Key Points
Question
Can repeat selective laser trabeculoplasty (SLT) be beneficial in open-angle glaucoma (OAG) regardless of initial response?
Findings
In this post hoc analysis of a randomized clinical trial including 180 newly diagnosed OAG eyes, using repeat SLT as the first choice of treatment escalation regardless of the initial response, repeat SLT was associated with similar intraocular pressure (IOP) control to initial laser with longer duration of effect.
Meaning
This analysis supports the consideration of repeat SLT in OAG regardless of initial response.
This post hoc analysis of a randomized clinical trial evaluates the responsiveness of open-angle glaucoma and ocular hypertension to selective laser trabeculoplasty.
Abstract
Importance
Selective laser trabeculoplasty (SLT) is becoming the recommended first choice in the treatment of open-angle glaucoma (OAG). However, whether repeat SLT can be recommended regardless of initial response remains controversial.
Objective
To assess the potential of OAG and ocular hypertension (OHT) undergoing repeat laser to respond favorably to SLT, termed responsiveness to SLT.
Design, Setting, and Participants
This post hoc analysis of the Laser in Glaucoma and Ocular Hypertension Trial in China (LiGHT China) was conducted from March 2015 to April 2023 in Zhongshan Ophthalmic Center. Of 1376 newly diagnosed OAG and OHT eyes of 771 adults in the original trial, 180 eyes of 105 participants were included in the present study, which underwent initial and repeat SLT as primary treatments.
Exposures
Standard SLT was the primary treatment. Repeat SLT was the first choice of treatment escalation regardless of initial response. IOP reduction after SLT and the duration of effect were analyzed. The maximum reduction in IOP within 2 years after initial SLT and repeat SLT was used to identify potential nonresponsiveness.
Main Outcomes and Measures
IOP reduction 2 months after SLT.
Results
A total of 180 eyes from 105 Chinese participants (mean [SD] age, 45.6 [14.5] years; 58 [55.2%] male and 47 [44.8%] female) underwent repeat SLT. Initial SLT and repeat SLT were both associated with a reduction in IOP (mean, 4.5 mm Hg; 95% CI, 3.9 to 5.1; P < .001 and mean, 3.3 mm Hg; 95% CI, 2.7 to 3.8; P < .001, respectively). The mean (SD) IOP after repeat SLT was 15.8 (3.4) mm Hg, similar to 16.0 (4.0) mm Hg after initial SLT (difference, −0.4mm Hg; 95% CI, −1.0 to 0.3; P = .24). Duration of effect after repeat SLT was longer than after initial SLT (1043 days vs 419 days; hazard ratio, 0.38; 95% CI, 0.29 to 0.50; P < .001). IOP reduction after initial SLT was uncorrelated with that after repeat SLT, and 153 eyes (85.0%) responded favorably to SLT at least once. A subset of 27 eyes (15.0%) was identified as potentially nonresponsive and found distinctive with older age (mean [SD], 54.1 [12.5] years vs 44.2 [14.2] years; difference, 10.5 years; 95% CI, 2.9 to 18.1; P = .009), higher proportion of female participants (difference, 27.5%; 95% CI, 3.6 to 51.5; P = .03), and lower baseline IOP (difference, −3.2 mm Hg; 95% CI, −5.2 to −1.3; P = .001).
Conclusions and Relevance
These post hoc analyses showed that most cases of OAG and OHT were highly responsive to SLT and support the consideration of repeat SLT regardless of initial response, while individuals who are nonresponsive to this treatment may have specific features.
Introduction
Glaucoma is the leading cause of irreversible blindness worldwide,1 and the affected population is continuously increasing.2 Selective laser trabeculoplasty (SLT) has been endorsed as the primary treatment option for open-angle glaucoma (OAG), the most prevalent subtype,1 in the latest editions of guidelines.3,4,5 Several advantages of SLT have been demonstrated, including comparable efficacy to topical medication,6,7 superior cost-effectiveness,6 and minimal tissue damage.8 However, the potential of OAG to respond favorably to SLT, termed here the responsiveness to SLT, has not been thoroughly explored. Previous studies have reported inconsistent results. Thus, there is a pressing need for high-quality evidence to elucidate this aspect.
Recent studies have identified a subset of participants who achieved limited intraocular pressure (IOP) reduction following SLT.9 Empirically, these participants were regarded as nonresponsive to SLT and received topical medications as subsequent treatments instead of repeat SLT. In contrast, another study reported that participants exhibited similar responses to repeat SLT irrespective of their initial response.10 Whether repeat SLT is appropriate for patients with a poor initial response remains controversial. Resolving the controversy is crucial for refining our understanding of SLT’s applicability.
