Abstract
Objectives:
Lack of access to timely, accurate, and linguistically appropriate COVID-19 information has complicated the dissemination of evidence-based information and contributed to vaccine hesitancy among racial and ethnic minority groups in the United States. We developed community events that provided outreach, education, and access to COVID-19 vaccination to overcome vaccine hesitancy in these communities.
Methods:
Using spatial analysis techniques, we identified 3 communities with low vaccine uptake in Houston, Texas, in fall 2021; engaged 20 stakeholders from these communities via 4 focus groups to understand barriers to vaccination; and developed and implemented 3 COVID-19 vaccine education and outreach events tailored to the needs of these communities in January–March 2022. We used program evaluation surveys to assess attendee characteristics and satisfaction with the events. Vaccinated attendees also completed surveys on what motivated them to get vaccinated.
Results:
Two communities were predominantly Hispanic, and the third had an equal number of Black and Hispanic residents. Based on community stakeholder input, the study team organized 2 health fairs and 1 community festival featuring dialogue-based COVID-19 vaccine engagement in January and March 2022. Across the 3 events, a total of 865 attendees received COVID-19 education and 205 (24.0%) attendees received a COVID-19 vaccine or booster. Of 90 attendees who completed program evaluation surveys, 81 (90%) rated the outreach event as good or excellent. Of 145 attendees who completed postvaccination surveys, 132 (91%) endorsed ≥1 key program feature as motivating them to either get vaccinated or vaccinate their child that day.
Conclusion:
Community outreach events are important strategies for disseminating information, building trust, and facilitating COVID-19 vaccine uptake.
Keywords: COVID-19, vaccination, disparities, geomedicine, stakeholder-engaged research, community engagement
Racial and ethnic minority populations in the United States have high rates of COVID-19 transmission, morbidity, and mortality,1,2 which reflects health inequities rooted in the social determinants of health. 3 As the COVID-19 pandemic moves toward an endemic stage, 4 racial and ethnic disparities in COVID-19 vaccine uptake remain. 5 As of February 2023, nearly 70% of people in the United States had completed their primary COVID-19 vaccine series and 51 million bivalent booster doses had been administered. 6 However, a smaller percentage of non-Hispanic Black/African American (hereinafter, Black) people (51%) have received at least 1 COVID-19 vaccine dose as compared with Asian (73%), Hispanic (67%), and non-Hispanic White (hereinafter, White) (57%) people. 7 Uptake of COVID-19 booster shots is also low among Asian (39%), White (28%), Hispanic (24%), and Black (18%) people. 8 Unvaccinated people have higher mortality and infection rates than those receiving bivalent (mortality relative risk [RR] = 14.1; infection RR = 2.8) and monovalent (mortality RR = 5.4; infection RR = 2.8) doses. 9
Barriers to vaccine uptake vary widely among racial and ethnic groups and neighborhood or community contexts. 10 Some people are hesitant to get vaccinated because of historical social injustices or the increased politicization of science.11-13 Other people want to get vaccinated but face structural barriers such as language, transportation, and/or the inability to take time off work. 14 A systematic review found that multicomponent and dialogue-based programs directed toward racial and ethnic minority groups are effective in addressing vaccine hesitancy. 15 However, few formal evaluations of strategies to address COVID-19 vaccine uptake—particularly among racial and ethnic minority groups—have been conducted.16,17 Tailored programs that are informed by community-engaged approaches are needed. 18 At the same time, limited financial and personnel resources necessitate data-driven approaches to help local governments and organizations focus their outreach efforts.19-22
With the overall goal of reducing COVID-19 disparities, we sought to (1) use a data-driven approach to identify communities with low vaccine uptake, (2) engage stakeholders from these communities to understand barriers to vaccination, and (3) develop, implement, and evaluate COVID-19 vaccine education and outreach interventions tailored to the needs of these communities.
Methods
Design Overview
The Baylor College of Medicine Institutional Review Board approved this study (H-47505), which we conducted from August 2021 through March 2022. The study comprised 3 parts. First, we used geospatial methods to identify COVID-19 neighborhoods with low vaccine uptake in Harris County, Texas, and we selected 3 neighborhoods for outreach. Next, we used the Precede–Proceed model, which provides a multistep approach for the development and implementation of health promotion programs. 23 Community stakeholders were given a cover letter and provided verbal consent to participate in focus groups to identify determinants of lack of vaccine uptake as well as predisposing, reinforcing, and enabling factors. Based on focus group feedback, we developed 3 tailored outreach events, which we implemented and evaluated using the RE-AIM (Reach, Effectiveness, Adoption, Implementation, and Maintenance) 24 framework.
Study Setting
Located in Harris County, Texas, Houston is the fourth most populous and one of the most racially and ethnically diverse cities in the United States (45% Hispanic, 24% White, 23% Black, and 7% Asian). 25 In 2021, Harris County had 893.6 COVID-19 cases per 100 000 residents, which is high relative to other major metropolitan areas. 26 In addition, an estimated one-third of COVID-19–related deaths in Texas were caused by health disparities, 27 making Houston an ideal location in which to apply community-engaged approaches for improving COVID-19 vaccine uptake.
