Abstract
Background
Newborns with hypoxemia often require life-saving respiratory support. In low-resource settings, it is unknown if respiratory support is delivered more frequently to term infants or preterm infants. We hypothesized that in a registry-based birth cohort in 105 geographic areas in seven low-and middle-income countries, more term newborns received respiratory support than preterm newborns.
Methods
This is a hypothesis-driven observational study based on prospectively collected data from the Maternal and Newborn Health Registry of the NICHD Global Network for Women’s and Children’s Health Research. Eligible infants enrolled in the registry were live-born between 22 and 44 weeks gestation with a birth weight ≥400 grams and born from January 1, 2015 to December 31, 2018. Frequency data were obtained to report the number of term and preterm infants who received treatment with oxygen only, CPAP, or mechanical ventilation (MV). Test for trends over time were conducted using robust Poisson regression.
Results
177,728 (86.3%) infants included in this study were term and 28,249 (13.7%) were preterm. A larger number of term infants (n=5,108) received respiratory support compared to preterm infants (n=3,287). Receipt of each mode of respiratory support was more frequent in term infants. The proportion of preterm infants who received respiratory support (11.6%) was higher than the proportion of term infants receiving respiratory support (2.9%, p < 0.001). The rate of provision of respiratory support varied between sites.
Conclusions
Respiratory support was more frequently used in term infants expected to be at low risk for respiratory disorders compared to preterm infants.
Keywords: Infants, respiratory distress, low birth weight, low-resource setting, low- and middle-income countries, preterm infants
Introduction
Respiratory distress is a common sign of illness in newborn infants. Sick newborns with hypoxemia require oxygen supplementation, and those who develop respiratory failure may need life-saving respiratory support, including continuous positive airway pressure (CPAP) and/or mechanical ventilation. The need for respiratory support is more common in preterm infants compared to term infants, and decreasing gestational age is associated with higher respiratory morbidity. [1–6] In high-resource settings, the majority of infants who receive respiratory support are preterm infants, even though term birth is more common occurring in about 90% of newborns overall. [1–4, 7] However, in low-resource settings, it is unknown if respiratory support is delivered more frequently to term infants who are less likely to need respiratory support or to preterm infants who are fewer but at higher risk of respiratory disease.
Preventable neonatal deaths in low-resource settings may result from variable access to and low utilization of respiratory support. [8] The World Health Organization (WHO) recommends using supplemental oxygen and CPAP to treat neonatal respiratory disease; however, respiratory support therapies are not ubiquitously provided nor available in many rural settings. [9,10] In a two-year observational study of infants presenting to rural hospitals in Papua New Guinea, only 30% of all infants with signs of severe respiratory distress were treated with oxygen. [11] Similarly, only 55% of hospitalized neonates (0–28 days after birth) with hypoxemia were treated with oxygen during an intervention to improve oxygen systems in 12 hospitals in Nigeria. [12] In low-resource settings, the presence of respiratory disease does not guarantee receipt of or access to respiratory support. [11,12] There are no population-based studies that evaluate the distribution of respiratory support between term and preterm infants in low-and middle-income countries (LMICs). [13] Knowledge of the epidemiology of respiratory support receipt in low-resource settings will help address questions about access and use of respiratory support resources.
We hypothesized that the number of term babies receiving respiratory support would be larger than the number of preterm babies receiving such support, but that proportion of preterm infants who received respiratory support would be higher than that of term infants.
Methods
We used the Eunice Kennedy Shriver National Institute of Child Health and Human Development Global Network for Women’s and Children’s Health Research (Global Network)’s Maternal Newborn Health (MNH) Registry to describe the frequency and type of respiratory support received by term and preterm infants. The Registry is an ongoing large registry-based cohort of infants born in predominantly rural locations within LMICs. The methods of data collection for the MNH Registry have been published previously. [14] Study clusters within these countries are defined by geographical areas that report 300–500 deliveries annually. A data collection infrastructure is used to track the pregnancy and neonatal outcomes of all pregnant women who live or deliver within the clusters. For this secondary data analysis, we used data from all seven of the active MNH Registry sites in six countries - the Democratic Republic of the Congo (DRC), Guatemala, India (two sites), Kenya, Pakistan, and Zambia. The study period was from January 1, 2015 to December 31, 2018 as respiratory support data were collected in the registry for this period. For trend analysis, only clusters continuously part of the MNH Registry during the study period were included in the analysis. 10 out of 115 clusters were excluded for non-continuous enrollment in the Global Network during the study period.