The present study is a post hoc analysis of the Laser in Glaucoma and Ocular Hypertension Trial in China (LiGHT China), a randomized clinical trial.11 By focusing on participants with OAG and ocular hypertension (OHT) who received repeat SLT, we mainly analyzed IOP reduction after initial SLT and repeat SLT. We also endeavored to identify factors associated with participants’ responsiveness to SLT. Participants underwent repeat SLT regardless of their initial response in the LiGHT China trial.
Methods
This study adhered to the tenets of the Declaration of Helsinki. The LiGHT China trial was approved by the institutional review board of Zhongshan Ophthalmic Center, Guangzhou, China. Ethical approval was obtained from the ethics committee of Zhongshan Ophthalmic Center. All participants provided written informed consent for voluntary participation (without any incentive) in the study before enrollment. This study was reported in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Participants and Interventions
Eligible participants with newly diagnosed treatment-naive OAG and OHT were enrolled in the LiGHT China trial (eAppendix in Supplement 1). Details about the trial design have been described previously.11 Participants were randomly allocated to the Medication-1st Arm or Laser-1st Arm. In the Laser-1st Arm, standardized SLT was conducted. One hundred nonoverlapping shots of a preset 3-nanosecond duration and a preset 400-μm spot size were used on 360° trabecular meshwork, with the laser energy varied to achieve the desired end point: the production of a few fine champagne bubbles. This study mainly focused on the participants who underwent repeat SLT in the Laser-1st Arm.
Treatment Escalation
LiGHT China followed a treat in pursuit of control design. Treatment escalation would be triggered by 1 of the following 3 criteria: (1) IOP exceeding the target of 4 mm Hg or greater at a single visit; (2) strong evidence of deterioration, defined as likely progression by Glaucoma Progression Analysis (GPA) on visual field (VF) reports or rim area loss likely or probably greater than 1% per year by Heidelberg Retinal Tomography (HRT) reports; and (3) IOP exceeding the target of 2 mm Hg or greater and less than 4 mm Hg for 2 consecutive visits, together with less strong evidence of deterioration, defined as possible progression by GPA on VF reports or rim area loss possibly than 1% per year by HRT reports. Target IOP was customized based on severity stratification related to VF loss, including the Canadian Target IOP Workshop criteria12 and the additional central VF loss criteria.13 Target IOP was revised when IOP exceeded the target of 2 mm Hg or greater and less than 4 mm Hg for more than 2 consecutive visits but evidence of no deterioration occurred. Ophthalmic examinations were conducted by operators masked to clinical decisions. IOP was measured using Goldmann applanation tonometer on slitlamp microscopes following the Advanced Glaucoma Intervention Study (AGIS) approach.14 A minimum of 2 months of follow-up was required after SLT to ensure sufficient time for the effect to manifest. In the Laser-1st Arm, repeat SLT was the first choice for treatment escalation, regardless of participants’ responses to initial SLT. Clinicians made no selection based on empirical inference, and participants received medication instead only if they conveyed a strong preference. If further treatment escalation was required after repeat SLT, topical medication was the first choice.
Rationale of Analysis
The primary outcome of this study was IOP reduction following SLT. IOP was monitored at 1 to 2 hours and 2 weeks after SLT to prevent transient elevation and was formally recorded at 2 months as the first scheduled follow-up visit. After the 2-month mark, eyes would be censored from analysis if treatment escalation was performed. IOP recorded at 2 months after both initial and repeat SLT was the primarily concern in this analysis. Both the absolute reduction and the percentage of reduction in IOP were analyzed. To better clarify responsiveness to SLT, the maximum reduction in IOP within 2 years after SLT was explored. A poor response to SLT was defined if the maximum reduction in IOP was less than 20% during follow-up.
The unit of the analysis was the eye. All eyes were included in the original analysis. To assess the robustness of results, a subset comprising 1 eye selected randomly per participant was analyzed as sensitivity analysis (eTables 1-2 and eFigures 1-3 in Supplement 1).
Statistical Analysis
Mixed models with cross-random effects were applied to adjust the correlation between paired eyes and reduce regression to the mean in repeat measurement. One-way F test and Kruskal-Wallis test were used for continuous variables, and χ2 test and Fisher exact test were used for categorical variables. Survival analyses were used to estimate the duration of effect, where the failure event was defined as the onset of treatment escalation and the right-censored data type was used.
All P values were 2-sided but not adjusted for multiple analyses and were considered significant at P < .05. Statistical analyses were conducted using Python, with packages Scipy, Statsmodels, and Lifelines.
