Abstract
Background/Aims
In alcohol-associated hepatitis (AH), the Lille score is used to assess futility of steroids. However, the ability of the Lille score to predict 30-day survival in AH is not well-defined. Our aim is to compare the utility of the Lille score in predicting 30-day survival in those with AH treated with steroids.
Methods
Retrospective chart review of 882 patients hospitalized with AH from January 1st, 2012 through December 30th, 2019 was performed. Of these, 201 patients with severe AH met the threshold to receive steroids. Those with data to calculate Lille score < 0.45 on day 4 (n = 29) or 7 (n = 89) who continued steroids were compared to 83 patients with Lille scores ≥ 0.45 on day 4 (n = 18) or 7 (n = 65) who stopped steroids. The primary outcome was 30-day survival. For comparison, a contemporaneous matched control group was also analyzed of 110 patients who were hospitalized with severe AH, but did not receive steroids.
Results
In patients with Lille score < 0.45, survival was higher at 30-day when compared to those with Lille score ≥ 0.45 (94.9% vs. 80.72%; p = 0.002). The sensitivity, specificity, positive predictive value and negative predictive value of Lille score (< 0.45) to predict 30-day survival was 95%, 19%, 63%, and 73%, respectively.
Conclusions
In severe AH, those with Lille score < 0.45 at day 4 or 7 have improved 30-day survival compared to those with Lille score ≥ 0.45. In those receiving steroids, Lille score has excellent sensitivity to predict 30-day survival but poor specificity.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10620-024-08479-6.
Keywords: Lille, Alcohol-associated hepatitis, Survival, Steroids
Introduction
Alcohol-associated hepatitis (AH) is a clinical syndrome associated with severe morbidity and mortality in the setting of excessive alcohol use. Among those with severe forms of AH, short-term mortality approaches near 30% [1]. To define severity, Maddrey’s discriminant function (MDF) was created to determine indications to initiate steroids (MDF > 32) if no contraindications are present such as gastrointestinal bleeding or uncontrolled infection [2]. This finding has been confirmed regardless of the control prothrombin time (PT) used to calculate MDF [3]. More recently, Model for End-Stage Liver Disease (MELD) has been found to be a better prognostic marker for the severity of AH, with scores > 20 being the threshold for steroids in the appropriate clinical setting [4].
Although these markers help define severity of AH and identify those who might benefit from steroids, not all patients respond favorably to this therapeutic intervention. In fact, prednisone has failed to improve outcomes at 90 days and one year in AH [1]. Given the extensive side effect profile of steroids and their questionable benefit, the Lille score was created to assess the futility of steroids [1, 5]. For this score, the age of the patient, creatinine (Cr), total bilirubin (TB), albumin, and prothrombin time (PT) are calculated on admission, with the TB also being calculated after four or seven days of steroid therapy [5, 6]. Based on the computed calculation, a value < 0.45 at day 4 or 7 would signify patients as steroid responders; a 28-day course of steroids is typical in this setting if no contraindications are present [3]. For values ≥ 0.45 at day 4 or 7, patients are determined to be non-responders and thereby steroid therapy should be discontinued. While Lille score helps to identify which patients are likely to benefit from continued steroids after day 4 or day 7 of use, its impact on 30-day (30-day) survival alone is not well-defined. To address this gap, our aim was to compare the utility of the Lille score to predict 30-day survival in those with AH that met the threshold to be treated with steroids.
