Abstract
ABSTRACT
Background/purpose
Sepsis is a leading cause of morbidity, mortality and healthcare utilisation for children worldwide, particularly in resource-limited regions. In Kumasi, Ghana, organ system failure and mortality in children who present to the emergency department (ED) with symptoms of sepsis are often due to late presentation and lack of recognition and implementation of time-critical evidence-based interventions. The purpose of this study was to assess the barriers and facilitators for families in seeking healthcare for their septic children; and to understand the barriers and facilitators for ED providers in Kumasi to recognise and implement sepsis bundle interventions.
Design
Single-centre qualitative interviews of 39 caregivers and 35 ED providers in a teaching hospital in Kumasi, Ghana.
Results
Thematic analysis of data from caregivers about barriers included: fear of hospital, finances, transportation, delay from referring hospital, cultural/spiritual differences, limited autonomy and concerns with privacy and confidentiality. Negative impacts on family life included financial strain and neglect of other children. ED providers reported barriers included: lack of training, poor work environment and accessibility of equipment. Facilitators from caregivers and providers included some support from the National Health Insurance. Caregivers reported having positive experiences with frontline clinicians, which encouraged them to return to seek health services.
Implications
Qualitative structured interviews identified facilitator and critical barrier themes about seeking healthcare, and sepsis identification/management in the paediatric population arriving for care in our centre in Kumasi, Ghana. This study highlights significant deficiencies in healthcare systems that make sepsis management challenging in these settings.
Keywords: Child Health, Low and Middle Income Countries, Mortality, Qualitative research
WHAT IS ALREADY KNOWN ON THIS TOPIC
Delays in time-critical interventions and access to hospital interventions worsen sepsis outcomes in low- and middle-income countries.
Morbidity and mortality in children with sepsis presenting to Ghanaian hospitals are high.
WHAT THIS STUDY ADDS
Structured interviews of parents, caregivers and providers identified specific barriers and facilitators to sepsis treatment.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Targeted interventions to address barriers to hospital access and time-critical sepsis interventions can be developed.
Introduction
Worldwide, paediatric sepsis is a leading cause of morbidity and mortality, particularly in resource-limited regions1 2 and a global health emergency.3 When not identified/treated early, there is risk of progression to organ failure and death. This is linked to disparities: training in management of shock, health facilities lacking resources for basic care4 and late presentation to healthcare facilities.5 6 In Ghana, a Sub-Saharan low-middle-income country (LMIC), there are descriptions of spiritual and traditional illness constructs (ie, Asram) having a role in family healthcare-seeking behaviour for children aged under 5.7 Other factors such as the location of a hospital, availability of transportation, and economic status influence the ability of caregivers to seek healthcare for children.
At Komfo Anokye Teaching Hospital, a 1-year audit was performed and found a 9% prevalence of paediatric sepsis for admitted patients, with a 79% mortality rate for paediatric septic shock.8 There are institutional guidelines for the management of sepsis and shock,9 but prehospital and early hospital factors are not well studied. We sought to explore the perceived barriers and facilitators to seeking healthcare by caregivers whose children are septic and gained the perspectives of paediatric emergency department (ED) frontline clinicians.
Methods
We conducted a qualitative study between September 2023 and December 2023. We used an exploratory descriptive approach10 with in-depth interviews. The purpose of the interviews was fully explained to the study participants and voluntary written/signed consent was obtained, and monetary compensation was provided for participation. The funder of the study had no role in study design, data collection, data analysis, data interpretation or writing of this report.
Setting
This study was conducted at Komfo Anokye Teaching Hospital in Kumasi, Ghana. The hospital is an urban, tertiary care, public academic hospital that has a large catchment area serving most of central and northern Ghana. It has 1200 beds (mixed paediatrics and adult). The paediatric ED has 20 beds, and the paediatric intensive care unit (PICU) has six beds, with a paediatric ward of 240 beds. The paediatric ED sees approximately 300 cases of sepsis each year, with approximately 60 cases admitted to the PICU. The main providers in the ED include house officers, residents, attendings and nurses (average nurse to patient ratio, 1:4). Patients are triaged on entering the ED and deemed to go to the high-dependent ED unit or low-dependent ED unit, based on vitals and initial examination.