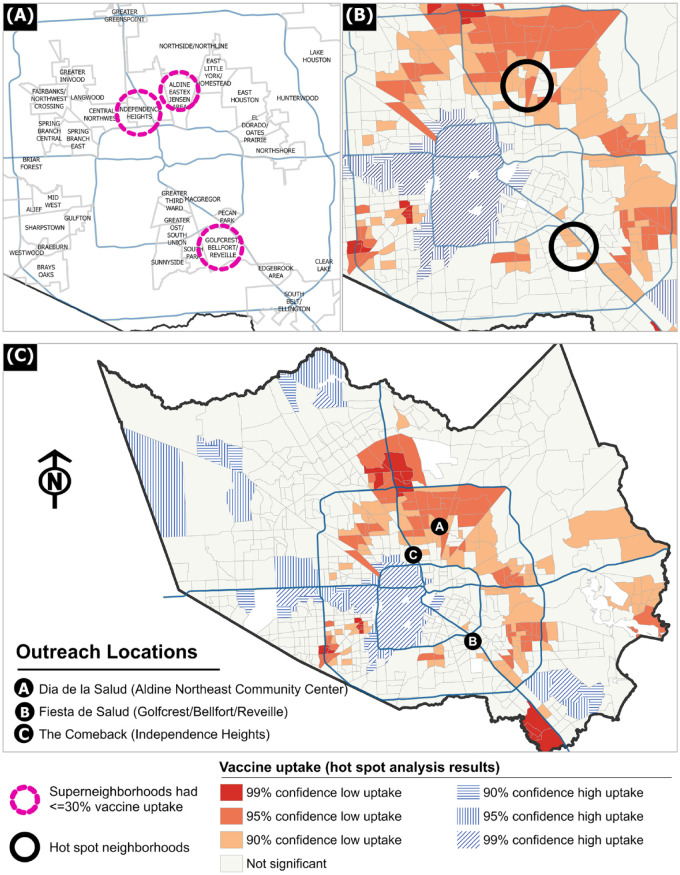
Community Identification
The Harris County Office of Science, Surveillance, and Technology provided the count and percentage of census tract residents who had been fully vaccinated as of August 10, 2021, based on the census tract population in the 2018 American Community Survey 1-year estimates. 28 To select neighborhoods in which to conduct our outreach efforts, we first identified (1) census tracts where ≤30% of residents were fully vaccinated and (2) superneighborhoods that intersected with the census tracts in which ≤30% of residents had been vaccinated (Figure 1A). A superneighborhood is a City of Houston–approved geographically designated area that groups contiguous communities that share common characteristics. 29 Next, we performed a hot-spot analysis in ArcGIS Pro (Esri) using the Getis-Ord Gi* cluster analysis method30,31 to investigate spatial dependency of vaccine uptake levels in the county. The Getis Ord Gi* is an inferential spatial pattern analysis technique grounded in probability theory. The tool calculates a z score and P value to indicate whether the null hypothesis (that observed values are randomly distributed) may be rejected. Using the P values, the tool calculates a confidence level bin for each census tract. The bin has 7 classes, ranging from −3 (99% confidence that a census tract is a cold spot) through +3 (99% confidence that a census tract is a hot spot), with 0 being not significant. (Figure 1B and C).
Figure 1.
Superneighborhoods identified for outreach based on low COVID-19 vaccine uptake, Houston, Texas, 2022. Three iterative steps were used to identify focus neighborhoods for community outreach. (A) Identify the tracts where ≤30% of the population was fully vaccinated as of August 10, 2021, and then identify the superneighborhoods that intersected the low-vaccine-uptake tracts. (A superneighborhood groups contiguous communities that share common characteristics. 29 ) (B) Perform hot-spot analysis to identify significant spatial clusters of tracts with low vaccine uptake (ie, hot spots). Several tracts on the eastern and north-central part of the county were hot spots. (C) Reach out to known/connected community stakeholders that worked in and around neighborhoods that were identified during the first step (≤30% uptake) or the second step (hot spots). Three neighborhoods were chosen for outreach based on the ability of community partner organizations to facilitate engagement with key stakeholders. Vaccination data were from the Harris County Health Department. Spatial data processing was performed in ArcGIS Pro 2.8 (Esri).
Results showed several superneighborhoods on the eastern and north-central parts of the county that intersected these hot spots (Figure 1B). We then reached out to community health workers (CHWs) and outreach organizations working in and around the identified superneighborhoods to join our scientific and community advisory board (hereinafter, advisory board). The 5-member advisory board (2 researchers and 3 community partners) selected 3 superneighborhoods for outreach on the basis of the ability of community partner organizations to facilitate our engagement with community stakeholders (Figure 1C). Two superneighborhoods were in north-central Houston (Aldine, Independence Heights), and 1 superneighborhood was in southeastern Houston (Golfcrest/Bellfort/Reveille).
Community Assessment
Four community stakeholder mini–focus groups (2 English, 2 Spanish) were conducted from September through November 2021 to assess barriers to and facilitators of vaccine uptake. Mini–focus groups (4-6 participants) offer an opportunity for all participants to speak and fully express their views and are easier to moderate than a large group is. 32 Questions included: (1) How has your community been affected by COVID-19? (2) What has your community been saying (positive or negative) about COVID-19 vaccination? (3) What are the concerns? (4) Where are people getting their information? (5) What is motivating vaccination? (6) What are the barriers to vaccination? and (7) What would you recommend to address community concerns/barriers to vaccination? Focus groups lasted for 60 minutes. They were digitally recorded, transcribed, and analyzed by using rapid qualitative analysis.33-36 We used a templated summary table to extract focus group data based on our focus group questions. 37 We consolidated summaries in a data matrix to capture themes, subthemes, and supporting quotes. 38 The principal investigator (H.B.) and 2 trained analysts (C.M.L., N.M.B.) met to discuss resulting patterns. We defined saturation as the point at which linking concepts of 2 consecutive focus groups revealed no additional second-level categories. 39
Program Development, Implementation, and Evaluation
The advisory board developed broad goals that were applied across events to
develop academic–community partnerships to gain community trust and improve vaccination uptake,
provide accurate information and education about COVID-19 vaccine,
provide vaccination education in an accessible and linguistically and culturally appropriate manner,
make COVID-19 vaccination more convenient and accessible, and
incentivize vaccination.