Methods
Patient Cohort
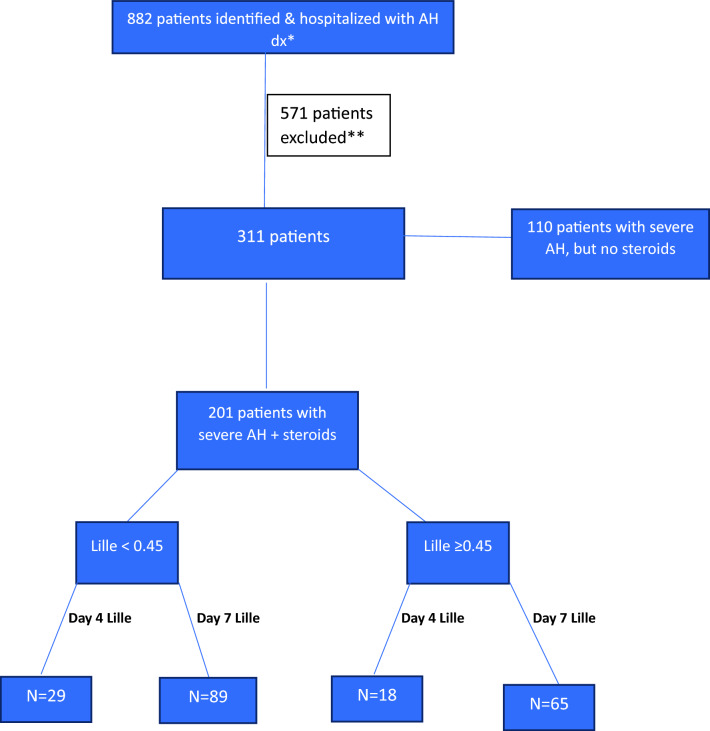
A retrospective chart review was performed on 882 patients with AH based on ICD-10 codes (Fig. 1) at a tertiary care institution from January 1st, 2012 through December 30th 2019. Of this group, 511 patients were excluded for either being given an incorrect ICD-10 code where an alternative diagnosis was more plausible, not meeting National Institute on Alcohol Abuse and Alcoholism (NIAAA) criteria for diagnosis of AH, not having a high enough MELD or MDF (≥ 20 and/or > 32, respectively) to be considered severe AH, or lack of laboratory data to calculate Lille score [7]. Among those excluded, there was no separate analysis performed as to how many patients were excluded per each reason above. Since those with AH that was not severe did not meet the threshold to receive steroids, a Lille score was not calculated to determine response to steroids. After exclusions, 311 patients were included in this analysis.
Fig. 1.
Flowsheet depicting breakdown of AH cohort. dx diagnosis, N number of patient’s. *given diagnosis based off ICD-10 code criteria and NIAAA criteria, **exclusion criteria were not being given correct ICD-10 and/or another disease process was more plausible, lack of laboratory data to calculate Lille score, or MELD/MDF not high enough to meet threshold to receive steroids
Of the 311 patients analyzed, 110 were used as a comparison group and defined as those who had severe AH but did not receive steroids. The remainder of the patients (n = 201) was the focus of the analysis and was further sub-divided according to Lille score at Day’s 4 and 7. Of this cohort, 118 receiving steroids had a Lille score < 0.45, with the Lille score taken on day 4 (n = 29) or day 7 (n = 89) depending on the length of hospitalization. Steroids were continued for a planned 28-day course in these groups after discharge. Eighty-three patients with a Lille score ≥ 0.45 on day 4 (n = 18) and on day 7 (n = 65) in whom steroids were stopped due to futility were included for comparison. Consent was waived in this study as it was retrospective.
Inclusion and Exclusion Criteria
The use and futility of steroids to treat severe AH was made by the treating inpatient team in consultation with the hepatology attending in this uncontrolled analysis. The admitting team used clinical intuition taken together with the patient’s clinical presentation and laboratory data to confirm or refute the diagnosis of AH. To define eligibility for steroids, MDF > 32 and/or MELD > 20 were strictly used as cutoffs. However, some patients may not have received steroids despite having severe AH due to contraindications that were present such as uncontrolled infection and bleeding. Other exclusion criteria used at our institution to withhold steroids despite having met criteria for severe AH included sepsis, septic shock, positive blood cultures, multiorgan failure, and if another plausible explanation for abnormal liver enzymes and/or chemistries was present. Anemia was not an absolute contraindication to steroid use, but active gastrointestinal bleeding was a relative contraindication if not properly controlled by endoscopic or interventional radiologist guided therapy.
Study Measures
For all patients included in the analysis, data on age, gender, race, ethnicity, weight, body mass index (BMI), obesity (BMI ≥ 30 kg/m2) and presence of type 2 diabetes mellitus (T2DM) to define metabolic dysfunction with alcohol related liver disease (MetALD) were gathered. In addition, laboratory markers such as aspartate aminotransferase (AST), alanine aminotransferase (ALT), TB, international normalized ratio (INR), PT, albumin, and Cr were obtained. MELD upon admission and discharge, as well as MDF on admission was calculated using a control PT value of 13.5 [3].
