Abstract
Background
The HIV epidemic continues to be a major public health challenge worldwide, particularly in sub-Saharan African countries such as Ethiopia. Community-based antiretroviral refill groups are emerging as a patient-centered approach, but there is limited evidence. Therefore, this study aimed to assess attrition and predictors in community antiretroviral refill groups among ART users in Eastern Ethiopia.
Methods
Institutional-based retrospective cohort study was conducted. Systematic random sampling techniques were used. Data were collected via Kobo Collect and exported to Stata. Statistically significant effects were assumed for a P-value < 0.05 at a confidence interval of 95%.
Results
The incidence of attrition in community-based ART refill groups was 6.63 (95% CI: 5.78, 7.48) per 100 person-years. The median duration of months in CAGs from the start till the end of the follow-up period was 9 months (IQR = 24). Thus, recruitment level from health facilities, history of LTFU, and stage IV were statistically significant variables.
Conclusion
The findings of this study highlight the importance of improving the use of community antiretroviral groups in care. Healthcare programs can ultimately improve health outcomes for individuals living with HIV.
Keywords: attrition, community ART groups, predictors
Background
The HIV epidemic remains a global public health threat, with an estimated 37 million people living with HIV worldwide, 24.4 million in Sub-Saharan African countries, and Ethiopia, approximately 60% of PLHIV know their status.1,2 Of the 37 million people estimated to be living with HIV globally, approximately 62% are on life-saving antiretroviral therapy3 and 53% are virally suppressed. 4 The prevalence of antiretroviral treatment(ART) failure was 15.9%. 5 ART plays a crucial role in managing HIV by reducing viral load, morbidity, mortality, and transmission. 6 There is presently no cure for HIV. However, it can be manageable with life-long antiretroviral therapy by patient-centered approaches to ART delivery, a strategy termed differentiated service delivery models (DSDM) therapy. 3 The community-based ART model is one of the DSDM strategies for stable ART clients, who aim to provide a more client-centered approach to HIV care and treatment. 7 In sub-Saharan Africa, 8 two community ART delivery models exist: group models managed by clients and individual models overseen by health facilities. In the group models, PLHIV self-organizes groups and represents each other to collect ART refills. The use of these two models has been associated with high retention and favorable clinical outcomes however, community Art refill groups (CAGs) are more recommendable.4,9,10 CAGs are more recommendable for stable ART patients who live in the same geographic area and have agreed to join the group. Each group will consist of 6 to 12 individuals who will pick up their ART refill outside of a medical institution.11,12
Though, Ethiopia has implemented decentralization of services and task shifting of ART delivery service through community ART group refill approach and the model is a critical step in treating people living with HIV, there is limited evidence about the attrition of ART clients in this model, particularly in the study area. Therefore, this study aimed to assess attrition and its predictors in community antiretroviral ART refill groups among ART users in Eastern Ethiopia.
Methods
Study Design and Setting
The study was conducted in public health facilities of Dessie, Eastern Ethiopia. Dessie is located 401 kilometers away from Addis Ababa. 6 It has five health facilities for serving community ART refill delivery service and there were a total of 6306 HIV positive clients enrolled in ART service. 11
Study Design and Period
Institutional-based retrospective cohort study design was conducted from January 1, 2021, to December 31, 2023.
Population
All HIV-positive adult clients on ART receiving care in CAGs at Dessie public health facilities were the source population. Those whose age ≥ 18 years enrolled in CAGs between January 1, 2021, and December 31, 2023, were the study population. Those who didn’t receive their first ART refill in the group and missed their refill appointment for more than 3 consecutive months were excluded from the study.
Sample Size and Sampling Procedure
The sample size was determined by using a single population proportion formula with 95% confidence level, 5% margin of error, and 50% (rules of thumb) since there is no previous study was conducted in the study area. With 10% contingency, the final sample size was 423.