Results
Demographic and Clinical Characteristics of Participants
From March 10, 2015, to April 25, 2023, a total of 180 eyes of 105 Chinese participants (mean [SD] age, 45.6 [14.5] years; 58 [55.2%] male and 47 [44.8%] female) received repeat SLT in the Laser-1st Arm of the LiGHT China trial. The median (IQR) follow-up was 1159 (714-1792) days. Another 50 eyes received topical medications rather than repeat laser due to the strong preference of the participants (eFigure 4 in Supplement 1).
As presented in Table 1, the eyes subjected to repeat SLT exhibited a higher proportion of moderate (29.4% vs 13.6%) to severe (11.7% vs 4.1%) OAG (P < .001), coupled with worse baseline VF mean deviation (MD) of −5.2 dB on average (difference, −1.8 dB; 95% CI, −2.4 to −1.3; P < .001), compared to those undergoing single SLT. Participants who opted out of the repeat SLT procedure and received topical medications instead were of an older age demographic (mean [SD], 53.8 [16.2] years vs 45.6 [14.5] years; difference, 8.3 years; 95% CI, 2.1 to 14.6; P = .01), but their other characteristics closely resembled those of the individuals who underwent repeat SLT. There were 73 eyes of 42 participants requiring additional treatment escalation after repeat SLT, and these eyes were characterized by a higher proportion of moderate (28 eyes [38.4%]) to severe (9 eyes [12.3%]) OAG (P = .04) with a worse baseline VF MD of −5.9 dB on average (difference, −1.3 dB; 95% CI, −2.5 to −0.2; P = .05) compared to those without further treatment escalation.
Table 1. Comparison of Demographic and Clinical Characteristics at Baseline.
| Characteristic | Mean (SD) | Difference (repeat SLT vs single SLT), mean (95% CI) | P value | ||
|---|---|---|---|---|---|
| Repeat SLT (n = 180) | SLT and topical medication (n = 50) | Single SLT, no treatment escalation (n = 412) | |||
| Age, y | 45.6 (14.5) | 53.8 (16.2) | 44.1 (16.4) | 1.2 (−2.4 to 4.9) | .38 |
| Sex, No. of participants (%) | |||||
| Male | 58 (55.2) | 16 (50.0) | 141 (57.8) | −2.6 (−14.0 to 8.8) | .75 |
| Female | 47 (44.8) | 16 (50.0) | 103 (42.2) | 2.6 (−8.8 to 14.0) | |
| Disease severity, No. of eyes (%) | |||||
| OHT | 10 (5.6) | 1 (2.0) | 110 (26.7) | −21.1 (−26.5 to −15.7) | <.001 |
| Mild OAG | 96 (53.3) | 25 (50.0) | 229 (55.6) | −2.3 (−11.0 to 6.4) | |
| Moderate OAG | 53 (29.4) | 14 (28.0) | 56 (13.6) | 15.8 (8.4 to 23.2) | |
| Severe OAG | 21 (11.7) | 10 (10.0) | 17 (4.1) | 7.6 (2.5 to 12.7) | |
| Baseline VF MD, dB | −5.2 (3.9) | −6.0 (3.8) | −3.3 (2.9) | −1.8 (−2.4 to −1.3) | <.001 |
| Baseline IOP, mm Hg | 20.4 (4.9) | 22.4 (7.5) | 21.2 (4.5) | −0.7 (−1.5 to 0.1) | .08 |
| Target IOP, mm Hg | 15.3 (3.7) | 15.8 (3.2) | 16.6 (3.5) | −1.3 (−1.9 to −0.7) | <.001 |
| Required IOP reduction, mm Hg | 5.2 (2.1) | 6.6 (5.7) | 4.6 (1.7) | 0.6 (0.3 to 0.9) | .01 |
Abbreviations: IOP, intraocular pressure; OAG, open-angle glaucoma; OHT, ocular hypertension; SLT, selective laser trabeculoplasty; VF MD, visual field mean deviation.
Reduction in IOP After SLT
The mean (SD) target IOP of eyes undergoing repeat SLT was 15.3 (3.7) mm Hg, lower than the mean (SD) 16.6 (3.5) mm Hg of those undergoing single SLT (difference, −1.3 mm Hg; 95% CI, −1.9 to −0.7; P < .001), which required considerably greater IOP reduction to achieve (difference, 0.6 mm Hg; 95% CI, 0.3 to 0.9; P = .01). Upon completion of the initial SLT, the actual IOP reduction in the eyes undergoing repeat SLT was 4.5 mm Hg (95% CI, 3.9 to 5.1), less than the 5.3-mm Hg reduction (95% CI, 4.9 to 5.7) in those undergoing single SLT (difference, −0.9 mm Hg; 95% CI, −1.6 to −0.3; P < .001).
