Abstract
Background
Exercise that challenges balance is the most effective fall prevention intervention in community-dwelling older adults. Identifying factors influencing implementation of community fall prevention exercise programs is a critical step in developing strategies to support program delivery.
Objective
To identify implementation facilitators, barriers, and details reported in peer-reviewed publications on community fall prevention exercise for older adults.
Design
Scoping review.
Methods
We searched multiple databases up to July 2023 for English-language publications that reported facilitators and/or barriers to implementing an evidence-based fall prevention exercise program in adults aged 50+ years living independently. At least two reviewers independently identified publications and extracted article, implementation, and exercise program characteristics and coded barriers and facilitators using the Consolidated Framework for Implementation Research (CFIR).
Results
We included 22 publications between 2001 and July 2023 that reported factors influencing implementation of 10 exercise programs. 293 factors were reported: 183 facilitators, 91 barriers, 6 described as both a facilitator and barrier, and 13 unspecified factors. Factors represented 33 CFIR constructs across all five CFIR domains: implementation inner setting (n = 95 factors); innovation (exercise program) characteristics (n = 84); individuals involved (n = 54); implementation process (n = 40) and outer setting (n = 20). Eight publications reported implementation strategies used; 6 reported using a conceptual framework; and 13 reported implementation outcomes.
Conclusion
The high number of factors reflects the complexity of fall prevention exercise implementation. The low reporting of implementation strategies, frameworks and outcomes highlight the ongoing need for work to implement and sustain community fall prevention exercise programs.
Keywords: facilitators, barriers, balance, physical activity, synthesis, systematic review, older people
Key Points
Challenging balance exercise prevents falls in older adults, but uptake is low and few community programs meet recommendations.
293 factors influencing implementation of effective fall prevention community exercise programs have been reported in 22 studies.
Few studies have used implementation conceptual frameworks and reported implementation strategies.
Most factors represent the organizational inner setting and nature of the exercise programs
Introduction
Preventing falls and their consequences are critical for supporting health and well-being in later life [1], and new guidelines recommended that fall risk be considered in all older people [2]. For the many older people who live independently, a robust body of evidence has unequivocally indicated that exercise that targets and challenges postural balance is the most effective intervention to reduce the risk and incidence of falls [3]. In fact, when performed year-round and for three hours or more weekly, the risk can be reduced up to 42%–51% [4]. Although fall prevention strategies have traditionally focused on people aged 65 and above, new studies suggest that these should be expended to younger people, especially if balance is an issue [5].
However, uptake of balance exercise among ageing adults is low. For example, in 2020 just 16% of Canadians aged 65 and over met balance exercise recommendations for community-dwelling older adults [6]. As one strategy to support fall prevention and balance exercise recommendations, many community exercise programs exist for older people with an aim to reduce falls. Community programs are critical for meeting population needs to support health and well-being and alleviate pressure on limited health system resources. A 2019 study identified 334 community fall prevention exercise programs for older people in Canada [7]. However, in a survey completed by 140 instructors of these programs, just 6% reported program characteristics that met all criteria for effective fall prevention exercise.
Challenges with implementing evidence-informed recommendations are well-recognized throughout health and social care, and community fall prevention exercise is no exception. Implementation refers to the process of integrating evidence-informed interventions into policy and practice. The burgeoning field of implementation science that studies methods to advance systematic update of research findings can enhance evidence uptake in real word settings [8], and evidence-based implementation guidance emphasizes identifying and understanding barriers and facilitators to evidence use as a critical step in the implementation process [9].
Many factors are known to influence implementation success. For example, the Consolidated Framework for Implementation Research (CFIR), a highly used conceptual framework informed by published research, identifies 48 constructs and 19 sub-constructs within five domains to explain implementation effectiveness [10]. These five domains pertain to the ‘inner setting’– the setting where the innovation is implemented; ‘innovation’– the ‘thing’ being implemented (i.e. the exercise program); ‘individuals’– roles and characteristics of those involved; ‘outer setting’– the broader context or environment where the inner setting exists; and the ‘implementation process’– relating to the activities and strategies undertaking to implement the innovation. Understanding the factors affecting implementation and evidence use in a particular context can inform the tailoring and development of interventions to support implementation and in turn, evidence use and individual outcomes [9]. The CFIR constructs have been systematically mapped to specific implementation strategies recommended to target each construct [11], making it a useful tool for facilitating implementation planning and decision-making.
