Summary
Background
Lower respiratory infections (LRIs) are a major global contributor to morbidity and mortality. In 2020–21, non-pharmaceutical interventions associated with the COVID-19 pandemic reduced not only the transmission of SARS-CoV-2, but also the transmission of other LRI pathogens. Tracking LRI incidence and mortality, as well as the pathogens responsible, can guide health-system responses and funding priorities to reduce future burden. We present estimates from the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2021 of the burden of non-COVID-19 LRIs and corresponding aetiologies from 1990 to 2021, inclusive of pandemic effects on the incidence and mortality of select respiratory viruses, globally, regionally, and for 204 countries and territories.
Methods
We estimated mortality, incidence, and aetiology attribution for LRI, defined by the GBD as pneumonia or bronchiolitis, not inclusive of COVID-19. We analysed 26 259 site-years of mortality data using the Cause of Death Ensemble model to estimate LRI mortality rates. We analysed all available age-specific and sex-specific data sources, including published literature identified by a systematic review, as well as household surveys, hospital admissions, health insurance claims, and LRI mortality estimates, to generate internally consistent estimates of incidence and prevalence using DisMod-MR 2.1. For aetiology estimation, we analysed multiple causes of death, vital registration, hospital discharge, microbial laboratory, and literature data using a network analysis model to produce the proportion of LRI deaths and episodes attributable to the following pathogens: Acinetobacter baumannii, Chlamydia spp, Enterobacter spp, Escherichia coli, fungi, group B streptococcus, Haemophilus influenzae, influenza viruses, Klebsiella pneumoniae, Legionella spp, Mycoplasma spp, polymicrobial infections, Pseudomonas aeruginosa, respiratory syncytial virus (RSV), Staphylococcus aureus, Streptococcus pneumoniae, and other viruses (ie, the aggregate of all viruses studied except influenza and RSV), as well as a residual category of other bacterial pathogens.
Findings
Globally, in 2021, we estimated 344 million (95% uncertainty interval [UI] 325–364) incident episodes of LRI, or 4350 episodes (4120–4610) per 100 000 population, and 2·18 million deaths (1·98–2·36), or 27·7 deaths (25·1–29·9) per 100 000. 502 000 deaths (406 000–611 000) were in children younger than 5 years, among which 254 000 deaths (197 000–320 000) occurred in countries with a low Socio-demographic Index. Of the 18 modelled pathogen categories in 2021, S pneumoniae was responsible for the highest proportions of LRI episodes and deaths, with an estimated 97·9 million (92·1–104·0) episodes and 505 000 deaths (454 000–555 000) globally. The pathogens responsible for the second and third highest episode counts globally were other viral aetiologies (46·4 million [43·6–49·3] episodes) and Mycoplasma spp (25·3 million [23·5–27·2]), while those responsible for the second and third highest death counts were S aureus (424 000 [380 000–459 000]) and K pneumoniae (176 000 [158 000–194 000]). From 1990 to 2019, the global all-age non-COVID-19 LRI mortality rate declined by 41·7% (35·9–46·9), from 56·5 deaths (51·3–61·9) to 32·9 deaths (29·9–35·4) per 100 000. From 2019 to 2021, during the COVID-19 pandemic and implementation of associated non-pharmaceutical interventions, we estimated a 16·0% (13·1–18·6) decline in the global all-age non-COVID-19 LRI mortality rate, largely accounted for by a 71·8% (63·8–78·9) decline in the number of influenza deaths and a 66·7% (56·6–75·3) decline in the number of RSV deaths.
Interpretation
Substantial progress has been made in reducing LRI mortality, but the burden remains high, especially in low-income and middle-income countries. During the COVID-19 pandemic, with its associated non-pharmaceutical interventions, global incident LRI cases and mortality attributable to influenza and RSV declined substantially. Expanding access to health-care services and vaccines, including S pneumoniae, H influenzae type B, and novel RSV vaccines, along with new low-cost interventions against S aureus, could mitigate the LRI burden and prevent transmission of LRI-causing pathogens.
Funding
Bill & Melinda Gates Foundation, Wellcome Trust, and Department of Health and Social Care (UK).
Research in context.
Evidence before this study
Lower respiratory infection (LRI) is a common and deadly infectious disease, particularly in children and older adults. Previous iterations of the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) and estimates from WHO and the Maternal and Child Epidemiology Estimation Group have quantified the LRI burden for select aetiologies in the pre-COVID-19 era. In addition, many studies have estimated the decrease in incidence or mortality due to LRI or select respiratory pathogens during the COVID-19 pandemic, but these studies are generally limited to one or a few surveillance networks, countries, or clinical sites. We searched PubMed with the search terms (“lower respiratory infection*”[Title/Abstract] OR “LRI”[Title/Abstract]) AND (“mortality” OR “incidence”) AND “global*” AND (“etiology” OR “pathogen”) with no language restrictions, for articles published from Jan 1, 2021 to June 16, 2023. We did not identify any studies that evaluated global levels and trends of LRI burden in all ages, attributable to a comprehensive set of aetiologies, across all countries, and inclusive of the COVID-19 pandemic's effects to the year 2021.
Added value of this study
This study provides two key improvements on the past GBD study: expanded aetiology estimation and evaluation of COVID-19 pandemic impact. We produced estimates of non-COVID-19 LRI burden attributable to a comprehensive set of 18 different aetiologies (Acinetobacter baumannii, Chlamydia spp, Enterobacter spp, Escherichia coli, fungi, group B streptococcus, Haemophilus influenzae, influenza, Klebsiella pneumoniae, Legionella spp, Mycoplasma spp, polymicrobial infections, Pseudomonas aeruginosa, respiratory syncytial virus [RSV], Staphylococcus aureus, Streptococcus pneumoniae, and other viruses, as well as a residual category of other bacterial pathogens). 13 of these aetiologies are newly included in the GBD study, significantly expanding our understanding of the diverse causes of LRI. In addition, this research, which models through the year 2021, estimates the reduction in non-COVID-19 LRI incidence and mortality observed during the COVID-19 pandemic period. In addition, we added many new data sources on LRI morbidity and mortality since GBD 2019, which span widely across time and geography, enabling us to revise and improve estimates from previous years. Overall, these enhancements contribute to a more comprehensive and up-to-date understanding of the global burden of LRI, incorporating previously unaccounted for aetiologies and considering the influence of the COVID-19 pandemic on respiratory infections. This information is invaluable for health-care practitioners, policy makers, and researchers in effectively developing targeted interventions to combat LRIs.
Implications of all the available evidence
With a comprehensive understanding of the aetiologies of LRI and their impact, health-care authorities can design targeted interventions to address specific pathogens responsible for respiratory infections. These interventions might include vaccination campaigns, improved infection control measures, and early detection and treatment strategies. This study found S pneumoniae to be the most common cause of LRI deaths in 2021, followed by S aureus and K pneumoniae. During the COVID-19 pandemic, following the implementation of non-pharmaceutical interventions such as facemask use and mobility restrictions, we observed a decline in global influenza and RSV infection incidence and mortality. Since 1990, incidence and mortality due to LRI have greatly decreased, especially in children younger than 5 years, while mortality rates in adults, especially those aged 70 years and older, have had a slower rate of decline. Our analysis particularly highlights the decrease in vaccine-preventable aetiologies, S pneumoniae and H influenzae, and the importance of maintaining and expanding vaccine coverage against these bacteria. We also found high mortality attributable to non-vaccine-preventable aetiologies, including S aureus; development of preventive therapies and vaccines for these pathogens should receive further investment and research. Furthermore, as the threat of antimicrobial resistance grows, robust pathogen surveillance, point-of-care pathogen identification, and implementation of strategies to reduce antibiotic overuse become essential. The LRI burden remains highly inequitable, with both deaths and cases highly concentrated in low-income and middle-income countries; thus, all interventions must be financially accessible and distributed to areas with a high burden of LRI.
Introduction
Lower respiratory infections (LRIs) were the leading infectious cause of death globally in 2019.1, 2 Gram-positive and Gram-negative bacteria, atypical bacteria, viruses, and fungi can all cause LRI. Mortality rates are highest in adults older than 70 years and in children younger than 5 years, and both incidence and mortality are generally higher in males.3, 4, 5 Risk factors for LRI mortality in all age groups include exposure to tobacco smoke, indoor and outdoor particulate matter, and extreme temperatures.3 In children younger than 5 years, wasting is estimated to be responsible for over half of LRI deaths.3 Among adults aged 65 years and older, host-level risk factors can include frailty and presence of comorbid conditions such as asthma.6, 7 Vaccination against Streptococcus pneumoniae is protective against pneumococcal pneumonia in both infants and older adults.7, 8
Among community-acquired bacterial LRIs, S pneumoniae remains the most prevalent pathogen in children and adults and across different income-level settings.9, 10 Historically, Haemophilus influenzae was the second-leading cause of childhood pneumonia.11 However, with the widespread implementation of H influenzae type b (Hib) vaccination, the incidence of H influenzae pneumonia has declined substantially over the past decade.8, 12 Staphylococcus aureus, which is not vaccine-preventable, is a noteworthy cause of complicated pneumonia, with substantially higher rates of poor clinical outcomes, including sepsis and death, than S pneumoniae.13, 14 S aureus also has the ability to develop resistance to multiple antibiotics, posing further barriers to care.15 In school-age children, the atypical bacterium Mycoplasma pneumoniae is a leading cause of pneumonia, with one review estimating that it is responsible for 4–39% of cases of paediatric community-acquired pneumonia.16, 17
Viruses, including influenza and respiratory syncytial virus (RSV), are highly prevalent causes of LRIs, particularly in children.10, 18 A 2021 global meta-analysis estimated that influenza viruses were responsible for 14·1% of adult LRI hospitalisations, or more than 5 million hospitalisations.19 Another global meta-analysis estimated that RSV was responsible for 3·6 million hospitalisations in 2019 among children younger than 5 years.20 In addition, viral infections increase patients' risk for superimposed bacterial infections, most commonly by S pneumoniae and S aureus, causing substantial morbidity and mortality.21
Beginning in 2020, the COVID-19 pandemic promoted the adoption of non-pharmaceutical interventions, including stay-at-home orders, school and community closures, and facemask requirements. These measures effectively curbed the incidence of respiratory infections in 2020 and 2021, for both COVID-19 and other respiratory viruses.22, 23, 24, 25 RSV and influenza infection incidence declined in response to these non-pharmaceutical interventions, although some locations had outbreaks of these viruses in atypical seasons as non-pharmaceutical interventions were relaxed.22, 23, 24, 25
This study presents the results from the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2021, which estimates LRI incidence and mortality, combined with the findings of the Global Research on Antimicrobial Resistance (AMR) project, which estimates LRI pathogen distribution. We aimed to describe the burden and trends of LRIs and the pathogens responsible across 204 countries and territories from 1990 to 2021. Previous GBD studies included estimates of four aetiologies that were not mutually exclusive or collectively exhaustive.2, 26 In the current study, we provide estimates for a comprehensive set of 18 pathogen categories across all age groups.27, 28 Additionally, the estimates for 2020 and 2021 account for the reduction of LRIs seen during the COVID-19 pandemic and implementation of non-pharmaceutical interventions.
Methods
Overview
This Article was produced as part of the GBD Collaborator Network and in accordance with the GBD protocol. GBD 2021 produced estimates of mortality and morbidity due to LRI by age and sex for 204 countries and territories between 1990 and 2021. The Global Burden of AMR study produced estimates of aetiology-specific fatal and non-fatal burdens of select infectious syndromes, including LRI.27 LRI is defined as acute pneumonia or bronchiolitis, not inclusive of COVID-19. ICD codes mapped to LRI in GBD are provided in appendix 1 (pp 17–18) for ICD-9 and ICD-10. The GBD case definition of LRI does not include tuberculosis, pertussis, or COVID-19; although the pathogens that cause these diseases can infect the lower respiratory tract, they are modelled separately due to their individual public health significance and are not included in the GBD category of LRI.
GBD uses a set of modelling tools, described in the sections below, to extrapolate available data out to produce results for the entire global population, by age, sex, and year. Modelling was done at the 1000 draw level, where the point estimate was computed as the mean of 1000 draws, and the 95% uncertainty intervals (UIs) were computed as the 25th and 975th ranked values of 1000 draws. We used the GBD 2021 global population age standard to calculate age-standardised rates, which allow for comparison of rates between locations or years with different age structures.29 In the following sections, we summarise key methods from the GBD and Global Burden of AMR studies for the estimation of LRI and its aetiologies. More details on these methods, including a flowchart, are provided in appendix 1 (pp 4–29). Full descriptions of the GBD and Global Burden of AMR studies have been published previously.2, 27
All metadata for input sources described below are available on the GBD Sources Tool, found on the Global Health Data Exchange (GHDx), which readers can use to identify which sources were used for estimating an outcome in any given location. GBD 2019 complies with the GATHER statement (appendix 1 pp 30–31).30 Statistical code used for GBD estimation is publicly available online on the GHDx.
Mortality estimation
As inputs to the GBD LRI mortality-estimation model, we used a total of 26 259 site-years of data: 23 062 site-years from vital registration, 825 site-years from sample vital registration, 1682 site-years from verbal autopsy, 681 site-years from surveillance sources, and 9 site-years from minimally invasive tissue sampling. Data are processed using a set of standard algorithms accounting for incompleteness, misclassification of the underlying cause of death, garbage coding, and stochastic variability.2
We estimated overall LRI mortality using the Cause of Death Ensemble model (CODEm),31 which evaluates a wide array of potential models using various combinations of covariates and four model classes. Each model class uses either cause fraction or death rate as the outcome variable, and either a mixed-effects linear model or a spatiotemporal Gaussian process model as the regression method. Models included fixed effects on covariates and age dummies. Random effects are applied at the levels of super-region, region, and age in the spatiotemporal model's mixed-effects structure, and at the levels of super-region, region, country, and age in the mixed-effects linear models. In mixed-effects regression, the random effects are assumed to follow a normal distribution with a mean of zero and a variance–covariance matrix that is to be estimated from the data. Models were evaluated using out-of-sample predictive validity and integrated into one ensemble model. A full list of covariates is provided in appendix 1 (pp 8–9). Final LRI mortality estimates are scaled by a procedure known as CoDCorrect to ensure consistency between the sum of cause-specific mortality and the total envelope of all-cause mortality.2
Morbidity estimation
For LRI morbidity estimation, we used data from published studies identified via a systematic review (appendix 1 p 10), surveillance data, LRI mortality estimates (described above), health insurance claims data, and inpatient data.2 To correct for potential systematic bias among different categories of data sources, we used a standardised crosswalking technique to adjust the data to enhance comparability before modelling (appendix 1 pp 10–13). We estimated LRI incidence and prevalence using DisMod-MR 2.1, a compartmental Bayesian meta-regression model that enforces consistency among prevalence, incidence, remission, and mortality.2, 32 More details on DisMod-MR, including information on priors and a full list of covariates, is provided in appendix 1 (pp 15–17).
Aetiology estimation
Data used for aetiology estimation originated from multiple cause-of-death vital registration, hospital discharges, microbial laboratory data, and published studies from the literature.27 Mortality and morbidity are estimated for the following causes of LRI: Acinetobacter baumannii, Chlamydia spp, Enterobacter spp, Escherichia coli, fungi, group B streptococcus, H influenzae, influenza viruses, Klebsiella pneumoniae, Legionella spp, Mycoplasma spp, polymicrobial infections, Pseudomonas aeruginosa, RSV, S aureus, S pneumoniae, and other viruses (ie, the aggregate of all viruses except for influenza and RSV), as well as a residual category of other bacterial pathogens. The ICD-9 and ICD-10 codes mapped to each cause are listed in appendix 1 (pp 18–19).
Incidence proportions were estimated using multinomial estimation as part of a network analysis model, which allows for the inclusion of data sources that are considered to be partial observations—ie, which do not contain all pathogen groups modelled in the study.27 Proportions were estimated as a function of age group, infection type, Hib and pneumococcal vaccination, and Healthcare Access and Quality (HAQ) Index. These covariates vary across geography and time, creating unique predictions for each age group, location, and year. For data sources that only reported deaths, we used modelled case-fatality rates (CFRs) to retroactively estimate the number of cases. These CFRs for each pathogen were modelled using a Bayesian meta-regression tool, MR-BRT (meta-regression—Bayesian, regularised, trimmed), as a function of age group, pathogen, and HAQ Index, with random effects on data source.27, 33, 34 For S pneumoniae, we used a vaccine probe design as an additional input to the incidence proportion model, due to the documented challenge in the microbiological identification of this pathogen.35 Modelled CFRs were then used again to compute mortality proportions from case proportions. More details on aetiology estimation can be found in appendix 1 (pp 17–26). Ultimately, all estimated incident LRI cases were distributed to an estimated aetiology, even those with no aetiology detected, following the modelled aetiology distribution patterns by age, location, and year.
COVID-19 impact adjustment
We developed a multistep modelling process to estimate the reduction of incidence of influenza and RSV in 2020 and 2021. Our source data were reported cases of influenza by country, from notifications reported by countries to WHO's FluNet.36 First, we interpolated the number of reported cases of influenza in 2020 and 2021 by month using the RegMod framework, a Poisson model that estimates the underlying rate of infection in each month as a function of a seasonal pattern and an underlying temporal trend.37 Second, we calculated an under-reporting ratio in the pre-pandemic reference period, 2017–19, for each location by dividing the interpolated number of reported cases from RegMod by the GBD estimated number of cases of LRI due to influenza. Third, we estimated the pandemic disruption-free counterfactual number of reported cases, meaning the number of reported cases we would have expected during 2020 and 2021 in the hypothetical pandemic-free scenario. We did this by multiplying the under-reporting ratio by the estimated number of cases of LRI due to influenza, for 2020 and 2021, that GBD would have estimated in a pandemic-free scenario. Finally, we calculated a yearly disruption influenza scalar for each location for 2020 and 2021. This scalar was computed by dividing the interpolated number of reported cases from RegMod (result of first step) by the counterfactual disruption-free number of reported cases (result of third step).
These influenza disruption scalars (result of final step) were multiplied by counterfactual incident cases and deaths for both influenza and RSV (result of third step), to estimate adjusted cases and deaths. More details on the adjustments are provided in appendix 1 (pp 26–29).
Role of the funding source
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Results
Incidence of LRIs
Globally, in 2019, before the reductions in incidence observed during the COVID-19 pandemic, we estimated 369 million (95% UI 349–391) LRI episodes, for an all-age incidence rate of 4770 episodes (4510–5040) per 100 000 population (table 1).
Table 1.
Lower respiratory infection incidence counts and rates for all-ages and selected age groups in 1990, 2019, 2020, and 2021, and incidence rate percentage change from 1990 to 2019 and from 2019 to 2021, globally and by SDI quintile and GBD super-region
|
1990 |
2019 |
2020 |
2021 |
Incidence rate change, % |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Episode count | Incidence rate per 100 000 population | Episode count | Incidence rate per 100 000 population | Episode count | Incidence rate per 100 000 population | Episode count | Incidence rate per 100 000 population | 1990–2019 | 2019–21 | |
| Global | ||||||||||
| All ages | 314 000 000 (294 000 000 to 333 000 000) | 5884·6 (5513·2 to 6249·0) | 369 000 000 (349 000 000 to 391 000 000) | 4766·4 (4507·5 to 5041·7) | 342 000 000 (324 000 000 to 360 000 000) | 4369·4 (4144·4 to 4608·3) | 344 000 000 (325 000 000 to 364 000 000) | 4354·2 (4121·1 to 4606·5) | −19·0% (−21·9 to −16·0) | −8·6% (−10·4 to −6·6) |
| <5 years | 101 000 000 (89 800 000 to 114 000 000) | 16 302·6 (14 489·0 to 18 341·7) | 45 000 000 (40 000 000 to 50 800 000) | 6639·0 (5903·8 to 7493·3) | 39 800 000 (35 500 000 to 45 000 000) | 5940·8 (5296·9 to 6720·0) | 37 800 000 (33 500 000 to 43 000 000) | 5747·5 (5085·2 to 6537·1) | −59·3% (−60·1 to −58·3) | −13·4% (−15·9 to −10·6) |
| 5–14 years | 43 600 000 (35 500 000 to 52 800 000) | 3893·0 (3169·1 to 4719·6) | 34 000 000 (28 100 000 to 40 700 000) | 2560·4 (2117·1 to 3062·5) | 32 500 000 (26 800 000 to 38 900 000) | 2420·2 (1995·5 to 2900·1) | 32 100 000 (26 500 000 to 38 500 000) | 2369·3 (1954·0 to 2841·8) | −34·2% (−37·0 to −31·2) | −7·5% (−9·3 to −5·8) |
| 15–49 years | 66 700 000 (60 400 000 to 73 300 000) | 2460·2 (2229·3 to 2703·7) | 94 200 000 (85 700 000 to 103 000 000) | 2415·0 (2197·9 to 2641·6) | 87 700 000 (79 800 000 to 95 900 000) | 2235·5 (2034·2 to 2444·1) | 88 800 000 (80 800 000 to 97 100 000) | 2249·6 (2046·5 to 2458·9) | −1·8% (−4·0 to 0·6) | −6·8% (−8·6 to −4·8) |
| 50–69 years | 56 800 000 (51 400 000 to 62 100 000) | 8325·7 (7540·4 to 9112·5) | 95 900 000 (87 400 000 to 104 000 000) | 6965·5 (6349·8 to 7581·7) | 89 500 000 (81 500 000 to 97 100 000) | 6352·7 (5787·5 to 6890·2) | 91 500 000 (83 300 000 to 99 600 000) | 6366·3 (5802·0 to 6936·2) | −16·3% (−19·0 to −13·7) | −8·6% (−10·3 to −6·4) |
| ≥70 years | 45 800 000 (41 100 000 to 50 700 000) | 22 654·9 (20 326·7 to 25 095·8) | 100 000 000 (90 900 000 to 112 000 000) | 21 560·2 (19 575·2 to 24 087·4) | 92 300 000 (83 800 000 to 102 000 000) | 19 279·4 (17 503·3 to 21 229·6) | 93 400 000 (84 300 000 to 104 000 000) | 18 897·7 (17 055·2 to 21 025·2) | −4·8% (−9·1 to −0·4) | −12·3% (−14·2 to −10·3) |
