomas DT, Deveci U, Ozer Z. A new technique for sensory blockage of posterior branches of sacral nerves: Ultrasound guided sacral erector spinae plane block. J Clin Anesth. 2019;57:129–30. doi: 10.1016/j.jclinane.2019.04.014. [DOI] [PubMed] [Google Scholar]
- 3.Aksu C, Gurkan Y. Sacral Erector Spinae Plane Block with longitudinal midline approach: Could it be the new era for pediatric postoperative analgesia? J Clin Anesth. 2020;59:38–9. doi: 10.1016/j.jclinane.2019.06.007. [DOI] [PubMed] [Google Scholar]
- 4.Mostafa SF, Abdelghany MS, Abdelraheem TM, Abu Elyazed MM. Ultrasound guided erector spinae plane block for postoperative analgesia in paediatric patients undergoing splenectomy: A prospective randomized controlled trial. Pediatr Anesth. 2019;29:1201–7. doi: 10.1111/pan.13758. [DOI] [PubMed] [Google Scholar]
- 5.Singh S, Jha RK, Sharma M. The analgesic effect of bilateral ultrasound guided erector spinae plane block in paediatric lower abdominal surgeries: A randomised, prospective trial. Indian J Anaesth. 2020;64:762–7. doi: 10.4103/ija.IJA_630_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.El-Emam ESM, El Motlb EA. Ultrasound guided erector spinae versus ilioingui- nal/iliohypogastric block for postoperative analgesia in children undergoing inguinal surgeries. Anesth Essays Res. 2019;13:274–9. doi: 10.4103/aer.AER_81_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kukreja P, Deichmann P, Selph JP, Hebbard J, Kalagara H. Sacral erector spinae plane block for gender reassignment surgery. Cureus. 2020;12:e7665. doi: 10.7759/cureus.7665. doi: 10.7759/cureus.7665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oksuz G, Arslan M, Bilal B, Gisi G, Yavuz C. Ultrasound guided sacral erector spinae block for postoperative analgesia in pediatric anoplasty surgeries. J Clin Anesth. 2019;60:88. doi: 10.1016/j.jclinane.2019.08.006. doi: 10.1016/j.jclinane.2019.08.006. [DOI] [PubMed] [Google Scholar]
- 9.Piraccini E, Antioco M, Maitan S. Ultrasound guided sacral erector spinae plane block: A useful tool for radicular pain treatment. J Clin Anesth. 2020;59:11–2. doi: 10.1016/j.jclinane.2019.06.011. [DOI] [PubMed] [Google Scholar]
- 10.Kilicaslan A, Aydin A, Kekec AF, Ahiskalioglu A. Sacral erector spinae plane block provides effective postoperative analgesia for pelvic and sacral fracture surgery. J Clin Anesth. 2020;61:83–4. doi: 10.1016/j.jclinane.2019.109674. [DOI] [PubMed] [Google Scholar]
- 11.Bilge A, Arican S. Sacral erector spinae plane block for analgesia after hip surgery. J Surg Med. 2021;5:648–50. [Google Scholar]
- 12.Kaya C, Dost B, Tulgar S. Sacral erector spinae plane block provides surgical anaesthesia in ambulatory anorectal surgery: Two case Reports. Cureus. 2021;13:e12598. doi: 10.7759/cureus.12598. doi: 10.7759/cureus.12598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bansal T, Yadav N, Singhal S, Kadian Y, Lal J, Jain M. Evaluation of USG guided novel sacral erector spinae block for postoperative analgesia in pediatric patients undergoing hypospadias repair: A randomized controlled trial. J Anaesthesiol Clin Pharmacol. 2024;40:330–5. doi: 10.4103/joacp.joacp_418_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mermer A, Simsek G, Mermer HA, Tire Y, Kozanhan B. Effect of sacral erector spinae plane block on post-hemorrhoidectomy pain: A randomized controlled trial. Medicine. 2023;102:37e35168. doi: 10.1097/MD.0000000000035168. doi: 10.1097/MD.0000000000035168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Elbadry AA, Elrahwan SM, Mostafa TAH, Elahwal L. Analgesic effect of sacral erector spinae, penile and caudal block after hypospadias surgery: A randomized single blind controlled trial. Egypt J Anaesth. 2023;39:563–70. [Google Scholar]
- 16.Raghove P, Singh K, Saini S, Hooda S. Feasibility and effectiveness of ultrasound guided caudal epidural block in adolescents undergoing surgery for hypospadias. Indian J Appl Res. 2016;6:377–9. [Google Scholar]
- 17.Mohamed A. Evaluation of the analgesic effect of caudal dexamethasone combined with bupivacaine in hypospadias repair surgery. Res Opin Anesth Intensive Care. 2016;3:42–7. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
De-identified data may be requested with reasonable justification from the authors (email to the corresponding author) and shall be shared upon request.


