Abstract
Background
Lactobacilli are gram-positive, lactic acid-producing, facultative anaerobes of the human microbiota located in the human gastrointestinal tract, genitourinary tract, and the oral cavity and are considered non-pathogenic. When certain risk factors are present, they have the potential to cause serious infections. The incidence of localized infections associated with Lactobacilli are rare and to our knowledge we present the first known case of severe soft tissue infection of the extremity linked to a Lactobacillus strain.
Case presentation
We describe the case of a 41-year-old man with a history of type 2 Diabetes Mellitus (DM), arterial hypertension and schizophrenia, who was admitted for weakness, high fever of 39.7 °C (103.5°F) and an abscess formation of the left thigh caused by an infection with Lactobacillus gasseri (L.gasseri)
Conclusion
While infections caused by Lactobacilli are rare, it is crucial not to underestimate the potential of typically non-pathogenic bacteria like L. gasseri to act as infectious agents in immunocompromised patients. Abscess drainage and antibiotic treatment were successful treatment strategies for this rare case of soft tissue infection cause by L.gasseri.
Key words: Lactobacillus gasseri, Severe soft tissue infection, Pathogenic potential of Lactobacillus strains, Abscess of the lower extremity
Background
Lactobacilli are gram-positive, lactic acid-producing, facultative anaerobes of the human microbiota located in the human gastrointestinal tract, genitourinary tract, and the oral cavity and are considered non-pathogenic [1]. When certain risk factors are present, they have the potential to cause serious infections, such as bacteremia, infective endocarditis, abscesses of the liver, peritonitis, pulmonary infections and meningitis [2], [3], [4], [5]. Common underlying factors include immunosuppressive therapy, human immunodeficiency virus (HIV), cancer, diabetes mellitus, renal failure and broad-spectrum antibiotic therapy [3], [6]. The incidence of localized infections associated with Lactobacilli are rare and to our knowledge we present the first known case of severe soft tissue infection of the extremity linked to a Lactobacillus strain.
Case
A 41-year-old man with a history of type 2 DM, arterial hypertension and schizophrenia was admitted for weakness, high fever of 39.7 °C (103.5°F) and a severely swollen and painful left leg. Upon arrival he was hemodynamically unstable, presented with an altered mental status and the initial bloodwork showed elevated infection parameters with a c-reactive protein (CRP; normal: <0.5 mg/dl) of 40 mg/dl. The NEWS score was 13 (respiration rate between 21–24, temperature > 39.1 °C, systolic blood pressure <90 mmHg, heart rate between 111–130 and abnormal level of consciousness) and the SIRS score suggested a septic condition. A computed tomography (CT) of the thorax, abdomen and both legs were performed, showing a 32 × 2×11 cm in diameter holding abscess formation in the area of the left thigh, whereby the main part could be delimited laterally along the rectus femoris and also spread medially in the distal third. Caudally, the abscess formation extended both medially and laterally up to the level of the retinacula. This resulted in the indication for acute surgical debridement and necrosectomy. The patient had multiple sets of blood cultures drawn and multiple wound swabs were taken. Since the patient had a known penicillin allergy, intravenous empirical antibiotic treatment with Linezolid 600 mg twice a day and Meropenem 2 g three times a day was started directly after intervention. The wound was then lavaged several times over the next few days under sterile conditions and vacuum-assisted closure therapy was subsequently applied on the 7th postoperative day. The blood cultures showed no bacterial or fungal growth, however 5 individual wounds swabs were repeatedly positive for only L. gasseri.
12 days after initial presentation the postoperative defects were successfully covered with split skin grafts. Another 3 days later, the established antibiotic treatment could be terminated as the patient was in a satisfactory condition with a CRP of 2 mg/dl and a dry wound showing no signs of irritation. The patient was subsequently discharged and sent home.
Conclusion
An abscess is caused by an inflammatory melting of tissue, which in most cases is triggered by a bacterial infection. Cutaneous abscesses represent prevalent outcomes of bacterial infections. They may appear as temporary, painful nodules that naturally resolve, or in more severe instances, as significant deep-seated abscesses linked with the spread of bacteria through the bloodstream. While various Gram-positive and Gram-negative bacteria can trigger abscess formation, Staphylococcus aureus (S. aureus), notably community-associated methicillin-resistant Staphylococcus aureus (MRSA), stands out as the primary culprit [11].
