Abstract
Our study aimed to describe patient experience of information coordination between their primary care physician and specialists and to examine the associations between their experience and their personal and primary care characteristics. We conducted a cross-sectional study of Ontario residents rostered to a primary care physician and visited a specialist physician in the previous 12 months by linking population-based health administrative data to the Health Care Experience Survey collected between 2013 and 2020. We described respondents’ sociodemographic and health care utilization characteristics and their experience of information coordination between their primary care physician and specialists. We measured the adjusted association between patient-reported measures of information coordination before and after respondents received care from a specialist physician and their type of primary care model. 1,460 out 20,422 (weighted 7.5%) of the respondents reported that their specialist physician did not have basic medical information about their visit from their primary care physician in the previous 12 months. 2,298 out of 16,442 (weighted 14.9%) of the respondents reported that their primary care physician seemed uninformed about the care they received from the specialist. Females, younger individuals, those with a college or undergraduate level of education, and users of walk-in clinics had a higher likelihood of reporting a lack of information coordination between the primary care and specialist physicians. Only respondents rostered to an enhanced fee-for-service model had a higher odds of reporting that the specialist physician did not have basic medical information about their visit compared to those rostered to a Family Health Team (OR 1.22, 95% Cl 1.12–1.40). We found no significant association between respondent’s type of primary care model and that their primary care physician was uninformed about the care received from the specialist physician. In this population-based health study, respondents reported high information coordination between their primary care physician and specialists. Except for respondents rostered to an enhanced fee-for-service model of care, we did not find any difference in information coordination across other primary care models.
Introduction
Primary care is the first point of contact with the health care system and often coordinates services with other parts of the health care system, including care provided by specialist physicians [1, 2]. Information coordination is defined as the degree which patient medical information from different sources is shared and incorporated into patient’s current health care plan [3–5]. In Canada, health care is publicly funded through federal and provincial taxation with the federal government transferring funds to provinces and territories, which are responsible for administering and delivering health care services, including physician services [2]. In Ontario, patients typically need a referral from a physician or nurse practitioner to see a specialist physician. The gatekeeping role of primary care is reinforced through guidelines relevant to the practice of medicine and financial incentives [6, 7]. Recent reports suggest that 27% Ontario’s population (3.9 million) had a consultation with a specialist physician referred by a primary care physician [8]. Primary care physicians are required to communicate the medical reason for the patient’s visit to the specialist [7]. Once the course of care is completed, the specialist must transmit details of their findings and recommendations back to the primary care physician [7, 9].
Gaps in patient care information could undermine the quality-of-care patients receive and their satisfaction with care, particularly for complex patients who might feel overwhelmed navigating the health care system [10–12]. A longitudinal relationship to a primary care physician has shown to improve coordination of care with specialists [13, 14]. Also, information coordination with specialists have been shown to improve a patient experience, patient trust, chronic disease management (i.e., diabetes, cancer, COPD) and management of mental health issues [11, 15–17]. A physician survey showed that although 98% of primary care physicians sent information to specialists, only 67% received information back from the specialist physician about changes made to their patient’s medication or health care plan [18]. It is also reported that a greater use of specialist services may reduce information coordination among physicians [19–23].
In Ontario, different primary care models were introduced though a series of reform since early 2000 [24, 25]. These models are highly diverse in terms of their characteristics, governance and financial incentives to provide services for patients. While some models are paid per capita or salaried receive and receive support from a team of allied health care professionals including social works and care coordinators, such support is not available for 70% of Ontarians [24–26].
Patients directly experience the impact of information coordination in their care, influencing their perception of their overall health and their behavior of accessing health care services [27, 28]. Existing evidence on information coordination between primary care and specialist physicians has mostly focused on small patient populations [29–31], specific health conditions (e.g., depression, diabetes, cancer) [16, 17, 32], and reported the experiences of providers in coordinating information [10, 19, 33]. Also, large scale and multiyear data on patients’ experience of information coordination between primary care and specialist physicians are rarely available for research studies. Such data are necessary to understand the quality of information coordination between primary care and specialist physicians as experienced by patients.
Our objective was to describe patient reported experience on information coordination between their rostered primary care physician and specialist physician. We also wanted to examine the associations between their experience of information coordination and their personal and primary care characteristics. We hypothesized that respondents’ primary care model would be associated with the experience of information coordination between their rostered primary care physician and specialist physician.
Methods
Study design and setting
We conducted a cross-sectional study of Ontario residents who had a primary care physician and reported a visit to a specialist in the previous 12 months. We linked population-level administrative data to Ontario’s Health Care Experience Survey (HCES) collected between 2013 and 2020 using unique encoded identifiers.
Ontario had over 15.4 million residents in January 2023 and is the most populous province in Canada [34]. Physician services are publicly funded in Ontario and in most cases, delivered by private physician practices or non-for-profit organizations through different payment models. Over 87% of the population is formally rostered with a primary care physician in a patient enrolment model [24]. The remaining population receives care from fee-for-service or salaried primary care physicians nurse-practitioner-led clinics or do not have a primary care physician [24]. Patient enrolment models combine formal patient registration, blended funding consisting of a varying proportion of capitation payments, and bonuses for meeting preventive care targets [24]. Specialists are paid through a combination of alternative funding agreements and fee-for-service and can practice solo or as a team in the community or in a hospital setting [35]. The majority (87%) of physicians use an electronic medical record (EMR) system [36]. Yet, physicians still commonly use fax machines to send patient information [36] and only 37% of the primary care physicians use electronic referral system to exchange clinical information with a specialist physician outside their practice [36]. The use of data in this study was authorized under section 45 of Ontario’s Personal Health Information Protection Act, 2004 and did not require ethics review board approval.
Data sources
We linked the HCES survey data using unique anonymized identifiers with other health administrative datasets (S1 Appendix lists databases used) housed at ICES (formerly known as Institute for Clinical Evaluative Sciences) in September 2021. ICES is an independent, non-profit research institute whose legal status under Ontario’s health information privacy law allows it to collect and analyze health care and demographic data, without consent, for health system evaluation and improvement.
The HCES is a large population based cross-sectional household survey of Ontario residents created by the Ministries of Health and Long-Term Care to report on patients’ experience with the primary care system [37]. It has been active from 2012 to the present and is administered by telephone (mobile phone or landline) in English or French, to a target population that is 16 years and older living in private dwellings.
Potential participants for the HCES are selected from the Registered Persons Database (RPDB) which contains information on persons registered under the universal Ontario Health Insurance Plan (OHIP). The sample is collected using a stratified design (Ontario is first divided into 76 population strata, households were randomly selected from each stratum, and then one respondent is randomly selected from each household) [37]. Once a household is sampled, they are removed from the sampling frame for two years [38]. The survey excluded people living in institutions and households without telephones [37]. The total sample size of the survey was 11,200 each year, from 2013 to 2020 [37]. The overall response rate was 47.3% for our study period and ranged from 29% to 54% in each survey year [37].
Study population
Our study population included all participants of the HCES from Wave 2, January 2013 (the first complete survey wave after the pilot) to Wave 29, February 2020 (the last survey wave before pausing due to COVID-19) who reported seeing a specialist in past 12 months. We excluded those who were under 16 years old, reported not having a primary care provider and those who could not be linked to a primary care physician in the OHIP system on April 1 of the interview year.
