Abstract
Background
Previous systematic reviews have failed to find an association between the use of real-time feedback during cardiopulmonary resuscitation (CPR) and patient outcomes. However, these reviews excluded studies examining feedback with other system changes. As part of the International Liaison Committee on Resuscitation (ILCOR) continuous evidence evaluation process, we conducted a scoping review to examine the current state of this literature and the use of real-time feedback in this form.
Methods/Data sources
A protocol and search strategy was developed. We searched Medline, EMBASE, and Allied Health Literature (CINAHL) from inception to May 2024. Cochrane (Cochrane (specifically, the Cochrane Database of Systematic Reviews) is contained in Medline so was not searched separately. Studies were eligible for inclusion if they were published or unpublished (grey-literature) studies involving children or adults that examined the effect of real-time feedback or prompting on the quality of CPR following cardiac arrest. Data were extracted and audited independently. For each study, the following information were extracted: the author(s); year of publication; timeframe; study design; country; population; intervention and comparator; type of feedback or prompt; outcomes measured; main findings for CPR quality, and; main findings for patient outcomes. Reviewers also allocated key themes to each study and held a series of consensus discussions to consolidate themes across the included studies.
Results
We screened 2,657 titles and included 60 studies. Our analysis identified five overlapping themes in the extended literature: system change and quality improvement; impact on patient outcomes; better CPR quality without improved patient outcome; CPR feedback as a generator of other CPR metrics; and CPR feedback as a potential harm. Results revealed a substantial adjacent literature, particularly on implementing high-performance CPR as part of quality improvement programs.
Conclusions
This scoping review has identified a large body of literature and specific themes of interest in relation to feedback for CPR quality. Future systematic reviews should include studies examining real-time feedback with other system changes.
Keywords: Cardiopulmonary resuscitation, Real-time CPR feedback, CPR feedback devices, Scoping review
Introduction
The quality of cardiopulmonary resuscitation (CPR) has direct impacts on survival and neurological outcomes for patients who have a cardiac arrest.1 Despite extensive studies and numerous quality improvement projects, the quality of CPR has remained a significant issue in both out-of-hospital and in-hospital settings. Previous studies have identified challenges of consistently performing high-quality CPR even among highly trained healthcare professionals.2
Real-time CPR feedback has been studied as a potential method not only to improve the quality of CPR but also survival and neurological outcomes of victims of cardiac arrest. However, the results of the studies have been mixed and implementation of real-time CPR feedback in the clinical setting is somewhat limited globally.3 The 2020 recommendation of the International Liaison Committee on Resuscitation (ILCOR) in relation to the use of real-time feedback for CPR quality (BLS361) was as following: “We suggest the use of real-time audiovisual feedback and prompt devices during CPR in clinical practice as part of a comprehensive quality improvement program for cardiac arrest designed to ensure high-quality CPR delivery and resuscitation care across resuscitation systems (weak recommendation, very-low-certainty evidence). We suggest against the use of real-time audiovisual feedback and prompt devices in isolation (i.e. not part of a comprehensive quality improvement program) (weak recommendation, very-low-certainty evidence).”3 The 2020 systematic review did not exclude based on the user of real-time CPR feedback, therefore studies where laypersons were users were potentially included. Additionally, articles related to the system change and quality improvement initiatives were excluded.
To explore the impact of this evidence and address this gap, as part of the International Liaison Committee on Resuscitation (ILCOR) continuous evidence evaluation process, the Basic Life Support (BLS) Task Force decided to conduct a scoping review to examine the current state of this literature, including this broader adjacent literature, on the use of real-time feedback.
Methods
The scoping review followed the recommendations of the Preferred Reporting Items for Systematic review and Meta-Analysis (PRISMA) extension for scoping reviews.4 A six-stage methodological framework for scoping reviews was also adopted, which consisted of: identifying the research question, searching for relevant studies, selecting studies, charting the data, reporting the results, and consultation.5 The review protocol was not prospectively registered, but the review question and methodology was approved by the Basic Life Support Task Force before the commencement of the search.
Research question
In line with ILCOR’s process for evidence reviews, the research question was structured in the ‘PICOST’ (Population, Intervention, Comparison, Outcome, Study Design, Timeframe) format as follows:
-
•
Population: Adults and children (excluding neonates) in any setting (in-hospital or out-of-hospital) with cardiac arrest who are resuscitated by health professionals responding in a professional capacity.
-
•
Intervention: Real-time feedback or prompt devices for CPR quality (e.g. rate and depth of compressions and/or ventilations).
-
•
Comparators: No real-time feedback and prompt devices or alternative real-time feedback and prompt devices.
-
•
Outcomes: Any patient outcome or measure of CPR quality.
-
•
Study Designs: Randomized controlled trials (RCTs) and non-randomized studies (non-randomized controlled trials, interrupted time series, controlled before-and-after studies, cohort studies) are eligible for inclusion. Case series were included in the initial search. Grey literature and non-peer reviewed studies, unpublished studies, conference abstracts and trial protocols were eligible for inclusion. All relevant publications in any language are included if there was an English abstract. Animal and simulation studies were excluded.
-
•
Timeframe: From database inception to 31st May 2024.
Eligibility criteria
In this review, we considered real-time feedback or prompting of CPR quality to include any form of feedback from humans or device/technology involving audio or visual prompts during the course of a resuscitation. Metronomes were considered ‘prompt’ devices and were included in this definition. In addition, we included articles that examined real-time coaching or verbal instructions during resuscitation. This scoping review was limited to studies involving healthcare professionals as the users of real-time feedback as it was felt that laypersons as users might dilute the true effect of real-time CPR feedback devices and make it difficult to examine its effectiveness. Additionally, literature related to the system change and quality improvement initiatives was specifically included in this scoping review.