| High SDI | ||||||||||
| All ages | 15 700 000 (14 900 000 to 16 600 000) | 1783·6 (1689·8 to 1890·0) | 17 900 000 (17 000 000 to 18 900 000) | 1647·3 (1562·4 to 1738·8) | 16 600 000 (15 700 000 to 17 500 000) | 1519·6 (1439·4 to 1608·0) | 14 800 000 (14 100 000 to 15 700 000) | 1354·6 (1285·3 to 1433·2) | −7·6% (−10·1 to −5·3) | −17·8% (−18·9 to −16·5) |
| <5 years | 1 920 000 (1 660 000 to 2 190 000) | 3104·5 (2686·7 to 3556·3) | 908 000 (775 000 to 1 060 000) | 1623·3 (1386·1 to 1900·3) | 750 000 (638 000 to 874 000) | 1365·2 (1160·7 to 1590·2) | 600 000 (513 000 to 702 000) | 1114·0 (952·4 to 1302·9) | −47·7% (−50·6 to −45·1) | −31·4% (−32·9 to −29·4) |
| 5–14 years | 1 040 000 (820 000to 1 340 000) | 841·3 (660·5 to 1080·0) | 604 000 (476 000 to 761 000) | 511·0 (402·9 to 643·8) | 565 000 (447 000 to 720 000) | 476·7 (376·7 to 607·5) | 533 000 (420 000 to 675 000) | 449·5 (354·2 to 569·0) | −39·3% (−41·5 to −36·6) | −12·0% (−13·5 to −10·7) |
| 15–49 years | 2 490 000 (2 220 000 to 2 790 000) | 539·5 (481·7 to 604·4) | 2 120 000 (1 900 000 to 2 340 000) | 418·8 (376·0 to 462·7) | 1 930 000 (1 740 000 to 2 130 000) | 382·9 (344·4 to 422·8) | 1 820 000 (1 630 000 to 2 010 000) | 363·3 (324·8 to 400·7) | −22·4% (−24·3 to −20·5) | −13·3% (−14·6 to −11·8) |
| 50–69 years | 3 860 000 (3 560 000 to 4 170 000) | 2354·7 (2173·2 to 2542·5) | 4 520 000 (4 180 000 to 4 880 000) | 1663·0 (1537·2 to 1796·6) | 4 190 000 (3 860 000 to 4 530 000) | 1532·8 (1412·3 to 1654·1) | 3 860 000 (3 560 000 to 4 160 000) | 1399·4 (1290·0 to 1509·6) | −29·4% (−30·9 to −27·5) | −15·9% (−17·1 to −14·3) |
| ≥70 years | 6 380 000 (5 880 000 to 6 960 000) | 9244·5 (8509·4 to 10 077·5) | 9 760 000 (9 050 000 to 10 600 000) | 7192·4 (6664·9 to 7805·8) | 9 140 000 (8 480 000 to 9 840 000) | 6534·2 (6059·1 to 7036·3) | 8 000 000 (7 420 000 to 8 680 000) | 5578·0 (5172·7 to 6051·3) | −22·2% (−24·4 to −20·1) | −22·4% (−23·7 to −21·1) |
| High-middle SDI | ||||||||||
| All ages | 37 200 000 (34 900 000 to 39 700 000) | 3498·3 (3279·9 to 3730·9) | 45 900 000 (43 000 000 to 48 900 000) | 3535·0 (3316·4 to 3772·9) | 42 400 000 (39 900 000 to 45 200 000) | 3261·4 (3065·9 to 3474·3) | 40 900 000 (38 500 000 to 43 500 000) | 3138·7 (2951·6 to 3339·3) | 1·1% (−4·2 to 6·3) | −11·2% (−13·3 to −9·2) |
| <5 years | 11 300 000 (9 950 000 to 12 900 000) | 12 155·7 (10 709·8 to 13 896·9) | 3 220 000 (2 710 000 to 3 790 000) | 4201·3 (3537·7 to 4940·8) | 2 720 000 (2 290 000 to 3 200 000) | 3682·0 (3096·2 to 4325·9) | 2 240 000 (1 880 000 to 2 620 000) | 3202·9 (2686·7 to 3735·4) | −65·4% (−68·5 to −62·2) | −23·8% (−26·1 to −21·2) |
| 5–14 years | 4 980 000 (4 020 000 to 6 130 000) | 2756·3 (2224·9 to 3392·1) | 3 730 000 (2 940 000 to 4 640 000) | 2412·3 (1902·9 to 3001·3) | 3 640 000 (2 870 000 to 4 540 000) | 2304·1 (1819·7 to 2877·3) | 3 640 000 (2 870 000 to 4 540 000) | 2260·8 (1782·5 to 2824·0) | −12·5% (−19·4 to −4·8) | −6·3% (−9·2 to −3·5) |
| 15–49 years | 6 710 000 (6 030 000 to 7 440 000) | 1188·4 (1068·1 to 1318·7) | 8 620 000 (7 700 000 to 9 620 000) | 1345·6 (1202·4 to 1502·0) | 7 950 000 (7 120 000 to 8 830 000) | 1252·6 (1121·2 to 1390·1) | 7 620 000 (6 840 000 to 8 460 000) | 1211·1 (1085·7 to 1343·0) | 13·2% (9·7 to 17·3) | −10·0% (−11·8 to −8·1) |
| 50–69 years | 7 460 000 (6 830 000 to 8 080 000) | 4284·7 (3925·4 to 4640·2) | 12 100 000 (11 000 000 to 13 200 000) | 3825·6 (3485·4 to 4174·3) | 11 500 000 (10 500 000 to 12 500 000) | 3581·3 (3281·3 to 3888·7) | 11 100 000 (10 100 000 to 12 100 000) | 3417·1 (3094·2 to 3705·9) | −10·7% (−13·8 to −6·9) | −10·7% (−13·3 to −7·7) |
| ≥70 years | 6 770 000 (6 140 000 to 7 390 000) | 13 149·2 (11 923·5 to 14 362·2) | 18 200 000 (16 300 000 to 20 300 000) | 16 585·7 (14 816·6 to 18 516·2) | 16 600 000 (14 900 000 to 18 300 000) | 14 660·6 (13 102·3 to 16 151·7) | 16 300 000 (14 600 000 to 18 100 000) | 13 866·9 (12 398·2 to 15 377·7) | 26·1% (19·2 to 34·3) | −16·4% (−19·6 to −13·1) |
| Middle SDI | ||||||||||
| All ages | 87 100 000 (81 400 000 to 92 900 000) | 5054·4 (4726·3 to 5390·2) | 96 700 000 (91 100 000 to 102 000 000) | 4012·3 (3778·5 to 4251·6) | 89 000 000 (84 200 000 to 94 300 000) | 3662·1 (3461·7 to 3879·0) | 89 500 000 (84 700 000 to 95 300 000) | 3657·2 (3457·2 to 3892·0) | −20·6% (−24·1 to −16·7) | −8·8% (−10·8 to −6·7) |
| <5 years | 29 700 000 (26 300 000 to 33 500 000) | 14 797·3 (13 136·4 to 16 713·9) | 8 680 000 (7 630 000 to 9 890 000) | 4632·6 (4071·5 to 5274·5) | 7 590 000 (6 680 000 to 8 680 000) | 4148·5 (3650·8 to 4740·1) | 6 850 000 (5 990 000 to 7 890 000) | 3879·7 (3392·6 to 4469·1) | −68·7% (−69·7 to −67·6) | −16·3% (−18·8 to −13·2) |
| 5–14 years | 12 800 000 (10 500 000 to 15 500 000) | 3402·6 (2778·2 to 4121·3) | 7 370 000 (5 990 000 to 8 910 000) | 1930·1 (1568·4 to 2332·2) | 6 970 000 (5 660 000 to 8 430 000) | 1803·1 (1465·3 to 2183·1) | 6 830 000 (5 560 000 to 8 280 000) | 1750·7 (1426·0 to 2122·5) | −43·3% (−46·4 to −39·5) | −9·3% (−11·2 to −7·4) |
| 15–49 years | 18 900 000 (17 200 000 to 20 800 000) | 2074·9 (1885·7 to 2280·5) | 24 600 000 (22 300 000 to 27 000 000) | 1966·6 (1781·8 to 2159·1) | 22 500 000 (20 500 000 to 24 700 000) | 1799·4 (1634·5 to 1973·7) | 22 600 000 (20 500 000 to 24 900 000) | 1803·5 (1633·0 to 1986·2) | −5·2% (−8·0 to −2·8) | −8·3% (−10·5 to −6·1) |
| 50–69 years | 14 400 000 (13 000 000 to 15 800 000) | 7609·8 (6853·4 to 8360·1) | 27 800 000 (25 200 000 to 30 500 000) | 6042·7 (5495·9 to 6633·2) | 25 900 000 (23 600 000 to 28 300 000) | 5468·6 (4987·2 to 5975·0) | 26 600 000 (24 200 000 to 29 000 000) | 5470·5 (4990·1 to 5976·3) | −20·6% (−23·4 to −17·6) | −9·5% (−11·4 to −7·1) |
| ≥70 years | 11 300 000 (10 100 000 to 12 500 000) | 24 697·8 (22 037·6 to 27 426·9) | 28 300 000 (25 700 000 to 31 600 000) | 21 637·0 (19 643·2 to 24 127·6) | 26 000 000 (23 700 000 to 28 800 000) | 19 223·2 (17 467·8 to 21 269·0) | 26 700 000 (24 100 000 to 29 600 000) | 18 911·1 (17 100·3 to 21 016·6) | −12·4% (−16·4 to −7·2) | −12·6% (−15·0 to −10·1) |
| Low-middle SDI | ||||||||||
| All ages | 119 000 000 (111 000 000 to 127 000 000) | 10 254·0 (9596·2 to 10 941·0) | 137 000 000 (129 000 000 to 145 000 000) | 7301·1 (6889·2 to 7748·4) | 126 000 000 (119 000 000 to 133 000 000) | 6638·3 (6282·2 to 7006·3) | 130 000 000 (122 000 000 to 138 000 000) | 6742·4 (6355·3 to 7173·5) | −28·8% (−31·5 to −26·0) | −7·7% (−10·3 to −4·6) |
| <5 years | 37 500 000 (33 300 000 to 42 000 000) | 21 604·0 (19 187·8 to 24 200·3) | 16 700 000 (14 900 000 to 18 700 000) | 8530·6 (7610·6 to 9580·6) | 14 500 000 (13 000 000 to 16 600 000) | 7512·9 (6704·2 to 8555·4) | 14 100 000 (12 400 000 to 16 000 000) | 7343·5 (6464·9 to 8356·5) | −60·5% (−61·5 to −59·4) | −13·9% (−17·8 to −10·0) |
| 5–14 years | 17 000 000 (13 900 000 to 20 800 000) | 5694·7 (4647·4 to 6948·8) | 13 000 000 (10 700 000 to 15 400 000) | 3353·2 (2768·0 to 3977·9) | 12 100 000 (10 100 000 to 14 500 000) | 3136·1 (2604·9 to 3745·9) | 12 000 000 (9 930 000 to 14 400 000) | 3099·9 (2556·6 to 3718·7) | −41·1% (−44·2 to −38·0) | −7·6% (−10·6 to −4·4) |
| 15–49 years | 26 800 000 (24 200 000 to 29 600 000) | 4865·4 (4397·2 to 5362·7) | 38 600 000 (35 200 000 to 42 100 000) | 3908·7 (3562·9 to 4260·6) | 35 800 000 (32 500 000 to 39 100 000) | 3573·6 (3242·2 to 3907·2) | 36 700 000 (33 300 000 to 40 100 000) | 3613·3 (3279·4 to 3947·7) | −19·7% (−21·7 to −17·1) | −7·6% (−10·5 to −4·5) |
| 50–69 years | 22 000 000 (19 800 000 to 24 400 000) | 19 664·4 (17 647·7 to 21 804·9) | 36 300 000 (33 000 000 to 39 700 000) | 14 999·1 (13 644·8 to 16 423·3) | 33 600 000 (30 500 000 to 36 500 000) | 13 488·6 (12 241·0 to 14 682·2) | 35 000 000 (31 800 000 to 38 200 000) | 13 744·2 (12 491·8 to 14 995·5) | −23·7% (−27·4 to −19·9) | −8·4% (−11·4 to −5·2) |
| ≥70 years | 15 800 000 (13 900 000 to 17 800 000) | 60 146·0 (52 905·4 to 67 732·4) | 32 600 000 (29 400 000 to 36 900 000) | 48 877·1 (44 089·3 to 55 283·6) | 30 100 000 (27 000 000 to 33 700 000) | 43 991·0 (39 501·2 to 49 353·2) | 31 700 000 (28 200 000 to 35 900 000) | 45 178·2 (40 213·6 to 51 217·1) | −18·7% (−24·0 to −13·3) | −7·6% (−11·3 to −3·5) |
| Low SDI | ||||||||||
| All ages | 54 600 000 (50 900 000 to 58 200 000) | 10 899·1 (10 149·8 to 11 601·2) | 71 500 000 (67 300 000 to 75 400 000) | 6698·9 (6308·8 to 7070·2) | 67 500 000 (63 600 000 to 71 100 000) | 6176·0 (5823·9 to 6510·0) | 68 600 000 (65 000 000 to 72 600 000) | 6143·1 (5812·8 to 6500·9) | −38·5% (−40·4 to −36·5) | −8·3% (−10·2 to −6·3) |
| <5 years | 20 600 000 (18 200 000 to 23 400 000) | 22 738·9 (20 015·8 to 25 809·9) | 15 500 000 (13 900 000 to 17 400 000) | 9564·9 (8563·1 to 10 736·1) | 14 200 000 (12 600 000 to 15 900 000) | 8642·5 (7675·9 to 9724·6) | 14 000 000 (12 500 000 to 15 900 000) | 8480·2 (7543·0 to 9585·9) | −57·9% (−59·1 to −56·7) | −11·3% (−14·0 to −8·6) |
| 5–14 years | 7 700 000 (6 290 000 to 9 290 000) | 5576·6 (4554·1 to 6725·8) | 9 320 000 (7 750 000 to 11 100 000) | 3263·0 (2713·8 to 3892·8) | 9 130 000 (7 650 000 to 10 900 000) | 3146·1 (2636·6 to 3757·0) | 9 020 000 (7 500 000 to 10 900 000) | 3061·6 (2543·7 to 3691·2) | −41·5% (−44·4 to −38·1) | −6·2% (−8·3 to −3·8) |
| 15–49 years | 11 800 000 (10 600 000 to 12 900 000) | 5317·4 (4806·8 to 5850·9) | 20 200 000 (18 300 000 to 22 000 000) | 3951·9 (3580·5 to 4303·3) | 19 500 000 (17 700 000 to 21 100 000) | 3693·8 (3367·2 to 4009·8) | 20 000 000 (18 300 000 to 21 900 000) | 3686·4 (3364·9 to 4029·7) | −25·7% (−28·1 to −22·8) | −6·7% (−8·7 to −4·5) |
| 50–69 years | 9 010 000 (8 030 000 to 9 980 000) | 21 438·0 (19 102·1 to 23 759·2) | 15 200 000 (13 800 000 to 16 700 000) | 17 480·9 (15 878·6 to 19 177·8) | 14 300 000 (13 100 000 to 15 600 000) | 15 844·2 (14 473·5 to 17 304·6) | 14 800 000 (13 500 000 to 16 200 000) | 15 955·7 (14 491·9 to 17 459·3) | −18·5% (−22·4 to −14·2) | −8·7% (−11·6 to −6·0) |
| ≥70 years | 5 530 000 (4 900 000 to 6 210 000) | 59 241·9 (52 529·8 to 66 532·7) | 11 200 000 (10 000 000 to 12 700 000) | 53 575·8 (47 915·3 to 60 574·5) | 10 400 000 (9 300 000 to 11 700 000) | 48 762·8 (43 489·0 to 54 900·8) | 10 800 000 (9 600 000 to 12 200 000) | 49 111·1 (43 765·6 to 55 612·9) | −9·6% (−15·4 to −2·0) | −8·3% (−11·6 to −4·8) |
| Central Europe, Eastern Europe, and Central Asia | ||||||||||
| All ages | 10 800 000 (10 200 000 to 11 400 000) | 2570·4 (2426·7 to 2718·0) | 8 010 000 (7 600 000 to 8 450 000) | 1913·5 (1816·4 to 2018·3) | 7 860 000 (7 490 000 to 8 240 000) | 1877·0 (1788·7 to 1969·3) | 6 950 000 (6 600 000 to 7 330 000) | 1664·0 (1580·1 to 1754·3) | −25·6% (−28·0 to −23·0) | −13·0% (−14·1 to −11·9) |
| <5 years | 3 150 000 (2 800 000 to 3 520 000) | 8779·0 (7807·7 to 9795·9) | 874 000 (783 000 to 980 000) | 3234·3 (2897·7 to 3628·1) | 812 000 (719 000 to 908 000) | 3078·0 (2726·4 to 3440·6) | 607 000 (542 000 to 689 000) | 2363·2 (2110·1 to 2679·0) | −63·2% (−65·2 to −61·0) | −26·9% (−28·8 to −24·9) |
| 5–14 years | 1 440 000 (1 200 000 to 1 750 000) | 2055·0 (1708·4 to 2500·7) | 669 000 (557 000 to 801 000) | 1249·0 (1040·5 to 1496·1) | 666 000 (555 000 to 806 000) | 1223·6 (1018·6 to 1479·8) | 609 000 (504 000 to 739 000) | 1105·0 (914·2 to 1341·5) | −39·2% (−41·5 to −37·0) | −11·5% (−13·9 to −9·0) |
| 15–49 years | 1 730 000 (1 600 000 to 1 880 000) | 843·2 (775·8 to 914·7) | 1 670 000 (1 550 000 to 1 800 000) | 836·5 (775·5 to 899·6) | 1 660 000 (1 550 000 to 1 790 000) | 834·4 (777·3 to 900·3) | 1 490 000 (1 390 000 to 1 610 000) | 754·8 (701·2 to 815·4) | −0·8% (−4·4 to 3·0) | −9·8% (−11·4 to −8·0) |
| 50–69 years | 2 560 000 (2 370 000 to 2 770 000) | 3054·6 (2822·0 to 3303·6) | 2 500 000 (2 290 000 to 2 700 000) | 2499·2 (2292·1 to 2703·0) | 2 470 000 (2 290 000 to 2 650 000) | 2470·0 (2287·9 to 2655·1) | 2 240 000 (2 070 000 to 2 420 000) | 2244·8 (2073·3 to 2431·5) | −18·2% (−20·3 to −16·3) | −10·2% (−11·7 to −8·5) |
| ≥70 years | 1 930 000 (1 760 000 to 2 120 000) | 7626·4 (6970·1 to 8376·3) | 2 290 000 (2 110 000 to 2 530 000) | 6037·4 (5559·7 to 6670·9) | 2 250 000 (2 060 000 to 2 470 000) | 5773·6 (5297·5 to 6327·9) | 2 010 000 (1 850 000 to 2 210 000) | 5062·9 (4662·7 to 5579·0) | −20·8% (−23·0 to −18·7) | −16·1% (−17·6 to −14·6) |
| High-income | ||||||||||
| All ages | 14 300 000 (13 500 000 to 15 100 000) | 1572·4 (1490·5 to 1665·2) | 15 900 000 (15 100 000 to 16 800 000) | 1465·3 (1388·2 to 1546·9) | 14 600 000 (13 900 000 to 15 500 000) | 1341·4 (1272·7 to 1418·8) | 13 000 000 (12 300 000 to 13 700 000) | 1188·6 (1125·1 to 1257·8) | −6·8% (−9·1 to −4·7) | −18·9% (−20·0 to −17·7) |
| <5 years | 1 520 000 (1 320 000 to 1 730 000) | 2464·9 (2137·1 to 2814·1) | 777 000 (661 000 to 906 000) | 1375·3 (1170·6 to 1604·2) | 617 000 (521 000 to 726 000) | 1114·0 (940·6 to 1310·9) | 510 000 (436 000 to 594 000) | 939·6 (803·2 to 1093·5) | −44·2% (−47·1 to −41·7) | −31·7% (−33·5 to −29·6) |
| 5–14 years | 726 000 (566 000 to 925 000) | 576·7 (449·6 to 735·0) | 453 000 (358 000 to 570 000) | 369·6 (292·5 to 465·3) | 414 000 (328 000 to 521 000) | 338·4 (268·2 to 425·7) | 392 000 (310 000 to 491 000) | 320·7 (254·1 to 402·2) | −35·9% (−38·2 to −33·1) | −13·2% (−14·6 to −11·8) |
| 15–49 years | 2 200 000 (1 960 000 to 2 470 000) | 467·4 (417·2 to 524·1) | 1 660 000 (1 490 000 to 1 830 000) | 340·4 (306·2 to 375·2) | 1 490 000 (1 340 000 to 1 640 000) | 306·8 (276·3 to 337·0) | 1 420 000 (1 270 000 to 1 560 000) | 292·8 (261·8 to 322·8) | −27·2% (−29·0 to −25·0) | −14·0% (−15·2 to −12·6) |
| 50–69 years | 3 540 000 (3 270 000 to 3 820 000) | 2019·0 (1867·6 to 2179·5) | 3 850 000 (3 560 000 to 4 150 000) | 1406·3 (1302·5 to 1516·7) | 3 530 000 (3 270 000 to 3 790 000) | 1282·8 (1188·9 to 1376·1) | 3 230 000 (2 970 000 to 3 480 000) | 1164·2 (1070·6 to 1255·5) | −30·3% (−32·0 to −28·4) | −17·2% (−18·5 to −16·0) |
| ≥70 years | 6 310 000 (5 820 000 to 6 870 000) | 8318·1 (7666·1 to 9051·3) | 9 180 000 (8 520 000 to 9 950 000) | 6284·8 (5830·6 to 6814·7) | 8 560 000 (7 980 000 to 9 210 000) | 5705·6 (5324·0 to 6143·0) | 7 420 000 (6 870 000 to 8 050 000) | 4846·6 (4486·3 to 5252·9) | −24·4% (−26·6 to −22·4) | −22·9% (−24·2 to −21·6) |
| Latin America and Caribbean | ||||||||||
| All ages | 15 800 000 (14 900 000 to 17 000 000) | 4052·0 (3806·2 to 4347·7) | 15 000 000 (14 200 000 to 15 800 000) | 2558·8 (2420·0 to 2702·8) | 13 300 000 (12 600 000 to 14 000 000) | 2256·3 (2131·9 to 2373·9) | 12 900 000 (12 100 000 to 13 700 000) | 2165·7 (2044·1 to 2300·0) | −36·9% (−39·4 to −34·2) | −15·4% (−17·6 to −12·6) |
| <5 years | 5 940 000 (5 280 000 to 6 740 000) | 11 992·5 (10 660·4 to 13 618·8) | 2 390 000 (2 080 000 to 2 740 000) | 4912·8 (4271·4 to 5627·1) | 1 870 000 (1 620 000 to 2 140 000) | 3891·1 (3365·0 to 4461·9) | 1 680 000 (1 450 000 to 1 930 000) | 3560·6 (3072·6 to 4087·7) | −59·0% (−60·5 to −57·7) | −27·5% (−30·9 to −23·0) |
| 5–14 years | 2 360 000 (1 970 000 to 2 850 000) | 2491·9 (2074·2 to 3010·9) | 1 160 000 (943 000 to 1 430 000) | 1211·6 (983·5 to 1495·9) | 1 040 000 (854 000 to 1 270 000) | 1086·2 (890·3 to 1326·2) | 1 000 000 (819 000 to 1 240 000) | 1045·7 (853·1 to 1290·9) | −51·4% (−53·8 to −48·8) | −13·7% (−15·8 to −11·3) |
| 15–49 years | 2 860 000 (2 630 000 to 3 110 000) | 1449·4 (1332·4 to 1578·4) | 2 650 000 (2 450 000 to 2 870 000) | 859·9 (794·1 to 930·7) | 2 400 000 (2 210 000 to 2 600 000) | 772·8 (713·0 to 837·7) | 2 330 000 (2 150 000 to 2 540 000) | 746·6 (688·9 to 814·1) | −40·7% (−42·1 to −39·1) | −13·2% (−15·3 to −10·8) |
| 50–69 years | 2 260 000 (2 080 000 to 2 460 000) | 5947·3 (5462·6 to 6460·2) | 3 630 000 (3 330 000 to 3 910 000) | 3645·6 (3346·4 to 3922·1) | 3 380 000 (3 100 000 to 3 640 000) | 3302·0 (3035·8 to 3559·9) | 3 320 000 (3 060 000 to 3 600 000) | 3181·4 (2925·2 to 3449·4) | −38·7% (−40·0 to −37·3) | −12·7% (−15·0 to −10·1) |
| ≥70 years | 2 400 000 (2 190 000 to 2 620 000) | 21 978·6 (20 058·6 to 24 044·7) | 5 140 000 (4 710 000 to 5 630 000) | 15 764·3 (14 439·0 to 17 253·9) | 4 630 000 (4 210 000 to 5 040 000) | 13 775·5 (12 531·4 to 14 985·4) | 4 530 000 (4 140 000 to 4 990 000) | 13 119·2 (11 991·9 to 14 468·1) | −28·3% (−30·1 to −26·2) | −16·8% (−19·4 to −14·0) |
| North Africa and Middle East | ||||||||||
| All ages | 11 200 000 (10 200 000 to 12 200 000) | 3287·9 (3003·6 to 3598·4) | 10 500 000 (9 850 000 to 11 200 000) | 1731·5 (1625·1 to 1843·1) | 10 000 000 (9 370 000 to 10 800 000) | 1631·0 (1523·4 to 1757·7) | 9 380 000 (8 820 000 to 9 980 000) | 1505·4 (1415·1 to 1601·6) | −47·3% (−49·8 to −44·1) | −13·1% (−15·4 to −10·2) |
| <5 years | 5 690 000 (4 890 000 to 6 590 000) | 11 105·8 (9544·3 to 12 868·0) | 2 270 000 (1 960 000 to 2 640 000) | 3558·6 (3073·1 to 4150·2) | 1 940 000 (1 640 000 to 2 300 000) | 3108·6 (2619·8 to 3682·1) | 1 670 000 (1 430 000 to 1 960 000) | 2725·0 (2334·8 to 3202·1) | −68·0% (−69·4 to −66·3) | −23·4% (−27·5 to −18·2) |
| 5–14 years | 1 640 000 (1 310 000 to 2 020 000) | 1840·2 (1464·4 to 2265·8) | 1 290 000 (1 020 000 to 1 600 000) | 1088·8 (862·9 to 1346·5) | 1 240 000 (999 000 to 1 520 000) | 1032·4 (829·0 to 1258·8) | 1 190 000 (944 000 to 1 460 000) | 970·5 (772·4 to 1195·0) | −40·8% (−43·9 to −37·8) | −10·9% (−13·8 to −7·3) |
| 15–49 years | 1 660 000 (1 500 000 to 1 840 000) | 1035·9 (934·6 to 1150·3) | 2 600 000 (2 350 000 to 2 870 000) | 797·0 (720·6 to 880·3) | 2 510 000 (2 280 000 to 2 790 000) | 761·6 (690·0 to 845·4) | 2 410 000 (2 190 000 to 2 660 000) | 722·0 (655·6 to 795·1) | −23·1% (−25·6 to −20·3) | −9·4% (−11·8 to −6·3) |
| 50–69 years | 1 180 000 (1 050 000 to 1 300 000) | 3772·2 (3378·9 to 4165·4) | 2 210 000 (2 010 000 to 2 410 000) | 2793·3 (2538·5 to 3049·8) | 2 230 000 (2 020 000 to 2 440 000) | 2712·6 (2456·1 to 2975·9) | 2 150 000 (1 960 000 to 2 340 000) | 2528·9 (2307·4 to 2757·0) | −26·0% (−29·7 to −21·8) | −9·5% (−12·4 to −6·0) |
| ≥70 years | 983 000 (870 000to 1 090 000) | 13 606·8 (12 046·8 to 15 107·9) | 2 140 000 (1 940 000 to 2 360 000) | 11 094·4 (10 077·1 to 12 259·5) | 2 100 000 (1 890 000 to 2 370 000) | 10 609·3 (9538·0 to 11 978·7) | 1 960 000 (1 790 000 to 2 180 000) | 9653·6 (8803·5 to 10 726·7) | −18·5% (−23·7 to −12·8) | −13·0% (−16·2 to −9·2) |
| South Asia | ||||||||||
| All ages | 143 000 000 (134 000 000 to 153 000 000) | 13 099·4 (12 268·7 to 13 973·1) | 180 000 000 (169 000 000 to 192 000 000) | 9965·4 (9363·5 to 10 604·1) | 165 000 000 (156 000 000 to 174 000 000) | 9021·6 (8518·1 to 9543·7) | 172 000 000 (161 000 000 to 184 000 000) | 9319·4 (8733·8 to 9984·8) | −23·9% (−27·0 to −20·8) | −6·5% (−9·8 to −2·8) |
| <5 years | 38 400 000 (34 100 000 to 42 900 000) | 24 450·9 (21 713·4 to 27 340·1) | 16 900 000 (15 100 000 to 18 800 000) | 10 340·6 (9243·4 to 11 556·0) | 15 400 000 (13 600 000 to 17 500 000) | 9575·9 (8470·8 to 10 885·7) | 15 300 000 (13 400 000 to 17 700 000) | 9627·6 (8435·1 to 11 133·9) | −57·7% (−58·9 to −56·3) | −6·9% (−12·7 to −0·7) |
| 5–14 years | 20 600 000 (16 800 000 to 25 200 000) | 7453·7 (6064·5 to 9107·7) | 15 700 000 (12 900 000 to 18 900 000) | 4461·8 (3668·6 to 5362·4) | 14 600 000 (12 000 000 to 17 700 000) | 4170·0 (3413·6 to 5042·5) | 14 600 000 (11 900 000 to 17 700 000) | 4197·6 (3426·9 to 5077·4) | −40·1% (−43·9 to −36·3) | −5·9% (−9·5 to −2·3) |
| 15–49 years | 35 700 000 (32 100 000 to 39 300 000) | 6743·8 (6060·6 to 7427·6) | 53 200 000 (48 200 000 to 58 200 000) | 5436·5 (4925·2 to 5949·9) | 48 500 000 (43 900 000 to 53 300 000) | 4881·7 (4425·5 to 5366·7) | 50 100 000 (45 200 000 to 55 200 000) | 4974·0 (4491·6 to 5479·6) | −19·4% (−21·5 to −17·0) | −8·5% (−11·6 to −5·2) |
| 50–69 years | 29 000 000 (25 900 000 to 32 200 000) | 26 980·0 (24 062·2 to 29 943·6) | 50 700 000 (46 000 000 to 55 700 000) | 20 611·3 (18 699·2 to 22 650·5) | 46 300 000 (42 000 000 to 50 600 000) | 18 270·9 (16 562·3 to 19 978·4) | 48 900 000 (44 400 000 to 53 700 000) | 18 843·4 (17 118·0 to 20 687·0) | −23·6% (−27·3 to −19·8) | −8·6% (−11·6 to −4·8) |
| ≥70 years | 19 600 000 (17 200 000 to 22 100 000) | 83 238·5 (73 340·4 to 94 207·4) | 43 700 000 (39 100 000 to 49 700 000) | 63 388·1 (56 714·2 to 71 959·6) | 40 200 000 (35 800 000 to 45 200 000) | 56 615·1 (50 503·2 to 63 669·3) | 43 200 000 (38 200 000 to 49 200 000) | 59 004·4 (52 213·3 to 67 237·2) | −23·8% (−28·8 to −18·3) | −6·9% (−11·2 to −2·4) |
| Southeast Asia, East Asia, and Oceania | ||||||||||
| All ages | 74 600 000 (69 600 000 to 79 900 000) | 4418·3 (4117·6 to 4731·3) | 75 400 000 (71 000 000 to 80 400 000) | 3487·6 (3283·4 to 3716·3) | 69 700 000 (65 500 000 to 74 100 000) | 3204·6 (3012·0 to 3408·7) | 67 300 000 (63 400 000 to 71 400 000) | 3080·4 (2900·2 to 3268·2) | −21·1% (−25·7 to −16·4) | −11·7% (−13·0 to −10·1) |
| <5 years | 28 900 000 (25 500 000 to 32 900 000) | 16 514·4 (14 541·9 to 18 804·0) | 6 830 000 (5 880 000 to 7 850 000) | 4564·0 (3928·0 to 5243·7) | 5 850 000 (5 010 000 to 6 860 000) | 4023·1 (3441·5 to 4717·5) | 4 880 000 (4 190 000 to 5 680 000) | 3529·1 (3032·2 to 4105·8) | −72·4% (−74·1 to −70·6) | −22·7% (−24·4 to −20·8) |
| 5–14 years | 10 700 000 (8 720 000 to 13 000 000) | 3253·2 (2656·2 to 3973·7) | 6 240 000 (4 970 000 to 7 810 000) | 2119·7 (1687·6 to 2649·8) | 6 020 000 (4 790 000 to 7 510 000) | 2002·8 (1593·2 to 2499·4) | 5 940 000 (4 710 000 to 7 370 000) | 1936·7 (1535·5 to 2402·1) | −34·8% (−40·2 to −28·5) | −8·6% (−10·5 to −6·7) |
| 15–49 years | 12 700 000 (11 400 000 to 14 100 000) | 1364·0 (1226·0 to 1514·3) | 13 500 000 (12 100 000 to 15 000 000) | 1244·5 (1116·4 to 1382·7) | 12 500 000 (11 100 000 to 13 800 000) | 1160·4 (1034·9 to 1282·4) | 11 900 000 (10 600 000 to 13 100 000) | 1116·0 (995·9 to 1233·0) | −8·8% (−11·7 to −5·6) | −10·3% (−11·8 to −8·9) |
| 50–69 years | 11 900 000 (10 700 000 to 13 000 000) | 5720·0 (5163·4 to 6283·5) | 20 000 000 (18 200 000 to 21 800 000) | 4053·7 (3682·9 to 4420·0) | 19 000 000 (17 400 000 to 20 700 000) | 3744·9 (3426·5 to 4080·0) | 18 600 000 (16 800 000 to 20 200 000) | 3571·8 (3236·8 to 3892·7) | −29·1% (−31·3 to −26·2) | −11·9% (−13·6 to −10·0) |
| ≥70 years | 10 500 000 (9 370 000 to 11 600 000) | 21 063·0 (18 768·0 to 23 319·3) | 28 800 000 (25 900 000 to 32 000 000) | 20 500·9 (18 415·1 to 22 744·8) | 26 300 000 (23 600 000 to 29 000 000) | 17 997·9 (16 137·1 to 19 827·2) | 26 000 000 (23 400 000 to 28 700 000) | 16 906·4 (15 228·1 to 18 662·1) | −2·7% (−8·4 to 4·2) | −17·5% (−19·5 to −15·1) |
| Sub-Saharan Africa | ||||||||||
| All ages | 43 900 000 (41 000 000 to 46 800 000) | 8936·4 (8335·8 to 9525·6) | 64 200 000 (60 700 000 to 67 700 000) | 5952·8 (5620·3 to 6277·1) | 61 400 000 (58 000 000 to 64 600 000) | 5546·3 (5245·1 to 5840·1) | 62 000 000 (58 500 000 to 65 200 000) | 5474·6 (5165·0 to 5753·4) | −33·4% (−35·3 to −31·3) | −8·0% (−9·6 to −6·5) |
| <5 years | 17 500 000 (15 400 000 to 19 800 000) | 19 478·0 (17 143·7 to 22 080·6) | 15 000 000 (13 400 000 to 16 900 000) | 8863·0 (7932·3 to 9960·6) | 13 300 000 (11 800 000 to 15 000 000) | 7766·1 (6918·0 to 8749·9) | 13 200 000 (11 800 000 to 14 800 000) | 7642·8 (6825·6 to 8583·4) | −54·5% (−55·8 to −53·1) | −13·8% (−16·0 to −11·4) |
| 5–14 years | 6 130 000 (5 060 000 to 7 350 000) | 4547·4 (3752·5 to 5452·7) | 8 490 000 (7 110 000 to 10 100 000) | 2915·6 (2442·3 to 3475·8) | 8 470 000 (7 130 000 to 10 000 000) | 2849·9 (2399·7 to 3372·7) | 8 320 000 (6 920 000 to 9 950 000) | 2743·5 (2282·0 to 3281·2) | −35·9% (−38·4 to −32·6) | −5·9% (−8·0 to −3·7) |
| 15–49 years | 9 890 000 (8 990 000 to 10 800 000) | 4511·4 (4100·7 to 4925·8) | 18 900 000 (17 200 000 to 20 600 000) | 3673·6 (3345·0 to 3992·1) | 18 700 000 (17 100 000 to 20 300 000) | 3526·2 (3227·0 to 3824·5) | 19 200 000 (17 700 000 to 20 800 000) | 3509·4 (3230·1 to 3809·5) | −18·6% (−21·0 to −15·6) | −4·5% (−6·0 to −2·8) |
| 50–69 years | 6 350 000 (5 730 000 to 6 990 000) | 16 502·6 (14 891·8 to 18 163·4) | 13 000 000 (11 800 000 to 14 200 000) | 15 344·8 (13 882·5 to 16 730·5) | 12 600 000 (11 500 000 to 13 800 000) | 14 331·7 (13 087·7 to 15 656·8) | 13 000 000 (11 900 000 to 14 200 000) | 14 391·6 (13 110·3 to 15 695·7) | −7·0% (−10·5 to −3·8) | −6·2% (−7·8 to −4·6) |
| ≥70 years | 4 070 000 (3 620 000 to 4 560 000) | 44 066·2 (39 216·4 to 49 342·5) | 8 810 000 (7 940 000 to 9 880 000) | 46 676·0 (42 070·1 to 52 387·7) | 8 290 000 (7 480 000 to 9 300 000) | 43 028·9 (38 829·9 to 48 260·3) | 8 280 000 (7 500 000 to 9 260 000) | 42 264·9 (38 278·7 to 47 260·2) | 5·9% (0·7 to 12·1) | −9·5% (−11·2 to −7·6) |
Values in parentheses are 95% uncertainty intervals. Count data are presented to three significant figures. GBD=Global Burden of Diseases, Injuries, and Risk Factors Study. SDI=Socio-demographic Index.