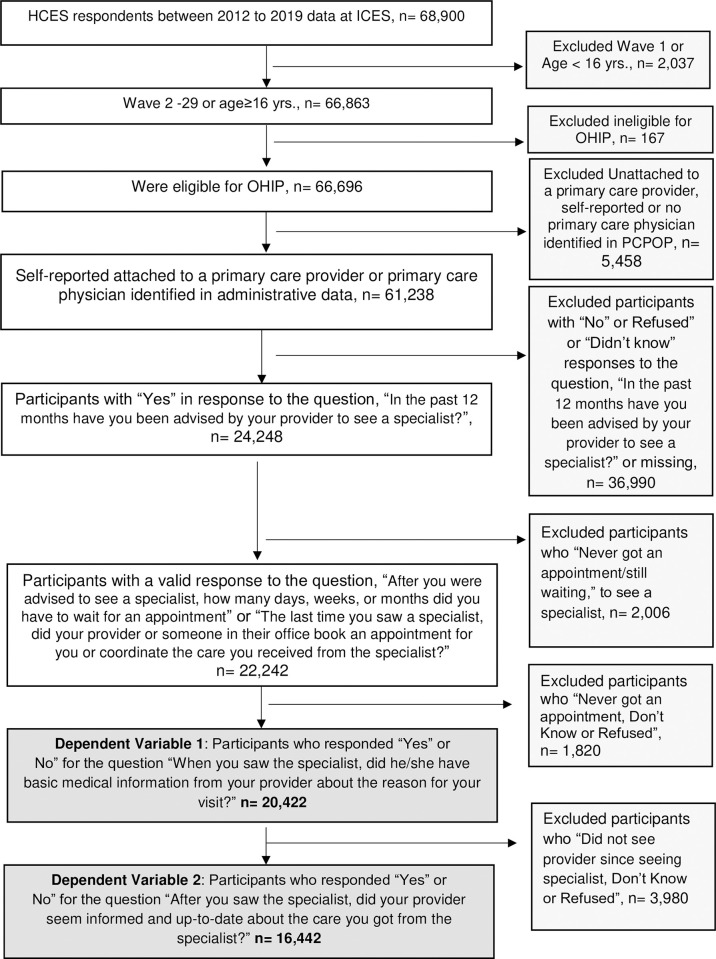
To analyze information coordination from the primary care physician to the specialist, we restricted the study population to those who reported “Yes” or “No” to the question: “When you last saw the specialist, did he/she have basic medical information from your [primary care] provider about the reason for your visit?”. And to analyze information coordination back to primary care from the specialist, we restricted the study population to those who reported “Yes” or “No” to the question: “After you saw the specialist, did your [primary care] provider seem informed and up to date about the care you got from the specialist?”. We excluded those who responded, “don’t know,” “refused” or were missing in each question. Fig 1 presents the complete exclusion criteria of the study population.
Fig 1. Inclusion and exclusion criteria for study population.
Dependent measures
Our two dependent measures were based on the survey questions: “When you last saw the specialist, did he/she have basic medical information from your [primary care] provider about the reason for your visit?” or “After you saw the specialist, did your [primary care] provider seem informed and up to date about the care you got from the specialist?” A “No” response was coded as 0 and a “Yes” response was coded as 1 in each question.
Independent measures
We included respondents’ age, sex, self-reported level of education, self-reported financial situation, the most commonly spoken language at home, self-reported wait-time to see the referred specialist, and self-reported use of walk-in clinic in the previous 12 months. Walk-in clinics provide medical services without requiring an appointment or referral for people who do not have a primary care physician or have one but are unable to reach them [38].
Patient’s rurality was calculated using the Rurality Index of Ontario (Large urban = 0; Medium urban = 1–9; Small urban = 10–39; and Rural ≥ 40). We determined respondent’s general medical complexity score using the CIHI Grouping Methodology at the time of the interview [39]. Respondents’ primary care model and rostered primary care physician, (including formally enrolled and virtually rostered to the physician with the highest total value of fee-for-service billing claims for primary care services over the previous 2 years [40] were obtained from the OHIP billing system. The total number of visits to the rostered primary care physician, the total number of visits to any specialists, and the number of specialties visited were calculated using physician billing data over the previous two years from the interview date. For descriptive purposes only, we included the total number of visits to any primary care physician, whether the patient reported receiving conflicting information from their rostered primary care physician and a specialist physician (data available only between wave 20 and 27 of the survey), whether the primary care physician or someone else in the office helped to book the specialist appointment or coordinated the care with the specialist physician (available only between wave 6 and 15). S2 Appendix includes the complete description of variables and data sources.
Statistical analysis
We reported demographic characteristics, count of visits to rostered primary care physician, count of visits to a specialist and respondent’s complexity score using weighted mean and standard deviation. For categorical variables, we reported raw counts and weighted proportions. We also calculated standardized mean difference, with difference greater than 10% considered meaningful [41]. We used separate multivariable logistic regression models to estimate unadjusted and adjusted odds ratios for each of the dependent variables (complete-case analysis). Data imputation was deemed unnecessary as the proportion of missing data was smaller than 5% [42]. We used generalized estimating equations with an exchangeable correlation structure to account for clustering at the level of rostered physician. We adjusted for age, sex, most commonly spoken language at home, self-reported levels of education, self-reported financial situation, self-reported wait-time to see a specialist, use of walk-in clinics in the previous 12 months, respondent’s primary care model, complexity score, total number of specialist visits, total number of visits to rostered primary care physician, and count of unique specialties visited over two years. We reported the results as adjusted odds ratios (ORs) with 95% confidence intervals (CIs).
We weighted all results using the post-stratification weight calculated from respondents’ age, sex, survey strata, total population in each stratum and the sampling probability weight. We considered a 2-tailed p value of less than 0.05 significant. We conducted all analysis using SAS Enterprise Guide software, Version 8.3 Copyright© 2020 SAS Institute Inc.
Results
After exclusions (Fig 1), there were 20,422 participants providing yes/no responses for our first dependent measure (whether specialist had basic medical information about reason for the visit from the primary care physician) and 16,442 for our second dependent measure (primary care physician seemed uninformed about the care received from the specialist physician). Table 1 presents the sample characteristics for both groups.
Table 1. Baseline characteristic of each respondent groups, Ontario Health Experience Survey, waves 2 to 29 (January 2013—February 2020).