Statistical Analysis
The primary outcome was 30-day survival, which was analyzed for Lille score < 0.45 at day’s 4 and 7, Lille score ≥ 0.45 at day’s 4 and 7, and in those patients who had severe AH but did not receive steroids as a contemporaneous matched control group. The sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) for the Lille score’s utility to predict 30-day survival was also computed. Odds ratio was gathered for this sub-group analysis. Statistical analysis was performed for patients who received steroids based on Lille score < 0.45 vs. Lille score ≥ 0.45. Additionally, patients who were eligible to receive steroids compared to those who were not was performed by assessing statistical differences between two groups.Statistical differences for all continuous variables were assessed using the two-sample t-test with unequal variances. Statistical differences for the 30-day survival categorical variable were assessed using Fisher exact test. The impact of BMI, obesity and/or T2DM (Met-ALD) was also performed. All analyses were performed in R statistical software (R Core Team (2023), Vienna, Austria).
Results
Demographic and clinical characteristics comparing all patients with severe AH who received steroids to those with severe AH whom did not receive steroids are found in Table 1. Those with severe AH who received steroids were found to be younger (mean age 46 vs. 49; p = 0.008), have higher TB (18.4 mg/dL vs. 12.2 mg/dL; p = 0.002), and MDF (59.1 vs. 46.1; p = 0.001). Those whom received steroids also had lower Cr (1.09 mg/dL vs. 1.38 mg/dL; p = 0.013) and MELD on admission (24.6 vs. 26; p = 0.027). No differences in weight, obesity, T2DM, MetALD, AST, ALT, albumin, INR, MELD at discharge, or 30-day survival were found between these groups.
Table 1.
Patients who were hospitalized with AH and eligible but did not receive steroids, compared to those who were eligible and received steroids
| Contents | Steroids yes | Steroids no | P-value |
|---|---|---|---|
| Number of subjects | 201 | 110 | – |
| Age in years | 45.6 (11.2) | 48.9(10.3) | 0.008 |
| Female/Male | 103/98 | 53/57 | – |
| Race (AA/W/unknown) | 31/149/21 | 34/63/13 | – |
| Ethnicity % non-Hispanic | 91.54% | 86.36% | – |
| Weight in kg | 85.0 (24.4) | 82.1(22.7) | 0.299 |
| BMI kg/m2 | 30.0 (13.8) | 30.7(24.7) | 0.746 |
| Obesity (BMI ≥ 30 kg/m2) | 82 (41%) | 40 (36%) | 0.54 |
| Type 2 Diabetes Mellitus | 33 (16%) | 18 (16%) | 1.0 |
| MetALD | 97 (48%) | 50 (45%) | 0.81 |
| AST U/L | 215 (167) | 291(907) | 0.250 |
| ALT U/L | 59.7 (45.6) | 101(363) | 0.112 |
| Total bilirubin mg/dL | 18.4 (11.3) | 12.2(9.34) | 0.001 |
| Albumin g/dL | 2.68 (0.533) | 2.80(0.675) | 0.073 |
| PT sec | 22.3 (5.93) | 21.1(7.28) | 0.102 |
| INR | 1.98 (0.682) | 1.84(0.867) | 0.134 |
| Creatinine mg/dL | 1.09 (0.771) | 1.38(1.26) | 0.013 |
| MDF (using PT 13.5) | 59.1 (30.8) | 46.1(36.3) | 0.001 |
| MELD (admission) | 24.6 (7.69) | 26.(5.40) | 0.027 |
| MELD (discharge) | 26.4 (15.8) | 25.6(8.15) | 0.627 |
| 30-day survival rate | 89.05% | 80.90% | 0.058 |
AA African American, W white, BMI body mass index, MetALD metabolic dysfunction associated alcoholic liver disease, AST aspartate aminotransferase, ALT alanine aminotransferase, PT prothrombin time, INR international normalized ratio, MDF maddrey discriminatory function, MELD model for end stage liver disease
The demographic and clinical characteristics delineated by Lille score’s < 0.45 and ≥ 0.45 at day’s 4 and 7 of calculation are found in Table 2. For terminology, those with a Lille score < 0.45 were defined as steroid responsive, while those with a Lille score ≥ 0.45 were non-responders to steroids. Compared to all patients (days 4 and 7) with Lille score ≥ 0.45, those with scores < 0.45 were younger (mean age 43 vs. 49; p = 0.001), with lower TB (16 mg/dL vs. 22 mg/dL; p = 0.001), INR (1.8 vs. 2.2; p = 0.001), Cr (0.9 mg/dL vs. 1.3 mg/dL; p = 0.001), MELD on admission (22 vs. 28; p = 0.001) and MDF (50 vs. 72; p = 0.001), though achieved higher albumin (2.8 g/dL vs. 2.5 g/dL; p = 0.001). There were no differences in demographics, weight, AST, ALT, or MELD at discharge between groups.