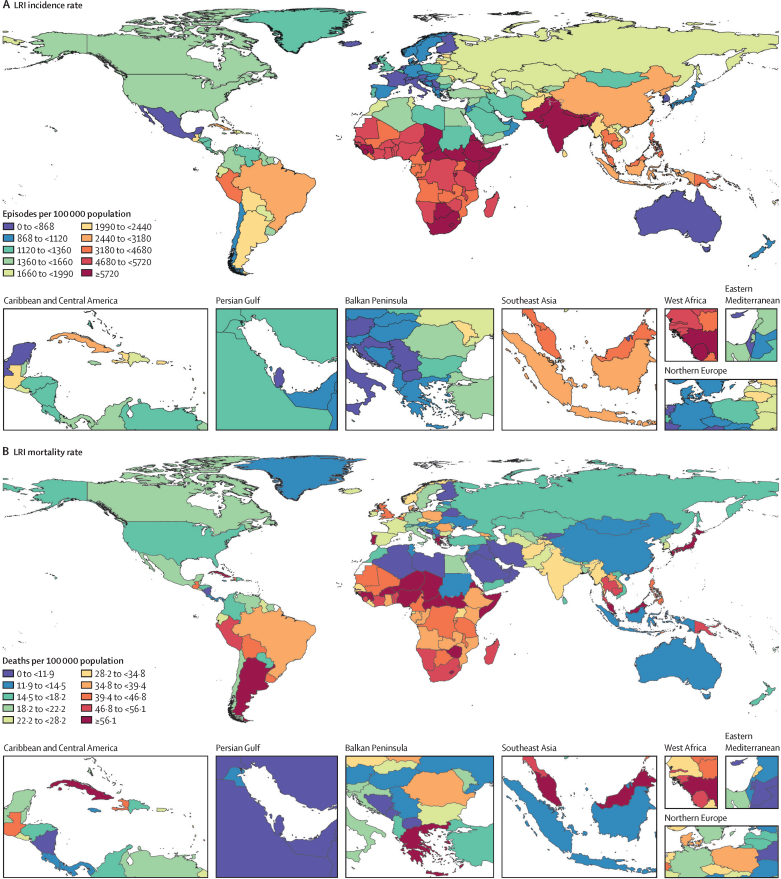
In 2021, we estimated 344 million (325–364) incident episodes of LRI globally, for an all-age incidence rate of 4350 episodes (4120–4610) per 100 000 (table 1). Across 204 modelled locations, the all-age incidence rate in 2021 ranged from 463 episodes (428–500) per 100 000 in Cyprus to 9980 episodes (9220–10 800) per 100 000 in Nepal (figure 1; appendix 2 p 5). Adults aged 70 years and older had the highest global incidence rate at 18 900 episodes (17 100–21 000) per 100 000, followed by adults aged 50–69 years at 6370 episodes (5800–6940) per 100 000 (table 1). Among children younger than 5 years, we estimated 37·8 million (33·5–43·0) incident episodes of LRI and an incidence rate of 5750 episodes (5090–6540) per 100 000 (table 1), ranging from 413 episodes (335–504) per 100 000 in the Netherlands to 12 190 episodes (10 600–13 900) per 100 000 in Pakistan (appendix 2 p 5).
Figure 1.
Global maps of LRI incidence and mortality rates across all ages, 2021
Maps show incidence rates (A) and mortality rates (B) per 100 000 population, with colours representing global deciles. LRI=lower respiratory infection.
Since 1990, the all-age global LRI incidence rate decreased 19·0% (95% UI 16·0–21·9), from 5880 (5510–6250) episodes per 100 000 in 1990 to 4770 episodes (4510–5040) per 100 000 in 2019 (table 1). This decline was primarily attributable to reductions in incidence among children younger than 5 years, which decreased 59·3% (58·3–60·1), from 16 300 episodes (14 500–18 300) per 100 000 in 1990 to 6640 episodes (5900–7490) per 100 000 in 2019 (table 1). By contrast, the global incidence rate among adults aged 70 years and older declined at a lower rate from 1990 to 2019, with an overall decrease of 4·8% (0·4–9·1; table 1).
Mortality of LRIs
Globally in 2019, before reductions in mortality observed during the COVID-19 pandemic, we estimated 2·55 million (95% UI 2·32–2·74) global LRI deaths and an all-age mortality rate of 32·9 deaths (29·9–35·4) per 100 000 population, representing a 41·7% decrease (35·9–46·9) in mortality rate since 1990 (table 2). Among children younger than 5 years, we estimated 693 000 (580 000–822 000) deaths, for a mortality rate of 102·2 deaths (85·5–121·3) per 100 000 in this age group in 2019 (table 2).
Table 2.
Lower respiratory infection mortality counts and rates for all-ages and selected age groups in 1990, 2019, 2020, and 2021, and mortality rate percentage change from 1990 to 2019 and from 2019 to 2021, globally and by SDI quintile and GBD super-region
|
1990 |
2019 |
2020 |
2021 |
Mortality rate change, % |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Death count | Mortality rate per 100 000 population | Death count | Mortality rate per 100 000 population | Death count | Mortality rate per 100 000 population | Death count | Mortality rate per 100 000 population | 1990–2019 | 2019–21 | |
| Global | ||||||||||
| All ages | 3 010 000 (2 730 000 to 3 300 000) | 56·5 (51·3 to 61·9) | 2 550 000 (2 320 000 to 2 740 000) | 32·9 (29·9 to 35·4) | 2 280 000 (2 080 000 to 2 460 000) | 29·1 (26·5 to 31·4) | 2 180 000 (1 980 000 to 2 360 000) | 27·7 (25·1 to 29·9) | −41·7% (−46·9 to −35·9) | −16·0% (−18·6 to −13·1) |
| <5 years | 1 940 000 (1 690 000 to 2 230 000) | 313·7 (272·4 to 359·3) | 693 000 (580 000 to 822 000) | 102·2 (85·5 to 121·3) | 557 000 (455 000 to 665 000) | 83·1 (67·9 to 99·3) | 502 000 (406 000 to 611 000) | 76·2 (61·7 to 92·9) | −67·4% (−72·2 to −61·3) | −25·4% (−30·0 to −20·3) |
| 5–14 years | 89 000 (74 200 to 99 900) | 7·9 (6·6 to 8·9) | 51 900 (45 300 to 58 500) | 3·9 (3·4 to 4·4) | 46 100 (40 100 to 51 900) | 3·4 (3·0 to 3·9) | 43 700 (37 600 to 49 400) | 3·2 (2·8 to 3·7) | −50·8% (−56·3 to −42·5) | −17·4% (−21·2 to −13·6) |
| 15–49 years | 141 000 (130 000 to 150 000) | 5·2 (4·8 to 5·5) | 174 000 (161 000 to 189 000) | 4·5 (4·1 to 4·9) | 162 000 (150 000 to 176 000) | 4·1 (3·8 to 4·5) | 160 000 (147 000 to 175 000) | 4·1 (3·7 to 4·4) | −14·2% (−19·6 to −7·3) | −9·0% (−12·1 to −5·7) |
| 50–69 years | 243 000 (224 000 to 261 000) | 35·6 (32·8 to 38·2) | 394 000 (367 000 to 421 000) | 28·6 (26·7 to 30·6) | 373 000 (345 000 to 400 000) | 26·5 (24·5 to 28·4) | 367 000 (335 000 to 394 000) | 25·5 (23·3 to 27·4) | −19·6% (−24·8 to −13·2) | −10·9% (−14·2 to −7·2) |
| ≥70 years | 596 000 (542 000 to 642 000) | 295·0 (268·1 to 318·0) | 1 240 000 (1 100 000 to 1 330 000) | 266·3 (236·5 to 287·2) | 1 140 000 (1 020 000 to 1 230 000) | 238·5 (212·1 to 256·7) | 1 110 000 (978 000 to 1 200 000) | 224·6 (197·8 to 243·7) | −9·7% (−14·7 to −4·5) | −15·7% (−18·2 to −12·9) |
| High SDI | ||||||||||
| All ages | 269 000 (244 000 to 281 000) | 30·6 (27·7 to 32·0) | 363 000 (308 000 to 393 000) | 33·4 (28·4 to 36·1) | 332 000 (284 000 to 359 000) | 30·4 (26·0 to 32·9) | 299 000 (252 000 to 325 000) | 27·4 (23·0 to 29·7) | 9·2% (2·0 to 13·4) | −18·0% (−19·2 to −17·0) |
| <5 years | 8370 (7650 to 9280) | 13·6 (12·4 to 15·0) | 1750 (1640 to 1870) | 3·1 (2·9 to 3·3) | 1350 (1220 to 1470) | 2·5 (2·2 to 2·7) | 998 (898 to 1080) | 1·9 (1·7 to 2·0) | −76·9% (−79·5 to −74·9) | −40·8% (−45·0 to −37·1) |
| 5–14 years | 1360 (1270 to 1460) | 1·1 (1·0 to 1·2) | 469 (448 to 497) | 0·4 (0·4 to 0·4) | 398 (374 to 428) | 0·3 (0·3 to 0·4) | 354 (333 to 381) | 0·3 (0·3 to 0·3) | −63·9% (−66·5 to −61·1) | −24·9% (−27·2 to −22·8) |
| 15–49 years | 10 500 (10 200 to 10 700) | 2·3 (2·2 to 2·3) | 9230 (8760 to 9810) | 1·8 (1·7 to 1·9) | 8350 (7840 to 8970) | 1·7 (1·6 to 1·8) | 7330 (6850 to 7910) | 1·5 (1·4 to 1·6) | −19·8% (−24·3 to −14·8) | −20·1% (−22·3 to −17·6) |
| 50–69 years | 31 000 (30 200 to 31 600) | 18·9 (18·5 to 19·3) | 37 500 (36 200 to 38 500) | 13·8 (13·3 to 14·2) | 34 300 (33 100 to 35 400) | 12·5 (12·1 to 12·9) | 31 100 (29 900 to 32 200) | 11·3 (10·8 to 11·7) | −27·1% (−28·9 to −25·3) | −18·3% (−19·8 to −16·7) |
| ≥70 years | 218 000 (192 000 to 230 000) | 315·2 (278·4 to 332·6) | 314 000 (260 000 to 343 000) | 231·4 (191·6 to 252·8) | 288 000 (239 000 to 313 000) | 205·7 (171·2 to 224·0) | 260 000 (213 000 to 284 000) | 180·9 (148·2 to 198·0) | −26·6% (−31·8 to −23·6) | −21·8% (−22·9 to −20·8) |
| High-middle SDI | ||||||||||
| All ages | 248 000 (231 000 to 268 000) | 23·3 (21·7 to 25·2) | 275 000 (249 000 to 296 000) | 21·2 (19·2 to 22·8) | 252 000 (226 000 to 272 000) | 19·3 (17·4 to 20·9) | 242 000 (216 000 to 266 000) | 18·5 (16·6 to 20·4) | −9·0% (−17·0 to −0·9) | −12·7% (−17·4 to −7·3) |
| <5 years | 114 000 (101 000 to 131 000) | 122·3 (108·3 to 140·9) | 9000 (7880 to 10 300) | 11·8 (10·3 to 13·4) | 7190 (6200 to 8300) | 9·7 (8·4 to 11·2) | 6000 (5050 to 7020) | 8·6 (7·2 to 10·0) | −90·4% (−92·2 to −88·6) | −27·0% (−31·6 to −22·7) |
| 5–14 years | 5900 (5370 to 6460) | 3·3 (3·0 to 3·6) | 1520 (1410 to 1700) | 1·0 (0·9 to 1·1) | 1280 (1180 to 1440) | 0·8 (0·7 to 0·9) | 1210 (1110 to 1380) | 0·8 (0·7 to 0·9) | −69·9% (−72·9 to −65·9) | −23·5% (−26·5 to −20·8) |
| 15–49 years | 17 100 (16 000 to 18 100) | 3·0 (2·8 to 3·2) | 20 400 (19 600 to 21 300) | 3·2 (3·1 to 3·3) | 18 400 (17 600 to 19 400) | 2·9 (2·8 to 3·1) | 17 200 (16 200 to 18 400) | 2·7 (2·6 to 2·9) | 5·0% (−1·5 to 12·6) | −14·0% (−19·7 to −7·9) |
| 50–69 years | 29 700 (27 800 to 31 700) | 17·1 (16·0 to 18·2) | 48 000 (45 700 to 50 500) | 15·2 (14·5 to 16·0) | 44 700 (42 300 to 47 400) | 13·9 (13·2 to 14·8) | 42 300 (39 600 to 45 300) | 13·0 (12·1 to 13·9) | −10·7% (−17·1 to −3·7) | −14·8% (−19·9 to −8·8) |
| ≥70 years | 81 700 (73 800 to 88 600) | 158·7 (143·5 to 172·1) | 197 000 (171 000 to 216 000) | 178·9 (156·0 to 197·0) | 180 000 (156 000 to 198 000) | 158·7 (137·8 to 174·3) | 175 000 (151 000 to 196 000) | 149·1 (128·3 to 167·0) | 12·7% (4·3 to 21·4) | −16·7% (−21·6 to −11·0) |
| Middle SDI | ||||||||||
| All ages | 777 000 (715 000 to 840 000) | 45·1 (41·5 to 48·8) | 605 000 (555 000 to 647 000) | 25·1 (23·0 to 26·8) | 548 000 (502 000 to 588 000) | 22·5 (20·6 to 24·2) | 543 000 (494 000 to 589 000) | 22·2 (20·2 to 24·1) | −44·3% (−48·9 to −39·2) | −11·7% (−16·1 to −7·3) |
| <5 years | 509 000 (457 000 to 568 000) | 253·9 (227·7 to 283·2) | 90 900 (78 300 to 106 000) | 48·5 (41·8 to 56·4) | 70 200 (59 900 to 82 000) | 38·3 (32·7 to 44·8) | 60 400 (50 800 to 71 200) | 34·2 (28·8 to 40·3) | −80·9% (−83·8 to −77·4) | −29·4% (−34·0 to −24·6) |
| 5–14 years | 26 300 (22 100 to 28 600) | 7·0 (5·9 to 7·6) | 9510 (8610 to 10 700) | 2·5 (2·3 to 2·8) | 8170 (7440 to 9070) | 2·1 (1·9 to 2·3) | 7660 (6950 to 8440) | 2·0 (1·8 to 2·2) | −64·3% (−68·2 to −57·6) | −21·2% (−24·9 to −17·3) |
| 15–49 years | 46 100 (42 500 to 48 900) | 5·1 (4·7 to 5·4) | 47 000 (44 800 to 50 000) | 3·8 (3·6 to 4·0) | 42 700 (40 500 to 45 300) | 3·4 (3·2 to 3·6) | 42 700 (40 000 to 45 900) | 3·4 (3·2 to 3·7) | −25·7% (−30·5 to −20·1) | −9·5% (−14·1 to −4·9) |
| 50–69 years | 60 400 (55 100 to 65 500) | 31·9 (29·1 to 34·6) | 111 000 (104 000 to 117 000) | 24·1 (22·5 to 25·4) | 105 000 (97 800 to 112 000) | 22·3 (20·6 to 23·7) | 106 000 (97 300 to 114 000) | 21·8 (20·0 to 23·4) | −24·5% (−30·5 to −17·2) | −9·5% (−14·7 to −4·5) |
| ≥70 years | 135 000 (122 000 to 149 000) | 295·5 (266·1 to 326·0) | 348 000 (309 000 to 376 000) | 265·6 (236·1 to 287·7) | 321 000 (284 000 to 349 000) | 237·0 (209·5 to 258·0) | 326 000 (288 000 to 358 000) | 231·5 (204·3 to 254·2) | −10·1% (−17·4 to −1·8) | −12·9% (−17·5 to −7·8) |
| Low-middle SDI | ||||||||||
| All ages | 954 000 (850 000 to 1 070 000) | 82·1 (73·2 to 91·9) | 712 000 (641 000 to 777 000) | 37·9 (34·2 to 41·4) | 619 000 (558 000 to 680 000) | 32·6 (29·4 to 35·8) | 594 000 (528 000 to 657 000) | 30·9 (27·5 to 34·2) | −53·8% (−59·2 to −47·8) | −18·5% (−22·8 to −13·5) |
| <5 years | 719 000 (626 000 to 827 000) | 414·3 (360·7 to 476·8) | 263 000 (222 000 to 307 000) | 134·3 (113·6 to 156·9) | 200 000 (168 000 to 238 000) | 103·4 (86·7 to 122·8) | 180 000 (148 000 to 215 000) | 94·0 (77·5 to 112·4) | −67·6% (−73·0 to −61·3) | −30·0% (−35·9 to −23·2) |
| 5–14 years | 31 500 (26 000 to 36 500) | 10·6 (8·7 to 12·2) | 17 300 (15 000 to 19 700) | 4·5 (3·9 to 5·1) | 15 000 (12 900 to 17 100) | 3·9 (3·3 to 4·4) | 14 200 (12 100 to 16 300) | 3·6 (3·1 to 4·2) | −57·6% (−63·5 to −49·2) | −18·5% (−23·0 to −13·9) |
| 15–49 years | 37 200 (33 900 to 42 200) | 6·7 (6·1 to 7·7) | 50 400 (45 400 to 56 900) | 5·1 (4·6 to 5·8) | 47 400 (42 600 to 53 600) | 4·7 (4·3 to 5·4) | 47 200 (41 900 to 53 500) | 4·6 (4·1 to 5·3) | −24·4% (−31·0 to −15·8) | −9·0% (−13·8 to −4·1) |
| 50–69 years | 68 000 (60 400 to 75 700) | 60·8 (54·0 to 67·6) | 123 000 (110 000 to 135 000) | 50·8 (45·7 to 56·0) | 116 000 (103 000 to 129 000) | 46·5 (41·4 to 51·8) | 114 000 (100 000 to 127 000) | 44·8 (39·3 to 50·0) | −16·5% (−25·4 to −4·8) | −11·7% (−17·0 to −5·5) |
| ≥70 years | 98 100 (85 900 to 114 000) | 374·0 (327·5 to 435·3) | 259 000 (232 000 to 286 000) | 388·4 (348·6 to 428·5) | 241 000 (215 000 to 268 000) | 352·6 (314·0 to 391·8) | 238 000 (209 000 to 268 000) | 340·2 (298·2 to 382·1) | 3·8% (−8·4 to 17·7) | −12·4% (−17·3 to −7·2) |
| Low SDI | ||||||||||
| All ages | 763 000 (644 000 to 891 000) | 152·2 (128·5 to 177·7) | 591 000 (512 000 to 681 000) | 55·4 (48·0 to 63·8) | 527 000 (452 000 to 611 000) | 48·3 (41·4 to 56·0) | 503 000 (430 000 to 582 000) | 45·0 (38·5 to 52·1) | −63·6% (−68·8 to −57·2) | −18·9% (−22·5 to −15·1) |
| <5 years | 593 000 (477 000 to 726 000) | 653·5 (525·6 to 800·1) | 328 000 (262 000 to 403 000) | 202·5 (162·0 to 249·0) | 277 000 (217 000 to 346 000) | 169·3 (132·5 to 211·1) | 254 000 (197 000 to 320 000) | 153·2 (118·7 to 193·4) | −69·0% (−74·4 to −62·1) | −24·3% (−29·4 to −19·3) |
| 5–14 years | 23 800 (18 100 to 28 600) | 17·3 (13·1 to 20·7) | 23 100 (19 200 to 26 900) | 8·1 (6·7 to 9·4) | 21 200 (17 500 to 24 600) | 7·3 (6·0 to 8·5) | 20 300 (16 700 to 23 900) | 6·9 (5·7 to 8·1) | −53·2% (−60·5 to −41·8) | −14·7% (−19·2 to −9·7) |
| 15–49 years | 29 800 (25 600 to 33 700) | 13·5 (11·6 to 15·2) | 46 600 (40 300 to 54 000) | 9·1 (7·9 to 10·6) | 44 900 (38 900 to 52 000) | 8·5 (7·4 to 9·9) | 45 600 (39 200 to 52 700) | 8·4 (7·2 to 9·7) | −32·4% (−40·1 to −22·8) | −7·8% (−12·3 to −3·3) |
| 50–69 years | 53 400 (46 100 to 60 500) | 127·2 (109·8 to 144·1) | 74 800 (65 300 to 85 400) | 85·9 (75·0 to 98·1) | 72 600 (63 300 to 83 000) | 80·4 (70·2 to 92·0) | 72 900 (63 200 to 83 500) | 78·5 (68·1 to 90·0) | −32·5% (−39·9 to −23·3) | −8·6% (−12·9 to −4·4) |
| ≥70 years | 62 800 (54 500 to 72 200) | 673·0 (584·5 to 773·7) | 119 000 (106 000 to 136 000) | 567·4 (504·6 to 647·7) | 111 000 (99 300 to 126 000) | 521·0 (464·4 to 590·1) | 110 000 (97 900 to 126 000) | 501·7 (446·2 to 572·5) | −15·7% (−24·7 to −5·3) | −11·6% (−15·9 to −7·4) |
| Central Europe, Eastern Europe, and Central Asia | ||||||||||
| All ages | 108 000 (104 000 to 112 000) | 25·6 (24·7 to 26·7) | 102 000 (96 600 to 106 000) | 24·3 (23·1 to 25·3) | 96 200 (91 200 to 101 000) | 23·0 (21·8 to 24·1) | 82 800 (77 800 to 87 500) | 19·8 (18·6 to 21·0) | −5·3% (−9·8 to −0·9) | −18·4% (−21·5 to −15·2) |
| <5 years | 63 600 (60 000 to 67 600) | 177·0 (167·0 to 188·2) | 16 200 (13 700 to 19 000) | 59·9 (50·8 to 70·2) | 14 500 (12 300 to 17 000) | 55·1 (46·7 to 64·5) | 11 000 (9240 to 13 200) | 43·0 (35·9 to 51·3) | −66·2% (−71·1 to −60·2) | −28·3% (−32·0 to −24·5) |
| 5–14 years | 2640 (2520 to 2740) | 3·8 (3·6 to 3·9) | 1460 (1330 to 1610) | 2·7 (2·5 to 3·0) | 1370 (1240 to 1500) | 2·5 (2·3 to 2·8) | 1190 (1080 to 1320) | 2·2 (2·0 to 2·4) | −27·5% (−33·9 to −20·0) | −20·9% (−23·3 to −18·2) |
| 15–49 years | 8800 (8620 to 8980) | 4·3 (4·2 to 4·4) | 14 600 (14 100 to 15 200) | 7·3 (7·0 to 7·6) | 13 600 (13 000 to 14 300) | 6·9 (6·6 to 7·2) | 12 200 (11 300 to 13 300) | 6·2 (5·7 to 6·7) | 70·7% (64·2 to 78·3) | −15·2% (−21·7 to −8·5) |
| 50–69 years | 13 800 (13 500 to 14 100) | 16·5 (16·1 to 16·8) | 26 200 (25 400 to 27 000) | 26·1 (25·4 to 26·9) | 24 700 (23 700 to 25 700) | 24·7 (23·7 to 25·7) | 21 900 (20 600 to 23 500) | 22·0 (20·6 to 23·5) | 58·9% (53·7 to 64·3) | −15·8% (−21·0 to −10·6) |
| ≥70 years | 19 200 (18 100 to 19 900) | 75·7 (71·4 to 78·5) | 43 200 (39 500 to 45 300) | 113·8 (103·9 to 119·2) | 42 000 (38 100 to 44 700) | 107·9 (97·8 to 114·7) | 36 400 (32 900 to 38 600) | 91·9 (82·9 to 97·6) | 50·4% (43·8 to 56·0) | −19·3% (−21·9 to −16·5) |
| High-income | ||||||||||
| All ages | 280 000 (252 000 to 293 000) | 30·8 (27·7 to 32·2) | 400 000 (339 000 to 432 000) | 36·8 (31·2 to 39·8) | 361 000 (306 000 to 390 000) | 33·1 (28·1 to 35·8) | 321 000 (267 000 to 348 000) | 29·4 (24·5 to 31·9) | 19·6% (11·8 to 24·2) | −20·2% (−21·2 to −19·3) |
| <5 years | 6180 (5970 to 6410) | 10·0 (9·7 to 10·4) | 1640 (1570 to 1720) | 2·9 (2·8 to 3·0) | 1180 (1070 to 1270) | 2·1 (1·9 to 2·3) | 855 (760 to 943) | 1·6 (1·4 to 1·7) | −71·1% (−72·4 to −69·5) | −45·8% (−51·1 to −40·8) |