Metrics for success were developed in conjunction with county public health officials and community partners and were based on their experience conducting other COVID-19 public health outreach events.
1. Reach: at least 200 attendees at each event
2. Adoption: vaccinate 20% of attendees
3. Effectiveness
a. 80% of outreach event attendees who complete program evaluations will rate the event as good to excellent on a 4-point scale, where 1 = excellent, 2 = good, 3 = fair, and 4 = poor
b. 80% of outreach event attendees who complete the postvaccination survey will endorse 1 program component (ie, convenience, education, linguistic appropriateness, incentives, trust of organizers) as a motivating factor for their decision to get vaccinated or to vaccinate their children that day
4. Implementation: volunteers will rate satisfaction with logistics as 8 or higher on a 10-point scale, where 0 = not at all satisfied and 10 = extremely satisfied
Results
Community Characteristics
The racial and ethnic composition in the 3 superneighborhoods was 85.5% Hispanic and 9.3% Black in Golfcrest/Bellfort/Reveille, 87.5% Hispanic and 6.8% Black in Aldine, and 60.0% Hispanic and 31.9% Black in Independence Heights. The percentage of households living below the federal poverty level ranged from 24.4% to 38.4%, and the percentage of uninsured residents ranged from 26.8% to 34.2% (eTable in Supplemental Material).
Community Assessment
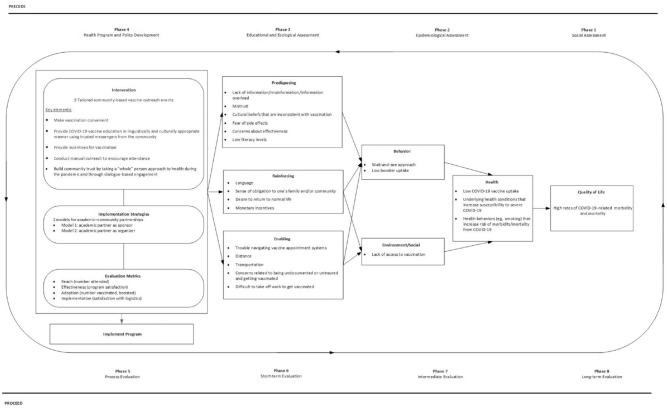
Twenty community stakeholders (70% female, aged 31-68 y), including 6 CHWs, 12 community activists, and 2 community leaders (eg, clergy, law enforcement officials), participated in the focus groups. Focus group findings mapped onto constructs of the Precede–Proceed model showed that, across focus groups, participants cited lack of access, lack of credible information sources, and adoption of a wait-and-see attitude as reasons for lack of vaccine uptake (Figure 2). Predisposing, reinforcing, and enabling factors were also identified.
Figure 2.
Summary of themes from 4 focus groups that were conducted with community stakeholders (N = 20) from September through November 2021 to assess barriers and facilitators of COVID-19 vaccine uptake in Houston, Texas, mapped onto the components of the Precede–Proceed model. 23
Community stakeholders differed on how to build community trust and their preferred event format. Those from Independence Heights wanted dialogue-based engagement with trusted messengers (ie, physicians who looked and talked like them). They preferred a festival format with carnival-style activities, food trucks, and live music. Community stakeholders from Golfcrest/Bellfort/Reveille and Aldine wanted Spanish-speaking CHWs to provide vaccine education and a format that would address the myriad health concerns of the community, in addition to the COVID-19 pandemic. To attract attendees, a health fair with a family fiesta–style theme with free food, entertainment, raffles, door prizes, and children’s activities was recommended.
Program Development
Based on community stakeholder feedback, we worked with our advisory board to develop 3 outreach events and explored 2 models of academic–community partnerships. In the first model, our community partners, Dia de la Mujer Latina and CAN DO Houston, both of which have deep ties and ongoing health outreach initiatives in the Golfcrest/Bellfort/Reveille and Independence Heights superneighborhoods, respectively, preferred to be the main organizers and “face” of the events tailored for these communities. The research team served as event sponsor and provided financial support, compensation for CHWs, bilingual education and evaluation materials, and incentives for vaccination. In the second model, the research team organized the event, supported by community partners. Harris County Precinct 2 provided the venue free of charge, assisted with publicity, and facilitated on-site vaccination and connections to local organizations and federally qualified health centers. Latino Learning Center, a local nonprofit organization, provided Spanish-speaking CHWs to conduct COVID-19 vaccine education.
Program Implementation
Fiesta de Salud was designed for Golfcrest/Bellfort/Reveille and was held at St. Paul’s Episcopal Church in January 2022. The church announced the event, and Dia de la Mujer Latina contacted attendees of their prior events to inform them about the health fair. Bilingual CHWs managed the crowd, conducted health screenings, and provided vaccine education. The Houston Health Department administered vaccinations. Health-screening activities included blood pressure and glucose screening, cervical cancer screening, vision acuity checks, and COVID-19 testing. Health resources and education focused on cancer prevention and cardiovascular health were also provided. The event also featured a taco truck with free lunch and live entertainment for children. Children who were vaccinated were entered into a raffle for an hourly bicycle giveaway, and adults and children who were vaccinated received $50 gift cards. Attendees completed a brief evaluation survey at a table next to the vaccination station and received a small promotional item (eg, pen) for their time. On the evaluation survey, respondents were asked to rate their satisfaction with the event and to indicate whether any of the program components (eg, convenience, education, linguistic appropriateness, incentives, trust of organizers) was a motivating factor for getting vaccinated.
