Abstract
Background
The influence of socio-demographic variables was widely explored to evaluate their impact on indigenous and local ethnobotanical knowledge. However, the studies conducted in Ethiopia mainly focused on rural areas. They were limited to exploring and documenting ethnobotanical knowledge and the associated impacts of socio-demographic variables in rural–urban interface areas among ethnic groups. Hence, this study aimed to document plant-based indigenous and local ethnomedicinal knowledge and the associated impacts of socio-demographic variables among selected three ethnic groups in south-central Ethiopia.
Methods
Ethnobotanical data were collected using semi-structured interviews with 189 key informants, floristic species inventories, and field observations. Quantitative approaches were used to evaluate the use values (UV) of the most important medicinal plants, the informant consensus factor (ICF), fidelity level (FL), relative popularity level (RPL), and rank-order priority (ROP). Statistical tests were applied to evaluate the influences of socio-demographic factors and associations between variables on local ethnobotanical knowledge across ethnic groups in different informant categories.
Results
Statistical analysis revealed significant differences (p < 0.05) in the mean number of medicinal plants reported among age categories. There was also a positive association between the respondent's age and plant knowledge acquisition. Croton macrostachyus Hochst. ex Delile, Albizia gummifera C.A.Sm., Zingiber officinale Roscoe, Aloe macrocarpa Tod., Gymnanthemum amygdalinum (Delile) Sch.Bip., Calpurnia aurea (Aiton) Benth, and Allium sativum L. had the highest use values among ethnic groups. The highest informant consensus factor values were recorded for circulatory system disorders (0.68) followed by febrile illness and reproductive organ complications (0.66 each) across the three studied ethnic groups. The highest FL, RPL, and ROP values were noted for Lactuca inermis Forssk., Moringa stenopetala (Baker f.) Cufod., Withania somnifera (L.) Dunal, Allium sativum L., Citrus limon (L.) Osbeck, Ricinus communis L., Schinus molle L., Antiaris toxicaria (J.F.Gmel.) Lesch., Brucea antidysenterica J.F.Mill., Echinops kebericho Mesfin, Ocimum jamesii Sebald, Afrocarpus falcatus (Thunb.) C.N.Page, Searsia natalensis (Bernh. ex Krauss) F.A.Barkley, and Ricinus communis L. across ethnic groups in the study areas, which showed the conformity of knowledge on species curing potential and their prevalent uses.
Conclusion
The study revealed that the ethnic groups of Gedeo, Oromo, and Sidama have considerable indigenous and local ethnobotanical knowledge practices. Statistical analysis shown high variation in the acquisition of local ethnobotanical knowledge among age groups, which boosted our understanding of the effects of socio-demographic factors on the local ethnobotanical knowledge dynamics. Thus, this finding advocates for efforts to repair the observed generation gap via continued professional support and educating local communities to preserve traditional knowledge and practices through systematic documentation.
Keywords: Ethiopia, Indigenous knowledge, Rural–urban interface, Socio-demographic variables, Traditional knowledge
Introduction
Long before were scientific inquiry established, humans created, disseminated, and utilized information about the natural world [1]. Over millennia, indigenous peoples across the globe have developed, maintained, and evolved knowledge systems through direct interaction with biophysical and biological processes and species [1, 2]. As a result, knowledge held by people about their environment evolved gradually and accumulated throughout their histories [3]. Across the globe, including Ethiopia, this local knowledge was significantly dependent on generations’ constant connection with their surroundings and elders [3, 4] and regarded as a body of place-based knowledge accumulated and transmitted across generations within specific cultural contexts [1, 3, 5]. According to [5–7], indigenous and local knowledge is not only direct observation and contact with the environment but also a wide range of cultural and spiritual knowledge and values that enhance human–environment relationships. Ethnobotanical studies conducted elsewhere explained the associations between socio-demographic factors and knowledge of plant use [4, 8–12]. Some of them revealed that age and ethnobotanical knowledge have a direct relationship and that ethnobotanical knowledge accumulation increases with an individual’s age [8–10, 13] and is widely used among communities with poor health facilities [12]. Others explained the influences of gender and education level: males and lower-grade attendees were more familiar with the medicinal values of local flora [4, 8], and traditional healers possess richer ethnobotanical knowledge than laypeople [10, 13]. Thus, the cultural variables seem essential in explaining and determining plant use knowledge [5, 10, 14].
Ethiopia is one of the world’s most ethnically and culturally diverse country, with over 70 different languages spoken across and more than 80 distinct ethnicities [16, 17]. Several ethnobotanical studies have been conducted to document traditional medicinal plant knowledge and the associated factors elsewhere in the country [4, 8–10, 13, 16, 19–25]. However, they are insignificant when compared to the 80 diverse ethnolinguistic communities, and most of them are largely unexplored and limited to rural areas. According to CSA [25], south-central Ethiopia is home to diverse ethnic groups, representing more than half of the country's indigenous ethnic communities; but, evidences from [8, 18–20, 23, 24, 26–29] reveal that studies conducted on medicinal plants have so far focused in the south and southwestern parts, covering only a few out of the estimated 45 or more socio-cultural (language) groups. Thus, medicinal plant resources and indigenous knowledge about the use of medicinal plants in south-central Ethiopia, particularly in the current study's peri-urban area, are inadequate.
As a result, the current study was conducted to fill this gap by documenting the abundance of indigenous and local ethnobotanical knowledge and understanding the corresponding socio-demographic drivers among the three ethnic groups in south-central Ethiopia. Specifically, the study aimed at (i) documenting plant-based indigenous and local ethnomedicinal knowledge of the Gedeo, Oromo, and Sidama ethnic groups against human ailments in Dilla, Shashemene, and Hawassa peri-urban areas, respectively; (ii) evaluating the impact of socio-demographic variables on medicinal plant knowledge among the three studied ethnic groups; (iii) determining the use values (UV) of the most important medicinal plants among the three studied ethnic groups; and (iv) identifying potential medicinal plant species among the three ethnic groups for future phytochemical and pharmacological investigations. The hypothesis is that medicinal plant knowledge varies depending on the socio-demographic variables among ethnic groups. The study will contribute scientific information about the medicinal flora and associated ethnobotanical knowledge, as well as understanding the influences of socio-demographic variables on local and indigenous medicinal plant knowledge in the rural–urban interface areas of south-central Ethiopia.
Materials and methods
Description of the study area
The study was conducted in three selected sites of neighboring ethnic groups in the south-central part of Ethiopia: Hawassa, Shashemene, and Dilla. Administratively, Hawassa district is part of the Sidama National Regional State, whereas Shashemene and Dilla districts are parts of the Oromia and Southern National Regional States, respectively (Fig. 1). Nine peri-urban kebeles (lowest administrative units; three from each study site) were purposely selected at different distances from the peri-urban administrative parts of Hawassa, Shashemene, and Dilla (Fig. 1). These areas were chosen because the ethnic groups living in the districts have coexisted and interacted for many years in specific regions of south-central Ethiopia. Additionally, they are geographically close to the town, have similar urbanization pressures, and are facing aggressive degradation of natural resources owing to urbanization [30–33]
Fig. 1.
Map of the study sites Dilla, Shashemene, and Hawassa peri-urban areas
Hawassa is situated 273 km south of Addis Ababa [34], at 6°55′–07°06′N and 38°25′–38°33′E, with elevation ranges of 1656 to 2137 m a.s.l.[35]. The borders of Hawassa area are defined by Lake Hawassa to the west, Oromia National Regional State to the north, Wondo Genet and Malga districts to the east, and Shebedino and Gorge districts to the south. Hawassa had 15,720 hectares of land within its administrative boundary, while only 6,465 hectares (24.4%) were demarcated within the municipal boundary and planned as urban land, while the rest is rural land [34]. Administratively, the city was organized into three tiers of administration: which divided into 8 sub-cities and 32 kebeles (lowest administrative units) (Hawassa City Administration annual unpublished report, 2019). Among the sub-cities, Hawella-Tulla and its 12 kebeles were categorized as rural and rural–urban interface areas, where the current study was conducted (Fig. 1). Residents of the study area are ethnically and religiously diverse. The majority of indigenous and local people living in the area are Sidama (48.68%), followed by Amhara (15.43%), Welaita (13.9%), Oromo (5.21%), Gurage (4.33%) and others (12.45%), CSA [25]. The major language spoken in the area belongs to the Sidama ethnic group ‘Sidamu afoo’ (47.97%), followed by Amharic (31.01%), Welaita (9.58%), Afan Oromo (2.53%), Gurage (1.98%), Kembata (1.82%), and others (5.09%). More than half of the people in the research area practice the Protestant religion (52.71%), followed by Ethiopian Orthodox Christianity (39.99%), Islam (7.3%), and Catholicism (3.78%). According to the CSA [25] population forecasts, the projected population for 2022 was 555,480, of whom 277,032 were males and 278,448 were females.
Shashemene district is located at 7°04′50″ to 7°22′45″N and 38°23′00″ to 38°48′00″E. Which is 250 km to the south of Ethiopia's capital city, Addis Ababa, and 25 km north of Hawassa, the capital city of Sidama National Regional State [36]. Hawassa city borders it to the south, Seraro to the west, Arsi Negele to the north, and Arsi Zone to the east. Its elevation ranges from 1,500 to 2,300 m a.s.l. [36]. The district had a 767.9km2 area with 458.3/km2 population density [25]. The district rural and rural–urban interface areas have assembled into 28 kebeles (lowest administrative units), where the current study was conducted (Fig. 1). Residents of the study area were ethnically and religiously diverse. The Oromo ethnic group makes up the majority of the indigenous inhabitants in the district (74.11%), followed by the Amhara (9.26%), Welaita (95%), Kembata (2.3%), Gurage (2.13%), and others accounted for 7.2%, CSA [37]. The major language spoken in the area belongs to the Oromo ethnic group ‘Afan Oromo’ (71.7%), followed by Amharic (18.23%), Welaita (3.49%), Kembata (1.52%), Gurage (1.14%), and others (2.02%). The majority of the inhabitants were Islamic religion followers, with 69.38% of the population, followed by Ethiopian Orthodox Christianity (23.5%), Protestantism (5.62%), and Catholicism (1.05%). According to the CSA [25] population forecasts, the projected population for 2022 was 351,898, of whom 174,711 were males and 177,187 were females in the district (Table 1).
Table 1.
Detailed locations of the study sites
| Study sites | Longitude (o) | Latitude (o) | Elevation | Agro-ecology |
|---|---|---|---|---|
| Kori Borojota | 38.480479305928 | 7.187481904610 | 1806 | Moist mid-highland (Moist Weina Dega) |
| Dalati Guracha Bishan | 38.476134272769 | 7.142100771683 | 1744 | Moist mid-highland (Moist Weina Dega) |
| Ebicha | 38.602659011844 | 7.136859913447 | 2043 | Moist mid-highland (Moist Weina Dega) |
| Tullo | 38.459627749373 | 6.996525786840 | 1700 | Moist mid-highland (Moist Weina Dega) |
| Alamura | 38.497456580871 | 6.989165780928 | 1704 | Moist mid-highland (Moist Weina Dega) |
| Chefasine | 38.495170076222 | 6.939687380283 | 1926 | Moist mid-highland (Moist Weina Dega) |
| Gola | 38.327582906735 | 6.401188224290 | 1760 | Wet mid-highland (Wet Weina Dega) |
| Andida | 38.349498162680 | 6.400104445130 | 1883 | Wet mid-highland (Wet Weina Dega) |
| Shigedo | 38.365856530154 | 6.398218606985 | 1981 | Wet mid-highland (Wet Weina Dega) |
The agro-ecologies are described based on the agro-climatic zone classification of Ethiopia, Tesemma [39]
Dilla district was located in southern Ethiopia, 359 km from the capital city, Addis Ababa [38], and an altitude range of 1,350 to 2,550 m a.s.l. It is situated at 6°15′05" to 6°26′35 N and 38°15′55" to 38°24′02"E. The district had a 122.3 km2 area with a 1,047/km2 population density [25]. The district rural and rural–urban interface areas were assembled into 19 kebeles (lowest administrative units), where the current study was carried out (Fig. 1). The district residents are heterogeneous, both in ethnicity and in religion. The majority of indigenous people inhabiting the area belong to the Gedeo ethnic group (73.5%), followed by the Amhara (6.98%), Oromo (6.37%), Sidama (3.34%), Silte (2.33%), and others (7.48%), CSA [37]. The Gedeo ethnic group language 'Gedeoffa' was spoken widely (73.22%), followed by Amharic (13.5%), Afan Oromo (5.43%), Sidamu afoo (3.25%), Silte (1.39%), and others (3.21%). The majority of the people were Protestants religion followers, accounting for 83.13% of the population, followed by traditional belief (7.81%), Ethiopian Orthodox Christianity (5.31%), Catholicism (1.16%), Islam (1.02%), and others (1.57%), CSA [25]. According to the CSA [25] population forecasts, the projected population for 2022 was expected to reach 128,050, of whom 64,276 were males and 63,774 were females in the district.
Informant selection
To ensure a detailed representation of indigenous and local knowledge dynamics and plant uses, traditional healers of the three ethnic groups were selected based on their gender, age, experience, level of education, and religion. For the survey, 189 key informants (133 males and 56 females) with the age range of 35 to 77 were selected using purposive and snowball sampling techniques based on recommendations from local communities, local government heads, and development workers following [16, 17]. Of the total, 63 were from the Sidama (43 males and 20 females), 63 were from the Oromo (41 males and 22 females), and 63 were from the Gedeo ethnic group (49 males and 14 females). Informed consent has been obtained from all informants who served as informants before the start of the interviews.
Ethnobotanical data collection and specimen identification
Ethnobotanical data were collected from January to May 2023, using semi-structured interviews with local traditional healers and inventories of plant species following an approach of [40–42]. The first session included information regarding the socio-demographic characteristics of the informants. Secondly, information related to the detailed ethnobotanical application of the local flora. Most of the interviews were carried out in local languages (Sidamu Afoo, Afan Oromo, and Gedeoffa) with the help of local translators or a language native to the respective research locations. Each ethnic group studied was an indigenous and local resident of the study area. All floristic voucher specimens were collected with the help of traditional healers and development professionals. Specimens were identified in the field and later confirmed at the National Herbarium of Addis Ababa University and Wondo Genet College of Forestry and Natural Resources, Hawassa University using taxonomic keys and flora [43–48]. The verified specimens in the National Herbarium were further checked using Plants of the World Online (https://powo.science.kew.org.) websites to confirm the correctness of the scientific names and author citations. Finally, the plants were dried, pressed, mounted on a herbarium sheet, and placed at Hawassa University's Wondo Genet College of Forestry and Natural Resources Herbarium.
Data analysis
Both qualitative and quantitative data were analyzed using the ethnobotanyR package, Version 0.1.8, 2022. Age, gender, education, and religion were used to determine the impacts of socio-demographic variables on ethnobotanical knowledge. The Kruskal–Wallis chi-squared test, a non-parametric approach to the one-way ANOVA, was performed between age, education, religion, and the number of medicinal plants cited, and the Wilcoxon test for gender. The mean and standard deviation of the number of medicinal plants reported concerning the socio-demographic variables were evaluated. Regression analysis was conducted to determine the association between respondent's ethnobotanical knowledge and age. Quantitative ethnobotanical tools such as the informant consensus factor (ICF), use values (UV), fidelity level (FLs), relative popularity level (RPL), and rank-order priority (ROP) were also used for data analysis.
Use Value index (UVi)
The use value index (UVI) was calculated to find out the relative importance of medicinal plant species following [49].
where ’Ui’ is the number of different uses mentioned by each informant i and ‘N’ is the total number of informants interviewed for the given plant species.
Informant consensus factor (ICF)
The informant consensus factor was calculated to investigate the degree of homogeneity among informants for the plants to be used in each ailment category [50]. The ICF values vary from zero to one, with a high ICF achieved when one or a few plant species were reported to treat a certain condition by a large proportion of informants.
where ‘Nur’ is the number of use reports in each ailment category and ‘Nt’ is the total number of taxa used in each ailment category by all the informants.
The result of this factor ranges from 0 to 1. A high value (close to 1) indicates that relatively few plant species are used by a large proportion of people, and a low value indicates that the informants disagree on the plant species used to treat a category of illness.
Fidelity level (FL)
The fidelity level is applied to determine which species are most frequently employed by the key informants to treat particular conditions. Higher FL values would indicate medicinal plants are more commonly used by the local communities, reveal the proportion of informants who reported using a specific plant species for the same purposes, and highlight the significance of the species for specific conditions. Following [51] and [52], all reported illnesses were arranged into major categories before determining the values using the formula [51].
where Ns is the number of informants that use a particular plant for a specific purpose and FCs is the total number of uses for the species.
Relative popularity level (RPL)
The relative popularity level (RPL) is a ratio of the number of important use reports mentioning a certain plant species to the number of interviewees mentioning that taxon in any use reports. RPL values vary from zero to one, with one representing total popularity and zero representing unpopularity [53].
Rank-order priority (ROP)
Relative popularity level (RPL) value multiplied by fidelity level (FL) value yielded the rank-order priority or accurate value of fidelity level (FL) (ROP = RPL * FL) [51]. A high ROP value suggests that the plant has great potential. It might be beneficial for screening plants for bioactive compounds.
Results
Socio-demographic characteristics and knowledge of traditional healers
According to interviews with key informants (Table 2), 189 medicinal plant species were collected and documented (Table 3). Among the 189 informants, the majority of participants were farmers, 155 (82%); others were merchants, 23 (12%); and students, 11 (6%). Male participants were outnumbered female participants (Table 2). About 70% of participants in this study were between the ages of 45 and 65. In comparison, those under 45 (young) and over 65 (elderly) accounted for 30% of the remaining population (Table 2). Illiterate and lower-grade informants were higher compared to high school attendees. Most interviewees were protestant religion followers, followed by Muslims and Orthodox Christians (Table 2).
Table 2.
Demographic details of the participants from peri-urban areas of Dilla, Hawassa, and Shashemene
| Socio-demographic features | Categories | Frequency | Percentage |
|---|---|---|---|
| Ethnicity | Gedeo | 63 | 33.33 |
| Oromo | 63 | 33.33 | |
| Sidama | 63 | 33.33 | |
| Age | 35–44 | 33 | 17 |
| 45–54 | 45 | 24 | |
| 55–64 | 88 | 47 | |
| 65 + | 23 | 12 | |
| Gender | Male | 133 | 70 |
| Female | 56 | 30 | |
| Education | Illiterate | 89 | 47 |
| Primary (1–8 grade) | 81 | 43 | |
| Secondary level | 19 | 10 | |
| Religion | Protestant | 101 | 53 |
| Orthodox | 13 | 7 | |
| Islam | 75 | 40 |
Table 3.