| Respondents’ Characteristics | Specialist had basic medical information from the primary care physician about the reason for the visit | Primary care physician seemed informed about the care received from the specialist physician |
|---|---|---|
| (n = 20,422) | (n = 16,442) | |
| n (%) | n (%) | |
| Sex | ||
| Female | 12,275 (55.2) | 9,807 (55.2) |
| Male | 8,147 (44.8) | 6,635 (44.8) |
| Age (mean, SE) | 51.3 (0.19) | 51.5 (0.21) |
| Age category | ||
| 16–39 | ||
| 40–64 | 9,695 (42.7) | 7,727 (42.2) |
| 65–84 | 6,182 (26.5) | 5,094 (27,1) |
| 85+ | 472 (1.7) | 401 (1.8) |
| Rurality | ||
| Large urban (RIO score 0) | 7,352 (43.0) | 6,004 (43.5) |
| Medium urban (RIO score 1–9) | 5,447 (27.8) | 4,424 (28.1) |
| Small urban (RIO score 10–39) | 5,139 (20.6) | 4,073 (20.1) |
| Rural (RIO score 40+) | 2,484 (8.6) | 1,941 (8.3) |
| Self-reported education | ||
| High school | 5,959 (27.0) | 4,936 (27.8) |
| College or bachelor’s degree | 11,712 (58.3) | 9,306 (57.4) |
| Graduate or professional degree | 2,589 (14.0) | 2,068 (14.0) |
| Missing | 162 (0.7) | 132 (0.8) |
| Self-reported financial situation | ||
| Very comfortable | 3,229 (15.8) | 2,554 (15.6) |
| Comfortable | 11,987 (59.6) | 9,662 (59.8) |
| Tight/very tight/poor | 4,663 (22.0) | 3,799 (22.1) |
| Don’t know or refused | 543 (2.6) | 427 (2.4) |
| Language most often spoken at home | ||
| English or French | 18,537 (86.8) | 14,826 (86.0) |
| Other than English or French | 1,885 (13.2) | 1,616 (14.0) |
| Primary care physician or clinic booked the appointment or coordinated care with the specialist * | ||
| Yes | 5,378 (79.7) | 4,306 (80.4) |
| No | 1,245 (19.0) | 925 (18.3) |
| NA/I don’t know | 95 (1.3) | 72 (1.3) |
| Received conflicting information from primary care provider and specialist ** | ||
| Yes | 938 (13.0) | 807 (13.6) |
| No | 6,001 (83.2) | 4,995 (84.2) |
| Don’t know/Refused | 295 (3.8) | 134 (2.2) |
| Self-reported time waited to see a specialist | ||
| 2 weeks | 5,751 (29.1) | 4,685 (29.8) |
| 3–8 weeks | 8,411 (41.0) | 6,779 (40.9) |
| More than 8 weeks | 6,260 (29.9) | 4,978 (29.3) |
| Number of specialty types receiving care from | ||
| 1 type | 2,216 (13.1) | 1,719 (12.6) |
| 2 types | 2,980 (15.9) | 2,248 (14.7) |
| 3 types or more | 15,226 (71.0) | 12,475 (72.8) |
| Types of primary care models *** | ||
| Solo FFS | 861 (4.8) | 708 (5.0) |
| Enhanced FFS | 5,647 (32.4) | 4,728 (33.4) |
| Non-team Capitation | 6,231 (32.1) | 4,948 (31.6) |
| Team Capitation | 7,100 (29.9) | 5,611 (29.2) |
| Other PEM models | 583 (0.9) | 447 (0.8) |
| Self-reported use of a walk-in clinic in the last 12 months | ||
| Yes | 6,110 (33.7) | 5,025 (34.1) |
| No | 14,201 (65.8) | 11,330 (65.4) |
| I don’t know/Refused | 111 (0.5) | 87 (0.5) |
| Complexity score based on CIHI Pop Grouper (mean, SE) | 1.6 (0.03) | 1.7 (0.03) |
| Total visits to the rostered primary care physician over two years (mean, SE) | 8.9 (0.12) | 9.4 (0.14) |
| Total visits to any specialist physicians over two years (mean, SE) | 15.0 (0.15) | 15.8 (0.17) |
Note: Reporting raw counts, weighted proportions, and weighted means.
*Added in wave 6 and dropped in wave 15 of the survey and calculated for smaller sample size.
** Added in wave 20 of the survey and calculated for smaller sample size.
*** Solo FFS: Patients are not formally part of an enrolment model but receive care from a regular primary care physician who is paid purely fee-for-service. Enhanced Fee-for-Service includes Comprehensive Care Model and Family Health Group where physicians are paid a mix of fee-for-service along with bonuses and premiums. Non-team Capitation includes Capitation models, i.e., Family Health Organization and Family Health Network where physicians are paid a mix of capitation payment, bonuses, premiums, and fee-for-service but they are not signatory to a Family Health Team (FHT). FHTs are interdisciplinary models of care. Team Capitation: Capitation models, i.e., Family Health Organization and Family Health Network, are part of a Family Health Team (FHT). Other PEM models include smaller specialized patient enrolment models.
Descriptive comparisons
7.5% (n = 1,460) of the respondents reported that in the previous 12 months their specialist physician did not have basic medical information from the primary care physician about the reason for the visit. These respondents were more likely to be female, younger and a greater proportion of them reported having college or undergraduate levels of education. A higher proportion of them also reported that their primary care physician or clinic did not book or coordinate their care with the specialist physician (46.5% vs. 16.4%, SMD = 0.68) and received conflicting information from their primary care physician and specialist physician (23.0% vs. 12.2%, SMD = 0.28). They also visited a walk-in clinic in the last 12 months (43.9% vs. 32.8%, SMD = 0.23) were less complex (mean of complexity score 1.4 vs. 1.7, SMD = 0.10) and had a lower total number of visits to any specialist physician over the 2 years period (mean 13.4 vs. 15.1, SMD = 0.10) (Table 2).
Table 2. Descriptive comparison of those who reported that the specialist had basic medical information from the primary care physician about the reason for the visit (n = 20,422).
| Respondents’ Characteristics | Specialist had basic medical information from the primary care physician about the reason for the visit n (%) | Standardized Mean Difference | |
|---|---|---|---|
| Yes | No | ||
| 18,962 (92.5) | 1,460 (7.5) | ||
| Sex | |||
| Female | 11,324 (54.8) | 951 (60.1) | 0.11 |
| Male | 7.638 (45.2) | 509 (39.9) | |
| Age (mean, SE) | 51.7 (0.19) | 46.0 (0.57) | 0.32 |
| Age category | |||
| 16–39 | 3,639 (28.2) | 434 (40.6) | 0.26 |
| 40–64 | 9,006 (42.8) | 689 (41.4) | -0.03 |
| 65–84 | 5,869 (27.3) | 313 (17.0) | -0.25 |
| 85+ | 448 (1.7) | 24 (1.0) | -0.06 |
| Rurality | |||
| Large urban (RIO score 0) | 6,779 (42.7) | 573 (47.0) | 0.09 |
| Medium urban (RIO score 1–9) | 5,047 (27.8) | 400 (27.9) | 0.00 |
| Small urban (RIO score 10–39) | 4,800 (20.8) | 339 (18.3) | -0.06 |
| Rural (RIO score 40+) | 2,336 (8.7) | 148 (6.8) | -0.07 |
| Self-reported education | |||
| High school | 5.614 (27.5) | 345 (20.8) | -0.16 |
| College or bachelor’s degree | 10,799 (57.7) | 913 (64.7) | 0.14 |
| Graduate-professional degree | 2,394 (14.1) | 195 (14.1) | 0.00 |
| Missing | 155 (0.7) | 7 (0.4) | |
| Self-reported financial situation | |||
| Very comfortable | 3,010 (15.8) | 219 (15.5) | 0.00 |
| Comfortable | 11,164 (59.8) | 823 (57.3) | -0.05 |
| Tight/very tight/poor | 4,289 (21.8) | 374 (24.3) | 0.06 |
| Don’t know or refused | 499 (2.6) | 44 (2.9) | 0.03 |
| Language most often spoken at home | |||
| English or French | 17,211 (86.7) | 1,326 (87.9) | |
| Other | 1,751 (13.3) | 134 (12.1) | 0.04 |
| Primary care physician or clinic booked the appointment or coordinated care with the specialist * | |||
| Yes | 5,099 (82.2) | 279 (52.1) | -0.67 |
| No | 1,013 (16.4) | 232 (46.5) | 0.68 |
| NA/I don’t know | 86 (13.4) | 9 (1.4) | 0.00 |
| Received conflicting information from primary care provider and specialist ** | |||