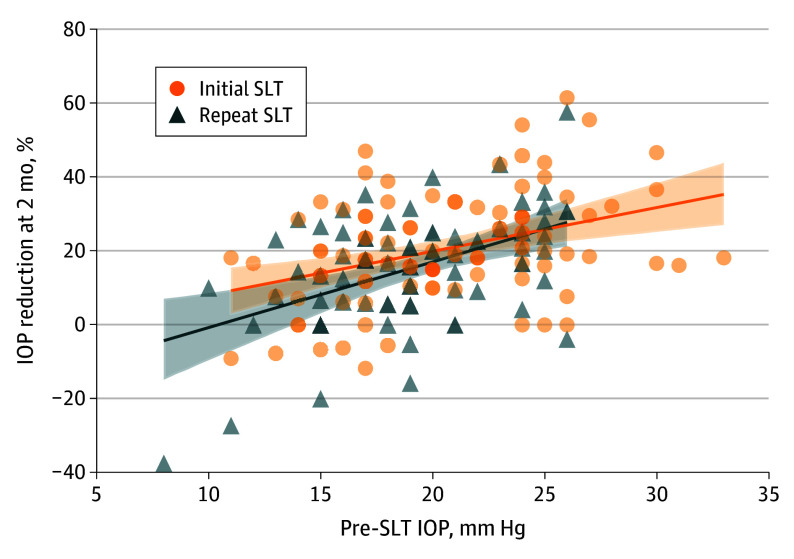
As outlined in Table 2, the mean (SD) IOP before repeat SLT was 18.8 (4.3) mm Hg, lower than the mean (SD) 20.4 (4.9) mm Hg before initial SLT (difference, −1.6 mm Hg; 95% CI, −2.1 to −1.2; P < .001). IOP reduction at the 2-month mark following repeat SLT was 3.3 mm Hg (95% CI, 2.7 to 3.8), or 15.4% (95% CI, 12.7 to 18.0), less than the 4.5-mm Hg reduction (95% CI, 3.9 to 5.1), or 20.3% (95% CI, 18.1 to 22.6), observed after the initial SLT (difference, −1.3 mm Hg; 95% CI, −2.1 to −0.5; P = .001 or −5.3%; 95% CI, −8.9 to −1.8; P = .003, respectively). However, mean (SD) IOP recorded at 2 months was 15.8 (3.4) and 16.0 (4.0) mm Hg, respectively (difference, −0.4 mm Hg; 95% CI, −1.0 to 0.3; P = .24). Both the absolute and percentage reduction in IOP at 2 months were positively correlated with the corresponding pre-SLT IOP, with the latter being illustrated in Figure 1. No correlation was found between IOP reduction at 2 months after repeat SLT and after initial SLT, as depicted in Figure 2. A subset of 12 eyes underwent a third SLT following the second SLT. The mean (SD) IOP for these eyes was 16.1 (3.5) mm Hg before the third SLT and 13.9 (3.0) mm Hg at 2 months after, yielding an average reduction of 2.0 mm Hg. The mean (SD) total power of the initial SLT and the repeat SLT was 51.3 (11.7) mJ and 57.1 (14.3) mJ, respectively (difference, −5.8 mJ; 95% CI, −7.7 to −3.9; P < .001).
Table 2. Comparison of Intraocular Pressure (IOP) Reduction at the 2-Month Mark After Initial and Repeat Selective Laser Trabeculoplasty (SLT).
| IOP and IOP reduction | SLT | Difference, mean (95% CI) | P value | |
|---|---|---|---|---|
| Repeat (n = 180) | Initial (n = 180) | |||
| Pretreatment IOP, mean (SD), mm Hg | 18.8 (4.3) | 20.4 (4.9) | −1.6 (−2.0 to −1.2) | <.001 |
| IOP at 2 mo after SLT, mean (SD), mm Hg | 15.8 (3.4) | 16.0 (4.0) | −0.4 (−1.0 to 0.3) | .24 |
| IOP reduction at 2 mo after SLT, mean (95% CI), mm Hg | 3.3 (2.7 to 3.8) | 4.5 (3.9 to 5.1) | −1.3 (−2.1 to −0.5) | .001 |
| IOP reduction at 2 mo after SLT, mean (95% CI), % | 15.4 (12.7 to 18.0) | 20.3 (18.1 to 22.6) | −5.3 (−8.9 to −1.8) | .003 |
Figure 1. Intraocular Pressure (IOP)–Dependent Reduction Pattern of Selective Laser Trabeculoplasty (SLT).
The percentage of reduction in IOP after both initial SLT and repeat SLT was positively correlated with the corresponding pre-SLT IOP.
Figure 2. Uncorrelation Between Initial and Repeat Response.