Medicinal plants mentioned by the three studied ethnic groups (Sidama (S), Gedeo (G), and Oromo (O)) in south-central Ethiopia (N = 189)
| Scientific name | Family | Local name | Ha | Sources | Pu | Ethnic group | Medicinal uses against | Other local uses | Voucher number |
|---|---|---|---|---|---|---|---|---|---|
| Allium cepa L | Amaryllidaceae | Qulubi addi | H | Hg/Mt | Fb | G | Nasal bleeding, Passive sexual interest, Weight loss | Fo, Sp | St 2022 (1) |
| Ananas comosus (L.) Merr | Bromeliaceae | Anannase | H | Hg | Ff, Ffb | G | Skin infection | Fo, Env | St 2022 (2) |
| Oldeania alpina (K.Schum.) Stapleton | Poaceae | Lemma | Sh | Hg/Wl | As | G | Wound | Co, F, Fl, Env | St 2022 (3) |
| Arundo donax L | Poaceae | Hophetikka | Sh | Hg/Wl | Dl | G | Swellings | Co, F, Fl, Env | St 2022 (4) |
| Bidens macroptera (Sch.Bip. ex Chiov.) Mesfin | Asteraceae | Addeyi | H | Wl | Fr | G | Abnormal menstruation cycle, amoeba, diarrhea | Nt | St 2022 (5) |
| Capsicum frutescens L | Solanaceae | Mixmixxo | H | Hg/Mt | Ff | G | Amoeba, intestinal worms | Fo, Sp | St 2022 (6) |
| Celtis africana Burm.f | Cannabaceae | Shishu | T | Wl | Fb, Db, Or, Yfl, Yr, Fs | G | Stomachache, Jaundice, Skin infection, Wound, Headache, Diarrhea, Asthma, Intestinal worms, Glandular, Lung infection, Giardia | Fl, Co, Tm, Env, Sh, Ch, Fr | St 2022 (7) |
| Clausena anisata (Willd.) Hook.f. ex Benth | Rutaceae | Lichee/Limich | Sh | Wl | Fl | G | Swellings | Env, Fr | St 2022 (8) |
| Clutia lanceolata Forssk | Peraceae | Kudhure | Sh | Wl | Fl | G | Ear infection | Env, Fr, Fl | St 2022 (9) |
| Colocasia esculenta (L.) Schott | Araceae | Colcomma | H | Wl | Dr, Fr | G | Deep sores and Cancer-like ailments, Toothache | Env | St 2022 (10) |
| Cymbopogon citratus (DC.) Stapf | Poaceae | Hancura | H | Wl | Fl | G | Abortion, Bath of mother after giving birth, Blood pressure, Deep sores and Cancer-like ailments, Cholesterol, Kidney infection, Stomachache, Gonorrhea, Vomiting | Env | St 2022 (11) |
| Dalbergia lactea Vatke | Fabaceae | Batissa | Sh | Wl | Fl, Fs | G | Gonorrhea, Amoeba | Env, Fl, Fr | St 2022 (12) |
| Drynaria volkensii Heiron | Polypodiaceae | Bobile | Ep | Wl | Fr, Fl | G | Deep sores and cancer-like ailments, ear infection, swellings, nasal bleeding | Nt | St 2022 (13) |
| Embelia schimperi Vatke | Primulaceae | Honkoko | T | Wl | Fl | G | Glandular, Gonorrhea, Jaundice | Fl, Co | St 2022 (14) |
| Euphorbia pulcherrima Willd. ex Klotzsch | Euphorbiaceae | Qorsa abeba | Sh | Hg | Fr | G | Fever | F, Fl | St 2022 (15) |
| Euphorbia tirucalli L | Euphorbiaceae | Qinchibi | Sh | Hg | L | G | Deep sores and Cancer-like ailments | F, Fl | St 2022 (16) |
| Fagaropsis angolensis (Engl.) H.M.Gardner | Rutaceae | Sissa | T | Wl | Ds, Fl | G | Stomachache, Wound, Swellings | Fl, Env, Co | St 2022 (17) |
| Flacourtia indica (Burm.f.) Merr | Salicaceae | Hagala | Sh | Wl | Ff, Fr | G | Snake venom, Respiratory organ infection | F, Fl | St 2022 (18) |
| Hibiscus macranthus Hochst. ex A. Rich | Malvaceae | Abeba | Sh | Wl | Fl | G | Fire accident | F, Fl | St 2022 (19) |
| Hyparrhenia rufa (Nees) Stapf | Poaceae | Qoricha bekekko | H | Wl | Fl | G | Swellings, Cough, Lung infection | Env, Fr | St 2022 (20) |
| Juniperus procera Hochst. ex Endl | Cupressaceae | Honcho | T | Hg/Wl | Ds | G | Respiratory organ infection | Co, Tm, Fl, F | St 2022 (21) |
| Kanahia laniflora (Forssk.) R.Br | Asclepidaceae | Cigga | Sh | Wl | Fl | G | Jaundice | Fl | St 2022 (22) |
| Leucas tomentosa Gürke | Lamiaceae | Balbalato | H | Wl | Fl | G | Febrile illness | Env, Fl | St 2022 (23) |
| Rubia cordifolia L | Rubiaceae | Dummo | Cl | Wl | Fl | G | Malaria | Nt | St 2022 (24) |
| Sesbania sesban (L.) Merr | Fabaceae | Shashatto | Sh | Wl | Fl | G | Rabies, Snake venom | Env, Fr, Fl, Co | St 2022 (25) |
| Sida ovata Forssk | Malvaceae | Qirqixxe | Sh | Wl | Fl | G | Deep sores and Cancer-like ailments | Env, Fl | St 2022 (26) |
| Solanum indicum L | Solanaceae | Dimoxxa | Sh | Wl | Fl | G | Nasal bleeding, Skin infection, Snake venom | F, Fl | St 2022 (27) |
| Sorghum bicolor (L.) Moench | Poaceae | Xinqisha | H | Wl | Fr | G | Febrile illness, Respiratory organ infection | Fo | St 2022 (28) |
| Strychnos spinosa Lam | Loganiaceae | Goqqumma | T | Wl | Fl, Fb | G | Bad/evil spirit, Fire accident, Toothache | Fo, Env, Fl | St 2022 (29) |
| Gymnanthemum myrianthum (Hook.f.) H.Rob | Asteraceae | Rejii | Sh | Wl | Fl, Dr | G | Headache, Respiratory organ infection | Fr, Fl, Env, Co | St 2022 (30) |
| Xanthium strumarium. L | Asteraceae | Qorsi butika | H | Wl | Fl | G | Nerve case | Fl | St 2022 (31) |
| Vachellia oerfota (Forssk.) Kyal. & Boatwr | Fabaceae | Ajoo | Sh | Hg/Wl | Fr, Fb | O | Bad/evil spirit, General health | Co, Env, Fl, Hn, Fr, Ch, Sh, H | St 2022 (32) |
| Vachellia seyal (Delile) P.J.H.Hurter | Fabaceae | Waccu | T | Wl | Fb | O | Intestinal worms | Co, Env, Fl, Env, Co, Fr, Ch, Sh, Hn | St 2022 (33) |
| Vachellia tortilis (Forssk.) Galasso & Banfi | Fabaceae | Dhadacha | T | Wl | Fb | O | Malaria, Bad/evil spirit | Co, Env, Fl, Env, Co, Fr, Ch, Sh | St 2022 (34) |
| Argemone mexicana L | Papaveraceae | Wajota | H | Wl | L, Fl | O | Deep sores and Cancer-like ailments, Blood pressure, Wound, Jaundice | Fl | St 2022 (35) |
| Beta vulgaris L | Amaranthaceae | Keyisir | H | Hg/Mt | Fr, Fl | O | Anemia, Wound | Fo, Env | St 2022 (36) |
| Calendula officinalis L | Asteraceae | Olaati | H | Wl | Fs | O | Amoeba | Nt | St 2022 (37) |
| Capsella bursa-pastoris Medik | Brassicaceae | Bursi | H | Wl | Fr | O | Lung infection, Asthma, Cough | Env | St 2022 (38) |
| Casimiroa edulis La Llave | Rutaceae | Kazmiree | T | Hg | Ff | O | Gastric diseases | Fr, Fo, Fl, Co, Tm, Env, Ch | St 2022 (39) |
| Casuarina equisetifolia L | Casuarinaceae | Shawshawee | T | Wl | Fl | O | Rabies | Fl, Co | St 2022 (40) |
| Citrus limon (L.) Osbeck | Rutaceae | Lomme | T | Hg/Wl | Fl, Ff | O | Blood pressure, Fever, Stomachache, Common cold, Amoeba | Fo, Env | St 2022 (41) |
| Rotheca myricoides (Hochst.) Steane & Mabb | Lamiaceae | Marachissa | Sh | Wl | Fb, Fl | O | Rabies, Stomachache, Bad/evil spirit | Fr, Env | St 2022 (42) |
| Cyathula polycephala Baker | Amaranthaceae | Hixxicho | H | Wl | Fl | O | Febrile illness | Fl | St 2022 (43) |
| Daucus carota L | Apiaceae | Karotee | H | Hg/Mt | Fr, Ff | O | Jaundice, Passive sexual interest | Fo | St 2022 (44) |
| Eleusine coracana (L.) Gaertn | Poaceae | Dagussa | H | Wl | Fs | O | Bone injury, Wound | Fo | St 2022 (45) |
| Eragrostis tef (Zuccagni) Trotter | Poaceae | Gashee | H | Hg/Mt | Fs | O | Bone injury, Wound | Fo | St 2022 (46) |
| Erica arborea L | Ericaceae | Satto | Sh | WL | Fr, Dr, Dl | O | Malaria, Bad/evil spirit, Wound | Fl | St 2022 (47) |
| Corymbia citriodora (Hook.) K.D.Hill & L.A.S.Johnson | Myrtaceae | Bargamo sayiti | T | Hg/Wl | Fl | O | Gonorrhea | Co, Tm, F, Fl, Ch | St 2022 (48) |
| Ficus sycomorus L | Moraceae | Odda | T | Wl | Ds, Db, Fs | O | Tonsillitis, Glandular | Fl, Co, Env, Sh | St 2022 (49) |
| Helianthus annuus L | Asteraceae | Suffa | H | Hg/Mt | Fs | O | Febrile illness, Tung infection | Fo | St 2022 (50) |
| Indigofera arrecta Hochst. ex A.Rich | Fabaceae | Hinna | Sh | Wl | Fl | O | General health | Fr, Env, Fl | St 2022 (51) |
| Kalanchoe densiflora Rolfe | Crassulaceae | Hanculule Ancura | H | Wl | Fl | O | Muscular/joint pain | Nt | St 2022 (52) |
| Kniphofia foliosa Hochst | Asphodelaceae | Shushune | Sh | Wl | Fr | O | Stomachache | Nt | St 2022 (53) |
| Lantana camara L | Verbenaceae | Qoso jarti | Sh | Wl | Fl | O | Sneezing | Fl, F | St 2022 (54) |
| Lippia abyssinica (Otto & A.Dietr.) Cufod | Verbenaceae | Sukayi | H | Wl | Dl | O | Blood pressure, Diarrhea, Stomachache | Env, Fl, Sp | St 2022 (55) |
| Gymnosporia senegalensis (Lam.) Loes | Celastraceae | Kombolcha | Sh | Hg/Wl | Fb | O | Jaundice, Malaria, Skin infection | Fl, Ch, Co | St 2022 (56) |
| Mimusops kummel Bruce ex A.DC | Sapotaceae | Olaatee | T | Wl | Fs, Ds | O | Diarrhea, Lung infection | Fl, Co, Fr | St 2022 (57) |
| Myrica salicifolia Hochst. ex A.Rich | Myricaceae | Qammo | T | Wl | Fb | O | Bad/evil spirit | Fl, Co | St 2022 (58) |
| Pavonia urens Cav | Malvaceae | Hincinnii | H | Wl | Fl | O | Bad/evil spirit | Nt | St 2022 (59) |
| Persicaria senegalensis (Meisn.) Soják | Polygonaceae | Shulta | H | Wl | Fl | O | Jaundice, Malaria | Nt | St 2022 (60) |
| Pittosporum viridiflorum Sims | Pittosporaceae | Harbu | T | Wl | Fl, Fb | O | Rabies, Fever, Bad/evil spirit | Fl, Co | St 2022 (61) |
| Plantago lanceolata L | Plantaginaceae | Qorxxo | H | Wl | Fr | O | Epilepsy | Fr, Env | St 2022 (62) |
| Aningeria altissima (A.Chev.) Aubrév. & Pellegr | Sapotaceae | Kore | T | Wl | Fb | O | Swellings | Fl, Co, Env, Ch | St 2022 (63) |
| Rubus apetalus Poir | Rosaceae | Goorra | Sh | Wl | Yb, Fs | O | Toothache | Fo, F, Env | St 2022 (64) |
| Rubus steudneri Schweinf | Rosaceae | Goorra | Sh | Wl | Db, Fb, Fr, Fl | O | Headache, Nasal bleeding, Skin infection, Amoeba, Diarrhea, Urinary organ infection, Febrile illness, Stomachache | F, Fl | St 2022 (65) |
| Salvia nilotica Juss. ex Jacq | Lamiaceae | Hulegebi | H | Wl | As | O | Heart case | Env | St 2022 (66) |
| Schinus molle L | Anacardiaceae | Qondo | T | Wl | Fl, Fs, Yb | O | Jaundice, Tonsillitis, Nasal bleeding | Fl, Co, Fr, Sh | St 2022 (67) |
| Schrebera alata (Hochst.) Welw | Oleaceae | Dhamma’e | T | Wl | Fr | O | Deep sores and Cancer-like ailments, Swellings | Sh, Co, F, Fl, Env | St 2022 (68) |
| Senna auriculata (L.) Roxb | Fabaceae | Ajawa | Sh | Wl | Dr, Fl | O | Constipation, Skin infection | Fl, Fr, Env | St 2022 (69) |
| Solanum marginatum L.f | Solanaceae | Hidhi oromo | Sh | Wl | Fr, Ff, Fl | O | Febrile illness, Acid injury, Nasal bleeding, Snake venom, Autism, Bad/evil spirit | Fl, F | St 2022 (70) |
| Vepris nobilis (Delile) Mziray | Rutaceae | Hadhessa | T | Wl | Fl, Dl, Fr | O | Blood pressure, Skin infection, Dry skin treatment, Ear infection, Eye infection | Co, Env, Fl, Fr | St 2022 (71) |
| Terminalia brownii Fresen | Combretaceae | Rukessa | Sh | Hg | Fl | O | Common cold, Headache | Fl, Sh, Env | St 2022 (72) |
| Trichilia dregeana Sond | Meliaceae | Sissa | T | Wl | Ds, Fl | O | Jaundice | Fr, Co, Env, Sh | St 2022 (73) |
| Ximenia americana L | Olacaceae | Hudha | Sh | Wl | Fs, Fr | O | Swellings, Intestinal worms, Wound, Stomachache | Fo, Fl | St 2022 (74) |
| Zea mays L | Poaceae | Badala | H | Hg | Ds | O | Sneezing | Fo, Fl, Fr | St 2022 (75) |
| Ziziphus spina-christi (L.) Willd | Rhamnaceae | Qurqura | T | Wl | Fl, Fr, Ds, L, Fb | O | Skin infection, Bad/evil spirit, Rabies, Giardia, Gonorrhea, Eye infection, Intestinal worms, Wound | Co, Fo, Fr, Env, Sh, Ch | St 2022 (76) |
| Aloe pirottae A.Berger | Asphodelaceae |
Sibri (G) Hargessa (O) |
H | Wl | Fl, Dl | O, G | Gastric diseases, Jaundice, Kidney infection, Menstruation cycle disorder, Passive sexual interest, Vaginal infection, Ear infection | Fl, Env | St 2022 (77) |
| Asparagus africanus Lam | Asparagaceae |
Uffae (G) Siriitii (O) |
Sh | Wl | Fb, Fl, Ds | O, G | Rabies, Deep sores and Cancer-like ailments, Jaundice, Ear infection, Skin infection, Epilepsy, Swellings, Lung infection | Nt | St 2022 (78) |
| Brassica carinata A.Braun | Brassicaceae |
Shaaana (G) Danqalle (O) |
H | Hg | Fl, Ds | O, G | Constipation, Fever, Skin infection, Toothache, Cough, Lung infection | Fo, Env | St 2022 (79) |
| Commelina benghalensis L | Commelinaceae |
Butikka (G) Lalunxe (O) |
H | Wl | Fst, L | O, G | Swellings, Amoeba, Skin infection | Env | St 2022 (80) |
| Delonix elata (L.) Gamble | Fabaceae |
Harangama (G) Sukeelaa (O) |
Sh | Wl | Ds, Fs | O, G | Stomachache | F, Fl, Co, Env | St 2022 (81) |
| Euphorbia ampliphylla Pax | Euphorbiaceae |
Caree (G) Surre (O) |
Sh | Hg | Fr, L, Dr | O, G | Epilepsy Deep sores and Cancer-like ailments, Bad/evil spirit | F, Fr | St 2022 (82) |
| Grewia ferruginea Hochst. ex A.Rich | Malvaceae |
Ogomodi (G) Dhoqona (O) |
Sh | Wl | Fb, Fl, Dl, Fr, Fs | O, G | Respiratory organ infection, Jaundice, Febrile illness, Headache, Swellings, Wound, Epilepsy, Deep sores and Cancer-like ailments, Amoeba | Fl, Co, Env | St 2022 (83) |
| Hagenia abyssinica (Bruce) J.F.Gmel | Rosaceae |
Kosso (G) Hexxo (O) |
T | Wl | Ds, Fb, Fr | O, G | Tapeworms, Amoeba, Diarrhea, Gonorrhea, Febrile illness, Intestinal worms | Tm, Env, Ch | St 2022 (84) |
| Hordeum vulgare L | Poaceae |
Dinae (G) Hayixxe (O) |
H | Hg/Mt | Fs, Ds | O, G | Bone injury, Wound, Lightning | Fo, Env | St 2022 (85) |
| Lepidium sativum L | Brassicaceae |
Fexxo (G) Sinfa (O) |
H | Hg/Mt | Ds, Fr | O, G | Common cold, Febrile illness, Malaria, Vaginal infection, Dry skin treatment, Gastric diseases | Nt | St 2022 (86) |
| Maesa lanceolata Forssk | Primulaceae |
Kagaye (G) Abbaye (O) |
Sh | Wl |
Fr, Fl, Ds, Fb |
O, G | Jaundice, Nerve case, Muscular/joint pain, Skin infection, Gastric diseases, Ear infection, Amoeba, Gonorrhea, Cough | Fl, Fr, Co, Env | St 2022 (87) |
| Nuxia congesta R.Br. ex Fresen | Stilbaceae | Burcana (G,O) | T | Wl | Db, Fb | O, G | Deep sores and Cancer-like ailments, Skin infection, Wound | Co, Fl, Env, Ch | St 2022 (88) |
| Ocimum gratissimum L | Lamiaceae |
Damakase (G) Qoricha michi (O) |
Sh | Hg/Wl | Fl | O, G | Febrile illness, Fever, Eye infection, Vomiting, Malaria, Stomachache, Amoeba, Kidney infection | Fl | St 2022 (89) |
| Prunus africana (Hook.f.) Kalkman | Rosaceae | Garbicho (G,O) | T | Wl | Fb, Fs | O, G | Skin infection, Glandular, Goiter | Tm, Co, Fl, Fr, Ch, Sh | St 2022 (90) |
| Psydrax schimperianus (A.Rich.) Bridson | Rubiaceae |
Dibexxo (G) Gallo (O) |
T | Wl | Fb, Fl, Yfl | O, G | Blood pressure, Febrile illness, Skin infection, Deep sores and Cancer-like ailments, Wound, Muscle pain, Muscular/joint pain | Fl, Co, Env | St 2022 (91) |
| Searsia pyroides (Burch.) Moffett | Anacardiaceae |
Dobossa (G) Dobobessa (O) |
Sh | Wl | Fl, Fs, Ds, Dr | O, G | Deep sores and Cancer-like ailments, Autism, Passive sexual interest, Common cold, Bad/evil spirit, Epilepsy | Fl, Env | St 2022 (92) |
| Sida schimperiana Hochst. ex A.Rich | Malvaceae |
Gebresso (G) Koti jebessa (O) |
Sh | Wl | Fr, Fb, Dl, Db, Fl, Dr | O, G | Swellings, Gonorrhea, Headache, Lung infection, Toothache, Wound, Fever, Jaundice, Glandular | Env, Fl | St 2022 (93) |
| Solanecio gigas (Vatke) C.Jeffrey | Asteraceae | Dumbolla (G) Yeshikoko gomen (O) | Sh | Wl | Fs, Fl, Yr, Ds, Yfl, Fr | O, G | Lung infection, Gastric diseases, Jaundice, Malaria, Swellings, Amoeba, Diarrhea, Nasal bleeding, Glandular, Fever | Fl, Env | St 2022 (94) |
| Aframomum corrorima (A.Braun) P.C.M.Jansen | Zingiberaceae | Janjiwello | H | Hg/Mt | Ds | S | Skin infection, Tonsillitis | Sp | St 2022 (95) |
| Antiaris toxicaria (J.F.Gmel.) Lesch | Moraceae | Dimbicho | T | Wl | Fl, Fb | S | Rabies | Fl, Co | St 2022 (96) |
| Artemisia absinthium L | Asteraceae | Arity | H | Wl | Fl | S | Diabetes, Bad/evil spirit | Nt | St 2022 (97) |
| Commelina africana L | Commelinaceae | Lalunxe | H | Wl | Fl, L | S | Skin infection | Nt | St 2022 (98) |
| Coriandrum sativum L | Apiaceae | Dimbilale | H | Hg/Wl | Ds | S | Overall health | Sp | St 2022 (99) |
| Cucumis dipsaceus Ehrenb. ex Spach | Cucurbitaceae | Basu baqula | Cl | Wl | Ff | S | Jaundice | Nt | St 2022 (100) |
| Cucumis prophetarum L | Cucurbitaceae | Basu baqula | Cl | Hg/Wl | Ff, Fr, Ds, Dr | S | Deep sores and Cancer-like ailments, Amoeba, Diarrhea, Lung infection, Jaundice, Rheumatic, Balanced diet, Glandular, Respiratory organ infection | Nt | St 2022 (101) |
| Cynodon dactylon (L.) Pers | Poaceae | Qorcisha | H | Wl | Fst | S | Swellings | Env | St 2022 (102) |
| Cynoglossum coeruleum Hochst. ex A.DC | Boraginaceae | Hifaticho | H | Wl | Fl, Drh, Fr | S | Skin infection, Lung infection | Fl | St 2022 (103) |
| Dovyalis caffra (Hook.f. & Harv.) Warb | Salicaceae | Faranjete shisho | Sh | Hg/Wl | Fb | S | Snake venom | F, Fo, Fl, Co | St 2022 (104) |
| Echinops kebericho Mesfin | Asteraceae | Kebericho | H | Wl | Dr, Fr | S | Common cold, Febrile illness, Headache, Fever | Nt | St 2022 (105) |
| Euclea racemosa subsp. schimperi (A.DC.) F.White | Ebenaceae | Mi’essa | Sh | Wl | Db | S | Stomachache | Fr, Fl | St 2022 (106) |
| Vicia lens (L.) Coss. & Germ | Fabaceae | Misirra | H | Hg/Mt | Ds, Fs | S | Chickenpox, Spider poison, Wound | Fo | St 2022 (107) |
| Lippia javanica (Burm.f.) Spreng | Verbenaceae | Hanasho | Sh | Wl | Fl | S | Blood pressure | Fl, Sp, Fr | St 2022 (108) |
| Momordica boivinii Baill | Cucurbitaceae | Kiree | Cl | Wl | Fr, Fl, Ff, Ds | S | Bad/evil spirit, Lung infection, Jaundice, Stomachache, Toothache, Amoeba | Nt | St 2022 (109) |
| Premna schimperi Engl | Lamiaceae | Uddo | Sh | Wl | Fr, Fl | S | Lung infection, Febrile illness | Fl | St 2022 (110) |
| Searsia natalensis (Bernh. ex Krauss) F.A.Barkley | Anacardiaceae | Dawowesa | T | Wl | Fb, Or, Fl, Fs | S | Snake venom | Fl, Co, Sh, Env, Sh, Ch | St 2022 (111) |
| Triticum turgidum subsp. dicoccum (Schrank ex Schübl.) Thell | Poaceae | Ajja | H | Wl | Fs | S | Wound | Env, Fo | St 2022 (112) |
| Ajuga integrifolia Buch.-Ham. ex D.Don | Lamiaceae |
Amessa (S) Anamuro (G) |
H | Wl | Fl | S, G | Pain relief, Anemia, Stomachache, Malaria, Weight loss | Env | St 2022 (113) |
| Capsicum annuum L | Solanaceae |
Mixmixxa (S) Mixmixxo (G) |
H | Hg/Mt | Ff, Fl | S, G | Intestinal worms, Anemia, Common cold, Tonsillitis | Fo, Sp | St 2022 (114) |
| Cinnamomum verum J.Presl | Lauraceae |
Kerefa (S) Kereffoe (G) |
T | Wl | Db | S, G | Asthma, Common cold, Fever | Tm, Fl, Sh, Co, Env, Ch | St 2022 (115) |
| Cucurbita pepo L | Cucurbitaceae |
Baqulla (S) Buqqee (G) |
Cl | Hg/Mt | Ds | S, G | Tapeworms, Intestinal worms, Amoeba | Env | St 2022 (116) |
| Ensete ventricosum (Welw.) Cheesman | Musaceae |
Wesse (S) Werqqoo (G) |
H | Hg | Fl, Yfl | S, G | Lightning, Swellings, Amoeba, Gastric diseases | Env, Fo | St 2022 (117) |
| Galinsoga quadriradiata Ruiz & Pav | Asteraceae |
Qorcisha (S) Qoricha (G) |
H | Wl | Frw | S, G | Goiter, Tonsillitis, Toothache, Cancer, Swellings | Env | St 2022 (118) |
| Impatiens ethiopica Grey-Wilson | Balsaminaceae |
Enshoshila (S) Abebba (G) |
H | Wl | Fr, Fl | S, G | Gonorrhea | Nt | St 2022 (119) |
| Linum usitatissimum L | Linaceae |
Telba (S) Telibao (G) |
H | Hg/Wl | Ds, Drh | S, G | Gastric diseases, Blood pressure, Diabetes, Weight loss, Kidney infection, Cough, Lung infection, Tuberculosis | Fr, Env, Fo | St 2022 (120) |
| Coleus igniarius Schweinf | Lamiaceae |
Tontona (S) Tontonammo (G) |
Sh | Wl | Fl, Fr, Drh | S, G | Amoeba, Skin infection, Febrile illness, Bad/evil spirit, Wound, Stomachache, Intestinal worms | Fl, Fr, Env | St 2022 (121) |
| Solanum nigrum L | Solanaceae |
Xunayee (S) Awuxxi (G) |
Sh | Wl | Fl, S, F | S, G | Stomachache | Fo, Fr | St 2022 (122) |
| Rumex nepalensis Spreng | Polygonaceae |
Tulte (S) Gangago (G) |
H | Wl | Fr, Dl | S, G | Stomachache, Intestinal worms, Wound | Env | St 2022 (123) |
| Saccharum officinarum L | Poaceae |
Shaonkora (S) Sukari (G) |
H | Hg | Fst | S, G | Gastric diseases | Fo | St 2022 (124) |
| Thymus schimperi Ronniger | Lamiaceae |
Tosign (S) Sogetti (G) |
H | Wl | Dl, Fl | S, G | Blood pressure, Cholesterol, Bad/evil spirit | Sp, Env | St 2022 (125) |
| Trigonella foenum-graecum L | Fabaceae |
Shiqoo (S) Shiqoe (G) |