Table 2.
Demographic and clinical characteristics of cohort according to Lille score cutoff of < 0.45 and ≥ 0.45 at day 4 and 7
| Contents | Lille score < 0.45 | Lille score ≥ 0.45 | ||||
|---|---|---|---|---|---|---|
| Day 4 | Day 7 | Combined | Day 4 | Day 7 | Combined | |
| No. of subjects | 29 | 89 | 118 | 18 | 65 | 83 |
| Age in yearsa | 42.5 (9.28) | 42.5 (10.0) | 43.0 (10.2) |
53.4 (12.1) |
48.1 (11.2) |
49.2 (11.6) |
| Female/Male | 15/14 | 46/43 | 61/57 | 9/9 | 35/30 | 44/39 |
| Race (AA/W/unknown) | 3/23/3 | 15/64/10 | 18/87/13 | 3/12/3 | 9/52/4 | 12/64/7 |
| Ethnicity % non-Hispanic | 88.46% | 88.37% | 88.4% | 88.88% | 96.92% | 95.18% |
| Weight in kg |
84.1 (20.2) |
81.9 (23.2) |
82.8 (22.3) |
81.2 (23.4) |
90.1 (27.8) |
88.2 (27.0) |
| BMI kg/m2 |
29.2 (7.28) |
28.2 (6.78) |
28.6 (6.81) |
37.4 (39.8) |
30.5 (8.40) |
32.0 (19.8) |
| Obesity (BMI ≥ 30 kg/m2) |
18.18% (8) |
21.85% (33) |
22.38% (41) |
15.90% (7) |
19.86% (30) |
18.40% (37) |
| Type 2 diabetes mellitus |
9.09% (4) |
8.60% (13) |
8.95% (17) |
9.09% (4) |
7.28% (11) |
7.46% (15) |
| MetALD |
22.72% (10) |
28.47% (43) |
28.3% (53) |
15.90% (7) |
21.85% (33) |
19.9% (40) |
| AST U/L |
187 (120) |
243 (222) |
226 (200) |
183 (77.2) |
203 (108) |
199 (102) |
| ALT U/L |
69 (76.3) |
58.5 (43.3) |
60.2 (51.7) |
63.4 (41.1) |
57.7 (34.2) |
58.9 (35.6) |
| Total bilirubin mg/dL |
14.2 (10.1) |
17.2 (10.2) |
16.2 (10.4) |
23.5 (12.9) |
21.1 (11.7) |
21.7 (11.9) |
| Albumin g/dL |
2.79 (0.476) |
2.76 (0.523) |
2.79 (0.532) |
2.65 (0.695) |
2.48 (0.422) |
2.51 (0.494) |
| PT sec |
20.5 (3.25) |
21.3 (5.66) |
20.9 (5.25) |
22.8 (5.61) |
24.8 (6.40) |
24.4 (6.26) |
| INR |
1.78 (0.363) |
1.85 (0.640) |
1.81 (0.588) |
2.03 (0.578) |
2.26 (0.777) |
2.21 (0.741) |
| Creatinine mg/dL |
0.753 (0.415) |
0.968 (0.632) |
0.927 (0.584) |
1.07 (0.478) |
1.39 (1.02) |
1.32 (0.934) |
| DF (using PT 13.5) |
46.6 (19.5) |
52.9 (27.4) |
50.2 (26.9) (19.5) |
66.5 (32.2) |
73.2 (31.8) |
71.7 (31.8) |
| MELD (admission) |
21.7 (5.74) |
22.5 (7.35) |
22.1 (7.03) |
27.2 (5.95) |
28.3 (7.58) |
28.1 (7.24) |
| MELD (discharge) |
30.0 (39.3) |
23.4 (5.62) |
24.8 (19.7) |