The most recent synthesis of fall prevention exercise implementation only includes data until 2013, was limited to secondary reporting of implementation factors within the primary efficacy trial, and did not analyse data with any established implementation framework [12]. We need an up-to-date analysis of factors influencing fall prevention exercise in community settings to inform evidence-informed implementation efforts to attract, adapt, implement and sustain evidence-informed community fall prevention exercise for older people. The primary aim of this study was to identify barriers and facilitators reported when implementing fall prevention exercise for older people in community settings. Our secondary aim was to describe characteristics of community fall prevention exercise implementation reported to date, including implementation strategies; conceptual frameworks used, and outcomes.
Methods
Design
We conducted a scoping review following established methodological guidance [13].
Search strategy
We developed a search strategy in collaboration with a professional librarian (HL) (Appendix 1). We searched Ovid MEDLINE, Ovid EMBASE, EBSCO AgeLine, EBSCO and SPORTDiscus from inception to July 2023 using controlled vocabulary including, (but not limited to): falls, exercise programs, knowledge translation, implementation, older adults, community residing.
Screening and eligibility criteria
Two reviewers independently completed screening after an initial calibration activity to refine processes. They met to resolve conflicts if necessary, and any outstanding conflicts were resolved by consensus or by the lead author if no consensus was reached. Publications of any design were included if they met the following inclusion criterion: (i) referred to evidence-based exercise programs demonstrated to reduce falls [i.e. references another study that shows efficacy of the program] OR met the following recommendations: include exercises that reduce the base of support, move the centre of gravity and control body positioning, standing without use of arms or as little use of upper body as possible, and are offered 3 hours per week [3]; (ii) the exercise program includes individuals aged 50 and older living independently in community; (iii) reports barriers and/or facilitators to implementation of the evidence-based exercise program; and (iv) full text published in English. We excluded reviews, articles that only reported on barriers and facilitators to program participation, and those that reported on a protocol, conference abstract, editorial, or letter to the Editor.
Data extraction, coding, and synthesis
Two reviewers independently extracted article details (authors, title, journal/DOI, date of publication, country of publication, methods, participants), exercise program details (name, population, frequency, intensity, time, type), implementation details (facilitators; barriers; strategies; conceptual frameworks; implementation outcomes) following an initial calibration exercise. We extracted any implementation facilitators and barriers reported, including from results and discussion sections. Conflicts were resolved by consensus or the lead author if needed. We coded extracted implementation barriers and facilitators with CFIR [10]. Due to the high number of CFIR codes and potential for conflicts we identified during the calibration exercise, three reviewers independently coded barriers and facilitators to CFIR domains and constructs. We used the majority for determining the final code, and resolved conflicts through consensus or the lead author when there was no majority. We coded reported implementation strategies using a peer-reviewed inventory of 73 strategies [14] and coded implementation outcomes using established definitions of ‘reach’; ‘effectiveness’; ‘adoption’; ‘implementation’; ‘maintenance’ [15] and ‘client’ outcomes [16]. We present our findings through descriptive summary statistics (i.e. counts, frequencies and proportions) and narrative description.
Results
Our search identified 4424 citations. After removing duplicates and screening, we identified 22 eligible articles and included them in our review [17–38] (Figure 1).
Figure 1.
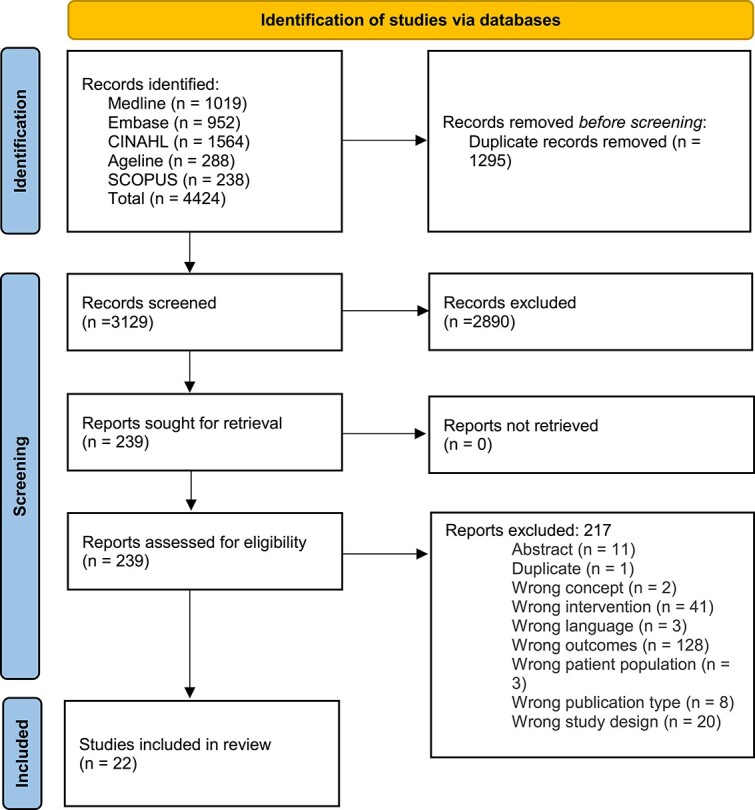
Article flow diagram.