Data sources
A comprehensive search strategy was developed with input from an information specialist. Articles for review were obtained by searching PubMed, EMBASE, Cochrane, and Allied Health Literature (CINAHL), for all entries from database inception to 31st May 2024. A grey literature search was also performed in the Google search engine. Articles were identified using the following key terms for real-time feedback and prompting: “feedback”, “feed-back”, “feed back”, “CPR-sensing”, “Q-CPR”, “CPR-plus”, “CPREzy”, “CPR-Ezy”, “high performance cardiopulmonary resuscitation”, “high performance resuscitation”, “prompt*”, “sensor*”, “metronome”, “real time”, “realtime”, “resuscitat*”. Where appropriate, we included MESH terms and Embase exploded terms. A detailed search strategy including all search terms is shown in supplementary appendix. Grey literature searching using the google search engine adopted similar search terms. We also searched the reference lists of identified studies to identify relevant articles that may have been missed.
Study selection
Studies meeting the search criteria across databases were exported and reviewed in Nested Knowledge. Two reviewers independently screened all titles and abstracts for relevance. A third review independently adjudicated any conflicts. Relevant titles then underwent full-text review by two reviewers, independently, for eligibility criteria. A third reviewer resolved any conflicts in decisions. During full-text review, simulation studies, commentaries and opinion pieces that did not cite references related to real-time CPR feedback were excluded. In addition, poster abstracts were excluded if the data presented was subsequently published in a full report. Reference lists in relevant systematic reviews were also screened to identify any articles that may have been missed. Finally, articles relating to the use of real-time feedback during resuscitation of neonates were excluded as the ILCOR Neonatal Life Support Task Force completed a scoping review of the same topic in January 2023.6
Data extraction, charting and consultation
Articles meeting eligible criteria underwent data extraction. Data were extracted independently by three reviewers (SM, TN, TK) and then audited by another (ZN). For each study, the following information were extracted: the author(s); year of publication; timeframe; study design; country; population; intervention and comparator; type of feedback or prompt; outcomes measured; main findings for CPR quality, and; main findings for patient outcomes. In order to pilot the data extraction tool, SM, TN and TK independently reviewed ten articles each, then met to compare extraction results. Based on this meeting, explanatory notes were added to each extraction field to ensure consistency in the terminology used in the data extraction process. Disagreements were resolved by discussion. Reviewers also allocated key themes to each study and held a series of consensus discussions to consolidate themes across the included studies. Extracted information was presented in tabular format for each study individually and then aggregated by major study characteristics. Tables were accompanied by a narrative of results identifying key themes. The results of the scoping review were shared with the ILCOR BLS Task Force and made available for public consultation and feedback on the ILCOR website. A formal appraisal of study quality was not undertaken.7
Results
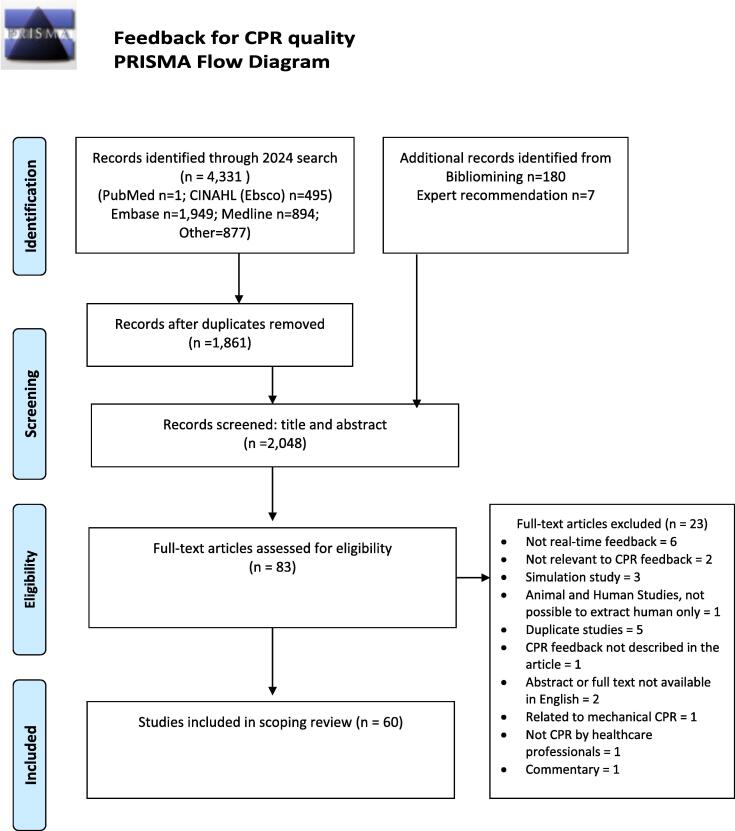
In total, 4,518 articles were identified. After de-duplication, the total number of articles screened was 2,657. A total of 83 articles underwent full-text review. Twenty-three articles were excluded at this stage and 60 articles were included in the final review (see Fig. 1). Details of all articles included are presented in the Supplemental Table.
Fig. 1.
PRISMA Flow Diagram.