| Yes | 823 (12.2) | 115 (23.0) | 0.28 |
| No | 5,666 (84.1) | 335 (71.6) | -0.30 |
| Don’t know/Refused | 263 (3.7) | 32 (5.4) | 0.08 |
| Self-reported waited to see a specialist | |||
| 2 weeks | 5,327 (29.1) | 424 (29.3) | 0.00 |
| 3–8 weeks | 7,891(41.3) | 520 (37.7) | -0.07 |
| More than 8 weeks | 5,744 (29.6) | 516 (33.1) | 0.07 |
| Number of specialty types receiving care from | |||
| 1 type | 1,977 (12.6) | 239 (19.7) | 0.20 |
| 2 types | 2,756 (15.8) | 224 (16.4) | 0.02 |
| 3 types or more | 14,229 (71.6) | 997 (63.9) | -0.17 |
| Types of primary care models *** | |||
| Solo FFS | 795 (4.7) | 66 (5.3) | 0.01 |
| Enhanced FFS | 5,185 (32.1) | 462 (35.7) | 0.03 |
| Non-team Capitation | 5,792 (32.1) | 439 (32.4) | -0.09 |
| Team Capitation | 6,637 (30.2) | 463 (26.0) | -0.04 |
| Other PEM models | 553 (0.9) | 30 (0.6) | 0.08 |
| Self-reported use of a walk-in clinic in the last 12 months | |||
| Yes | 5,532 (32.8) | 578 (43.9) | 0.23 |
| No | 13,331 (66.7) | 870 (55.0) | -0.24 |
| I don’t know/Refused | 99 (0.5) | 12 (1.1) | 0.07 |
| Complexity score based on CIHI Pop Grouper (mean, SE) | 1.7 (0.03) | 1.4 (0.06) | 0.10 |
| Total visits to any primary care physician over two years (mean, SE) | 13.0 (0.14) | 12.6 (0.45) | 0.03 |
| Total visits to the rostered primary care physician over two years (mean, SE) | 8.9 (0.12) | 8.1 (0.30) | 0.09 |
| Total visits to any specialist physicians over two years (mean, SE) | 15.1 (0.16) | 13.4 (0.48) | 0.10 |
Note: Reporting raw counts, weighted proportions, and weighted means.
*Added in wave 6 and dropped in wave 15 of the survey and calculated for smaller sample size.
** Added in wave 20 of the survey and calculated for smaller sample size.
***Solo FFS: Patients are not formally part of an enrolment model but receive care from a regular primary care physician who is paid purely fee-for-service. Enhanced Fee-for-Service includes Comprehensive Care Model and Family Health Group where physicians are paid a mix of fee-for-service along with bonuses and premiums. Non-team Capitation includes Capitation models, i.e., Family Health Organization and Family Health Network where physicians are paid a mix of capitation payment, bonuses, premiums, and fee-for-service but they are not signatory to a Family Health Team (FHT). FHTs are interdisciplinary models of care. Team Capitation: Capitation models, i.e., Family Health Organization and Family Health Network, are part of a Family Health Team (FHT). Other PEM models include smaller specialized patient enrolment models.
14.9% (n = 2,298) of the respondents reported that their primary care physician seemed uninformed about the care they received from the specialist physician. These respondents were also more likely to be female, younger and a greater proportion of them had a college or undergraduate level of education. A higher proportion of them received conflicting information from primary care physician and specialist physician (22.3% vs. 12.2%, SMD = 0.45). They were more likely to visit only 1 type of specialist over 2 years period (17.7% vs. 11.7%, SMD = 0.18) and a higher proportion of them reported visited a walk-in clinic in the previous 12 months (45.1% vs. 32.2%, SMD = 0.27). They were less likely to be complex (mean of complexity score 1.2 vs. 1.8, SMD = 0.28), had lower number of visits to their primary care physician (7.7 visits vs. 9.7 visits, SMD = 0.22) and lower number of visits to any specialist physician over the 2 years period (mean 12.7 vs. 16.3, SMD = 0.23) (Table 3).
Table 3. Descriptive analysis of those who reported that their primary care physician seemed uninformed about the care received from the specialist physician (n = 16,442).
| Respondents’ Characteristics | Primary care physician seemed informed about the care received from the specialist physician n (%) | Standardized Mean Difference | |
|---|---|---|---|
| Yes | No | ||
| 14,144 (85.1) | 2,298 (14.9) | ||
| Sex | |||
| Female | 8,332 (54.3) | 1,457 (60.4) | 0.13 |
| Male | 5,912 (45.7) | 823 (39.6) | |
| Age (mean, SE) | 52.9 (0.22) | 44.0 (0.42) | 0.51 |
| Age category | |||
| 16–39 | 2,433 (25.1) | 787 (45.5) | 0.42 |
| 40–64 | 6,618 (42.4) | 1,109 (40.8) | -0.03 |
| 65–84 | 4,715 (29.6) | 379 (12.9) | -0.42 |
| 85+ | 373 (1.9) | 23 (0.8) | -0.1 |
| Rurality | |||
| Large urban (RIO score 0) | 5,165 (43.4) | 839 (44.0) | 0.01 |
| Medium urban (RIO score 1–9) | 3,756 (27.8) | 668 (29.6) | 0.04 |
| Small urban (RIO score 10–39) | 3,530 (20.2) | 543 (19.6) | -0.02 |
| Rural (RIO score 40+) | 1,693 (8.6) | 248 (6.8) | -0.07 |
| Self-reported education | |||
| High school | 4,428 (29.2) | 508 (20.2) | -0.21 |
| College or bachelor’s degree | 7,864 (56.1) | 1,442 (64.6) | 0.18 |
| Graduate-professional degree | 1,734 (13.9) | 334 (14.4) | 0.02 |
| Missing | 118 (0.8) | 14 (0.8) | |
| Self-reported financial situation | |||
| Very comfortable | 2,215 (15.8) | 339 (14.1) | -0.05 |
| Comfortable | 8,371 (60.3) | 1,291 (56.9) | -0.07 |
| Tight/very tight/poor | 3,177 (31.3) | 622 (26.9) | -0.13 |
| Don’t know or refused | 381 (2.6) | 46 (2.1) | -0.03 |
| Language most often spoken at home | |||
| English or French | 12,784 (86.2) | 2,042 (85.0) | -0.03 |
| Other | 1,360 (13.8) | 256 (15.0) | |
| Primary care physician or clinic booked the appointment or coordinated care with the specialist * | |||
| Yes | 3,780 (83.3) | 526 (64.5) | 0.27 |
| No | 677 (15.4) | 248 (34.4) | -0.30 |
| NA/I don’t know | 63 (1.3) | 9 (1.1) | 0.11 |
| Received conflicting information from primary care provider and specialist ** | |||
| Yes | 4,440 (85.9) | 555 (73.9) | -0.44 |
| No | 613 (12.2) | 194 (22.3) | 0.45 |
| Don’t know/Refused | 103 (1.9) | 31 (3.8) | -0.02 |
| Self-reported waited to see a specialist | |||
| 2 weeks | 4,184 (30.8) | 501 (24.2) | -0.15 |
| 3–8 weeks | 5,895 (41.2) | 884 (39.6) | -0.03 |
| More than 8 weeks | 4,065 (28.0) | 913 (36.2) | 0.18 |
| Number of specialty types receiving care from | |||
| 1 type | 1,379 (11.7) | 340 (17.7) | 0.18 |
| 2 types | 1,864 (14.1) | 384 (17.9) | 0.10 |
| 3 types or more | 10,901 (74.2) | 1,574 (64.4) | -0.22 |
| Types of primary care models *** | |||
| Solo FFS | 608 (4.9) | 100 (5.6) | -0.03 |
| Enhanced FFS | 4,023 (33.2) | 705 (34.7) | 0.03 |
| Non-team Capitation | 4,283 (31.7) | 665 (30.3) | -0.02 |
| Team Capitation | 4,843 (29.3) | 768 (28.6) | -0.01 |
| Other PEM models | 387 (0.9) | 60 (0.8) | 0.03 |
| Self-reported use of a walk-in clinic in the last 12 months | |||
| Yes | 4,090 (32.2) | 935 (45.1) | 0.27 |
| No | 9,983 (67.3) | 1,347 (54.1) | -0.27 |
| I don’t know/Refused | 71 (0.5) | 16 (0.8) | 0.04 |
| Complexity score based on CIHI Pop Grouper (mean, SE) | 1.8 (0.03) | 1.2 (0.04) | 0.28 |
| Total visits to any primary care physician over two years (mean, SE) | 13.9 (0.17) | 12.0 (0.34) | 0.15 |
| Total visits to the rostered primary care physician over two years (mean, SE) | 9.7 (0.16) | 7.7 (0.20) | 0.22 |
| Total visits to any specialist physicians over two years (mean, SE) | 16.3 (0.18) | 12.7 (0.34) | 0.23 |
Note: Reporting raw counts, weighted proportions, and weighted means.