L. gasseri are gram-positive, non-spore forming bacilli that flourish in anaerobic environments. It is part of the natural human microbiome and is usually found in the gastrointestinal tract, where it plays a vital role in keeping the intestinal micro-flora healthy [7]. L. gasseri can be found in the majority of fermented foods and in probiotics. Lactobacilli are non-pathogenic and rarely the causative agent of severe infections however, under the right circumstances, these non-virulent pathogens can cause illness [7], [8]. Immunocompromised patients are particularly vulnerable and therefore more susceptible to illness and complications caused by Lactobacillus species [7]. It is noteworthy, that L. gasseri is not a very frequently reported pathogen among case reports of patients suffering from Lactobacilli infections. The vast majority of cases seem to be linked to Lactobacillus rhamnosus, Lactobacillus casei or Lactobacillus paracasei [8].
Documented cases of infections with Lactobacilli in literature encompass a heterogeneous spectrum of clinical presentations, spanning from critical conditions, such as endocarditis, bacteremia, meningitis to pneumonia and abscesses [9]. In this case report we presented a patient with a large mono-bacterial abscess on his left thigh. L. gasseri was the only opportunistic pathogen that was isolated from multiple deep wound swabs performed before antibiotic treatment and during surgical intervention. Our patient was immunocompromised due to his diabetes with a highly elevated hemoglobin A1c (HbA1c) at 13.2 % indicating poor blood sugar control. He also did not have any exposure to antibiotics prior to hospitalization and rarely sought healthcare for his medical conditions, as he told us upon arrival that the symptoms started approximately 3 weeks before seeking help for his swollen leg. Some instances of infections associated with Lactobacilli have been documented in patients who have consumed probiotics containing Lactobacilli [12], [13] however the patient denied taking any form of food supplements..
Table 1.
Antibiogram: The antibiogram describes a germ that is sensitive to Penicillin-G and meropenem.
minimum inhibitory concentration in mg/l
The suggested diagnostic tools to optimally identify Lactobacilli as a causative agent is via matrix-assisted laser desorption ionization time-of-flight spectrometry (MALDI-TOF) and microbiological evaluation and genetic molecular methods, such as polymerase chain reaction (PCR) testing [7], [10]. Our patient was diagnosed using PCR and MALDI-TOF to identify L. gasseri. Antibiotic treatment with Linezolid and Meropenem was initiated empirically after consultation with the Department of Infectious Diseases, before the identification of L. gasseri and antimicrobial susceptibility testing. For the detection of antibiotic resistance and susceptibility an ETEST® by bioMérieux was carried out. MHS agar was used as the culture medium. After the antibiotic therapy and surgical drainage of the abscess our patient rapidly improved and a skin-graft could be applied. While infections caused by Lactobacilli are rare, it is crucial not to underestimate the potential of typically non-pathogenic bacteria like L. gasseri to act as infectious agents in immunocompromised patients..
Fig. 1.
CRP under antibiotic treatment: CRP at the time of initial presentation was of 40 mg/dl and continuously decreased under antibiotic treatment with Linezolid 600 mg twice a day and Meropenem 2 g three times a day.
Fig. 2.
CT (initial presentation), Abscess formation in the left thigh marked with an arrow: Here you can see a 32 × 2×11 cm in diameter holding abscess formation in the area of the left thigh, whereby the main part could be delimited laterally along the rectus femoris and also spread medially in the distal third. Caudally, the abscess formation extended both medially and laterally up to the level of the retinacula.
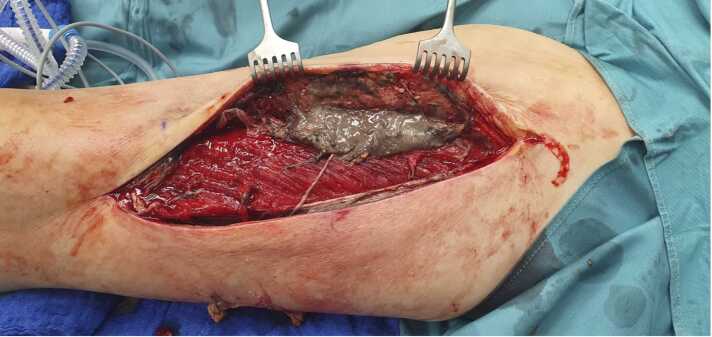
Fig. 3.
Initial intraoperative findings: After incision the radiological findings were confirmed. We were able to drain the abscess formation completely and performed surgical debridement and necrosectomy.
Funding Statement
The authors received no funding for this work.
Author Contributions
A.C. designed the concept. All authors contributed their specific expertise, wrote the manuscript, and revised it critically and approved the final version of the manuscript.
Author Contributions
AC designed the concept. All authors analyzed data, contributed their specific expertise, wrote the manuscript, and revised it critically and approved the final version of the manuscript.