The intraocular pressure (IOP) reduction at the 2-month mark after repeat SLT was uncorrelated with that after initial selective laser trabeculoplasty (SLT).
Identification of Potential Nonresponsiveness Through Maximum Reduction in IOP
The median (IQR) time for the occurrence of the maximum reduction in IOP following initial SLT was 58 (18-179) days and following repeat SLT was 69 (19-218) days. The mean (SD) value of the maximum reduction in IOP 2 years following initial SLT was 5.9 (3.7) mm Hg or 27.4% (13.4), and that following repeat SLT was 4.4 (3.4) mm Hg or 21.8% (14.9).
Taking 20% as a threshold, a subset of 27 eyes (15.0%) of 18 participants responded poorly to both initial SLT and repeat SLT, while 84 eyes (46.7%) responded favorably to one and 69 eyes (38.3%) to both. The latter 2 subsets with high responsiveness exhibited similar characteristics (eTable 4 in Supplement 1). In contrast, the former subset, as potentially nonresponsive, was found to have distinct features, including older age (mean [SD], 54.1 [12.5] years vs 44.2 [14.2] years; difference, 10.5 years; 95% CI, 2.9 to 18.1; P = .009), a higher proportion of female individuals (difference, 27.5%; 95% CI, 3.6 to 51.5; P = .03), and lower baseline IOP (difference, −3.2 mm Hg; 95% CI, −5.2 to −1.3; P = .001). Using these features as independent variables and responsiveness clusters as the dependent variable (1 = responsive, 0 = nonresponsive), a multivariate linear regression model showed that the coefficient of age was −0.004 (95% CI, −0.007 to −0.001; P = .03), the coefficient of male sex was 0.13 (95% CI, 0.02 to 0.23; P = .01), and the coefficient of baseline IOP was 0.012 (95% CI, 0.002 to 0.023; P = .01).
Duration of Effect After SLT
The median (IQR) interval between initial SLT and repeat SLT was 423 (205-791) days. Kaplan-Meier curves of the 180 eyes that underwent repeat SLT are plotted with a 95% CI in Figure 3. The median duration of effect following initial SLT and repeat SLT were 419 days and 1043 days, respectively. Cox regression demonstrated that the duration of effect was longer after the repeat SLT, with a hazard ratio of 0.38 (95% CI, 0.29 to 0.50, P < .001).
Figure 3. Duration of Effect After Initial and Repeat Selective Laser Trabeculoplasty (SLT).
The duration of intraocular pressure control and no progression after repeat SLT was longer. Eyes were censored when treatment escalation was performed. The median duration after initial and repeat SLT was 419 and 1043 days, respectively.
Safety of SLT
No evidence of harm caused by SLT was found. The IOP spikes at 1 to 2 hours after SLT were monitored, and no spike greater than 5 mm Hg was found. The adverse events were self-limiting, and no sight-threatening events were found. More details are available in eTable 4 in Supplement 1.
Discussion
Current guidelines from the American Academy of Ophthalmology, the National Institute for Health and Care Excellence, and the European Glaucoma Society recommend SLT as the first choice in the treatment of OAG based on its distinctive advantages.3,4,5 However, the applicable scope of SLT has not been thoroughly clarified. In this study, we focused on a persistent controversy9,10 regarding participants’ responsiveness to SLT and demonstrated that most cases of OAG and OHT were highly responsive. New evidence was posed that the response to only 1 SLT intervention was not a proper indicator of individual responsiveness. Repeat SLT was still promising even if a participant poorly responded to the initial SLT. Nevertheless, we identified a subset of potentially nonresponsive individuals with poor response to repeat SLT, and they shared some characteristics.
The common reason for treatment escalation was not the poor response to initial SLT. However, a stricter target IOP and a more considerable gap to reach the target resulted in treatment escalation. A lower target IOP was necessary because of a worse severity grading related to worse baseline VF. A small subset of participants who needed additional treatment escalation after repeat SLT exhibited even worse VF and grades. These findings support a previous prospective study.9
The initial IOP reduction in those undergoing repeat SLT was less than in those undergoing single SLT. A proportion of eyes responded poorly to the initial SLT. Except for potentially nonresponsive participants, various other factors during and after the operating process can influence the actual IOP reduction in individuals.15,16 A better response to repeat SLT can be expected if participants were initially affected by these uncertain factors instead of experiencing low responsiveness.
In this study, we advocated for repeat SLT as the first choice of treatment escalation to avoid bias. We only allowed participants to receive topical medications as the treatment escalation if they firmly conveyed their preference. The similarities in background characteristics demonstrated the effectiveness of our effort. Those choosing topical medication after the initial SLT exhibited an older age, possibly because of a higher preference for more conservative treatment in older participants. IOP reduction in these participants seemed good, although older age was found to be a risk factor associated with inferior responsiveness to SLT.