The study population included live-born infants with gestational ages between 22 and 44 weeks and birthweights ≥400 grams. Gestational age was determined in two ways, and a separate analysis was completed for each. First, gestational age was determined by the Global Network gestational age algorithm that estimates gestational age from the most reliable variable using the following hierarchy of reliability: 1) gestational dating ultrasound completed at any time during the pregnancy (with preference to the earliest exam), 2) date of last menstrual period if menses are regular, and 3) neonatal examination based on clinical assessment of care provider. Second, we restricted the analysis to only infants with gestational age confirmed by a first- or second-trimester fetal ultrasound. Term birth was defined as ≥37 weeks gestational age and preterm birth was defined as <37 weeks gestational age. Infants with missing data for gestational age, birthweight, or receipt of respiratory support therapies (oxygen only, CPAP, and/or mechanical ventilation) were excluded.
The primary outcome was receipt of respiratory support defined as receipt of oxygen only (via small caliber oxygen tubing), CPAP, or mechanical ventilation. Advanced respiratory support was defined as CPAP or mechanical ventilation. Respiratory support received was coded by highest level of support received.
Statistical analysis
Frequency data were obtained to report the number of term and preterm infants who received treatment with oxygen only, CPAP, or mechanical ventilation. The proportion of term and preterm infants who received any and each type of respiratory support was calculated. The frequency of receipt of any and each type of respiratory support was also obtained for each gestational age ≥22 weeks and ≤44 weeks. The frequency and proportion of receipt of any and each type of respiratory support by term and preterm infants were analyzed by site.
The frequency and proportion of receipt of any and each type of respiratory support by preterm and term infants each year were calculated. Poisson regression with variance estimators determined relative risk and 95% confidence intervals for the change per year in the number of term and preterm infants receiving each of the respiratory support adjusting for the site.
Test for trends were conducted using robust Poisson regression while adjusting for cluster as a random effect. The two-sided significance threshold was set at 0.05. All analyses were conducted with the use of SAS software, version 9.4 (SAS Institute).