Dia de la Salud was hosted at the Aldine Northeast Community Center in March 2022. It was publicized via press release to local media outlets in English and Spanish, flyers distributed to local businesses, and a neighborhood-canvassing campaign of 300 homes. Fifty-dollar gift cards for adults and children incentivized vaccination. Spanish-speaking CHWs provided vaccine education, and Harris County Public Health employees administered vaccinations. Health professionals from Baylor College of Medicine and the community provided health screenings (eg, glucose, hypertension, audiology, foot, dental) and first-aid demonstrations. Staff from the Dan L Duncan Comprehensive Cancer Center provided education about lung and liver cancer, colorectal cancer screening, and smoking cessation. Other events included fitness and cooking demonstrations, face painting and balloon artists, Zoomba, raffles and prizes, a mariachi band, and free tacos. Attendees who completed an evaluation survey were entered in a drawing for a $10 gift card that was held every 30 minutes.
The Comeback was held outside a local event hall in Independence Heights in March 2022. The festival was publicized on neighborhood websites and via announcements at local churches. A Zydeco band, carnival games and face painting for children, and food trucks were provided. Local youth sports teams were recognized, raffles were held, and prizes were given out. The Houston Health Department provided vaccinations, and the research team provided $50 gift cards for adults and children who got vaccinated. A Black female infectious disease physician from Baylor College of Medicine led the dialogue-based engagement segment of the program, which was called Community Conversations. A CAN DO representative moderated. The segment was divided into two 15-minute sections, with live music in between, comparable to the concept of a commercial break to keep people engaged. The physician first talked briefly about the importance of COVID-19 vaccination, and then the moderator asked questions from attendees who submitted them anonymously at a booth. A brief question-and-answer period followed. We were advised by community stakeholders and the community partner organization representative to minimize the number and type of questions asked by the research team to outreach event attendees. As a consequence, we made the decision to forego soliciting program evaluations from all attendees (as we had done in the previous 2 outreach events) and asked only those who were vaccinated to complete a modified version of the postvaccination survey, which asked whether any program components influenced their intention to get vaccinated that day.
Program Evaluation
Fiesta de Salud attracted 500 attendees and Dia de la Salud attracted 300 attendees (Table 1), and The Comeback attracted 65 attendees. Ninety attendees across all 3 events completed program evaluation surveys. Health fair attendees were primarily middle-aged (mean [SD] age = 49.9 [15.7] y), female (73%), Hispanic (98.8%), and spoke either Spanish only or Spanish and English at home (81.8%). Most were unemployed or employed part-time (67.3%) and had ≤high school diploma (56%). Most had already received at least 1 COVID-19 vaccine dose. Only 10.0% of Fiesta de Salud attendees and 8.0% of Dia de la Salud attendees cited vaccination as their reason for attendance.
Table 1.
Characteristics of adult attendees (N = 90) who completed program evaluation surveys at the Fiesta de Salud and Dia de la Salud COVID-19 outreach events in Houston, Texas, 2022 a
| Variable | Fiesta de Salud (n = 40), no. (%) | Dia de la Salud (n = 50), no. (%) |
|---|---|---|
| Age, y | ||
| Mean (SD) | 45.9 (14.6) | 54.1 (16.8) |
| Missing | 0 | 1 (2.0) |
| Sex | ||
| Male | 12 (30.0) | 11 (22.0) |
| Female | 28 (70.0) | 38 (76.0) |
| Missing | 0 | 1 (2.0) |
| Ethnicity | ||
| Hispanic | 39 (97.5) | 5 (10.0) |
| Not Hispanic | 1 (2.5) | 0 |
| Race | ||
| White | 38 (95.0) | 49 (98.0) |
| Black | 2 (5.0) | 1 (2.0) |
| Language spoken at home | ||
| Spanish only | 22 (55.0) | 10 (20.0) |
| English only | 2 (5.0) | 8 (16.0) |
| Both | 15 (37.5) | 28 (56.0) |
| Neither | 1 (2.5) | 0 |
| Missing | 0 | 4 (8.0) |
| Employment | ||
| Full-time | 11 (27.5) | 16 (32.0) |
| Part-time | 15 (37.5) | 8 (16.0) |
| Unemployed | 14 (35.0) | 20 (40.0) |
| Missing | 0 | 6 (12.0) |
| Education | ||
| Elementary/middle school | 2 (5.0) | 0 |
| Some high school | 5 (12.5) | 3 (6.0) |
| High school | 17 (42.5) | 23 (46.0) |
| Bachelor’s degree | 9 (22.5) | 6 (12.0) |
| Graduate degree | 6 (15.0) | 6 (12.0) |
| Prefer not to say | 1 (2.5) | 12 (24.0) |
| Missing | 1 (2.5) | 9 (18.0) |
| Health insurance coverage | ||
| Yes | 6 (15.0) | 36 (72.0) |
| Already vaccinated | ||
| Yes | 36 (90.0) | 45 (90.0) |
Fiesta de Salud took place at a church in January 2022 and was designed for the Golfcrest/Bellfort/Reveille superneighborhood in Houston. A superneighborhood is a City of Houston–approved geographically designated area that groups contiguous communities that share common characteristics. Bilingual community health workers conducted health screenings, and COVID-19 testing and vaccine education were provided. COVID-19 vaccines were administered at the event. Dia de la Salud took place at the Aldine Northeast Community Center in March 2022 in Houston. COVID-19 vaccine education was provided and COVID-19 vaccines were administered at the event.
Vaccination rates were 24.0% at Fiesta de Salud, 20.0% at Dia de la Salud, and 34.0% at The Comeback (Table 2). Sociodemographic characteristics of those who got vaccinated at the 2 health fairs reflected characteristics of those who completed the evaluation survey (Table 1). Those who were vaccinated at The Comeback were middle-aged (mean [SD] = 43.1 [14.0] y), female (64.3%), Black (57.1%), employed full-time (64.3%), high school graduates (92.9%), and had already received at least 1 COVID-19 vaccine dose (92.8%).
Table 2.