H | Hg/Wl | Ds, Fs | S, G | Cholesterol, Blood pressure, Kidney infection, Cough, Lung infection, Tuberculosis, Abnormal menstruation cycle, Weight loss, Gastric diseases, Loss of appetite, Menstruation cycle disorder, Stomachache | Sp | St 2022 (126) |
| Vicia faba L | Fabaceae |
Attarra (S) Baqello (G) |
H | Hg | Fs | S, G | Gastric diseases | Fo, Fr | St 2022 (127) |
| Aloe vera (L.) Burm.f | Asphodelaceae | Argissa (S) Algae (O) | H | Hg/Wl | Fl, L | S, O | Amoeba, Malaria, Blood pressure, Stomachache | Fl | St 2022 (128) |
| Balanites aegyptiaca (L.) Delile | Zygophyllaceae |
Gidicho (S) Bedenno (O) |
T | Wl | Ds, Fb, Fs, Dst | S, O | Amoeba, Diarrhea, Stomachache, Mental case, Headache | Fl, Co, Fr, Sh | St 2022 (129) |
| Carissa spinarum L | Apocynaceae |
Gora (S) Hagamssa (O) |
Cl | Wl | Fr, Fs, Fb, Fl | S, O | Gonorrhea, Diarrhea, Bad/evil spirit, Febrile illness, Headache | Nt | St 2022 (130) |
| Dodonaea viscosa subsp. angustifolia (L.f.) J.G.West | Sapindaceae |
Itancha (S) Xidacha (O) |
Sh | Wl | Fl, Fb, Fr | S, O | Lung infection, Headache, Bone injury, Circumcision wound, Gastric diseases, Stomachache | Fl, Fr, Env, Co | St 2022 (131) |
| Euclea divinorum Hiern | Ebenaceae |
Mi’essa (S) Miessa (O) |
Sh | Wl | Fr, Dl, Fl, Fb | S, O | Intestinal worms, Skin infection, Weight loss, Circumcision wound | Fl | St 2022 (132) |
| Mentha spicata L | Lamiaceae |
Nana (S) Naana (O) |
H | Wl | Fl, Dl | S, O | Blood pressure | Sp | St 2022 (133) |
| Ocimum jamesii Sebald | Lamiaceae |
Ambibisha (S) Hancabii (O) |
Sh | Wl | Fl | S, O | Febrile illness, Worms | Fl | St 2022 (134) |
| Persea americana Mill | Lauraceae |
Abukato (S) Abokaato (O) |
T | Hg | Ds | S, O | Passive sexual interest, Blood pressure, Amoeba | Fo, Fl, Co, Sh, Fr, Ch | St 2022 (135) |
| Pittosporum abyssinicum Delile | Pittosporaceae |
Boncho (S) Bobanticha (O) |
T | Wl | Fl, Fb | S, O | Tuberculosis, Intestinal worms | Co, Fl, Fr | St 2022 (136) |
| Rhamnus prinoides L'Hér | Rhamnaceae |
Xaaddo (S) Geshoo (O) |
Sh | Hg | Yb, Or, Fl, Fr, Fs | S, O | Tonsillitis, Gonorrhea, Skin infection, Stomachache | Fl, Fr | St 2022 (137) |
| Searsia glutinosa (Hochst. ex A.Rich.) Moffett | Anacardiaceae |
Oloncho (S) Olonchissaa (O) |
T | Wl | Fl, Fr, Db, Fb | S, O | Lung infection, Bad/evil spirit, Glandular | Co, Tm, Sh, Fl, Fr, Sh, Ch | St 2022 (138) |
| Rumex abyssinicus Jacq | Polygonaceae |
Shishone (S) Dhangogo (O) |
H | Wl | Fr, Fb | S, O | Skin infection, Gastric diseases, Amoeba, Deep sores and Cancer-like ailments | Nt | St 2022 (139) |
| Solanum incanum L | Solanaceae |
Borbodho (S) Hidhi loni (O) |
Sh | Wl | Fl, Fr | S, O | Nasal bleeding, Snake venom, Bad/evil spirit, Diarrhea | Fl, F | St 2022 (140) |
| Taverniera abyssinica A.Rich | Fabaceae |
Dingatagna (S) Dingataagnaa (O) |
Sh | Wl | Drh, Fr, Dst | S, O | Febrile illness, Fever, Headache | Nt | St 2022 (141) |
| Zehneria scabra (L.f.) Sond | Cucurbitaceae | Abajole (S) Aba ejole (O0 | Cl | Wl | Ds, Fl, Fr | S, O | Cancer, Gastric diseases, Bad/evil spirit, Swellings | Nt | St 2022 (142) |
| Achyranthes aspera L | Amaranthaceae |
Cikicho (S) Maxxane (O) Derguu (G) |
H | Wl | Fr, Fl | S, O, G | Gonorrhea, Stomachache, Headache, Muscle pain, Joint pain, Deep sores and Cancer-like ailments, Skin infection, Diarrhea, Respiratory organ infection, Bad/evil spirit, Jaundice, Lung infection, Ear infection, Nerve case | Env | St 2022 (143) |
| Acokanthera schimperi (A.DC.) Benth. & Hook.f. ex Schweinf | Apocynaceae |
Qararo (S) Qararu (O) Dumugaa (G) |
Sh | Wl | Ds, Fl, Fs | S, O, G | Bad/evil spirit, Skin infection, Wound | Fl, Sh, Fo, Env, Co | St 2022 (144) |
| Albizia gummifera (J.F.Gmel.) C.A.Sm | Fabaceae |
Maticho (S) Mukarbaa (O) Gorbe (G) |
T | Hg/Wl | Fb, Db, Fl, Fr | S, O, G | Deep sores and Cancer-like ailments, Goiter, Toothache, Dizziness, Stomachache, Jaundice, Lung infection, Amoeba, Malaria, Fire accident, Skin infection, Epilepsy, Febrile illness, Glandular, Gonorrhea, Swellings, Fever, Bad/evil spirit, Cough, Tuberculosis, Menstruation cycle disorder, Typhoid, Intestinal worms | Tm, Sh, Env, Fl, Fr, Co, Ch | St 2022 (145) |
| Allium sativum L | Amaryllidaceae |
Wajjo tuma (S) Qulubii adi (O) Dimoxxa Sunkurta (G) |
H | Hg/Mt | Fbb | S, O, G | Common cold, Malaria, Typhoid, Fever, Headache, Febrile illness, Gonorrhea, Chicken pox, Tonsillitis, Blood pressure, Skin infection, Stomachache, Asthma, Tung infection | Sp | St 2022 (146) |
| Aloe macrocarpa Tod | Asphodelaceae |
Argissa (S) Hargissa (O) Algae (G) |
H | Wl | L, Fl, Dl | S, O, G | Malaria, Jaundice, Typhoid, Fever, Deep sores and Cancer-like ailments, Lung infection, Gonorrhea, Pain relief, Urinary organ infection, Intestinal worms, Wound, Stomachache, Diarrhea | Fl | St 2022 (147) |
| Artemisia abyssinica Sch.Bip. ex Oliv. & Hiern | Asteraceae |
Ciqugn (S) Qoricha (O) Sugeete (G) |
H | Wl | Fl | S, O, G | Bad/evil spirit, Blood pressure, Malaria, Nasal bleeding, Chicken pox, Febrile illness, Skin infection, Bath of mother after giving birth, Headache | Env | St 2022 (148) |
| Bersama abyssinica Fresen | Francoaceae |
Xewerako (S) Lolichissa (O) Jejeba (G) |
T | Wl | Yb, Fl, Fs, Db, Fb, Yfl | S, O, G | Jaundice, Bad/evil spirit, Amoeba, deep sores and Cancer-like ailments, Intestinal worms, skin infection, Stomachache, Lung infection | Co, Fl, Fr, Env | St 2022 (149) |
| Brucea antidysenterica J.F.Mill | Simaroubaceae |
Laffa (S) Abalcho (O) Waginos (G) |
T | Wl | Fs, Ds, Db, Fb | S, O, G | Gonorrhea, Diarrhea, Stomachache | Tm, Co, Fl, Sh, Env, Fr | St 2022 (150) |
| Calpurnia aurea (Aiton) Benth | Fabaceae |
Cekatta (S) Cekatta/ceqaa (O) Luxxa (G) |
Sh | Wl | Fl, Fs, Ds, Dr, Fr, Fb, Dl, Dst | S, O, G | Lung infection, Typhoid, Intestinal worms, Jaundice, Bad/evil spirit, Amoeba, Headache, Stomachache, Toothache, Fever, Skin infection, Wound, Circumcision wound, Febrile illness, Deep sores and Cancer-like ailments, Deep sores and Cancer-like ailments, Swellings, Glandular, Respiratory organ infection | Fr, Env, Co, Fl, | St 2022 (151) |
| Carica papaya L | Caricaceae |
Papaye (S) Papayee (O) Papayee (G) |
T | Hg | Ds, Fs, Ff, Fl, L | S, O, G | Malaria, Intestinal worms, Gastric diseases, Fever, Bath of mother after giving birth, Blood pressure, Deep sores and Cancer-like ailments, Typhoid, Skin infection | Fo | St 2022 (152) |
| Catha edulis (Vahl) Forssk. ex Endl | Celastraceae | Catte (S, O, G) | Sh | Hg | Fr, Fl, Yfl, Or | S, O, G | Amoeba, Depression, Gonorrhea, Bad/evil spirit, Skin infection, Diarrhea | Fl, Co, Fr | St 2022 (153) |
| Citrus × aurantiifolia (Christm.) Swingle | Rutaceae |
Qomxaxxe (S) Burtukanne (O, G) |
Sh | Hg | Ds, Ff | S, O, G | Amoeba, Anemia, Blood pressure, Giardia | Fo, Fl | St 2022 (154) |
| Clematis hirsuta Perr. & Guill | Ranunculaceae |
Fidhe (S) Fidhe Fittii (O) Labbicha (G) |
Cl | Wl | Fr, Fl | S, O, G | Jaundice, Deep sores and Cancer-like ailments, Wound, Ear infection | Nt | St 2022 (155) |
| Clutia abyssinica Jaub. & Spach | Peraceae |
Binjile (S) Ullefoni (O) Binjiloo (G) |
H | Wl | Fr, Fs, Wp, Fl, L | S, O, G | Deep sores and Cancer-like ailments, Diarrhea, swellings, Spiritual, Snake venom, Wound, Toothache | Nt | St 2022 (156) |
| Coffea arabica L | Rubiaceae |
Bunna (S) Buna (O) Buno (G) |
Sh | Hg/Mt | Ds, Dl, Fl, Fb, Ffb | S, O, G | Gastric diseases, Malaria, Wound, Sneezing, Kidney infection, Swellings, Jaundice, Deep sores and Cancer-like ailments, Toothache, Depression | Fo, Fr, Co, Fl | St 2022 (157) |
| Cordia africana Lam | Boraginaceae |
Wadicho (S) Wodessa (O) Wadissa (G) |
T | Hg/Wl | Fb, Fs, Ds | S, O, G | Nerve case, Passive sexual interest, Bad/evil spirit, Blood pressure, Diarrhea, Deep sores, and Cancer-like ailments | Co, Fl, Fr, Sh, Tm, Env, Fo, Ch. Hn | St 2022 (158) |
| Croton macrostachyus Hochst. ex Delile | Euphorbiaceae |
Masinna (S) Makkonissa (O) Mokonissa (G) |
T | Hg/Wl | Fb, L, Fl, Yb, Db, Fr, Dl, Ds, Fs, L, Or | S, O, G | Deep sores and Cancer-like ailments, Eye infection, Lightning, Tetanus, Lung infection, Gonorrhea, Dizziness, Febrile illness, Wound, Bad/evil spirit, Diarrhea, Jaundice, Amoeba, Glandular, Giardia, Abortion, Intestinal worms, Malaria, Asthma, Typhoid, Skin infection, Placental delay during birth, Circumcision wound, Stomachache, Ear infection, Allergy, Menstruation cycle disorder | Co, Fl, Fr, Sh, Tm, Env, Hn | St 2022 (159) |
| Datura stramonium L. test | Solanaceae |
Banje (S) Asanjiraa (O) Atefarisse (G) |
H | Wl | Fl, Ds, Fr | S, O, G | Skin infection, Head skin infection, Toothache, Rabies | Fl | St 2022 (160) |
| Ehretia cymosa Thonn | Boraginaceae |
Gidincho (S) Ulaga (O) Suggate (G) |
T | Wl | Fl, Fb, Fs | S, O, G | Wound, Nasal bleeding, Skin infection, Lung infection, Deep sores and Cancer-like ailments, Stomachache, Swellings | Co, Fl, Fr, Sh, Tm, Env | St 2022 (161) |
| Ekebergia capensis Sparrm | Meliaceae |
Oloncho (S) Onnonna (O) Olonchissaa (G) |
T | Wl | Ds, Fb, Fs, Fl, Drh, Rb, Db | S, O, G | Amoeba, Goiter, Jaundice, Gonorrhea, Tuberculosis, Typhoid, Fever, Stomachache, Deep sores and Cancer-like ailments, Placental delay during birth, Skin infection, Bad/evil spirit, Swellings, Wound, Glandular, Diarrhea, Febrile illness | Co, Fl, Fr, Sh, Tm, Env, Ch, Hn | St 2022 (162) |
| Erythrina abyssinica Lam | Fabaceae |
Welako (S) Wallenu (O) Walenu (G) |
T | Wl | Fb, Fs, Fl, Db | S, O, G | Toothache, Bad/evil spirit, Diarrhea, Rabies, Intestinal worms, Lung infection, Goiter, Fever, Malaria, Eye infection, Cough, Skin infection, Tuberculosis, Liver infection | Co, Fl | St 2022 (163) |
| Eucalyptus globulus Labill | Myrtaceae |
Wajo barzafe (S) Bargamo addi (O) Dimmu barzafe (G) |
T | Wl | Fl | S, O, G | Asthma, Common cold, Pain relief, Bath of mother after giving birth, Fever, Mental case, Headache, Dry skin treatment, Skin infection, Bad/evil spirit, Nerve case, Nasal bleeding, Amoeba | Co, Fl, Sh, Tm | St 2022 (164) |
| Justicia schimperiana (Hochst. ex Nees) T.Anderson | Acanthaceae |
Cikicho (S) Gulbana (O) Dummugaa (G) |
Sh | Wl | Fr, Fl, Or | S, O, G | Amoeba, Rabies, Gonorrhea, Stomachache, Sneezing, Jaundice, Ear infection, Glandular, Goiter, Malaria, Epilepsy | Fl, Env | St 2022 (165) |
| Kalanchoe petitiana A.Rich | Crassulaceae |
Hanculule (S) Qorso hoxisso (O) Wundifo (G) |
H | Wl | Fl, Fr | S, O, G | A broken bone, Pain relief, Muscular/joint pain, Glandular, Diarrhea, Bone injury | Env | St 2022 (166) |
| Lactuca inermis Forssk | Asteraceae |
Ameessa (S) Anamurro (O) Anamurro (G) |
H | Wl | Fl, Wp | S, O, G | Balanced diet, Weight loss, Anemia, Febrile illness, Stomachache | Nt | St 2022 (167) |
| Lagenaria siceraria (Molina) Standl | Cucurbitaceae |
Surupha (S) Buqee (O) Boto (G) |
Cl | Wl | Or, Fr, Ds, Ff, Fl | S, O, G | Lung infection, Jaundice, Glandular, Fever, Joint pain, Amoeba, Goiter, Pain relief | Nt | St 2022 (168) |
| Melia azedarach L | Meliaceae |
Niimi (S) Kininin (O) Kinini (G) |
T | Hg | Fb, Fl, Fs, Dr, Db | S, O, G | Diabetes, Malaria, Stomachache, Depression, Diarrhea, Blood pressure, Gastric diseases, Nasal bleeding, Pain relief, Jaundice, Toothache, Deep sores and Cancer-like ailments, Intestinal worms, Typhoid, Fever, Glandular, Breast cancer | Fl, Sh, Fo, Fr, Co | St 2022 (169) |
| Millettia ferruginea (Hochst.) Hochst. ex Baker | Fabaceae |
Hengedicho (S) Birbiraa (O) Birbirro (G) |
T | Wl | Fb, Fr, Fbb, Fl, Db | S, O, G | Amoeba, Gonorrhea, Typhoid, Skin infection, Blood pressure, Stomachache, Malaria, Deep sores and Cancer-like ailments, Jaundice, Toothache, Ear infection, Goiter, Lung infection, Pain relief | Co, Fl, Fr, Sh, Tm, Env, Hn | St 2022 (170) |
| Moringa stenopetala (Baker f.) Cufod | Moringaceae | Shiferaw (S, O, G) | T | Hg/Mt | Dl, Fb, Fl, Fr, Db | S, O, G | Blood pressure, Glandular, Jaundice, Malaria, Diarrhea, Kidney infection, Lung infection, Deep sores and Cancer-like ailments, Gastric diseases, Cholesterol, Nerve case, Pain relief, Intestinal worms, Typhoid | Fo, Fl, Co, Env, Fr | St 2022 (171) |
| Nicotiana tabacum L | Solanaceae |
Araddo (S) Tambo (O) Tambo (G) |
H | Hg | Dl | S, O, G | Headache, Wound, Depression, Common cold | Fl | St 2022 (172) |
| Nigella sativa L | Ranunculaceae |
Wajjo azmude (S) Qoricha adi (O) Azmuddo (G) |
H | Hg/Mt | Ds | S, O, G | Common cold, Respiratory organ infection, Febrile illness, Skin infection, Amoeba, Nasal bleeding, Fever, Malaria, Asthma, Pain relief, Stomachache, Nerve case, Bone injury, Deep sores and Cancer-like ailments | Sp | St 2022 (173) |
| Ocimum lamiifolium Hochst. ex Benth | Lamiaceae |
Michete xagicho (S) Qorsa mich I (O) Damakase (G) |
Sh | Wl | Fl, Fr | S, O, G | Headache, Malaria, Febrile illness, Fever, Stomachache, Muscular/joint pain, Amoeba, Gonorrhea, Typhoid, Diarrhea | Fl | St 2022 (174) |
| Olea europaea subsp. cuspidata (Wall. & G.Don) Cif | Oleaceae |
Ejerissa (S) Ejerissa (O) Woyira (G) |
T | Wl | Dst, Fs, Fl, Fb, Fr, Yp, Db | S, O, G | Deep sores and Cancer-like ailments, Skin infection, Wound, Anemia, Blood pressure, Cough, Malaria, Respiratory organ infection, Bad/evil spirit, Tuberculosis, Jaundice, Cancer, Swellings, Toothache, Kidney infection, Vaginal infection, Intestinal worms, Pain relief, Asthma | Co, Fl, Fr, Sh, Tm, Env, Ch | St 2022 (175) |
| Olinia rochetiana A.Juss | Penaeaceae |
Noole (S) Gunna (O) Dimexxo (G) |
T | Wl | Fl, Fb, Dl, Db | S, O, G | Stomachache, Glandular, Skin infection, Wound, Circumcision wound, Toothache, Deep sores and Cancer-like ailments, Tuberculosis | Co, Fl, Fr, Sh, Tm, Env, Ch | St 2022 (176) |
| Phytolacca dodecandra L'Hér | Phytolaccaceae |
Haranjicho (S) Andodde (O) Indoode (G) |
Sh | Wl | Fr, Fl, Or, Yr | S, O, G | Abortion, Amoeba, Intestinal worms, Gonorrhea, Swellings, Giardia, Stomachache, Skin infection | Fl | St 2022 (177) |
| Afrocarpus falcatus (Thunb.) C.N.Page | Podocarpaceae |
Dagucho (S) Zigbaa (O) Zigbo (G) |
T | Wl | Fl, Fb, Db | S, O, G | Gonorrhea, Typhoid, Malaria, Jaundice, Deep sores and Cancer-like ailments, Wound, Glandular, Toothache, Amoeba | Co, Fl, Fr, Sh, Tm, Env, Ch | St 2022 (178) |
| Psidium guajava L | Myrtaceae |
Zaytone (S) Zaytunna (O) Zayitunne (G) |
T | Hg | Fl, Dl | S, O, G | Blood pressure, Malaria, Diabetes, Stomachache, Deep sores and Cancer-like ailments, Intestinal worms, Typhoid | Co, Fl, Fo, Fr, Env, Ch | St 2022 (179) |
| Ricinus communis L | Euphorbiaceae |
Qomboho (S) Qobboo (O) Gullo (G) |
Sh | Hg | Fr, Ds, Yr, Fs | S, O, G | Jaundice, Lung infection, Swellings, Tonsillitis, Wound, Skin infection | Co, Fl, F | St 2022 (180) |
| Ruta chalepensis L | Rutaceae |
Sunkurta (S) Ciradamma (O) Xenadame (G) |
H | Hg | Fl, Fr, Frw, Dl | S, O, G | Gonorrhea, Typhoid, Febrile illness, Goiter, Tuberculosis, Skin infection, Diarrhea, Bad/evil spirit, Malaria, Vomiting, Nerve case, Dry skin treatment, Stomachache, Giardia, Jaundice, Nasal bleeding, Placental delay during birth, Epilepsy, Swellings, Asthma, Headache, Anemia, Glandular, Deep sores and Cancer-like ailments, Bath of mother after giving a birth, Menstruation cycle disorder | Nt | St 2022 (181) |
| Stephania abyssinica (Quart.-Dill. & A.Rich.) Walp | Menispermaceae |
Kelala (S, O) Kelaalaa (G) |
Cl | Wl | Fl, Fr | S, O, G | Jaundice, Glandular, Lung infection, Gonorrhea, Deep sores and Cancer-like ailments | Nt | St 2022 (182) |
| Syzygium guineense (Willd.) DC | Myrtaceae |
Duwancho (S) Badessa (O) Baddessa (G) |
T | Wl | Fb, Fl, Dr, Dl, Fr, Yr | S, O, G | Amoeba, Diarrhea, Muscle pain, Bad/evil spirit, Skin infection, Lung infection, Weight loss, Glandular, Circumcision wound, Pain relief, Swellings, Deep sores and Cancer-like ailments | Co, Fl, Fr, Sh, Tm, Env, Ch | St 2022 (183) |
| Urtica dioica L | Urticaceae |
Sonicho (S) Lalesa (O) Sonno (G) |
H | Wl | Fr, Dr | S, O, G | Amoeba, Bad/evil spirit, Gonorrhea, Febrile illness, Deep sores and Cancer-like ailments | Fl | St 2022 (184) |
| Urtica simensis Hochst. ex A.Rich | Urticaceae |
Sonicho (S) Lalesa (O) Sonno (G) |
H | Wl | Fl, Fr, Dr | S, O, G | Bad/evil spirit, Fire accident, Febrile illness, Gastric diseases, Amoeba, Intestinal worms, Stomachache | Fl | St 2022 (185) |
| Gymnanthemum amygdalinum (Delile) Sch.Bip | Asteraceae |
Hecho (S) Ebicha (O) Ebicha (G) |
Sh | Wl | Fl, Fr, Yr | S, O, G | Amoeba, Malaria, Skin infection, Stomachache, Diarrhea, Head skin infection, Gonorrhea, Rabies, Febrile illness, Intestinal worms, Gastric diseases, Lung infection, Blood pressure, Jaundice, Vomiting, Typhoid | Fr, Fl, Co, Env, Hn | St 2022 (186) |
| Gymnanthemum auriculiferum (Hiern) Isawumi | Asteraceae |
Rejee (S) Rejii (O) Ebicha (G) |
Sh | Wl | Fl, Fr | S, O, G | Bad/evil spirit, Snake venom, Bath of mother after giving birth | Fl, Fr, Co, Env | St 2022 (187) |
| Withania somnifera (L.) Dunal | Solanaceae |
Bula (S) Kummo (O) Bulla (G) |
Sh | Wl | Fl, Fb, Ds, Fr, Db, OrDst, | S, O, G | Bad/evil spirit, Asthma, Cough, Skin infection, Febrile illness | Fl, Co | St 2022 (188) |
| Zingiber officinale Roscoe | Zingiberaceae |
Janjiwello (S) Zinjibilla (O) Jaanjibeloo (G) |
H | Hg/Mt | Drh, Frh | S, O, G | Asthma, Blood pressure, Passive sexual interest, Common cold, Tonsillitis, Typhoid, Headache, Malaria, Wound, Fever, Cough, Tung infection, Goiter, Constipation, Febrile illness, Amoeba, Gastric diseases, Stomachache | Sp | St 2022 (189) |
(Ha = Habit, T = Tree, Sh = Shrub, H = Herb, Cl = Climber, Ep = Epiphyte, Pu = Parts used, Fl = Fresh leaf, Yfl = Young fresh leaf, Dl = Dry leaf, Fs = Fresh seed, Ds = Dry seed, Fr = Fresh root, Dr = Dry root, Or = Old root, Yr = Young root, Fb = Fresh bark, Db = Dry bark, Ff = Fresh fruit, L = Latex, Fbb = Fresh bulb, Drh = Dry rhizome, Frh = Fresh rhizome, Yl = Young leaf, Yr = Young root, Ffb = Fresh fruit bark, As = Ash, Yb = Young bud, Fst = Fresh stolon, Frw = Fresh flower, Fst = Fresh stem, Drs = Dry stem, Wp = Whole parts, Rb Root bark, Yp = Young petiole, Fl = Fuel wood, Env = Environmental role, F = Fence, Sh = Shading, Ch = Charcoal, Tm = Timber, Fo = Food, Co = Construction, Fr = Fodder, Nt = Not mentioned, Sp = Spice, Hn = Honey production)
Influences of socio-demographic variables on medicinal plant knowledge
The average number of medicinal plants reported by each socio-demographic variable was compared. It revealed that older traditional healers reported more medicinal plants (8) than others (Table 4 and Fig. 2A). Medicinal plants reported by followers of the Orthodox religion were higher (9) than Protestants and Muslims (Table 4 and Fig. 2D). The gender groups and education level categories reported a similar number of medicinal plants (7 each) (Table 4 and Fig. 2B).
Table 4.
Comparison of the number of medicinal plants cited by different socio-demographic parameters across ethnic groups (Gedeo, Oromo, and Sidama)
| Parameters | Categories | Number of informants (N = 189) | Mean ± SD | p-value |
|---|---|---|---|---|
| Age | Young (35–44) | 33 | 4.73 ± 0.94 | 0.0001* |
| Middle age (45–54) | 45 | 6.84 ± 1.74 | ||
| Older (55–64) | 88 | 7.9 ± 1.72 | ||
| Elderly (65 +) | 23 | 5.09 ± 1.47 | ||
| Gender | Male | 133 | 6.76 ± 2.02 | 0.77 |
| Female | 56 | 6.73 ± 2.09 | ||
| Education | Illiterate | 89 | 6.74 ± 2.03 | 0.54 |
| Primary level | 81 | 6.86 ± 2.09 | ||
| Secondary level | 19 | 6.37 ± 1.89 | ||
| Religion | Protestant | 101 | 6.51 ± 2.04 | 0.11 |
| Islam | 75 | 7.04 ± 1.95 | ||
| Orthodox | 13 | 8.33 ± 3.21 |
*Significance association (p < 0.05) between the averages of paired parameters
Fig. 2.