Both initial and repeat SLT were associated with a reduction in IOP. Repeat SLT was associated with similar IOP levels to initial SLT and showed a longer duration of effect, as reported in previous studies.9,17,18,19,20 IOP reduction at the 2-month mark after repeat SLT was less than that after initial SLT. It can be explained by the positive correlation between pre-SLT IOP and IOP reduction. The IOP before repeat SLT was lower as a result of timely treatment escalation following our protocol. However, IOP dropped even lower after repeat SLT in the LiGHT UK study.9 The additive effect of repeat lasers was prominent in their report because only eyes undergoing repeat SLT within 18 months after initial SLT were included, while the median (IQR) interval between lasers was 423 (205-791) days in this study. The wide interval flattened the additive effect, as we can also observe an apparent additive effect in a subset if we restrict the interval. Another reason was that the pre-SLT IOP in this study was much lower than in LiGHT UK, and the reduction was IOP dependent. We found that not only absolute reduction21 but also percentage of reduction in IOP was positively correlated with pre-SLT IOP. It could be inferred that the IOP level achieved through SLT possibly had a floor value.
Baseline IOP was lower in this study than in previous studies.9,22 Less OHT in this study and a higher percentage of normal-tension glaucoma in Chinese OAG23 may partly account for the difference. Our inferior IOP reduction compared to previous studies can be explained by the IOP-dependent pattern. Lower-power SLT applied on less pigmented trabecular meshwork may also have influenced the IOP reduction in this study. Ethnical variability in trabecular meshwork may explain the lower laser power in LiGHT China than in LiGHT UK, because the 2 trials shared the same SLT intervention protocol to the same clinical end point,11,24 and previous studies based on Chinese population supported relatively low SLT power similar to this study.25,26
We demonstrated that IOP reduction observed from only one SLT intervention, especially at an isolated time mark, was not predictive of the effectiveness of repeat SLT. This is likely because various uncertain factors can influence the actual effect, and IOP at an isolated time mark should not be considered representative. We found most participants to respond favorably to SLT at least once. They had the potential to acquire a considerable reduction in IOP even if they did not achieve reduction initially. Considering the advantages of SLT, it would be regrettable if patients were to miss the opportunity to try repeat SLT based on previous empirical judgment. As a refinement, we adopted the maximum reduction in IOP within a year after SLT to identify potentially nonresponsive participants, which seemed to result in better distinguishment.
Potentially nonresponsive participants exhibited unique features. Older age, female sex, and lower baseline IOP were previously reported to be associated with worse effects of SLT.15,21 We demonstrated that these 3 features were independently associated with nonresponsiveness despite their autocorrelation27 by multivariate analysis. However, the underlying mechanism is unknown. We can only explain the lower baseline IOP through the positive correlation between IOP reduction and pre-SLT IOP and the possible floor level of IOP through SLT. Medications can be considered if these risk factors are present, and more intense visits can be advised if SLT is still applied.
Topical medication was advised in our protocol when additional treatment escalation was required after repeat SLT. However, 12 eyes with OAG received a third SLT at the patients’ request. We observed effective IOP reduction and did not notice excess adverse events. We noted that a third SLT was conducted effectively and safely in OAG in Afro-Caribbean participants in another study.22 Relevant evidence is still insufficient.
Limitations
Certain limitations of this study should be noted. The foundation population was Chinese; thus, some inferences may not be universal in a different context. The participants were recruited in a single center, which resulted in less representation. The sample size of the participants revealed to be potentially nonresponsive was small, so the analysis of their features may not be precise enough.
Conclusions
In conclusion, most OAG and OHT cases had high responsiveness to SLT to achieve considerable IOP reduction. Repeat SLT was promising as the first choice of treatment escalation regardless of initial response. Potentially nonresponsive patients may have identifiable risk factors.