Article details are summarized in Table 1, and described in detail in Appendix 2. The 22 papers were published between 2001 and 2023, with the majority (n = 14, 73.7%) published between 2011 and 2020. Most articles (n = 20) reported facilitators and barriers retrospectively post implementation; two articles prospectively reported barriers and facilitators to inform implementation. The articles reported on implementation of 10 exercise programs (all of which had program efficacy established in a prior peer-reviewed paper) in seven countries, all of which were high income. The most frequently implemented program was the Otago Exercise Program [n = 13 (59%)]. Exercise program details are reported in Appendix 3. The implementation setting and period varied considerably, from single sites and program delivery cycles to multi jurisdiction, multi-year implementation periods. Most articles (n = 14, 64%) reported barriers and facilitators based on data from interviews or focus groups (n = 9), surveys (n = 3) or both (n = 2). These data were obtained from program staff (n = 6), participants (n = 3) or both (n = 5). Eight articles (36%) reported facilitators and barriers in the discussion only.
Table 1.
Article characteristics
| Characteristic | Number of articles (n) | Percent (%) |
|---|---|---|
| Year of publication | ||
| 2001–2010 | 2 | 9.1% |
| 2011–2020 | 14 | 63.6% |
| 2021 – July 2023 | 6 | 27.3% |
| Country of program implemented | ||
| United States | 9 | 40.9% |
| Norway | 3 | 13.6% |
| United Kingdom | 3 | 13.6% |
| Australia | 2 | 9.1% |
| Canada | 2 | 9.1% |
| Other (Netherlands, Sweden, not specified) | 3 | 13.6% |
| Name of exercise program implemented * | ||
| Otago Exercise Program | 13 | 59.0% |
| The Tai Ji Quan: Moving for better balance | 4 | 18.2% |
| A Matter of Balance | 2 | 9.1% |
| Stay Active and Independent for Life | 2 | 9.1% |
| Other (Stand Up!; Modified Stay Safe, Stay Active; Stay Balanced; Falls Management Exercise; In Balance; Nijmegen Falls Prevention Program) | 6 | 27.3% |
| Facilitator and barrier reporting methods | ||
| Interviews or focus groups | 9 | 40.9% |
| Survey | 3 | 13.6% |
| Both | 2 | 9.1% |
| Article discussion | 8 | 36.3% |
| Facilitator and barrier data source | ||
| Older adult exercise program participants | 6 | 27.2% |
| Program staff | 3 | 13.6% |
| Both | 5 | 22.7% |
| Authors | 8 | 36.3% |
More than one option possible, may sum to more than 100%
Factors influencing community fall prevention exercise implementation.
We extracted 293 factors influencing implementing community fall prevention exercise programs for older adults from the 22 articles: 183 facilitators, 91 barriers, 6 factors described as both a barrier and facilitator, and 13 factors unspecified as a facilitator or barrier. Reported factors represented 33 CFIR constructs across all five CFIR domains (summarized in Table 2, described in detail in Appendix 4). Findings are described by CFIR domain below.
Table 2.