Average number of medicinal plants reported by each socio-demographic variables
Our findings revealed a positive association between traditional healers' ethnobotanical knowledge and their ages (Kruskal–Wallis chi-squared = 84.375, df = 3, p-value = 0.0001) (Table 4). However, no significant association was found between the gender, education, and religion groups and ethnobotanical knowledge (p-value = 0.77, 0.54, and 0.11), respectively (Table 4).
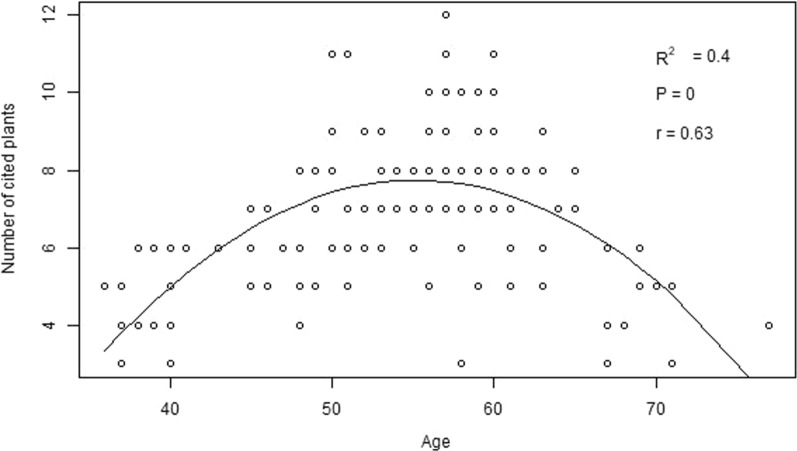
The correlation between ethnobotanical knowledge and age
The regression analyses across ethnic groups showed that the respondent's age is positively correlated with his/her knowledge of identifying medicinal plants used; however, it showed a curvilinear relationship at the end (Fig. 3). Overall, the influence of age accounted for 37% of the variation in knowledge of medicinal plants across ethnic groups.
Fig. 3.
Correlation between the respondent's knowledge of medicinal plant citation and his or her age
The most useful medicinal plant species of the studied ethnic groups
The use value index (UVI) is applied to measure various uses assigned to a specific plant species. Of the total 189 documented medicinal plants (Table 3), 78 medicinal plant species, which were claimed by three or more informants as remedies, were evaluated and revealed significant species use variation among the ethnic groups studied (Table 5). Meanwhile, 24 medicinal plant species scored the lowest use value; others were moderate to highest value (Table 5).
Table 5.
The use value index of the most important medicinal plant species among ethnic groups
| Species | Ethnic groups | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gedeo | Oromo | Sidama | ||||||||||
| Basic values | Index | Basic values | Index | Basic values | Index | |||||||
| FC | UR | NU | UV | FC | UR | NU | UV | FC | UR | NU | UV | |
| Vachellia oerfota (Forssk.) Kyal. & Boatwr | – | – | – | – | 8 | 8 | 2 | 0.127 | – | – | – | – |
| Achyranthes aspera L | 4 | 6 | 5 | 0.1 | 7 | 7 | 5 | 0.111 | 4 | 7 | 6 | 0.111 |
| Ajuga integrifolia Buch.-Ham. ex D.Don | – | – | – | – | – | – | – | – | 10 | 12 | 5 | 0.19 |
| Albizia gummifera (J.F.Gmel.) C.A.Sm | 20 | 47 | 20 | 0.75 | 6 | 10 | 7 | 0.159 | 7 | 13 | 8 | 0.206 |
| Allium sativum L | 4 | 11 | 7 | 0.18 | 5 | 12 | 6 | 0.19 | 8 | 23 | 9 | 0.365 |
| Aloe macrocarpa Tod | – | – | – | – | 16 | 38 | 14 | 0.603 | – | – | – | – |
| Aloe vera (L.) Burm.f | – | – | – | – | – | – | – | – | 5 | 6 | 4 | 0.095 |
| Argemone mexicana L | – | – | – | – | 5 | 5 | 4 | 0.079 | – | – | – | – |
| Artemisia abyssinica Sch.Bip. ex A.Rich | 6 | 11 | 6 | 0.18 | – | – | – | – | – | – | – | – |
| Asparagus africanus Lam | 10 | 13 | 7 | 0.21 | 6 | 6 | 5 | 0.095 | – | – | – | – |
| Balanites aegyptiaca (L.) Delile | – | – | – | – | – | – | – | – | 4 | 7 | 3 | 0.111 |
| Bersama abyssinica Fresen | 4 | 5 | 4 | 0.08 | – | – | – | – | – | – | – | – |
| Calpurnia aurea (Aiton) Benth | 19 | 31 | 13 | 0.49 | 11 | 14 | 9 | 0.222 | 4 | 5 | 5 | 0.079 |
| Carica papaya L | – | – | – | – | 4 | 7 | 6 | 0.111 | 7 | 10 | 4 | 0.159 |
| Carissa spinarum L | – | – | – | – | 6 | 6 | 3 | 0.095 | – | – | – | – |
| Catha edulis (Vahl) Forssk. ex Endl | – | – | – | – | – | – | – | – | 7 | 9 | 4 | 0.143 |
| Celtis africana Burm.f | 10 | 18 | 11 | 0.29 | – | – | – | – | – | – | – | – |
| Cinnamomum verum J.Presl | – | – | – | – | – | – | – | – | 3 | 5 | 3 | 0.079 |
| Citrus limon (L.) Osbeck | – | – | – | – | 6 | 11 | 5 | 0.175 | – | – | – | – |
| Clutia abyssinica Jaub. & Spach | – | – | – | – | 6 | 7 | 6 | 0.111 | 6 | 6 | 4 | 0.095 |
| Coffea arabica L | 9 | 12 | 8 | 0.19 | 5 | 9 | 5 | 0.143 | – | – | – | – |
| Croton macrostachyus Hochst. ex Delile | 28 | 80 | 21 | 1.3 | 21 | 48 | 22 | 0.80 | 17 | 36 | 15 | 0.60 |
| Cucumis prophetarum L | – | – | – | – | – | – | – | – | 14 | 20 | 9 | 0.317 |
| Cymbopogon citratus (DC.) Stapf | 5 | 15 | 9 | 0.24 | – | – | – | – | – | – | – | – |
| Datura stramonium L. test | – | – | – | – | 6 | 6 | 3 | 0.095 | – | – | – | – |
| Dodonaea viscosa subsp. angustifolia (L.f.) J.G.West | – | – | – | – | 8 | 9 | 6 | 0.143 | – | – | – | – |
| Drynaria volkensii Heiron | 4 | 6 | 4 | 0.1 | – | – | – | – | – | – | – | – |
| Echinops kebericho Mesfin | – | – | – | – | – | – | – | – | 4 | 10 | 4 | 0.159 |
| Ehretia cymosa Thonn | – | – | – | – | – | – | – | – | 5 | 5 | 5 | 0.079 |
| Ekebergia capensis Sparrm | 5 | 9 | 5 | 0.14 | 6 | 14 | 10 | 0.222 | 15 | 20 | 8 | 0.317 |
| Ensete ventricosum (Welw.) Cheesman | 6 | 7 | 4 | 0.11 | – | – | – | – | – | – | – | – |
| Erythrina abyssinica Lam | 6 | 10 | 8 | 0.16 | 6 | 6 | 6 | 0.095 | – | – | – | – |
| Eucalyptus globulus Labill | 5 | 7 | 5 | 0.11 | 9 | 16 | 5 | 0.254 | 9 | 20 | 11 | 0.317 |
| Galinsoga quadriradiata Ruiz & Pav | 7 | 9 | 4 | 0.14 | – | – | – | – | – | – | – | – |
| Grewia ferruginea Hochst. ex A.Rich | 5 | 9 | 8 | 0.14 | – | – | – | – | – | – | – | – |
| Hagenia abyssinica (Bruce) J.F.Gmel | – | – | – | – | 5 | 7 | 5 | 0.111 | – | – | – | – |
| Justicia schimperiana (Hochst. ex Nees) T.Anderson | 6 | 8 | 5 | 0.13 | 9 | 11 | 4 | 0.175 | 8 | 9 | 5 | 0.143 |
| Kalanchoe petitiana A.Rich | – | – | – | – | – | – | – | – | 6 | 7 | 5 | 0.111 |
| Lactuca inermis Forssk | 4 | 9 | 3 | 0.14 | – | – | – | – | – | – | – | – |
| Lagenaria siceraria (Molina) Standl | 3 | 5 | 4 | 0.08 | – | – | – | – | 5 | 6 | 3 | 0.095 |
| Linum usitatissimum L | – | – | – | – | – | – | – | – | 4 | 8 | 5 | 0.127 |
| Maesa lanceolata Forssk | 7 | 9 | 7 | 0.14 | – | – | – | – | – | – | – | – |
| Melia azedarach L | 3 | 6 | 6 | 0.1 | 11 | 16 | 11 | 0.254 | 8 | 15 | 9 | 0.238 |
| Millettia ferruginea (Hochst.) Hochst. ex Baker | 6 | 12 | 10 | 0.19 | – | – | – | – | – | – | – | – |
| Momordica boivinii Baill | – | – | – | – | – | – | – | – | 7 | 7 | 6 | 0.111 |
| Moringa stenopetala (Baker f.) Cufod | 4 | 9 | 5 | 0.14 | 13 | 25 | 14 | 0.397 | 3 | 5 | 2 | 0.079 |
| Nigella sativa L | 3 | 7 | 7 | 0.11 | 7 | 12 | 10 | 0.19 | – | – | – | – |
| Ocimum jamesii Sebald | – | – | – | – | – | – | – | – | 5 | 5 | 1 | 0.079 |
| Ocimum lamiifolium Hochst. ex Benth | 3 | 6 | 6 | 0.1 | – | – | – | – | – | – | – | – |
| Ocimum gratissimum L | 7 | 15 | 6 | 0.24 | 8 | 14 | 6 | 0.222 | – | – | – | – |
| Olea europaea subsp. cuspidata (Wall. & G.Don) Cif | 9 | 11 | 6 | 0.18 | 11 | 25 | 18 | 0.397 | – | – | – | – |
| Olinia rochetiana A.Juss | – | – | – | – | 12 | 13 | 8 | 0.206 | – | – | – | – |
| Phytolacca dodecandra L'Hér | 3 | 5 | 5 | 0.08 | – | – | – | – | 9 | 14 | 7 | 0.222 |
| Coleus igniarius Schweinf | – | – | – | – | – | – | – | – | 8 | 13 | 6 | 0.206 |
| Afrocarpus falcatus (Thunb.) C.N.Page | 16 | 26 | 10 | 0.41 | – | – | – | – | – | – | – | – |
| Psidium guajava L | – | – | – | – | 3 | 6 | 4 | 0.095 | – | – | – | – |
| Psydrax schimperianus (A.Rich.) Bridson | – | – | – | – | 5 | 7 | 5 | 0.111 | – | – | – | – |
| Searsia glutinosa (Hochst. ex A.Rich.) Moffett | – | – | – | – | – | – | – | – | 12 | 13 | 3 | 0.206 |
| Ricinus communis L | 5 | 9 | 4 | 0.14 | – | – | – | – | 3 | 7 | 5 | 0.111 |
| Rotheca myricoides (Hochst.) Steane & Mabb | – | – | – | – | – | – | – | – | 11 | 16 | 7 | 0.254 |
| Rubus steudneri Schweinf | – | – | – | – | 4 | 8 | 8 | 0.127 | – | – | – | – |
| Ruta chalepensis L | 15 | 28 | 17 | 0.44 | 9 | 19 | 13 | 0.302 | 14 | 21 | 8 | 0.333 |
| Schinus molle L | – | – | – | – | 4 | 6 | 3 | 0.095 | – | – | – | – |
| Searsia natalensis (Bernh. ex Krauss) F.A.Barkley | – | – | – | – | – | – | – | – | 7 | 7 | 1 | 0.111 |
| Sida schimperiana Hochst. ex A.Rich | 4 | 6 | 6 | 0.1 | – | – | – | – | – | – | – | – |
| Solanecio gigas (Vatke) C.Jeffrey | 13 | 20 | 10 | 0.32 | – | – | – | – | – | – | – | – |
| Solanum incanum L | – | – | – | – | 5 | 9 | 3 | 0.143 | 6 | 6 | 3 | 0.095 |
| Solanum marginatum L.f | – | – | – | – | 5 | 7 | 6 | 0.111 | – | – | – | – |
| Stephania abyssinica (Quart.-Dill. & A.Rich.) Walp | – | – | – | – | – | – | – | – | 6 | 6 | 2 | 0.095 |
| Syzygium guineense (Willd.) DC | 4 | 6 | 5 | 0.1 | 5 | 6 | 5 | 0.095 | 4 | 6 | 4 | 0.095 |
| Vepris nobilis (Delile) Mziray | – | – | – | – | 4 | 6 | 5 | 0.095 | – | – | – | – |
| Trigonella foenum-graecum L | 4 | 12 | 10 | 0.19 | – | – | – | – | – | – | – | – |
| Urtica simensis Hochst. ex A.Rich | – | – | – | – | – | – | – | – | 6 | 6 | 2 | 0.095 |
| Gymnanthemum amygdalinum (Delile) Sch.Bip | 11 | 17 | 8 | 0.27 | 21 | 34 | 15 | 0.54 | 13 | 25 | 6 | 0.397 |
| Vicia faba L | 6 | 6 | 1 | 0.1 | – | – | – | – | 10 | 10 | 1 | 0.159 |
| Withania somnifera (L.) Dunal | – | – | – | – | 5 | 8 | 5 | 0.127 | 8 | 10 | 3 | 0.159 |
| Zingiber officinale Roscoe | 3 | 7 | 5 | 0.11 | 8 | 16 | 11 | 0.254 | 12 | 46 | 13 | 0.70 |
| Ziziphus spina-christi (L.) Willd | – | – | – | – | 4 | 10 | 8 | 0.159 | – | – | – | – |
N.B: Broken lines indicate the absence of a citation for the indicated species in the study area
Informant consensus factor
Based on disease characteristics and treatment resemblances, fourteen (14) disease categories were identified from the 100 human ailments reported in the study areas (Table 3). Among these, the categories with the highest average ICF values among ethnic groups were circulatory system disorders (0.68), followed by febrile illness, reproductive organ disorders, and bad/evil spirit-related complications (0.66 each) across the studied ethnic groups (Table 6). In comparison, the highest plant use citation was noted for digestive system disorders, which are 100, 102, and 117 in the Sidama, Oromo, and Gedeo ethnic groups, respectively, followed by febrile illness (115, 94, and 87) in the Sidama, Oromo, and Gedeo ethnic groups (Table 6).
Table 6.
A detailed informant consensus factor of the three ethnic groups (Sidama (S), Gedeo (G), and Oromo (O))
| Category | Ailment | Species | Use report | No of species | ICF | Ethnic group |
|---|---|---|---|---|---|---|
| Deep sores and Cancer-like ailments | Deep sores and Cancer-like ailments | Asparagus africanus Lam., Calpurnia aurea (Aiton) Benth., Coffea arabica L., Croton macrostachyus Hochst. ex Delile, Olea europaea subsp. cuspidata (Wall. & G.Don) Cif., Afrocarpus falcatus (Thunb.) C.N.Page, Ruta chalepensis L | 9 | 7 | 0.25 | G |
| Deep sores and Cancer-like ailments | Deep sores and Cancer-like ailments | Aloe macrocarpa Tod., Croton macrostachyus Hochst. ex Delile, Olea europaea subsp. cuspidata (Wall. & G.Don) Cif | 4 | 3 | 0.33 | O |
| Deep sores and Cancer-like ailments | Deep sores and Cancer-like ailments | Albizia gummifera (J.F.Gmel.) C.A.Sm., Asparagus africanus Lam., Calpurnia aurea (Aiton) Benth., Croton macrostachyus Hochst. ex Delile, Cymbopogon citratus (DC.) Stapf, Galinsoga quadriradiata Ruiz & Pav., Moringa stenopetala (Baker f.) Cufod., Olea europaea subsp. cuspidata (Wall. & G.Don) Cif., Afrocarpus falcatus (Thunb.) C.N.Page | 27 | 9 | 0.69 | G |
| Deep sores and Cancer-like ailments | Deep sores and Cancer-like ailments | Aloe macrocarpa Tod., Coffea arabica L., Croton macrostachyus Hochst. ex Delile, Melia azedarach L., Moringa stenopetala (Baker f.) Cufod., Olea europaea subsp. cuspidata (Wall. & G.Don) Cif., Olinia rochetiana A.Juss., Psidium guajava L., Psydrax schimperianus (A.Rich.) Bridson | 13 | 9 | 0.33 | O |
| Deep sores and Cancer-like ailments | Deep sores and Cancer-like ailments | Albizia gummifera (J.F.Gmel.) C.A.Sm., Clutia abyssinica Jaub. & Spach, Croton macrostachyus Hochst. ex Delile, Cucumis prophetarum L., Rotheca myricoides (Hochst.) Steane & Mabb | 11 | 5 | 0.6 | S |
| Circulatory system | Anemia | Lactuca inermis Forssk., Ruta chalepensis L | 5 | 2 | 0.75 | G |
| Circulatory system | Anemia | Ajuga integrifolia Buch.-Ham. ex D.Don | 4 | 1 | 1 | S |
| Circulatory system | Blood pressure | Allium sativum L., Cymbopogon citratus (DC.) Stapf, Moringa stenopetala (Baker f.) Cufod., Olea europaea subsp. cuspidata (Wall. & G.Don) Cif., Trigonella foenum-graecum L | 12 | 5 | 0.64 | G |
| Circulatory system | Blood pressure | Allium sativum L., Citrus limon (L.) Osbeck, Melia azedarach L., Moringa stenopetala (Baker f.) Cufod., Olea europaea subsp. cuspidata (Wall. & G.Don) Cif., Psidium guajava L., Psydrax schimperianus (A.Rich.) Bridson, Gymnanthemum amygdalinum (Delile) Sch.Bip., Zingiber officinale Roscoe | 26 | 9 | 0.68 | O |
| Circulatory system | Blood pressure | Linum usitatissimum L., Melia azedarach L., Moringa stenopetala (Baker f.) Cufod., Zingiber officinale Roscoe | 8 | 4 | 0.57 | S |
| Circulatory system | Snake venom | Gymnanthemum auriculiferum (Hiern) Isawumi | 3 | 1 | 1 | G |
| Circulatory system | Snake venom | Solanum incanum L | 4 | 1 | 1 | O |
| Circulatory system | Snake venom | Searsia natalensis (Bernh. ex Krauss) F.A.Barkley | 7 | 1 | 1 | S |
| Dermal | Allergy | Croton macrostachyus Hochst. ex Delile | 5 | 1 | 1 | G |
| Dermal | Bath of mother after giving birth | Artemisia abyssinica Sch.Bip. ex A.Rich., Cymbopogon citratus (DC.) Stapf, Ruta chalepensis L., Gymnanthemum auriculiferum (Hiern) Isawumi | 6 | 4 | 0.4 | G |
| Dermal | Circumcision wound | Calpurnia aurea (Aiton) Benth., Croton macrostachyus Hochst. ex Delile, Dodonaea viscosa subsp. angustifolia (L.f.) J.G.West, Olinia rochetiana A.Juss | 8 | 4 | 0.57 | O |
| Dermal | Epilepsy | Asparagus africanus Lam., Justicia schimperiana T.Anderson., Ruta chalepensis L | 4 | 3 | 0.33 | G |
| Dermal | Eye infection | Croton macrostachyus Hochst. ex Delile, Erythrina abyssinica Lam | 5 | 2 | 0.75 | G |
| Dermal | Eye infection | Croton macrostachyus Hochst. ex Delile, Ocimum gratissimum L | 4 | 2 | 0.67 | O |
| Dermal | Eye infection | Croton macrostachyus Hochst. ex Delile | 3 | 1 | 1 | S |
| Dermal | Skin infection | Albizia gummifera (J.F.Gmel.) C.A.Sm., Allium sativum L., Artemisia abyssinica Sch.Bip. ex A.Rich., Asparagus africanus Lam., Celtis africana Burm.f., Croton macrostachyus Hochst. ex Delile, Erythrina abyssinica Lam., Maesa lanceolata Forssk., Olea europaea subsp. cuspidata (Wall. & G.Don) Cif., Ricinus communis L., Gymnanthemum amygdalinum (Delile) Sch.Bip | 19 | 11 | 0.44 | G |
| Dermal | Skin infection | Calpurnia aurea (Aiton) Benth., Croton macrostachyus Hochst. ex Delile, Datura stramonium L. test, Olinia rochetiana A.Juss., Psydrax schimperianus (A.Rich.) Bridson, Gymnanthemum amygdalinum (Delile) Sch.Bip., Withania somnifera (L.) Dunal | 16 | 7 | 0.6 | O |
| Dermal | Skin infection | Datura stramonium L. test, Eucalyptus globulus Labill., Coleus igniarius Schweinf., Rotheca myricoides (Hochst.) Steane & Mabb., Ruta chalepensis L., Gymnanthemum amygdalinum (Delile) Sch.Bip | 14 | 6 | 0.62 | S |
| Dermal | Swellings | Albizia gummifera (J.F.Gmel.) C.A.Sm., Asparagus africanus Lam., Calpurnia aurea (Aiton) Benth., Coffea arabica L., Ekebergia capensis Sparrm., Ensete ventricosum (Welw.) Cheesman, Galinsoga quadriradiata Ruiz & Pav., Ricinus communis L., Ruta chalepensis L., Solanecio gigas (Vatke) C.Jeffrey | 29 | 10 | 0.68 | G |
| Dermal | Swellings | Olea europaea subsp. cuspidata (Wall. & G.Don) Cif., Ricinus communis L | 5 | 2 | 0.75 | O |
| Dermal | Swellings | Clutia abyssinica Jaub. & Spach, Phytolacca dodecandra L'Hér., Ricinus communis L | 5 | 3 | 0.5 | S |
| Dermal | Tetanus | Croton macrostachyus Hochst. ex Delile | 3 | 1 | 1 | S |
| Dermal | Wound | Calpurnia aurea (Aiton) Benth., Celtis africana Burm.f., Coffea arabica L., Croton macrostachyus Hochst. ex Delile, Afrocarpus falcatus (Thunb.) C.N.Page, Ricinus communis L | 10 | 6 | 0.44 | G |
| Dermal | Wound | Aloe macrocarpa Tod., Calpurnia aurea (Aiton) Benth., Coffea arabica L., Croton macrostachyus Hochst. ex Delile, Olea europaea subsp. cuspidata (Wall. & G.Don) Cif., Olinia rochetiana A.Juss., Psydrax schimperianus (A.Rich.) Bridson, Zingiber officinale Roscoe | 13 | 8 | 0.42 | O |
| Dermal | Wound | Croton macrostachyus Hochst. ex Delile, Coleus igniarius Schweinf, Ricinus communis L., Zingiber officinale Roscoe | 12 | 4 | 0.73 | S |
| Digestive system | Amoeba | Albizia gummifera (J.F.Gmel.) C.A.Sm., Calpurnia aurea (Aiton) Benth., Croton macrostachyus Hochst. ex Delile, Ekebergia capensis Sparrm., Ensete ventricosum (Welw.) Cheesman, Maesa lanceolata Forssk., Ocimum gratissimum L., Afrocarpus falcatus (Thunb.) C.N.Page, Solanecio gigas (Vatke) C.Jeffrey, Gymnanthemum amygdalinum (Delile) Sch.Bip | 23 | 10 | 0.59 | G |
| Digestive system | Amoeba | Calpurnia aurea (Aiton) Benth., Citrus limon (L.) Osbeck, Croton macrostachyus Hochst. ex Delile, Hagenia abyssinica (Bruce) J.F.Gmel., Gymnanthemum amygdalinum (Delile) Sch.Bip., Zingiber officinale Roscoe | 11 | 6 | 0.5 | O |
| Digestive system | Amoeba | Albizia gummifera (J.F.Gmel.) C.A.Sm., Balanites aegyptiaca (L.) Delile, Catha edulis (Vahl) Forssk. ex Endl., Croton macrostachyus Hochst. ex Delile, Cucumis prophetarum L., Ekebergia capensis Sparrm., Justicia schimperiana (Hochst. ex Nees) T.Anderson, Phytolacca dodecandra L'Hér., Coleus igniarius Schweinf., Rotheca myricoides (Hochst.) Steane & Mabb., Gymnanthemum amygdalinum (Delile) Sch.Bip | 35 | 11 | 0.71 | S |
| Digestive system | Diarrhea | Brucea antidysenterica J.F.Mill., Celtis africana Burm.f., Croton macrostachyus Hochst. ex Delile, Ekebergia capensis Sparrm., Solanecio gigas (Vatke) C.Jeffrey, Gymnanthemum amygdalinum (Delile) Sch.Bip | 11 | 6 | 0.5 | G |