27.8 (7.99) |
28.8 (6.31) |
28.6 (6.67) |
AA African American, W white, BMI body mass index, MetALD metabolic dysfunction associated alcoholic liver disease, AST aspartate aminotransferase, ALT alanine aminotransferase, PT prothrombin time, INR international normalized ratio, MDF maddrey discriminatory function, MELD model for end stage liver disease
aData presented as number (n), mean (± SD), or %
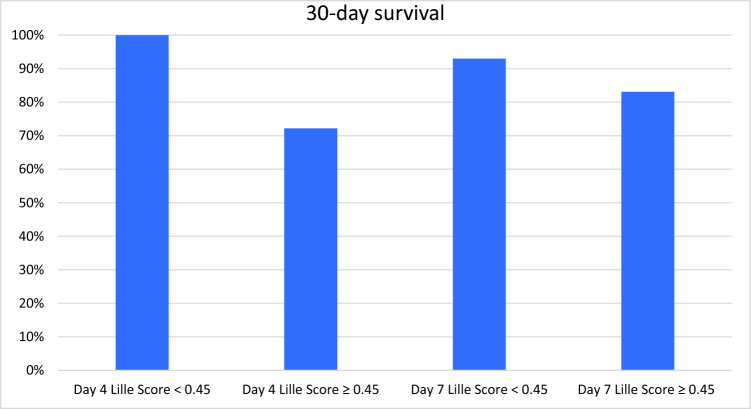
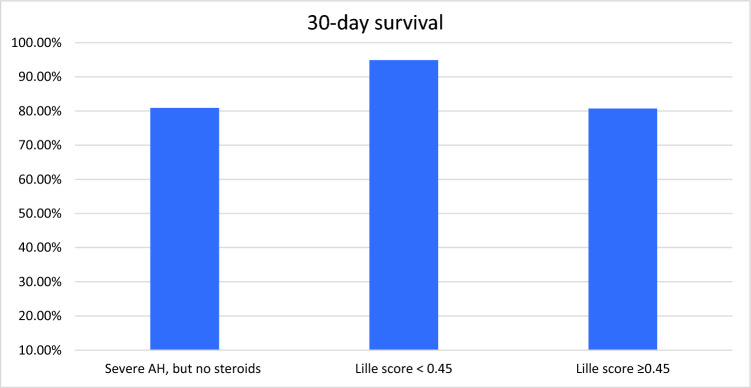
When looking at differences in demographics and clinical characteristics by Lille score at day 4, those with Lille score < 0.45 were younger (mean age 43 vs. 53; p = 0.003), had lower TB (14 mg/dL vs. 24 mg/dL; p = 0.015), Cr (0.8 mg/dL vs. 1.1 mg/dL; p = 0.032), MDF (46.6 vs. 66.5; p = 0.014) and MELD on admission (22 vs. 27; p = 0.005) (Table 2). Patients that had MetALD were more likely to have a lower Lille score (OR 3.14; 95% confidence interval 1.03–1.067; p = 0.025). However, having MetALD had no impact on 30-day survival (p = 0.42). Those with Lille < 0.45 at day 4 also achieved better 30-day survival (100% vs. 72.2%; p = 0.002) shown in Fig. 2. However, there were no differences in demographics, weight, AST, ALT, INR, PT, albumin, or MELD at discharge. In those with Lille score assessed at day 7, those with Lille score < 0.45 were younger (mean age 42 vs. 48; p = 0.002), had lower TB (17 mg/dL vs. 21 mg/dL; p = 0.032), INR (1.9 vs. 2.3; p = 0.001), Cr (0.97 vs. 1.39; p = 0.002), MDF (53 vs. 73; p = 0.001), MELD on admission (23 vs. 28; p = 0.001) and MELD at discharge (23 vs. 29; p = 0.001) (Table 2). When compared to those with Lille ≥ 0.45 at day 7, those with Lille < 0.45 at day 7 also had higher albumin (2.76 g/dL vs. 2.48 g/dL; p = 0.001) and higher 30-day survival (93% vs. 83%; p = 0.002) (Fig. 2). As a comparison, 30-day survival was also computed for the cohort of 110 patients with severe AH whom did not receive steroids as shown in Fig. 3. This cohort, despite not receiving steroids, had a 30-day survival of 80.9% that was similar to those that were non-responders to steroids (Lille ≥ 0.45) at 80.72%
Fig. 2.