Reported factors influencing older adult community fall prevention exercise implementation by CFIR domain and construct
| Domain | No articles | Construct | N | Facilitator | Barrier | Both | Unspecified | Examples/Explanation |
|---|---|---|---|---|---|---|---|---|
| Inner Setting (n = 95) | 21 | Access to knowledge & information | 31 | 22 | 9 | 0 | 1 | Training manuals, workshops etc. for instructors; awareness of fall prevention for participants and staff |
| Available resources | 24 | 14 | 11 | 0 | 0 | Funding; materials; space | ||
| Structural characteristics | 16 | 9 | 6 | 0 | 0 | Physical (venue); technological; staff organization | ||
| Relational connections | 8 | 6 | 1 | 0 | 1 | Between organisations, staff &/or participants | ||
| Communications | 7 | 4 | 2 | 0 | 1 | Between organisations, staff &/or participants | ||
| Compatibility | 4 | 3 | 1 | 0 | 0 | With & between other programs & organisations | ||
| Culture | 3 | 2 | 1 | 0 | 0 | Within & between groups, especially participants | ||
| Incentive systems | 1 | 1 | 0 | 0 | 0 | Provide to complete data collection form | ||
| Mission alignment | 1 | 1 | 0 | 0 | 0 | Between stakeholders | ||
| Innovation (n = 84) | 21 | Innovation design | 57 | 41 | 14 | 1 | 1 | Home/virtual options; social setting; program timing & frequency; instructor support; language considerations; group size; exercise appropriateness; relevance |
| Innovation adaptability | 12 | 11 | 1 | 0 | 0 | Tailor, individualise; provide alternatives for varying abilities | ||
| Innovation cost | 10 | 2 | 5 | 2 | 1 | Program & participant costs | ||
| Innovation evidence-base | 4 | 4 | 0 | 0 | 0 | Evidence provides credibility | ||
| Innovation trialability | 1 | 1 | 0 | 0 | 0 | Supports program design | ||
| Individuals (n = 54) | 18 | Innovation recipients | 24 | 4 | 16 | 1 | 3 | Participant health status; motivation; priorities; transportation considerations |
| Innovation deliverers | 14 | 9 | 4 | 0 | 1 | Instructor capability & experience; confidence; demeanour | ||
| Implementation facilitators | 11 | 5 | 4 | 0 | 2 | Researchers & or other professionals as facilitators | ||
| High level leaders | 2 | 2 | 0 | 0 | 0 | Administrator/leader as facilitator | ||
| Implementation leads | 1 | 1 | 0 | 0 | 0 | Designated lead | ||
| Implementation team members | 1 | 1 | 0 | 0 | 0 | Support personnel | ||
| Other implementation support | 1 | 1 | 0 | 0 | 0 | Program staff | ||
| Implementation Process (n = 40) | 12 | Teaming | 20 | 19 | 1 | 0 | 0 | Within & between organisations; with academics |
| Engaging | 9 | 4 | 5 | 0 | 0 | Potential volunteers, referral channels, delivery sites | ||
| Assessing needs | 3 | 2 | 1 | 0 | 0 | Of programs & participants | ||
| Reflecting & evaluating | 3 | 2 | 1 | 0 | 0 | With data, testimonials, summaries | ||
| Planning | 2 | 2 | 0 | 0 | 0 | With committees & formal agreements | ||
| Tailoring strategies | 2 | 2 | 0 | 0 | 0 | For specific communities | ||
| Assessing context | 1 | 1 | 0 | 0 | 0 | With an implementation framework | ||
| Outer Setting (n = 20) | 11 | Local conditions | 7 | 0 | 1 | 0 | 1 | Seasonal; system issues; geographic |
| Partnerships & Connections | 7 | 7 | 0 | 0 | 0 | With/across organizations & or communities | ||
| Financing | 3 | 2 | 1 | 0 | 0 | Funding models | ||
| Policies & law | 2 | 0 | 2 | 0 | 0 | Liability concerns; paperwork | ||
| Critical incidents | 1 | 0 | 2 | 0 | 0 | Impact of COVID-19 pandemic |
Inner setting
Most reported factors influencing community fall prevention exercise implementation were categorized in the ‘Inner Setting’ domain. The most identified factors were coded as ‘access to knowledge and information’ (n = 31, from 14 articles), ‘available resources’ (n = 24, from 15 articles) and ‘structural characteristics’ (n = 16, from 6 articles). ‘Access to knowledge and information’ factors related primarily to the importance of instructor training, as well as staff and participant knowledge considerations (such as ensuring that older adults understand the importance of fall prevention). ‘Available resources’ related to program ‘funding’, ‘materials’ (mostly a program manual but also exercise equipment) and ‘space’. ‘Structural characteristics’ pertained to ‘work infrastructure’ issues such as staffing and coordination of tasks, ‘physical infrastructure’ considerations, and information ‘technology infrastructure’ to support programs.