The sample size was sufficient to report numbers and proportions of term and preterm infants who receive respiratory support based on the expectation that around 5% of infants received some type of respiratory support and around 15% would be born preterm. These assumptions were based on data collected within the Global Network prior to the study period.
Results
A total of 105 clusters within the Global Network sites were included in the analysis. During the study period, 205,977 infants met inclusion criteria (Figure 1). 177,728 (86.3%) infants included were born at term and 28,249 (13.7%) were born preterm (Table 1).
Figure 1:
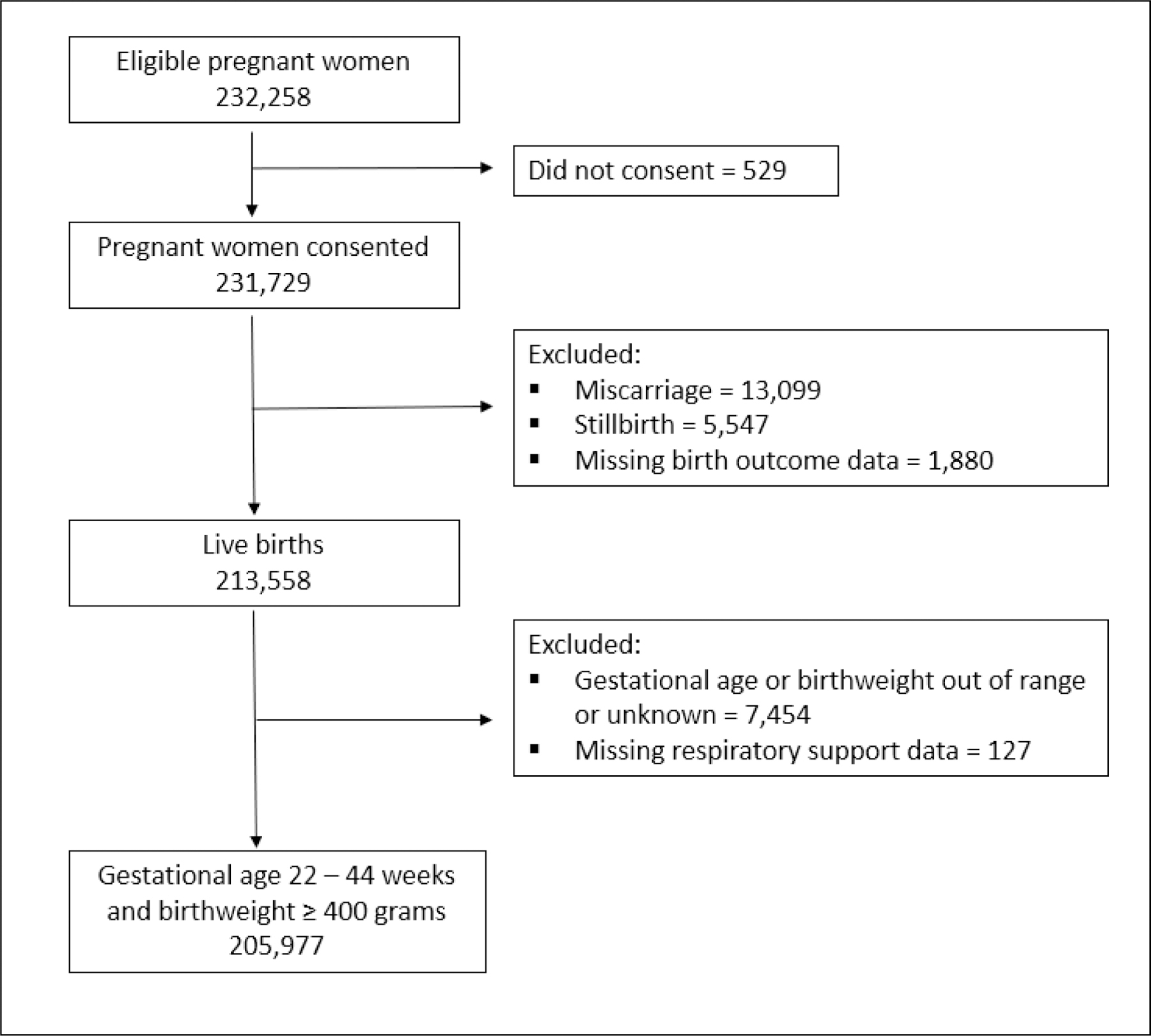
Flow diagram of the sample selection
Table 1:
Maternal and Newborn Characteristics
| Term | Preterm | ||
|---|---|---|---|
|
| |||
| Mothers, N | 176,800 | 27,137 | |
|
| |||
| Maternal age (years), n (%) | <20 | 25,163 (14.2) | 4,659 (17.2) |
| 20–35 | 142,063 (80.4) | 20,737 (76.4) | |
| >35 | 9,543 (5.4) | 1,737 (6.4) | |
| Missing | 31 | 4 | |
|
| |||
| Maternal education, n (%) | None | 32,763 (18.5) | 8,368 (30.8) |
| Primary | 38,588 (21.8) | 6,259 (23.1) | |
| Secondary | 92,912 (52.6) | 11,295 (41.6) | |
| University | 12,493 (7.1) | 1,213 (4.5) | |
| Missing | 44 | 2 | |
|
| |||
| Nulliparous, n (%) | 56,478 (31.9) | 8,347 (30.8) | |
|
| |||
| Births, N | 177,728 | 28,249 | |
|
| |||
| Male, n (%) | 91,228 (51.6) | 14,251 (52.5) | |
|
| |||
| Birthweight (grams), n (%) | <1000 | 6 (0) | 317 (1.2) |
| 1000–1499 | 156 (0.1) | 1,166 (4.3) | |
| 1500–1999 | 1,578 (0.9) | 3,106 (11.4) | |
| 2000–2499 | 15,683 (8.9) | 8,575 (31.6) | |
| ≥2500 | 160,247 (90.6) | 14,951 (55.1) | |
| Missing | 58 | 134 | |
|
| |||
| Delivery site, n (%) | DRC | 18,627 (10.5) | 4,718 (17.4) |
| Guatemala | 37,335 (21.1) | 4,787 (17.6) | |
| Belagavi, India | 27,318 (15.5) | 2,856 (10.5) | |
| Nagpur, India | 27,879 (15.8) | 3,002 (11.1) | |
| Kenya | 24,496 (13.9) | 2,976 (11.0) | |
| Pakistan | 19,107 (10.8) | 6,185 (22.8) | |
| Zambia | 22,966 (13.0) | 3,725 (13.7) | |
|
| |||
| Delivery location, n (%) | Hospital | 78,550 (44.4) | 11,812 (43.5) |
| Clinic/Health center | 64,222 (36.3) | 10,053 (37.0) | |
| Home | 34,955 (19.8) | 6,381 (23.5) | |
| Missing | 1 | 3 | |
|
| |||
| C-section, n (%) | 29,909 (16.9) | 4,632 (17.1) | |
|
| |||
| Respiratory support received | O2 only | 4,269 (2.4) | 2,689 (9.9) |
| CPAP | 362 (0.2) | 244 (0.9) | |
| Mechanical ventilation | 477 (0.3) | 354 (1.3) | |
| Any support | 5,108 (2.9) | 3,287 (11.6) | |
8,395 (4.1%) infants received respiratory support (Table 1). 6,958 infants (3.4%) received oxygen only and 1,437 infants (0.7%) received CPAP and/or mechanical ventilation with or without oxygen. Mechanical ventilation use (n=831, 0.4%) was more common than the use of CPAP (n=606, 0.3%), and this was true in both preterm and term infants.