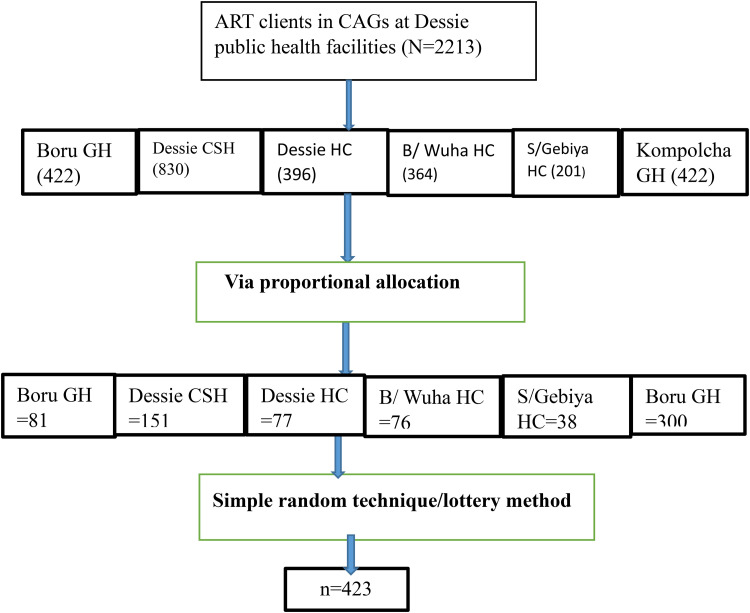
Based on the city administration health department report, approximately 2213 PLHIV were enrolled in CAGs in six health facilities. Due to the different numbers of clients in each health facility, the proportional allocation was done based on the medical records between January 01, 2021 and December 31, 2023. Finally, from the selected cards in each facility, a simple random sampling technique (lottery methods) was used (Figure 1).
Figure 1.
Schematic presentation of the sampling procedure for CAG model attrition among ART users in public health facilities in Eastern Ethiopia, 2023.
Measurements of Variables
Attrition: Was defined as the number of participants documented as either died, lost, stopped/ participant known to be alive and retained in care, but temporarily discontinued taking ART from CAGS due to medical or personal reasons. 13
Stable Clients: WHO defined clinical stability as being on ART for at least 12 months and most recent VL < 1000 or in the absence of VL, CD4 count should be > 200, ideally through viral load monitoring. 9
Virological suppression: Was defined as when PLHIV VL count less than 1000 copies per ml. 14
Event: The amount of PLHIV stayed in their CAGs
Time: The time in months when PLHIV staying in their initial CAGs.
Data Collection Procedure
Data were collected from five health facilities using medical registration of clients’ files. The instrument was developed by reviewing different literature and modified to the local context. The questionnaire consisted socio socio-demographic questions, clinical questions, and personal related questions. Five data collectors who were BSC nurses and one BSC nurse supervisor were assigned. After the client records had been first observed, an appropriate data extraction format was prepared.
Data Duality Assurance
The data extraction tool was pre-tested on twenty-two client files was done. The data collectors were trained for two days about data collection techniques. All collected data was checked for completeness every day. Consistency was examined through a random selection of cards by the principal investigator and cross-checked for their similarity.
Data Management, and Analysis
The filled questionnaires were exported from the open data kit/ODK to STATA version 16 for further analysis. Descriptive and summary statistics were presented in the form of text and tables. Chi-square assumption and multicollinearity (using VIF) were checked. The Cox proportional hazards model was performed to identify the variables that predicted post-CAG attrition. Multivariate Cox regression models were used to identify predictor variables with a p-value < 0.05.
Results
In the study, a total of 423 respondents with a mean age of 40.90 (SD ± 8.12) years were included. The majority of the respondents, 319 (75.11% had community recruitment levels. Two-thirds, 285(67.38%) respondents had ART regimen change (Table 1).
Table 1.