30-day survival comparison based off Lille score day of calculation and scores of < 0.45 vs. ≥ 0.45
Fig. 3.
30-day survival for those with severe AH, but whom did not receive steroids vs. combined Lille score < 0.45 and combined Lille score ≥ 0.45
Table 2 shows the utility of the Lille score when it is used to predict 30-day survival. The sensitivity of the Lille score was found to be 95% in our cohort with a specificity of 19%. The PPV and NPV of Lille < 0.45 was found to be 63% and 73%, respectively. Odds ratio to calculate survival was also computed, and found to be 0.226 for the steroid-treated group compared to those who did not receive steroids, with a 95% confidence interval of 0.069 to 0.645.
Discussion
The Lille score was first created to assess the futility of steroids in those with severe AH [3]. While it remains a widely used method to determine steroid responsiveness, its effects on 30-day survival with improvements in overall care in AH are not well established. In this study, we found that the sensitivity of the Lille score to predict 30-day survival was excellent, but it did possess poor specificity with only moderate PPV and NPV. Our study showed a similar but increased rate of survival among steroid responders when compared to prior reports [1, 8]. However, we also found that survival was higher than prior reports and similar among those who were steroid non-responders to those who were eligible based on MELD and/or MDF but did not receive steroids [5].
There was an insignificant trend in 30-day survival for those with severe AH that did not receive steroids when compared to those with severe AH that did receive steroids (p = 0.058). Our observations support those of prior studies that steroids are associated with improved 30-day survival that did not reach statistical significance [1]. However, it should also be noted that the p-value in this situation is only marginally insignificant with using an alpha significance level of 0.05. This may indicate that steroids are useful for some patients, but are not currently generalizable to the population level for standard of care treatment for factors that are not yet known about the disease and treatment of this condition.
Historically, MDF has been the most widely used tool to define severity and short term-mortality in AH. However, it has prognostic limitations and has been proven to be inferior to MELD in recent studies [3, 4]. The inferiority of MDF is at least in part due to the omission of creatinine, which is an important prognostic marker in this population [3, 4]. Additionally, scores such as the Age-Bilirubin-International Normalized Ratio-Creatinine score (ABIC) and Glasgow Alcoholic Hepatitis Scores (GAHS) incorporate age as a variable, a proven independent predictor of mortality in the AH population [9, 10]. ABIC, GAHS, and MELD have all been proven to outperform MDF in predicting short term 28-day mortality [9, 11, 12]. However, all these scores have been found to be inferior when used alone as static scores and not with a dynamic score such as the Lille score [9]. This is likely because early improvement in liver function is known to decrease short-term mortality, implying a reassessment of lab values after a short treatment duration may be of benefit. This was observed in our cohort as those with Lille score < 0.45 at day 4, signifying earlier improvements in laboratory parameters, had excellent 30-day survival (100%).
Although it is implied by its dynamic assessment of steroid response to be effective, the Lille score’s lack of specificity shows the need for more specific tests to predict survival. One possible improvement to increase the Lille score’s specificity in predicting short-term mortality would be to have both age and Cr have larger numerical product values in the calculation, as they are known variables to affect mortality. Additionally, MELD and Lille in combination may need to become the standard of care to assess mortality in this population as it has been shown to have the highest prognostic utility [9].