Patient and public involvement
Patient caregivers and clinical providers were involved in the design of the research. Practice interviews were conducted with caregivers and providers at the hospital to obtain feedback on the interview guide prior to the start of the study
Participants
The participants in the study included caregivers and frontline clinicians in the paediatric ED. We used a purposive sampling strategy to recruit the participants. Inclusion criteria for caregivers were (a) >18 years old, with a child (between 2 months and 14 years old) with sepsis in the ED, PICU or paediatric ward and (b) consent to participate. Sepsis was defined with the systemic inflammatory response syndrome criteria plus a suspected infection,11 and a child was identified for the study as vitals and/or labs were screened in the ED triage, PICU, or paediatric ward. Once a child was identified as meeting criteria, the caregivers were approached by the research team and invited to participate. The timing of approach depended on the location of the child. If identified in the ED, caregivers were approached after triage in the ED, for the PICU and paediatric ward—caregivers were approached during the hospitalisation. Frontline clinicians were selected based on consent to participate and were sampled by profession; nursing, house officer (medical school graduates who are completing 2 years of general rotations pre-residency), resident (postgraduate specialised trainee) to achieve diverse experiences and perspectives. Recruitment was discontinued when responses reached saturation.
Data collection and analysis
Face-to-face individual semistructured interviews were guided by interview templates, and focused on roles, facilitators, barriers/challenges and strategies for overcoming the barriers. Interviews were conducted by local Ghanaian research assistants from the Kwame Nkrumah University of Science and Technology who specialise in qualitative studies, led by qualitative expert, PRA. Interviewers were from outside institutions from the hospital and had no relationship with the patients, caregivers or frontline clinicians. Interviews were conducted either in English or the local language, Twi, based on the participant’s preference. The interview guide was first piloted with a caregiver and a frontline clinician (responses not included in final study). The interviews lasted 30–45 min. Audio recordings were transcribed verbatim by a team of local research assistants and translated into English (online supplemental file 1) .
Data analysis was performed using the six steps of thematic analysis.12 This analysis was concurrent with data collection, as it enabled researchers to understand the emerging themes. Four researchers (VCD, EGM, ED and PRA) reviewed each transcript independently to ensure a consistent approach to the data coding and identified themes as true reflection. The individual interviews were coded first to obtain individual accounts of their experiences and perspectives. The identified codes were then cross-referenced to evaluate whether different perspectives emerged using this approach. As the initial codes were found to be consistent, across for both caregivers and healthcare providers, the data were combined for the next step of the thematic analysis.
To ensure rigour, team meetings were then held that included the researchers, who reviewed the respective coding matrices to identify potential themes and subthemes.
Results
83 participants were approached—44 caregivers (3 had a child die) and 39 ED frontline clinicians; 74 participants (39 caregivers and 35 ED frontline clinicians) were interviewed (tables1 2). The caregivers who declined to be interviewed did not feel comfortable doing so, the clinicians declined due to their availability.
Table 1. Sociodemographic characteristics of caregivers.
| Characteristics | Total participants, n=39(%) |
| Age of caregivers | |
| 18–49 | 30 (77) |
| 50 and above | 9 (23) |
| Gender | |
| Male | 4 (10) |
| Female | 35 (90) |
| Level of education | |
| Tertiary | 9 (23) |
| Secondary | 12 (31) |
| Primary | 8 (20) |
| No formal education | 10 (26) |
Table 2. Sociodemographic characteristics of frontline clinicians.