*Added in wave 6 and dropped in wave 15 of the survey and calculated for smaller sample size. Included only for descriptive purposes.
** Added in wave 20 of the survey and calculated for smaller sample size. Included only for descriptive purposes.
*** Solo FFS: Patients are not formally part of an enrolment model but receive care from a regular primary care physician who is paid purely fee-for-service. Enhanced Fee-for-Service includes Comprehensive Care Model and Family Health Group where physicians are paid a mix of fee-for-service along with bonuses and premiums. Non-team Capitation includes Capitation models, i.e., Family Health Organization and Family Health Network where physicians are paid a mix of capitation payment, bonuses, premiums, and fee-for-service but they are not signatory to a Family Health Team (FHT). FHTs are interdisciplinary models of care. Team Capitation: Capitation models, i.e., Family Health Organization and Family Health Network, are part of a Family Health Team (FHT). Other PEM models include smaller specialized patient enrolment models.
Adjusted association
Specialist did not have basic medical information from the primary care physician about the reason for the visit.
Female respondents and younger respondents had a higher odds reporting that their specialised physician did not have basic medical information from the primary care physician about the reason for the visit compared to male and older respondents. Respondents with a walk-in clinic visit in the previous 12 months also had a higher odds of reporting that the specialist physician did not have basic medical information from the primary care physician about the reason for the visit comparing to non-walk-in users (aOR 1.39, 95% Cl 1.19–1.61). Those who visited to more than one type of specialist had a lower odds of reporting that the specialist physician was uninformed about the reason for their visits compared to those visiting only 1 type of specialist. Only respondents rostered to an enhanced fee-for-service model (Family Health Group and Comprehensive Care Model) had a higher odds of reporting that the specialist physician did not have basic medical information from the primary care physician about the reason for the visit comparing to those rostered to a Family Health Team (aOR 1.22, 95% Cl 1.12–1.40) (Table 4).
Table 4. Adjusted odds ratios for dependent variables.
| Respondents’ Characteristics | Specialist did not have basic medical information from the primary care physician about the reason for the visit | Primary care physician seemed uninformed about the care received from the specialist physician | ||
|---|---|---|---|---|
| (n = 19,679 –missing 743) | (n = 15,827 –missing 615) | |||
| Unadjusted OR (CL) | Adjusted OR (CL) | Unadjusted OR (CL) | Adjusted OR (CL) | |
| Sex | ||||
| Male | Ref | Ref | Ref | Ref |
| Female | 1.25 (1.09–1.43) | 1.20 (1.14–1.38) | 1.28 (1.14–1.43) | 1.17 (1.04–1.31) |
| Age category | ||||
| 16–39 (ref) | Ref | Ref | Ref | Ref |
| 40–64 | 0.67 (0.58–0.78) | 0.73 (0.62–0.87) | 0.55 (0.48–0.62) | 0.58 (0.51–0.66) |
| 65–84 | 0.43 (0.36–0.52) | 0.55 (0.44–0.68) | 0.25 (0.21–0.29) | 0.35 (0.29–0.42) |
| 85+ | 0.40 (0.24–0.65) | 0.57 (0.34–0.94) | 0.24 (0.15–0.40) | 0.44 (0.27–0.73) |
| Self-reported education | ||||
| Graduate or professional degree | Ref | Ref | Ref | Ref |
| High school | 0.76 (0.61–0.95) | 0.80 (0.63–1.02) | 0.67 (0.55–0.81) | 0.72 (0.59–0.88) |
| College or bachelor’s degree | 1.12 (0.92–1.36) | 1.06 (0.86–1.29) | 1.11 (0.95–1.30) | 1.02 (0.86–1.20) |
| Self-reported financial situation | ||||
| Very comfortable | Ref | Ref | Ref | Ref |
| Comfortable | 1.14 (0.92–1.42) | 1.05 (0.83–1.32) | 1.41 (1.17–1.69) | 1.26 (1.05–1.53) |
| Tight/very tight/poor | 0.97 (0.81–1.18) | 0.93 (0.77–1.14) | 1.06 (0.89–1.24) | 0.98 (0.83–1.14) |
| Don’t know or refused | 1.16 (0.78–1.74) | 1.29 (0.85–1.96) | 0.89 (0.58–1.37) | 0.84 (0.54–1.30) |
| Language most often spoken at home | ||||
| English or French | Ref | Ref | Ref | Ref |
| Other than English or French | 1.89 (1.72–2.12) | 0.76 (0.60–0.96) | 1.10 (1.01–1.28) | 0.90 (0.76–1.08) |
| Self-reported waited to see a specialist | ||||
| 2 weeks | Ref | Ref | Ref | Ref |
| 3–8 weeks | 0.91 (0.77–1.07) | 0.95 (0.80–1.13) | 1.23 (1.06–1.42) | 1.2 (1.05–1.41) |
| More than 8 weeks | 1.11 (0.93–1.31) | 1.17 (0.98–1.39) | 1.64 (1.41–1.91) | 1.63 (1.40–1.80) |
| Number of specialty types receiving care from | ||||
| 1 type | Ref | Ref | Ref | Ref |
| 2 types | 0.66 (0.52–0.84) | 0.72 (0.55–0.95) | 0.83 (0.68–1.01) | 0.93 (0.75–1.17) |
| 3 types or more | 0.57 (0.48–0.68) | 0.71 (0.6.0–0.96) | 0.57 (0.48–0.67) | 0.89 (0.72–1.10) |
| Types of primary care models^ | ||||
| Team Capitation | Ref | Ref | Ref | Ref |
| Solo FFS | 1.29 (0.92–1.80) | 1.29 (0.91–1.80) | 1.17 (0.87–1.57) | 1.04 (0.77–1.14) |
| Enhanced FFS | 1.28 (1.09–1.52) | 1.22 (1.12–1.40) | 1.07 (0.93–1.23) | 0.93 (0.79–1.08) |
| Non-team Capitation | 1.17 (1.01–1.38) | 1.11 (0.93–1.32) | 0.98 (0.85–1.13) | 0.91 (0.78–1.05) |
| Other PEM models | 0.75 (0.36–1.57) | 0.82 (0.38–1.07) | 0.94 (0.59–1.38) | 1.05 (0.67–1.64) |
| Self-reported use of a walk-in clinic in the last 12 months | ||||
| No | Ref | Ref | Ref | Ref |
| Yes | 1.62 (1.41–1.86) | 1.39 (1.19–1.61) | 1.74 (1.55–1.95) | 1.40 (1.24–1.58) |
| I don’t know/Refused | 2.95 (1.46–5.96) | 3.01 (1.48–6.30) | 2.17 (0.12–1.43) | 0.44 (0.18–1.10) |
| Complexity score based on CIHI Pop Grouper (1 unit increase) | 0.95 (0.92–0.98) | 1.01 (0.98–1.04) | 0.85 (0.82–0.88) | 0.91 (0.90–0.97) |
| Total visits to the rostered primary care physician over two years (1 visit increase) | 0.98 (0.97–0.99) | 0.99 (0.98–1.01) | 0.97 (0.95–0.98) | 0.98 (0.97–0.99) |
| Total visits to any specialist physicians over two years (1 visit increase) | 0.99 (0.98–0.99) | 1.00 (0.99–1.00) | 0.98 (0.97–0.99) | 0.99 (0.99–1.01) |
Note: Rurality was excluded from the final multivariable regression model as it remained statistically not significant in both unadjusted and adjusted models. RIO’s unadjusted are included in S3 Appendix.