Patient Consent/Consent to publish
The authors affirm that the patient provided informed consent for publication of all the data that we present in this case report. He has given his verbal and written consent. The signed consent document is available on request from the author Alexandra Christ.
CRediT authorship contribution statement
Alexandra Christ: Writing – original draft, Conceptualization. Michelle Nägeli: Writing – review & editing, Conceptualization. Clement Staud: Writing – review & editing. Christine Radtke: Supervision.
Declaration of Competing Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Data Availability
The data used in this manuscript is available from the first author on reasonable request. Requests to access this data should be directed to alexandra.christ@meduniwien.ac.at.
References
- 1.Zheng J., Wittouck S., Salvetti E., Franz C., Harris H.M.B., Mattarelli P., et al. A taxonomic note on the genus Lactobacillus: Description of 23 novel genera, emended description of the genus Lactobacillus Beijerinck 1901, and union of Lactobacillaceae and Leuconostocaceae. Int J Syst Evol Microbiol. 2020;70(4):2782–2858. doi: 10.1099/ijsem.0.004107. [DOI] [PubMed] [Google Scholar]
- 2.Rocca M.F., Aguerre L., Cipolla L., Martínez C., Armitano R., Dangiolo G., et al. Lactobacillus spp. invasive infections in Argentina. Int J Infect Dis. 2018;73:163. [Google Scholar]
- 3.Sherid M., Samo S., Sulaiman S., Husein H., Sifuentes H., Sridhar S. Liver abscess and bacteremia caused by lactobacillus: role of probiotics? Case report and review of the literature. BMC Gastroenterol. 2016;16(1):138. doi: 10.1186/s12876-016-0552-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ramos-Coria D., Canto-Losa J., Carrillo-Vázquez D., Carbajal-Morelos L., Estrada-León R., Corona-Rodarte E. Lactobacillus gasseri liver abscess and bacteremia: a case report. BMC Infect Dis. 2021;21(1):518. doi: 10.1186/s12879-021-06181-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Campagne J., Guichard J.F., Moulhade M.C., Kawski H., Maurier F. Lactobacillus endocarditis: a case report in France and literature review. IDCases. 2020;21 doi: 10.1016/j.idcr.2020.e00811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cannon J.P., Lee T.A., Bolanos J.T., Danziger L.H. Pathogenic relevance of Lactobacillus: a retrospective review of over 200 cases. Eur J Clin Microbiol Infect Dis. 2005;24(1):31–40. doi: 10.1007/s10096-004-1253-y. [DOI] [PubMed] [Google Scholar]
- 7.Angela Esquibel, Ala S. Dababneh, and Bharath Raj Palraj et al. Lactobacillus gasseri Causing Bilateral Empyema. 2017 10.1155/2017/4895619. [DOI] [PMC free article] [PubMed]
- 8.Tleyjeh Imad M., Routh Jonathan, Qutub Mohammed O., Lischer Garrett, Liang Kelly V., Baddour Larry M. Lactobacillus gasseri Causing Fournier's Gangrene. Scand J Infect Dis. 2004;36(6-7):501–503. doi: 10.1080/00365540410015916. DOI: 10.1080/00365540410015916. [DOI] [PubMed] [Google Scholar]
- 9.Rossi F., Amadoro C., Gasperi M., Colavita G. Lactobacilli infection case reports in the last three years and safety implications. Nutrients. 2022;14:1178. doi: 10.3390/nu14061178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Monica Bapna, Jaslyn Maurer, Samantha Ruddy, Krupa Karnik et al. A case of Lactobacillus jensenii associated native valve endocarditis. 10.1016/j.idcr.2023.e01806. [DOI] [PMC free article] [PubMed]
- 11.Kolar S.L., Liu G.Y. Targeting bacterial abscess formation. EBioMedicine. 2016;12:16–17. doi: 10.1016/j.ebiom.2016.10.017. Epub 2016 Oct 17. PMID: 27765641; PMCID: PMC5078668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zein E.F., Karaa S., Chemaly A., Saidi I., Daou-Chahine W., Rohban R. [Lactobacillus rhamnosus septicemia in a diabetic patient associated with probiotic use: a case report]. (Article in French with English abstract) Ann Biol Clin (Paris) 2008;66(2):195–198. doi: 10.1684/abc.2008.0210. [DOI] [PubMed] [Google Scholar]
- 13.Ledoux D., Labombardi V.J., Karter D. Lactobacillus acidophilus bacteremia after use of a probiotic in a patient with AIDS and Hodgkin’s disease. Int J STD AIDS. 2006;17(4):280–282. doi: 10.1258/095646206776253507. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used in this manuscript is available from the first author on reasonable request. Requests to access this data should be directed to alexandra.christ@meduniwien.ac.at.