| Characteristics | Total participants, n=35(%) |
| Frontline clinicians | |
| Resident | 7 (20) |
| House officer | 19 (54) |
| Nurse | 7 (20) |
| Midwife | 2 (6) |
| Years of experience post-training | |
| <1 | 12 (34) |
| 1–5 | 13 (37) |
| 5–10 | 9 (26) |
| >10 | 1 (3) |
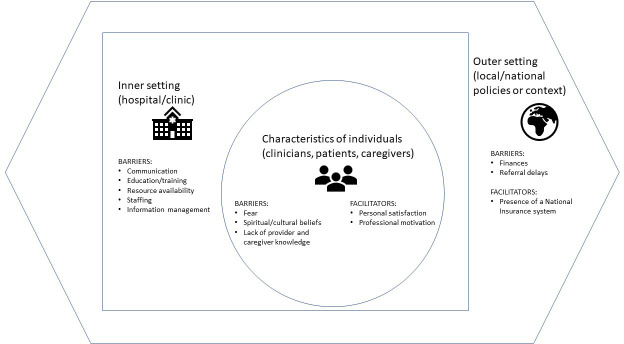
We identified three major domains (figure 1): (a) barriers to seeking healthcare, (b) facilitators to accessing healthcare and (c) strategies for enhancing access to healthcare.
Figure 1. Themes mapped to the Consolidated Framework for Implementation Research domains.21.
Barriers to seeking healthcare
Financial barriers
Caregivers highlighted financial constraints as a common challenge. Although the National Health Insurance Scheme (NHIS) in Ghana pays for most healthcare services for children, some caregivers still could not afford the high costs for medications and treatment, causing financial strain.
The challenge now is finances. The money we have spent is not easy, we have spent a lot buying medicines not covered by insurance. (Caregiver 4)
…I want my child to recover, but we are here so much I cannot work and take care of my other children, and I wonder if it’s better for her to die. (Caregiver 10)
Frontline clinicians affirmed similar sentiments.
…due to poverty, they usually come in late in a very bad state… the immediate goal is to stabilize such a child. (Physician 8)
Delays in referral system
Caregivers indicated they were referred from other rural facilities. Some asserted that they could not come immediately because there was no ambulance, and others reported the fear of going to the ‘big hospital in Kumasi’ and attributed the delay in referral to inadequate human resources. Caregivers mentioned that the limited staff led to extended waiting times, heightening children’s discomfort and aggravating their anxiety.
I spent 3 hours there because there was only one nurse who attended to many people. My child could no longer bear the pains because his temperature was rising, I cried because I was very anxious. (Caregiver 13)
Healthcare providers also described delays in referral, which delayed the treatment.
The delays in referral always happen. Some referring facilities only refer when it becomes critical. This is not helpful. (Physician 8)
Fear of the hospital
Fear of the hospital was seen as a barrier to seeking healthcare.
When I heard that we should come, I was terrified! Going to the big hospital meant either we would stay for a long time or return home without the child. (Caregiver 6)
Cultural and spiritual barriers
Some caregivers confirmed that severe illness is more spiritual than medical. They were confident that childhood illnesses were a result of something spiritual that needed traditional treatment.
…from a spiritual belief, when your stomach is swollen like this [referring to patient], it’s because you’ve been cursed, or drank poison, I just leave it to God. With this sickness, a Malam [ie, spiritual leader] can help with the treatment… (Caregiver 17)
Challenges in communication/information management
A notable barrier to accessing services was communication. Caregivers mentioned a lack of clarity and understanding regarding conditions and the treatment of their child. This left caregivers feeling uninformed or excluded, raising concerns about transparency and inclusivity in patient care. Caregivers mentioned that these communication challenges undermined the trust and confidence they hold in the healthcare system.
I don’t know what is wrong with my child. Nobody is telling me anything, whether there is hope for her to survive, I don’t know. I have to know so that I can decide if I have to seek help elsewhere. (Caregiver 20)
Similarly, frontline providers shared that an inadequate electronic medical record system prevents timely care by hindering timely and accurate sharing of patient information between healthcare professionals.