As shown in Table 1, of the 60 studies included, there were six randomized controlled trials,8, 9, 10, 11, 12, 13 eleven systematic reviews,14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24 41 observational studies,25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63 and two case series.64, 65 Five themes were identified in the 60 studies: system change & quality improvement; impact on patient outcomes; better CPR quality without improved patient outcome; CPR feedback as a generator of other CPR metrics; and CPR feedback as a potential harm. All articles included a description of the setting in which the study took place. Ten articles included both OHCA and IHCA,14, 15, 16, 20, 21, 22, 23, 24, 46 24 investigated OHCA only,8, 10, 11, 17, 19, 26, 28, 33, 34, 35, 37, 38, 39, 41, 44, 47, 48, 50, 51, 52, 54, 55, 61, 62 and 26 investigated IHCA only.9, 12, 13, 18, 25, 27, 29, 30, 31, 32, 36, 40, 42, 43, 45, 49, 53, 56, 57, 58, 59, 60, 63, 65, 66, 67
Table 1.
Summary of study characteristics.
| All Studies | Population of Interest |
|||
|---|---|---|---|---|
| All | Adults Only | Paediatric Only | ||
| Total number of studies, n | 60 | 14 | 41 | 5 |
| Cumulative feedback-CPR patients, n* | 55,889 | 1,379 | 54,376 | 134 |
| Year of publication, n (%) | ||||
| Before 2000 | 2 (3) | 0 | 1 (2) | 1 (20) |
| 2000–2009 | 8 (13) | 2 (14) | 5 (12) | 1 (20) |
| 2010–2019 | 26 (43) | 6 (43) | 17 (43) | 3 (60) |
| 2020+ | 24 (40) | 6 (43) | 17 (43) | 0 |
| Study Design, n (%) | ||||
| Randomised controlled trial | 6 (10) | 0 | 6 (15) | 0 |
| Observational study | 42 (70) | 7 (50) | 30 (73) | 5 (100) |
| Systematic review/meta-analysis | 11 (18) | 7 (50) | 4 (10) | 0 |
| Others | 1 (2) | 0 | 1 (2) | 0 |
| Feedback type, n (%) | ||||
| CC – audio & visual | 40 (67) | 6 (43) | 30 (73) | 4 (80) |
| CC – audio | 8 (13) | 3 (21) | 4 (10) | 1 (20) |
| CC – visual | 1 (2) | 0 | 1 (2) | 0 |
| Others | 11 (18) | 5 (36) | 6 (15) | 0 |
| Region, n (%) | ||||
| North America | 20 (33) | 4 (29) | 12 (30) | 4 (80) |
| Europe | 13 (22) | 1 (7) | 11 (28) | 1 (20) |
| Asia | 13 (22) | 1 (7) | 12 (30) | 0 |
| Africa | 0 | |||
| Australia and New Zealand | 3 (15) | 0 | 3 (25) | 0 |
| Multicontinental | 9 (15) | 6 (43) | 2 (5) | 1 (17) |
| OHCA vs IHCA, n (%) | ||||
| All CA | 12 (20) | 8 (57) | 4 (10) | 0 |
| OHCA | 30 (50) | 4 (29) | 24 (59) | 2 (40) |
| IHCA | 18 (30) | 2 (14) | 13 (32) | 3 (60) |
| Reported outcome, n (%) | ||||
| Patient and Process outcome | 26 (43) | 6 (43) | 19 (46) | 1 (20) |
| Only patient outcome | 13 (22) | 4 (29) | 9 (22) | 0 |
| Only process outcome | 21 (35) | 4 (29) | 13 (32) | 4 (80) |
| Themes Identified, n (%) | ||||
| System change/quality improvement | 16 (27) | 5 (36) | 11 (28) | |
| Impact on patient outcomes | 14 (23) | 3 (21) | 11 (28) | |
| Better CPR quality without improved patient outcomes | 26 (43) | 6 (50) | 16 (40) | 5 (100) |
| CPR feedback as a generator of other CPR metrics | 3 (5) | 1 (7) | 2 (5) | |
| CPR feedback as a potential harm | 1 (2) | 0 | 1 (3) | |
Abbreviations: CA = Cardiac Arrest; CC = Chest Compressions; CPR = Cardiopulmonary resuscitation; IHCA = In-hospital Cardiac Arrest; OHCA = Out-of-hospital Cardiac Arrest.
Excluded all systematic reviews/meta-analysis when counting the number of patients.
As described above, the vast majority of studies that described some aspect of real-time feedback for CPR were observational (n = 41). Nineteen studies reported an improvement in some aspect of CPR quality but did not report a consequent improvement in patient outcomes.11, 21, 25, 27, 36, 40, 41, 42, 44, 45, 48, 49, 51, 52, 57, 58, 59, 60, 61, 63, 66 Six studies investigated the impact of real-time feedback in out-of-hospital settings.11, 47, 50, 52, 54, 62 With the exception of a statistically significant improvement in ROSC rates in two studies,11, 62 improved patient outcomes were not reported. One study investigating the impact of a CPR coach giving corrective verbal feedback in pediatric IHCA and found an improvement in ROSC rates in centers with a CPR coach.56
System change/quality improvement
Of the eleven systematic reviews identified, three meta-analyses investigated the impact of ‘system performance improvement’, ‘implementation of high performance CPR’ and ‘quality improvement systems’.15, 19, 20 Thirteen primary studies described real-time feedback as part of overall system improvements.26, 28, 29, 30, 31, 32, 33, 34, 35, 37, 38, 39, 55 Of the seven studies that described CPR quality, all reported that at least some aspects of CPR quality had improved as a result of the intervention. Results on the impact on patient outcomes were more mixed, but the majority of the thirteen studies reported some degree of positive impact on patient outcomes.