Our study found that those with AH and Lille scores < 0.45 receiving steroids had significantly higher 30-day survival compared to those with a Lille score ≥ 0.45. Thus, the Lille score does show use in its ability to discriminate between steroid responders and steroid non-responders. We also show in our study that while a good Lille score at day 4 had 100% 30-day survival, there is comparable survival when using Lille score either at day 4 or day 7. To improve specificity and increase the Lille score’s ability to predict 30-day survival at day 7, future studies can determine if a decreased Lille score threshold to define steroid responsiveness and thereby continue treatment would be superior to the current threshold. For example, some studies have defined complete responders to steroids as those with Lille score’s ≤ 0.16 [13]. This cutoff would substantially decrease the number of patients that were continued on steroids and thereby were prone to infections. However, this would come with the acceptance of an overall lower sensitivity. Moreover, it could be argued that receiving less steroids would decrease rates of corticosteroid complications and thereby improve mortality. This is a valid argument, and one that would need to be investigated in future studies. Those whom were responders to steroids were also found to have lower MDF and MELD as shown in Table 1. This implies that those with less severe AH are more likely to respond to steroids. This suggests a potential unique population to target for steroid therapy.
This retrospective study has several limitations. The diagnosis of patients with AH was based on the discretion of the treating medical team and not always on NIAAA standard criteria [7]. Furthermore, the decision to use day 4 or day 7 Lille score to discontinue steroids was also at the discretion of the treating team which included a hepatologist. In addition, to calculate Lille score, values were taken at either day 4 or 7 which adds less uniformity to the sample. Nonetheless, we did show in our study that day 4 and day 7 Lille scores (in those with Lille < 0.45), had similar survival. Due to the retrospective study design, we cannot say what control PT was used to calculate MDF. However, the choice of control PT used in calculating MDF has not been shown to make a difference [3]. In addition, use of steroids was not limited to a specific high MELD threshold [14]. Therefore, our data may not be generalizable to all hospitalized patients with severe AH. Our analysis did not include patients with history of liver transplant or evaluate whether liver transplantation was being considered. This is important to consider, as recent studies have found that up to 58% of patients with severe AH fail to respond to steroids, and steroids should try and be avoided if liver transplant is being considered [15].
Of the 511 patients excluded, we did not delineate how many patients were excluded for non-severe AH. In those with severe AH that did not receive steroids, we did not analyze what specific contraindications existed for each patient. We found that those whom were steroid non-responders had higher BMI, which may suggest that Metabolic dysfunction-associated steatotic liver disease (MASLD) was a confounding variable in steroid non-responders. Additionally, through separate analysis, we found that MetALD impacted Lille score but not 30-day survival. Lastly, an analysis to detect optimal cutoffs of Lille score to predict 30-day survival by way of receiver operating curve (ROC) was not possible given this was an uncontrolled and retrospective analysis.
In summary, our study was performed to assess the utility of Lille score alone in predicting 30-day survival in AH. While survival was significantly different between Lille scores < 0.45 and ≥ 0.45, both groups achieved higher rates of survival when compared to prior studies despite having severe AH. We confirm as has been shown in prior studies that day 4 Lille score has comparable efficacy in defining steroid responsiveness to day 7. However, medical therapy outside of steroids are lacking and future studies into more effective treatment options are needed in this population. While Lille score had good sensitivity in predicting 30-day survival, its specificity was poor. Therefore, future studies will need to be performed to determine what is the best method to elucidate survival in this population.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgments
We would like to thank and acknowledge the patients in this study, for this work would not be possible without them
Author's contribution