Also, the information management software/data entry does not work efficiently, it is difficult to share vital information. (Physician 8)
Education and training
Caregivers explained they had little/no knowledge about sepsis, hence it was difficult to identify symptoms. They knew that when a child felt ‘hot’, it meant that the child was unwell; however, caregivers were unable to tell the danger signs and when it was necessary to seek healthcare. Some explained that because of the fear of the hospital, they resort to other treatment options. Others who saw childhood illnesses as ‘spiritual’ did not see the necessity for promptly seeking healthcare.
I wish I had reported earlier, my son wouldn’t have died. I thought it was spiritual. I did not know it was serious, we were at home trying different local options. (Caregiver 31)
All frontline clinicians mentioned the need for further training to enhance their capacity in appreciating signs of sepsis and the treatment options to improve patient outcomes.
…I wish that we and nursing, got a lot more training on sepsis and other disease conditions and that we had more resources for education… (Physician 21)
Resources
Clinicians expressed frustration with the lack of access to resources, preventing providing quality care to patients with sepsis.
…there are lot of compromises with the care that we give, we do the best we can. I think because of our limited resources, the system doesn't help us to do the best that we can do. (Nurse 5)
Facilitators to accessing healthcare
Personal satisfaction/professional motivation
Caregivers explained they were encouraged to seek healthcare services whenever their children responded positively to treatments. This satisfaction further strengthened their belief and trust in the effectiveness of the healthcare system.
…all I want is for my child to get better. I trust coming to the hospital because my child gets well after the doctors treat him. This encourages me to seek care here. (Caregiver 15)
Frontline clinicians indicated that professional motivation, marked by observing positive healthcare outcomes for children, boosted their dedication and commitment to providing quality care.
The fact that patients come, and they are helpless, and you can intervene and put a smile on their face when they get better…. It’s the smile that makes me happy and encourages me to do more. (Physician 13)
Strategies for enhancing access to healthcare
Increasing financial support
Caregivers and frontline clinicians consistently emphasised the critical need for more affordable healthcare. Although the NHIS covers most services, some specific services and medications are not covered, particularly in cases involving serious health conditions, such as sepsis, in which treatment is expensive, multifaceted and multidisciplinary. To enhance access, the caregivers subsequently discussed that the NHIS should be more inclusive and comprehensive, covering both direct medical costs (ie, costs of services and medications) and indirect expenses (costs for transportation, accommodation and feeding of both caregivers and children).
…we are pleading with the government to help us cut down on some of the cost by widening the scope of coverage for the NHIS. They should pay for labs, scans, and help us with where mothers sleep and eat… (Caregiver 20)
If there is a way to get the NHIS to cover the majority of the services and medications, like a special fund for child health…it will render management to be more affordable and effective. (Physician 3)
Strengthening healthcare staffing and response efficiency
Caregivers highlighted the need for additional healthcare staff and commented on long waiting hours, suggesting recruitment of more nurses to improve service delivery for their children.
We have heard that a lot of the nurses have left to seek greener pastures abroad. They need additional nurses. (Caregiver 11)
Caregivers felt that the waiting times were moments of anxiety and needed to be improved. Frontline clinicians also shared that employing adequate expertise enhanced care.
When the hands are many, we are able to attend to patients promptly…and it saves time and even lives of our patients. (Nurse 13)
Improving communication and information sharing
Caregivers consistently expressed a desire for clearer communication, particularly regarding diagnoses and treatment. They stressed that communication is pivotal in building trust and ensuring that caregivers were adequately informed about the health conditions of the child.
…The doctors and nurses should be frank with us on the condition of our children, so we know the decision to take in the future. (Caregiver 1)
Frontline clinicians emphasised that continuous information sharing should be encouraged, as it ensures frontline clinicians are up to date with the latest practices and knowledge, enhancing the quality of care provided.
There should be information sharing among healthcare professionals. Everyone should know about sepsis, focusing on the importance of recognizing the signs and symptoms. (Physician 2)
Enhancing the rights of caregivers and children
Caregivers emphasised the need to ensure respect for the rights of both caregivers and children. They suggested that their right to be informed and to actively participate in healthcare decisions concerning their children should be encouraged. Respecting the privacy and confidentiality of information gathered on children could boost the trust they hold in healthcare systems.