Impact on patient outcomes
One systematic review that examined the impact of real-time feedback on training and CPR performance found that feedback improved CPR quality but no direct impact on survival to discharge rates.24 Six other systematic reviews investigated the effect of real-time feedback on patient outcomes. Kirkbright (2014) also included manikin studies but reported human studies separately.14 For three human studies, they found no significant improvement in patient outcomes, but significant improvements in chest compression rate, depth, and no-flow fraction. In OHCA patients, Lyngby (2021) found that real-time feedback improved chest compression depth and rate but did not statistically improve patient outcomes.17 Pooled analysis by Lv (2022) found that real-time feedback did not improve ROSC, was associated with improved survival to discharge but not with good neurological outcome at discharge.16 A similar review by Wang (2020) found that improved survival to discharge was found only in studies where the Cardio First Angel device was used.23 Miller (2020) found that ‘free-standing non-AED AV feedback devices’ were associated with improved outcomes.18 Finally, Sood (2023) performed a meta-analysis and reported that the real time audiovisual feedback group were significantly more likely to achieve ROSC with a higher likelihood in the in-hospital setting, but with no significant improvement in survival to discharge.21
One study, using the Cardio First Angel (CFA),9 conducted with patients admitted to ICU from the ED found that patient outcomes were significantly improved in the CFA group: (66.7% vs. 42.4%, P < 0.001); survival to ICU discharge (59.8% vs. 33.6%); survival to hospital discharge (54% vs. 28.4%, P < 0.001). Similarly, Vahedin-Azimi (2016) found that real-time AV feedback improved CPR quality and outcomes for patients in ICUs (ROSC was observed more frequently in the intervention group (72% vs. 35%; p = 0.001)).13
Better CPR quality without improved patient outcomes
Twelve primary studies that examined both chest compression quality and patient outcomes reported that real-time feedback on chest compression quality did not significantly improve patient outcomes.8, 10, 25, 40, 41, 42, 48, 49, 51, 59, 63, 65
CPR feedback as a generator of other CPR metrics
Two studies under this theme used CPR feedback to measure leaning force during CPR and concluded that feedback reduced leaning force. Neither study included patient outcome data.
CPR feedback as a potential harm
This study described two case deceased patients and the visible damage to the chest wall that appeared to have been caused by the feedback device.64
Discussion
This scoping review exploring the impact of real-time feedback for cardiopulmonary resuscitation (CPR) quality on patient outcomes identified 60 studies that have been categorised into five themes with overlaps: system changes/quality improvement, impact on patient outcomes, better CPR quality without improved patient outcomes, CPR feedback as a generator of other CPR metrics, and CPR feedback as a potential harm. Of 60 studies, 6 were RCTs, 11 were systematic reviews, 41 were observational studies, and two were case series.
The previous 2015 and 2020 ILCOR Systematic Reviews (BLS361: SysRev) did not restrict the search strategy based on who performed CPR. However, while the population of interest in the current scoping review was limited to CPR performed by ‘health professionals responding in a professional capacity’, only studies where CPR was performed by health professionals were ultimately included in the 2015 and 2020 systematic review syntheses. Therefore, the upshot is that both the results of the current scoping review and the systematic review cover the same population of interest.
The 2015 and 2020 systematic reviews specifically excluded studies where real-time CPR feedback technology was used with system wide quality improvement initiatives, or only presented the real-time CPR feedback components of such studies. The current scoping review included 60 studies in the final synthesis, compared to 16 studies in the 2020 systematic review (and 11 in the 2015 systematic review). Sixteen of the new studies included in the current scoping review were related to system change/quality improvement. While a scoping review is, by definition, a broad reflection of the literature associated with a topic, it is clear there is a substantial adjacent literature on implementing high performance CPR/Quality Improvement programs which include a real-time CPR feedback component. Our findings suggest a need for critical appraisal of this particular body of literature to determine whether impact on patient outcomes can be ascertained.
The majority of studies suggest that real-time a positive association between CPR feedback and CPR quality. However, in common with the 2015 and 2020 systematic reviews, this association was often not directly aligned with a commensurate improvement in patient outcomes. The vast majority of studies included were observational in nature, meaning it is difficult to account for the impact of confounding and selection bias in these studies. Since the 2020 systematic review, the current scoping review identified an additional 16 studies that investigated the impact of CPR feedback on CPR quality and patient outcomes. While the quality of articles was not assessed as part of this scoping review, the volume of literature included in the results synthesis of the current scoping review illustrates how the body of evidence on this topic has increased, particularly since the last ILCOR Systematic review.
Studies relating to the impact of feedback for CPR quality on paediatric patients was limited when compared to adult patients This means that the impact of CPR feedback technology in the paediatric field is relatively under-researched and even less understood for this patient cohort.
It is of note that the RCTs conducted in specific in-hospital settings showed a more promising association between real-time feedback devices and patient outcomes, suggesting that setting may be a significant factor in determining the impact of real-time feedback. There was a small quantity of literature describing alternative and more invasive methods of measuring CPR quality. While there was insufficient literature to warrant a systematic review of this topic, it may be worth reconsidering this as these technologies advance and become more prevalent.
There are limitations to these results. Of particular note is that, as is normal for a scoping review, no assessment of literature quality has been performed, therefore it is not possible to draw practice-related conclusions from these results. However, the breadth of this scoping review has uncovered new and adjacent literature relating to the impact of real-time feedback on CPR quality and patient outcomes, which will inform formulation of future systematic review plans. It is also important to note that, in the absence of quality appraisal and meta-analysis, the themes identified by the authors are indicative and not definitive.