The proportion of preterm infants who received respiratory support (11.6%) was higher than the proportion of term infants receiving respiratory support (2.9%, p < 0.001, Table 1). However, an overall larger number of term infants (n=5,108) received respiratory support compared to preterm infants (n=3,287). Overall, 61.0% of all infants who received respiratory support were term. Receipt of each mode of respiratory support was more frequent in term infants. The percentage of newborns who received respiratory support was higher with decreasing gestational age (p< 0.001), and that trend persisted until the most preterm gestational ages (Figure 2a, Supplementary Table 1). The number of newborns treated with respiratory support was higher with increasing gestational age until a gestational age of 40 weeks (Figure 2b, Supplementary Table 1).
Figure 2:
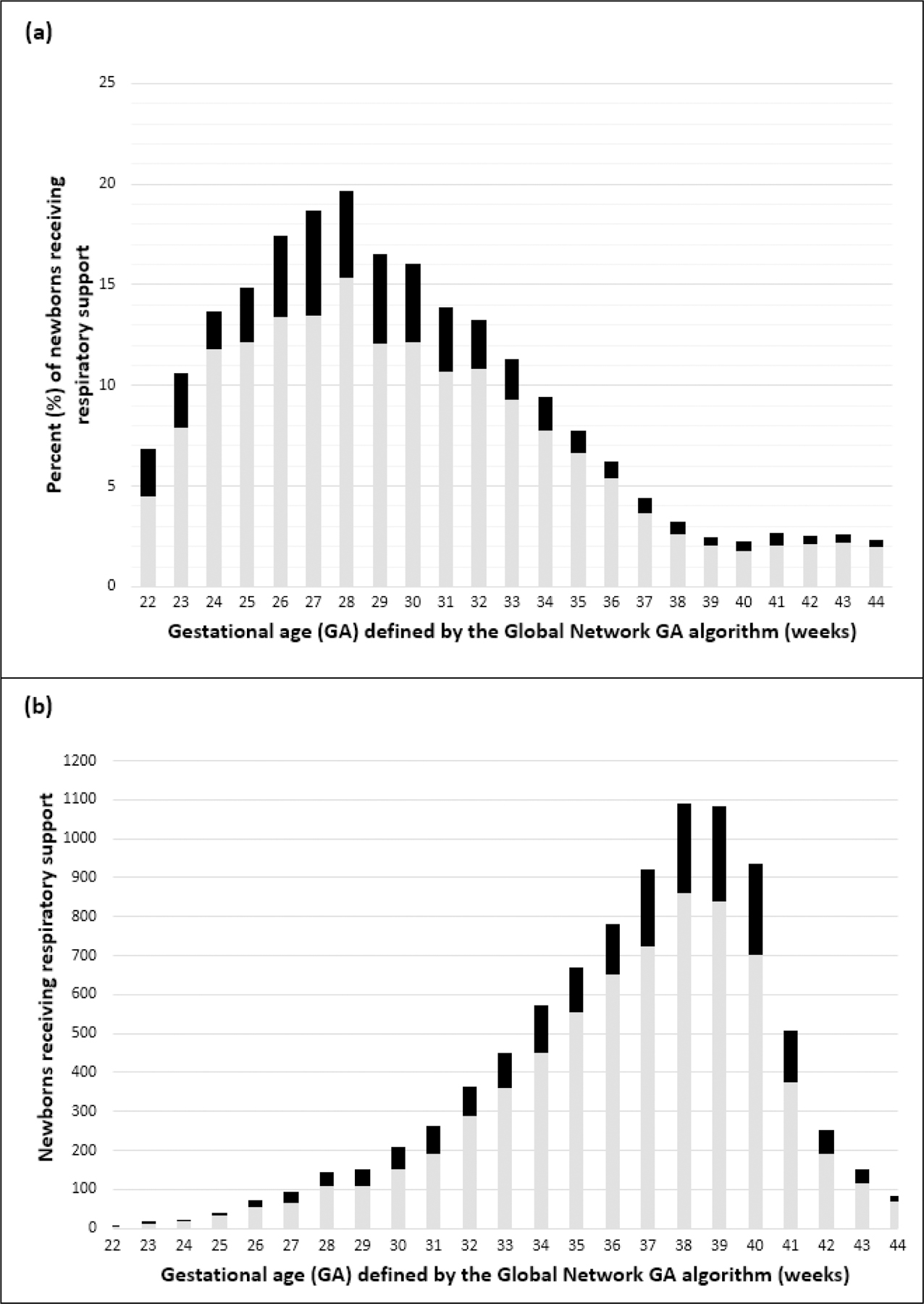
(a) Rate of respiratory support treatment by gestational age defined by the Global Network gestational age algorithm. The proportion of newborns that received respiratory support increased with decreasing gestational age. (b) The number of newborns that received respiratory support by gestational age. The number of newborns that received respiratory support increased with increasing gestational age. In both (a) and (b), the gray bars represent those infants treated with oxygen only. The black bars represent those infants treated with CPAP and/or mechanical ventilation.
The frequency and proportion analyses were repeated using birthweight, and a similar pattern in the receipt of respiratory support was found. Infants with a birthweight <2,500 grams had proportionally higher respiratory support use (3,963/30,587, 13.0%) than infants with birthweight ≥2500 grams (4,441/175,198, 2.5%). A higher number of babies with birthweight ≥2500 grams were treated with respiratory support (n=4,441) compared to the number of infants treated with birthweight <2,500 grams (n=3,963). The percentage of newborns who received respiratory support was higher with decreasing birthweight (p < 0.001, Supplementary Figure 1).