I think our contributions should be actively sought in making treatment decisions concerning our children in every facility because nobody knows my child better than I do… (Caregiver 27)
Discussion
The interviews highlighted the perceived importance of financial burden, referral delays, spiritual and traditional beliefs, transportation, overall knowledge of a sick child and the need for training to recognise sepsis and initiate time-critical interventions. Previous work has explored the barriers to care in LMIC settings. Thaddeus and Maine develop the Three Delays Model through a literature review that demonstrated that in LMICs, obstetric complication outcomes were dependent on three phases: treatment seeking delay (due to costs and distance), delay in identification and accessing a health facility and a delay in receiving adequate care due to scant accessibility of health services.13 Our study specifically explored these barriers for septic children in an LMIC setting. Most barriers to effective sepsis care that were found in this study are not necessarily specific to sepsis, but are the consequences of general healthcare system challenges in these settings. In low-resource settings, the burden of sepsis is multifactorial and significantly driven by poverty, politics, health inequity and under-resourced health systems; the lack of supplies, non-sufficient healthcare facilities and the lack of inadequate access to critical care all contribute to this global health crisis.5 Yaya et al found there was a low rate of healthcare-seeking behaviour among mothers for childhood illnesses and linked to disparities in maternal education.14 Although the findings of our study can be applied to healthcare seeking and management of diseases in LMICs in general, we specifically explored the barriers and facilitators to timely sepsis and appropriate sepsis care for children who accessed the ED in Kumasi, Ghana, by uniquely obtaining the caregiver’s point of view and the healthcare providers’ in this Sub-Saharan African setting.
One area of improvement that was highlighted was the delay in referral. For many morbidities, patients in LMIC settings as opposed to higher income settings may experience longer delays before transfer.15 Although complex, addressing referral delays should be a core focus of interventions, with future implementation programmes focusing on modes of transportation and sepsis educational interventions in community/referral health centres that provide support on training providers to stabilise patients with sepsis prior to transfer. For improved ED management and transfer process in the Sub-Saharan African setting, resources such as the WHO Emergency Care Toolkit are available to be used in resource-limited hospital settings to help improve the systemic care of acutely ill patients,16 as potential solutions for improved quality of care for the critically ill child with sepsis. Families also expressed fear going to hospitals with thoughts that their child would die there. This is a complex response that is multifactorial involving not only families but the overall health system; late presentation, lack of financial resources and poor quality of care may all play a role in families’ fear of hospitals.6 7 Encouraging family participation in medical decision-making could strengthen the trust between providers and families, which could lead to families seeking medical care earlier. A study in Ghana showed that empathy and medical decision-making were a concern for many patients, and addressing this may improve patients’ trust in the healthcare system and compliance to treatment.17 Spiritual beliefs also have a distinct role in the delay to seeking healthcare,7 which leaves room for more education of caregivers who prioritise traditional treatments. Studies have reported the increased use of traditional medicine throughout Africa18; this should be targeted by healthcare policy makers to address the paediatric mortality/morbidity rates in Ghana.
Interventions to address staff burn-out and provider retention should be prioritised. Many frontline clinicians expressed frustration with difficulty accessing necessary supplies and resources such as intravenous fluids and antibiotics, which require families to purchase these items prior to use. There was also a universal request for further training and the need for more frontline clinicians. Implementing a paediatric sepsis protocol in this setting has been studied, and should be simple, precise, educational, and incorporate teamwork and effective communication.19 A focus should be made to incorporate specific sepsis training on sepsis recognition, with support of new sepsis criteria,20 and management, which could be adapted as a part of the new provider’s training process. In addition, this should be incorporated in the community to help engage and educate families on sepsis and illness recognition. The findings in this study confirm previous findings, which emphasised the need to strengthen healthcare delivery systems, resources and the ability to identify sepsis, to reduce the burden in LMIC settings.5
Our study has several limitations. Although we were able to reach thematic saturation of answers in the interviews, some caregivers did not feel comfortable participating due to the loss of a child or lack of consent from spouses (a cultural necessity to seek consent from the head of the household, which is the man). This could be a source of bias, which we tried to mitigate by approaching both caregivers and ensuring the approach was by a culturally appropriate individual who was fluent in their native dialect. Interviews were conducted with caregivers of children who successfully accessed the ED/hospital, but did not include those who failed to access the system. This source of potential bias is acknowledged, and thus our Consolidated Framework for Implementation Research framework represents the facilitators/barriers of those who accessed healthcare in this setting. The perspective of those unsuccessful or unwilling is important, but beyond the scope of this manuscript. Finally, we restricted our healthcare worker interviews to frontline clinicians, who are specifically the target for our proposed future educational intervention. The lack of inclusion of other healthcare workers may exclude important viewpoints, but was beyond the scope of this investigation.