Demographic, Clinical, and Personal Characteristics of Respondents in CAGs among ART Users in Public Health Facilities of Eastern Ethiopia, 2023.
| Variables | Categories | Frequency | Percentage (%) |
|---|---|---|---|
| Age (years) | 18–24 | 154 | 36.41 |
| 25–67 | 260 | 61.47 | |
| ≥68 | 9 | 2.13 | |
| Sex | Male | 105 | 24.82 |
| female | 318 | 75.18 | |
| Marital status | married | 144 | 34.04 |
| unmarried | 279 | 65.96 | |
| Educational status | Can’t read and write | 57 | 13.48 |
| Can to read & write | 55 | 13.00 | |
| 1–8 grade | 114 | 26.95 | |
| 9–12 grade | 148 | 34.99 | |
| College and above | 49 | 11.58 | |
| Previous residency | Rural | 155 | 36.64 |
| Urban | 268 | 63.36 | |
| Recruitment level | Community | 319 | 75.11 |
| Health facility | 105 | 24.59 | |
| Distance from health facility | <5km | 160 | 37.83 |
| ≥5 km | 263 | 62.17 | |
| Group size | <3 | 12 | 3.31 |
| 3–12 | 396 | 93.62 | |
| >12 | 13 | 3.07 | |
| Viral load outcome | Suppressed | 104 | 24.59 |
| Unsuppressed | 279 | 65.96 | |
| Missed* | 40 | 9.46 | |
| WHO clinical stage | Stage I | 100 | 23.64 |
| Stage II | 101 | 23.88 | |
| Stage III | 129 | 30.49 | |
| Stage V | 93 | 21.99 | |
| ART regimen change | No | 138 | 32.62 |
| Yes | 285 | 67.38 | |
| History of LTFU | No | 134 | 31.68 |
| yes | 289 | 68.32 | |
| Duration on ART (years) | ≥ 5 | 104 | 24.59 |
| < 5 | 319 | 75.41 |
Key: Missed = viral load not detected by test used.
Incidence of Attrition and its Predictors
In this study, the incidence of attrition was 6.63 (95% CI: 5.78, 7.48) per 100 person-years. The median duration of months in CAGs from the start till the end of the follow-up period was 9 months (IQR = 24).
The study indicated that the recruitment level from health facilities was 39% times less likely to undergo attrition as compared to the community recruitment level [AHR = 0.61, 95% CI, 0.42, 0.90]. Respondents with no history of LTFU were 59% times less likely to undergo attrition as compared to their counterparts [AHR = 0.41, 95% CI, 0.09, 0.54]. The risk of attrition among those with stage IV was 1.13 times more likely as compared to those on WHO stage I [AHR = 1.13, 95% CI, 1.04, 3.76] (Table 2).
Table 2.
Factors Associated with Attrition of CAGs among ART Users in Public Health Facilities at Dessie, Eastern Ethiopia, 2023.
| Attrition in CAGs | CHR [95% CI] | AHR [95% CI] | |||
|---|---|---|---|---|---|
| Variables | Category | Yes | No | ||
| Age (in years) | 18–24 | 81 | 73 | 1.00 | 1.00 |
| 25–67 | 149 | 11 | 0.08 [0.32, 1.89] | 0.13 [0.32, 1.89] | |
| >68 | 7 | 2 | 2.10 [0.34, 3.83] | 0.64 [0.31, 4.72] | |
| Marital status | Unmarried | 150 | 129 | 1.00 | 1.00 |
| Married | 82 | 62 | 0.87 [0.40, 4.90] | 0.11 [0.31, 3.92] | |
| Recruitment level | Community | 192 | 127 | 1.00 | 1.00 |
| Health facility | 40 | 64 | 2.41 [0.80, 7.90] ** | 0.61 [0.42, 0.90] * | |
| History of LTFU | Yes | 71 | 63 | 1.00 | 1.00 |
| No | 161 | 128 | 0.89 [0.12, 0.90] ** | 0.41 [0.09, 0.54] * | |
| ART regimen change | No | 74 | 64 | 1.00 | 1.00 |
| Yes | 158 | 127 | 0.92 [0.39, 0.97] ** | 0.44 [0.28, 1.93] | |
| Viral load outcome | Suppressed | 60 | 44 | 1.00 | 1.00 |
| Unsuppressed | 143 | 136 | 1.29 [1.10, 3.95] ** | 1.11 [0.22, 3.55] | |
| Missed | 29 | 11 | 0.51 [0.10, 4.95] | 0.11 [0.02, 2.65] | |
| WHO clinical stage | Stage I | 68 | 32 | 1.00 | 1.00 |
| Stage II | 55 | 46 | 1.77 [1.05, 2.23] ** | 1.13 [0.94, 4.76] | |
| Stage III | 59 | 70 | 2.52 [0.85, 7.23] | 2.13 [0.64, 4.76] | |
| Stage V | 50 | 43 | 1.82 [1.05, 5.23] ** | 1.13 [1.04, 3.76] * | |
Key: ** = P < 0.25, * = p-value <0.05, CHR = Crude Hazard Ratio, AHR: Adjusted Hazard Ratio, CI = Confidence Interval &1.00= Reference.