-Dr. Marcus A. Healey, DO, MS: Primary roles of data collection, hypothesis creation, manuscript writing -Dr. Geetha Ramalingam, MBBS: primary roles of data collection, statistical analysis -Yiwei Hang: primary role of data collection -Dr. Ekaterina Smirnova, PhD, M.S: primary role of statistical analysis -Dr. Amon Asgharpour, MD: primary role of patient care -Dr. Vaishali Patel, MD: primary role of patient care -Dr. Hannah Lee, MD: primary role of patient care -Dr. Velimir Luketic, MD: primary role of patient care -Dr. Scott Matherly, MD: primary role of patient care -Dr. Mohammad Siddiqui, MD: primary role of patient care -Dr. Joel Wedd, MD: primary role of patient care -Dr. Arun Sanyal, MD: primary role of patient care -Dr. Richard Sterling, MD: primary role of patient care
Data availability
No datasets were generated or analysed during the current study
Declarations
Conflict of interest
All the authors have no conflicts of interest to disclose in the creation of this study. No grant support was used in the creation of this study. No financial interests related to this manuscript were used.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Thursz MR, Richardson P, Allison M et al. STOPAH Trial: prednisolone or pentoxifylline for alcoholic hepatitis. N Engl J Med. 2015;372:1619–1628. 10.1056/NEJMoa1412278 [DOI] [PubMed] [Google Scholar]
- 2.Maddrey WC, Boitnott JK, Bedine MS, Weber FL Jr, Mezey E, White RI Jr. Corticosteroid therapy of alcoholic hepatitis. Gastroenterology 1978;75:193–199. 10.1016/0016-5085(78)90401-8 [DOI] [PubMed] [Google Scholar]
- 3.Healey M, Sterling RK. Outnumbered: control prothrombin time in Maddrey’s discriminant function impacts steroid use but not mortality in alcoholic hepatitis. Biology 2022;11:1833. 10.3390/biology11121833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morales-Arráez D, Ventura-Cots M, Altamirano J et al. The MELD score is superior to the Maddrey discriminant function score to predict short-term mortality in alcohol-associated hepatitis: a global study. Am J Gastroenterol. 2022;117:301–310. 10.14309/ajg.0000000000001596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Louvet A, Naveau S, Abdelnour M et al. The Lille model: a new tool for therapeutic strategy in patients with severe alcoholic hepatitis treated with steroids. Hepatology. 2007;45:1348–1354. 10.1002/hep.21607 [DOI] [PubMed] [Google Scholar]
- 6.Foncea CG, Sporea I, Lupușoru R et al. Day-4 lille score is a good prognostic factor and early predictor in assessing therapy response in patients with liver cirrhosis and severe alcoholic hepatitis. J Clin Med. 2021;10:2338. 10.3390/jcm10112338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Crabb DW, Bataller R, Chalasani NP et al. NIAAA Alcoholic hepatitis consortia standard definitions and common data elements for clinical trials in patients with alcoholic hepatitis: recommendation from the NIAAA alcoholic hepatitis consortia. Gastroenterology. 2016;150:785–790. 10.1053/j.gastro.2016.02.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hughes E, Hopkins LJ, Parker R. Survival from alcoholic hepatitis has not improved over time. PLoS ONE. 2018;13:e0192393. 10.1371/journal.pone.0192393. 10.1371/journal.pone.0192393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Louvet A, Labreuche J, Artru F et al. Combining data from liver disease scoring systems better predicts outcomes of patients with alcoholic hepatitis. Gastroenterology. 2015;149:398–406. 10.1053/j.gastro.2015.04.044 [DOI] [PubMed] [Google Scholar]
- 10.Kamath PS, Therneau T, Shah VH. MELDing the lille score to more accurately predict mortality in alcoholic hepatitis. Gastroenterology. 2015;149:281–283. 10.1053/j.gastro.2015.06.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Forrest EH, Evans CD, Stewart S et al. Analysis of factors predictive of mortality in alcoholic hepatitis and derivation and validation of the Glasgow alcoholic hepatitis score. Gut 2005;54:1174–1179. 10.1136/gut.2004.050781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Božin T, Rob Z, Lucijanić M, Čmarec Buhin L, Grgurević I. Comparison of prognostic scores for alcoholic hepatitis: a retrospective study. Croat Med J. 2021;62:17–24. 10.3325/cmj.2021.62.17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sarin SK, Sharma S. Predictors of steroid non-response and new approaches in severe alcoholic hepatitis. Clin Mol Hepatol. 2020;26:639–651. 10.3350/cmh.2020.0196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arab JP, Díaz LA, Baeza N et al. Identification of optimal therapeutic window for steroid use in severe alcohol-associated hepatitis: a worldwide study. J Hepatol. 2021;75:1026–1033. 10.1016/j.jhep.2021.06.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Asgharpour A, Sterling RK, Smirnova E et al. Early liver transplantation for severe alcohol-associated hepatitis: a single-center experience. J Liver Transplant 2023;12:100184. 10.1016/j.liver.2023.100184 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study