In all delivery locations (hospital, clinic/health center, home), a higher number of term infants were treated with respiratory support (Supplementary Table 2). A higher number of term infants delivered in a hospital or clinic/health center were treated with any respiratory support (n=4740) compared to the number of preterm infants delivered in similar locations (n=3058). Infants born at home may have been transferred to higher level of care to receive respiratory support. A higher number of term infants delivered at home were treated with any respiratory support (n=368) compared to the number of preterm infants that delivered at home (n=228).
A sensitivity analysis restricting the sample to only those infants with gestational age confirmed by first or second trimester ultrasound agreed with the findings that a larger number of term infants received respiratory support compared to preterm infants. 28,109 infants had gestational age confirmed by first- or second-trimester ultrasound. Of these, 621 preterm (18.3%) and 1,002 term (4.1%) infants received respiratory support. The percentage of newborns who received respiratory support was higher with decreasing gestational age (p < 0.001, Supplementary Figure 2, Supplementary Table 3).
Across the four years, the percentage of newborns who received oxygen only remained constant at around 3% and the percentage of newborns who received CPAP and/or mechanical ventilation remained constant at around 1% (Figure 3). The trend in respiratory support use over the study period was found to depend on preterm status (p for interaction = 0.01). Among preterm infants, a trend in respiratory use was not detected across the four years (p = 0.35); the percentage of preterm infants who received any kind of respiratory support remained constant at around 12%. Among term infants, the percentage of newborns receiving oxygen increased from 2.3% in 2015 to 2.5% in 2018 (p <0.01), while no such increase was detected for treatment of term infants with CPAP and/or MV (p=0.28, Figure 3).