Discussion
The declining retention rates observed over time highlight the challenges in maintaining long-term adherence to treatment in community ART groups. 15 Our study showed that the incidence of attrition was 6.63 per 100 person-years This finding is supported by previous research highlighting the challenges of sustaining retention in care among ART users in community settings. 14 Because this study highlights the importance of addressing aggressiveness in community ART groups, the need for interventions to improve retention in these groups is further emphasized.
Recruitment level was found to be a significant predictor of attrition, with a lower risk observed among health facilities recruited. This finding suggests that individuals recruited from health facilities may have better access to care and support, leading to improved retention rates in community ART groups. Additionally, the Ministry of Health rolled out a plan for the scale-up of CAGs in the community to offer psychosocial support and they are comfortable rather than recruited from the health facilities. 16
Respondents with no history of LTFU were found to have a significantly lower likelihood of attrition compared to those with a history of LTFU. This finding suggests that individuals who have previously not experienced loss to follow-up may have a heightened awareness of the importance of adherence and engagement in care, leading to improved retention rates. 17
Furthermore, the study identified that individuals in the advanced WHO clinical stage (Stage IV) had a higher risk of attrition compared to those in the early stages. This finding highlights the need for targeted interventions and support for individuals with advanced disease stages to ensure their continued engagement in care. 18 Based on the study findings, it is recommended that healthcare programs and policymakers prioritize interventions targeted at the identified risk factors on improving CAGs, updating CAG recruiting levels, enhancing virologic monitoring, and providing continuous support and counseling. 19
Strengths and Limitations of the Study
This study assessed different predictors of attrition among ART users and contributed to the robustness and applicability of the study findings, making them valuable for future interventions to improve care and treatment from CAGs. However, the cross-sectional study design limits our ability to establish a causality effect.
Conclusion
Our study findings underscore the importance of targeted interventions to enhance long-term adherence to treatment. By addressing specific risk factors such as recruitment level, history of LTFU, and clinical stage, healthcare programs can design and implement interventions that promote sustained engagement in care for individuals living with HIV. These interventions may include strengthening recruitment processes, addressing loss to follow-up, tailoring support for advanced disease stages, and implementing continuous monitoring and evaluation.
Abbreviation
- ART
Antiretroviral Therapy
- CAG
Community ART refill Group
- DSDM
Differentiated Service Delivery Model
- HIV
Human immune-deficiency virus
- LTFU
Lost to Follow-up,
Footnotes
Authors’ Contribution: Conceptualization: LA, AE & SDK, data curation: LA & ETA, formal analysis: LA, AA & EBE, investigation: LA, TWT & CD, methodology: LA, EMG & FDB, software LA, MA & AMM, validation: LA & AAT, visualization: LA, YT & AK, writing original draft: LA, KMA & NK, writing review & editing: LA & AM. All authors contributed to the article and approved the submitted version accordingly based on the above descriptions.