eAppendix. Key protocol of LiGHT China
eFigure 1. The IOP-dependent Reduction Pattern of SLT (Sensitivity Analysis)
eFigure 2. Uncorrelation between Initial and Repeat Response (Sensitivity Analysis)
eFigure 3. Duration of Effect after Initial and Repeat SLT (Sensitivity Analysis)
eFigure 4. Schematic Plot
eTable 1. Comparison of Demographic and Clinical Characteristics at Baseline (Sensitivity Analysis)
eTable 2. Comparison of IOP Reduction at the 2-Month Mark after Initial and Repeat Selective Laser Trabeculoplasty (Sensitivity Analysis)
eTable 3. Comparison of Responders and Potential Non-responders to Selective Laser Trabeculoplasty
eTable 4. Details of Adverse Events after Selective Laser Trabeculoplasty
The members of the LiGHT China Trial Study Group
Data sharing statement
References
- 1.Jonas JB, Aung T, Bourne RR, Bron AM, Ritch R, Panda-Jonas S. Glaucoma. Lancet. 2017;390(10108):2183-2193. doi: 10.1016/S0140-6736(17)31469-1 [DOI] [PubMed] [Google Scholar]
- 2.Song P, Wang J, Bucan K, Theodoratou E, Rudan I, Chan KY. National and subnational prevalence and burden of glaucoma in China: a systematic analysis. J Glob Health. 2017;7(2):020705. doi: 10.7189/jogh.07.020705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American Academy of Ophthalmology . Primary open-angle glaucoma PPP 2020. Accessed July 24, 2024. https://www.aao.org/education/preferred-practice-pattern/primary-open-angle-glaucoma-ppp
- 4.National Institute for Health and Care Excellence . Glaucoma: diagnosis and management. Accessed July 24, 2024. https://www.nice.org.uk/guidance/ng81
- 5.European Glaucoma Society . Terminology and guidelines for glaucoma (5th edition). Accessed July 24, 2024. https://eugs.org/educational_materials/6 [DOI] [PubMed]
- 6.Gazzard G, Konstantakopoulou E, Garway-Heath D, et al. ; LiGHT Trial Study Group . Selective laser trabeculoplasty versus eye drops for first-line treatment of ocular hypertension and glaucoma (LiGHT): a multicentre randomised controlled trial. Lancet. 2019;393(10180):1505-1516. doi: 10.1016/S0140-6736(18)32213-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gazzard G, Konstantakopoulou E, Garway-Heath D, et al. ; LiGHT Trial Study Group . Laser in glaucoma and ocular hypertension (LiGHT) trial: six-year results of primary selective laser trabeculoplasty versus eye drops for the treatment of glaucoma and ocular hypertension. Ophthalmology. 2023;130(2):139-151. doi: 10.1016/j.ophtha.2022.09.009 [DOI] [PubMed] [Google Scholar]
- 8.Kramer TR, Noecker RJ. Comparison of the morphologic changes after selective laser trabeculoplasty and argon laser trabeculoplasty in human eye bank eyes. Ophthalmology. 2001;108(4):773-779. doi: 10.1016/S0161-6420(00)00660-6 [DOI] [PubMed] [Google Scholar]
- 9.Garg A, Vickerstaff V, Nathwani N, et al. ; Laser in Glaucoma and Ocular Hypertension Trial Study Group . Efficacy of repeat selective laser trabeculoplasty in medication-naive open-angle glaucoma and ocular hypertension during the LiGHT trial. Ophthalmology. 2020;127(4):467-476. doi: 10.1016/j.ophtha.2019.10.023 [DOI] [PubMed] [Google Scholar]
- 10.Khouri AS, Lin J, Berezina TL, Maltzman B, Fechtner RD. Repeat selective laser trabeculoplasty can be effective in eyes with initial modest response. Middle East Afr J Ophthalmol. 2014;21(3):205-209. doi: 10.4103/0974-9233.134668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang Y, Jiang Y, Huang S, et al. ; Light China Trial Study Group . Laser in glaucoma and ocular hypertension trial (LIGHT) in China—a randomized controlled trial: design and baseline characteristics. Am J Ophthalmol. 2021;230:143-150. doi: 10.1016/j.ajo.2021.04.020 [DOI] [PubMed] [Google Scholar]
- 12.Damji KF, Behki R, Wang L; Target IOP Workshop participants . Canadian perspectives in glaucoma management: setting target intraocular pressure range. Can J Ophthalmol. 2003;38(3):189-197. doi: 10.1016/S0008-4182(03)80060-1 [DOI] [PubMed] [Google Scholar]
- 13.Mills RP, Budenz DL, Lee PP, et al. Categorizing the stage of glaucoma from pre-diagnosis to end-stage disease. Am J Ophthalmol. 2006;141(1):24-30. doi: 10.1016/j.ajo.2005.07.044 [DOI] [PubMed] [Google Scholar]
- 14.The AGIS Investigators . The Advanced Glaucoma Intervention Study (AGIS): 7. the relationship between control of intraocular pressure and visual field deterioration. Am J Ophthalmol. 2000;130(4):429-440. doi: 10.1016/S0002-9394(00)00538-9 [DOI] [PubMed] [Google Scholar]