COVID-19 vaccines, by manufacturer and dose, given to adults and children during the Fiesta de Salud, Dia de la Salud, and The Comeback outreach events in Houston, Texas (N = 205), 2022 a
| Event | Pfizer | Moderna | Johnson & Johnson | |||||
|---|---|---|---|---|---|---|---|---|
| First dose | Second dose | Booster | First dose | Second dose | Booster | First dose | Booster | |
| Fiesta de Salud (N = 122) | ||||||||
| Adults (n = 106) | 15 (14.2) | 4 (3.8) | 41 (38.7) | 4 (3.8) | 1 (0.9) | 36 (34.0) | 0 | 5 (4.7) |
| Children (n = 16) | 15 (93.8) | 1 (6.3) | 0 | 0 | 0 | 0 | 0 | 0 |
| Dia de la Salud (N = 61) | ||||||||
| Adults (n = 42) | 3 (7.1) | 3 (7.1) | 20 (47.6) | 3 (7.1) | 3 (7.1) | 9 (21.4) | 0 | 1 (2.4) |
| Children (n = 19) | 11 (57.9) | 5 (26.3) | 3 (15.8) | 0 | 0 | 0 | 0 | 0 |
| The Comeback (N = 22) | ||||||||
| Adults (n = 14) | 1 (7.1) | 1 (7.1) | 7 (50.0) | 0 | 2 (14.3) | 3 (21.4) | 0 | 0 |
| Children (n = 8) | 5 (62.5) | 3 (37.5) | 0 | 0 | 0 | 0 | 0 | 0 |
Fiesta de Salud took place at a church in January 2022 and was designed for the Golfcrest/Bellfort/Reveille superneighborhood in Houston. A superneighborhood is a City of Houston–approved geographically designated area that groups contiguous communities that share common characteristics. Bilingual community health workers conducted health screenings, and COVID-19 testing and vaccine education were provided. COVID-19 vaccines were administered at the event. Dia de la Salud took place at the Aldine Northeast Community Center in March 2022 in Houston. COVID-19 vaccine education was provided and COVID-19 vaccines were administered at the event. The Comeback was a festival held in the Independence Heights neighborhood in Houston in March 2022. Vaccines were administered at the event, and a physician talked about the importance of vaccination and answered questions. All data are number (percentage).
Overall, 94.9% of Fiesta de Salud and 98.0% of Dia de la Salud attendees rated the events favorably. When queried about what they liked, 37.5% and 40.0% of Fiesta de Salud and 32.0% and 50.0% of Dia de la Salud attendees endorsed the variety of health services offered and education provided by the CHWs, respectively. Attendee suggestions for improvement included holding follow-up events to build trust, doing more advertising, holding longer events, and using a local food vendor. Across events, 59 of 145 people who completed postvaccination surveys (40.7%) endorsed ≥1 key program feature as motivating them to get vaccinated or vaccinate their children that day, and 106 (73.1%) endorsed ≥2 features (Table 3). The most commonly endorsed program feature was convenience, which was endorsed by 71.4%, 59.0%, and 76.8% of adults who got vaccinated and 71.4%, 47.1%, and 80.0% of adults who vaccinated their children at Fiesta de Salud, Dia de la Salud, and The Comeback, respectively.
Table 3.
Results of postvaccination surveys (N = 145) indicating the factors that prompted adults to get vaccinated or vaccinate their children against COVID-19 at the Fiesta de Salud, Dia de la Salud, and The Comeback outreach events in Houston, Texas, 2022 a
| Program features | Fiesta de Salud (Golfcrest/Bellfort/Reveille) | Dia de la Salud (Aldine) | The Comeback (Independence Heights) | |||
|---|---|---|---|---|---|---|
| Adults (n = 56), no. (%) | Kids (n = 14), no. (%) | Adults (n = 39), no. (%) | Kids (n = 17), no. (%) | Adults (n = 14), no. (%) | Kids (n = 5), no. (%) | |
| Convenience | 43 (76.8) | 10 (71.4) | 23 (59.0) | 8 (47.1) | 10 (71.4) | 4 (80.0) |
| Education | 24 (42.9) | 2 (14.3) | 7 (17.9) | 8 (47.1) | 10 (71.4) | 2 (40.0) |
| Ease of communication (language appropriate) | 29 (51.8) | 6 (42.9) | 15 (38.5) | 3 (17.6) | 1 (7.1) | 3 (60.0) |
| Incentives for vaccination | 22 (39.3) | 5 (35.7) | 10 (25.6) | 7 (41.2) | 0 | 0 |
| Trust of the event organizers | 30 (53.6) | 10 (71.4) | 11 (28.2) | 5 (29.4) | 3 (21.4) | 2 (40.0) |
| Worried about variants | 29 (51.8) | 3 (21.4) | 0 | 4 (23.5) | 0 | 2 (40.0) |
| Other | 1 (1.8) | 0 | 0 | 2 (11.8) | 0 | 0 |
Fiesta de Salud took place at a church in January 2022 and was designed for the Golfcrest/Bellfort/Reveille superneighborhood in Houston. A superneighborhood is a City of Houston–approved geographically designated area that groups contiguous communities that share common characteristics. Bilingual community health workers conducted health screenings, and COVID-19 testing and vaccine education were provided. COVID-19 vaccines were administered at the event. Dia de la Salud took place at the Aldine Northeast Community Center in March 2022 in Houston. COVID-19 vaccine education was provided and COVID-19 vaccines were administered at the event. The Comeback was a festival held in the Independence Heights neighborhood in Houston in March 2022. Vaccines were administered at the event, and a physician talked about the importance of vaccination and answered questions.