^ Solo FFS: Patients are not formally part of an enrolment model but receive care from a regular primary care physician who is paid purely fee-for-service. Enhanced Fee-for-Service includes Comprehensive Care Model and Family Health Group where physicians are paid a mix of fee-for-service along with bonuses and premiums. Non-team Capitation includes Capitation models, i.e., Family Health Organization and Family Health Network where physicians are paid a mix of capitation payment, bonuses, premiums, and fee-for-service but they are not signatory to a Family Health Team (FHT). FHTs are interdisciplinary models of care. Team Capitation: Capitation models, i.e., Family Health Organization and Family Health Network, are part of a Family Health Team (FHT). Other PEM models include smaller specialized patient enrolment models.
Adjusted associations
Primary care physician seemed uninformed about the care received from the specialist physician.
Female respondents and younger respondents had a higher likelihood of reporting that their primary care physician was uninformed about the care they received from the specialist physician compared to male and older respondents. Respondents with a walk-in clinic in the previous 12 months also had a higher odds of reporting that their primary care physician was uninformed about the care they received from the specialist physician compared to non-walk-in users (aOR 1.40, 95% Cl 1.24–1.58). Respondents with higher general medical complexity had lower odds of reporting that their primary care physician was uninformed about their specialist care (aOR 0.91, 95% Cl 0.90–0.97). We found no significant association with the patient’s primary care model (Table 4).
Discussion
We evaluated two patient-reported experience measures of information coordination between primary and specialist physicians in Ontario’s residents rostered to a primary care physician. Respondent’s experience of information coordination between primary care and specialist physicians was generally high. Respondents’ experience of information coordination generally did not differ across primary care models (except for those rostered in an enhanced FFS model). Walk-in clinic users reported lower information coordination with specialists. Older and complex respondents perceived that there was better information coordination between the primary care and specialist physicians.
By using a population-based multiyear patient-reported data, our study addresses the gap in previous studies (i.e., small sample size, focused on providers’ experience and disease-specific). Our findings align with the results of other surveys reporting high information coordination, especially among older age Canadians [43]. However, it appears that primary care physicians’ timely access to information from specialists remains a challenge [44]. Older respondents and those with complex health reported better information coordination, which may suggest that primary care and specialist physicians spend more time during visits with these patients [45] and the concentrated relationship primary care physician and specialists establish when caring for complex patients [46]. These findings may reflect years of investments and targeted government policies in improving health care for senior and complex patients [47, 48].
Enhanced FFS model of primary care and use of walk-in services appears to impact patients experience of information coordination between primary care and specialist physicians. Enhanced fee-for-service, fee-for-service and walk-in clinic models are financially incentivized to provide higher service volumes. Patients using walk-in clinics could often experience fragmented care given there is no formal relationship between the walk-in clinic physician and patients and information sharing could be challenging [49]. Thus, it is expected that respondents receiving care from these models would experience lower information coordination.
Information coordination could be supported with technological solutions that facilitate seamless information exchange between different levels of patients care achieving improved patients experience and quality of care. This could be supplemented by allowing patients to access their data, enabling them to actively participate in their care coordination and communicate with both their primary care provider and specialist physician. Also, our findings suggest that it is important to integrate walk-in clinics into the broader health care system to ensure continuity of patient information across different care providers. Patients with higher complexity scores may require additional support to feel supported, while also enabling seamless care transitions back to primary care.
Limitations
By using multiyear patient-reported data, we have addressed many of the limitations of earlier studies. However, the survey design is limited to households with a valid health insurance card, community dwellers, and those with an active phone number. This could exclude refugees, people experiencing homelessness, and some Indigenous populations resulting in an underrepresentation of these populations. Although survey results were weighted to represent the overall population, we cannot rule out the potential for selection bias from the survey’s design and non-response bias due to a decline of the survey’s overall response rate over time. We included data before the COVID-19 pandemic, since the practice of primary care has shifted (i.e., expanded virtual care and e-consultations) in Ontario which could also impact patients’ perception of how information is coordinated between physicians [50, 51]. As with all survey studies, our findings are subject to recall bias (e.g., influenced by patients’ previous healthcare experiences) resulting in a possible risk of misclassification. Further, information coordination between primary care and specialist physicians could be influenced by factors such as patients’ expectations and health literacy, and physician’s characteristics such as physicians’ communication skills. Many of these factors were not measurable from the existing health administrative datasets or the survey; thus, they could not be included in this study. Our findings are generalizable to jurisdictions with universal primary care where the primary care physician are the gatekeepers for accessing publicly funded services from specialist physicians.
Conclusion
Respondents reported high information coordination between their rostered primary care and specialist physicians. With exception to for respondents rostered to an enhanced FFS model of care, we did not find any difference across primary care models. Further research is needed to better understand physicians’ perspectives on the coordination of patient information and coordination of information with other sectors and providers (e.g., home care, acute care, pharmacists) given the shift in the role and function of primary care and increasing use of technology in delivering patient care.