Overall, this qualitative study highlighted many areas of potential action from both the caregiver and frontline clinician side that could be candidate interventions to improve mortality and morbidity of septic children. Future research should focus on a contextualised chain of survival for paediatric sepsis in LMIC settings that target prehospital measures to identify and treat septic children. In addition, these results open the opportunity for discussion with hospital administrators on addressing the systemic barriers.
supplementary material
Acknowledgements
Thank you to Dr Robert Tasker for his collaboration and contribution to this manuscript—Department of Anesthesiology, Critical Care and Pain Medicine, Boston Children’s Hospital, Boston, MA; Selwyn College, Cambridge University, UK. We thank all the participants, transcriptionists and qualitative teams.
Footnotes
Funding: VCD and VMN received unrestricted grants from CHOP’s Global Scientific Excellence Award, the CHOP Pediatric Critical Care Medicine Endowed Chair (VMN) and the University of Pennsylvania’s Global Holman Africa Research and Engagement Fund.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not applicable.
Ethics approval: This study involves human participants and was approved by the Institutional Review Board (IRB) of Komfo Anokye Teaching Hospital (24 August 2023; KATH IRB/AP/117/23) and deemed exempt by the IRB at the Children’s Hospital of Philadelphia. Participants gave informed consent to participate in the study before taking part.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Contributor Information
Vanessa C. Denny, Email: dennyv@chop.edu.
John Adabie Appiah, Email: adabiea@gmail.com.
Vinay M. Nadkarni, Email: Nadkarni@chop.edu.
Ebenezer Dassah, Email: edassah@gmail.com.
Ebenezer Gyimah Mensah, Email: gyimahebenezermensah@gmail.com.
Timothy Kwabena Adjei, Email: timkadjei@gmail.com.
Justicia Amisah, Email: justiciaamisah@gmail.com.
Gustav Nettey, Email: netteygustav1234@gmail.com.
Larko Owusu, Email: dlowusu@hotmail.com.
Charlotte Z. Woods-Hill, Email: woodshillc@chop.edu.
Heather A. Wolfe, Email: wolfeH@chop.edu.
Ebor Jacob G. James, Email: eborjacob@cmcvellore.ac.in.
Princess Ruhama Acheampong, Email: princessracheampong@gmail.com.
Data availability statement
Data are available upon reasonable request.