Conclusions
This scoping review has revealed a substantial body of literature related to the impact of real-time CPR feedback on CPR quality and patient outcomes, including a range of systematic reviews covering different aspects of the impact of this technology. The range and themes covered by this literature have broadened since the previous 2020 ILCOR Systematic Review on this topic, particularly in the theme of quality improvement and system change. This signals the need for a revised and updated systematic review to inform ILCOR Guidelines.
ILCOR statement
This review includes information on resuscitation questions developed through the continuous evidence evaluation process, managed by the ILCOR. The questions were developed by ILCOR Task Forces, using strict conflict of interest guidelines. Evidence evaluations are discussed at ILCOR meetings to reach consensus and produce a final summary document.
Funding
This Scoping review was funded by the American Heart Association, on behalf of The International Liaison Committee on Resuscitation (ILCOR). None of the following authors received payment from this funding source to complete this scoping review.
CRediT authorship contribution statement
Siobhán Masterson: Writing – review & editing, Writing – original draft, Formal analysis, Conceptualization. Tatsuya Norii: Writing – review & editing, Writing – original draft, Methodology, Formal analysis, Conceptualization. Mio Yabuki: Writing – original draft. Takaya Ikeyama: Writing – review & editing, Writing – original draft, Formal analysis, Conceptualization. Ziad Nehme: Writing – review & editing, Formal analysis. Janet Bray: Writing – review & editing, Supervision, Formal analysis.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: ‘The ILCOR Continuous Evidence Evaluation process is guided by a rigorous ILCOR Conflict of Interest policy. The following Task Force members and other authors were recused from the discussion as they declared a conflict of interest: none applicable’.
Acknowledgement
The authors would like to thank the following International Liaison Committee on Resuscitation Basic Life Support Task Force members, associate members and emeritus members who provided input to the review protocol, interpretation of the results and on the manuscript as experts in resuscitation: Michael Smyth; Anthony Lagina; Baljit Singh; Bridget Dicker; Carolina Hansen; Christopher Smith; Fredrik Folke; Guillame Debatey; Katie Dainty; Maya Dewan; Nicholas Johnson; Rebecca Cash; Violetta Raffay; Aloka Samantaray; George Lukas and Vihara Dassanayake; Chika Nishiyama; Christian Vaillancort; Federico Semeraro; Giuseppe Ristagno; Sung Phil Chung and Tetsuo Hatanaka. Especial thanks are due to Emeritus Member Julie Considine for her guidance and input throughout. The authors also wish to thank the following members of the ILCOR Scientific Advisory Council for their review and guidance: Peter Morley, Theresa Olasveengen and Laurie Morrison. The authors would also like to thank Brendan Leen, Lead for Evidence, Health Service Executive, Ireland, who advised on and conducted the primary literature search.
Footnotes
Supplementary material to this article can be found online at https://doi.org/10.1016/j.resplu.2024.100730.
Appendix A. Supplementary material
The following are the Supplementary material to this article:
References
- 1.Talikowska M., Tohira H., Finn J. Cardiopulmonary resuscitation quality and patient survival outcome in cardiac arrest: a systematic review and meta-analysis. Resuscitation. 2015;96:66–77. doi: 10.1016/j.resuscitation.2015.07.036. [DOI] [PubMed] [Google Scholar]
- 2.Wik L., Kramer-Johansen J., Myklebust H., et al. Quality of cardiopulmonary resuscitation during out-of-hospital cardiac arrest. Jama. 2005;293:299–304. doi: 10.1001/jama.293.3.299. [DOI] [PubMed] [Google Scholar]
- 3.Olasveengen T.M., Mancini M.E., Perkins G.D., et al. Adult basic life support: international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation. 2020;156:A35–A79. doi: 10.1016/j.resuscitation.2020.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tricco A.C., Lillie E., Zarin W., et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Internal Med. 2018;169:467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 5.Arksey H., O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8 [Google Scholar]
- 6.Ramachandran S., Bruckner M., Wyckoff M.H., Schmölzer G.M. Chest compressions in newborn infants: a scoping review. Archiv Dis Childhood Fetal Neonatal Ed. 2023;108:442–450. doi: 10.1136/archdischild-2022-324529. [DOI] [PubMed] [Google Scholar]
- 7.Grant M.J., Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J. 2009;26:91–108. doi: 10.1111/j.1471-1842.2009.00848.x. [DOI] [PubMed] [Google Scholar]
- 8.Bohn A., Weber T.P., Wecker S., et al. The addition of voice prompts to audiovisual feedback and debriefing does not modify CPR quality or outcomes in out of hospital cardiac arrest–a prospective, randomized trial. Resuscitation. 2011;82:257–262. doi: 10.1016/j.resuscitation.2010.11.006. [DOI] [PubMed] [Google Scholar]