Supporting information
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Acknowledgments
This study was supported by the ICES, which is funded by an annual grant from the Ontario Ministry of Health (MOH) and the Ministry of Long-Term Care (MLTC). Parts of this material are based on data and information compiled and provided by the Canadian Institute for Health Information (CIHI), and Cancer Care Ontario (CCO). The analyses, conclusions, opinions, and statements expressed herein are solely those of the authors and do not reflect those of the funding or data sources; no endorsement is intended or should be inferred.
Abbreviations
- CAPE
Client Agency Program Enrolment
- CCM
Comprehensive Care Model
- CCO
Cancer Care Ontario
- eFFS
Enhanced Fee-for-Service
- FFS
Fee-for-Service
- FHG
Family Health Group
- FHN
Family Health Network
- FHO
Family Health Organization
- FHT
Family Health Team
- HCES
Health Care Experience Survey
- IPDB
ICES Physician Database
- MLTC
Ministry of Long-Term Care
- MOH
Ministry of Health
- OHIP
Ontario Health Insurance Plan
- OHIP Claims
Ontario Health Insurance Plan Claims Database
- PCPOP
ICES Primary Care Population
- RPDB
Registered Persons Database
- RIO
Rurality Index of Ontario
Data Availability
Data cannot be shared publicly because of legal data sharing agreements between ICES (formerly known as Institute for Clinical Evaluative Sciences) and data providers (e.g., health care organizations and government) prohibit ICES from making the dataset publicly available. Data are available from the ICES (at https://www.ices.on.ca/DAS/AHRQ via email: das@ices.on.ca) to those who meet pre-specified criteria for confidential access. The dataset creation plan and underlying analytic code are available from the authors upon request.
Funding Statement
The work was originally part of a thesis internally funded by operating funds from St. Joseph’s Centre for Integrated Care that is funded by St. Joseph’s Health System (https://sjhs.ca/), and the Schlegel Chair in Clinical Epidemiology and Aging, McMaster University. There is no grant funding number available.
References
- 1.Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. The Milbank Quarterly. 2005;83(3):457–502. doi: 10.1111/j.1468-0009.2005.00409.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Deber RB, Mah CL. Case Studies in Canadian Health Policy and Management, Second Edition. University of Toronto Press; 2014. [Google Scholar]
- 3.Hofmarcher MM, Oxley H, Rusticelli E. Improved health system performance through better care coordination [Internet]. OECD; 2007. [cited 2024 May 19]. Available from: https://www.oecd-ilibrary.org/social-issues-migration-health/improved-health-system-performance-through-better-care-coordination_246446201766 [Google Scholar]
- 4.Longest BB, Young G. Coordination and Communication. In: Shortell SM, Kaluzny A, eds. Health Care Management: Organization Design and Behavior. 4th ed. Delmar; 2000. Pp. 210–243. [Google Scholar]
- 5.Ehrlich C, Kendall E, Muenchberger H, Armstrong K. Coordinated care: what does that really mean? Health Soc Care Community. 2009;17(6):619–27. doi: 10.1111/j.1365-2524.2009.00863.x [DOI] [PubMed] [Google Scholar]
- 6.Ontario Ministry of Health. Assessment and Consultations [Internet]; 2023. [cited 2024 May 19]. Available from: https://files.ontario.ca/moh/moh-resources-physicians-assessment-and-consultation-en-2023-05-12.pdf [Google Scholar]
- 7.College of Physicians and Surgeons of Ontario. CPSO—Transitions in Care [Internet]; 2019. [cited 2024 May 19]. Available from: https://www.cpso.on.ca/Physicians/Policies-Guidance/Policies/Transitions-in-Care [Google Scholar]
- 8.Referral to Specialists’ Data Table. Health Analytics and Insights Branch. Ontario Ministry of Health; 2023. [Google Scholar]
- 9.Williams TF, White KL, Fleming WL, Greenberg BG. The referral process in medical care and the university clinic’s role. J Med Educ. 1961; 36:899–907. [PubMed] [Google Scholar]
- 10.Ireson CL, Slavova S, Steltenkamp CL, Scutchfield FD. Bridging the care continuum: Patient information needs for specialist referrals. BMC Health Services Research. 2009;9(1): 1–12. doi: 10.1186/1472-6963-9-163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nickel S, Thiedemann B, Dem KO. The effects of integrated inpatient health care on patient satisfaction and health-related quality of life: Results of a survey among heart disease patients in Germany. Health Policy. 2020;98(2–3):156–163. [DOI] [PubMed] [Google Scholar]
- 12.Eastman MR, Kalesnikava VA, Mezuk B. Experiences of care coordination among older adults in the United States: Evidence from the Health and Retirement Study. Patient Education and Counseling. 2022;105(7):2429–2435. doi: 10.1016/j.pec.2022.03.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Starfield B. Primary Care: Balancing Health Needs, Services and Technology. Oxford University Press; 1998. [Google Scholar]
- 14.Liaw W, Moore M, Iko C. Bazemore A Lessons for primary care from the first ten years of Medicare coordinated care demonstration projects. J Am Board Fam Med. 2015;28(5):556–564. [DOI] [PubMed] [Google Scholar]
- 15.Butler M, Kane RL, McAlpine D. Does integrated care improve treatment for depression? A systematic review. J Ambul Care Manage. 2011;34(2):113–125. doi: 10.1097/JAC.0b013e31820ef605 [DOI] [PubMed] [Google Scholar]
- 16.Mohr DC, Benzer JK, Vimalananda VG, Singer SJ, Meterko M, McIntosh N. Organizational coordination and patient experiences of Specialty Care Integration. Journal of General Internal Medicine. 2019;34(S1):30–36. doi: 10.1007/s11606-019-04973-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stille CJ, Jerant A, Bell D, Meltzer D, Elmore JG. Coordinating care across diseases, settings, and clinicians: a key role for the generalist in practice. Ann Intern Med. 2005;142(8):700–708. doi: 10.7326/0003-4819-142-8-200504190-00038 [DOI] [PubMed] [Google Scholar]
- 18.Canadian Institute for Health Information (CIHI). How Canada Compares: Results from the Commonwealth Fund’s 2019 International Health Policy Survey of Primary Care Physicians. 2020. [Google Scholar]
- 19.Gandhi TK, Sittig DF, Franklin M, Sussman AJ, Fairchild DG, Bates DW. Communication breakdown in the outpatient referral process. J Gen Intern Med. 2000;15(9):626–631. doi: 10.1046/j.1525-1497.2000.91119.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Forrest CB, Nutting PA, Schrader S, Rohde C, Starfield B. Primary care physician specialty referral decision making: Patient, physician, and health care system determinants. Medical Decision Making. 2006;26(1):76–85. doi: 10.1177/0272989X05284110 [DOI] [PubMed] [Google Scholar]
- 21.Olmos-Ochoa TT, Bharath P, Ganz DA. Staff perspectives on primary care teams as de facto “hubs” for care coordination in VA: a qualitative study. J Gen Intern Med. 2019;34(Suppl 1):82–89. doi: 10.1007/s11606-019-04967-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Doty MM, Tikkanen R, Shah A, Schneider EC. Primary care physicians’ role in coordinating medical and health-related social needs in eleven countries. Health Affairs. 2020;39(1):115–123. doi: 10.1377/hlthaff.2019.01088 [DOI] [PubMed] [Google Scholar]