Figure 3:
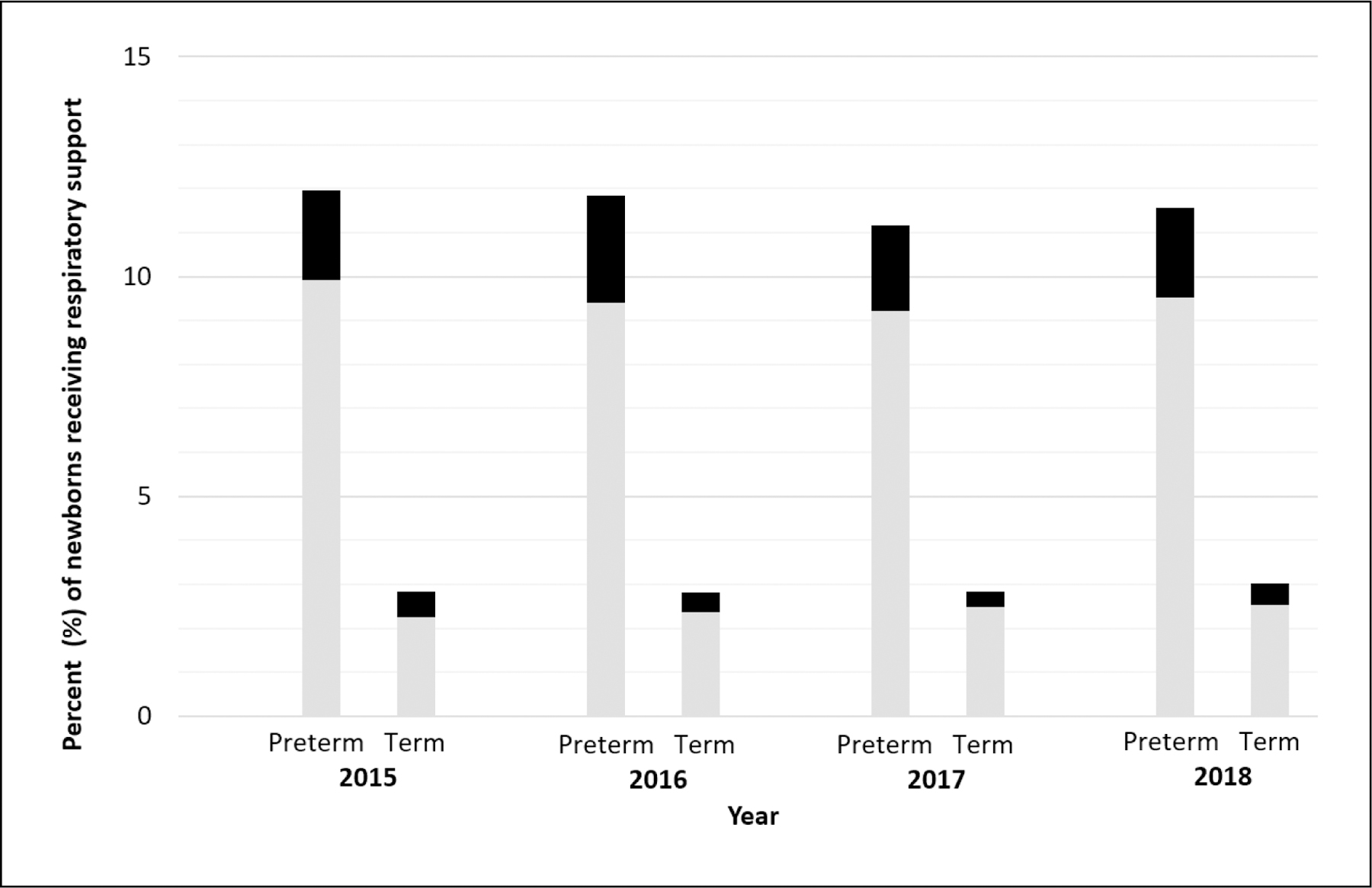
Rate of respiratory support treatment by year. In preterm infants, there was no change in the rate of receipt of respiratory support. In term infants, there was a small increase in the rate of receipt of oxygen only. The gray bars represent those infants treated with oxygen only. The black bars represent those infants treated with CPAP and/or mechanical ventilation.
The rate of provision of respiratory support varied between sites. The sites in the DRC, Zambia, and Kenya had the lowest rates of respiratory support provision while the Indian and Pakistani sites had relatively higher rates (Figure 4). All of the country sites provided all three types of respiratory support throughout the study period. However, at the cluster level there were multiple sites that did not record cases of one or more types of respiratory support. 4/14 clusters in the DRC reported no provision of oxygen only. 14/14 clusters in the DRC, 3/10 clusters in Zambia, 4/16 clusters in Kenya, 1/17 clusters in Guatemala, 1/16 clusters in Belagavi, India, and 1/14 clusters in Pakistan reported no provision of CPAP. 14/14 clusters in the DRC, 1/10 clusters in Zambia, 4/16 clusters in Kenya, and 1/14 clusters in Pakistan reported no provision of mechanical ventilation.
Figure 4:

Rate of respiratory support treatment by global network site. There were differences among sites in the percentage of newborns treated with respiratory support with the DRC reporting the lowest rates and Pakistan reporting the highest rates. The gray bars represent those infants treated with oxygen only. The black bars represent those infants treated with CPAP and/or mechanical ventilation.