- 9.Goharani R., Vahedian-Azimi A., Farzanegan B., et al. Real-time compression feedback for patients with in-hospital cardiac arrest: a multi-center randomized controlled clinical trial. J Intensive Care. 2019;7:5. doi: 10.1186/s40560-019-0357-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hostler D., Everson-Stewart S., Rea T.D., et al. Effect of real-time feedback during cardiopulmonary resuscitation outside hospital: prospective, cluster-randomised trial. Bmj. 2011;342 doi: 10.1136/bmj.d512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee E.D., Jang Y.D., Kang J.H., et al. Effect of a real-time audio ventilation feedback device on the survival rate and outcomes of patients with out-of-hospital cardiac arrest: a prospective randomized controlled study. J Clin Med. 2023;12:6023. doi: 10.3390/jcm12186023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vahedian-Azimi A., Rahimibashar F., Miller A.C. A comparison of cardiopulmonary resuscitation with standard manual compressions versus compressions with real-time audiovisual feedback: a randomized controlled pilot study. Int J Crit Illn Inj Sci. 2020;10:32–37. doi: 10.4103/IJCIIS.IJCIIS_84_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vahedian-Azimi A., Hajiesmaeili M., Amirsavadkouhi A., et al. Effect of the Cardio First Angel™ device on CPR indices: a randomized controlled clinical trial. Crit Care. 2016;20:147. doi: 10.1186/s13054-016-1296-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kirkbright S., Finn J., Tohira H., Bremner A., Jacobs I., Celenza A. Audiovisual feedback device use by health care professionals during CPR: a systematic review and meta-analysis of randomised and non-randomised trials. Resuscitation. 2014;85:460–471. doi: 10.1016/j.resuscitation.2013.12.012. [DOI] [PubMed] [Google Scholar]
- 15.Ko Y.C., Hsieh M.J., Ma M.H., Bigham B., Bhanji F., Greif R. The effect of system performance improvement on patients with cardiac arrest: a systematic review. Resuscitation. 2020;157:156–165. doi: 10.1016/j.resuscitation.2020.10.024. [DOI] [PubMed] [Google Scholar]
- 16.Lv G.W., Hu Q.C., Zhang M., et al. Effect of real-time feedback on patient's outcomes and survival after cardiac arrest: A systematic review and meta-analysis. Medicine (Baltimore) 2022;101 doi: 10.1097/MD.0000000000030438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lyngby R.M., Händel M.N., Christensen A.M., et al. Effect of real-time and post-event feedback in out-of-hospital cardiac arrest attended by EMS – a systematic review and meta-analysis. Resusc Plus. 2021;6 doi: 10.1016/j.resplu.2021.100101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miller A.C., Scissum K., McConnell L., et al. Real-time audio-visual feedback with handheld nonautomated external defibrillator devices during cardiopulmonary resuscitation for in-hospital cardiac arrest: A meta-analysis. Int J Crit Illn Inj Sci. 2020;10:109–122. doi: 10.4103/IJCIIS.IJCIIS_155_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ng Q.X., Han M.X., Lim Y.L., Arulanandam S. A systematic review and meta-analysis of the implementation of high-performance cardiopulmonary resuscitation on out-of-hospital cardiac arrest outcomes. J Clin Med. 2021;10 doi: 10.3390/jcm10102098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schultz R., Bigham B., Bhanji F., E. L. Quality improvement systems for patient-important outcomes in resuscitation. Can J Emerg Med. 2015;17 [Google Scholar]
- 21.Sood N., Sangari A., Goyal A., et al. Do cardiopulmonary resuscitation real-time audiovisual feedback devices improve patient outcomes? A systematic review and meta-analysis. World J Cardiol. 2023;15:531. doi: 10.4330/wjc.v15.i10.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Targett C., Harris T. Towards evidence-based emergency medicine: best BETs from the Manchester Royal Infirmary. BET 3: Can metronomes improve CPR quality? Emerg Med J. 2014;31:251–254. doi: 10.1136/emermed-2014-203617.3. [DOI] [PubMed] [Google Scholar]
- 23.Wang S.A., Su C.P., Fan H.Y., Hou W.H., Chen Y.C. Effects of real-time feedback on cardiopulmonary resuscitation quality on outcomes in adult patients with cardiac arrest: a systematic review and meta-analysis. Resuscitation. 2020;155:82–90. doi: 10.1016/j.resuscitation.2020.07.024. [DOI] [PubMed] [Google Scholar]
- 24.Yeung J., Meeks R., Edelson D., Gao F., Soar J., Perkins G.D. The use of CPR feedback/prompt devices during training and CPR performance: a systematic review. Resuscitation. 2009;80:743–751. doi: 10.1016/j.resuscitation.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 25.Abella B.S., Edelson D.P., Kim S., et al. CPR quality improvement during in-hospital cardiac arrest using a real-time audiovisual feedback system. Resuscitation. 2007;73:54–61. doi: 10.1016/j.resuscitation.2006.10.027. [DOI] [PubMed] [Google Scholar]
- 26.Alqudah Z., Smith K., Stephenson M., Walker T., Stub D., Nehme Z. The impact of a high-performance cardiopulmonary resuscitation protocol on survival from out-of-hospital cardiac arrests witnessed by paramedics. Resusc Plus. 2022;12 doi: 10.1016/j.resplu.2022.100334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Berg R.A., Sanders A.B., Milander M., Tellez D., Liu P., Beyda D. Efficacy of audio-prompted rate guidance in improving resuscitator performance of cardiopulmonary resuscitation on children. Acad Emerg Med. 1994;1:35–40. [PubMed] [Google Scholar]