Innovation
‘Innovation design’ factors were the most coded construct overall (n = 57, 15 articles). These included the relevance and applicability of the program, exercise appropriateness, program timing and frequency issues, group size, social considerations for participants, instructor support, language and communication considerations and provision of home exercise and virtual options. ‘Innovation adaptability’ (n = 12, 8 articles), was almost entirely noted as an implementation facilitator. ‘Innovation cost’ (n = 10, 8 articles), both related to program costs and participant costs, were identified.
Individuals
‘Innovation recipients’ were the most reported construct (n = 24, 13 articles) related to the ‘Individuals’ domain, and mostly described as a barrier to implementation. These factors included participant health status, competing priorities and motivation. ‘Innovation deliverers’ (n = 14, 10 articles), in particular, their ‘capability’ in leading the programs, were often reported as facilitators. ‘Implementation facilitators’ (those with subject matter expertise who assist, mentor, coach, or support implementation), were also noted (n = 11, 3 articles). In numerous cases researchers were identified and it was noted how they could enhance or detract from exercise program implementation.
Implementation process
The most frequently reported ‘implementation process’ factors included ‘teaming’ (n = 20, 11 articles) and ‘engaging’ (n = 9, 5 articles). Teaming factors related mostly to issues within programs, but in some cases noted specific considerations between researchers and programs.
Outer setting
The fewest reported factors influencing community fall prevention exercise implementation pertained to the ‘outer setting’ domain. The ‘local conditions’ construct (n = 7), was most often reported as a barrier, and the ‘partnerships and connections’ construct (n = 7), was always reported as a facilitator.
Implementation strategies, use of conceptual frameworks and outcomes
Thirteen articles (59%) reported implementation characteristics related to strategies, conceptual frameworks or outcomes (Appendix 5). Eight articles reported a total of 24 implementation strategies (range 2–11 strategies reported per study). The most frequently reported strategies were: develop educational materials (n = 4); develop a formal implementation plan (n = 3); and obtain a formal commitment (n = 3). Eight articles reported use of an implementation framework: six used an implementation determinants framework (Promoting Action in Research Implementation in Health Services (PARIHS) (n = 1), Reach, Effectiveness, Adoption, Implementation, Maintenance (RE-AIM) (n = 4) or Theoretical Domains Framework (TDF) (n = 1) to evaluate exercise program implementation; one used a classic theory (Diffusion of Innovation); and one used an academic community model to build relationships and capacity. Thirteen articles reported a total of 8 implementation outcomes (range 1–8 outcomes reported per study). The most frequently reported outcomes were: reach (n = 11); implementation- setting level (n = 8); and client outcomes (n = 8).
Discussion
This synthesis is the first to systematically identify reported factors influencing older adult community fall prevention exercise implementation and link them to established constructs from implementation science. This data can inform the development of implementation strategies and programs, advancing our ability to facilitate fall prevention exercise delivery in community settings and support healthy ageing.
The high number of factors reported (n = 293) and implementation constructs represented (n = 32) reflect the magnitude and complexity of community fall prevention exercise implementation. Although all five implementation domains included in CFIR were represented in the data, not all studies reported factors from every domain. This may reflect the fact that none of the studies used a comprehensive implementation framework to guide examination and reporting of barriers and facilitators. The distribution of reported factors weighed primarily on the inner (community exercise program) setting, innovation (exercise program) design and individuals involved, with fewer in the outer setting and implementation process domains. This pattern is understandable given that study participants primarily included program staff and older adult program participants and with few system or policy representatives and that only one study reported an implementation strategy was used.
The distribution of implementation constructs reported is critical for guiding future community fall prevention exercise implementation planning. The most reported construct overall was innovation design, indicating that the nature of the program plays an important role in its implementability. In particular, the reported factors pertaining to exercise appropriateness, program frequency, group size, social considerations for participants, instructor support, and provision of home exercise and virtual options are all actionable. Many of these design features were recognized in the previous review on fall prevention exercise implementation [12]. A key finding was the consistent reporting that innovation adaptability was a facilitator of implementation, reinforcing the need for community fall prevention exercise programs to include appropriate adaptations to meet the needs of each participant. We note recent developments in assessing and reporting balance exercise challenge [39] which may help appropriately tailor exercise adaptations for participants.