| 5–14 years | 1040 (976 to 1100) | 0·8 (0·8 to 0·9) | 439 (427 to 451) | 0·4 (0·3 to 0·4) | 358 (343 to 375) | 0·3 (0·3 to 0·3) | 327 (310 to 343) | 0·3 (0·3 to 0·3) | −56·6% (−59·2 to −53·6) | −25·2% (−28·3 to −22·5) |
| 15–49 years | 9940 (9780 to 10 100) | 2·1 (2·1 to 2·1) | 8020 (7850 to 8210) | 1·6 (1·6 to 1·7) | 6950 (6710 to 7190) | 1·4 (1·4 to 1·5) | 6040 (5860 to 6220) | 1·2 (1·2 to 1·3) | −22·1% (−24·1 to −20·1) | −24·3% (−25·7 to −22·8) |
| 50–69 years | 31 300 (30 500 to 31 800) | 17·8 (17·4 to 18·2) | 37 200 (36 000 to 38 200) | 13·6 (13·2 to 14·0) | 33 700 (32 600 to 34 700) | 12·2 (11·8 to 12·6) | 30 300 (29 200 to 31 300) | 10·9 (10·5 to 11·3) | −23·7% (−25·7 to −21·7) | −19·8% (−20·9 to −18·6) |
| ≥70 years | 231 000 (204 000 to 244 000) | 304·4 (268·8 to 321·5) | 352 000 (292 000 to 384 000) | 241·2 (199·9 to 263·2) | 318 000 (264 000 to 347 000) | 212·3 (176·1 to 231·3) | 283 000 (231 000 to 310 000) | 184·9 (150·5 to 202·3) | −20·8% (−26·1 to −17·7) | −23·4% (−24·3 to −22·5) |
| Latin America and Caribbean | ||||||||||
| All ages | 166 000 (158 000 to 174 000) | 42·6 (40·6 to 44·7) | 215 000 (195 000 to 228 000) | 36·7 (33·2 to 39·0) | 187 000 (169 000 to 200 000) | 31·7 (28·7 to 33·9) | 177 000 (157 000 to 194 000) | 29·8 (26·5 to 32·6) | −13·9% (−21·0 to −8·2) | −18·9% (−22·5 to −14·8) |
| <5 years | 89 000 (82 600 to 95 800) | 179·7 (166·8 to 193·6) | 20 100 (16 400 to 23 800) | 41·2 (33·8 to 48·8) | 14 400 (11 700 to 17 400) | 30·0 (24·5 to 36·1) | 12 200 (9570 to 15 200) | 25·7 (20·2 to 32·1) | −77·0% (−81·2 to −72·7) | −37·6% (−44·2 to −30·5) |
| 5–14 years | 4890 (4640 to 5130) | 5·2 (4·9 to 5·4) | 2250 (2010 to 2500) | 2·4 (2·1 to 2·6) | 1820 (1630 to 2030) | 1·9 (1·7 to 2·1) | 1620 (1430 to 1850) | 1·7 (1·5 to 1·9) | −54·4% (−59·2 to −49·5) | −28·0% (−33·8 to −22·1) |
| 15–49 years | 13 000 (12 600 to 13 400) | 6·6 (6·4 to 6·8) | 18 000 (17 300 to 18 800) | 5·8 (5·6 to 6·1) | 16 000 (15 100 to 16 900) | 5·1 (4·9 to 5·4) | 15 500 (14 500 to 16 900) | 5·0 (4·6 to 5·4) | −11·7% (−15·6 to −7·5) | −14·5% (−18·9 to −9·8) |
| 50–69 years | 16 000 (15 400 to 16 500) | 42·0 (40·5 to 43·5) | 38 400 (36 600 to 39 900) | 38·5 (36·8 to 40·1) | 36 200 (34 400 to 38 300) | 35·4 (33·6 to 37·4) | 35 400 (32 800 to 38 400) | 33·9 (31·4 to 36·7) | −8·2% (−12·4 to −4·1) | −12·1% (−16·7 to −7·1) |
| ≥70 years | 43 500 (40 100 to 45 600) | 398·9 (367·7 to 417·9) | 136 000 (119 000 to 146 000) | 417·6 (363·7 to 446·6) | 119 000 (103 000 to 128 000) | 353·3 (306·4 to 379·4) | 112 000 (96 000 to 123 000) | 325·1 (278·3 to 356·4) | 4·7% (−1·5 to 9·3) | −22·1% (−25·8 to −18·3) |
| North Africa and Middle East | ||||||||||
| All ages | 181 000 (159 000 to 218 000) | 53·3 (46·8 to 64·2) | 113 000 (102 000 to 126 000) | 18·7 (16·8 to 20·7) | 103 000 (91 000 to 116 000) | 16·8 (14·8 to 18·9) | 92 200 (81 400 to 105 000) | 14·8 (13·1 to 16·8) | −64·9% (−70·7 to −60·0) | −20·9% (−24·8 to −16·5) |
| <5 years | 138 000 (118 000 to 176 000) | 270·2 (230·0 to 343·4) | 32 700 (26 900 to 39 900) | 51·4 (42·2 to 62·7) | 25 900 (21 000 to 31 300) | 41·4 (33·6 to 50·1) | 20 200 (16 600 to 24 600) | 33·1 (27·1 to 40·3) | −81·0% (−84·8 to −77·0) | −35·6% (−41·6 to −28·8) |
| 5–14 years | 7290 (6190 to 8320) | 8·2 (6·9 to 9·3) | 3610 (3010 to 4380) | 3·0 (2·5 to 3·7) | 3200 (2660 to 3900) | 2·7 (2·2 to 3·2) | 2880 (2350 to 3550) | 2·4 (1·9 to 2·9) | −62·7% (−70·0 to −55·2) | −22·8% (−27·8 to −17·8) |
| 15–49 years | 7660 (6870 to 8970) | 4·8 (4·3 to 5·6) | 11 800 (10 400 to 13 300) | 3·6 (3·2 to 4·1) | 11 100 (9600 to 12 800) | 3·4 (2·9 to 3·9) | 10 500 (8980 to 12 200) | 3·1 (2·7 to 3·6) | −24·4% (−32·7 to −15·3) | −13·4% (−18·2 to −8·6) |
| 50–69 years | 9840 (8750 to 11 400) | 31·5 (28·0 to 36·6) | 18 700 (16 600 to 20 800) | 23·6 (21·0 to 26·4) | 18 300 (16 000 to 20 700) | 22·3 (19·5 to 25·3) | 17 600 (15 100 to 20 500) | 20·7 (17·7 to 24·1) | −25·0% (−34·0 to −15·6) | −12·5% (−18·9 to −6·1) |
| ≥70 years | 17 600 (15 300 to 21 400) | 243·0 (211·8 to 296·3) | 46 600 (40 300 to 51 500) | 241·9 (209·1 to 267·6) | 44 600 (38 400 to 50 200) | 224·8 (193·8 to 253·1) | 41 000 (35 300 to 46 200) | 201·6 (173·4 to 227·0) | −0·5% (−15·0 to 11·3) | −16·6% (−20·3 to −12·6) |
| South Asia | ||||||||||
| All ages | 802 000 (696 000 to 902 000) | 73·3 (63·7 to 82·5) | 609 000 (548 000 to 674 000) | 33·7 (30·3 to 37·3) | 522 000 (465 000 to 582 000) | 28·5 (25·4 to 31·8) | 516 000 (451 000 to 584 000) | 27·9 (24·4 to 31·6) | −54·1% (−60·3 to −46·5) | −17·1% (−24·2 to −9·2) |
| <5 years | 610 000 (516 000 to 707 000) | 388·6 (328·5 to 450·2) | 229 000 (191 000 to 273 000) | 140·6 (117·4 to 167·3) | 167 000 (135 000 to 202 000) | 103·6 (84·2 to 125·9) | 154 000 (124 000 to 190 000) | 97·3 (78·5 to 119·7) | −63·8% (−70·8 to −54·9) | −30·8% (−39·5 to −20·1) |
| 5–14 years | 27 900 (21 800 to 33 400) | 10·1 (7·9 to 12·1) | 13 000 (10 800 to 15 300) | 3·7 (3·1 to 4·4) | 10 800 (8890 to 12 800) | 3·1 (2·5 to 3·6) | 10 200 (8360 to 12 100) | 2·9 (2·4 to 3·5) | −63·4% (−69·9 to −53·9) | −20·4% (−27·6 to −12·6) |
| 15–49 years | 27 200 (24 300 to 32 700) | 5·1 (4·6 to 6·2) | 31 300 (28 100 to 37 600) | 3·2 (2·9 to 3·8) | 30 000 (26 500 to 35 800) | 3·0 (2·7 to 3·6) | 30 800 (26 600 to 37 100) | 3·1 (2·6 to 3·7) | −37·7% (−44·2 to −29·7) | −4·5% (−14·4 to 6·2) |
| 50–69 years | 58 900 (51 000 to 68 000) | 54·8 (47·5 to 63·3) | 108 000 (95 200 to 122 000) | 44·1 (38·8 to 49·7) | 101 000 (88 600 to 116 000) | 39·9 (35·0 to 45·9) | 101 000 (86 800 to 117 000) | 38·9 (33·4 to 45·2) | −19·6% (−29·5 to −6·7) | −11·8% (−21·0 to −1·5) |
| ≥70 years | 77 600 (64 200 to 93 800) | 330·4 (273·4 to 399·3) | 227 000 (199 000 to 257 000) | 329·4 (288·5 to 372·3) | 213 000 (186 000 to 244 000) | 300·7 (262·1 to 344·2) | 219 000 (187 000 to 257 000) | 299·7 (255·5 to 350·5) | −0·3% (−14·1 to 18·0) | −9·0% (−17·2 to −0·4) |
| Southeast Asia, East Asia, and Oceania | ||||||||||
| All ages | 734 000 (666 000 to 809 000) | 43·5 (39·4 to 47·9) | 455 000 (410 000 to 499 000) | 21·1 (19·0 to 23·1) | 424 000 (378 000 to 469 000) | 19·5 (17·4 to 21·6) | 431 000 (384 000 to 482 000) | 19·7 (17·6 to 22·0) | −51·5% (−56·9 to −45·6) | −6·2% (−13·6 to 2·1) |
| <5 years | 486 000 (426 000 to 557 000) | 277·7 (243·2 to 318·4) | 57 700 (48 400 to 68 100) | 38·5 (32·3 to 45·5) | 48 700 (40 900 to 57 400) | 33·4 (28·1 to 39·5) | 41 700 (34 400 to 49 200) | 30·1 (24·9 to 35·6) | −86·1% (−88·5 to −83·2) | −21·8% (−26·1 to −17·0) |
| 5–14 years | 23 400 (19 000 to 26 000) | 7·1 (5·8 to 7·9) | 5790 (5130 to 6860) | 2·0 (1·7 to 2·3) | 5070 (4530 to 5970) | 1·7 (1·5 to 2·0) | 4810 (4220 to 5640) | 1·6 (1·4 to 1·8) | −72·4% (−76·3 to −64·5) | −20·3% (−24·1 to −15·9) |
| 15–49 years | 36 000 (31 700 to 39 600) | 3·9 (3·4 to 4·3) | 26 200 (24 100 to 29 300) | 2·4 (2·2 to 2·7) | 23 900 (21 700 to 26 800) | 2·2 (2·0 to 2·5) | 23 500 (21 000 to 26 200) | 2·2 (2·0 to 2·5) | −37·5% (−45·0 to −28·8) | −9·1% (−17·0 to −0·5) |
| 50–69 years | 55 200 (48 400 to 61 800) | 26·6 (23·3 to 29·8) | 72 600 (65 700 to 79 600) | 14·7 (13·3 to 16·1) | 69 500 (62 700 to 76 500) | 13·7 (12·3 to 15·1) | 69 800 (62 000 to 77 700) | 13·4 (11·9 to 15·0) | −44·7% (−51·9 to −36·3) | −8·6% (−17·3 to 1·4) |
| ≥70 years | 134 000 (116 000 to 150 000) | 267·5 (232·5 to 300·6) | 293 000 (257 000 to 327 000) | 208·4 (182·3 to 232·3) | 276 000 (239 000 to 309 000) | 188·9 (163·6 to 211·5) | 292 000 (252 000 to 331 000) | 189·5 (163·6 to 214·7) | −22·1% (−30·8 to −12·0) | −9·1% (−17·0 to 0·1) |
| Sub-Saharan Africa | ||||||||||
| All ages | 742 000 (629 000 to 875 000) | 151·1 (127·9 to 178·0) | 655 000 (557 000 to 757 000) | 60·7 (51·6 to 70·1) | 588 000 (494 000 to 686 000) | 53·1 (44·6 to 62·0) | 563 000 (472 000 to 655 000) | 49·7 (41·6 to 57·8) | −59·8% (−65·1 to −53·2) | −18·2% (−21·9 to −14·1) |
| <5 years | 551 000 (443 000 to 683 000) | 614·5 (494·0 to 761·5) | 335 000 (261 000 to 418 000) | 197·9 (153·7 to 246·8) | 285 000 (217 000 to 361 000) | 166·6 (126·7 to 211·0) | 261 000 (197 000 to 334 000) | 151·2 (113·9 to 193·4) | −67·8% (−73·4 to −60·8) | −23·6% (−28·6 to −18·3) |
| 5–14 years | 21 900 (17 000 to 26 300) | 16·2 (12·6 to 19·5) | 25 400 (20 700 to 30 100) | 8·7 (7·1 to 10·3) | 23 500 (18 900 to 27 800) | 7·9 (6·4 to 9·4) | 22 700 (18 100 to 27 100) | 7·5 (6·0 to 8·9) | −46·3% (−54·5 to −33·2) | −14·2% (−19·0 to −8·6) |
| 15–49 years | 38 100 (33 000 to 42 300) | 17·4 (15·0 to 19·3) | 63 800 (55 200 to 73 300) | 12·4 (10·7 to 14·2) | 60 400 (52 000 to 69 700) | 11·4 (9·8 to 13·1) | 61 500 (53 200 to 71 000) | 11·3 (9·7 to 13·0) | −28·8% (−36·6 to −18·8) | −9·2% (−13·9 to −3·9) |
| 50–69 years | 57 700 (50 100 to 65 400) | 150·0 (130·3 to 169·8) | 92 600 (81 100 to 105 000) | 109·2 (95·7 to 123·8) | 89 600 (78 200 to 102 000) | 102·1 (89·1 to 115·7) | 90 600 (78 900 to 103 000) | 100·1 (87·2 to 113·7) | −27·2% (−35·0 to −16·6) | −8·4% (−12·6 to −3·9) |
| ≥70 years | 73 300 (64 500 to 83 000) | 793·6 (698·0 to 898·2) | 138 000 (124 000 to 155 000) | 732·9 (656·0 to 820·7) | 129 000 (115 000 to 143 000) | 668·2 (595·9 to 742·1) | 127 000 (113 000 to 141 000) | 646·4 (576·2 to 718·2) | −7·6% (−16·2 to 2·8) | −11·8% (−15·7 to −7·6) |
Values in parentheses are 95% uncertainty intervals. Count data are presented to three significant figures. GBD=Global Burden of Diseases, Injuries, and Risk Factors Study. SDI=Socio-demographic Index.
In 2021, we estimated 2·18 million (1·98–2·36) deaths globally due to LRI and an all-age mortality rate of 27·7 deaths (25·1–29·9) per 100 000 (table 2). The all-age mortality rate ranged from 2·3 deaths (1·8–2·9) per 100 000 in Qatar to 104·0 deaths (81·8–129·2) per 100 000 in Chad (figure 1; appendix 2 p 86). Among children younger than 5 years, we estimated 502 000 deaths (406 000–611 000) due to LRI globally, or 76·2 deaths (61·7–92·9) per 100 000 (table 2), ranging from 0·3 deaths (0·2–0·5) per 100 000 in Andorra to 357·9 deaths (271·4–456·4) per 100 000 in Chad (appendix 2 p 86). Across the aggregated age groups, adults aged 70 years and older had the highest global mortality rate (224·6 deaths [197·8–243·7] per 100 000), followed by children younger than 5 years (table 2).
LRI fatalities in 2021, especially among children, were concentrated in countries with a low Socio-demographic Index (SDI; appendix 2 p 5).38 Of 204 modelled countries and territories, 57 had an LRI mortality rate greater than 60 per 100 000 among children younger than 5 years in 2021 (appendix 2 p 86). In 2021, among children younger than 5 years, mortality rates per 100 000 population were 153·2 deaths (118·7–193·4) in low SDI countries, 94·0 (77·5–112·4) in low-middle SDI countries, 34·2 (28·8–40·3) in middle SDI countries, 8·6 (7·2–10·0) in high-middle SDI countries, and 1·9 (1·7–2·0) in high SDI countries (table 2). In total, 254 000 LRI deaths (197 000–320 000) in children younger than 5 years occurred in low SDI countries (table 2). However, although the low SDI quintile had the highest burden in 2021, these countries also showed the greatest improvement in all-age mortality rates over time (table 2).
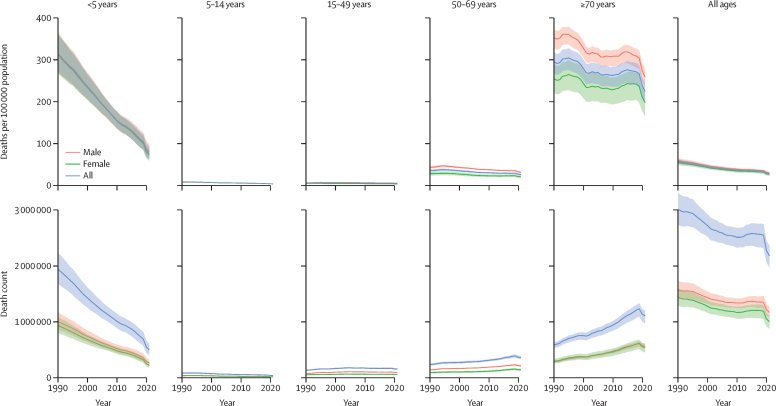
Globally, between 1990 and 2021, the all-age LRI mortality rate decreased by 50·9% (95% UI 45·6–55·9), from 56·5 deaths (51·3–61·9) to 27·7 deaths (25·1–29·9) per 100 000 population (figure 2). For males, it decreased by 49·4% (44·0–54·4), from 58·6 deaths (53·0–64·6) to 29·6 deaths (27·2–32·1) per 100 000. For females, it decreased by 52·7% (46·3–58·6), from 54·4 deaths (48·8–60·5) to 25·7 deaths (22·5–28·3) per 100 000 (figure 2). Analogous to incidence, the decline in mortality was largely attributable to reductions in deaths among children; LRI mortality rate decreased by 75·6% (70·7–79·8) in children younger than 5 years and 59·2% (52·7–64·2) in children aged 5–14 years (figure 2). Adults aged 70 years and older had the smallest decrease in LRI mortality rate, with a 23·8% (18·7–28·7) decline (figure 2). More detailed results on LRI incidence and mortality for additional age groups by sex, country, and year are available online via the GBD Results Tool on the GHDx.
Figure 2.
LRI mortality rates and death counts by age and sex, 1990–2021
Upper graphs show mortality rates per 100 000 population. Lower graphs show death counts. Shaded areas represent 95% uncertainty intervals. LRI=lower respiratory infection.
Aetiologies of LRIs
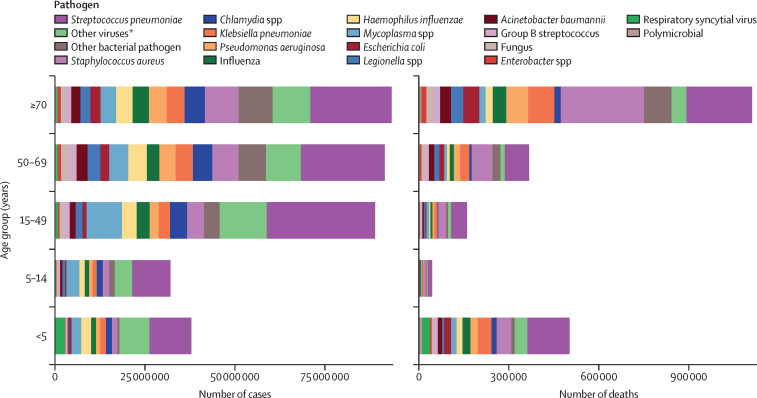
In 2021, the pathogen responsible for the largest proportion of LRI incident episodes globally was S pneumoniae, which caused an estimated 97·9 million (95% UI 92·1–104·0) episodes (Figure 3, Figure 4; appendix 2 p 2104). This was followed by the categories of other viruses (ie, the aggregate of all viruses studied except influenza and RSV; 46·4 million [43·6–49·3] episodes) and Mycoplasma spp (25·3 million [23·5–27·2] episodes; Figure 3, Figure 4; appendix 2 p 2104). Key pathogens varied by age and geography. S pneumoniae was responsible for the largest number of episodes in 165 of the 204 modelled countries and territories in 2021, while the category of other viruses was responsible for the largest number of episodes in 39 countries (appendix 2 p 156). For all five studied age subdivisions, S pneumoniae caused the most episodes (figure 3; appendix 2 p 2104).
Figure 3.
Aetiology distribution of global LRI cases and deaths by age group, 2021
LRI=lower respiratory infection. *“Other viruses” represents the aggregate of all viruses studied except influenza and respiratory syncytial virus.
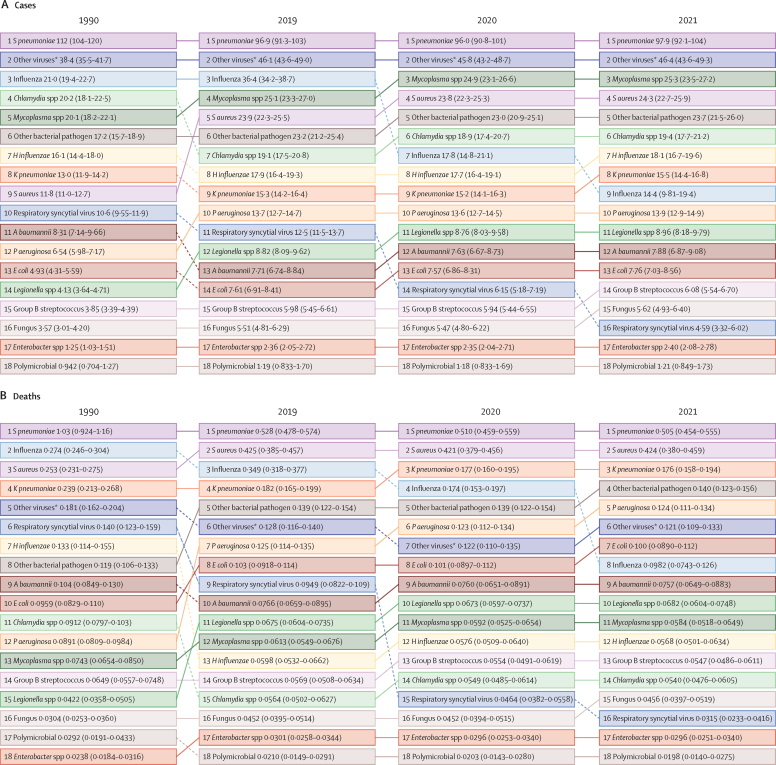
Figure 4.
Ranked aetiologies by number of global cases and deaths across all ages, 1990, 2019, 2020, and 2021
Values are estimated millions of cases (A) or deaths (B) caused by each pathogen, with 95% uncertainty intervals in parentheses. Estimates are presented to three significant figures. A baumannii=Acinetobacter baumannii. E coli=Escherichia coli. H influenzae=Haemophilus influenzae. K pneumoniae=Klebsiella pneumoniae. P aeruginosa=Pseudomonas aeruginosa. S aureus=Staphylococcus aureus. S pneumoniae=Streptococcus pneumoniae. *“Other viruses” represents the aggregate of all viruses studied except influenza and respiratory syncytial virus.
In 2019, before the COVID-19 pandemic and the decline in observed incidence of influenza and RSV, the first and second most common aetiologies were the same as for 2021, but the third most common aetiology was influenza, responsible for 36·4 million (95% UI 34·2–38·7) episodes globally (figure 4). S pneumoniae was responsible for the most LRI episodes in all five age groups in 2019, and was followed by the category of other viruses in all age groups except 70 years and older, in which influenza ranked second highest (appendix 2 p 2104). The third most common aetiology was other viruses in people aged 70 years and older, RSV in children younger than 5 years, Mycoplasma spp in children aged 5–14 years and people aged 15–49 years, and influenza in people aged 50–69 years (appendix 2 p 1971).