- 28.Bobrow B.J., Vadeboncoeur T.F., Stolz U., et al. The influence of scenario-based training and real-time audiovisual feedback on out-of-hospital cardiopulmonary resuscitation quality and survival from out-of-hospital cardiac arrest. Ann Emerg Med. 2013;62:47–56.e1. doi: 10.1016/j.annemergmed.2012.12.020. [DOI] [PubMed] [Google Scholar]
- 29.Couper K., Kimani P.K., Abella B.S., et al. The system-wide effect of real-time audiovisual feedback and postevent debriefing for in-hospital cardiac arrest: the cardiopulmonary resuscitation quality improvement initiative. Crit Care Med. 2015;43:2321–2331. doi: 10.1097/CCM.0000000000001202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Couper K., Mason A.J., Gould D., et al. The impact of resuscitation system factors on in-hospital cardiac arrest outcomes across UK hospitals: an observational study. Resuscitation. 2020;151:166–172. doi: 10.1016/j.resuscitation.2020.04.006. [DOI] [PubMed] [Google Scholar]
- 31.Crowe C., Bobrow B.J., Vadeboncoeur T.F., et al. Measuring and improving cardiopulmonary resuscitation quality inside the emergency department. Resuscitation. 2015;93:8–13. doi: 10.1016/j.resuscitation.2015.04.031. [DOI] [PubMed] [Google Scholar]
- 32.Davis D.P., Graham P.G., Husa R.D., et al. A performance improvement-based resuscitation programme reduces arrest incidence and increases survival from in-hospital cardiac arrest. Resuscitation. 2015;92:63–69. doi: 10.1016/j.resuscitation.2015.04.008. [DOI] [PubMed] [Google Scholar]
- 33.Fletcher D., Galloway R., Chamberlain D., Pateman J., Bryant G., Newcombe R.G. Basics in advanced life support: a role for download audit and metronomes. Resuscitation. 2008;78:127–134. doi: 10.1016/j.resuscitation.2008.03.003. [DOI] [PubMed] [Google Scholar]
- 34.Freese J., Menegus M., Rabrich J., et al. Addition of real-time CPR feedback improves immediate outcomes for out-of-hospital cardiac arrest. Circulation. 2014;130:A72-A. [Google Scholar]
- 35.Hopkins C.L., Burk C., Moser S., Meersman J., Baldwin C., Youngquist S.T. Implementation of pit crew approach and cardiopulmonary resuscitation metrics for out-of-hospital cardiac arrest improves patient survival and neurological outcome. J Am Heart Assoc. 2016;5 doi: 10.1161/JAHA.115.002892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kern K.B., Sanders A.B., Raife J., Milander M.M., Otto C.W., Ewy G.A. A study of chest compression rates during cardiopulmonary resuscitation in humans. The importance of rate-directed chest compressions. Arch Intern Med. 1992;152:145–149. [PubMed] [Google Scholar]
- 37.Lukas R.P., Gräsner J.T., Seewald S., et al. Chest compression quality management and return of spontaneous circulation: a matched-pair registry study. Resuscitation. 2012;83:1212–1218. doi: 10.1016/j.resuscitation.2012.03.027. [DOI] [PubMed] [Google Scholar]
- 38.Nehme Z., Ball J., Stephenson M., Walker T., Stub D., Smith K. Effect of a resuscitation quality improvement programme on outcomes from out-of-hospital cardiac arrest. Resuscitation. 2021;162:236–244. doi: 10.1016/j.resuscitation.2021.03.007. [DOI] [PubMed] [Google Scholar]
- 39.Park J.H., Shin S.D., Ro Y.S., et al. Implementation of a bundle of Utstein cardiopulmonary resuscitation programs to improve survival outcomes after out-of-hospital cardiac arrest in a metropolis: a before and after study. Resuscitation. 2018;130:124–132. doi: 10.1016/j.resuscitation.2018.07.019. [DOI] [PubMed] [Google Scholar]
- 40.Bolstridge J., Delaney H.M., Matos R.I. Use of a metronome to improve quality of in-hospital cardiopulmonary resuscitation. Circulation. 2016;134 [Google Scholar]
- 41.Chandra S., Hess E.P., Kolb L., Myers L., White R.D. Effect of real-time automated and delayed summative feedback on CPR quality in adult out-of-hospital cardiac arrest: a prospective multicenter controlled clinical trial. Acad Emerg Med. 2011:18. [Google Scholar]
- 42.Chiang W.C., Chen W.J., Chen S.Y., et al. Better adherence to the guidelines during cardiopulmonary resuscitation through the provision of audio-prompts. Resuscitation. 2005;64:297–301. doi: 10.1016/j.resuscitation.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 43.Fried D.A., Leary M., Smith D.A., et al. The prevalence of chest compression leaning during in-hospital cardiopulmonary resuscitation. Resuscitation. 2011;82:1019–1024. doi: 10.1016/j.resuscitation.2011.02.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kennedy J., Machado K., Maynard C., Walker R.G., Sayre M.R., Counts C.R. Metronome use improves achievement of a target compression rate in out-of-hospital cardiac arrest: a retrospective analysis. Resusc Plus. 2023;15 doi: 10.1016/j.resplu.2023.100417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Khorasani-Zadeh A., Krowl L.E., Chowdhry A.K., et al. Usefulness of a metronome to improve quality of chest compressions during cardiopulmonary resuscitation. Proc (Bayl Univ Med Cent) 2020;34:54–55. doi: 10.1080/08998280.2020.1805840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Koch M., Mueller M., Warenits A.M., Holzer M., Spiel A., Schnaubelt S. Carotid artery ultrasound in the (peri-) arrest setting-a prospective pilot study. J Clin Med. 2022:11. doi: 10.3390/jcm11020469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kramer-Johansen J., Myklebust H., Wik L., et al. Quality of out-of-hospital cardiopulmonary resuscitation with real time automated feedback: a prospective interventional study. Resuscitation. 2006;71:283–292. doi: 10.1016/j.resuscitation.2006.05.011. [DOI] [PubMed] [Google Scholar]