- 23.Liss DT, Chubak J, Anderson ML. Patient-reported care coordination: associations with primary care continuity and specialty care use. Ann Fam Med. 2011;9(4):323–329. doi: 10.1370/afm.1278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kiran T, Green ME, DeWit Y, Khan S, Schultz S, Kopp A. Association of Physician Payment Model and team-based care with timely access in primary care: A population-based cross-sectional study. CMAJ Open. 2020;8(2): E328–37. doi: 10.9778/cmajo.20190063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aggarwal M, Williams AP. Tinkering at the margins: evaluating the pace and direction of primary care reform in Ontario, Canada. BMC Family Practice. 2019. Dec; 20:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Glazier R, Kopp A, Schultz S, Kiran T, Henry D. All the right intentions but few of the desired results: Lessons on access to primary care from Ontario’s patient enrolment models. Healthcare Quarterly. 2012;15(2):17–21. [DOI] [PubMed] [Google Scholar]
- 27.Elliott J, Stolee P, Boscart V, Giangregorio L, Heckman G. Coordinating care for older adults in primary care settings: Understanding the current context. BMC Family Practice. 2018;19: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shunmuga Sundaram C, Campbell R, Ju A, King M, Rutherford C. Patient and healthcare provider perceptions on using patient-reported experience measures (prems) in routine clinical care: A systematic review of qualitative studies. Journal of Patient-Reported Outcomes. 2022;6(1):122. doi: 10.1186/s41687-022-00524-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Greenstone CL, Peppiatt J, Cunningham K, et al. Standardizing care coordination within the department of veterans affairs. J Gen Intern Med. 2019;34(Suppl 1).: 4–6. doi: 10.1007/s11606-019-04997-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jones D, Smith R. Kaiser Permanente: a fully integrated health care system. Nurs Adm Q. 2000;24(4):18–28. [Google Scholar]
- 31.Craver GA, Girnm G, Hill KEV. Understanding care coordination experiences in a state Medicare-Medicaid financial alignment demonstration. J Health Hum Serv Adm. 2018;41(2):196–236. [Google Scholar]
- 32.Gorin SS, Haggstrom D, Han PKJ, Fairfield KM, Krebs P, Clauser S. Cancer care coordination: A Systematic review and meta-analysis of over 30 years of empirical studies. Ann Behav Med. 2017;51(4):532–46. [DOI] [PubMed] [Google Scholar]
- 33.Forrest CB, Glade GB, Baker AE, Bocian A, Schrader S, Starfield B. Coordination of specialty referrals and physician satisfaction with referral care. Archives of Pediatrics & Adolescent Medicine. 2000;154(5): 499–506. doi: 10.1001/archpedi.154.5.499 [DOI] [PubMed] [Google Scholar]
- 34.StatsCan. Table: 17-10-0009-01: Population estimates by province or territory [Internet]. 2023. [cited 2024 May 19]. Available from: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1710000901 [Google Scholar]
- 35.Ontario Ministry of Health. Ontario Health Insurance Plan Division. Specialist Physician Contracts 101; 2023. [Google Scholar]
- 36.Canada Health Infoway. National survey of Canadian physicians [Internet]; 2021. [cited 2024 May 19]. Available from: https://insights.infoway-inforoute.ca/cma-digital-health-use/ [Google Scholar]
- 37.Ontario Ministry of Health and Ministry of Long-Term Care. Health Care Experience Survey (HCES) User’s Guide and Technical Documentation; 2021. [Google Scholar]
- 38.Ontario Ministry of Health. Walk-in Clinics [Internet]; 2019. [cited 2024 May 19]. Available from: https://www.ontario.ca/page/walk-clinics [Google Scholar]
- 39.Canadian Institute for Health Information (CIHI). CIHI’s Population Grouping Methodology 1.4: Overview and Outputs [Internet]; 2023. [cited 2024 May 19]. Available from: https://www.cihi.ca/sites/default/files/document/Infosheet-PopGroupMethod-2020-en.pdf [Google Scholar]
- 40.Stukel TA, Glazier RH, Schultz SE, Guan J, Zagorski BM, Gozdyra P, et al. Multispecialty physician networks in Ontario. Open medicine. 2013;7(2): e40. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Austin PC. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Communications in Statistics–Simulation and Computation. 2009;38(6):1228–1234. [Google Scholar]
- 42.Jakobsen JC, Gluud C, Wetterslev J, Winkel P. When and How Should Multiple Imputation Be Used for Handling Missing Data in Randomised Clinical Trials–a Practical Guide with Flowcharts. BMC Medical Research Methodology. 2017. Dec;17(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Canadian Institute for Health Information (CIHI). How Canada Compares: Results from the Commonwealth Fund’s 2021 International Health Policy Survey of Older Adults in 11 Countries [Internet]; 2022. [cited 2024 May 19]. Available from; https://www.cihi.ca/sites/default/files/document/how-canada-compares-cmwf-survey-2020-meth-note-en.pdf [Google Scholar]
- 44.Canadian Institute for Health Information (CIHI). The Commonwealth Fund’s 2022 International Health Policy Survey of Primary Care Physicians [Internet]; 2023. Available from: https://www.cihi.ca/en/improved-use-of-information-technology-can-result-in-more-coordinated-care-for-patients [Google Scholar]
- 45.Lin C, Albertson G, Schilling L, et al. Is patients’ perception of time spent with the physician a determinant of ambulatory patient satisfaction? Archives of Internal Medicine. 2001;161(11):1437–42. doi: 10.1001/archinte.161.11.1437 [DOI] [PubMed] [Google Scholar]
- 46.Agha L, Ericson K, Geissler K, Rebitzer J. Team Relationships and Performance: Evidence from Healthcare Referral Networks. Management Science. 2022;68(5):3735–3754. doi: 10.1287/mnsc.2021.4091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bielska IA, Cimek K, Guenter D, et al. Change in Health Care Use after Coordinated Care Planning: a quasi-experimental Study. CMAJ Open. 2018;6(2): E218–E226. doi: 10.9778/cmajo.20170053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Government of Ontario. Aging with confidence: Ontario’s action plan for seniors [Internet]; 2017. [cited 2024 May 19]. Available from: https://files.ontario.ca/ontarios_seniors_strategy_2017.pdf [Google Scholar]
- 49.Lapointe-Shaw L, Kiran T, Salahub C, et al. Walk-in clinic patient characteristics and utilization patterns in Ontario, Canada: A cross-sectional study. CMAJ Open. 2023;11(2): E345–56. doi: 10.9778/cmajo.20220095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ashcroft R, Ryan B, Mehta K, et al. “Healthcare at its finest”: Patient perspectives on virtual care appointments in primary care. The Annals of Family Medicine. 2022;22(Supplement 1):1544–1709. [Google Scholar]
- 51.Wu K, Nguyen MD, Rouleau G, Azavedo R, Srinivasan D, Desveaux L. Understanding how virtual care has shifted primary care interactions and patient experience: A qualitative analysis. Journal of Telemedicine and Telecare. 2023;0(0). doi: 10.1177/1357633X231167905 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
Data cannot be shared publicly because of legal data sharing agreements between ICES (formerly known as Institute for Clinical Evaluative Sciences) and data providers (e.g., health care organizations and government) prohibit ICES from making the dataset publicly available. Data are available from the ICES (at https://www.ices.on.ca/DAS/AHRQ via email: das@ices.on.ca) to those who meet pre-specified criteria for confidential access. The dataset creation plan and underlying analytic code are available from the authors upon request.