Discussion
We found that more term compared to preterm infants received respiratory support in the LMIC settings studied. Specifically, more term infants received oxygen only, CPAP, and mechanical ventilation. However, a larger proportion of preterm than term infants received each type of respiratory support.
The larger number of term infants receiving respiratory support may not seem surprising because term birth is more common than preterm birth. Contrasting results were reported in a large observational study of hospital births in the United States that described respiratory support receipt in term and preterm infants. [2] Compared to term infants, a larger number of late preterm infants received respiratory support even though late preterm infants were a much smaller proportion of the births in this high-income country (HIC) setting. [2] 10.5% of late preterm infants received respiratory support in this HIC setting while only 7.7% received respiratory support in the LMIC settings included in this study. In contrast, 1.1% of term infants in the HIC setting received respiratory support compared to 3.0% in the LMIC settings included in our study.
The majority of infants who received mechanical ventilation in the LMIC settings included in this study were term. This differs from the findings of an observational study of neonatal intensive care admissions to the state hospital system in California which reported that low-birth weight infants (<2,500 grams) made up 62.0% of all the cases who received mechanical ventilation. [1] However, this study concluded that the majority of infants who received cases of mechanical ventilation had normal birthweight. [1] We have shown that term infants received the majority of the respiratory support in the LMIC settings studied. Our findings demonstrate the importance of universal access to respiratory support modalities even in LMIC settings serving primarily low-risk term deliveries.
In this study, the use of CPAP was less frequent than the use of mechanical ventilation, with no change over time. This differs from a descriptive study from two large national clinical databases between 2008–2018 in the US that showed that the use of CPAP was more common in preterm infants compared to the use of mechanical ventilation and that the use of CPAP increased over time while the use of mechanical ventilation declined. [15] Data is not available to describe the use of surfactant in the study sites. This study showed an increase in respiratory support use by term infants but it is unclear if this is a clinically meaningful trend because of the effect size and the duration of the study.
There are many reasons why respiratory support provision patterns differ in LMIC and HIC settings. Access to respiratory support required for the survival of preterm infants may not be available in places where labor and delivery occur, for example at clinics or at home. In the current study, only 41.8% of preterm babies were born in a hospital. It is also possible that preterm infants with a perceived lower chance of survival are not prioritized to receive respiratory support before term infants especially if they are very preterm. Finally, preterm infants may have died prior to provision of respiratory support. In the home birth population in particular, there may have been a survival bias that favored provision of respiratory support to term infants who were more likely to survive to receipt of support in a healthcare setting. The MNH Registry database does not identify which infants required respiratory support and did not receive treatment. Provider bias favoring treatment of term infants and resource scarcity may have influenced the results.
The finding that the use of mechanical ventilation was more common than CPAP in the LMIC settings included in the study suggests a lack of availability and education regarding non-invasive respiratory support modes in these low-resource settings. The use of CPAP in the newborn is a relatively new respiratory support mode compared to mechanical ventilation, which has been increasingly adopted in high-resource settings. [15] Improvement in neonatal CPAP programs has potential to increase the availability of respiratory support in low-resource settings given the lower cost and lower complexity of CPAP compared to mechanical ventilation. The current study suggests that there is potential for expansion of CPAP resources in LMICs.
The current study has many strengths including the geographic breadth and diversity of the Global Network sites, the substantial size of this prospective newborn registry, and the rigor of maintenance of the MNH registry research database. The sample had very few exclusions for missing data regarding respiratory support.
This study has several limitations. The MNH Registry does not collect information on respiratory distress or presence of hypoxemia in the neonate, so the reason for use of respiratory support is unknown. Similarly, there is no information on duration of respiratory support. The sites have varying access to resources including for respiratory support. The sites do not necessarily represent the countries in which they are located, so no conclusions can be made about differences between countries. The results do not represent each country as a whole, but may be generalizable to other similar cohorts in low-resource settings.
Conclusion
More term infants received respiratory support compared to preterm infants in this registry-based observational study in LMICs. Knowledge of the characteristics of newborns who receive respiratory support and the type of support used will inform stakeholders to consider and address resource needs and clinical practice guidelines as well as modify programs geared towards delivering high-quality, effective respiratory support to sick infants in low-resource settings. Receipt of respiratory support was common in both term and preterm infants. Wider access to respiratory support may improve care of term and preterm infants born in low-resource settings.