In 2021, the pathogen responsible for the largest proportion of all-age LRI deaths globally was also S pneumoniae, which led to an estimated 505 000 deaths (95% UI 454 000–555 000; figure 4; appendix 2 p 2107). This was followed by S aureus (424 000 deaths [380 000–459 000]) and K pneumoniae (176 000 deaths [158 000–194 000]; figure 4; appendix 2 p 2104). In 2019, before COVID-19 impacted the transmission of influenza and RSV, the first and second most common aetiologies leading to LRI death were the same as in 2021, but the third most common aetiology was influenza, which led to 349 000 deaths (318 000–377 000) globally (figure 4). Across age groups, in both 2019 and 2021, S pneumoniae was responsible for the most LRI deaths in people younger than 70 years, whereas S aureus caused the most deaths in people aged 70 years and older (figure 3; appendix 2 p 2104). In 2019, the second largest number of deaths came from S aureus in all age groups except children younger than 5 years, for whom the second-ranked aetiology was RSV, and people aged 70 years and older, for whom the second-ranked aetiology was S pneumoniae. The third most common aetiology leading to death was influenza for all five age groups (appendix 2 p 1971). In 2021, S pneumoniae was responsible for the highest number of deaths in 103 of 204 modelled countries and territories, whereas S aureus was responsible for the most deaths in the remaining 101 countries. These differences were largely attributable to differences in age structures across countries (appendix 2 p 156).
From 1990 to 2019, H influenzae had the largest reduction in global mortality (a 54·8% decrease [95% UI 48·8–60·6] to 59 800 deaths [53 200–66 200]), followed by S pneumoniae (48·5% decrease [42·8–53·9]; appendix 2 p 1971). Most of this improvement for both pathogens was in children younger than 5 years, with a 77·4% (72·9–81·2) decline in deaths due to H influenzae (from 102 000 [83 800–123 000] to 23 000 [18 600–27 700]) and a 76·1% (71·4–79·7) decline in deaths due to S pneumoniae (from 721 000 [621 000–843 000] to 172 000 [142 000–205 000]) during this period (appendix 2 p 1971).
COVID-19 impact
Following the onset of the COVID-19 pandemic, we estimated that from 2019 to 2021, the number of influenza episodes decreased by 60·3% (95% UI 47·1–72·9) to 14·4 million (9·81–19·4) episodes, and deaths decreased by 71·8% (63·8–78·9) to 98 200 (74 300–126 000; appendix 2 p 1951). Across 18 modelled pathogen categories, influenza fell from being the third leading cause of both LRI episodes and deaths globally in 2019, to the ninth leading cause of episodes and the eighth leading cause of deaths in 2021 (figure 4). The high-income super-region saw the largest decrease in influenza episodes from 2019 to 2021 (91·5% [86·6–94·7]), and south Asia had the smallest decrease in influenza episodes in that same time frame (44·0% [14·6–71·8]; appendix 2 p 1951).
Similarly, since 2019, we estimated that global RSV episodes declined by 63·2% (53·1–72·7) to reach 4·59 million (3·32–6·02) in 2021, with a similar decrease in RSV deaths (66·7% [56·6–75·3]), to 31 500 (23 300–41 600) in 2021 (figure 4; appendix 2 p 1951).
Overall, for non-COVID-19 LRIs from 2019 to 2021, we estimated an 8·6% (6·6–10·4) decline in the overall incidence rate, from 4770 episodes (4510–5040) to 4350 episodes (4120–4610) per 100 000 population (from 369 million [349–391] to 344 million [325–364] total episodes), and a 16·0% (13·1–18·6) decline in mortality rate, from 32·9 deaths (29·9–35·4) to 27·7 deaths (25·1–29·9) per 100 000 (table 2).
Discussion
This study provides comprehensive global, regional, and national estimates of LRI episodes and deaths attributable to 18 pathogen categories, by age group, from 1990 until 2021. These estimates are inclusive of the reduction in transmission of certain respiratory viruses observed during the COVID-19 pandemic and implementation of non-pharmaceutical interventions. We estimated 344 million (95% UI 325–364) incident episodes of LRIs and 2·18 million (1·98–2·36) deaths worldwide in 2021. S pneumoniae was responsible for the highest proportion of both incidence and mortality in all ages, followed by the category of other viral aetiologies and Mycoplasma spp for incidence, and S aureus and K pneumoniae for mortality. Between 2019 and 2021, during the COVID-19 pandemic, we estimated substantial declines in global influenza incidence and RSV incidence.
Although LRIs are ubiquitous across the world, the burden disproportionately falls on people living in poverty.39 In 2013, WHO and UNICEF formulated the Global Action Plan for the Prevention and Control of Pneumonia and Diarrhea (GAPPD), with the ambitious goal to end preventable childhood pneumonia and diarrhoea deaths by 2025.40 A specific target for 2025 is to reduce mortality from pneumonia in children younger than 5 years to fewer than 3 deaths per 1000 livebirths, roughly equivalent to a mortality rate of less than 60 deaths per 100 000 people per year among children younger than 5 years. As of 2021, we estimated a global LRI mortality rate of 76·2 deaths (61·7–92·9) per 100 000 children in this age group, and that 57 countries and territories, all but one of which were low-income and middle-income countries (LMICs), had a mortality rate over the global benchmark of 60 deaths per 100 000. To reduce mortality, the action plan calls for promotion of exclusive breastfeeding in infants younger than 6 months, reduction of indoor air pollution, expanded access to health care, and ongoing pneumonia case management in LMICs—approaches that have historically driven progress towards reducing LRI child mortality.41, 42
The WHO and UNICEF GAPPD also calls for increased coverage of pneumococcal conjugate vaccines (PCVs) and Hib vaccines. From 1990 to 2019, H influenzae showed the largest decline in global deaths, followed by S pneumoniae, both largely attributable to vaccination. Between 2000 and 2015, use of the Hib vaccine prevented an estimated 1·2 million deaths due to H influenzae infection globally, and PCV prevented an estimated 250 000 deaths due to pneumococcal infection.8 However, global coverage of these vaccines shows substantial room for improvement. According to WHO–UNICEF estimates of national immunisation coverage, global final-dose coverage of PCV among 1-year-olds was 60% and Hib coverage was 76% in 2022, both of which are above 2019 levels, suggesting recovery from pandemic immunisation disruptions.42, 43, 44 Although these global increases are promising, they can mask substantial inequities, and many vulnerable communities remain without access to vaccination.44, 45, 46 Strategies described by the WHO Immunization Agenda 2030 to increase coverage—including focusing on children who have not received any routine immunisations, building trust to avert vaccine hesitancy, and increasing vaccine access across the lifespan—can help reduce pneumonia mortality in areas with the highest burden.46, 47, 48, 49
The age groups of children younger than 5 years and adults aged 70 years and older had the highest LRI mortality rates in 1990. Time trends showed a steep decline in mortality in children younger than 5 years between 1990 and 2021, whereas no substantial decrease was observed in adults aged 70 years and older (figure 2). This trend holds true for the more granular age groups of 70–74 years and 75–79 years (appendix 2 p 4). Decline in immune function with ageing, called immunosenescence, promotes susceptibility to LRIs, as do age-related organ system changes and the development of comorbid conditions.50, 51 Influenza and pneumococcal vaccination remain effective tools to address LRIs in older adults.7 Pneumococcal immunisation of infant populations provides some herd protection for older adults.52, 53 In addition, pneumococcal vaccine administration to adults aged 65 years and older has been shown to be cost-effective54 with modest efficacy,55, 56, 57 at least in high-income settings. Because immunosenescence limits the efficacy of some vaccines in older adults, improved vaccine efficacy has emerged as a priority.51 Strategies towards more effective vaccines for older adults include higher doses of vaccines, repeated vaccinations, mucosal, subcutaneous, or intradermal administration, and use of more potent adjuvants.58 In LMICs, vaccine access for older adults is severely limited.59 More research is needed to assess the potential benefits of adult vaccination, understand barriers and challenges, and establish evidence-based guidelines in these settings.60, 61
RSV, the second-leading cause of LRI deaths in children younger than 5 years in 2019, has historically not been vaccine preventable. The development of affordable RSV vaccines and long-acting, affordable monoclonal antibodies (mAbs) was a priority for WHO's Vaccine Product and Delivery Research Unit and an active area of research.62, 63 These efforts came to fruition in 2023, when two vaccines for RSV were approved in the EU and the USA.64, 65, 66, 67 Both are for use in adults aged 60 years and older, and one is also approved for pregnant women to protect their infants. In addition, a new long-acting mAb injection, nirsevimab, was approved in 2022 in the EU and in 2023 in the USA to prevent RSV hospitalisation in both healthy and high-risk infants.68, 69 Generally, mAbs, including the long-approved, short-acting, RSV-preventive palivizumab, are too costly for use in most LMICs.70 The affordability of long-acting mAbs for LMICs is not yet known; preliminary cost-effectiveness analyses suggest a benefit, but this cost-effectiveness will depend on multiple factors, including pricing.62, 70, 71, 72 These long-acting mAbs and RSV vaccines, available for the first time, have the potential to avert unprecedented numbers of RSV cases and deaths in the 2023–24 respiratory infection season and beyond. A 2023 modelling study forecasts that with 60% vaccine coverage, in the USA alone, up to 2·0 million symptomatic RSV respiratory infections could be averted per year in adults older than 60 years, plus another 690 000 infections in the non-vaccinated population through indirect effects.73 However, these benefits will only reach locations where patients can access the vaccines. For the full global benefit of these preventives to be realised, equitable distribution is essential. It will be crucial for pharmaceutical companies, non-governmental organisations, and governments to work together to reduce barriers to access in LMICs.74
We have quantified the global burden of LRI attributable to S aureus in all ages and, for the first time in a comprehensive global study, we have identified the pathogen as the second-leading cause of LRI mortality after S pneumoniae in 2021. Although S aureus is a less frequent cause of LRI cases than S pneumoniae, it has a higher incidence of complications and a higher CFR. In a multisite US study, adult patients with S aureus LRI (n=37) had worse outcomes than those with S pneumoniae (n=115), including higher rates of intensive care unit (ICU) admission (62·2% vs 34·8%), mechanical ventilation (24·3% vs 12·2%), and inpatient mortality (10·8% vs 4·4%).13 Because of this poor prognosis, antistaphylococcal therapy is frequently included in empirical treatment for severe pneumonia.13, 75 Finding the causative pathogen in a patient with pneumonia can be challenging, and clinicians face the trade-off of balancing sufficiently broad empirical treatment with antibiotic stewardship.75, 76 In a global meta-analysis of S aureus pneumonia, 51% of isolates were meticillin-resistant S aureus (MRSA).77 The emergence of vancomycin-intermediate and vancomycin-resistant S aureus represents an escalating concern, and multidrug-resistant S aureus is classified as high-priority on the WHO global priority antimicrobial resistance pathogen list.78, 79 Antibiotic overuse, a key driver of resistance, remains an important concern across high-income countries and LMICs. Improved point-of-care diagnostics, including targeted PCR testing for MRSA, can prevent antibiotic overuse.80, 81, 82 In addition, although efforts to develop a vaccine against S aureus have so far been unsuccessful, ongoing research might generate a new method for prevention or treatment.83, 84
Our overall estimates of LRI mortality among children younger than 5 years are consistent with findings from a publication by WHO and the Maternal and Child Epidemiology Estimation Group, which estimated 740 000 (95% UI 620 000–840 000) child LRI deaths in 2019.85 We estimated 693 000 (580 000–822 000) child LRI deaths in 2019. Our estimates of pathogen distribution are also similar to other global reports. A 2016 study from the Global Initiative for MRSA Pneumonia (GLIMP),77 which included data across 54 countries, identified S aureus in 188 (6%) of 3193 adults with community-acquired pneumonia, in alignment with the current study. Likewise, a 2021 meta-analysis across eight countries estimated that 18% (95% CI 13–24) of community-acquired pneumonia cases in adults aged 50 years and older were attributable to S pneumoniae.86 Our estimates for the 50–69 years and 70 years and older global age groups are within the 95% CI of this meta-analysis.
In addition, we have estimated the COVID-19 pandemic-era reduction in influenza and RSV mortality and incidence by country, applied to a comprehensive set of global LRI estimates. From 2019 to 2021, we estimated a 71·8% (95% UI 63·8–78·9) decrease in influenza deaths and a 66·7% (56·6–75·3) decrease in RSV deaths worldwide (appendix 2 p 1951). These reductions were observed following the implementation of non-pharmaceutical interventions such as facemask use and mobility restriction, which have been implicated in the reduction of transmission of respiratory viruses, including influenza and RSV, in 2020 and 2021.22, 87, 88, 89, 90 However, other respiratory viruses, such as rhinovirus, adenovirus, and respiratory enteroviruses, quickly rebounded within a few months and persisted despite non-pharmaceutical interventions, showing fewer fluctuations in case counts with changing policies compared with influenza and RSV.22 Overall, hospitals across the world have reported reductions in admissions for community-acquired pneumonia during the COVID-19 pandemic.91, 92, 93
This study has several limitations. First, we quantified the COVID-19 pandemic-attributable reduction in LRI for influenza and RSV only. New evidence from a global surveillance network including 26 countries shows a decline in incidence of invasive infections attributable to respiratory pathogens, including S pneumoniae and H influenzae, during the COVID-19 pandemic.94 The decline in pneumococcal disease incidence might be primarily attributable to the decline in transmission of co-infecting respiratory viruses, including influenza and RSV, rather than reduced transmissibility or serotype selection of S pneumoniae itself.95 For the bacterial aetiologies that are predominantly health-care acquired, evidence is mostly limited to single-site studies and mixed, with some studies showing a reduction,96, 97 others showing an increase,91 and others showing no change.98 In the post-pandemic period, studies suggest that several of the pathogens that decreased in 2020 rebounded, including RSV, influenza, and pneumococcus.99, 100, 101, 102 Other pathogens—namely, Mycoplasma spp—showed a decline that persisted for a longer duration after the COVID-19 pandemic, with continued decreased detection observed until the end of 2022, followed by a delayed re-emergence in some countries in mid-2023.103, 104, 105 Due to interruption of established data exchanges caused by the COVID-19 pandemic, we were unable to estimate how bacterial pathogen distributions might have changed between 2019 and 2021. As data become available for more locations, pathogens, and years, we can comprehensively quantify the indirect effects of the pandemic on the incidence of LRI and its aetiologies in future rounds of GBD.
A second limitation is that, when estimating the effect of the COVID-19 pandemic on influenza and RSV incidence, we relied exclusively on case notification data from national and multinational surveillance networks. Our method cannot separate the effects of a true decrease in LRI incidence from the effects of a decrease in health-care-seeking behaviour; we also did not account for potential changes in reporting capability over time. Third, to calculate the reduction in RSV, we applied modelled estimates of COVID-19 pandemic-associated influenza reduction directly to RSV estimates. This decision was based on a meta-analysis of the ratio of the percentage change in influenza to the percentage change in RSV in 2020, relative to the pre-pandemic period, which showed no statistically significant difference in the reduction of the two pathogens. However, empirical studies published since the pandemic have shown that the resurgence patterns of RSV and influenza have differed.106, 107, 108, 109, 110 Fourth, limited data availability and quality are constraints, particularly in low-income countries, where the LRI burden is highest. Our assessment of LRI mortality in countries lacking vital registration data relies largely on verbal autopsy studies, which have modest sensitivity in accurately identifying deaths due to LRIs.111 Covariates and regional trends were leveraged to predict the burden of LRI and corresponding aetiologies for locations with few or no data. In selecting these covariates, some degree of model misspecification is possible due to potential omitted variables that are not captured in the dataset, which could affect the accuracy of our predictive model. Fifth, misclassification might be present in pathogen proportion data if certain pathogens are more difficult to detect than others, or if some pathogens, such as viruses in the population of older adults, are irregularly tested in a laboratory or clinical setting. Sixth, although we used a crosswalking process to adjust for systematic differences in incidence data source categories, this process might not fully account for all forms of bias. Finally, we directly applied LRI aetiology proportions from the Global Burden of AMR study to GBD estimates of LRI cases and deaths, although the two studies use slightly different definitions of LRI. In particular, the Global Burden of AMR study's definition of LRI deaths covers any event for which LRI was present in the causal chain, regardless of the underlying cause of death, whereas the GBD definition only includes instances in which LRI was the underlying cause of death.
In summary, we have shown that, despite declines in incidence during the COVID-19 pandemic, LRIs remain a significant cause of morbidity and mortality worldwide. Increased access to existing vaccines, as well as rollout of novel vaccines and therapies, could reduce the burden of LRIs. Supporting research for low-cost interventions against S aureus could accelerate progress in reducing LRI-related mortality and incidence, especially in resource-constrained settings. In addition, the growing threat of antimicrobial resistance highlights the importance of antibiotic stewardship and investment in improved diagnostic technologies to improve the specificity and accuracy of therapy. Finally, all these interventions must come at an affordable cost, so that they can reduce inequities seen in LRI mortality, rather than exacerbate them.
Data sharing
To download the data used in these analyses, please visit the GHDx GBD 2021 website.
Declaration of interests
J A Berkley reports support for the present manuscript from research grants from the Bill & Melinda Gates Foundation, Wellcome Trust, the National Institute for Health and Care Research (NIHR), and the Medical Research Council (MRC). C Brown reports other financial support from an ad-hoc one-off market research advisory role (anonymously conducted via market research companies with no direct communication, none specifically related to lower respiratory tract infections), all outside the submitted work. K Krishan reports other non-financial support from the UGC Centre of Advanced Study, CAS II, awarded to the Department of Anthropology, Panjab University (Chandigarh, India) outside the submitted work. M-C Li reports support for the present manuscript from the National Science and Technology Council in Taiwan (112-2410-H-003-031) and other financial or non-financial support as a Technical Editor of the Journal of the American Heart Association, Review Editor of Frontiers in Public Health, and Editorial Board Member of BMC Public Health, outside the submitted work. S A Meo reports grants or contracts from King Saud University (Riyadh, Saudi Arabia; RSP-2024 R47), outside the submitted work. L Monasta reports support for the present manuscript from the Italian Ministry of Health (Ricerca Corrente 34/2017), with payments made to the Institute for Maternal and Child Health IRCCS Burlo Garofolo. C Moore reports participation with Dr Gwen Knight as a member of the advisory board for MRC grants (no payments made), with the WHO Advisory group, and with the REVIVE Advisory group as a member of the steering group; and leadership or fiduciary roles in board, society, committee, or advocacy groups (unpaid) as the co-chair of the Impact and Influence Group of the Microbiology Society, outside the submitted work. A Pollard reports grants or contracts from the Bill & Melinda Gates Foundation, Wellcome Trust, Cepi, MRC, NIHR, AstraZeneca, European Commission, and the Serum Institute of India; royalties or licenses from AstraZeneca; consulting fees from Shionogi; leadership or fiduciary roles in board, society, committee, or advocacy groups (unpaid) as the chair of the Department of Health and Social Care's Joint Committee on Vaccination and Immunisation and as a member of the WHO Strategic Advisory Group of Experts on Immunization until 2022; and receipt of equipment, materials, drugs, medical writing, gifts, or other services from Moderna, outside the submitted work. L F Reyes reports grants or contracts from MSD and Pfizer; consulting fees from GlaxoSmithKline, MSD, and Pfizer; payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing, or educational events from GlaxoSmithKline, MSD, and Pfizer; payment for expert testimony from GlaxoSmithKline, MSD, and Pfizer; and support for attending meetings or travel from GlaxoSmithKline and Pfizer, outside the submitted work. Y L Samodra reports grants or contracts from Taipei Medical University, and leadership or fiduciary roles in board, society, committee, or advocacy groups (paid or unpaid) as the co-founder of Benang Merah Research Center, outside the submitted work. E A F Simôes reports support for the present manuscript from the Bill & Melinda Gates Foundation; grants or contracts from AstraZeneca, Merck & Co, Pfizer, and Icosavax; consulting fees from Merck & Co, Pfizer, GlaxoSmithKline, Sanofi Pasteur, Cidara Therapeutics, Adagio Therapeutics, Nuance Pharmaceuticals, Enanta, and Icosavax; payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing, or educational events from Pfizer and AstraZeneca; support for attending meetings or travel from Pfizer and AstraZeneca; and participation on a data safety monitoring board or advisory board with AbbVie, GlaxoSmithKline, the Bill & Melinda Gates Foundation, and Moderna, outside the submitted work. M Zielińska reports other financial support as an AstraZeneca employee, outside the submitted work.
Acknowledgments
Acknowledgments
This study was funded by the Bill & Melinda Gates Foundation, Wellcome Trust, and Department of Health and Social Care using UK aid funding managed by the Fleming Fund.
Editorial note: The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
GBD 2021 Lower Respiratory Infections and Antimicrobial Resistance Collaborators
Rose Grace Bender*, Sarah Brooke Sirota, Lucien R Swetschinski, Regina-Mae Villanueva Dominguez, Amanda Novotney, Eve E Wool, Kevin S Ikuta, Avina Vongpradith, Emma Lynn Best Rogowski, Matthew Doxey, Christopher E Troeger, Samuel B Albertson, Jianing Ma, Jiawei He, Kelsey Lynn Maass, Eric A F Simões, Meriem Abdoun, Jeza Muhamad Abdul Aziz, Deldar Morad Abdulah, Samir Abu Rumeileh, Hasan Abualruz, Salahdein Aburuz, Abiola Victor Adepoju, Rishan Adha, Wirawan Adikusuma, Saryia Adra, Ali Afraz, Shahin Aghamiri, Antonella Agodi, Amir Mahmoud Ahmadzade, Haroon Ahmed, Ayman Ahmed, Karolina Akinosoglou, Tareq Mohammed Ali AL-Ahdal, Rasmieh Mustafa Al-amer, Mohammed Albashtawy, Mohammad T AlBataineh, Hediyeh Alemi, Adel Ali Saeed Al-Gheethi, Abid Ali, Syed Shujait Shujait Ali, Jaber S Alqahtani, Mohammad AlQudah, Jaffar A Al-Tawfiq, Yaser Mohammed Al-Worafi, Karem H Alzoubi, Reza Amani, Prince M Amegbor, Edward Kwabena Ameyaw, John H Amuasi, Abhishek Anil, Philip Emeka Anyanwu, Mosab Arafat, Damelash Areda, Reza Arefnezhad, Kendalem Asmare Atalell, Firayad Ayele, Ahmed Y Azzam, Hassan Babamohamadi, François-Xavier Babin, Yogesh Bahurupi, Stephen Baker, Biswajit Banik, Martina Barchitta, Hiba Jawdat Barqawi, Zarrin Basharat, Pritish Baskaran, Kavita Batra, Ravi Batra, Nebiyou Simegnew Bayileyegn, Apostolos Beloukas, James A Berkley, Kebede A Beyene, Ashish Bhargava, Priyadarshini Bhattacharjee, Julia A Bielicki, Mariah Malak Bilalaga, Veera R Bitra, Colin Stewart Brown, Katrin Burkart, Yasser Bustanji, Sinclair Carr, Yaacoub Chahine, Vijay Kumar Chattu, Fatemeh Chichagi, Hitesh Chopra, Isaac Sunday Chukwu, Eunice Chung, Sriharsha Dadana, Xiaochen Dai, Lalit Dandona, Rakhi Dandona, Isaac Darban, Nihar Ranjan Dash, Mohsen Dashti, Mohadese Dashtkoohi, Denise Myriam Dekker, Ivan Delgado-Enciso, Vinoth Gnana Chellaiyan Devanbu, Kuldeep Dhama, Nancy Diao, Thao Huynh Phuong Do, Klara Georgieva Dokova, Christiane Dolecek, Arkadiusz Marian Dziedzic, Tim Eckmanns, Abdelaziz Ed-Dra, Ferry Efendi, Aziz Eftekharimehrabad, David William Eyre, Ayesha Fahim, Alireza Feizkhah, Timothy William Felton, Nuno Ferreira, Luisa S Flor, Santosh Gaihre, Miglas W Gebregergis, Mesfin Gebrehiwot, Christine Geffers, Urge Gerema, Kazem Ghaffari, Mohamad Goldust, Pouya Goleij, Shi-Yang Guan, Mesay Dechasa Gudeta, Cui Guo, Veer Bala Gupta, Ishita Gupta, Farrokh Habibzadeh, Najah R Hadi, Emily Haeuser, Wase Benti Hailu, Ramtin Hajibeygi, Arvin Haj-Mirzaian, Sebastian Haller, Mohammad Hamiduzzaman, Nasrin Hanifi, Jan Hansel, Md Saquib Hasnain, Johannes Haubold, Nguyen Quoc Hoan, Hong-Han Huynh, Kenneth Chukwuemeka Iregbu, Md Rabiul Islam, Abdollah Jafarzadeh, Ammar Abdulrahman Jairoun, Mahsa Jalili, Nabi Jomehzadeh, Charity Ehimwenma Joshua, Md Awal Kabir, Zul Kamal, Kehinde Kazeem Kanmodi, Rami S Kantar, Arman Karimi Behnagh, Navjot Kaur, Harkiran Kaur, Faham Khamesipour, M Nuruzzaman Khan, Mahammed Ziauddin Khan Suheb, Vishnu Khanal, Khaled Khatab, Mahalaqua Nazli Khatib, Grace Kim, Kwanghyun Kim, Aiggan Tamene Tamene Kitila, Somayeh Komaki, Kewal Krishan, Ralf Krumkamp, Md Abdul Kuddus, Maria Dyah Kurniasari, Chandrakant Lahariya, Kaveh Latifinaibin, Nhi Huu Hanh Le, Thao Thi Thu Le, Trang Diep Thanh Le, Seung Won Lee, Alain Lepape, Temesgen L Lerango, Ming-Chieh Li, Amir Ali Mahboobipour, Kashish Malhotra, Tauqeer Hussain Mallhi, Anand Manoharan, Bernardo Alfonso Martinez-Guerra, Alexander G Mathioudakis, Rita Mattiello, Jürgen May, Barney McManigal, Steven M McPhail, Tesfahun Mekene Meto, Max Alberto Mendez Mendez-Lopez, Sultan Ayoub Meo, Mohsen Merati, Tomislav Mestrovic, Laurette Mhlanga, Le Huu Nhat Minh, Awoke Misganaw, Vinaytosh Mishra, Arup Kumar Misra, Nouh Saad Mohamed, Esmaeil Mohammadi, Mesud Mohammed, Mustapha Mohammed, Ali H Mokdad, Lorenzo Monasta, Catrin E Moore, Rohith Motappa, Vincent Mougin, Parsa Mousavi, Francesk Mulita, Atsedemariam Andualem Mulu, Pirouz Naghavi, Ganesh R Naik, Firzan Nainu, Tapas Sadasivan Nair, Shumaila Nargus, Mohammad Negaresh, Hau Thi Hien Nguyen, Dang H Nguyen, Van Thanh Nguyen, Taxiarchis Konstantinos Nikolouzakis, Efaq Ali Noman, Chisom Adaobi Nri-Ezedi, Ismail A Odetokun, Patrick Godwin Okwute, Matifan Dereje Olana, Titilope O Olanipekun, Omotola O Olasupo, Antonio Olivas-Martinez, Michal Ordak, Edgar Ortiz-Brizuela, Amel Ouyahia, Jagadish Rao Padubidri, Anton Pak, Anamika Pandey, Ioannis Pantazopoulos, Pragyan Paramita Parija, Romil R Parikh, Seoyeon Park, Ashwaghosha Parthasarathi, Ava Pashaei, Prince Peprah, Hoang Tran Pham, Dimitri Poddighe, Andrew Pollard, Alfredo Ponce-De-Leon, Peralam Yegneswaran Prakash, Elton Junio Sady Prates, Nguyen Khoi Quan, Pourya Raee, Fakher Rahim, Mosiur Rahman, Masoud Rahmati, Shakthi Kumaran Ramasamy, Shubham Ranjan, Indu Ramachandra Rao, Ahmed Mustafa Rashid, Sayaphet Rattanavong, Nakul Ravikumar, Murali Mohan Rama Krishna Reddy, Elrashdy Moustafa Mohamed Redwan, Robert C Reiner Jr, Luis Felipe Reyes, Tamalee Roberts, Mónica Rodrigues, Victor Daniel Rosenthal, Priyanka Roy, Tilleye Runghien, Umar Saeed, Amene Saghazadeh, Narjes Saheb Sharif-Askari, Fatemeh Saheb Sharif-Askari, Soumya Swaroop Sahoo, Monalisha Sahu, Joseph W Sakshaug, Afeez Abolarinwa Salami, Mohamed A Saleh, Hossein Salehi omran, Malik Sallam, Sara Samadzadeh, Yoseph Leonardo Samodra, Rama Krishna Sanjeev, Made Ary Sarasmita, Aswini Saravanan, Benn Sartorius, Jennifer Saulam, Austin E Schumacher, Seyed Arsalan Seyedi, Mahan Shafie, Samiah Shahid, Sunder Sham, Muhammad Aaqib Shamim, Mohammad Ali Shamshirgaran, Rajesh P Shastry, Samendra P Sherchan, Desalegn Shiferaw, Aminu Shittu, Emmanuel Edwar Siddig, Robert Sinto, Aayushi Sood, Reed J D Sorensen, Andy Stergachis, Temenuga Zhekova Stoeva, Chandan Kumar Swain, Lukasz Szarpak, Jacques Lukenze Tamuzi, Mohamad-Hani Temsah, Melkamu B Tessema Tessema, Pugazhenthan Thangaraju, Nghia Minh Tran, Ngoc-Ha Tran, Munkhtuya Tumurkhuu, Sree Sudha Ty, Aniefiok John Udoakang, Inam Ulhaq, Tungki Pratama Umar, Abdurezak Adem Umer, Seyed Mohammad Vahabi, Asokan Govindaraj Vaithinathan, Jef Van den Eynde, Judd L Walson, Muhammad Waqas, Yuhan Xing, Mukesh Kumar Yadav, Galal Yahya, Dong Keon Yon, Abed Zahedi Bialvaei, Fathiah Zakham, Abyalew Mamuye Zeleke, Chunxia Zhai, Zhaofeng Zhang, Haijun Zhang, Magdalena Zielińska, Peng Zheng, Aleksandr Y Aravkin, Theo Vos, Simon I Hay, Jonathan F Mosser, Stephen S Lim, Mohsen Naghavi†, Christopher J L Murray†, Hmwe Hmwe Kyu†. *First author. †Co-senior authors.