- 15.Gulati V, Fan S, Gardner BJ, et al. Mechanism of action of selective laser trabeculoplasty and predictors of response. Invest Ophthalmol Vis Sci. 2017;58(3):1462-1468. doi: 10.1167/iovs.16-20710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dahlgren T, Ayala M, Zetterberg M. Optimal performance of selective laser trabeculoplasty: results from the Swedish Optimal SLT Multicenter Randomized Controlled Trial. Ophthalmol Glaucoma. 2024;7(2):105-115. doi: 10.1016/j.ogla.2023.10.004 [DOI] [PubMed] [Google Scholar]
- 17.Hong BK, Winer JC, Martone JF, Wand M, Altman B, Shields B. Repeat selective laser trabeculoplasty. J Glaucoma. 2009;18(3):180-183. doi: 10.1097/IJG.0b013e31817eee0b [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Avery N, Ang GS, Nicholas S, Wells A. Repeatability of primary selective laser trabeculoplasty in patients with primary open-angle glaucoma. Int Ophthalmol. 2013;33(5):501-506. doi: 10.1007/s10792-013-9729-3 [DOI] [PubMed] [Google Scholar]
- 19.Francis BA, Loewen N, Hong B, et al. Repeatability of selective laser trabeculoplasty for open-angle glaucoma. BMC Ophthalmol. 2016;16:128. doi: 10.1186/s12886-016-0299-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Polat J, Grantham L, Mitchell K, Realini T. Repeatability of selective laser trabeculoplasty. Br J Ophthalmol. 2016;100(10):1437-1441. doi: 10.1136/bjophthalmol-2015-307486 [DOI] [PubMed] [Google Scholar]
- 21.Garg A, Vickerstaff V, Nathwani N, et al. ; Laser in Glaucoma and Ocular Hypertension Trial Study Group . Primary selective laser trabeculoplasty for open-angle glaucoma and ocular hypertension: clinical outcomes, predictors of success, and safety from the Laser in Glaucoma and Ocular Hypertension Trial. Ophthalmology. 2019;126(9):1238-1248. doi: 10.1016/j.ophtha.2019.04.012 [DOI] [PubMed] [Google Scholar]
- 22.Realini T, Shillingford-Ricketts H, Burt D, Balasubramani GK. Long-term outcomes of selective laser trabeculoplasty for open-angle glaucoma in the Caribbean. Am J Ophthalmol. 2021;232:83-89. doi: 10.1016/j.ajo.2021.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang D, Huang W, Li Y, et al. Intraocular pressure, central corneal thickness, and glaucoma in Chinese adults: the liwan eye study. Am J Ophthalmol. 2011;152(3):454-462.e1. doi: 10.1016/j.ajo.2011.03.005 [DOI] [PubMed] [Google Scholar]
- 24.Gazzard G, Konstantakopoulou E, Garway-Heath D, et al. ; LiGHT Trial Study Group . Laser in Glaucoma and ocular hypertension (LiGHT) trial. a multicentre, randomised controlled trial: design and methodology. Br J Ophthalmol. 2018;102(5):593-598. doi: 10.1136/bjophthalmol-2017-310877 [DOI] [PubMed] [Google Scholar]
- 25.Zhang H, Yang Y, Xu J, Yu M. Selective laser trabeculoplasty in treating post-trabeculectomy advanced primary open-angle glaucoma. Exp Ther Med. 2016;11(3):1090-1094. doi: 10.3892/etm.2015.2959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang HY, Qin YJ, Yang YF, Xu JG, Yu MB. Intraocular pressure-lowering potential of subthreshold selective laser trabeculoplasty in patients with primary open-angle glaucoma. J Ophthalmol. 2016;2016:2153723. doi: 10.1155/2016/2153723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yang Y, Zhang X, Chen Z, et al. Intraocular pressure and diurnal fluctuation of open-angle glaucoma and ocular hypertension: a baseline report from the LiGHT China trial cohort. Br J Ophthalmol. 2023;107(6):823-827. doi: 10.1136/bjophthalmol-2021-320128 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Key protocol of LiGHT China
eFigure 1. The IOP-dependent Reduction Pattern of SLT (Sensitivity Analysis)
eFigure 2. Uncorrelation between Initial and Repeat Response (Sensitivity Analysis)
eFigure 3. Duration of Effect after Initial and Repeat SLT (Sensitivity Analysis)
eFigure 4. Schematic Plot
eTable 1. Comparison of Demographic and Clinical Characteristics at Baseline (Sensitivity Analysis)
eTable 2. Comparison of IOP Reduction at the 2-Month Mark after Initial and Repeat Selective Laser Trabeculoplasty (Sensitivity Analysis)
eTable 3. Comparison of Responders and Potential Non-responders to Selective Laser Trabeculoplasty
eTable 4. Details of Adverse Events after Selective Laser Trabeculoplasty
The members of the LiGHT China Trial Study Group
Data sharing statement