Supplementary Material
Funding Sources
The Maternal Newborn Health Registry is supported by the NICHD Global Network for Women’s and Children’s Health grant (NCT01073475). A National Institute of Health representative reviewed the manuscript, but was not involved in data collection or analysis.
Footnotes
Statements
Statement of Ethics
The study was approved by the ethics review committees of all research sites, the institutional review board at each partner university in the United States, and RTI International. All women, or the parents or guardians of minors, enrolled in the Maternal Newborn Health Registry (NCT01073475) provided written informed consent. This study protocol was reviewed and approved by University of Alabama at Birmingham Institutional Review Board, approval number IRB-080521010.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Data Availability Statement
Maternal Newborn Health Registry data are available through the NICHD Data and Specimen Hub, https://dash.nichd.nih.gov/. Further enquiries can be directed to the corresponding author.
References
- 1.Angus DC, Linde-Zwirble WT, Clermont G, et al. Epidemiology of neonatal respiratory failure in the United States: projections from California and New York. Am J Respir Crit Care Med 2001; 164: 1154–60. [DOI] [PubMed] [Google Scholar]
- 2.Hibbard JU, Wilkins I, Sun L, et al. Respiratory morbidity in late preterm births. JAMA 2010; 304:419–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kitsommart R, Phatihattakorn C, Pornladnun P, et al. A prospective study of the severity of early respiratory distress in late preterms compared to term infants. J Matern Fetal Neonatal Med 2016; 29:207–12. [DOI] [PubMed] [Google Scholar]
- 4.Kumar A, Bhat BV. Epidemiology of respiratory distress of newborns. Indian J Pediatr 1996; 63: 93–8. [DOI] [PubMed] [Google Scholar]
- 5.Condò V, Cipriani S, Colnaghi M, et al. Neonatal respiratory distress syndrome: are risk factors the same in preterm and term infants? J Matern Fetal Neonatal Med 2017; 30: 1267–72. [DOI] [PubMed] [Google Scholar]
- 6.St Clair C, Norwitz ER, Woensdregt K, et al. The probability of neonatal respiratory distress syndrome as a function of gestational age and lecithin/sphingomyelin ratio. Am J Perinatol 2008; 25: 473–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blencowe H, Cousens S, Chou D, et al. Born too soon: the global epidemiology of 15 million preterm births. Reprod Health 2013; 10 Suppl 1(Suppl 1):S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Griffin JB, McClure EM, Kamath-Rayne BD, et al. Interventions to reduce neonatal mortality: a mathematical model to evaluate impact of interventions in sub-Saharan Africa. Acta Paediatr 2017;106: 1286–95. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization. Oxygen guide therapy for children [Internet]. Geneva: World Health Organization, 2016. Available: https://apps.who.int/iris/bitstream/handle/10665/204584/9789241549554_eng.pdf;jsessionid=8BE34A50A524521C0B4DCF1928CC02C8?sequence=1 [Accessed June 2021]. [Google Scholar]
- 10.World Health Organization. Recommendations on interventions to improve preterm birth outcomes [Internet]. Geneva: World Health Organization; 2016. Available: https://www.who.int/reproductivehealth/publications/maternal_perinatal_health/preterm-birth-guideline/en/ [Accessed June 2021]. [Google Scholar]
- 11.Duke T, Oa O, Mokela D, et al. The management of sick young infants at primary health centres in a rural developing country. Arch Dis Child 2005; 90: 200–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Graham HR, Bakare AA, Ayede A, et al. Oxygen systems to improve clinical care and outcomes for children and neonates: A stepped-wedge cluster-randomised trial in Nigeria. PLoS Med 2019; 16: e1002951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zelasko J, Omotato MO, Berkelhamer SK, et al. Neonatal oxygen therapy in low-and-middle-income countries: a pragmatic review. Journal of Global Health Reports 2020; 4: e2020020. [Google Scholar]
- 14.McClure EM, Garces AL, Hibberd PL, et al. The Global Network Maternal Newborn Health Registry: a multi-country, community-based registry of pregnancy outcomes. Reprod Health 2020; 17 (Suppl 2): 184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hatch LD 3rd, Clark RH, Carlo WA, et al. Changes in use of respiratory support for preterm infants in the US, 2008–2018. JAMA Pediatr 2021; doi: 10.1001/jamapediatrics.2021.1921. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Maternal Newborn Health Registry data are available through the NICHD Data and Specimen Hub, https://dash.nichd.nih.gov/. Further enquiries can be directed to the corresponding author.