Affiliations
Institute for Health Metrics and Evaluation (R G Bender MSc, S B Sirota MA, L R Swetschinski MSc, R-M V Dominguez BS, A Novotney MPH, E E Wool MPH, K S Ikuta MD, A Vongpradith BA, E L B Rogowski MPH, C E Troeger MPH, S B Albertson BS, J He MSW, K L Maass PhD, K Burkart PhD, S Carr BSc, E Chung MSc, X Dai PhD, Prof L Dandona MD, Prof R Dandona PhD, L S Flor MPH, E Haeuser PhD, T Mestrovic PhD, A H Mokdad PhD, V Mougin BA, R C Reiner Jr PhD, A E Schumacher PhD, R J D Sorensen PhD, P Zheng PhD, A Y Aravkin PhD, Prof T Vos PhD, Prof S I Hay FMedSci, J F Mosser MD, Prof S S Lim PhD, Prof M Naghavi PhD, Prof C J L Murray DPhil, H H Kyu PhD), Department of Health Metrics Sciences, School of Medicine (K Burkart PhD, X Dai PhD, L S Flor MPH, A Misganaw PhD, A H Mokdad PhD, R C Reiner Jr PhD, Prof A Stergachis PhD, P Zheng PhD, Prof T Vos PhD, Prof S I Hay FMedSci, Prof S S Lim PhD, Prof M Naghavi PhD, Prof C J L Murray DPhil, H H Kyu PhD, Prof R Dandona PhD, B Sartorius PhD, A Y Aravkin PhD), Department of Internal Medicine (Y Chahine MD), Department of Cardiology (Y Chahine MD), Department of Biostatistics (A Olivas-Martinez MD), Department of Global Health (R J D Sorensen PhD, Prof J L Walson MD), Department of Pharmacy (Prof A Stergachis PhD), Department of Applied Mathematics (A Y Aravkin PhD), University of Washington, Seattle, WA, USA; School of Medicine (R G Bender MSc), Department of Dermatology (M Goldust MD), Yale University, New Haven, CT, USA; Division of Infectious Diseases (K S Ikuta MD), Veterans Affairs Greater Los Angeles, Los Angeles, CA, USA; School of Medicine (E L B Rogowski MPH), Emory University, Atlanta, GA, USA; Urban Indian Health Institute (M Doxey MPH), Seattle Indian Health Board, Seattle, WA, USA; Center for Biostatistics (J Ma MS), Ohio State University, Columbus, OH, USA; Center for Global Health (Prof E A F Simões MD), University of Colorado, Denver, CO, USA; Department of Medicine (Prof M Abdoun BMedSc), University of Setif Algeria, Sétif, Algeria; Department of Medical Laboratory of Science (J M Abdul Aziz MSc), University of Human Development, Sulaymaniyah, Iraq; Baxshin Hospital (J M Abdul Aziz MSc), Baxshin Research Center, Sulaymaniyah, Iraq; Community and Maternity Nursing Unit (D M Abdulah MPH), University of Duhok, Duhok, Iraq; Department of Neurology (S Abu Rumeileh MD), Martin Luther University Halle-Wittenberg, Halle, Germany; Department of Nursing (H Abualruz PhD), Al Zaytoonah University of Jordan, Amman, Jordan; Department of Therapeutics (Prof S Aburuz PhD), United Arab Emirates University, Al Ain, United Arab Emirates; College of Pharmacy (Prof S Aburuz PhD) and Department of Biopharmaceutics and Clinical Pharmacy (Y Bustanji PhD), University of Jordan, Amman, Jordan; HIV and Infectious Diseases Department (A V Adepoju MD), Jhpiego, Abuja, Nigeria; Department of Adolescent Research and Care (A V Adepoju MD), Adolescent Friendly Research Initiative and Care, Ado Ekiti, Nigeria; Department of Business Administration (R Adha PhD), Department of Pharmacy (W Adikusuma PhD), Muhammadiyah University of Mataram, Mataram, Indonesia; Clinical Sciences Department (S Adra MD, H J Barqawi MPhil, N R Dash MD, N Saheb Sharif-Askari PhD), Department of Pharmacy Practice and Pharmacotherapeutics (Prof K H Alzoubi PhD), Department of Clinical Sciences (M Bilalaga MBBS), Department of Basic Biomedical Sciences (Y Bustanji PhD), Sharjah Institute of Medical Sciences (F Saheb Sharif-Askari PhD), College of Medicine (M A Saleh PhD), University of Sharjah, Sharjah, United Arab Emirates; Department of Medical Information Sciences (A Afraz MSc), Department of Immunology (Prof A Jafarzadeh PhD), Research Center for Hydatid Disease (F Khamesipour PhD), Kerman University of Medical Sciences, Kerman, Iran; Department of Biotechnology (S Aghamiri PhD), Obesity Research Center (A Haj-Mirzaian MD), Tracheal Diseases Research Center (A Mahboobipour MD), Department of Biology and Anatomical Sciences (P Raee PhD), Urology and Nephrology Research Center (H Salehi omran MD), Shahid Beheshti University of Medical Sciences, Tehran, Iran; Department of Medical and Surgical Sciences and Advanced Technologies “GF Ingrassia” (Prof A Agodi PhD, M Barchitta PhD), University of Catania, Catania, Italy; Department of Neuroscience (A Ahmadzade MD), Mashhad University of Medical Sciences, Mashhad, Iran; Department of Biosciences (H Ahmed PhD), COMSATS Institute of Information Technology, Islamabad, Pakistan; Institute of Endemic Diseases (A Ahmed MSc), Unit of Basic Medical Sciences (E E Siddig MD), University of Khartoum, Khartoum, Sudan; Swiss Tropical and Public Health Institute (A Ahmed MSc), Department of Paediatric Infectious Diseases (J A Bielicki PhD), University of Basel, Basel, Switzerland; Department of Internal Medicine (K Akinosoglou PhD), University of Patras, Patras, Greece; Department of Internal Medicine and Infectious Diseases (K Akinosoglou PhD), University General Hospital of Patras, Patras, Greece; Heidelberg Institute of Global Health (HIGH) (T M A AL-Ahdal MPH), Heidelberg University, Heidelberg, Germany; School of Nursing (R M Al-amer PhD), Yarmouk University, Irbid, Jordan; School of Nursing and Midwifery (R M Al-amer PhD), Department of Engineering (G R Naik PhD), Western Sydney University, Sydney, NSW, Australia; Community and Mental Health Department (Prof M Albashtawy PhD), Al al-Bayt University, Mafraq, Jordan; Department of Molecular Biology and Genetics (Prof M T AlBataineh PhD), Khalifa University, Abu Dhabi, United Arab Emirates; Hematology, Oncology and Stem Cell Transplantation Research Center (H Alemi MD), Department of Scientific Research (F Chichagi MD), Department of Obstetrics and Gynecology (M Dashtkoohi MD), Department of Radiology (R Hajibeygi MD), Center for Research and Training in Skin Diseases and Leprosy (F Khamesipour PhD), School of Medicine (M Merati MD), Faculty of Medicine (E Mohammadi MD, S Vahabi MD), Non-communicable Diseases Research Center (P Mousavi MD), Research Center for Immunodeficiencies (A Saghazadeh MD), Endocrinology and Metabolism Research Institute (S Seyedi MD), Department of Neurology (M Shafie MD), Tehran University of Medical Sciences, Tehran, Iran (E Mohammadi MD); Global Centre for Environmental Remediation (A A S Al-Gheethi PhD), University of Newcastle, Newcastle, NSW, Australia; Cooperative Research Centre for Contamination Assessment and Remediation of the Environment, Newcastle, NSW, Australia (A A S Al-Gheethi PhD); Department of Zoology (A Ali PhD), Abdul Wali Khan University Mardan, Mardan, Pakistan; Center for Biotechnology and Microbiology (S S Ali PhD), University of Swat, Swat, Pakistan; Department of Respiratory Care (J S Alqahtani PhD), Prince Sultan Military College of Health Sciences, Dammam, Saudi Arabia; Department of Pathology and Microbiology (M AlQudah MD), Department of Clinical Pharmacy (Prof K H Alzoubi PhD), Jordan University of Science and Technology, Irbid, Jordan; Cell Therapy and Applied Genomics Department (M AlQudah MD), King Hussein Cancer Center, Amman, Jordan; Department of Specialty Internal Medicine (Prof J A Al-Tawfiq MD), Johns Hopkins Aramco Healthcare, Dhahran, Saudi Arabia; Medicine Department (Prof J A Al-Tawfiq MD), Indiana University School of Medicine, Indianapolis, IN, USA; Department of Medical Sciences (Prof Y M Al-Worafi PhD), Azal University for Human Development, Sana'a, Yemen; Department of Clinical Sciences (Prof Y M Al-Worafi PhD), University of Science and Technology of Fujairah, Fujairah, United Arab Emirates; Interdisciplinary Graduate Program in Human Toxicology (R Amani DVM), University of Iowa, Iowa City, IA, USA; Health Policy Research Center (R Amani DVM), Department of Anatomy (R Arefnezhad MSc), Shiraz University of Medical Sciences, Shiraz, Iran; School of Global Public Health (P M Amegbor PhD), New York University, New York, NY, USA; School of Graduate Studies (E K Ameyaw MPhil), Lingnan University, Hong Kong Special Administrative Region, China; Department of Global Health (J H Amuasi PhD), Kwame Nkrumah University of Science and Technology, Kumasi, Ghana; Global Health and Infectious Diseases (J H Amuasi PhD), Kumasi Center for Collaborative Research in Tropical Medicine, Kumasi, Ghana; Department of Pharmacology (A Anil MD, M Shamim MBBS), Department of Community Medicine and Family Medicine (P Baskaran MD), Department of Pharmacology and Research (A Saravanan MD), All India Institute of Medical Sciences, Jodhpur, India; All India Institute of Medical Sciences, Bhubaneswar, India (A Anil MD); Warwick Medical School (P E Anyanwu PhD), University of Warwick, Coventry, UK (J W Sakshaug PhD); College of Pharmacy (M Arafat PhD), Al Ain University, Abu Dhabi, United Arab Emirates; College of Art and Science (D Areda PhD), Ottawa University, Surprise, AZ, USA; School of Life Sciences (D Areda PhD), Arizona State University, Tempe, AZ, USA; Department of Pediatrics and Child Health Nursing (K A Atalell MSc), University of Gondar, Gondar, Ethiopia; School of Medical Laboratory Sciences (F Ayele MSc), Department of Clinical Pharmacy (M D Gudeta MSc), Haramaya University, Harar, Ethiopia; Department of Neurovascular Research (A Y Azzam MBBCh), Nested Knowledge, Saint Paul, MN, USA; Faculty of Medicine (A Y Azzam MBBCh), October 6 University, 6th of October City, Egypt; Department of Nursing (H Babamohamadi PhD), Semnan University of Medical Sciences and Health Services, Semnan, Iran; Mérieux Foundation, Lyon, France (F Babin PharmD); Department of Community Medicine and Family Medicine (Y Bahurupi MD), All India Institute of Medical Sciences, Rishikesh, India; Department of Medicine (Prof S Baker PhD), Department of Clinical Medicine (P Bhattacharjee MD), University of Cambridge, Cambridge, UK; Institute of Health and Wellbeing (IHW) (B Banik PhD), Federation University Australia, Melbourne, VIC, Australia; Manna Institute (B Banik PhD), University of New England, Armidale, NSW, Australia; Alpha Genomics, Islamabad, Pakistan (Z Basharat PhD); Department of Medical Education (K Batra PhD), School of Public Health (R Batra MS), University of Nevada Las Vegas, Las Vegas, NV, USA; IT Department (R Batra MS), Coforge, Georgia, GA, USA; Department of Surgery (N S Bayileyegn MD), Department of Public Health (U Gerema MSc), Department of Epidemiology (D Shiferaw MPH), Jimma University, Jimma, Ethiopia; Department of Biomedical Sciences (Prof A Beloukas PhD), University of West Attica, Athens, Greece; Institute of Infection and Global Health (Prof A Beloukas PhD), University of Liverpool, Liverpool, UK; Clinical Research Department (Prof J A Berkley PhD), Kenya Medical Research Institute/Wellcome Trust Research Programme, Kilifi, Kenya; Centre for Tropical Medicine and Global Health (Prof J A Berkley PhD, T Roberts PhD) and Nuffield Department of Medicine (T Runghien MSc), Oxford University, Oxford, UK; School of Pharmacy (K A Beyene PhD), University of Auckland, Auckland, New Zealand; Department of Pharmaceutical and Administrative Sciences (K A Beyene PhD), University of Health Sciences and Pharmacy in St Louis, St Louis, MO, USA; Department of Internal Medicine (A Bhargava MD), Wayne State University, Detroit, MI, USA; Department of Clinical Medicine (P Bhattacharjee MD), Cambridge University Hospitals NHS Foundation Trust, Cambridge, UK; Department of Infection and Immunity (J A Bielicki PhD), St George's University of London, London, UK; Faculty of Health Sciences (V R Bitra PhD), University of Botswana, Gaborone, Botswana; Faculty of Medicine (Prof A Ouyahia PhD), University Ferhat Abbas of Setif, Setif, Algeria; HCAI, Fungal, AMR, AMU and Sepsis Division (C S Brown MD), United Kingdom Health Security Agency, London, UK; Department of Infection (C S Brown MD), Imperial College London, London, UK; Temerty Faculty of Medicine (V Chattu MD), University of Toronto, Toronto, ON, Canada; Department of Community Medicine (V Chattu MD), Datta Meghe Institute of Medical Sciences, Sawangi, India; Department of Biosciences (H Chopra PhD), Saveetha Institute of Medical and Technical Sciences, Chennai, India; Department of Paediatric Surgery (I S Chukwu BMedSc), Federal Medical Centre, Umuahia, Nigeria; Department of Internal Medicine (S Dadana MD), Cheyenne Regional Medical Center, Cheyenne, WY, USA; Public Health Foundation of India (Prof L Dandona MD, Prof R Dandona PhD, A Pandey PhD), Gurugram, India; Indian Council of Medical Research (Prof L Dandona MD), New Delhi, India; Department of Medical Microbiology (I Darban BSc), University of Ghana, Accra, Ghana; Department of Radiology (M Dashti MD), Tabriz University of Medical Sciences, Tabriz, Iran; Department of Gynecology and Obstetrics (M Dashtkoohi MD), Vali-E-Asr Reproductive Health Research Center, Family Health Research Institute, Tehran, Iran; Department Implementation Research (D M Dekker PhD), Institute of Tropical Medicine, Hamburg, Germany; School of Medicine (I Delgado-Enciso DSc), University of Colima, Colima, Mexico; Department of Research (I Delgado-Enciso DSc), Colima State Health Services, Colima, Mexico; Department of Community Medicine (V G C Devanbu MD), Chettinad Academy of Research and Education, Chennai, India; Division of Pathology (K Dhama PhD), ICAR-Indian Veterinary Research Institute, Bareilly, India; Department of Environmental Health (N Diao DSc), Department of Pulmonary and Critical Care (T O Olanipekun MD), Harvard University, Boston, MA, USA; Department of Medicine (T H Do MD), Can Tho University of Medicine and Pharmacy, Can Tho, Viet Nam; Department of Social Medicine and Health Care Organisation (K G Dokova PhD), Medical University “Prof Dr Paraskev Stoyanov”, Varna, Bulgaria; Oxford Centre for Global Health Research (C Dolecek PhD), Nuffield Department of Population Health (Prof D W Eyre DPhil), Big Data Institute, Nuffield Department of Medicine (B McManigal PhD), Oxford Vaccine Group (A Pollard FMedSci), Department of Pediatrics (A Pollard FMedSci), Nuffield Department of Medicine (B Sartorius PhD), University of Oxford, Oxford, UK; Mahidol Oxford Tropical Medicine Research Unit (C Dolecek PhD), Mahidol University, Bangkok, Thailand; Department of Conservative Dentistry with Endodontics (A M Dziedzic DSc), Medical University of Silesia, Katowice, Poland; Department of Infectious Disease Epidemiology (S Haller MD), Robert Koch Institute, Berlin, Germany (T Eckmanns MD); Higher School of Technology (Prof A Ed-Dra PhD), Sultan Moulay Slimane University, Beni Mellal, Morocco; Advanced Nursing Department (F Efendi PhD), Universitas Airlangga, Surabaya, Indonesia; Department of Biochemistry (A Eftekharimehrabad PhD), Ege University, Izmir, Türkiye; Azerbaijan State University of Economics (UNEC), Baku, Azerbaijan (A Eftekharimehrabad PhD); Department of Oral Biology (A Fahim PhD), University Institute of Public Health (S Nargus PhD, S Nargus PhD), Institute of Molecular Biology and Biotechnology (IMBB) (S Shahid PhD), Research Centre for Health Sciences (RCHS) (S Shahid PhD), The University of Lahore, Lahore, Pakistan; Department of Social Medicine and Epidemiology (A Feizkhah MD), Guilan University of Medical Sciences, Rasht, Iran; Division of Immunology, Immunity to Infection & Respiratory Medicine (T W Felton PhD, J Hansel MSc, A G Mathioudakis PhD), University of Manchester, Manchester, UK; Department of Social Sciences (Prof N Ferreira PhD), University of Nicosia, Nicosia, Cyprus; Institute of Applied Health Sciences (S Gaihre PhD), University of Aberdeen, Aberdeen, UK; Department of Midwifery (M W Gebregergis MSc), Adigrat University, Adigrat, Ethiopia; Department of Environmental Health (M Gebrehiwot DSc), Wollo University, Dessie, Ethiopia; Institute for Hygiene and Environmental Medicine (Prof C Geffers PhD), Department of Neurology (S Samadzadeh MD), Charité University Medical Center Berlin, Berlin, Germany; Department of Laboratory Sciences (K Ghaffari MSc), Khomein University of Medical Sciences, Khomein, Iran; Department of Genetics (P Goleij MSc), Sana Institute of Higher Education, Sari, Iran; Universal Scientific Education and Research Network (USERN) (P Goleij MSc), Kermanshah University of Medical Sciences, Kermanshah, Iran; Department of Epidemiology and Biostatistics (S Guan MD), Anhui Medicla University, Hefei, China; Department of Urban Planning and Design (C Guo PhD), University of Hong Kong, Hong Kong Special Administrative Region, China; School of Medicine (V Gupta PhD), Deakin University, Geelong, VIC, Australia; Department of Internal Medicine (I Gupta MD), Independent Consultant, Bharatpur, India; NGO (I Gupta MD), Independent Consultant, Delhi, India; Global Virus Network, Middle East Region, Shiraz, Iran (F Habibzadeh MD); Department of Clinical Pharmacology and Medicine (Prof N R Hadi PhD), University of Kufa, Najaf, Iraq; Department of Public Health (W B Hailu MPH), Wollega University, Nekemte, Ethiopia; Department of Radiology (A Haj-Mirzaian MD), Division of Cardiology (D H Nguyen BS), Massachusetts General Hospital, Boston, MA, USA; Department of Public Health (S Haller MD), Charité Institute of Public Health, Berlin, Germany; Faculty of Health (M Hamiduzzaman PhD), Southern Cross University, Bilinga, QLD, Australia; Department of Critical Care and Emergency Nursing (N Hanifi PhD), Zanjan University of Medical Sciences, Zanjan, Iran; Department of Pharmacy (Prof M S Hasnain PhD), Palamau Institute of Pharmacy, Daltonganj, India; Department of Diagnostic and Interventional Radiology and Neuroradiology (J Haubold MD), Institute of Artificial Intelligence in Medicine (J Haubold MD), University Hospital Essen, Essen, Germany; School of Dentistry (N Q Hoan DDS), Hanoi Medical University, Hanoi, Viet Nam; International Master Program for Translational Science (H Huynh BS), Nursing School (M Kurniasari PhD), International Ph D Program in Medicine (L Minh MD), Research Center for Artificial Intelligence in Medicine (L Minh MD), School of Public Health (Y L Samodra MPH, Y L Samodra MPH), Department of Clinical Pharmacy (M A Sarasmita PharmD), Taipei Medical University, Taipei, Taiwan; Department of Medical Microbiology (K C Iregbu MD), University of Abuja, Abuja, Nigeria; Department of Medical Microbiology (K C Iregbu MD), National Hospital, Abuja, Nigeria; Department of Pharmacy (M R Islam PhD), University of Asia Pacific, Dhaka, Bangladesh; Department of Immunology (Prof A Jafarzadeh PhD), Rafsanjan University of Medical Sciences, Rafsanjan, Iran; Health and Safety Department (A A Jairoun PhD), Dubai Municipality, Dubai, United Arab Emirates; Department of Microbiology (M Jalili MSc), Hamadan University of Medical Sciences, Hamadan, Iran; Department of Microbiology (N Jomehzadeh PhD), Abadan School of Medical Sciences, Abadan, Iran; Department of Economics (C E Joshua BSc), National Open University, Benin City, Nigeria; Department of Social Work (M Kabir PhD), Pabna University of Science and Technology, Pabna, Bangladesh; Department of Pharmacy (Z Kamal PhD), Shaheed Benazir Bhutto University, Dir Upper, Pakistan; School of Pharmacy (Z Kamal PhD), Shanghai Jiao Tong University, Shanghai, China; Faculty of Dentistry (K K Kanmodi MPH), University of Puthisastra, Phnom Penh, Cambodia; Office of the Executive Director (K K Kanmodi MPH), Campaign for Health and Neck Cancer Education (CHANCE) Programme (A A Salami BDS), Cephas Health Research Initiative, Ibadan, Nigeria; The Hansjörg Wyss Department of Plastic and Reconstructive Surgery (R S Kantar MD), Nab'a Al-Hayat Foundation for Medical Sciences and Health Care, New York, NY, USA; Cleft Lip and Palate Surgery Division (R S Kantar MD), Global Smile Foundation, Norwood, MA, USA; Endocrine Research Center (A Karimi Behnagh MD), Department of Echocardiography (A Karimi Behnagh MD), Department of Anesthesiology (K Latifinaibin MD), Microbial Biotechnology Research Center (A Zahedi Bialvaei PhD), Iran University of Medical Sciences, Tehran, Iran; Department of ENT (N Kaur MS), Dr B R Ambedkar State Institute of Medical Sciences (AIMS), Mohali, India; Public Health Foundation of India, New Delhi, India (H Kaur MPH); Population Science Department (M Khan PhD), Jatiya Kabi Kazi Nazrul Islam University, Mymensingh, Bangladesh; Department of Public Health (M Khan PhD), University of Sydney, Sydney, NSW, Australia; Department of Critical Care Medicine (M Z Khan Suheb MD), St Luke's Aurora Medical Center, Milwaukee, WI, USA; Department of Health (V Khanal PhD), Nepal Development Society, Chitwan, Nepal; Preventable Non Communicable Disease (V Khanal PhD), Menzies School of Health Research, Alice Springs, NT, Australia; College of Health, Wellbeing and Life Sciences (Prof K Khatab PhD), Sheffield Hallam University, Sheffield, UK; College of Arts and Sciences (Prof K Khatab PhD), Ohio University, Zanesville, OH, USA; Global Consortium for Public Health Research (Prof M Khatib PhD), Datta Meghe Institute of Higher Education and Research, Wardha, India; Department of Pediatrics (G Kim MD), Case Western Reserve University School of Medicine, Cleveland, OH, USA; Division of Pediatric Hospital Medicine (G Kim MD), UH Rainbow Babies and Children's Hospital, Cleveland, OH, USA; Department of Preventive Medicine (K Kim MD), Yonsei University, Seoul, South Korea; Department of Public Health (A T Kitila MPH), Wachemo University, Addis Ababa, Ethiopia; Department of Preventive and Social Medicine (A T Kitila MPH), University of Otago, Dunedin, New Zealand; Department of Physiology (S Komaki MD), Hamedan University of Medical Sciences, Hamedan, Iran; Department of Anthropology (Prof K Krishan PhD), Panjab University, Chandigarh, India; Department of Infectious Disease Epidemiology (R Krumkamp DrPH, Prof J May MD), Bernhard Nocht Institute for Tropical Medicine, Hamburg, Germany; Department of Mathematics (M Kuddus PhD), Department of Population Science and Human Resource Development (M Rahman DrPH), University of Rajshahi, Rajshahi, Bangladesh; Faculty of Medicine and Health Science (M Kurniasari PhD), Universitas Kristen Satya Wacana, Salatiga, Indonesia; Department of Health Policy and Strategy (Prof C Lahariya MD), Foundation for People-centric Health Systems, New Delhi, India; SD Gupta School of Public Health (Prof C Lahariya MD), Indian Institute of Health Management Research University, Jaipur, India; Faculty of Medicine (N Le MD), Department of General Medicine (V T Nguyen MD), Department of Otolaryngology (N Tran MSc), University of Medicine and Pharmacy at Ho Chi Minh City, Ho Chi Minh City, Viet Nam (T T Le MD, T D T Le MD); Cardiovascular Research Department (N Le MD), Methodist Hospital, Merrillville, IN, USA; Independent Consultant, Ho Chi Minh City, Viet Nam (T D T Le MD); Department of Precision Medicine (Prof S W Lee MD), Sungkyunkwan University, Suwon-si, South Korea; REA-REZO (A Lepape MD), Hospices Civils de Lyon, Lyon, France; Public Health, Epidemiology and Evolutionary Ecology of Infectious Diseases (PHE3ID) (A Lepape MD), Centre International de Recherche en Infectiologie (CIRI), Lyon, France; Department of Public Health (T L Lerango MPH), Dilla University, Dilla, Ethiopia; Department of Health Promotion and Health Education (M Li PhD), National Taiwan Normal University, Taipei, Taiwan; Department of Internal Medicine (K Malhotra MBBS), Dayanand Medical College and Hospital, Ludhiana, India; Department of Clinical Pharmacy (T Mallhi PhD), Jouf University, Sakaka, Saudi Arabia; Molecular Laboratory (A Manoharan PhD), The CHILDS Trust Medical Research Foundation, Chennai, India; Department of Infectious Diseases (B A Martinez-Guerra MSc, E Ortiz-Brizuela MSc, Prof A Ponce-De-Leon MD), Department of Medicine (A Olivas-Martinez MD), Instituto Nacional de Nutrición Salvador Zubirán (Salvador Zubiran National Institute of Medical Sciences and Nutrition), Mexico City, Mexico; North West Lung Centre (A G Mathioudakis PhD), Manchester University NHS Foundation Trust, Manchester, UK; Department of Social Medicine (R Mattiello PhD), Federal University of Rio Grande do Sul, Porto Alegre, Brazil; Department of Tropical Medicine (Prof J May MD), Medical Center Hamburg-Eppendorf (UKE), Hamburg, Germany; Australian Centre for Health Services Innovation (Prof S M McPhail PhD), Queensland University of Technology, Kelvin Grove, QLD, Australia; Digital Health and Informatics Directorate (Prof S M McPhail PhD), Queensland Health, Brisbane, QLD, Australia; Department of Public Health (T Mekene Meto MPH), Arba Minch University, Arbaminch, Ethiopia; Department of Medical Oncology and Hematology (M A M Mendez-Lopez PhD), Kantonsspital St Gallen, St Gallen, Switzerland; Department of Physiology (Prof S A Meo PhD), Pediatric Intensive Care Unit (M Temsah MD), King Saud University, Riyadh, Saudi