| Digestive system | Diarrhea | Aloe macrocarpa Tod., Croton macrostachyus Hochst. ex Delile, Hagenia abyssinica (Bruce) J.F.Gmel., Melia azedarach L., Moringa stenopetala (Baker f.) Cufod., Solanum incanum L., Gymnanthemum amygdalinum (Delile) Sch.Bip | 12 | 7 | 0.45 | O |
| Digestive system | Diarrhea | Balanites aegyptiaca (L.) Delile, Clutia abyssinica Jaub. & Spach, Croton macrostachyus Hochst. ex Delile, Cucumis prophetarum L., Melia azedarach L., Rotheca myricoides (Hochst.) Steane & Mabb., Ruta chalepensis L., Gymnanthemum amygdalinum (Delile) Sch.Bip | 14 | 8 | 0.46 | S |
| Digestive system | Gastric diseases | Ensete ventricosum (Welw.) Cheesman, Maesa lanceolata Forssk., Solanecio gigas (Vatke) C.Jeffrey, Trigonella foenum-graecum L., Vicia faba L | 11 | 5 | 0.6 | G |
| Digestive system | Gastric diseases | Coffea arabica L., Dodonaea viscosa subsp. angustifolia (L.f.) J.G.West, Moringa stenopetala (Baker f.) Cufod., Gymnanthemum amygdalinum (Delile) Sch.Bip., Zingiber officinale Roscoe | 6 | 5 | 0.2 | O |
| Digestive system | Gastric diseases | Carica papaya L., Linum usitatissimum L., Melia azedarach L., Saccharum officinarum L., Vicia faba L | 19 | 5 | 0.78 | S |
| Digestive system | Giardia | Croton macrostachyus Hochst. ex Delile, Ruta chalepensis L | 3 | 2 | 0.5 | O |
| Digestive system | Intestinal worms | Albizia gummifera (J.F.Gmel.) C.A.Sm., Calpurnia aurea (Aiton) Benth., Celtis africana Burm.f., Croton macrostachyus Hochst. ex Delile, Gymnanthemum amygdalinum (Delile) Sch.Bip | 10 | 5 | 0.56 | G |
| Digestive system | Intestinal worms | Aloe macrocarpa Tod., Croton macrostachyus Hochst. ex Delile, Melia azedarach L., Moringa stenopetala (Baker f.) Cufod., Olea europaea subsp. cuspidata (Wall. & G.Don) Cif., Psidium guajava L., Gymnanthemum amygdalinum (Delile) Sch.Bip | 11 | 7 | 0.4 | O |
| Digestive system | Intestinal worms | Carica papaya L., Phytolacca dodecandra L'Hér | 3 | 2 | 0.5 | S |
| Digestive system | Jaundice | Asparagus africanus Lam., Calpurnia aurea (Aiton) Benth., Celtis africana Burm.f., Coffea arabica L., Justicia schimperiana (Hochst. ex Nees) T.Anderson, Maesa lanceolata Forssk., Moringa stenopetala (Baker f.) Cufod., Afrocarpus falcatus (Thunb.) C.N.Page, Ruta chalepensis L., Solanecio gigas (Vatke) C.Jeffrey | 22 | 10 | 0.57 | G |
| Digestive system | Jaundice | Aloe macrocarpa Tod., Croton macrostachyus Hochst. ex Delile, Justicia schimperiana T.Anderson., Melia azedarach L., Moringa stenopetala (Baker f.) Cufod., Olea europaea subsp. cuspidata (Wall. & G.Don) Cif., Ruta chalepensis L., Schinus molle L., Gymnanthemum amygdalinum (Delile) Sch.Bip | 31 | 9 | 0.73 | O |
| Digestive system | Jaundice | Albizia gummifera (J.F.Gmel.) C.A.Sm., Croton macrostachyus Hochst. ex Delile, Cucumis prophetarum L., Ekebergia capensis Sparrm., Lagenaria siceraria (Molina) Standl., Ricinus communis L., Rotheca myricoides (Hochst.) Steane & Mabb., Stephania abyssinica (Quart.-Dill. & A.Rich.) Walp | 12 | 8 | 0.36 | S |
| Digestive system | Stomachache | Albizia gummifera (J.F.Gmel.) C.A.Sm., Allium sativum L., Brucea antidysenterica J.F.Mill., Celtis africana Burm.f, Croton macrostachyus Hochst. ex Delile, Cymbopogon citratus (DC.) Stapf, Ekebergia capensis Sparrm., Lactuca inermis Forssk., Ocimum gratissimum L., Ruta chalepensis L., Trigonella foenum-graecum L., Gymnanthemum amygdalinum (Delile) Sch.Bip | 31 | 12 | 0.63 | G |
| Digestive system | Stomachache | Aloe macrocarpa Tod., Calpurnia aurea (Aiton) Benth., Citrus limon (L.) Burm.F., Rotheca myricoides (Hochst.) Steane & Mabb, Croton macrostachyus Hochst. ex Delile, Dodonaea viscosa subsp. angustifolia (L.f.) J.G.West, Melia azedarach L., Ocimum gratissimum L., Olinia rochetiana A.Juss., Ruta chalepensis L., Gymnanthemum amygdalinum (Delile) Sch.Bip | 21 | 11 | 0.5 | O |
| Digestive system | Stomachache | Ajuga integrifolia Buch.-Ham. ex D.Don, Albizia gummifera (J.F.Gmel.) C.A.Sm., Balanites aegyptiaca (L.) Delile, Ekebergia capensis Sparrm., Justicia schimperiana (Hochst. ex Nees) T.Anderson, Melia azedarach L., Phytolacca dodecandra L'Hér., Gymnanthemum amygdalinum (Delile) Sch.Bip | 14 | 8 | 0.46 | S |
| Digestive system | Tapeworm | Hagenia abyssinica (Brace) J.F.Gmel | 3 | 1 | 1 | O |
| Digestive system | Vomiting | Cymbopogon citratus (DC.) Stapf, Ruta chalepensis L | 3 | 2 | 0.5 | G |
| Digestive system | Vomiting | Ocimum gratissimum L., Ruta chalepensis L., Gymnanthemum amygdalinum (Delile) Sch.Bip | 4 | 3 | 0.33 | O |
| Digestive system | Weight loss | Lactuca inermis Forssk., Trigonella foenum-graecum L | 6 | 2 | 0.8 | G |
| Digestive system | Weight loss | Ajuga integrifolia Buch.-Ham. ex D.Don, Linum usitatissimum L | 3 | 2 | 0.5 | S |
| Febrile illness | Dizziness | Albizia gummifera (J.F.Gmel.) C.A.Sm., Croton macrostachyus Hochst. ex Delile, | 18 | 2 | 0.94 | G |
| Febrile illness | Dizziness | Croton macrostachyus Hochst. ex Delile | 4 | 1 | 1 | O |
| Febrile illness | Dizziness | Albizia gummifera (J.F.Gmel.) C.A.Sm., Croton macrostachyus Hochst. ex Delile, | 8 | 2 | 0.86 | S |
| Febrile illness | Sudden sickness (Dingetegna) in the local language | Albizia gummifera (J.F.Gmel.) C.A.Sm., Artemisia abyssinica Sch.Bip. ex A.Rich., Calpurnia aurea (Aiton) Benth., Croton macrostachyus Hochst. ex Delile, Ekebergia capensis Sparrm., Ocimum gratissimum L., Ruta chalepensis L | 23 | 7 | 0.73 | G |
| Febrile illness | Sudden sickness (Dingetegna) in the local language | Allium sativum L., Carissa spinarum L., Croton macrostachyus Hochst. ex Delile, Hagenia abyssinica (Brace) J.F.Gmel., Ocimum gratissimum L., Psydrax schimperianus (A.Rich.) Bridson, Ruta chalepensis L., Gymnanthemum amygdalinum (Delile) Sch.Bip., Withania somnifera (L.) Dunal, Zingiber officinale Roscoe | 27 | 10 | 0.65 | O |
| Febrile illness | Sudden sickness (Dingetegna) in the local language | Allium sativum L., Croton macrostachyus Hochst. ex Delile, Echinops kebericho Mesfin, Ocimum jamesii Sebald, Coleus igniarius Schweinf., Ruta chalepensis L | 22 | 6 | 0.76 | S |
| Febrile illness | Fever | Albizia gummifera (J.F.Gmel.) C.A.Sm., Erythrina abyssinica Lam., Ocimum gratissimum L., Solanecio gigas (Vatke) C.Jeffrey | 6 | 4 | 0.4 | G |
| Febrile illness | Fever | Allium sativum L., Aloe macrocarpa Tod., Calpurnia aurea (Aiton) Benth., Citrus limon (L.) Osbeck, Melia azedarach L., Ocimum gratissimum L., Zingiber officinale Roscoe | 11 | 7 | 0.4 | O |
| Febrile illness | Fever | Allium sativum L., Carica papaya L., Ocimum gratissimum L., Ekebergia capensis Sparrm., Eucalyptus globulus Labill., Zingiber officinale Roscoe | 10 | 6 | 0.44 | S |
| Febrile illness | Headache | Artemisia abyssinica Sch.Bip. ex A.Rich., Calpurnia aurea (Aiton) Benth., Celtis africana Burm.f, Ruta chalepensis L | 4 | 4 | 0 | G |
| Febrile illness | Headache | Calpurnia aurea (Aiton) Benth., Carissa spinarum L., Dodonaea viscosa subsp. angustifolia (L.f.) J.G.West, Eucalyptus globulus Labill | 5 | 4 | 0.25 | O |
| Febrile illness | Headache | Allium sativum L., Echinops kebericho Mesfin, Eucalyptus globulus Labill., Zingiber officinale Roscoe | 8 | 4 | 0.57 | S |
| Febrile illness | Malaria | Albizia gummifera (J.F.Gmel.) C.A.Sm., Croton macrostachyus Hochst. ex Delile, Erythrina abyssinica Lam., Justicia schimperiana (Hochst. ex Nees) T.Anderson, Ocimum gratissimum L., Afrocarpus falcatus (Thunb.) C.N.Page, Ruta chalepensis L., Solanecio gigas (Vatke) C.Jeffrey, Gymnanthemum amygdalinum (Delile) Sch.Bip | 18 | 9 | 0.53 | G |
| Febrile illness | Malaria | Aloe macrocarpa Tod., Croton macrostachyus Hochst. ex Delile, Moringa stenopetala (Baker f.) Cufod., Ocimum gratissimum L., Olea europaea subsp. cuspidata (Wall. & G.Don) Cif., Ruta chalepensis L., Gymnanthemum amygdalinum (Delile) Sch.Bip | 21 | 7 | 0.7 | O |
| Febrile illness | Malaria | Ajuga integrifolia Buch.-Ham. ex D.Don, Allium sativum L., Carica papaya L., Melia azedarach L., Gymnanthemum amygdalinum (Delile) Sch.Bip., Zingiber officinale Roscoe | 30 | 6 | 0.83 | S |
| Febrile illness | Pain relief | Aloe macrocarpa Tod., Moringa stenopetala (Baker f.) Cufod., Olea europaea subsp. cuspidata (Wall. & G.Don) Cif., | 3 | 3 | 0 | O |
| Febrile illness | Pain relief | Ajuga integrifolia Buch.-Ham. ex D.Don, Eucalyptus globulus Labill., Melia azedarach L | 3 | 3 | 0 | S |
| Febrile illness | Tonsillitis | Galinsoga quadriradiata Ruiz & Pav., Ricinus communis L | 8 | 2 | 0.86 | G |
| Febrile illness | Tonsillitis | Allium sativum L., Schinus molle L., Zingiber officinale Roscoe | 5 | 3 | 0.5 | O |
| Febrile illness | Tonsillitis | Allium sativum L., Ricinus communis L., Zingiber officinale Roscoe | 16 | 3 | 0.87 | S |
| Febrile illness | Typhoid | Albizia gummifera (J.F.Gmel.) C.A.Sm., Allium sativum L., Croton macrostachyus Hochst. ex Delile, Afrocarpus falcatus (Thunb.) C.N.Page, Ruta chalepensis L., Gymnanthemum amygdalinum (Delile) Sch.Bip | 14 | 6 | 0.62 | G |
| Febrile illness | Typhoid | Allium sativum L., Aloe macrocarpa Tod., Calpurnia aurea (Aiton) Benth., Croton macrostachyus Hochst. ex Delile, Melia azedarach L., Moringa stenopetala (Baker f.) Cufod., Psidium guajava L., Ruta chalepensis L., Zingiber officinale Roscoe | 21 | 9 | 0.6 | O |
| Febrile illness | Typhoid | Allium sativum L., Ekebergia capensis Sparrm., Ruta chalepensis L., Zingiber officinale Roscoe | 21 | 4 | 0.85 | S |
| Genitourinary system | Kidney infection | Cymbopogon citratus (DC.) Stapf, Moringa stenopetala (Baker f.) Cufod., Ocimum gratissimum L | 3 | 3 | 0 | G |
| Genitourinary system | Kidney infection | Coffea arabica L., Moringa stenopetala (Baker f.) Cufod., Olea europaea subsp. cuspidata (Wall. & G.Don) Cif | 4 | 3 | 0.33 | O |
| Gland | Glandular | Albizia gummifera (J.F.Gmel.) C.A.Sm., Calpurnia aurea (Aiton) Benth., Celtis africana Burm.f, Croton macrostachyus Hochst. ex Delile, Justicia schimperiana (Hochst. ex Nees) T.Anderson, Moringa stenopetala (Baker f.) Cufod., Afrocarpus falcatus (Thunb.) C.N.Page, Ruta chalepensis L., Solanecio gigas (Vatke) C.Jeffrey | 16 | 9 | 0.47 | G |
| Gland | Glandular | Justicia schimperiana (Hochst. ex Nees) T.Anderson, Melia azedarach L., Moringa stenopetala (Baker f.) Cufod., Olinia rochetiana A.Juss | 6 | 4 | 0.4 | O |
| Gland | Glandular | Croton macrostachyus Hochst. ex Delile, Cucumis prophetarum L., Lagenaria siceraria (Molina) Standl., Moringa stenopetala (Baker f.) Cufod., Searsia glutinosa (Hochst. ex A.Rich.) Moffett, Rotheca myricoides (Hochst.) Steane & Mabb., Stephania abyssinica (Quart.-Dill. & A.Rich.) Walp | 24 | 7 | 0.74 | S |
| Gland | Goiter | Albizia gummifera (J.F.Gmel.) C.A.Sm., Ekebergia capensis Sparrm., Ruta chalepensis L., Zingiber officinale Roscoe | 6 | 4 | 0.4 | S |
| Lightning | Lightning | Croton macrostachyus Hochst. ex Delile, Ensete ventricosum (Welw.) Cheesman | 6 | 2 | 0.8 | G |
| Mental | Depression | Catha edulis (Vahl) Forssk. ex Endl., Melia azedarach L | 3 | 2 | 0.5 | S |
| Mental | Rabies | Rotheca myricoides (Hochst.) Steane & Mabb, Datura stramonium L. test, Gymnanthemum amygdalinum (Delile) Sch.Bip | 5 | 3 | 0.5 | O |
| Mental | Rabies | Antiaris toxicaria (J.F.Gmel.) Lesch., Justicia schimperiana (Hochst. ex Nees) T.Anderson | 5 | 2 | 0.75 | S |
| Musculoskeletal | Cancer-like ailments | Calpurnia aurea (Aiton) Benth., Croton macrostachyus Hochst. ex Delile | 3 | 2 | 0.5 | G |
| Periodontal | Toothache | Albizia gummifera (J.F.Gmel.) C.A.Sm., Coffea arabica L., Galinsoga quadriradiata Ruiz & Pav., Olea europaea subsp. cuspidata (Wall. & G.Don) Cif., Afrocarpus falcatus (Thunb.) C.N.Page | 7 | 5 | 0.33 | G |
| Periodontal | Toothache | Calpurnia aurea (Aiton) Benth., Datura stramonium L. test, Melia azedarach L., Olea europaea subsp. cuspidata (Wall. & G.Don) Cif., Olinia rochetiana A.Juss | 7 | 5 | 0.33 | O |
| Reproductive | Abortion | Cymbopogon citratus (DC.) Stapf | 3 | 1 | 1 | G |
| Reproductive | Abortion | Phytolacca dodecandra L'Hér | 4 | 1 | 1 | S |
| Reproductive | Gonorrhea | Albizia gummifera (J.F.Gmel.) C.A.Sm., Croton macrostachyus Hochst. ex Delile, Cymbopogon citratus (DC.) Stapf, Maesa lanceolata Forssk., Afrocarpus falcatus (Thunb.) C.N.Page, Ruta chalepensis L | 24 | 6 | 0.78 | G |
| Reproductive | Gonorrhea | Aloe macrocarpa Tod., Croton macrostachyus Hochst. ex Delile, Hagenia abyssinica (Bruce) J.F.Gmel., Ruta chalepensis L., Gymnanthemum amygdalinum (Delile) Sch.Bip | 11 | 5 | 0.6 | O |
| Reproductive | Gonorrhea | Allium sativum L., Brucea antidysenterica J.F.Mill., Catha edulis (Vahl) Forssk. ex Endl., Croton macrostachyus Hochst. ex Delile, Ekebergia capensis Sparrm., Justicia schimperiana T.Anderson, Phytolacca dodecandra L'Hér., Afrocarpus falcatus (Thunb.) C.N.Page, Ruta chalepensis L | 27 | 9 | 0.69 | S |
| Reproductive | Menstruation cycle disorder | Albizia gummifera (J.F.Gmel.) C.A.Sm., Croton macrostachyus Hochst. ex Delile, Ruta chalepensis L., Trigonella foenum-graecum L | 5 | 4 | 0.25 | G |
| Respiratory | Asthma | Allium sativum L., Celtis africana Burm.f, Ruta chalepensis L | 3 | 3 | 0 | G |
| Respiratory | Asthma | Croton macrostachyus Hochst. ex Delile, Eucalyptus globulus Labill., Olea europaea subsp. cuspidata (Wall. & G.Don) Cif., Withania somnifera (L.) Dunal | 11 | 4 | 0.7 | O |
| Respiratory | Asthma | Eucalyptus globulus Labill., Withania somnifera (L.) Dunal, Zingiber officinale Roscoe | 8 | 3 | 0.71 | S |
| Respiratory | Common cold | Allium sativum L | 3 | 1 | 1 | G |
| Respiratory | Common cold | Allium sativum L., Citrus limon (L.) Osbeck, Eucalyptus globulus Labill., Zingiber officinale Roscoe | 14 | 4 | 0.77 | O |
| Respiratory | Common cold | Allium sativum L., Echinops kebericho Mesfin, Eucalyptus globulus Labill., Zingiber officinale Roscoe | 27 | 4 | 0.88 | S |
| Respiratory | Cough | Albizia gummifera (J.F.Gmel.) C.A.Sm., Erythrina abyssinica Lam., Maesa lanceolata Forssk., Trigonella foenum-graecum L | 7 | 4 | 0.5 | G |
| Respiratory | Lung infection | Albizia gummifera (J.F.Gmel.) C.A.Sm., Asparagus africanus Lam., Celtis africana Burm.f, Erythrina abyssinica Lam., Solanecio gigas (Vatke) C.Jeffrey, Trigonella foenum-graecum L | 6 | 6 | 0 | G |
| Respiratory | Lung infection | Aloe macrocarpa Tod., Croton macrostachyus Hochst. ex Delile, Dodonaea viscosa subsp. angustifolia (L.f.) J.G.West, Moringa stenopetala (Baker f.) Cufod., Ricinus communis L., Gymnanthemum amygdalinum (Delile) Sch.Bip | 6 | 6 | 0 | O |
| Respiratory | Lung infection | Albizia gummifera (J.F.Gmel.) C.A.Sm., Croton macrostachyus Hochst. ex Delile, Cucumis prophetarum L., Lagenaria siceraria (Molina) Standl., Searsia glutinosa (Hochst. ex A.Rich.) Moffett, Ricinus communis L., Rotheca myricoides (Hochst.) Steane & Mabb | 17 | 7 | 0.62 | S |
| Respiratory | Nasal bleeding | Ruta chalepensis L., Solanecio gigas (Vatke) C.Jeffrey | 3 | 2 | 0.5 | G |
| Respiratory | Nasal bleeding | Eucalyptus globulus Labill., Ruta chalepensis L., Schinus molle L., Solanum incanum L | 7 | 4 | 0.5 | O |
| Respiratory | Sneezing | Coffea arabica L., | 3 | 1 | 1 | O |
| Respiratory | Tuberculosis | Albizia gummifera (J.F.Gmel.) C.A.Sm., Erythrina abyssinica Lam., Trigonella foenum-graecum L | 3 | 3 | 0 | G |
| Respiratory | Tuberculosis | Olea europaea subsp. cuspidata (Wall. & G.Don) Cif., Olinia rochetiana A.Juss., Ruta chalepensis L | 3 | 3 | 0 | O |
| Respiratory | Tuberculosis | Ekebergia capensis Sparrm., Ruta chalepensis L | 4 | 2 | 0.67 | S |
| Bad/evil spirit | Bad/evil spirit | Albizia gummifera (J.F.Gmel.) C.A.Sm., Artemisia abyssinica Sch. Bip. ex A. Rich., Calpurnia aurea (Aiton) Benth., Croton macrostachyus Hochst. ex Delile, Withania somnifera (L.) Dunal | 11 | 5 | 0.6 | G |
| Bad/evil spirit | Bad/evil spirit | Vachellia oerfota (Forssk.) Kyal. & Boatwr., Carissa spinarum L., Rotheca myricoides (Hochst.) Steane & Mabb, Olea europaea subsp. cuspidata (Wall. & G.Don) Cif., Withania somnifera (L.) Dunal | 17 | 5 | 0.75 | O |
| Bad/evil spirit | Bad/evil spirit | Catha edulis (Vahl) Forssk. ex Endl., Clutia abyssinica Jaub. & Spach, Croton macrostachyus Hochst. ex Delile, Eucalyptus globulus Labill., Coleus igniarius Schweinf., Searsia glutinosa (Hochst. ex A.Rich.) Moffett, Ruta chalepensis L., Urtica simensis Hochst. ex A.Rich., Withania somnifera (L.) Dunal | 23 | 9 | 0.64 | S |
Fidelity level (FLs), relative popularity level (RPL), and rank-order priority (ROP)
The relative healing potential of medicinal plants is calculated for plants at least cited by three or more informants against particular ailments, and the FLs, RPL, and ROP values ranged from 50 to 100%, 0.5 to 1, and 24 to 100%, respectively (Table 7). Twenty-six plant species were identified as the most preferred plants (ROP > 50%) across ethnic groups (Table 7). Lactuca inermis Forssk., Moringa stenopetala (Baker f.) Cufod., and Withania somnifera (L.) scored the highest FLs and ROP values in the Gedeo ethnic group, whereas Allium sativum L., Citrus limon (L.) Osbeck, Ricinus communis L., and Schinus molle L., in the Oromo ethnic group, and Antiaris toxicaria (J.F.Gmel.) Lesch., Brucea antidysenterica J.F.Mill., Echinops kebericho Mesfin, Ocimum jamesii Sebald, Afrocarpus falcatus (Thunb.) C.N.Page, Searsia natalensis (Bernh. ex Krauss) F.A.Barkley, and Ricinus communis L. in the Sidama ethnic group (Table 7).
Table 7.