Availability of Data and Materials: All necessary data are included in this manuscript
Ethical Approval and Informed Consent: The Ethical Review Committee of the College of Medicine and Health Sciences, Wollo University had secured the ethical clearance letter (approval #CMHS806). The study involved the analysis of de-identified patient data extracted from medical charts at public health facilities in Dessie. As this was a retrospective study using secondary data from patient charts, individual informed consent was not required. The data was anonymized before analysis to protect patient confidentiality.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Lakew Asmare https://orcid.org/0009-0006-0455-9460
References
- 1.Bedaso W. Prevalence and associated factors of HIV among family members of index cases on chronic HIV care at west Arsi Zone. HUCMHS; 2021. [Google Scholar]
- 2.Melak D, Bayou FD, Yasin H, et al., eds. Virological suppression and its predictors among HIV/AIDS patients on antiretroviral therapy in Ethiopia: Systematic review and meta-analysis. Open Forum Infect Dis 2024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Decroo T, Koole O, Remartinez D, et al. Four-year retention and risk factors for attrition among members of community ART groups in Tete, M Mozambique. Trop Med Int Health. 2014;19(5):514‐521. [DOI] [PubMed] [Google Scholar]
- 4.Grimsrud A, Bygrave H, Doherty M, et al. Reimagining HIV service delivery: the role of differentiated care from prevention to suppression. J Int AIDS Soc. 2016;19(1):21484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tadesse AW, Mohammed Z, Foster N, et al. Evaluation of implementation and effectiveness of digital adherence technology with differentiated care to support tuberculosis treatment adherence and improve treatment outcomes in Ethiopia: A study protocol for a cluster randomised trial. BMC Infect Dis. 2021;21(1):1‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Organization WH. Guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV. World Health Organization; 2015. [PubMed] [Google Scholar]
- 7.Arage G, Tessema GA, Kassa H. Adherence to antiretroviral therapy and its associated factors among children at South Wollo Zone Hospitals, northeast Ethiopia: a cross-sectional study. BMC Public Health. 2014;14(1):365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Keefer P, Khemani S. 2016. When do Legislators pass on “Pork”? the determinants of legislator utilization of a constituency development fund in India. When Do Legislators Pass On “Pork”? The Determinants of Legislator Utilization of a Constituency Development Fund in India: Keefer, Philip| uKhemani, Stuti: [Sl]: SSRN.
- 9.Organization WH. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: recommendations for a public health approach. World Health Organization; 2016. [PubMed] [Google Scholar]
- 10.Rosen S, Grimsrud A, Ehrenkranz P, Katz I. Models of service delivery for optimizing a patient’s first six months on antiretroviral therapy for HIV: An applied research agenda. Gates Open Research. 2020;4:116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grimsrud A, Sharp J, Kalombo C, Bekker LG, Myer L. Implementation of community-based adherence clubs for stable antiretroviral therapy patients in Cape Town, South Africa. J Int AIDS Soc. 2015;18(1):19984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dakum P, Ajav-Nyior J, Attah TA, et al. Effect of community antiretroviral therapy on treatment outcomes among stable antiretroviral therapy patients in Nigeria: A quasi experimental study. PloS one. 2021;16(4):e0250345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nimwesiga C, Taremwa IM, Nakanjako D, Nasuuna E. Factors associated with retention in HIV care among HIV-positive adolescents in public antiretroviral therapy clinics in ibanda district, rural south Western Uganda. HIV/AIDS-Research and Palliative Care. 2023;15:71‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Melku M, Abebe G, Teketel A, et al. Immunological status and virological suppression among HIV-infected adults on highly active antiretroviral therapy. Environ Health Prev Med. 2020;25(1):1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hoffmann CJ, Mabuto T, McCarthy K, Maulsby C, Holtgrave DR. A framework to inform strategies to improve the HIV care continuum in low-and middle-income countries. AIDS Educ Prev. 2016;28(4):351‐364. [DOI] [PubMed] [Google Scholar]
- 16.Torpey KE, Kabaso ME, Mutale LN, et al. Adherence support workers: a way to address human resource constraints in antiretroviral treatment programs in the public health setting in Zambia. PloS one. 2008;3(5):e2204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gesesew HA, Ward P, Hajito KW, Feyissa GT, Mohammadi L, Mwanri L. Discontinuation from antiretroviral therapy: a continuing challenge among adults in HIV care in Ethiopia: A systematic review and meta-analysis. PloS one. 2017;12(1):e0169651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Biru M, Hallström I, Lundqvist P, Jerene D. Rates and predictors of attrition among children on antiretroviral therapy in Ethiopia: a prospective cohort study. PloS one. 2018;13(2):e0189777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Amosu AM. Texila International Journal Of Public Health.