Thirty Fiesta de Salud volunteers rated satisfaction with logistics as a 9.0 of 10 (SD = 0.9). Suggestions for improvement were to hold the event at a larger location and for a longer amount of time so that people would not be turned away. Sixty-five volunteers at Dia de la Salud rated it as 9.4 of 10 (SD = 1.0). Their main feedback was to conduct more local outreach to attract unvaccinated people. Eleven volunteers at The Comeback rated satisfaction as 8.2 of 10 (SD = 1.8). Their feedback was to have more tailored advertising and incentives to attract more children and young adults to the event.
Discussion
Grounded by the Precede–Proceed model, this study identified communities with low COVID-19 vaccine uptake, engaged community stakeholders to understand barriers to and facilitators of vaccination, and worked with community partners to systematically plan, implement, and evaluate 3 COVID-19 vaccine outreach events. Across communities, stakeholders agreed that lack of access and misinformation were barriers to vaccination, but they differed in what should be done to gain community trust. Based on their feedback, 2 health fairs and 1 festival were organized. During these events, 865 people from racial and ethnic minority groups received COVID-19 education, and 205 (24%) attendees were vaccinated. More than 90% of attendees who responded to an evaluation survey rated the events favorably, and 89% of those vaccinated endorsed at least 1 program feature as encouraging vaccination. Overall, findings underscore the value of tailored community outreach events and stakeholder engagement in improving vaccine uptake. They also extend prior work by providing a formal evaluation of strategies to improve vaccine uptake.40,41
Attendance decreased over time as we implemented the 3 outreach events. Possible reasons may have been location and timing. Fiesta de Salud was held in a church in January, but Dia de la Salud and The Comeback were held in a community center and event hall, respectively, in late March after a citywide campaign to incentivize first-dose vaccination with $100 gift card incentives. Consistent with previous research, 42 our engagement of racial and ethnic minority groups in a faith-based setting may have facilitated trust. Another reason for decreased attendance over time may have been differing publicity methods. The telephone bank and neighborhood canvassing approaches appear to have been more successful than community announcements for drawing people to the events. Notably, 72.0% of children’s vaccinations were first doses and 50.0% to 63.0% of adult vaccinations were boosters. Thus, while the outreach events did not appear to attract or encourage hesitant individuals to get vaccinated, they did engage people to vaccinate their children and to receive booster doses by making vaccination convenient, offering incentives, and providing linguistically appropriate education. These factors are important given the low rates of COVID-19 booster uptake among Hispanic people and the low rates of COVID-19 vaccination among children nationwide.8,43
Strengths and Limitations
This study had several strengths. First, a data-driven approach for identifying the neighborhoods in which to conduct community outreach, coupled with a community stakeholder–informed needs assessment, resulted in maximal use of resources and tailored programs. Second, we used 2 academic–community partnership models, and both were successful. Thus, the specific model used may be less important than the development of trusting partnerships, clear communication, and equitable relationships. Third, incorporation of a formal evaluation of the tailored engagement strategies used contributes to a growing body of knowledge on effective approaches to increasing COVID-19 vaccination rates in medically underserved communities.
This study also had several limitations. First, we did not collect follow-up data, so vaccination behaviors after the outreach events are not known. Second, our sample was mostly female and middle-aged and, thus, may not be representative of neighborhood residents. Future research should examine the role that tailored outreach events play in increasing vaccination knowledge and attitudes, increasing other preventive health behaviors, and promoting full-series vaccination completion. Finally, the descriptive nature of the study precluded the establishment of cause-and-effect relationships.
Conclusion
Community outreach events are useful for disseminating information, building trust, and facilitating vaccine uptake. However, one size does not fit all, and several implementation lessons were learned. First, using a data-driven approach to identify communities in which to conduct vaccine outreach can help distribute resources effectively, but, ultimately, developing trusting partnerships, clear communication, and equitable relationships with community partners are critical to successful engagement and trust building. Second, tailored outreach strategies, informed by community stakeholder feedback, can be effective in improving vaccine uptake in medically underserved communities. Third, offering incentives and enhancing convenience may be effective strategies for increasing vaccine uptake. Possible future enhancements include collecting follow-up data to assess the impact of outreach events on attendees’ vaccination behaviors, expanding outreach efforts to reach a more diverse sample of community members, and examining the role of outreach events in promoting other preventive health behaviors.
Supplemental Material
Supplemental material, sj-docx-1-phr-10.1177_00333549231213848 for Development, Implementation, and Evaluation of Three Outreach Events to Improve COVID-19 Vaccine Uptake Among Racial and Ethnic Minority Communities in Houston, Texas, 2022 by Carmin Munoz-Lavanderos, Abiodun Oluyomi, Omar Rosales, Norvin Hernandez, Nana Mensah-Bonsu and Hoda Badr in Public Health Reports
Acknowledgments
The authors thank Chris Amos, PhD, MS, Sharmila Anandasabapathy, MD, Abigail Martinez, BA, and Regan Stigall, BA (Baylor College of Medicine); Jasmine Opusunju, DrPH (CAN DO Houston); Venus Ginés, MA (Dia de la Mujer Latina); Connie Assiff, MBA, Chara Bowie, MA, LPC-S, and Commissioner Adrian Garcia, MA (Harris County Precinct 2); and Donaji Stelzig, DrPH (Trust CHWs) for their support of this project.
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by a TX Community Engaged Alliance (CEAL) Supplement grant from the National Heart, Lung, and Blood Institute under RF 50087-2021-0309-S9 (principal investigator, H.B.) and the facilities and resources of the Dan L Duncan Comprehensive Cancer Center (P30 CA125123).
ORCID iD: Hoda Badr, PhD  https://orcid.org/0000-0002-4549-9111
https://orcid.org/0000-0002-4549-9111
Supplemental Material: Supplemental material for this article is available online. The authors have provided these supplemental materials to give readers additional information about their work. These materials have not been edited or formatted by Public Health Reports’s scientific editors and, thus, may not conform to the guidelines of the AMA Manual of Style, 11th Edition.