The most curative medicinal plant species with their FL, RPL, and ROP values among ethnic groups
| Ethnic groups | Species name | Ailment treated | FL (%) | RPL | ROP |
|---|---|---|---|---|---|
| Gedeo | Achyranthes aspera L | Jaundice | 50 | 0.5 | 25 |
| Allium sativum L | Stomachache | 50 | 0.5 | 25 | |
| Allium sativum L | Common cold | 75 | 0.75 | 56 | |
| Artemisia abyssinica Sch.Bip. ex A.Rich | Bad/evil spirit | 66.67 | 0.67 | 45 | |
| Brucea antidysenterica J.F.Mill | Diarrhea | 75 | 0.75 | 56 | |
| Celtis africana Burm.f | Stomachache | 50 | 0.5 | 25 | |
| Commelina benghalensis L | Skin infection | 66.67 | 0.67 | 45 | |
| Clutia abyssinica Jaub. & Spach | Deep sores /cancer-like ailments | 50 | 0.5 | 25 | |
| Cymbopogon citratus (DC.) Stapf | Blood pressure | 80 | 0.8 | 64 | |
| Cymbopogon citratus (DC.) Stapf | Abortion | 60 | 0.6 | 36 | |
| Datura stramonium L. test | Rabies | 66.67 | 0.67 | 45 | |
| Drynaria volkensii Heiron | Swellings | 50 | 0.5 | 25 | |
| Drynaria volkensii Heiron | Ear infection | 50 | 0.5 | 25 | |
| Ekebergia capensis Sparrm | Diarrhea | 66.67 | 0.67 | 45 | |
| Ekebergia capensis Sparrm | Stomachache | 66.67 | 0.67 | 45 | |
| Ensete ventricosum (Welw.) Cheesman | Lightning | 66.67 | 0.67 | 45 | |
| Erythrina abyssinica Lam | Cough | 0.5 | 25 | ||
| Galinsoga quadriradiata Ruiz & Pav | Tonsillitis | 85.71 | 0.86 | 74 | |
| Grewia ferruginea Hochst. ex A.Rich | Headache | 66.67 | 0.67 | 45 | |
| Hyparrhenia rufa (Nees) Stapf | Swellings | 66.67 | 0.67 | 45 | |
| Justicia schimperiana (Hochst. ex Nees) T.Anderson | Jaundice | 50 | 0.5 | 25 | |
| Lactuca inermis Forssk | Anemia | 100 | 1 | 100 | |
| Lactuca inermis Forssk | Stomachache | 50 | 0.5 | 25 | |
| Lagenaria siceraria (Molina) Standl | Amoeba | 66.67 | 0.67 | 45 | |
| Moringa stenopetala (Baker f.) Cufod | Blood pressure | 100 | 1 | 100 | |
| Moringa stenopetala (Baker f.) Cufod | Glandular | 50 | 0.5 | 25 | |
| Ocimum gratissimum L | Febrile illness | 71.43 | 0.71 | 51 | |
| Coleus igniarius Schweinf | Stomachache | 66.67 | 0.67 | 45 | |
| Ricinus communis L | Swellings | 80 | 0.8 | 64 | |
| Syzygium guineense (Willd.) DC | Pain relief | 66.67 | 0.67 | 45 | |
| Solanecio gigas (Vatke) C.Jeffrey | Jaundice | 53.85 | 0.54 | 29 | |
| Gymnanthemum auriculiferum (Hiern) Isawumi | Snake venom | 66.67 | 0.67 | 45 | |
| Withania somnifera (L.) Dunal | Bad/evil spirit | 100 | 1 | 100 | |
| Zingiber officinale Roscoe | Tonsillitis | 66.67 | 0.67 | 45 | |
| Oromo | Vachellia oerfota (Forssk.) Kyal. & Boatwr | Bad/evil spirit | 87.50 | 0.88 | 77 |
| Allium sativum L | Common cold | 100 | 1 | 100 | |
| Allium sativum L | Typhoid | 60 | 0.4 | 24 | |
| Allium sativum L | Tonsillitis | 60 | 0.4 | 24 | |
| Aloe macrocarpa Tod | Malaria | 62.5 | 0.62 | 39 | |
| Aloe macrocarpa Tod | Typhoid | 50 | 0.5 | 25 | |
| Albizia gummifera (J.F.Gmel.) C.A.Sm | Dizziness | 50 | 0.5 | 25 | |
| Brassica carinata A.Braun | Fever | 66.67 | 0.67 | 45 | |
| Carissa spinarum L | Bad/evil spirit | 66.67 | 0.67 | 45 | |
| Citrus limon (L.) Osbeck | Blood pressure | 100 | 1 | 100 | |
| Rotheca myricoides (Hochst.) Steane & Mabb | Stomachache | 75 | 0.5 | 38 | |
| Coffea arabica L | Sneezing | 60 | 0.6 | 36 | |
| Ekebergia capensis Sparrm | Skin infection | 50 | 0.5 | 25 | |
| Erica arborea L | Wound | 66.67 | 0.67 | 45 | |
| Eucalyptus globulus Labill | Asthma | 77.78 | 0.78 | 61 | |
| Eucalyptus globulus Labill | Common cold | 53.85 | 0.54 | 29 | |
| Ficus sycomorus L | Tonsillitis | 66.67 | 0.67 | 45 | |
| Hagenia abyssinica (Bruce) J.F.Gmel | Tapeworm | 60 | 0.6 | 36 | |
| Justicia schimperiana (Hochst. ex Nees) T.Anderson | Jaundice | 77.78 | 0.78 | 61 | |
| Phytolacca dodecandra L'Hér | Abortion | 66.67 | 0.67 | 45 | |
| Ocimum lamiifolium Hochst. ex Benth | Febrile illness | 66.67 | 0.67 | 45 | |
| Ocimum gratissimum L | Febrile illness | 87.5 | 0.75 | 66 | |
| Searsia natalensis (Bernh. ex Krauss) F.A.Barkley | Autism | 50 | 05 | 25 | |
| Ricinus communis L | Swellings | 100 | 1 | 100 | |
| Solanum incanum L | Nasal bleeding | 80 | 0.8 | 64 | |
| Schinus molle L | Jaundice | 100 | 1 | 100 | |
| Stephania abyssinica (Quart.-Dill. & A.Rich.) Walp | Gonorrhea | 50 | 0.5 | 25 | |
| Withania somnifera (L.) Dunal | Bad/evil spirit | 66.67 | 0.6 | 36 | |
| Ziziphus spina-christi (L.) Willd | Gonorrhea | 50 | 0.5 | 25 | |
| Ziziphus spina-christi (L.) Willd | Bad/evil spirit | 50 | 0.5 | 25 | |
| Sidama | Achyranthes aspera L | Headache | 50 | 0.5 | 25 |
| Albizia gummifera (J.F.Gmel.) C.A.Sm | Dizziness | 57.14 | 0.57 | 33 | |
| Allium sativum L | Fever | 50 | 0.38 | 19 | |
| Allium sativum L | Typhoid | 87.5 | 0.75 | 66 | |
| Antiaris toxicaria (J.F.Gmel.) Lesch | Rabies | 100 | 1 | 100 | |
| Balanites aegyptiaca (L.) Delile | Amoeba | 75 | 0.75 | 56 | |
| Balanites aegyptiaca (L.) Delile | Diarrhea | 75 | 0.75 | 56 | |
| Brucea antidysenterica J.F.Mill | Gonorrhea | 100 | 1 | 100 | |
| Carica papaya L | Malaria | 100 | 0.86 | 86 | |
| Carissa spinarum L | Diarrhea | 66.67 | 0.67 | 45 | |
| Catha edulis (Vahl) Forssk. ex Endl | Gonorrhea | 71.43 | 0.71 | 51 | |
| Cinnamomum verum J.Presl | Asthma | 66.67 | 0.67 | 45 | |
| Cinnamomum verum J.Presl | Common cold | 66.67 | 0.67 | 45 | |
| Clutia abyssinica Jaub. & Spach | Diarrhea | 50 | 0.5 | 25 | |
| Echinops kebericho Mesfin | Common cold | 100 | 1 | 100 | |
| Echinops kebericho Mesfin | Febrile illness | 100 | 1 | 100 | |
| Echinops kebericho Mesfin | Headache | 75 | 0.75 | 56 | |
| Ekebergia capensis Sparrm | Amoeba | 60 | 0.6 | 36 | |
| Eucalyptus globulus Labill | Common cold | 60 | 0.54 | 29 | |
| Lagenaria siceraria (Molina) Standl | Jaundice | 60 | 0.6 | 36 | |
| Melia azedarach L | Malaria | 75 | 0.62 | 47 | |
| Moringa stenopetala (Baker f.) Cufod | Glandular | 66.67 | 0.67 | 45 | |
| Ocimum jamesii Sebald | Febrile illness | 100 | 1 | 100 | |
| Afrocarpus falcatus (Thunb.) C.N.Page | Gonorrhea | 100 | 1 | 100 | |
| Searsia natalensis (Bernh. ex Krauss) F.A.Barkley | Glandular | 83.33 | 0.83 | 69 | |
| Ricinus communis L | Swellings | 100 | 1 | 100 | |
| Ricinus communis L | Tonsillitis | 66.67 | 0.33 | 22 | |
| Ruta chalepensis L | Typhoid | 57.14 | 0.57 | 33 | |
| Searsia natalensis (Bernh. ex Krauss) F.A.Barkley | Snake venom | 100 | 1 | 100 | |
| Stephania abyssinica (Quart.-Dill. & A.Rich.) Walp | Jaundice | 50 | 0.5 | 25 | |
| Stephania abyssinica (Quart.-Dill. & A.Rich.) Walp | Glandular | 50 | 0.5 | 25 | |
| Syzygium guineense (Willd.) DC | Amoeba | 50 | 0.5 | 25 | |
| Syzygium guineense (Willd.) DC | Bad/evil spirit | 50 | 0.5 | 25 | |
| Taverniera abyssinica A.Rich | Febrile illness | 66.67 | 0.67 | 45 | |
| Urtica simensis Hochst. ex A.Rich | Bad/evil spirit | 83.33 | 0.83 | 69 | |
| Gymnanthemum amygdalinum (Delile) Sch.Bip | Amoeba | 61.54 | 0.62 | 38 | |
| Gymnanthemum amygdalinum (Delile) Sch.Bip | Malaria | 53.85 | 0.54 | 29 | |
| Withania somnifera (L.) Dunal | Bad/evil spirit | 75 | 0.75 | 56 | |
| Zingiber officinale Roscoe | Tonsillitis | 100 | 0.83 | 83 | |
| Zingiber officinale Roscoe | Malaria | 50 | 0.5 | 25 | |
| Zingiber officinale Roscoe | Wound | 50 | 0.5 | 25 |
Discussion
The medicinal plant resources and their associated indigenous and local ethnobotanical knowledge documented revealed time-honored ethnobotanical knowledge practices of the three ethnic groups studied (Table 3). The plant families Fabaceae, Asteraceae, Lamiaceae, and Poaceae were the most abundant, followed by Solanaceae, Rutaceae, and Euphorbiaceae. The hypothesis by [39–42] that the dominance of these families in disease treatment may be due to their aromatic properties and abundance of essential oil is supported by our record of a higher number of relevant plant species from Fabaceae, Asteraceae, and Lamiaceae (Table 3). Of the total 189 medicinal plants collected, several studies conducted in Ethiopia and abroad reported diverse amounts of therapeutic plants, which witnessed about the relevance of several traditional medicinal plants documented in this study. For instance, Regassa et al. [28], Woldeamanuel et al. [56], Eshete and Molla [10], Mekuria and Abduro [57], Marshet and Dalle [58], Kidane et al. [13], Tefera and Kim [8], and Teka et al. [5] compiled 39, 39, 41, 67, 59, 71, 64, and 88 medicinal plant species, respectively, in their ethnobotanical investigations in different parts of Ethiopia. Tugume et al. [59], Hussain et al. [60], Faruque et al. [61], Lautenschläger et al. [62], Wiryono et al. [63] and Al-Robai et al. [64] documented 33, 12, 13, 22, 13, and 20 therapeutic plants, respectively, in Uganda, Pakistani-Afghan borders, Bangladesh, Angola, Indonesia, and Saudi Arabia.
In this study, Croton macrostachyus Hochst. ex Delile is reported as curing plants against deep sores and cancer-like ailments, eye infections, abrupt lightning, tetanus, lung infection, gonorrhea, dizziness, febrile illness, wounds, bad/evil spirit, diarrhea, jaundice, amoeba, glandular, giardia, abortion, intestinal worms, malaria, asthma, typhoid, skin infection, placental delay during birth, circumcision wound, stomachache, ear infection, allergy, and menstruation cycle disorder. Similarly, [5, 52] reported the efficacy of the species against wounds, blood clotting, tinea versicolor, common wart, nasal congestion, indigestion, abdominal pain, bloating, intestinal parasite, retained placenta, general malaise (Michi), headache, jaundice, malaria, rabies, swelling, allergies, eye infection, and pyoderma in their ethnobotanical investigations in the south-central and southwestern parts of the country. In another study, in the southern parts of Ethiopia [8, 10], the medicinal values of this species were revealed against toothache, swelling and forming deep openings, cold disease, gonorrhea, amoeboid, wounds, kidney infection, ringworm, stomachache, hepatitis, shivering, abnormal breathing, tuberculosis, gastritis, and goiter, and against jaundice in the northern parts of Ethiopia [13]. Besides, [65] reported the efficacy of this species against typhoid, measles, and skin diseases in Kenya, [59] against headache in Uganda, and [66] against abdominal pain in Tanzania.
This study revealed ethnomedicinal values of Zingiber officinale Roscoe against asthma, blood pressure, passive sexual interest, common cold, tonsillitis, typhoid, headache, malaria, wounds, fever, cough, tung infection, goiter, constipation, febrile illness, amoeba, gastric diseases, and stomachache. Correspondingly, it was also reported against tonsillitis, abdominal pain, toothache, common cold, and coughing in other studies in the south-central and southwestern parts of Ethiopia [5, 52]. In addition, against eye disease in Hawassa zuria districts [8]. Abroad [67] reported the significance of Zingiber officinale Roscoe against abdominal problems, laxative dyspepsia, dysentery and vomiting, coughs, bronchitis, asthma, and tuberculosis in Bangladesh; [68] reported against respiratory, digestive, and sexual disorders in India, and [64] reported against GIT disorders, respiratory disorders, CNS disorders, hematological disorders, endocrine disorders, rheumatic disorders, orthopedic disorders, immunological disorders, and antibacterial activities in Saudi Arabia. Albizia gummifera (J.F.Gmel.) C.A.Sm. is reported against deep sores and cancer-like ailments, goiter, toothache, dizziness, stomachache, jaundice, lung infection, amoeba, malaria, fire accident, skin infection, epilepsy, febrile illness, glandular, gonorrhea, swellings, fever, bad/evil spirit, cough, tuberculosis, menstruation cycle disorder, typhoid, and intestinal worms in this study. Correspondingly, [8] witnessed the significance of this species against swelling of the stomach and evil eye in Hawassa districts, southern Ethiopia, and [13] against febrile illness in northern Ethiopia. Other use reports indicated the novelty of this species against different ailments in the study areas.
Aloe macrocarpa Tod. is a novel for use against malaria, jaundice, typhoid, fever, deep sores and cancer-like ailment, lung infection, gonorrhea, pain relief, urinary organ infection, intestinal worms, wounds, stomachache, and diarrhea, because this is a new report and has not been reported before. However, [13] reported Aloe megalacantha Baker and Aloe camperi Schweinf. against dislocated bone, malaria, hemorrhoid, and eye disease; [14] reported Aloe weloensis Sebsebe against wounds, and malaria in northern Ethiopia, respectively; [28] reported Aloe gilbertii T. Reynolds ex Sebsebe and Brandham against malaria, intestinal parasites, tonsillitis, wounds, stomach pain, sudden disease, constipation, and eye problems in southern Ethiopia; and [21] reported Aloe otallensis Baker against blood clothing, wounds, and tuberculosis in southwestern Ethiopia. Calpurnia aurea (Aiton) Benth. is reported against lung infection, typhoid, intestinal worms, jaundice, bad/evil spirit, amoeba, headache, stomachache, toothache, fever, skin infection, wound, circumcision wound, febrile illness, deep sores and cancer-like ailment, swellings, glandular, and respiratory organ infection in our investigation. In addition, Eshete and Molla [10] reported this medicinal plant species against hepatitis, ear ache, and hypertension in the southern parts of the country. Likewise, [5] reported against toothache in south-central and in addition, [13] reported against eye diseases in the northern parts of the country. Gymnanthemum amygdalinum (Delile) Sch.Bip. is reported against amoeba, malaria, skin infection, stomachache, diarrhea, head skin infection, gonorrhea, rabies, febrile illness, intestinal worms, gastric diseases, lung infection, blood pressure, jaundice, vomiting, and typhoid. Correspondingly, [5, 10, 13, 52] confirmed the efficacy of this species used against intestinal parasites, abdominal pain, malaria, gastritis, fibril illness, and diarrhea in their ethnobotanical investigations in different parts of the country. Likewise, [59] confirmed its great medicinal role against malaria, convulsions, and stomachache in Uganda.
Besides, several ethno-veterinary studies conducted elsewhere in the country identified numerous therapeutic plants against different livestock ailments, demonstrating the significance of the traditional medicinal plants recorded in this study. Asfaw et al. [69], Alemneh [70], Tekle [71], Lulekal et al. [72], Eshetu et al. [73], and Yigezu et al. [74] compiled 25, 16, 20, 24, 20, and 27 medicinal plant species, respectively, in their ethno-veterinary investigations in different parts of the country. For instance, Asfaw et al. [69], Alemneh [70], Tekle [71], Lulekal et al. [72], Eshetu et al. [73], and Yigezu et al. [74] mentioned the effectiveness of Croton macrostachyus Hochst. ex Delile against foot rot, gastrointestinal disorders, abdominal pains, dysentery, wounds, scabies, dermatophilosis, blackleg, and trypanosomiasis. The authors also reported the medicinal use of Gymnanthemum amygdalinum (Delile) Sch.Bip. against jaundice, gastrointestinal disorders, abdominal pain, retained placenta, diarrhea, skin infection, and blackleg in their studied. Asfaw et al. [69], Alemneh [70], and Yigezu et al. [74] explained the therapeutic potentials of Justicia schimperiana (Hochst. ex Nees) T.Anderson against jaundice, swellings, gastrointestinal diseases, diarrhea, and blackleg. Asfaw et al. [69], Lulekal et al. [72], Eshetu et al. [73], and Yigezu et al. [74] described the relevance of Allium sativum L. against blackleg, mastitis, diarrhea, and internal body parasites.
In general, comparison of our findings with other researchers' work conducted elsewhere in the country and abroad revealed that the documented medicinal plants have wide and novel uses in the study areas and demonstrated that people from different areas employ the same medicinal plants to treat the same or different types of human ailments. This revealed that the reported medicinal plants have therapeutic and pioneering uses in the research areas and beyond. This makes it easier for further efficacy evaluation and drug synthesis from the documented plants. Their pharmacological activity should be further confirmed for use at the local and worldwide levels. Most (71%) of the identified medicinal plants were harvested from the wild (Table 3). Conservation efforts specifically targeted at medicinal plants are still a challenge in the study areas and elsewhere in the country [8, 9, 25, 47]. The well-known natural forest of the Wondo Genet areas, Munessa-Shashemene natural and plantation forest, Adaba-Dodola forest, Bale Mountains National Park, wide agro-forestry practices, and local markets are potential sources for medicinal plants. We have also seen local farmers practicing their indigenous knowledge to protect some important medicinal plants in their home gardens (Table 3). Moreover, healers discussed the challenges of cultivating plant species outside their natural habitats, as well as the need to travel considerable distances for several hours to get the necessary therapeutic plants outside their villages.
The association between ethnobotanical knowledge and socio-demographic variables
The indigenous and local knowledge of medicinal plant uses of the three ethnic groups was not evenly distributed among respondents’ age groups (Table 4 and Fig. 2A). The indigenous and local knowledge of medicinal plant use is still higher among the older (age groups > 44) than among the younger (< 45 years old) across ethnic groups. Likewise, Lulekal et al. [9], Geta et al. [76], Eshete and Molla [10], Bekele et al. [22], Demie et al. [4], and Kidane et al. [13] reported similar findings in different parts of the country that older informants have better ethnobotanical knowledge as compared to younger. Besides, similar patterns of knowledge distribution were also witnessed abroad. Beltrán-Rodríguez et al. [77], Sharma et al. [78], Wiryono et al. [63], Amjad et al. [79], Pathy et al. [80], and Khakurel et al. [81] in Mexico, Himalaya (South Asia), Indonesia, Pakistan, DR Congo, and Nepal, respectively. Silva et al. [82] and Chekole et al. [75] also explained that older people have more opportunities for cultural interaction and familiarity with plants and their therapeutic benefits than younger. This helped them be more experienced and knowledgeable than the younger informants. The regression analysis also confirmed that the respondent's age was positively correlated with his or her ability to recognize and use ethnomedicinal plants across ethnic groups (Figs. 3, 4, 5); however, it showed a slight curvilinear relationship at the end in this study. This does not mean that the knowledge of elderly people has declined, but their openness and willingness to disclose their knowledge to outsiders are very weak, and they were too secretive and conservative in our study areas. During our discussion with them, they informed us that if all knowledge of medicinal plants is freely shared, their effectiveness in curing the illness becomes weak, particularly for those in the age group above 64. They showed disinclination to participate in the study and were reluctant to disclose their knowledge. Thus, comparatively, the individuals (age ranges between 45 and 64) mentioned a greater number of ethnomedicinal plant species than elders (Table 4). As a result, informants' disparities in ethnobotanical knowledge sharing, particularly between age groups 55–64 (older) and above 64 (elder), may have had an unintended impact on the outcome of the study.
Fig. 4.
Correlation between male respondent’s knowledge of medicinal plant citation and age
Fig. 5.
Correlation between female respondent’s knowledge of medicinal plant citation and age
Different ethnobotanical studies conducted elsewhere in the country also reported similar challenges. For instance, Mesfin et al. [20], in their ethnobotanical investigation in Amaro Woreda, southern Ethiopia, mentioned that the majority of participants were hesitant to disclose their knowledge of the medicinal value of the plants. They fear that their societal recognition and reputation, which they have earned due to their knowledge, will be lost, and hence they want to keep them secret. The traditional knowledge acquired from their ancestors is freely transferred within the family, preferably to the eldest son. Transfer of this knowledge to the outside world was deemed acceptable only based on substantial payment. In other studies in southern and central parts of the country, Eshete and Molla [10] and Woldeamanuel et al. [56] mentioned that most traditional healers consider traditional knowledge to be ancestral and divine, and thus, they are reluctant to disclose it to the outside world and keep it extremely secret because they think that the medicine would become ineffective if it were disseminated to others. Agize et al. [21], in their ethnobotanical investigation in southwestern Ethiopia, explained that aged informants were reluctant to disclose their ethnobotanical knowledge early as compared to other age groups, and kept it up to their last life span. Overall, this study revealed a decline in indigenous and local ethnobotanical knowledge among the younger generation across the studied ethnic groups and called for an effort to repair the observed generation gap via ongoing professional support and training of local communities to maintain traditional knowledge and practices through systematic recording. Lack of interest in traditional knowledge among young generations coupled with poor knowledge-sharing mechanisms (by word of mouth, secrecy, and only among family members) and weak policy support from concerned bodies are reported challenges for the rapid loss of indigenous and local ethnobotanical knowledge and a threat to the future potential of the country [9, 10, 59, 66, 67]. Besides, informants claimed that in recent decades, young healers had traveled to urban areas in other conditions in pursuit of work because of a lack of support from the government and a low income from traditional medication. This is important since such activities hurt the sustainability of local ethnomedicinal knowledge across generations.
Gender is another test to determine the distribution of ethnobotanical knowledge across ethnic groups. However, the difference was not statistically significant (Table 4 and Fig. 2B). Similar results were reported by [9, 10, 12–14, 66] elsewhere in the country and abroad in Nepal and Tunisia, where gender did not influence ethnomedicine claims. Thus, it was indicated that both men and women are knowledgeable about the use of traditional plant remedies, despite the relative dominance of medicinal plant traditions by men in the country, which could relate to the flow of information along the male line in the country [9, 14, 67]. Earlier studies conducted elsewhere in Ethiopia and Ecuador found that traditional medicine practitioners had nearly comparable ethnobotanical knowledge practices between the gender groups [9, 45]. In contrast, [4, 8, 59, 65, 69] elsewhere in the country and abroad in Mexico reported that significant differences were found in ethnobotanical knowledge between male and female practitioners.