References
- 1.World Health Organization . World Health Organization; 2020. Global report on the epidemiology and burden of sepsis. [Google Scholar]
- 2.Reinhart K, Daniels R, Kissoon N, et al. Recognizing Sepsis as A Global Health Priority - A WHO Resolution. N Engl J Med. 2017;377:414–7. doi: 10.1056/NEJMp1707170. [DOI] [PubMed] [Google Scholar]
- 3.Kissoon N, Reinhart K, Daniels R, et al. Sepsis in Children: Global Implications of the World Health Assembly Resolution on Sepsis. Pediatr Crit Care Med. 2017;18:e625–7. doi: 10.1097/PCC.0000000000001340. [DOI] [PubMed] [Google Scholar]
- 4.James EJG, Vyasam S, Venkatachalam S, et al. Low-Cost “Telesimulation” Training Improves Real Patient Pediatric Shock Outcomes in India. Front Pediatr. 2022;10:904846. doi: 10.3389/fped.2022.904846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rudd KE, Kissoon N, Limmathurotsakul D, et al. The global burden of sepsis: barriers and potential solutions. Crit Care. 2018;22:232. doi: 10.1186/s13054-018-2157-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hill Z, Kendall C, Arthur P, et al. Recognizing childhood illnesses and their traditional explanations: exploring options for care-seeking interventions in the context of the IMCI strategy in rural Ghana. Trop Med Int Health. 2003;8:668–76. doi: 10.1046/j.1365-3156.2003.01058.x. [DOI] [PubMed] [Google Scholar]
- 7.Acheampong PR, Mohammed A, Twumasi-Ankrah S, et al. “This disease is not meant for the hospital, it is Asram”: Implications of a traditionally-defined illness on healthcare seeking for children under-5 in rural Ashanti, Ghana. PLOS Glob Public Health . 2022;2:e0000978. doi: 10.1371/journal.pgph.0000978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Appiah J. Komfo Anokye Teaching Hospital; 2022. Quality improvement report. [Google Scholar]
- 9.Weiss SL, Peters MJ, Alhazzani W, et al. Surviving Sepsis Campaign International Guidelines for the Management of Septic Shock and Sepsis-Associated Organ Dysfunction in Children. Pediatr Crit Care Med . 2020;21:e52–106. doi: 10.1097/PCC.0000000000002198. [DOI] [PubMed] [Google Scholar]
- 10.Hunter DJ, McCallum J, Howes D. Defining exploratory-descriptive qualitative (EDQ) research and considering its application to healthcare. Proceedings of Worldwide Nursing Conference; 2018. [Google Scholar]
- 11.Goldstein B, Giroir B, Randolph A. Members of the International Consensus Conference on Pediatric Sepsis. International pediatric sepsis consensus conference: Definitions for sepsis and organ dysfunction in pedatrics. Pediatr Crit Care Med. 2005;6 doi: 10.1097/00130478-200501000-00037. [DOI] [PubMed] [Google Scholar]
- 12.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- 13.Thaddeus S, Maine D. Too far to walk: maternal mortality in context. Soc Sci Med. 1994;38:1091–110. doi: 10.1016/0277-9536(94)90226-7. [DOI] [PubMed] [Google Scholar]
- 14.Yaya S, Odusina EK, Adjei NK. Health care seeking behaviour for children with acute childhood illnesses and its relating factors in sub-Saharan Africa: evidence from 24 countries. Trop Med Health. 2021;49:95. doi: 10.1186/s41182-021-00385-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zimmerman A, Fox S, Griffin R, et al. An analysis of emergency care delays experienced by traumatic brain injury patients presenting to a regional referral hospital in a low-income country. PLoS ONE . 2020;15:e0240528. doi: 10.1371/journal.pone.0240528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.WHO ECT
- 17.Atinga RA, Kuganab-Lem RB, Aziato L, et al. Strengthening quality of acute care through feedback from patients in Ghana. Afr J Emerg Med. 2015;5:24–30. doi: 10.1016/j.afjem.2014.10.008. [DOI] [Google Scholar]
- 18.James PB, Wardle J, Steel A, et al. Traditional, complementary and alternative medicine use in Sub-Saharan Africa: a systematic review. BMJ Glob Health. 2018;3:e000895. doi: 10.1136/bmjgh-2018-000895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Medeiros DNM, Shibata AO, Pizarro CF, et al. Barriers and Proposed Solutions to a Successful Implementation of Pediatric Sepsis Protocols. Front Pediatr. 2021;9:755484. doi: 10.3389/fped.2021.755484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sanchez-Pinto LN, Bennett TD, DeWitt PE, et al. Development and Validation of the Phoenix Criteria for Pediatric Sepsis and Septic Shock. JAMA. 2024;331:675–86. doi: 10.1001/jama.2024.0196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Damschroder LJ, Aron DC, Keith RE, et al. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci . 2009;4:50. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]