References
- 1. Boserup B, McKenney M, Elkbuli A. Disproportionate impact of COVID-19 pandemic on racial and ethnic minorities. Am Surg. 2020;86(12):1615-1622. doi: 10.1177/0003134820973356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rentsch CT, Kidwai-Khan F, Tate JP, et al. Patterns of COVID-19 testing and mortality by race and ethnicity among United States veterans: a nationwide cohort study. PLoS Med. 2020;17(9):e1003379. doi: 10.1371/journal.pmed.1003379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Paul A, Englert P, Varga M. Socio-economic disparities and COVID-19 in the USA. J Physics. 2021;2(3):035017. doi: 10.1088/2632-072X/ac0fc7 [DOI] [Google Scholar]
- 4. Frellick M. It’s (finally) time to stop calling it a pandemic: experts. March 17, 2023. Accessed May 3, 2023. https://www.webmd.com/covid/news/20230317/time-to-stop-calling-it-a-pandemic
- 5. Nguyen LH, Joshi AD, Drew DA, et al. Self-reported COVID-19 vaccine hesitancy and uptake among participants from different racial and ethnic groups in the United States and United Kingdom. Nat Commun. 2022;13(1):636. doi: 10.1038/s41467-022-28200-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Centers for Disease Control and Prevention. An update on the ongoing federal response to COVID 19: current status and future planning. February 8, 2023. Accessed May 3, 2023. https://www.cdc.gov/washington/testimony/2023/t20230208.htm
- 7. Hill L, Artiga S, Ndugga N. COVID-19 cases, deaths, and vaccinations by race/ethnicity as of winter 2022. March 7, 2023. Accessed May 3, 2023. https://www.kff.org/coronavirus-covid-19/issue-brief/covid-19-cases-deaths-and-vaccinations-by-race-ethnicity-as-of-winter-2022
- 8. Baker L, Phillips B, Faherty LJ, Ringel JS, Kranz AM. Racial and ethnic disparities in COVID-19 booster uptake. Health Aff (Millwood). 2022;41(8):1202-1207. doi: 10.1377/hlthaff.2022.00287 [DOI] [PubMed] [Google Scholar]
- 9. Johnson AG, Linde L, Ali AR, et al. COVID-19 incidence and mortality among unvaccinated and vaccinated persons aged ≥12 years by receipt of bivalent booster doses and time since vaccination—24 U.S. jurisdictions, October 3, 2021–December 24, 2022. MMWR Morb Mortal Wkly Rep. 2023;72(6):145-152. doi: 10.15585/mmwr.mm7206a.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Tsui J, Gee GC, Rodriguez HP, et al. Exploring the role of neighborhood socio-demographic factors on HPV vaccine initiation among low-income, ethnic minority girls. J Immigr Minor Health. 2013;15(4):732-740. doi: 10.1007/s10903-012-9736-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Thompson HS, Manning M, Mitchell J, et al. Factors associated with racial/ethnic group–based medical mistrust and perspectives on COVID-19 vaccine trial participation and vaccine uptake in the US. JAMA Netw Open. 2021;4(5):e2111629. doi: 10.1001/jamanetworkopen.2021.11629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zhang Y, Fisk RJ. Barriers to vaccination for coronavirus disease 2019 (COVID-19) control: experience from the United States. Glob Health J. 2021;5(1):51-55. doi: 10.1016/j.glohj.2021.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. King WC, Rubinstein M, Reinhart A, Mejia R. Time trends, factors associated with, and reasons for COVID-19 vaccine hesitancy: a massive online survey of US adults from January–May 2021. PLoS One. 2021;16(12):e0260731. doi: 10.1371/journal.pone.0260731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Moyce S, Velazquez M, Claudio D, et al. Exploring a rural Latino community’s perception of the COVID-19 pandemic. Ethn Health. 2021;26(1):126-138. doi: 10.1080/13557858.2020.1838456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jarrett C, Wilson R, O’Leary M, Eckersberger E, Larson HJ. Strategies for addressing vaccine hesitancy—a systematic review. Vaccine. 2015;33(34):4180-4190. doi: 10.1016/j.vaccine.2015.04.040 [DOI] [PubMed] [Google Scholar]
- 16. Marquez C, Kerkhoff AD, Naso J, et al. A multi-component, community-based strategy to facilitate COVID-19 vaccine uptake among Latinx populations: from theory to practice. PLoS One. 2021;16(9):e0257111. doi: 10.1371/journal.pone.0257111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Diaz D, Chacko S, Sperling A, et al. Assessment of digital and community-based outreach interventions to encourage COVID-19 vaccination uptake in an underserved community. JAMA Netw Open. 2022;5(6):e2217875. doi: 10.1001/jamanetworkopen.2022.17875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Betsch C, Böhm R, Chapman GB. Using behavioral insights to increase vaccination policy effectiveness. Policy Insights Behav Brain Sci. 2015;2(1):61-73. doi: 10.1177/2372732215600716 [DOI] [Google Scholar]
- 19. Muscoplat MH, Rajamani S. Immunization information system and informatics to promote immunizations: perspective from Minnesota Immunization Information Connection. Biomed Inform Insights. 2017;9:1178222616688893. doi: 10.1177/1178222616688893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Stern RJ, Rafferty HF, Robert AC, et al. Concentrating vaccines in neighborhoods with high COVID-19 burden. NEJM Catal. 2021;2(2):1-9. doi: 10.1056/CAT.21.0056 [DOI] [Google Scholar]