Arabia; University Centre Varazdin (T Mestrovic PhD), University North, Varazdin, Croatia; Department of Preventive Medicine (L Mhlanga PhD), Northwestern University, Chicago, IL, USA; South African Centre for Epidemiological Modelling and Analysis (SACEMA) (L Mhlanga PhD), Department of Epidemiology (J L Tamuzi MSc), Stellenbosch University, Cape Town, South Africa; National Data Management Center for Health (A Misganaw PhD), Ethiopian Public Health Institute, Addis Ababa, Ethiopia; College of Healthcare Management and Economics (V Mishra PhD), Gulf Medical University, Ajman, United Arab Emirates; Department of Research and Development (V Mishra PhD), Panacea Institute of Interdisciplinary Research and Education, Varanasi, India, Varanasi, India; Department of Pharmacology (A K Misra MD), All India Institute of Medical Sciences, Mangalagiri, India; Molecular Biology Unit (N S Mohamed MSc), Bio-Statistical and Molecular Biology Department (N S Mohamed MSc), Sirius Training and Research Centre, Khartoum, Sudan; Department of Pharmacy (M Mohammed MSc), Madda Walabu University, Bale Robe, Ethiopia; QU Health (M Mohammed PhD), Qatar University, Doha, Qatar; Clinical Epidemiology and Public Health Research Unit (L Monasta DSc), Burlo Garofolo Institute for Maternal and Child Health, Trieste, Italy; Centre for Neonatal and Paediatric Infection (C E Moore PhD), St George's University of London, London, UK; Department of Community Medicine (R Motappa MD), Department of Internal Medicine (M M R Reddy MD), Manipal Academy of Higher Education, Mangalore, India; Department of Surgery (F Mulita PhD), General University Hospital of Patras, Patras, Greece; Faculty of Medicine (F Mulita PhD), Department of Emergency Medicine (I Pantazopoulos PhD), University of Thessaly, Larissa, Greece; Department of Nursing (A A Mulu MSc), Injibara University, Injibara, Ethiopia; Department of Computer and Information Science and Engineering (P Naghavi MSc), University of Florida, Gainesville, FL, USA; College of Medicine and Public Health (G R Naik PhD), Flinders University, Adelaide, SA, Australia; Faculty of Pharmacy (F Nainu PhD), Hasanuddin University, Makassar, Indonesia; Department of Community Medicine (T S Nair MD), MOSC Medical College, Kolenchery, India; Independent Consultant, Tehran, Iran (M Negaresh MD); Department of Internal Medicine (M Negaresh MD), Ardabil University of Medical Science, Ardabil, Iran; Faculty of Medicine (H T H Nguyen MD), Institute for Research and Training in Medicine, Biology and Pharmacy (H T H Nguyen MD), Duy Tan University, Da Nang, Viet Nam; Department of Medical Engineering (D H Nguyen BS), University of South Florida, Tampa, FL, USA; Department of General Surgery (T K Nikolouzakis PhD), University Hospital of Heraklion, Heraklion, Greece; Department of Laboratory of Toxicology (T K Nikolouzakis PhD), University of Crete, Heraklion, Greece; Department of Applied Microbiology (E A Noman PhD), Taiz University, Taiz, Yemen; Faculty of Applied Sciences and Technology (E A Noman PhD), Universiti Tun Hussein Onn Malaysia, Johor, Malaysia; Department of Paediatrics (C A Nri-Ezedi MD), Nnamdi Azikiwe University, Awka, Nigeria; Department of Veterinary Public Health and Preventive Medicine (I A Odetokun PhD), University of Ilorin, Ilorin, Nigeria; Department of Medical Physiology (P G Okwute MSc), Babcock University, Ilisan-Remo, Nigeria; Department of Medical Physiology (P G Okwute MSc), University of Lagos, Lagos, Nigeria; Department of Microbiology, Immunology and Parasitology (M D Olana PhD), Addis Ababa University, Addis Ababa, Ethiopia; Department of Medical Laboratory Sciences (M D Olana PhD), Ambo University, Ambo, Ethiopia; Helath Information Research Unit (O O Olasupo PhD), McMaster University, Hamilton, ON, Canada; Department of Pharmacotherapy and Pharmaceutical Care (M Ordak PhD), Department of Biochemistry and Pharmacogenomics (M Zielińska MPharm), Medical University of Warsaw, Warsaw, Poland; Department of Epidemiology, Biostatistics and Occupational Health (E Ortiz-Brizuela MSc), McGill University, Montreal, QC, Canada; Division of Infectious Diseases (Prof A Ouyahia PhD), University Hospital of Setif, Setif, Algeria; Department of Forensic Medicine and Toxicology (J Padubidri MD), Kasturba Medical College, Mangalore, Mangalore, India; Centre for the Business and Economics of Health (A Pak PhD), Faculty of Medicine (B Sartorius PhD), The University of Queensland, Brisbane, QLD, Australia; Australian Institute of Tropical Health and Medicine (A Pak PhD), James Cook University, Townsville, QLD, Australia; Department of Emergency Medicine (I Pantazopoulos PhD), University of Bern, Bern, Switzerland; Department of Community Medicine (P P Parija MD), All India Institute of Medical Sciences, Jammu, India; Department of Epidemiology and Community Health (R R Parikh MD), University of Minnesota School of Public Health, Minneapolis, MN, USA; Department of Biomedical Data Science (S Park MD), Department of Radiology (S Ramasamy MD), Stanford University, Stanford, CA, USA; Center for Pharmacoepidemiology and Treatment Science (A Parthasarathi MD), Rutgers University, New Brunswick, NJ, USA; Research Center (A Parthasarathi MD), Allergy Asthma and Chest Center, Mysore, India; School of Nursing (A Pashaei MSc), University of British Columbia, Vancouver, BC, Canada; Centre for Primary Health Care and Equity (P Peprah MSc), University of New South Wales, Kensington, Australia; School of Medicine (H Pham MD), Pham Ngoc Thach University of Medicine, Ho Chi Minh City, Viet Nam; Department of Medicine (Prof D Poddighe PhD), Nazarbayev University, Astana, Kazakhstan; Clinical Academic Department of Pediatrics (Prof D Poddighe PhD), University Medical Center (UMC), Astana, Kazakhstan; Department of Microbiology (P Y Prakash PhD), Department of Nephrology (I Rao DM), Manipal Academy of Higher Education, Manipal, India; Department of Maternal and Child Nursing and Public Health (E J S Prates BS), Federal University of Minas Gerais, Belo Horizonte, Brazil; College of Health Sciences (N Quan MD), VinUniversity, Hanoi, Viet Nam; Department of Health Sciences (Prof F Rahim PhD), Cihan University-Sulaymaniyah, Sulaymaniyah, Iraq; Cihan University Sulaimaniya Research Center (CUSRC), Sulaymaniyah, Iraq (Prof F Rahim PhD); Department of Physical Education and Sport Sciences (Prof M Rahmati PhD), Lorestan University, Khoramabad, Iran; School of Humanities and Social Sciences (S Ranjan MA), Indian Institute of Technology Mandi, Mandi, India; Department of Medicine (A M Rashid MD), Jinnah Sindh Medical University, Karachi, Pakistan; Emergency Department (S Rattanavong MD), Savannakhet Provincial Hospital, Savannakhet, Laos; Section of Pulmonary and Critical Care Medicine (N Ravikumar MD), University of Chicago, Chicago, IL, USA; Department Biological Sciences (Prof E M M Redwan PhD), King Abdulaziz University, Jeddah, Egypt; Department of Protein Research (Prof E M M Redwan PhD), Research and Academic Institution, Alexandria, Egypt; Unisabana Center for Translational Science (L F Reyes PhD), Universidad de La Sabana (Savannah University), Chia, Colombia; Critical Care Department (L F Reyes PhD), Clinica Universidad De La Sabana (Savannah University Clinic), Chia, Colombia; Department of Microbiology (T Roberts PhD), Lao- Oxford- Mahosot Hospital Wellcome Trust Research Unit, Vientiane, Laos; Department of Geography and Demography (M Rodrigues PhD), University of Coimbra, Coimbra, Portugal; Department of Public Health Sciences (V D Rosenthal MD), University of Miami, Miami, FL, USA; Department of Labour (P Roy PhD), Directorate of Factories, Government of West Bengal, Kolkata, India; Institute for Health Metrics and Evaluation (T Runghien MSc), University of Washington, Seattle, USA; Multidisciplinary Laboratory Foundation University School of Health Sciences (FUSH) (Prof U Saeed PhD), Foundation University, Islamabad, Pakistan; International Center of Medical Sciences Research (ICMSR), Islamabad, Pakistan (Prof U Saeed PhD); Department of Community Medicine and Family Medicine (S S Sahoo MD), All India Institute of Medical Sciences, Bathinda, India; Department of Preventive & Social Medicine (M Sahu MD), Independent Consultant, Kolkata, India; Institute for Employment Research, Nuremberg, Germany (J W Sakshaug PhD); Department of Oral and Maxillofacial Surgery (A A Salami BDS), University College Hospital, Ibadan, Ibadan, Nigeria; Faculty of Pharmacy (M A Saleh PhD), Mansoura University, Mansoura, Egypt; Department of Pathology, Microbiology and Forensic Medicine (M Sallam PhD), Department of Clinical Laboratories and Forensic Medicine (M Sallam PhD), Independent Consultant, Amman, Jordan; Department of Neurology (S Samadzadeh MD), University of Southern Denmark, Odense, Denmark; Department of Pediatrics (R K Sanjeev MD), Pravara Institute of Medical Sciences, Loni, India; Pharmacy Study Program (M A Sarasmita PharmD), Udayana University, Badung, Indonesia; Indira Gandhi Medical College and Research Institute, Puducherry, India (A Saravanan MD); Department of Medical Informatics (J Saulam MSc), Kagawa University, Miki-cho, Japan; Food Processing and Nutrition (J Saulam MSc), Karnataka State Akkamahadevi Women's University, Vijayapura, India; Department of Pathology and Laboratory Medicine (S Sham MD), Northwell Health, New York, NY, USA; Department of Pathobiology (M Shamshirgaran PhD), Shahid Bahonar University of Kerman, Kerman, Iran; Department of Microbiology (R P Shastry PhD), Yenepoya University, Mangalore, India; Department of Biology (S P Sherchan PhD), Morgan State University, Baltimore, MD, USA; Department of Environmental Health Sciences (S P Sherchan PhD), Tulane University, New Orleans, USA; Department of Public Health (D Shiferaw MPH), Dambi Dollo University, Dembi Dollo, Ethiopia; Department of Veterinary Public Health and Preventive Medicine (A Shittu MSc), Usmanu Danfodiyo University, Sokoto, Nigeria; Department of Medical Microbiology and Infectious Diseases (E E Siddig MD), Erasmus University, Rotterdam, Netherlands; Department of Internal Medicine (R Sinto MD), University of Indonesia, Jakarta Pusat, Indonesia; Department of Internal Medicine (R Sinto MD), Dr Cipto Mangunkusumo National Hospital, Jakarta Pusat, Indonesia; Internal Medicine Department (A Sood MD), The Wright Center for Graduate Medical Education, Scranton, PA, USA; Department of Microbiology and Virology (Prof T Z Stoeva PhD), Medical University of Varna, Varna, Bulgaria; Microbiology Laboratory (Prof T Z Stoeva PhD), University Hospital, Varna, Bulgaria; Department of Analytical and Applied Economics (C K Swain MPhil), Utkal University, Bhubaneswar, India; Department of Clinical Outcomes (Prof L Szarpak PhD), Maria Sklodowska-Curie Medical Academy, Warsaw, Poland; Department of Clinical Research and Development (Prof L Szarpak PhD), LUXMED Group, Warsaw, Poland; Department of Medicine (J L Tamuzi MSc), Northlands Medical Group, Omuthiya, Namibia; Department of Microbiology and Immunology (M B T Tessema PhD), University of Maryland, Baltimore, MD, USA; Department of Pharmacology (P Thangaraju MD), All India Institute of Medical Sciences, Raipur, India; Department of Health (N M Tran MD), Children's Hospital 1, Ho Chi Minh City, Viet Nam; Department of Physiology (M Tumurkhuu PhD), East Carolina University, Greenville, NC, USA; Department of Pharmacology (S Ty MD), All India Institute of Medical Sciences, Deoghar, India; Department of Biosciences and Biotechnology (A J Udoakang PhD), University of Medical Sciences, Ondo, Ondo, Nigeria; Health Department (I Ulhaq PhD), Ministry of Health, Peshawar, Pakistan; Health Department (I Ulhaq PhD), Directorate General of Health Services, Peshawar, Pakistan; Division of Surgery and Interventional Science (T Umar MD), University College London, London, UK; Department of Public Health (A A Umer MPH), Dire Dawa University, Dire Dawa, Ethiopia; College of Health and Sport Sciences (A G Vaithinathan MSc), University of Bahrain, Salmanya, Bahrain; Department of Cardiovascular Sciences (J Van den Eynde BSc), Katholieke Universiteit Leuven (University of Leuven), Leuven, Belgium; Natural and Medical Sciences Research Center (M Waqas PhD), University of Nizwa, Nizwa, Oman; Department of Biotechnology and Genetic Engineering (M Waqas PhD), Hazara University Mansehra, Mansehra, Pakistan; Department of Paediatrics (Y Xing PhD), The Chinese University of Hong Kong, Hong Kong Special Administrative Region, China; Department of Microbiology (M K Yadav PhD), Central University of Punjab, Bathinda, India; Department of Microbiology and Immunology (G Yahya PhD), Zagazig University, Zagazig, Egypt; Department of Cells and Tissues (G Yahya PhD), Molecular Biology Institute of Barcelona, Barcelona, Spain; Department of Pediatrics (Prof D Yon MD), Kyung Hee University, Seoul, South Korea; Faculty of Medicine and Health Sciences (F Zakham PhD), Hodeidah University, Hodeidah, Yemen; Department of Virology (F Zakham PhD), University of Helsinki, Helsinki, Finland; School of Nursing (A M Zeleke MSc), Hawassa University, Hawassa, Ethiopia; Department of Epidemiology and Biostatistics (C Zhai MD), Anhui Medical University, Hefei, China; Department of Nutrition and Food Hygiene (Z Zhang PhD), School of Public Health (H Zhang MS), Peking University, Beijing, China; Department of International Health (H Zhang MS), Johns Hopkins University, Baltimore, MD, USA.
Contributors
Please see appendix 1 (pp 34–37) for more detailed information about individual author contributions to the research, divided into the following categories: managing the overall research enterprise; writing the first draft of the manuscript; primary responsibility for applying analytical methods to produce estimates; primary responsibility for seeking, cataloguing, extracting, or cleaning data; designing or coding figures and tables; providing data or critical feedback on data sources; developing methods or computational machinery; providing critical feedback on methods or results; drafting the manuscript or revising it critically for important intellectual content; and managing the estimation or publications process. Members of the core research team (R G Bender, S B Sirota, L R Swetschinski, R-M V Dominguez, A Novotney, E E Wool, K S Ikuta, A Vongpradith, E L B Rogowski, S B Albertson, C J L Murray, M Naghavi, and H H Kyu) for this topic area had full access to the underlying data used to generate the estimates presented in this Article. All other authors had access to and reviewed the estimates as part of the research evaluation process, which included additional formal stages of review. H H Kyu and M Naghavi accessed and verified the underlying data reported in this study. The corresponding author had final responsibility for the decision to submit the manuscript for publication.
Contributor Information
GBD 2021 Lower Respiratory Infections and Antimicrobial Resistance Collaborators:
Rose Grace Bender, Sarah Brooke Sirota, Lucien R Swetschinski, Regina-Mae Villanueva Dominguez, Amanda Novotney, Eve E Wool, Kevin S Ikuta, Avina Vongpradith, Emma Lynn Best Rogowski, Matthew Doxey, Christopher E Troeger, Samuel B Albertson, Jianing Ma, Jiawei He, Kelsey Lynn Maass, Eric A.F.Simões, Meriem Abdoun, Jeza Muhamad Abdul Aziz, Deldar Morad Abdulah, Samir Abu Rumeileh, Hasan Abualruz, Salahdein Aburuz, Abiola Victor Adepoju, Rishan Adha, Wirawan Adikusuma, Saryia Adra, Ali Afraz, Shahin Aghamiri, Antonella Agodi, Amir Mahmoud Ahmadzade, Haroon Ahmed, Ayman Ahmed, Karolina Akinosoglou, Tareq Mohammed Ali AL-Ahdal, Rasmieh Mustafa Al-amer, Mohammed Albashtawy, Mohammad T. AlBataineh, Hediyeh Alemi, Adel Ali Saeed Al-Gheethi, Abid Ali, Syed Shujait Shujait Ali, Jaber S Alqahtani, Mohammad AlQudah, Jaffar A. Al-Tawfiq, Yaser Mohammed Al-Worafi, Karem H Alzoubi, Reza Amani, Prince M Amegbor, Edward Kwabena Ameyaw, John H Amuasi, Abhishek Anil, Philip Emeka Anyanwu, Mosab Arafat, Damelash Areda, Reza Arefnezhad, Kendalem Asmare Atalell, Firayad Ayele, Ahmed Y Azzam, Hassan Babamohamadi, François-Xavier Babin, Yogesh Bahurupi, Stephen Baker, Biswajit Banik, Martina Barchitta, Hiba Jawdat Barqawi, Zarrin Basharat, Pritish Baskaran, Kavita Batra, Ravi Batra, Nebiyou Simegnew Bayileyegn, Apostolos Beloukas, James A Berkley, Kebede A Beyene, Ashish Bhargava, Priyadarshini Bhattacharjee, Julia A Bielicki, Mariah Malak Bilalaga, Veera R Bitra, Colin Stewart Brown, Katrin Burkart, Yasser Bustanji, Sinclair Carr, Yaacoub Chahine, Vijay Kumar Chattu, Fatemeh Chichagi, Hitesh Chopra, Isaac Sunday Chukwu, Eunice Chung, Sriharsha Dadana, Xiaochen Dai, Lalit Dandona, Rakhi Dandona, Isaac Darban, Nihar Ranjan Dash, Mohsen Dashti, Mohadese Dashtkoohi, Denise Myriam Dekker, Ivan Delgado-Enciso, Vinoth Gnana Chellaiyan Devanbu, Kuldeep Dhama, Nancy Diao, Thao Huynh Phuong Do, Klara Georgieva Dokova, Christiane Dolecek, Arkadiusz Marian Dziedzic, Tim Eckmanns, Abdelaziz Ed-Dra, Ferry Efendi, Aziz Eftekharimehrabad, David William Eyre, Ayesha Fahim, Alireza Feizkhah, Timothy William Felton, Nuno Ferreira, Luisa S Flor, Santosh Gaihre, Miglas W Gebregergis, Mesfin Gebrehiwot, Christine Geffers, Urge Gerema, Kazem Ghaffari, Mohamad Goldust, Pouya Goleij, Shi-Yang Guan, Mesay Dechasa Gudeta, Cui Guo, Veer Bala Gupta, Ishita Gupta, Farrokh Habibzadeh, Najah R Hadi, Emily Haeuser, Wase Benti Hailu, Ramtin Hajibeygi, Arvin Haj-Mirzaian, Sebastian Haller, Mohammad Hamiduzzaman, Nasrin Hanifi, Jan Hansel, Md Saquib Hasnain, Johannes Haubold, Nguyen Quoc Hoan, Hong-Han Huynh, Kenneth Chukwuemeka Iregbu, Md. Rabiul Islam, Abdollah Jafarzadeh, Ammar Abdulrahman Jairoun, Mahsa Jalili, Nabi Jomehzadeh, Charity Ehimwenma Joshua, Md. Awal Kabir, Zul Kamal, Kehinde Kazeem Kanmodi, Rami S. Kantar, Arman Karimi Behnagh, Navjot Kaur, Harkiran Kaur, Faham Khamesipour, M Nuruzzaman Khan, Mahammed Ziauddin Khan suheb, Vishnu Khanal, Khaled Khatab, Mahalaqua Nazli Khatib, Grace Kim, Kwanghyun Kim, Aiggan Tamene Tamene Kitila, Somayeh Komaki, Kewal Krishan, Ralf Krumkamp, Md Abdul Kuddus, Maria Dyah Kurniasari, Chandrakant Lahariya, Kaveh Latifinaibin, Nhi Huu Hanh Le, Thao Thi Thu Le, Trang Diep Thanh Le, Seung Won Lee, Alain LEPAPE, Temesgen L. Lerango, Ming-Chieh Li, Amir Ali Mahboobipour, Kashish Malhotra, Tauqeer Hussain Mallhi, Anand Manoharan, Bernardo Alfonso Martinez-Guerra, Alexander G. Mathioudakis, Rita Mattiello, Jürgen May, Barney McManigal, Steven M McPhail, Tesfahun Mekene Meto, Max Alberto Mendez Mendez-Lopez, Sultan Ayoub Meo, Mohsen Merati, Tomislav Mestrovic, Laurette Mhlanga, Le Huu Nhat Minh, Awoke Misganaw, Vinaytosh Mishra, Arup Kumar Misra, Nouh Saad Mohamed, Esmaeil Mohammadi, Mesud Mohammed, Mustapha Mohammed, Ali H Mokdad, Lorenzo Monasta, Catrin E Moore, Rohith Motappa, Vincent Mougin, Parsa Mousavi, Francesk Mulita, Atsedemariam Andualem Mulu, Pirouz Naghavi, Ganesh R Naik, Firzan Nainu, Tapas Sadasivan Nair, Shumaila Nargus, Mohammad Negaresh, Hau Thi Hien Nguyen, Dang H Nguyen, Van Thanh Nguyen, Taxiarchis Konstantinos Nikolouzakis, Efaq Ali Noman, Chisom Adaobi Nri-Ezedi, Ismail A. Odetokun, Patrick Godwin Okwute, Matifan Dereje Olana, Titilope O Olanipekun, Omotola O. Olasupo, Antonio Olivas-Martinez, Michal Ordak, Edgar Ortiz-Brizuela, Amel Ouyahia, Jagadish Rao Padubidri, Anton Pak, Anamika Pandey, Ioannis Pantazopoulos, Pragyan Paramita Parija, Romil R Parikh, Seoyeon Park, Ashwaghosha Parthasarathi, Ava Pashaei, Prince Peprah, Hoang Tran Pham, Dimitri Poddighe, Andrew Pollard, Alfredo Ponce-De-Leon, Peralam Yegneswaran Prakash, Elton Junio Sady Prates, Nguyen Khoi Quan, Pourya Raee, Fakher Rahim, Mosiur Rahman, Masoud Rahmati, Shakthi Kumaran Ramasamy, Shubham Ranjan, Indu Ramachandra Rao, Ahmed Mustafa Rashid, Sayaphet Rattanavong, Nakul Ravikumar, Murali Mohan Rama Krishna Reddy, Elrashdy Moustafa Mohamed Redwan, Robert C Reiner, Jr., Luis Felipe Reyes, Tamalee Roberts, Mónica Rodrigues, Victor Daniel Rosenthal, Priyanka Roy, Tilleye Runghien, Umar Saeed, Amene Saghazadeh, Narjes Saheb Sharif-Askari, Fatemeh Saheb Sharif-Askari, Soumya Swaroop Sahoo, Monalisha Sahu, Joseph W Sakshaug, Afeez Abolarinwa Salami, Mohamed A. Saleh, Hossein Salehi omran, Malik Sallam, Sara Samadzadeh, Yoseph Leonardo Samodra, Rama Krishna Sanjeev, Made Ary Sarasmita, Aswini Saravanan, Benn Sartorius, Jennifer Saulam, Austin E Schumacher, Seyed Arsalan Seyedi, Mahan Shafie, Samiah Shahid, Sunder Sham, Muhammad Aaqib Shamim, Mohammad Ali Shamshirgaran, Rajesh P. Shastry, Samendra P Sherchan, Desalegn Shiferaw, Aminu Shittu, Emmanuel Edwar Siddig, Robert Sinto, Aayushi Sood, Reed J D Sorensen, Andy Stergachis, Temenuga Zhekova Stoeva, Chandan Kumar Swain, Lukasz Szarpak, Jacques Lukenze Tamuzi, Mohamad-Hani Temsah, Melkamu B Tessema Tessema, Pugazhenthan Thangaraju, Nghia Minh Tran, Ngoc-Ha Tran, Munkhtuya Tumurkhuu, Sree Sudha Ty, Aniefiok John Udoakang, Inam Ulhaq, Tungki Pratama Umar, Abdurezak Adem Umer, Seyed Mohammad Vahabi, Asokan Govindaraj Vaithinathan, Jef Van den Eynde, Judd L Walson, Muhammad Waqas, Yuhan Xing, Mukesh Kumar Yadav, Galal Yahya, Dong Keon Yon, Abed Zahedi Bialvaei, Fathiah Zakham, Abyalew Mamuye Zeleke, Chunxia Zhai, Zhaofeng Zhang, Haijun Zhang, Magdalena Zielińska, Peng Zheng, Aleksandr Y Aravkin, Theo Vos, Simon I Hay, Jonathan F. Mosser, Stephen S Lim, Mohsen Naghavi, Christopher J L Murray, and Hmwe Hmwe Kyu
Supplementary Materials
References
- 1.WHO Global health estimates. https://www.who.int/data/global-health-estimates
- 2.Vos T, Lim SS, Abbafati C, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kyu HH, Vongpradith A, Sirota SB, et al. Age-sex differences in the global burden of lower respiratory infections and risk factors, 1990–2019: results from the Global Burden of Disease Study 2019. Lancet Infect Dis. 2022;22:1626–1647. doi: 10.1016/S1473-3099(22)00510-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Falagas ME, Mourtzoukou EG, Vardakas KZ. Sex differences in the incidence and severity of respiratory tract infections. Respir Med. 2007;101:1845–1863. doi: 10.1016/j.rmed.2007.04.011. [DOI] [PubMed] [Google Scholar]
- 5.Ursin RL, Klein SL. Sex differences in respiratory viral pathogenesis and treatments. Annu Rev Virol. 2021;8:393–414. doi: 10.1146/annurev-virology-091919-092720. [DOI] [PubMed] [Google Scholar]
- 6.Almirall J, Serra-Prat M, Bolíbar I, Balasso V. Risk factors for community-acquired pneumonia in adults: a systematic review of observational studies. Respiration. 2017;94:299–311. doi: 10.1159/000479089. [DOI] [PubMed] [Google Scholar]