Most studies reported access to knowledge and information was also reported as a factor influencing community exercise implementation. This was most often related to instructor training and the provision of an appropriate resource manual. This is a highly actionable finding that can be readily addressed through established implementation strategies (including developing and distributing educational materials, holding meetings), but users are cautioned against education alone as an implementation strategy [40, 41]. For example, available resources and infrastructure issues were also frequently identified in this review, indicating that implementation teams need to appropriately plan for program funding and associated equipment and materials costs as well as ensure that physical, personnel and technology supports are accounted for. Studies also reported specific knowledge considerations that should be captured in training sessions, such as improving older adult participants’ awareness and understanding of the importance of fall prevention [42].
The roles and characteristics of the innovation recipients in influencing implementation, that is, the older adult participants, was reported in more than half of articles. As many of these reports addressed participant health status and considered them a barrier to implementation, the already-noted importance of program adaptability and instructor support become further apparent. The critical interaction of recipient acceptance and adherence with implementation that together influence evidence adoption has been discussed elsewhere [43]. This analysis supports the need to continue developing and implementing fall prevention exercise strategies that align with older adult preferences and values.
Although all the articles included in this review reported on factors influencing implementation of older adult community exercise programming, we note the relative paucity of implementation research theory, evidence and guidance informing reported community fall prevention exercise implementation to date. Of the 20 articles reporting retrospectively on implementation of fall prevention exercise, less than half (n = 8) reported any implementation strategy, and none reported using an implementation theory, model or framework to plan and design implementation. Although 13 articles reported an implementation outcome, there was substantial variation in reporting and no outcome was consistently reported in all papers. This is an important barrier to synthesis of fall prevention exercise implementation data. These data highlight that there remain important opportunities to increase and advance theory- and evidence- informed fall prevention exercise implementation.
We acknowledge that our review is subject to language bias because we limited included articles to those published in English. We acknowledge that the decision to use CFIR as an analytic framework affects the interpretation of our findings, and that selection of a different framework or an inductive analysis would have led to different conclusions. There is a recognized need for continued CFIR development to clarify relationships between constructs [10]. Although beyond the scope of the present review, there is potential for future studies to examine these important questions through techniques such as reflexive thematic analysis. We also recognize that coding is a subjective activity, and despite calibration and multiple analysts, that other research teams may have chosen different codes during analysis. Lastly, due to heterogeneity across publications, including use of implementation strategies and reporting of implementation outcomes, we are not able to definitively examine implementation effectiveness. Realist evaluation approaches may prove useful in future analyses to examine what works under particular conditions.
Conclusion
Published factors influencing older adult community fall prevention exercise implementation reported by program staff and recipients predominantly reflect organizational considerations and program characteristics. The findings can inform actionable strategies to support and enhance implementation efforts, and can be paired with implementation research theory and evidence to optimise effectiveness.
Supplementary Material
Acknowledgements
We thank Hal Loewen for developing the search strategy and Adham Elsherbini for support screening and extracting data.
Contributor Information
Kathryn M Sibley, University of Manitoba, Winnipeg, Canada.
Brenda Tittlemier, University of Manitoba, Winnipeg, Canada.
Faith Olarinde, University of Manitoba, Winnipeg, Canada.
Brianna K Leadbetter, University of New Brunswick, Fredricton, Canada.
Danielle R Bouchard, University of New Brunswick, Fredricton, Canada.
Declaration of Conflicts of Interest
None.
Declarations of Sources of Funding
This project was supported through funding from the Canadian Institutes of Health Research Healthy Cities Implementation Science Team grant program [Grant Reference # 185014]. K.M.S. is supported by the Canada Research Chairs Program.