Even though illiterate and lower-grade informants of the studied peri-urban districts reported more medicinal plants than higher-grade informants (Table 4 and Fig. 2C), the difference was not statistically significant. This finding revealed that all interviewed informants were knowledgeable about using traditional plant remedies regardless of their education levels, showing that education is not a factor in influencing their local knowledge of plant utilization. A similar result was reported by [12, 59] in Mexico and Nepal. In contrast, [8–10, 13, 66, 69, 70] mentioned education has effect on the health-seeking behavior of the local communities in different parts of the country and abroad in Tunisia. Our findings also showed that religion has no effect on the health-seeking behavior of the local communities; despite the fact that the majority of the people in the research areas are Protestants and Muslim religion followers, they still preferred traditional plant medicines (Table 4 and Fig. 2D). This implies that most spiritual beliefs encourage the use of therapeutic plants in the study areas. Thus, in this community, we realized that religion is not a limiting factor that affects the distribution of the local ethnobotanical knowledge system. Correspondingly, other studies conducted in the southeastern parts of Ethiopia [4, 71] also indicated that informants believed religion encouraged the use of traditional plant medicine. Contrary to this, a study by [85] revealed that religion is a limiting factor influencing the distribution of medicinal plant knowledge in India.
Useful plants and their use values
The widespread use of plants for health treatment demonstrates an essential element of the culture [15] and is used to determine the relative significance of medicinal plants in the local communities [49]. Accordingly, Croton macrostachyus Hochst. ex Delile, Zingiber officinale Roscoe, Albizia gummifera C.A.Sm., and Aloe macrocarpa Tod. had scored the highest use value across the studied ethnic groups as a curative plant against different human ailments (Table 5). Aspects of these findings are consistent with those of other researchers [8, 10, 14, 51, 54, 55, 72, 73] who conducted ethnobotanical surveys in different parts of Ethiopia, South Africa, Bangladesh, India, and Saudi Arabia. They revealed that Croton macrostachyus Hochst.ex Delile and Zingiber officinale Roscoe had high use values against different ailments, and the in vitro investigations of [86–89] validated their efficacy on antimicrobial activities. Albizia gummifera C.A.Sm. has a significant use value against different human ailments in the studied communities, and the in vitro investigations of [90] confirmed the efficacy of this medicinal plant species antimicrobial activities in Cameroon. Aloe macrocarpa Tod. has a significant use value against different human ailments, and the in vitro investigations of [91] validated the efficacy of this medicinal plant species antimicrobial activities. Gymnanthemum amygdalinum (Delile) Sch.Bip., Calpurnia aurea (Aiton) Benth, and Allium sativum L. were also curative plants by all studied ethnic groups with varied use values (Table 5), and the in vitro investigations of [92–95] validated their antimicrobial activities, respectively.
In general, among the evaluated 78 important medicinal plant species, several studies conducted in Ethiopia and abroad reported different amounts of therapeutic plant use value against human ailments, which confirmed the efficacy of several traditional medicinal plants documented in this study. For instance, Chekole [14] mentioned the significant use values of 31 medicinal plant species in Gubalafto district in the northern parts of Ethiopia. Eucalyptus globulus Labill., Croton macrostachyus Hochst. ex Delile, Achyranthes aspera L., Allium sativum L., and Solanum incanum L. were reported medicinal plants with different use values. In another study, Agize et al. [21] reported the significant use values of Phytolacca dodecandra L'Hér., Gymnanthemum amygdalinum (Delile) Sch.Bip., Maesa lanceolata Forssk., and Eucalyptus globulus Labill. in the studied communities. Abroad, Shaheen et al. [96], Ishtiaq et al. [97], Faruque et al. [61], Gupta et al. [68], and Al-robai et al. [64] revealed 9, 7, 8, 6, and 14 significant medicinal plants in Pakistan, Bangladesh, India, and Saudi Arabia. Besides, it was also confirmed by Eshete and Molla [10] that repeatedly used plants are more likely to be biologically active and indicate the popularity of the local medicinal flora in the local culture. Therefore, these species should be prioritized for conservation. Their preferred uses may place their populations under threat due to overharvesting.
The general understanding among informants
Consensus analysis is a critical tool for establishing a comparative evaluation of the level of informant's agreement on the use of medicinal plants [50]. Beyond that, it would provide dependability for every claim supported by reliable facts in ethnobotanical investigations [98]. As a result, the majority of the clusters generated in this study confirmed the unique and shared knowledge of each ethnic group on similar or different plant species against a variety of ailments and the diffusion of information and cultural linkage (Table 6). Most of the clusters had an informant consensus value greater than 50, indicating that they might all be evaluated for validation in support of their traditional use. These demonstrate a high level of agreement among the informants regarding the use of specific plants to treat the similar disorder. Particularly, the four use categories (Circulatory system disorders, febrile illness, reproductive organ disorders, and Bad/evil spirit) scored high ICF values across the studied ethnic groups. Different studies conducted elsewhere in the country also reported high ICF value for the same illness categories [8, 10, 13, 14, 52]. Lulekal et al. [9] explained that the high informant consensus values obtained indicate reasonably high reliability of informants on the use of traditional medicinal plants, which are thought to have better potency and contain more biologically active ingredients in disease treatment.
In this study, six medicinal plant species gained common consensus among the studied ethnic groups against febrile illnesses, glandular problems, reproductive organ illnesses, respiratory organ illnesses, and bad or evil spirit complication categories (Table 6). Allium sativum L. obtained a common consensus against typhoid and common cold; Croton macrostachyus Hochst. ex Delile against dizziness and gonorrhea; Gymnanthemum amygdalinum (Delile) Sch.Bip. against malaria; Moringa stenopetala (Baker f.) Cufod. against glad-related complications; Ruta chalepensis L. against gonorrhea; and Withania somnifera (L.) Dunal against bad or evil spirits. Ethnobotanical studies conducted elsewhere in the country also revealed similar kinds of findings. For instance, [5] reported the efficacy of Allium sativum L. against cold and febrile illness (general malaise), Croton macrostachyus Hochst. ex Delile against febrile illness (general malaise), Gymnanthemum amygdalinum (Delile) Sch.Bip. against malaria, and Withania somnifera (L.) Dunal against bad or evil spirits. In another study, [14] revealed the significance of Croton macrostachyus Hochst. ex Delile against gonorrhea and febrile illnesses and Withania somnifera (L.) Dunal against bad or evil spirit complications. In the southern parts of the country, Tefera and Kim [8] also reported the medicinal value of Ruta chalepensis L. against gonorrhea. Again, in southern and southwestern parts of Ethiopia, [42, 52] confirmed the efficacy of Allium sativum L. against common cold. Similarly, [10, 52] reported the ethnomedicinal effectiveness of Croton macrostachyus Hochst. ex Delile against gonorrhea. Also [10, 42] reported the significance of Withania somnifera (L.) Dunal against bad or evil spirits in the southern parts of the country. However, Moringa stenopetala (Baker f.) Cufod. was found to be a novel finding in the study areas against gland-related problems. Therefore, further consideration and studies are needed to evaluate the information about the phytochemical and pharmacological potentials of the recorded ethnomedicinal plants for wider utilization.
Contrary to this, different consensuses were also noted among the three ethnic groups on some medicinal plants against circulatory system illness categories (snake venom). Those are Gymnanthemum auriculiferum (Hiern) Isawumi, which got the highest consensus within the Gedeo ethnic group against snake venom, whereas Solanum incanum L. and Searsia natalensis (Bernh. ex Krauss) F.A.Barkley were within the Oromo and Sidama ethnic groups, respectively, (Table 6). Besides, as compared to the Oromo ethnic group, the Sidama ethnic group showed great consensus to treat mental (rabies) disorders using Antiaris toxicaria (J.F.Gmel.) Lesch., and Justicia schimperiana (Hochst. ex Nees) T.Anderson. The Gedeo ethnic group informant has shown a unique agreement on the abruptness lightning complications using Croton macrostachyus Hochst. ex Delile and Ensete ventricosum (Welw.) Cheesman and against musculoskeletal illness using Calpurnia aurea (Aiton) Benth. and Croton macrostachyus Hochst. ex Delile. Informant consensus values near or zero indicate low informant agreement, which could be attributed to the community's use of different species for the same ailments [36, 45] (Table 6). Several studies conducted elsewhere also confirmed that conditions such as circulatory system disorders, gastrointestinal diseases, respiratory system disorders, Evil/bad spirits, and febrile illness were disease categories recognized as being efficiently treated by traditional plant medicine [8, 9, 39, 58, 60, 61].
Species consensus of informants
The fidelity level (FLs), relative popularity level (RPL), and rank-order priority (ROP) values are considered to determine for which illness a particular plant species is more effective in the study areas. In general, a rank-order priority (ROP) of 100% for a specific plant species indicates that all of the use reports mentioned were the same and an excellent choice for treating particular ailments [5, 62, 63]. In contrast, the low fidelity levels and low rank-order priority indicate the plant species will be employed for diverse purposes, according to [59]. The reported highest fidelity level values for Lactuca inermis Forssk., Moringa stenopetala (Baker f.) Cufod., Withania somnifera (L.) Dunal., Allium sativum L., Citrus limon (L.) Osbeck, Ricinus communis L., Schinus molle L., Antiaris toxicaria (J.F.Gmel.) Lesch., Brucea antidysenterica J.F.Mill., Echinops kebericho Mesfin, Ocimum jamesii Sebald, Afrocarpus falcatus (Thunb.) C.N.Page and Searsia natalensis (Bernh. ex Krauss) F.A.Barkley could be considered as evidence of the high healing potential of these plants against the corresponding diseases in the study areas (Table 7). In contrast, Ricinus communis L., and Allium sativum L. scored the lowest points against tonsillitis and fever, respectively. The revealed results confirmed that ethnic groups have diverse ethnobotanical knowledge of specific plants and disease conditions.
Different ethnobotanical investigations conducted elsewhere in the country and abroad revealed considerable evidence about the therapeutic potentials of some of the selected medicinal plants in the study areas. Consistently, Tefera and Kim [8] revealed the medicinal potential of Moringa stenopetala (Baker f.) Cufod. against cardiovascular diseases and [5, 10, 14] reported the efficacy of Withania somnifera (L.) Dunal. against bad or evil spirits in different parts of the country. Similarly, another study [5] confirmed the effectiveness of Allium sativum L. against common cold in the south-central parts of the country. In addition to our findings, [5, 9] reported the ethnomedicinal effectiveness of Echinops kebericho Mesfin against evil spirits, general malaise, abdominal pain, diarrhea, and amoebiasis in the central and south-central parts of the country. In other ethnobotanical investigations, [5, 9, 84] again elucidated the ethnomedicinal role of Allium sativum L. against skin diseases, malaria, toothache, general malaise, and tuberculosis. In Ethiopia and abroad, [5, 13, 14, 85] revealed the ethnomedicinal effectiveness of Withania somnifera (L.) Dunal. against febrile illnesses, general malaise, liver disorders, kidney pain, and blood purification. Thus, the use of the same plant species for related or dissimilar ethnomedicinal applications in different countries is a reliable indication of the recorded plant species' bioactivity potential, and the presence of a certain ailment in the area and the widespread use of traditional plant medicine [9, 64]. The findings will be used in future research to confirm the bioactivity of certain medicinal plants employed by traditional healers and boost their acceptance in broader healthcare systems in the country and abroad.
Use diversity and cultural roles of some medicinal plants
The medicinal plant species documented in this study are also cited for multiple local uses besides their medicinal role (Table 3). All medicinal plant species, particularly trees, shrubs, and herbs, were believed to be beneficial to the environment. Maintaining ecosystems through erosion regulation, soil enhancement, fodder and shelter for wild animals, and climate regulation were among the major roles. The mentioned environmental services were justified in the sense that each plant species has a role in supporting balanced biophysical systems. Based on the informants in our study, of the 189 identified medicinal plant species, 30 were reported for additional uses as food and 40 as livestock fodder, indicating their supplemental role in supporting the livestock and livelihood wealth of the study areas (Table 3). Additionally, more than 100 medical plant species were utilized as fuel (charcoal and firewood), whereas 16 were noted for timber production, which is the primary source of income for the majority of local communities. About 52 medicinal plant species were also employed for local construction uses, including 22 for social services such as cultural gathering under shade of those trees to resolve local conflict (Table 3). Around ten medicinal plant species were also identified as spices to food in the study areas. These findings demonstrated that the breadth of indigenous and local knowledge practices among local people in using plant resources for different purposes. On the other hand, the medicinal use values of plant species employed across different use categories demonstrated the relative importance of various plant species in people's everyday lives. Different studies conducted elsewhere in the countries also explained the diverse potentials of the documented medicinal plant species beyond their medicinal roles. For instance, Gurebiyaw et al. [102] mentioned the ecological significance of Albizia gummifera (J.F.Gmel.) C.A.Sm., Cordia africana Lam., and Croton macrostachyus Hochst. ex Delile on soil fertility enhancement. Negash [103] explained the promising options of Afrocarpus falcatus (Thunb.) C.N.Page, Cordia africana Lam., Croton macrostachyus Hochst. ex Delile, Ekebergia capensis Sparrm., Millettia ferruginea (Hochst.) Hochst. ex Baker, and Vachellia seyal (Delile) P.J.H.Hurter in maintaining soil fertility, soil regeneration and water conservation, provision of shade or shelter, as well as for windbreak.
In the study areas, it was also noted that farmers valued very much certain medicinal plant species for traditional farming tools and local buildings. Afrocarpus falcatus (Thunb.) C.N.Page and Olea europaea subsp. cuspidata (Wall. & G.Don) Cif. were preferred plant species for making three traditional Ethiopian farming tools, “Wanjoo, Gindii and Maneqoo” in the Oromo ethnic group and “Mofaara, Qanbaraa, and Maneqoo” in the Gedeo and Sidama ethnic groups, which are commonly drawn by a pair of oxen. Additionally, the wood and leaves of Olea europaea subsp. cuspidata (Wall. & G.Don) Cif. are burned to produce a characteristic smoke, which serves as a good flavor for fermenting milk and making local alcohol (e.g., locally known as Tella and Tej). Another intriguing aspect is that the Sidama ethnic group tendency for traditional house construction using bamboo species and Juniperus procera Hochst.Ex Endl. throughout the generations. The Sidama ethnic group is located in the southern Ethiopia and has unique expertise in how to create a stunning beehive-shaped traditional house entirely built of homogeneous woven bamboo. Juniperus procera Hochst. ex Endl. tree poles are used in the foundation because local communities think this species has natural resistance to microbes and termites and is long-lived. Dainty strands of bamboo are set around the edge of the house. The walls are made by parting the bamboo into more modest strips. The interior walls include two designs locally known as "Hilo and Himbiro".
Public health and roles of medicinal plants
Traditional medicine and medicinal plants have continued to play an essential role in the public healthcare system, both in the study areas and in elsewhere in the country. Because it is understandable that, in Ethiopia, almost 80% of the population uses traditional medicine, which is primarily based on medicinal plants [104], and more than 95% of folk medicine decoctions are derived from medicinal plants [105]. According to Lulekal et al. [9], the documented medicinal plants with high informant consensus (IC) and rank-order priority (ROP) values have promising potential against different pathogens and play a great role in maintaining the general public health of local communities and beyond. For instance, the authors reported high informant consensus and rank-order priority values for Afrocarpus falcatus (Thunb.) C.N.Page, Allium sativum L., Croton macrostachyus Hochst. ex Delile, Echinops kebericho Mesfin, Gymnanthemum amygdalinum (Delile) Sch.Bip., Moringa stenopetala (Baker f.) Cufod., Ruta chalepensis L., Withania somnifera (L.) Dunal, Ricinus communis L., and Zingiber officinale Roscoe (Tables 6 and 7) are indications for their role in maintaining the community’s health against different communicable and non-communicable diseases in the study areas. Besides, in vitro, investigations conducted by [79, 83, 85, 97–101] confirmed their effectiveness against many disease-causing pathogens in the country and abroad.
Conclusion
The medicinal plant resources in the studied rural–urban interface areas are considerably high. The associated knowledge of the local people is deep-rooted in the time-honored practices of traditional plant medicine, which depended heavily on medicinal plant species to cure different ailments. The study revealed a generational gap across ethnic groups in medicinal plant knowledge acquisition. Thus, older generations have continued to play a role as reservoirs for indigenous and local ethnobotanical knowledge practices. The use values of the most important medicinal plant species were evaluated and revealed considerable variability among the ethnic groups studied. Croton macrostachyus Hochst. ex Delile, Albizia gummifera (J.F.Gmel.) C.A.Sm., Zingiber officinale Roscoe, Aloe macrocarpa Tod., Gymnanthemum amygdalinum (Delile) Sch.Bip., Ruta chalepensis L., and Calpurnia aurea (Aiton) Benth. were noted species with high use value. Knowledge dissemination among informants was highest in the categories of circulatory system disorders, febrile illnesses, and reproductive organ complications across ethnic groups. The curative potential of some medicinal plants was evaluated and revealed significant fidelity values across ethnic groups. Lactuca inermis Forssk., Moringa stenopetala (Baker f.) Cufod., Withania somnifera (L.), Allium sativum L., Citrus limon (L.) Osbeck, Ricinus communis L., Schinus molle L., Antiaris toxicaria (J.F.Gmel.) Lesch., Brucea antidysenterica J.F.Mill., Echinops kebericho Mesfin, Ocimum jamesii Sebald, Afrocarpus falcatus (Thunb.) C.N.Page, and Searsia natalensis (Bernh. ex Krauss) F.A.Barkley are among the top ones. Thus, the revealed results will provide relevant information for further research focusing on investigating the bioactive compounds of some selected curative plants, sustaining indigenous and local ethnobotanical knowledge, and the associated most important medicinal flora. Besides, providing professional support to manage the ongoing dynamics and maintain the vast erosion of indigenous and local knowledge is vital.
Acknowledgements
The authors would like to express their cordial appreciation to the Regional Research School in Forest Sciences (REFOREST) Ph.D. scholarship program, supported financially by the Swedish Development Agency (Sida), which is hosted at the College of Forestry, Wildlife, and Tourism, Sokoine University of Agriculture. We acknowledge the Sidama, Oromo, and Gedeo traditional healers of Hawassa, Shashemene, and Dilla peri-urban areas, respectively, which unreservedly presented their impressive and valuable medicinal plant knowledge to us. We also extend our gratitude to the elders, and the local administrative authorities for their assistance in enabling the interviewing session. We are grateful to the Wondo Genet College of Forestry and Natural Resources, Hawassa University for providing us with logistical, field materials support and the herbarium facilities. We also greatly appreciated the support of the staff of the National Herbarium of Addis Ababa University for assisting us with plant identification.
Abbreviations
- CSA
Central Statistical Agency of Ethiopia
- US
Use value
- ICF
Informant consensus factor
- FL
Fidelity level
- RPL
Relative popularity level
- ROP
Rank-order priority
- SD
Standard deviation
- FC
Frequency of citation
- UR
Use reports
- NU
Number of uses
Author contributions
S.T. contributed to research conceptualization, methodology design and validation, data collection, plant identification, data entry and analysis, and writing the manuscript. F.B.M. contributed to planning the study and supervising manuscript development and revision of the manuscript. M.N. contributed to planning the study, research design, commenting on the manuscript’s development, and revision of the manuscript. L.C.K. contributed to designing, planning, and supervising the manuscript preparation.
Funding
The project was funded by the Regional Research School in Forest Sciences (REFOREST) Ph.D. scholarship program with financial support from the Swedish Development Agency (Sida) grant number 13394, hosted at the College of Forestry, Wildlife, and Tourism, Sokoine University of Agriculture, Tanzania.
Sokoine University of Agriculture,Sida Grant Number 13394,Sida Grant Number 13394,Sida Grant Number 13394,Sida Grant Number 13394
Availability of data and materials
All data generated or analyzed in this study are included in this manuscript.
Declarations
Ethics approval and consent to participate
Written permission to conduct the research was obtained from the Sokoine University of Agriculture (SUA) Office of the Vice-Chancellor research committee (Ref. no. SUA/FSC/D/2020/0012/12, dated February 17, 2022), and the three chosen peri-urban area local government heads (Hawassa, Shashemene, and Dilla District) were given authorization for the field study and plant collection via an official letter (Ref No: D/Z/W/03–23/1031, dated: 23/03/2022, (R/T/T/O/303/2021, dated March 28, 2021). Before providing oral informed consent, study participants were given a brief explanation of the study's objectives. Each participant gave his or her free consent to take part in the study. Finally, all interviewees' private information was protected and kept private.
Consent for publication
Not applicable.
Competing of interests
The authors state that no commercial, financial, or institutional ties that might be considered a possible conflict of interest existed during the research.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Jessen TD, Ban NC, Claxton NX, Darimont CT. Contributions of indigenous knowledge to ecological and evolutionary understanding. Front Ecol Environ. 2022;20(2):93–101. 10.1002/fee.2435 [DOI] [Google Scholar]
- 2.Saslis-Lagoudakis CH, Hawkins JA, Greenhill SJ, Pendry CA, Watson MF, Tuladhar-Douglas W, et al. The evolution of traditional knowledge: Environment shapes medicinal plant use in Nepal. Proc R Soc B Biol Sci. 2014;281:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Saynes-Vásquez A, Vibrans H, Vergara-Silva F, Caballero J. Intracultural differences in local botanical knowledge and knowledge loss among the Mexican Isthmus Zapotecs. PLoS ONE. 2016;11:1–19. 10.1371/journal.pone.0151693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Demie G, Negash M, Awas T. Ethnobotanical study of medicinal plants used by indigenous people in and around Dirre Sheikh Hussein heritage site of South-eastern Ethiopia. J Ethnopharmacol. 2018;220:87–93. 10.1016/j.jep.2018.03.033. 10.1016/j.jep.2018.03.033 [DOI] [PubMed] [Google Scholar]
- 5.Teka A, Asfaw Z, Demissew S, Van Damme P. Medicinal plant use practice in four ethnic communities (Gurage, Mareqo, Qebena, and Silti), south central Ethiopia. J Ethnobiol Ethnomed. 2020;16:1–12. 10.1186/s13002-020-00377-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dossou G, Sinsin B. butyracea in Benin: a quantitative approach. Atlantic. 2011;9:151–66. [Google Scholar]
- 7.Tudela-Talavera P, La Torre-Cuadros MDLÁ. Cultural importance and use of medicinal plants in the Shipibo-Conibo native community of Vencedor (Loreto) Peru. Ethnobot Res Appl. 2016;14:533–48. 10.17348/era.14.0.533-548 [DOI] [Google Scholar]
- 8.Tefera BN, Kim YD. Ethnobotanical study of medicinal plants in the Hawassa Zuria District, Sidama zone Southern Ethiopia. J Ethnobiol Ethnomed. 2019;15:1–21. 10.1186/s13002-019-0302-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lulekal E, Asfaw Z, Kelbessa E, Van Damme P. Ethnomedicinal study of plants used for human ailments in Ankober District, North Shewa Zone, Amhara Region, Ethiopia. J Ethnobiol Ethnomed. 2013;9:1–13. 10.1186/1746-4269-9-63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eshete MA, Molla EL. Cultural significance of medicinal plants in healing human ailments among Guji semi-pastoralist people, Suro Barguda District Ethiopia. J Ethnobiol Ethnomed. 2021;17:1–18. 10.1186/s13002-021-00487-4. 10.1186/s13002-021-00487-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.da Costa FV, Guimarães MFM, Messias MCTB. Gender differences in traditional knowledge of useful plants in a Brazilian community. PLoS ONE. 2021;16:1–16. 10.1371/journal.pone.0253820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kutal D, Kunwar RM, Baral K, Sapkota P, Sharma HP, Rimal B. Factors that influence the plant use knowledge in the middle mountains of Nepal. PLoS ONE. 2021;16:1–15. 10.1371/journal.pone.0246390. 10.1371/journal.pone.0246390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kidane L, Gebremedhin G, Beyene T. Ethnobotanical study of medicinal plants in ganta afeshum district, eastern zone of tigray, northern Ethiopia. J Ethnobiol Ethnomed. 2018;14:1–19. 10.1186/s13002-018-0266-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chekole G. Ethnobotanical study of medicinal plants used against human ailments in Gubalafto. J Ethnobiol Ethnomed. 2017;13:1–29. 10.1186/s13002-017-0182-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kunwar RM, Fadiman M, Cameron M, Bussmann RW, Thapa-Magar KB, Rimal B, et al. Cross-cultural comparison of plant use knowledge in Baitadi and Darchula districts Nepal Himalaya. J Ethnobiol Ethnomed. 2018;14:1–17. 10.1186/s13002-018-0242-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Giday M, Teklehaymanot T, Animut A, Mekonnen Y. Medicinal plants of the Shinasha, Agew-awi and Amhara peoples in northwest Ethiopia. J Ethnopharmacol. 2007;110:516–25. 10.1016/j.jep.2006.10.011 [DOI] [PubMed] [Google Scholar]
- 17.López S, Tarekegn A, Band G, Van Dorp L, Bird N, Morris S, et al. Evidence of the interplay of genetics and culture in Ethiopia. Nat Commun. 2021. 10.1038/s41467-021-23712-w. 10.1038/s41467-021-23712-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Belayneh A, Asfaw Z, Demissew S, Bussa NF. Medicinal plants potential and use by pastoral and agro-pastoral communities in Erer Valley of Babile Wereda Eastern Ethiopia. J Ethnobiol Ethnomed. 2012;8:1–11. 10.1186/1746-4269-8-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yineger H, Yewhalaw D, Teketay D. Ethnomedicinal plant knowledge and practice of the Oromo ethnic group in southwestern Ethiopia. J Ethnobiol Ethnomed. 2008;4(1):1–10. 10.1186/1746-4269-4-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mesfin F, Seta T, Assefa A. An ethnobotanical study of medicinal plants in Amaro Woreda Ethiopia. Ethnobot Res Appl. 2014;12:341–54. 10.17348/era.12.0.341-354 [DOI] [Google Scholar]
- 21.Agize M, Asfaw Z, Nemomissa S, Gebre T. Ethnobotany of traditional medicinal plants and associated indigenous knowledge in Dawuro Zone of Southwestern Ethiopia. J Ethnobiol Ethnomed. 2022;18:1–21. 10.1186/s13002-022-00546-4. 10.1186/s13002-022-00546-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bekele M, Woldeyes F, Lulekal E, Bekele T, Demissew S. Ethnobotanical investigation of medicinal plants in Buska Mountain range, Hamar district Southwestern Ethiopia. J Ethnobiol Ethnomed. 2022;18:1–26. 10.1186/s13002-022-00558-0. 10.1186/s13002-022-00558-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kassa Z, Asfaw Z, Demissew S. An ethnobotanical study of medicinal plants in Sheka Zone of Southern Nations Nationalities and Peoples Regional State, Ethiopia. J Ethnobot. 2020;7:5–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Megersa M, Woldetsadik S. Ethnobotanical study of medicinal plants used by local communities of Damot Ethnobotanical study of medicinal plants used by local communities of Damot Woyde District, Wolaita Zone, Southern Ethiopia. 2022
- 25.CSA. The 2007 Population and Housing Census of Ethiopia: Federal Democratic Republic of Ethiopia Population Census Commission. 2007;1–125.