- 48.Lakomek F., Lukas R.P., Brinkrolf P., et al. Real-time feedback improves chest compression quality in out-of-hospital cardiac arrest: A prospective cohort study. PLoS One. 2020;15 doi: 10.1371/journal.pone.0229431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lee H., Kim J., Joo S., et al. The effect of audiovisual feedback of monitor/defibrillators on percentage of appropriate compression depth and rate during cardiopulmonary resuscitation. BMC Anesthesiol. 2023;23:334. doi: 10.1186/s12871-023-02304-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lee S.G.W.G., Kim T.H.H., Song K.J., et al. Effect of audiovisual feedback device type on prehospital chest compression quality during prehospital resuscitation. Circulation. 2023;148 [Google Scholar]
- 51.Leis C.C., González V.A., Hernandez R.D.E., et al. Feedback on chest compression quality variables and their relationship to rate of return of spontaneous circulation. Emergencias. 2013;25:99–104. [Google Scholar]
- 52.Lyngby R.M., Quinn T., Oelrich R.M., et al. Association of real-time feedback and cardiopulmonary-resuscitation quality delivered by ambulance personnel for out-of-hospital cardiac arrest. J Am Heart Assoc. 2023;12 doi: 10.1161/JAHA.123.029457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Niles D., Nysaether J., Sutton R., et al. Leaning is common during in-hospital pediatric CPR, and decreased with automated corrective feedback. Resuscitation. 2009;80:553–557. doi: 10.1016/j.resuscitation.2009.02.012. [DOI] [PubMed] [Google Scholar]
- 54.Olasveengen T.M., Tomlinson A.E., Wik L., et al. A failed attempt to improve quality of out-of-hospital CPR through performance evaluation. Prehosp Emerg Care. 2007;11:427–433. doi: 10.1080/10903120701536628. [DOI] [PubMed] [Google Scholar]
- 55.Pearson D.A., Darrell Nelson R., Monk L., et al. Comparison of team-focused CPR vs standard CPR in resuscitation from out-of-hospital cardiac arrest: results from a statewide quality improvement initiative. Resuscitation. 2016;105:165–172. doi: 10.1016/j.resuscitation.2016.04.008. [DOI] [PubMed] [Google Scholar]
- 56.Pfeiffer S., Duval-Arnould J., Wenger J., et al. 345: CPR coach role improves depth, rate, and return of spontaneous circulation. Crit Care Med. 2018;46:155. [Google Scholar]
- 57.Picard C., Drew R., Norris C.M., et al. Cardiac arrest quality improvement: a single-center evaluation of resuscitations using defibrillator, feedback device, and survey data. J Emerg Nurs. 2022;48:224–232.e8. doi: 10.1016/j.jen.2021.11.005. [DOI] [PubMed] [Google Scholar]
- 58.Rainey K., Birkhoff S. Turn the beat on: an evidenced-based practice journey implementing metronome use in emergency department cardiac arrest. Worldviews Evid Based Nurs. 2021;18:68–70. doi: 10.1111/wvn.12486. [DOI] [PubMed] [Google Scholar]
- 59.Riyapan S., Naulnark T., Ruangsomboon O., et al. Improving quality of chest compression in thai emergency department by using real-time audio-visual feedback cardio-pulmonary resuscitation monitoring. J Med Assoc Thailand. 2019;102:245–251. [Google Scholar]
- 60.Saulle M.L., Tisch C.F., Mitchell O.J.L., B.S. A. Quantitative measurement of cardiopulmonary resuscitation delivery in the emergency department. Acad Emerg Med. 2023:30. [Google Scholar]
- 61.Setälä P., Virkkunen I., Kämäräinen A., et al. Nothing beats quality-controlled manual chest compressions: End-tidal carbon dioxide changes between manual cardiopulmonary resuscitation and with active compression–decompression device. Resuscitation. 2015;96:70–71. [Google Scholar]
- 62.Sainio M., Kämäräinen A., Huhtala H., et al. Real-time audiovisual feedback system in a physician-staffed helicopter emergency medical service in Finland: the quality results and barriers to implementation. Scand J Trauma Resusc Emerg Med. 2013;21:1–8. doi: 10.1186/1757-7241-21-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sutton R.M., Maltese M.R., Niles D., et al. Quantitative analysis of chest compression interruptions during in-hospital resuscitation of older children and adolescents. Resuscitation. 2009;80:1259–1263. doi: 10.1016/j.resuscitation.2009.08.009. [DOI] [PubMed] [Google Scholar]
- 64.Cho G.C. Skin and soft tissue damage caused by use of feedback-sensor during chest compressions. Resuscitation. 2009:600. doi: 10.1016/j.resuscitation.2009.02.014. discussion 1. [DOI] [PubMed] [Google Scholar]
- 65.Sainio M., Sutton R.M., Huhtala H., et al. Association of arterial blood pressure and CPR quality in a child using three different compression techniques, a case report. Scand J Trauma Resusc Emerg Med. 2013;21:1–6. doi: 10.1186/1757-7241-21-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Khajouei AS, Rabbani M, Bahrami P. Comparison of the CPR feedback device effect on the effective technique of the CPR in two modes of the device warning being on and off. [DOI] [PMC free article] [PubMed]
- 67.Leo W.Z., Chua D., Tan H.C., Ho V.K. Chest compression quality and patient outcomes with the use of a CPR feedback device: a retrospective study. Sci Rep. 2023;13:19852. doi: 10.1038/s41598-023-46862-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.