References
- 1. Falls - Key Facts. World Health Organization, 2018. [Google Scholar]
- 2. Montero-Odasso M, Velde N, Martin FCet al. World guidelines for falls prevention and management for older adults: a global initiative. Age Ageing 2022; 51: afac205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sherrington C, Michaleff ZA, Fairhall Net al. Exercise to prevent falls in older adults: an updated systematic review and meta-analysis. Br J Sports Med 2017; 51: 1750–8. [DOI] [PubMed] [Google Scholar]
- 4. Tricco AC, Thomas SM, Veroniki AAet al. Comparisons of interventions for preventing falls in older adults: a systematic review and meta-analysis. JAMA 2017; 318: 1687–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Araujo CG, Souza ESCG, Laukkanen JAet al. Successful 10-second one-legged stance performance predicts survival in middle-aged and older individuals. Br J Sports Med 2022; 56: 975–80. [DOI] [PubMed] [Google Scholar]
- 6. Prince SA, Lang JJ, Colley RCet al. Strength-training and balance activities in Canada: historical trends and current prevalence. Health Promot Chronic Dis Prev Can 2023; 43: 209–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Touchette AJ, Oates AR, Menec VHet al. Design characteristics and inclusion of evidence-based exercise recommendation in fall prevention community exercise programs for older adults in Canada: a National Descriptive Self-Report Study. BMC Geriatr 2021; 21: 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Eccles MP, Armstrong D, Baker Ret al. An implementation research agenda. Implement Sci 2009; 4: 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Graham ID, Logan J, Harrison MBet al. Lost in knowledge translation: time for a map? J Contin Educ Health Prof 2006; 26: 13–24. [DOI] [PubMed] [Google Scholar]
- 10. Damschroder L, Reardon CM, Widerquist MAOet al. The updated consolidated framework for implementation research based on user feedback. Implement Sci 2022; 17: 75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Waltz TJ, Powell BJ, Fernandez MEet al. Choosing implementation strategies to address contextual barriers: diversity in recommendations and future directions. Implement Sci 2019; 14: 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Shier V, Trieu E, Ganz DA. Implementing exercise programs to prevent falls: systematic descriptive review. Inj Epidemiol 2016; 3: 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Peters MDJ, Marnie C, Tricco ACet al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth 2020; 18: 2119–26. [DOI] [PubMed] [Google Scholar]
- 14. Powell BJ, Waltz TJ, Chinman MJet al. A refined compilation of implementation strategies: results from the expert recommendations for implementing change (Eric) project. Implement Sci 2015; 10: 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Glasgow RE, Harden SM, Gaglio Bet al. Re-aim planning and evaluation framework: adapting to new science and practice with a 20-year review. Front Public Health 2019; 7. 10.3389/fpubh.2019.00064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Proctor E, Silmere H, Raghavan Ret al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health 2011; 38: 65–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Agha A, Liu-Ambrose T, Backman Cet al. Understanding the experiences of rural community-dwelling older adults in using a new Dvd-delivered Otago exercise Programme. Arthritis Rheumatol 2014; 66: S1018. 10.1002/art.38914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Amacher AE, Nast I, Zindel Bet al. Experiences of general practitioners, home care nurses, physiotherapists and seniors involved in a multidisciplinary home-based fall prevention Programme: a mixed method study. BMC Health Serv Res 2016; 16: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Aviles J, Porter GC, Estabrooks PAet al. Potential implementation of reactive balance training within continuing care retirement communities. Transl J Am Coll Sports Med 2020; 5: 51–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Burton E, Boyle EJ, O'Connell Het al. Community care staff attitudes towards delivering a falls prevention exercise intervention to community care clients. Health Soc Care Community 2021; 29: 416–24. [DOI] [PubMed] [Google Scholar]
- 21. Buttery AK, Husk J, Lowe Det al. Older People's experiences of therapeutic exercise as part of a falls prevention service: survey findings from England, Wales and Northern Ireland. Age Ageing 2014; 43: 369–74. [DOI] [PubMed] [Google Scholar]
- 22. Cederbom S, Bjerk M, Bergland A. A qualitative study exploring physical Therapists' views on the Otago exercise Programme for fall prevention: a stepping stone to “age in place” and to give faith in the future. Physiother Theory Pract 2022; 38: 132–40. [DOI] [PubMed] [Google Scholar]