- 21. Maravi ME, Snyder LE, McEwen LD, DeYoung K, Davidson AJ. Using spatial analysis to inform community immunization strategies. Biomed Inform Insights. 2017;9:1178222617700626. doi: 10.1177/1178222617700626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Huber K, McClellan M. Improving immunization information sharing to support targeted COVID-19 vaccination outreach. July 6, 2021. Accessed October 11, 2022. https://healthpolicy.duke.edu/publications/improving-immunization-information-sharing-support-targeted-covid-19-vaccination
- 23. Green LW, Gielen AC, Ottoson JM, Peterson DV, Kreuter MW, Fielding JE, eds. Health Program Planning, Implementation, and Evaluation: Creating Behavioral, Environmental, and Policy Change. JHU Press; 2022. [Google Scholar]
- 24. Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999;89(9):1322-1327. doi: 10.2105/ajph.89.9.1322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. US Census Bureau. QuickFacts: Houston City, Texas; Harris County, Texas; United States. 2021. Accessed February 12, 2021. https://www.census.gov/quickfacts/fact/table/houstoncitytexas,harriscountytexas,US/RHI425219#RHI425219
- 26. City Mayors Research. American cities and COVID-19. 2022. Accessed October 11, 2022. http://www.citymayors.com/coronavirus/us-cities-covid-19-cases-2.html
- 27. Ernst SW. One-third of COVID-19 deaths in Texas are due to racial health disparities. Houston Public Media. January 15, 2021. Accessed October 11, 2022. https://www.houstonpublicmedia.org/articles/news/health-science/2021/01/15/389389/one-third-of-covid-19-deaths-in-texas-are-due-to-racial-health-disparities
- 28. US Census Bureau. 2018 American Community Survey single-year estimates. 2019. Accessed August 10, 2023. https://www.census.gov/newsroom/press-kits/2019/acs-1year.html
- 29. Qian Z. Without zoning: urban development and land use controls in Houston. Cities. 2010;27(1):31-41. doi: 10.1016/j.cities.2009.11.006 [DOI] [Google Scholar]
- 30. Ord JK, Getis A. Local spatial autocorrelation statistics: distributional issues and an application. Geogr Anal. 1995;27(4):286-306. doi: 10.1111/j.1538-4632.1995.tb00912.x [DOI] [Google Scholar]
- 31. Getis A, Ord JK. The analysis of spatial association by use of distance statistics. In: Anselin L, Rey S, eds. Perspectives on Spatial Data Analysis. Springer; 2010:127-145. [Google Scholar]
- 32. Krueger RA. Focus Groups: A Practical Guide for Applied Research. Sage; 2014. [Google Scholar]
- 33. Hamilton A. Qualitative methods in rapid turn-around health services research. 2013. Accessed July 11, 2023. https://www.hsrd.research.va.gov/for_researchers/cyber_seminars/archives/video_archive.cfm?SessionID=780
- 34. Sobo EJ, Simmes DR, Landsverk JA, Kurtin PS. Rapid assessment with qualitative telephone interviews: lessons from an evaluation of California’s Healthy Families program & Medi-Cal for Children. Am J Eval. 2003;24(3):399-408. doi: 10.1016/S1098-2140(03)00053-5 [DOI] [Google Scholar]
- 35. Koenig CJ, Abraham T, Zamora KA, et al. Pre-implementation strategies to adapt and implement a veteran peer coaching intervention to improve mental health treatment engagement among rural veterans. J Rural Health. 2016;32(4):418-428. doi: 10.1111/jrh.12201 [DOI] [PubMed] [Google Scholar]
- 36. Leslie M, Paradis E, Gropper MA, Reeves S, Kitto S. Applying ethnography to the study of context in healthcare quality and safety. BMJ Qual Saf. 2014;23(2):99-105. doi: 10.1136/bmjqs-2013-002335 [DOI] [PubMed] [Google Scholar]
- 37. Miles MB, Huberman AM, Saldana A. Qualitative Data Analysis: A Methods Sourcebook. Sage; 1994. [Google Scholar]
- 38. Averill JB. Matrix analysis as a complementary analytic strategy in qualitative inquiry. Qual Health Res. 2002;12(6):855-866. doi: 10.1177/104973230201200611 [DOI] [PubMed] [Google Scholar]
- 39. Guest G, Namey E, McKenna K. How many focus groups are enough? Building an evidence base for nonprobability sample sizes. Field Methods. 2017;29(1):3-22. doi: 10.1177/1525822X16639015 [DOI] [Google Scholar]
- 40. Peteet B, Belliard JC, Abdul-Mutakabbir J, Casey S, Simmons K. Community–academic partnerships to reduce COVID-19 vaccine hesitancy in minoritized communities. EClinicalMedicine. 2021;34:100834. doi: 10.1016/j.eclinm.2021.100834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. AuYoung M, Rodriguez Espinosa P, Chen WT, et al. Addressing racial/ethnic inequities in vaccine hesitancy and uptake: lessons learned from the California alliance against COVID-19. J Behav Med. 2023;46(1-2):153-166. doi: 10.1007/s10865-022-00284-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Islam N, Patel S. Best practices for partnering with ethnic minority–serving religious organizations on health promotion and prevention. AMA J Ethics. 2018;20(7):E643-E654. doi: 10.1001/amajethics.2018.643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Liu Y, Bruine de, Buin W, Kapteyn A, Szilagyi PG. Role of parents’ perceived risk and responsibility in deciding on children’s COVID-19 vaccination. Pediatrics. 2023;151(5):e2022058971. doi: 10.1542/peds.2022-058971 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-phr-10.1177_00333549231213848 for Development, Implementation, and Evaluation of Three Outreach Events to Improve COVID-19 Vaccine Uptake Among Racial and Ethnic Minority Communities in Houston, Texas, 2022 by Carmin Munoz-Lavanderos, Abiodun Oluyomi, Omar Rosales, Norvin Hernandez, Nana Mensah-Bonsu and Hoda Badr in Public Health Reports