- 26.Giday M, Asfaw Z, Woldu Z, Teklehaymanot T. Medicinal plant knowledge of the Bench ethnic group of Ethiopia: an ethnobotanical investigation. J Ethnobiol Ethnomed. 2009;5(1):1–10. 10.1186/1746-4269-5-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mesfin F, Demissew S, Teklehaymanot T. An ethnobotanical study of medicinal plants in Wonago Woreda, SNNPR Ethiopia. J Ethnobiol Ethnomed. 2009;5(1):1–18. 10.1186/1746-4269-5-28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Regassa R, Bekele T, Megersa M. Ethnobotonical study of traditional medicinal plants used to treat human ailments by halaba people, southern Ethiopia. J Med Plants Stud NAAS Rat JMPS. 2017;36:36–47. [Google Scholar]
- 29.Tamene S, Addisu D, Debela E, Tamene S, Addisu D, Debela E. Ethno-medicinal study of plants in Boricha district: use, preparation and application by traditional healers Southern Ethiopia. J Med plant Res. 2020;14:343–53. [Google Scholar]
- 30.Kindu M, Schneider T, Teketay D, Knoke T. Land use/land cover change analysis using object-based classification approach in Munessa-Shashemene landscape of the ethiopian highlands. Remote Sens. 2013;5:2411–35. 10.3390/rs5052411 [DOI] [Google Scholar]
- 31.Gebretsadik ZM. Watershed degradation and the growing risk of erosion in Hawassa-Zuria District Southern Ethiopia. J Flood Risk Manag. 2014;7:118–27. 10.1111/jfr3.12033 [DOI] [Google Scholar]
- 32.Girma T, Lika T, Maru M. Data on spatiotemporal land use land cover changes in peri-urban West Arsi Zone, Ethiopia: empirical evidences from Shashemene peri-urban areas. Data Br. 2018;18:747–52. 10.1016/j.dib.2018.03.082. 10.1016/j.dib.2018.03.082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Elias E, Seifu W, Tesfaye B, Girmay W. Impact of land use/cover changes on lake ecosystem of Ethiopia central rift valley. Cogent Food Agric. 2019. 10.1080/23311932.2019.1595876. 10.1080/23311932.2019.1595876 [DOI] [Google Scholar]
- 34.Kinfu E, Bombeck H, Nigussie A, Wegayehu F. The genesis of peri-urban Ethiopia: the case of Hawassa city. J Land Rural Stud. 2019;7(1):71–95. 10.1177/2321024918808125 [DOI] [Google Scholar]
- 35.Wondrade N, Dick OB, Tveite H. Landscape mapping to quantify degree-of-freedom, degree-of-sprawl, and degree-of-goodness of urban growth in Hawassa Ethiopia. Environ Nat Resour Res. 2014;4(4):223–37. [Google Scholar]
- 36.Jegora T, Asfaw Z, Anjulo A. Woody species diversity and management in homegarden agroforestry: the case of Shashemene District, Ethiopia. Int J For Res. 2019;2019:1–6. [Google Scholar]
- 37.CSA. The 1994 population and housing census in Ethiopia, result of Oromia Region. Central Statistical Authority, Addis Ababa, Ethiopia; 1994.
- 38.Debela MC, Muhye HK. Water supply and demand scenario of Dilla Town, Southern Ethiopia. Int J Water Resour Environ Eng. 2017;9:270–6. 10.5897/IJWREE2017.0748 [DOI] [Google Scholar]
- 39.Bekele-tesemma A. Useful trees and shrubs of Ethiopia: Identification, Propagation and Management for 17 Agroclimatic Zones. RELMA ICRAF Proj World Agrofor Cent—East Africa Reg Program P O Box 30677-00100, Nairobi Kenya Publ. 2007
- 40.Martin GJ. Ethnobotany: a methods manual. Routledge; 1995.
- 41.Alexiades MN. Collecting Ethnobotanical Data: An Introduction to Basic Concepts and Techniques. The New York Botabical Garden; 1996.
- 42.Balick MK, Cox PA. Plants, people, and culture. The sciences of ethnobotany. Selected guideline for ethnobotanical research. Taylor and Francis Group; 1996.
- 43.Tesemma AB. Useful trees and shrubs of Ethiopia: identification, propagation and managment for agricultral and pastoral communities. 1993.
- 44.Fichtl R, Adi A. Honeybee flora of ethiopi. In:Sue Edwards EK (ed.) In cooperation between the German Development Service (DED) and the Ministry of Agriculture–Livestock & Fishery Resources Main Department, Addis Ababa, Ethiopia; 1994.
- 45.Lock M, Edwards S, Tadesse M, Demissew S, Hedberg I, D. S, et al. Flora of Ethiopia and Eritraea Volume 2 Part 2. Canellaceae to Euphorbiaceae. Kew Bull. 1998.
- 46.Tadesse M. Flora of Ethiopia and Eritrea. Volume 4, Part 2: Asteraceae (Compositae). Biodivers. African Plants. 2004.
- 47.Awas T. Endemic plants of Ethiopia: preliminary working list to contribute to National plant conservation target. Inst Biodivers Conserv. 2006;14:1–14. [Google Scholar]
- 48.Hedberg I, Kelbessa E, Edwards S. Flora of ethiopia and eritrea volumes gentianaceae to cyclocheilaceae. Natl. Herb. Biol. Dep. Sci. Fac. Addis Ababa Univ. Ethiop.; Dep. Syst. Bot. Uppsala Univ. Sweden. 2006.
- 49.Tardío J, Pardo-De-Santayana M. Cultural importance indices: a comparative analysis based on the useful wild plants of southern Cantabria (northern Spain). Econ Bot. 2008;62:24–39. 10.1007/s12231-007-9004-5 [DOI] [Google Scholar]
- 50.Canales M, Hernández T, Caballero J, Romo-DeVivar A, Avila G, Duran A, et al. Informant consensus factor and antibacterial activity of the medicinal plants used by the people of San Rafael Coxcatlán, Puebla México. J Ethnopharmacol. 2005;97:429–39. 10.1016/j.jep.2004.11.013 [DOI] [PubMed] [Google Scholar]
- 51.Friedman J, Yaniv Z, Dafni A, Palewitch D. A preliminary classification of the healing potential of medicinal plants, based on a rational analysis of an ethnopharmacological field survey among Bedouins in the Negev Desert, Israel. J Ethnopharmacol. 1986;16:275–87. 10.1016/0378-8741(86)90094-2 [DOI] [PubMed] [Google Scholar]
- 52.Amjad MS, Ahmad I, Khan SU, Chaudhari SK, Malik NZ, Shaheen H, et al. Descriptive study of plant resources in the context of the ethnomedicinal relevance of indigenous flora: a case study from Toli Peer National Park , Azad Jammu and Kashmir. 2017. [DOI] [PMC free article] [PubMed]
- 53.Umair M, Altaf M, Abbasi AM. An ethnobotanical survey of indigenous medicinal plants in Hafizabad district Punjab-Pakistan. PLoS ONE. 2017;12:1–22. 10.1371/journal.pone.0177912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Renan L, Ferreira OO, Cruz JN, De JC, Franco P, Cascaes MM, et al. Lamiaceae essential oils, phytochemical profile, antioxidant, and biological activities. Hindawi Eviden-Based Comple Altern Med. 2021. 10.1155/2021/6748052. 10.1155/2021/6748052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sharma M, Sharma M, Bithel N, Sharma M. Ethnobotany, phytochemistry, pharmacology and nutritional potential of medicinal plants from asteraceae family. J Mt Res. 2022;17:67–83. [Google Scholar]
- 56.Woldeamanuel MM, Geda MK, Mohapatra S, Bastia TK, Rath P, Panda AK. Ethnobotanical study of endemic and non-endemic medicinal plants used by indigenous people in environs of Gullele botanical garden Addis Ababa, central Ethiopia: a major focus on Asteraceae family. Front Pharmacol. 2022;13:1–28. 10.3389/fphar.2022.1020097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mekuria T, Abduro H. Ethnobotanical study on medicinal plants used by local communities in Shashemene District, West Arsi Zone of Oromia Region Ethiopia Asian. J Plant Soil Sci. 2022;7:158–70. [Google Scholar]
- 58.Marshet G, Dalle M. Ethnobotanical study of medicinal plants in Nagelle Arsi District, West Arsi Zone of Oromia, Ethiopia. J Nat Sci Res. 2019;9
- 59.Tugume P, Kakudidi EK, Buyinza M, Namaalwa J, Kamatenesi M, Mucunguzi P, et al. Ethnobotanical survey of medicinal plant species used by communities around Mabira Central Forest Reserve, Uganda. J Ethnobiol Ethnomed. 2016;12:1–28. 10.1186/s13002-015-0077-4. 10.1186/s13002-015-0077-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hussain W, Badshah L, Ullah M, Ali M, Ali A, Hussain F. Quantitative study of medicinal plants used by the communities residing in Afghan borders. J Ethnobiol Ethnomed. 2018;14:1–18. 10.1186/s13002-018-0229-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Faruque MO, Uddin SB, Barlow JW, Hu S, Dong S, Cai Q, et al. Quantitative ethnobotany of medicinal plants used by indigenous communities in the Bandarban district of Bangladesh. Front Pharmacol. 2018;9:40. 10.3389/fphar.2018.00040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lautenschläger T, Monizi M, Pedro M, Mandombe JL, Bránquima MF, Heinze C, et al. First large-scale ethnobotanical survey in the province of Uíge, Northern Angola. J Ethnobiol Ethnomed. 2018;14:1–73. 10.1186/s13002-018-0238-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wiryono W, Wanandi Y, Ilahi AK, Deselina D, Senoaji G, Siswahyono S. The local knowledge of the plant names and uses by Semende tribe people in Kaur district, Bengkulu province Indonesia. Biodiversitas. 2019;20:754–61. 10.13057/biodiv/d200320 [DOI] [Google Scholar]
- 64.Al-robai SA, Ahmed AAE, Mohamed HA, Ahmed AA, Zabin SA, Alghamdi AAA. Qualitative and quantitative ethnobotanical survey in Al Baha Province Southwestern Saudi Arabia. J Divers. 2022;14:867. [Google Scholar]
- 65.Obey JK, Von Wright A, Orjala J, Kauhanen J, Tikkanen-kaukanen C. Antimicrobial activity of croton macrostachyus stem bark extracts against several human pathogenic bacteria. J Pathog 2016;2016. [DOI] [PMC free article] [PubMed]
- 66.Victor M, Mbunde N, Innocent E, Mabiki F. Ethnobotanical survey and toxicity evaluation of medicinal plants used for fungal remedy in the Southern Highlands of Tanzania. J Intercult Ethnopharmacol. 2017;6:84. 10.5455/jice.20161222103956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Faruque MO, Feng G, Khan MNA, Barlow JW, Ankhi UR, Hu S, et al. Qualitative and quantitative ethnobotanical study of the Pangkhua community in Bilaichari Upazilla, Rangamati District, Bangladesh. J Ethnobiol Ethnomed. 2019;15:1–29. 10.1186/s13002-019-0287-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gupta N, Agarwal AK, Kumar R. Ethnomedicinal and conservation evaluation of the traditional medicinal plant species employed by the Van Gujjar Tribe in the Dehradun Shivalik Hills, Uttarakhand, India. Ethnobot Res Appl. 2023;25:1–17. [Google Scholar]
- 69.Asfaw A, Lulekal E, Bekele T, Debella A, Debebe E, Sisay B. Medicinal plants used to treat livestock ailments in Ensaro District, North Shewa Zone, Amhara Regional State, Ethiopia. BMC Vet Res. 2022;18:1–17. 10.1186/s12917-022-03320-6. 10.1186/s12917-022-03320-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Alemneh D. Ethnobotanical study of medicinal plants used for the treatment of domestic animal diseases in yilmana densa and quarit districts, west gojjam zone, amhara region, ethiopia. Ethnobot Res Appl. 2021;22. [DOI] [PMC free article] [PubMed]
- 71.Tekle Y. An ethno-veterinary botanical survey of medicinal plants in Kochore district of Gedeo Zone, Southern Nations Nationalities and Peoples Regional State (SNNPRs) Ethiopia. J Sci Innov Res. 2014;3:433–45. 10.31254/jsir.2014.3407 [DOI] [Google Scholar]
- 72.Lulekal E, Asfaw Z, Kelbessa E, Van Damme P. Ethnoveterinary plants of Ankober District, North Shewa Zone, Amhara Region, Ethiopia. J Ethnobiol Ethnomed. 2014;10:1–19. 10.1186/1746-4269-10-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Eshetu GR, Dejene TA, Telila LB, Bekele DF. Ethnoveterinary medicinal plants: preparation and application methods by traditional healers in selected districts of southern Ethiopia. Veterinary World. 2015;8(5):674. 10.14202/vetworld.2015.674-684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Yigezu Y, Haile DB, Ayen WY. Ethnoveterinary medicines in four districts of Jimma zone, Ethiopia: cross sectional survey for plant species and mode of use. BMC Veterin Res. 2014;10:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chekole G, Asfaw Z, Kelbessa E. Ethnobotanical study of medicinal plants in the environs of Tara-gedam and Amba remnant forests of Libo Kemkem District, northwest Ethiopia. J Ethnobiol Ethnomed. 2015;11:1–38. 10.1186/1746-4269-11-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Geta O, Hansha H, Asafa O, Amde A. Ethnobotanical study of medicinal plants in ale woreda, South West Ethiopia. J Med Plants. 2020;8(5):121–9. [Google Scholar]
- 77.Beltrán-Rodríguez L, Ortiz-Sánchez A, Mariano NA, Maldonado-Almanza B, Reyes-García V. Factors affecting ethnobotanical knowledge in a mestizo community of the Sierra de Huautla Biosphere Reserve Mexico. J Ethnobiol Ethnomed. 2014;10:1–19. 10.1186/1746-4269-10-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sharma A, Thakur D, Uniyal SK. Plant-derived utility products: Knowledge comparison across gender, age and education from a tribal landscape of western Himalaya. J Ethnobiol Ethnomed. 2019;15:1–14. 10.1186/s13002-019-0346-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Amjad MS, Zahoor U, Bussmann RW, Altaf M. Ethnobotanical survey-of-the-medicinal-flora-of-Harighal-Azad-Jammu–Kashmir-PakistanJournal-of-Ethnobiology-and-Ethnomedicine.pdf. J Ethnobiol Ethnomed. 2020;16:1–28. 10.1186/s13002-020-00417-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Pathy KK, Flavien NB, Honoré BK, Vanhove W, Van Damme P. Ethnobotanical characterization of medicinal plants used in Kisantu and Mbanza-Ngungu territories, Kongo-Central Province in DR Congo. J Ethnobiol Ethnomed. 2021;17(1):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Khakurel D, Uprety Y, Ahn G, Cha JY, Kim WY, Lee SH, et al. Diversity, distribution, and sustainability of traditional medicinal plants in Kaski district, western Nepal. Front Pharmacol. 2022;13:1–15. 10.3389/fphar.2022.1076351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Silva FS, Ramos MA, Hanazaki N, de Albuquerque UP. Dynamics of traditional knowledge of medicinal plants in a rural community in the Brazilian semi-arid region. Rev Bras Farmacogn. 2011;21:382–91. 10.1590/S0102-695X2011005000054 [DOI] [Google Scholar]
- 83.Weckmüller H, Barriocanal C, Maneja R, Boada M. Factors affecting traditional medicinal plant knowledge of the Waorani, Ecuador. Sustainability. 2019;11(16):4460. 10.3390/su11164460 [DOI] [Google Scholar]
- 84.Mohammed AY, Kasso M, Demeke A. Knowledge, attitude and practice of community on traditional medicine in Jara Town, Bale Zone South East Ethiopia. Sci J Public Health. 2016;4(3):241. 10.11648/j.sjph.20160403.23 [DOI] [Google Scholar]
- 85.Silambarasan R, Sasidharan S, Kumar N, Aravind R, Nair AS, Selavinayagam KT. A multivariate and quantitative assessment of medicinal plants used by the indigenous Malayali tribes in the Javadhu hills of Tiruvannamalai district, Tamil Nadu, India. Heliyon. 2023;9:e15607. 10.1016/j.heliyon.2023.e15607. 10.1016/j.heliyon.2023.e15607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Maroyi A. Pharmacological properties of croton macrostachyus hochst. Ex Delile: a comprehensive review. Eviden-Based Complement Altern Med 2017;2017. [DOI] [PMC free article] [PubMed]
- 87.Dubale S, Kebebe D, Zeynudin A, Abdissa N, Suleman S. Phytochemical screening and antimicrobial activity evaluation of selected medicinal plants in Ethiopia. Exp Pharmacol. 2023;2023(15):51–62. 10.2147/JEP.S379805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Mao QQ, Xu XY, Cao SY, Gan RY, Corke H, Beta T, Li HB. 2019) Bioactive compounds and bioactivities of ginger (Zingiber officinale Roscoe. Foods. 2019;8(185):1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Moon YS, Lee HS, Lee SE. Inhibitory effects of three monoterpenes from ginger essential oil on growth and aflatoxin production of Aspergillus flavus and their gene regulation in aflatoxin biosynthesis. Appl Biol Chem. 2018;2018(61):243–50. 10.1007/s13765-018-0352-x. 10.1007/s13765-018-0352-x [DOI] [Google Scholar]
- 90.Atsafack S, Kodjio N, Fodouop S, Ntemafack A, Kuiate JR, Gatsing D. In vitro antisalmonellal and antioxidant activities of the crude extracts and fractions from the Stem Bark of Albizia gummifera (JF Gmel.) CA Sm. Brit J Pharm Res. 2016;10(6):1–11. 10.9734/BJPR/2016/24197 [DOI] [Google Scholar]
- 91.Tadesse WT, Endale A, Mohammedbrhan A, Tamiru TW. In vitro antibacterial activities of the leaf extracts of Aloe macrocarpa Tod (Aloaceae). Eur J Integr Med. 2017;12:74–8. 10.1016/j.eujim.2017.04.010 [DOI] [Google Scholar]
- 92.Lulekal E, Rondevaldova J, Bernaskova E, Cepkova J, Asfaw Z, Kelbessa E. Antimicrobial activity of traditional medicinal plants from Ankober district, north Shewa Zone, Amhara region Ethiopia. Pharm Biol. 2014;52(5):614–20. 10.3109/13880209.2013.858362 [DOI] [PubMed] [Google Scholar]
- 93.Bogale A, Alemayehu H, Nedi T, Engidawork E. Antidiarrheal and antibacterial activities of calpurnia aurea: benth seed different extracts. Eviden-Based Complem Altern Med 2022. [DOI] [PMC free article] [PubMed]
- 94.Gopalakrishnan VK, Tekluu B, Karri KC. The medicinal plant Calpurnia aurea leaves act as an anti-inflammatory source of 5-Lipoxygenase/Cyclooxygenase-2 dual inhibitors. 2020
- 95.Awan UA, Ali S, Shahnawaz AM, Shafique I, Zafar A. Biological activities of Allium sativum and Zingiber officinale extracts on clinically important bacterial pathogens, their phytochemical and FT-IR spectroscopic analysis. Pak J Pharm Sci. 2017;30(3):729–45. [PubMed] [Google Scholar]
- 96.Shaheen H, Qureshi R, Qaseem MF. Qualitative investigation techniques used for analysis of ethnobotanical data from Thal Desert Punjab Pakistan. J Med Plants. 2015;3:69–75. [Google Scholar]
- 97.Ishtiaq M, Khanum H, Hussain I, Parveen A, Maqbool M, Thind S, et al. Ethnobotanical inventory and medicinal perspectives of herbal flora of Shiwalik mountainous range of District Bhimber, Azad Jammu and Kashmir Pakistan. PLoS ONE. 2022. 10.1371/journal.pone.0265028. 10.1371/journal.pone.0265028 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 98.Singh AG, Kumar A, Tewari DD. An ethnobotanical survey of medicinal plants used in Terai forest of western Nepal. J Ethnobiol Ethnomed. 2012;8:14. 10.1186/1746-4269-8-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Islam MK, Saha S, Mahmud I, Mohamad K, Awang K, Jamal Uddin S, et al. An ethnobotanical study of medicinal plants used by tribal and native people of Madhupur forest area Bangladesh. J Ethnopharmacol. 2014;151:921–30. 10.1016/j.jep.2013.11.056 [DOI] [PubMed] [Google Scholar]
- 100.Cordero CS, Meve U, Alejandro GJD. Ethnobotanical documentation of medicinal plants used by the indigenous Panay Bukidnon in Lambunao, Iloilo Philippines. Front Pharmacol. 2022;12:790567. 10.3389/fphar.2021.790567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Enyew A, Asfaw Z, Kelbessa E, Nagappan R. Ethnobotanical study of traditional medicinal plants in and around Fiche District, Central Ethiopia. Curr Res J Biol Sci. 2014;6:154–67. 10.19026/crjbs.6.5515 [DOI] [Google Scholar]
- 102.Gurebiyaw K, Gelanew A, Yigzaw, M. Soil physical properties enhancement via native tree species in northern. J Adv Agric. 2019
- 103.Negash L. A selection of ethiopia’s indigenous trees biology uses and propagation techniques. Ethiopia: Addis Ababa University Press Addis Ababa; 2010. [Google Scholar]
- 104.Bekele E. Study on Actual Situation of Medicinal Plants in Ethiopia. Available from http://www.endashaw.com. Japan Assoc. Int. Collab. Agric. For. 2007.
- 105.Muluye AB, Ayicheh MW. Medicinal plants utilized for hepatic disorders in Ethiopian traditional medical practices: a review. Clin Phytoscience. 2020;6:1–11. 10.1186/s40816-020-00195-8 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed in this study are included in this manuscript.