- 23. Day L, Trotter MJ, Donaldson Aet al. Key factors influencing implementation of falls prevention exercise programs in the community. J Aging Phys Act 2016; 24: 45–52. [DOI] [PubMed] [Google Scholar]
- 24. Groot GCL, Fagerström L. Older Adults' motivating factors and barriers to exercise to prevent falls. Scand J Occup Ther 2011; 18: 153–60. [DOI] [PubMed] [Google Scholar]
- 25. Filiatrault J, Parisien M, Laforest Set al. Implementing a community-based falls-prevention program: from drawing board to reality. Can J Aging 2007; 26: 213–25. [DOI] [PubMed] [Google Scholar]
- 26. Fink D, Houston K. Implementing an evidence-based tai Ji Quan program in a multicultural setting: a pilot dissemination project. J Sport Health Sci 2014; 3: 27–31. [Google Scholar]
- 27. Gardner MM, Buchner DM, Robertson MCet al. Practical implementation of an exercise-based falls prevention Programme. Age Ageing 2001; 30: 77–83. [DOI] [PubMed] [Google Scholar]
- 28. Gumber L, Timmons S, Coupland Cet al. 'It is designed for everybody to find their own level and to improve Themselves'; views of older people and instructors of the falls management exercise (fame) Programme. Age Ageing 2022; 51: 1–9. [DOI] [PubMed] [Google Scholar]
- 29. Kiami SR, Sky R, Goodgold S. Facilitators and barriers to enrolling in falls prevention programming among community dwelling older adults. Arch Gerontol Geriatr 2019; 82: 106–13. [DOI] [PubMed] [Google Scholar]
- 30. Li F, Harmer P, Fitzgerald K. Implementing an evidence-based fall prevention intervention in community senior centers. Am J Public Health 2016; 106: 2026–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Li F, Harmer P, Stock Ret al. Implementing an evidence-based fall prevention program in an outpatient clinical setting. J Am Geriatr Soc 2013; 61: 2142–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Li F, Harmer P, Voit Jet al. Implementing an online virtual falls prevention intervention during a public health pandemic for older adults with mild cognitive impairment: a feasibility trial. Clin Interv Aging 2021; 16: 973–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lukaszyk C, Coombes J, Sherrington Cet al. The ironbark program: implementation and impact of a community-based fall prevention pilot program for older aboriginal and Torres Strait islander people. Health Promot J Austr 2018; 29: 189–98. [DOI] [PubMed] [Google Scholar]
- 34. Olij BF, Erasmus V, Barmentloo LMet al. Evaluation of implementing a home-based fall prevention program among community-dwelling older adults. Int J Environ Res Public Health 2019; 16. 10.3390/ijerph16061079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Shubert TE, Altpeter M, Busby-Whitehead J. Using the Re-aim framework to translate a research-based falls prevention intervention into a community-based program: lessons learned. J Safety Res 2011; 42: 509–16. [DOI] [PubMed] [Google Scholar]
- 36. Shubert TE, Smith ML, Ory MGet al. Translation of the Otago exercise program for adoption and implementation in the United States. Front Public Health 2015; 2. 10.3389/fpubh.2014.00152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Worum H, Lillekroken D, Ahlsen Bet al. Bridging the gap between research-based knowledge and clinical practice: a qualitative examination of patients and Physiotherapists' views on the Otago exercise Programme. BMC Geriatr 2019; 19: 278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. York SC, Shumway-Cook A, Silver IFet al. A translational research evaluation of the stay active and independent for life (sail) community-based fall prevention exercise and education program. Health Promot Pract 2011; 12: 832–9. [DOI] [PubMed] [Google Scholar]
- 39. Farlie MK, Keating JL, Molloy Eet al. The balance intensity scales for therapists and exercisers measure balance exercise intensity in older adults: initial validation using Rasch analysis. Phys Ther 2019; 99: 1394–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Al Zoubi FM, Menon A, Mayo NEet al. The effectiveness of interventions designed to increase the uptake of clinical practice guidelines and best practices among musculoskeletal professionals: a systematic review. BMC Health Serv Res 2018; 18: 435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Jones CA, Roop SC, Pohar SLet al. Translating knowledge in rehabilitation: systematic review. Phys Ther 2015; 95: 663–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Meekes WMA, Leemrijse CJ, Korevaar JCet al. Implementing falls prevention in primary care: barriers and facilitators. Clin Interv Aging 2022; 17: 885–902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Sibley KM, Korall AMB, Touchette AJ. Translating Fall Prevention Research into Practice. In: Sherrington C, Lord SR, Naganathan V, eds. Falls in Older People: Risk Factors, Strategies for Prevention and Implications for Practice. Cambridge, Cambridge University Press, 2021; 436–59. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