- 7.Cillóniz C, Rodríguez-Hurtado D, Torres A. Characteristics and management of community-acquired pneumonia in the era of global aging. Med Sci (Basel) 2018;6:35. doi: 10.3390/medsci6020035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wahl B, O'Brien KL, Greenbaum A, et al. Burden of Streptococcus pneumoniae and Haemophilus influenzae type b disease in children in the era of conjugate vaccines: global, regional, and national estimates for 2000–15. Lancet Glob Health. 2018;6:e744–e757. doi: 10.1016/S2214-109X(18)30247-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shoar S, Musher DM. Etiology of community-acquired pneumonia in adults: a systematic review. Pneumonia. 2020;12:11. doi: 10.1186/s41479-020-00074-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.O'Brien KL, Baggett HC, Brooks WA, et al. Causes of severe pneumonia requiring hospital admission in children without HIV infection from Africa and Asia: the PERCH multi-country case-control study. Lancet. 2019;394:757–779. doi: 10.1016/S0140-6736(19)30721-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rudan I, O'Brien KL, Nair H, et al. Epidemiology and etiology of childhood pneumonia in 2010: estimates of incidence, severe morbidity, mortality, underlying risk factors and causative pathogens for 192 countries. J Glob Health. 2013;3 doi: 10.7189/jogh.03.010401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Troeger C, Forouzanfar M, Rao PC, et al. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory tract infections in 195 countries: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Infect Dis. 2017;17:1133–1161. doi: 10.1016/S1473-3099(17)30396-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Self WH, Wunderink RG, Williams DJ, et al. Staphylococcus aureus community-acquired pneumonia: prevalence, clinical characteristics, and outcomes. Clin Infect Dis. 2016;63:300–309. doi: 10.1093/cid/ciw300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thabet N, Shindo Y, Okumura J, et al. Clinical characteristics and risk factors for mortality in patients with community-acquired staphylococcal pneumonia. Nagoya J Med Sci. 2022;84:247–259. doi: 10.18999/nagjms.84.2.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guo Y, Song G, Sun M, Wang J, Wang Y. Prevalence and therapies of antibiotic-resistance in Staphylococcus aureus. Front Cell Infect Microbiol. 2020;10:107. doi: 10.3389/fcimb.2020.00107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jain S, Williams DJ, Arnold SR, et al. Community-acquired pneumonia requiring hospitalization among U.S. children. N Engl J Med. 2015;372:835–845. doi: 10.1056/NEJMoa1405870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Meyer Sauteur PM, Unger WW, Nadal D, Berger C, Vink C, van Rossum AM. Infection with and carriage of Mycoplasma pneumoniae in children. Front Microbiol. 2016;7:329. doi: 10.3389/fmicb.2016.00329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jain S. Epidemiology of viral pneumonia. Clin Chest Med. 2017;38:1–9. doi: 10.1016/j.ccm.2016.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lafond KE, Porter RM, Whaley MJ, et al. Global burden of influenza-associated lower respiratory tract infections and hospitalizations among adults: a systematic review and meta-analysis. PLoS Med. 2021;18 doi: 10.1371/journal.pmed.1003550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li Y, Wang X, Blau DM, et al. Global, regional, and national disease burden estimates of acute lower respiratory infections due to respiratory syncytial virus in children younger than 5 years in 2019: a systematic analysis. Lancet. 2022;399:2047–2064. doi: 10.1016/S0140-6736(22)00478-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Klein EY, Monteforte B, Gupta A, et al. The frequency of influenza and bacterial coinfection: a systematic review and meta-analysis. Influenza Other Respir Viruses. 2016;10:394–403. doi: 10.1111/irv.12398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chow EJ, Uyeki TM, Chu HY. The effects of the COVID-19 pandemic on community respiratory virus activity. Nat Rev Microbiol. 2023;21:195–210. doi: 10.1038/s41579-022-00807-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sullivan SG, Carlson S, Cheng AC, et al. Where has all the influenza gone? The impact of COVID-19 on the circulation of influenza and other respiratory viruses, Australia, March to September 2020. Euro Surveill. 2020;25 doi: 10.2807/1560-7917.ES.2020.25.47.2001847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Islam N, Sharp SJ, Chowell G, et al. Physical distancing interventions and incidence of coronavirus disease 2019: natural experiment in 149 countries. BMJ. 2020;370 doi: 10.1136/bmj.m2743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chuang Y-C, Lin K-P, Wang L-A, Yeh T-K, Liu P-Y. The impact of the COVID-19 pandemic on respiratory syncytial virus infection: a narrative review. Infect Drug Resist. 2023;16:661–675. doi: 10.2147/IDR.S396434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kang L, Jing W, Liu J, Liu M. Trends of global and regional aetiologies, risk factors and mortality of lower respiratory infections from 1990 to 2019: an analysis for the Global Burden of Disease Study 2019. Respirology. 2023;28:166–175. doi: 10.1111/resp.14389. [DOI] [PubMed] [Google Scholar]
- 27.Murray CJ, Ikuta KS, Sharara F, et al. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. 2022;399:629–655. doi: 10.1016/S0140-6736(21)02724-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.GBD 2019 Antimicrobial Resistance Collaborators Global mortality associated with 33 bacterial pathogens in 2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2022;400:2221–2248. doi: 10.1016/S0140-6736(22)02185-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Naing NN. Easy way to learn standardization: direct and indirect methods. Malays J Med Sci. 2000;7:10–15. [PMC free article] [PubMed] [Google Scholar]
- 30.Stevens GA, Alkema L, Black RE, et al. Guidelines for Accurate and Transparent Health Estimates Reporting: the GATHER statement. Lancet. 2016;388:e19–e23. doi: 10.1016/S0140-6736(16)30388-9. [DOI] [PubMed] [Google Scholar]
- 31.Foreman KJ, Lozano R, Lopez AD, Murray CJ. Modeling causes of death: an integrated approach using CODEm. Popul Health Metr. 2012;10:1. doi: 10.1186/1478-7954-10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barendregt JJ, Van Oortmarssen GJ, Vos T, Murray CJ. A generic model for the assessment of disease epidemiology: the computational basis of DisMod II. Popul Health Metr. 2003;1:4. doi: 10.1186/1478-7954-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fullman N, Yearwood J, Abay SM, et al. Measuring performance on the Healthcare Access and Quality Index for 195 countries and territories and selected subnational locations: a systematic analysis from the Global Burden of Disease Study 2016. Lancet. 2018;391:2236–2271. doi: 10.1016/S0140-6736(18)30994-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zheng P, Barber R, Sorensen RJD, Murray CJL, Aravkin AY. Trimmed constrained mixed effects models: formulations and algorithms. J Comput Graph Stat. 2021;30:544–556. [Google Scholar]
- 35.Feikin DR, Scott JAG, Gessner BD. Use of vaccines as probes to define disease burden. Lancet. 2014;383:1762–1770. doi: 10.1016/S0140-6736(13)61682-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.WHO FluNet: global influenza programme. https://www.who.int/tools/flunet
- 37.Zheng P, He J, Maass K. RegMod. Feb 1, 2023. https://github.com/ihmeuw-msca/regmod
- 38.Kassebaum NJ, Arora M, Barber RM, et al. Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1603–1658. doi: 10.1016/S0140-6736(16)31460-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sonego M, Pellegrin MC, Becker G, Lazzerini M. Risk factors for mortality from acute lower respiratory infections (ALRI) in children under five years of age in low and middle-income countries: a systematic review and meta-analysis of observational studies. PLoS One. 2015;10 doi: 10.1371/journal.pone.0116380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.WHO. UNICEF Ending preventable child deaths from pneumonia and diarrhoea by 2025: the integrated global action plan for pneumonia and diarrhoea (GAPPD) 2013. https://apps.who.int/iris/handle/10665/79200 [DOI] [PubMed]
- 41.Niessen LW, ten Hove A, Hilderink H, Weber M, Mulholland K, Ezzati M. Comparative impact assessment of child pneumonia interventions. Bull World Health Organ. 2009;87:472–480. doi: 10.2471/BLT.08.050872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.WHO Immunization dashboard. https://immunizationdata.who.int/
- 43.Causey K, Fullman N, Sorensen RJD, et al. Estimating global and regional disruptions to routine childhood vaccine coverage during the COVID-19 pandemic in 2020: a modelling study. Lancet. 2021;398:522–534. doi: 10.1016/S0140-6736(21)01337-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Immunization Agenda 2030 Partnership Council Partnership Council statement on the latest WUENIC release. July 17, 2023. https://www.immunizationagenda2030.org/images/documents/final2IAPC17_July_WEUNIC_STATEMENT.pdf
- 45.Chopra M, Bhutta Z, Chang Blanc D, et al. Addressing the persistent inequities in immunization coverage. Bull World Health Organ. 2020;98:146–148. doi: 10.2471/BLT.19.241620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mutombo PN, Fallah MP, Munodawafa D, et al. COVID-19 vaccine hesitancy in Africa: a call to action. Lancet Glob Health. 2022;10:e320–e321. doi: 10.1016/S2214-109X(21)00563-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pertwee E, Simas C, Larson HJ. An epidemic of uncertainty: rumors, conspiracy theories and vaccine hesitancy. Nat Med. 2022;28:456–459. doi: 10.1038/s41591-022-01728-z. [DOI] [PubMed] [Google Scholar]
- 48.Cata-Preta BO, Santos TM, Mengistu T, Hogan DR, Barros AJD, Victora CG. Zero-dose children and the immunisation cascade: understanding immunisation pathways in low and middle-income countries. Vaccine. 2021;39:4564–4570. doi: 10.1016/j.vaccine.2021.02.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.WHO Immunization agenda 2030: a global strategy to leave no one behind. April 1, 2020. https://www.who.int/publications/m/item/immunization-agenda-2030-a-global-strategy-to-leave-no-one-behind [DOI] [PubMed]
- 50.Liu Y, Zhang Y, Zhao W, Liu X, Hu F, Dong B. Pharmacotherapy of lower respiratory tract infections in elderly—focused on antibiotics. Front Pharmacol. 2019;10 doi: 10.3389/fphar.2019.01237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Murray MA, Chotirmall SH. The impact of immunosenescence on pulmonary disease. Mediators Inflamm. 2015;2015 doi: 10.1155/2015/692546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shiri T, Datta S, Madan J, et al. Indirect effects of childhood pneumococcal conjugate vaccination on invasive pneumococcal disease: a systematic review and meta-analysis. Lancet Glob Health. 2017;5:e51–e59. doi: 10.1016/S2214-109X(16)30306-0. [DOI] [PubMed] [Google Scholar]
- 53.Tsaban G, Ben-Shimol S. Indirect (herd) protection, following pneumococcal conjugated vaccines introduction: a systematic review of the literature. Vaccine. 2017;35:2882–2891. doi: 10.1016/j.vaccine.2017.04.032. [DOI] [PubMed] [Google Scholar]
- 54.Leidner AJ, Murthy N, Chesson HW, et al. Cost-effectiveness of adult vaccinations: a systematic review. Vaccine. 2019;37:226–234. doi: 10.1016/j.vaccine.2018.11.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bonten MJM, Huijts SM, Bolkenbaas M, et al. Polysaccharide conjugate vaccine against pneumococcal pneumonia in adults. N Engl J Med. 2015;372:1114–1125. doi: 10.1056/NEJMoa1408544. [DOI] [PubMed] [Google Scholar]
- 56.Gessner BD, Jiang Q, Van Werkhoven CH, et al. A public health evaluation of 13-valent pneumococcal conjugate vaccine impact on adult disease outcomes from a randomized clinical trial in the Netherlands. Vaccine. 2019;37:5777–5787. doi: 10.1016/j.vaccine.2018.05.097. [DOI] [PubMed] [Google Scholar]
- 57.Kraicer-Melamed H, O'Donnell S, Quach C. The effectiveness of pneumococcal polysaccharide vaccine 23 (PPV23) in the general population of 50 years of age and older: a systematic review and meta-analysis. Vaccine. 2016;34:1540–1550. doi: 10.1016/j.vaccine.2016.02.024. [DOI] [PubMed] [Google Scholar]
- 58.Oh S-J, Lee JK, Shin OS. Aging and the immune system: the impact of immunosenescence on viral infection, immunity and vaccine immunogenicity. Immune Netw. 2019;19:e37. doi: 10.4110/in.2019.19.e37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Privor-Dumm LA, Poland GA, Barratt J, et al. A global agenda for older adult immunization in the COVID-19 era: a roadmap for action. Vaccine. 2021;39:5240–5250. doi: 10.1016/j.vaccine.2020.06.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sauer M, Vasudevan P, Meghani A, et al. Situational assessment of adult vaccine preventable disease and the potential for immunization advocacy and policy in low- and middle-income countries. Vaccine. 2021;39:1556–1564. doi: 10.1016/j.vaccine.2021.01.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Eiden AL, Barratt J, Nyaku MK. A review of factors influencing vaccination policies and programs for older adults globally. Hum Vaccin Immunother. 2023;19 doi: 10.1080/21645515.2022.2157164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sparrow E, Adetifa I, Chaiyakunapruk N, et al. WHO preferred product characteristics for monoclonal antibodies for passive immunization against respiratory syncytial virus (RSV) disease in infants—key considerations for global use. Vaccine. 2022;40:3506–3510. doi: 10.1016/j.vaccine.2022.02.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mazur NI, Terstappen J, Baral R, et al. Respiratory syncytial virus prevention within reach: the vaccine and monoclonal antibody landscape. Lancet Infect Dis. 2023;23:e2–21. doi: 10.1016/S1473-3099(22)00291-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Venkatesan P. First RSV vaccine approvals. Lancet Microbe. 2023;4:e577. doi: 10.1016/S2666-5247(23)00195-7. [DOI] [PubMed] [Google Scholar]
- 65.Walsh EE, Pérez Marc G, Zareba AM, et al. Efficacy and safety of a bivalent RSV prefusion F vaccine in older adults. N Engl J Med. 2023;388:1465–1477. doi: 10.1056/NEJMoa2213836. [DOI] [PubMed] [Google Scholar]
- 66.Papi A, Ison MG, Langley JM, et al. Respiratory syncytial virus prefusion F protein vaccine in older adults. N Engl J Med. 2023;388:595–608. doi: 10.1056/NEJMoa2209604. [DOI] [PubMed] [Google Scholar]
- 67.Kampmann B, Madhi SA, Munjal I, et al. Bivalent prefusion F vaccine in pregnancy to prevent RSV illness in infants. N Engl J Med. 2023;388:1451–1464. doi: 10.1056/NEJMoa2216480. [DOI] [PubMed] [Google Scholar]
- 68.Hammitt LL, Dagan R, Yuan Y, et al. Nirsevimab for prevention of RSV in healthy late-preterm and term infants. N Engl J Med. 2022;386:837–846. doi: 10.1056/NEJMoa2110275. [DOI] [PubMed] [Google Scholar]
- 69.Keam SJ. Nirsevimab: first approval. Drugs. 2023;83:181–187. doi: 10.1007/s40265-022-01829-6. [DOI] [PubMed] [Google Scholar]
- 70.Mahmud S, Baral R, Sanderson C, et al. Cost-effectiveness of pharmaceutical strategies to prevent respiratory syncytial virus disease in young children: a decision-support model for use in low-income and middle-income countries. BMC Med. 2023;21:138. doi: 10.1186/s12916-023-02827-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Li X, Willem L, Antillon M, Bilcke J, Jit M, Beutels P. Health and economic burden of respiratory syncytial virus (RSV) disease and the cost-effectiveness of potential interventions against RSV among children under 5 years in 72 Gavi-eligible countries. BMC Med. 2020;18:82. doi: 10.1186/s12916-020-01537-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Baral R, Higgins D, Regan K, Pecenka C. Impact and cost-effectiveness of potential interventions against infant respiratory syncytial virus (RSV) in 131 low-income and middle-income countries using a static cohort model. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2020-046563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Van Effelterre T, Hens N, White LJ, et al. Modeling respiratory syncytial virus adult vaccination in the United States with a dynamic transmission model. Clin Infect Dis. 2023;77:480–489. doi: 10.1093/cid/ciad161. [DOI] [PubMed] [Google Scholar]
- 74.Carbonell-Estrany X, Simões EA, Bont LJ, et al. Prioritising respiratory syncytial virus prevention in low-income and middle-income countries. Lancet Glob Health. 2023;11:e655–e657. doi: 10.1016/S2214-109X(23)00165-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Frush JM, Zhu Y, Edwards KM, et al. Prevalence of Staphylococcus aureus and use of antistaphylococcal therapy in children hospitalized with pneumonia. J Hosp Med. 2018;13:848–852. doi: 10.12788/jhm.3093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Murdoch DR. How recent advances in molecular tests could impact the diagnosis of pneumonia. Expert Rev Mol Diagn. 2016;16:533–540. doi: 10.1586/14737159.2016.1156536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Aliberti S, Reyes LF, Faverio P, et al. Global initiative for meticillin-resistant Staphylococcus aureus pneumonia (GLIMP): an international, observational cohort study. Lancet Infect Dis. 2016;16:1364–1376. doi: 10.1016/S1473-3099(16)30267-5. [DOI] [PubMed] [Google Scholar]
- 78.Tacconelli E, Carrara E, Savoldi A, et al. Discovery, research, and development of new antibiotics: the WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect Dis. 2018;18:318–327. doi: 10.1016/S1473-3099(17)30753-3. [DOI] [PubMed] [Google Scholar]
- 79.Shariati A, Dadashi M, Moghadam MT, van Belkum A, Yaslianifard S, Darban-Sarokhalil D. Global prevalence and distribution of vancomycin resistant, vancomycin intermediate and heterogeneously vancomycin intermediate Staphylococcus aureus clinical isolates: a systematic review and meta-analysis. Sci Rep. 2020;10 doi: 10.1038/s41598-020-69058-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Rodrigues CMC, Groves H. Community-acquired pneumonia in children: the challenges of microbiological diagnosis. J Clin Microbiol. 2018;56:e01318–e01417. doi: 10.1128/JCM.01318-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Baby N, Faust AC, Smith T, Sheperd LA, Knoll L, Goodman EL. Nasal methicillin-resistant Staphylococcus aureus (MRSA) PCR testing reduces the duration of MRSA-targeted therapy in patients with suspected MRSA pneumonia. Antimicrob Agents Chemother. 2017;61:e02432–e02516. doi: 10.1128/AAC.02432-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Smith MN, Brotherton AL, Lusardi K, Tan CA, Hammond DA. Systematic review of the clinical utility of methicillin-resistant Staphylococcus aureus (MRSA) nasal screening for MRSA pneumonia. Ann Pharmacother. 2019;53:627–638. doi: 10.1177/1060028018823027. [DOI] [PubMed] [Google Scholar]
- 83.Clegg J, Soldaini E, McLoughlin RM, Rittenhouse S, Bagnoli F, Phogat S. Staphylococcus aureus vaccine research and development: the past, present and future, including novel therapeutic strategies. Front Immunol. 2021;12 doi: 10.3389/fimmu.2021.705360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Proctor RA. Is there a future for a Staphylococcus aureus vaccine? Vaccine. 2012;30:2921–2927. doi: 10.1016/j.vaccine.2011.11.006. [DOI] [PubMed] [Google Scholar]
- 85.Perin J, Mulick A, Yeung D, et al. Global, regional, and national causes of under-5 mortality in 2000–19: an updated systematic analysis with implications for the Sustainable Development Goals. Lancet Child Adolesc Health. 2022;6:106–115. doi: 10.1016/S2352-4642(21)00311-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Lansbury L, Lim B, McKeever TM, Lawrence H, Lim WS. Non-invasive pneumococcal pneumonia due to vaccine serotypes: a systematic review and meta-analysis. EClinicalMedicine. 2022;44 doi: 10.1016/j.eclinm.2022.101271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ollila HM, Partinen M, Koskela J, et al. Face masks to prevent transmission of respiratory infections: systematic review and meta-analysis of randomized controlled trials on face mask use. PLoS One. 2022;17 doi: 10.1371/journal.pone.0271517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Chen Y, Wang Y, Quan N, Yang J, Wu Y. Associations between wearing masks and respiratory viral infections: a meta-analysis and systematic review. Front Public Health. 2022;10 doi: 10.3389/fpubh.2022.874693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Nouvellet P, Bhatia S, Cori A, et al. Reduction in mobility and COVID-19 transmission. Nat Commun. 2021;12 doi: 10.1038/s41467-021-21358-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Oh J, Lee H-Y, Khuong QL, et al. Mobility restrictions were associated with reductions in COVID-19 incidence early in the pandemic: evidence from a real-time evaluation in 34 countries. Sci Rep. 2021;11 doi: 10.1038/s41598-021-92766-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Tang H-J, Lai C-C, Chao C-M. Changing epidemiology of respiratory tract infection during COVID-19 pandemic. Antibiotics (Basel) 2022;11:315. doi: 10.3390/antibiotics11030315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Clemente I, Santini SJ, Vittorini P, et al. Fall of viral and bacterial pneumonia hospitalizations following COVID-19 pandemic mitigation strategies: a Central Italian Region retrospective study. Intern Emerg Med. 2023;18:1181–1189. doi: 10.1007/s11739-023-03213-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Yan Y, Tomooka K, Naito T, Tanigawa T. Decreased number of inpatients with community-acquired pneumonia during the COVID-19 pandemic: a large multicenter study in Japan. J Infect Chemother. 2022;28:709–713. doi: 10.1016/j.jiac.2022.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Brueggemann AB, Jansen van Rensburg MJ, Shaw D, et al. Changes in the incidence of invasive disease due to Streptococcus pneumoniae, Haemophilus influenzae, and Neisseria meningitidis during the COVID-19 pandemic in 26 countries and territories in the Invasive Respiratory Infection Surveillance Initiative: a prospective analysis of surveillance data. Lancet Digit Health. 2021;3:e360–e370. doi: 10.1016/S2589-7500(21)00077-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Danino D, Ben-Shimol S, van der Beek BA, et al. Decline in pneumococcal disease in young children during the coronavirus disease 2019 (COVID-19) pandemic in Israel associated with suppression of seasonal respiratory viruses, despite persistent pneumococcal carriage: a prospective cohort study. Clin Infect Dis. 2022;75:e1154–e1164. doi: 10.1093/cid/ciab1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Su C, Zhang Z, Zhao X, et al. Changes in prevalence of nosocomial infection pre- and post-COVID-19 pandemic from a tertiary hospital in China. BMC Infect Dis. 2021;21:693. doi: 10.1186/s12879-021-06396-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Geffers C, Schwab F, Behnke M, Gastmeier P. No increase of device associated infections in German intensive care units during the start of the COVID-19 pandemic in 2020. Antimicrob Resist Infect Control. 2022;11:67. doi: 10.1186/s13756-022-01108-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ahadi M, Shams AH, Yadollahi M. Effect of COVID-19 pneumonia infection control protocols on nosocomial infection incidence in trauma patients. Chin J Traumatol. 2023;26:284–289. doi: 10.1016/j.cjtee.2023.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lee SS, Viboud C, Petersen E. Understanding the rebound of influenza in the post COVID-19 pandemic period holds important clues for epidemiology and control. Int J Infect Dis. 2022;122:1002–1004. doi: 10.1016/j.ijid.2022.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Li Y, Wang X, Cong B, Deng S, Feikin DR, Nair H. Understanding the potential drivers for respiratory syncytial virus rebound during the coronavirus disease 2019 pandemic. J Infect Dis. 2022;225:957–964. doi: 10.1093/infdis/jiab606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Ankert J, Hagel S, Schwarz C, et al. Streptococcus pneumoniae re-emerges as a cause of community-acquired pneumonia, including frequent co-infection with SARS-CoV-2, in Germany, 2021. ERJ Open Res. 2023;9:00703–02022. doi: 10.1183/23120541.00703-2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Bertran M, Amin-Chowdhury Z, Sheppard CL, et al. Increased incidence of invasive pneumococcal disease among children after COVID-19 pandemic, England. Emerg Infect Dis. 2022;28:1669–1672. doi: 10.3201/eid2808.220304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Meyer Sauteur PM, Chalker VJ, Berger C, Nir-Paz R, Beeton ML. Mycoplasma pneumoniae beyond the COVID-19 pandemic: where is it? Lancet Microbe. 2022;3:e897. doi: 10.1016/S2666-5247(22)00190-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Meyer Sauteur PM, Beeton ML. Mycoplasma pneumoniae: gone forever? Lancet Microbe. 2023;4:e763. doi: 10.1016/S2666-5247(23)00182-9. [DOI] [PubMed] [Google Scholar]
- 105.Sauteur PM, Beeton ML, Pereyre S, et al. Mycoplasma pneumoniae: delayed re-emergence after COVID-19 pandemic restrictions. Lancet Microbe. 2024;5:e100–e101. doi: 10.1016/S2666-5247(23)00344-0. [DOI] [PubMed] [Google Scholar]
- 106.Foley DA, Phuong LK, Peplinski J, et al. Examining the interseasonal resurgence of respiratory syncytial virus in Western Australia. Arch Dis Child. 2022;107:e7. doi: 10.1136/archdischild-2021-322507. [DOI] [PubMed] [Google Scholar]
- 107.Baker RE, Park SW, Yang W, Vecchi GA, Metcalf CJE, Grenfell BT. The impact of COVID-19 nonpharmaceutical interventions on the future dynamics of endemic infections. Proc Natl Acad Sci USA. 2020;117:30 547–30 553. doi: 10.1073/pnas.2013182117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Mondal P, Sinharoy A, Gope S. The influence of COVID-19 on influenza and respiratory syncytial virus activities. Infect Dis Rep. 2022;14:134–141. doi: 10.3390/idr14010017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Fukuda Y, Togashi A, Hirakawa S, et al. Changing patterns of infectious diseases among hospitalized children in Hokkaido, Japan, in the post-COVID-19 era, July 2019 to June 2022. Pediatr Infect Dis J. 2023;42:766–773. doi: 10.1097/INF.0000000000003982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Kandeel A, Fahim M, Deghedy O, et al. Resurgence of influenza and respiratory syncytial virus in Egypt following two years of decline during the COVID-19 pandemic: outpatient clinic survey of infants and children, October 2022. BMC Public Health. 2023;23 doi: 10.1186/s12889-023-15880-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Murray CJ, Lozano R, Flaxman AD, et al. Using verbal autopsy to measure causes of death: the comparative performance of existing methods. BMC Med. 2014;12:5. doi: 10.1186/1741-7015-12-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
To download the data used in these analyses, please visit the GHDx GBD 2021 website.