Abstract
Objectives
Few panel studies have investigated how different types of mental health (MH) and socio-emotional wellbeing (SEW) outcomes have changed during the pandemic and if their burden has been equally distributed at the population-level. We aimed to examine temporal changes in these outcomes and their socio-ecological predictors using panel data.
Study design
Longitudinal population-based survey with overlapping panels.
Methods
Analyses were carried out using four measurements of data from the Health and Social Survey (April 2020 to April 2021). Participants included Andalusian (Spanish) residents aged 16 years or older who participated in all four measurements (n = 1223). Seven dichotomous MH and SEW outcomes, as well as several socio-ecological predictors informed by a conceptual model, were examined in descriptive and multivariate analyses.
Results
Unadjusted odds of regular/bad perceived mental health (vs. excellent/very good/good), low socio-emotional wellbeing (vs. regular), low happiness (vs. regular), and feeling anxious (vs. not feeling anxious) decreased significantly from the first to the second measurement; however, in the fourth, low socio-emotional wellbeing significantly increased while low optimism decreased. Considering varying coefficients, objectively measured COVID-19 status and self-reported severity levels of the infection were statistically significant. Health status, social support, and household financial difficulty predicted higher adjusted odds in most of the seven assessed outcomes.
Conclusions
Significant temporal variations in MH and SEW outcomes, along with their predictors, were observed during the first year of the pandemic. Some of these outcomes worsened as the pandemic progressed, whereas others improved. Findings also suggest that some individuals such as those experiencing poor health, limited social support, and low socioeconomic status are disproportionately impacted.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-024-19817-8.
Keywords: COVID-19, Mental health, Socio-emotional wellbeing, Panel survey, Inequalities
Introduction
The advent of the novel coronavirus (COVID-19) pandemic has created indisputable urgency to investigate the impact of this unprecedented global crisis on mental health outcomes, [1] as well as to strengthen existing infrastructures and strategies to better promote mental health and wellbeing across socioeconomically and demographically diverse populations [2]. Even before the emergence of this global public health crisis, there were growing demands for governments and decision-makers around the world to prioritize and address the increasing burden of poor mental and socio-emotional wellbeing [3]. The pandemic has undoubtedly further highlighted the global mental health crisis that has been unfolding in recent decades.
Nevertheless, in the new era of COVID-19, opportunities remain to better understand the trajectory of mental health (MH) and socio-emotional wellbeing (SEW) and their underlying social determinants. This is particularly salient when looking into the rapid influx of published research characterized by methodological shortcomings such as data reliant on cross-sectional designs or studies that employed small or selective sampling approaches [4]. For example, a recent systematic review and meta-analysis of 134 cohorts suggests that the pandemic did not significantly exacerbate poor mental health and related disparities, although this review mainly included studies with cross-sectional designs and non-probabilistic samples that are subject to significant bias [5]. In general, there has been increased need for carrying out better-designed studies [4, 6].
Under this purview, studies that leverage panel datasets that consist of multiple observations over time for the same group of individuals may bolster evidence on the impact of COVID-19 on the MH/SEW outcomes of diverse populations. The advantages of this design are well-documented (e.g., enhanced causal inference, better control of unobservable factors, precision in predicting individual outcomes, etc.) [7]. Within the context of COVID-19, panel studies also offer a more robust understanding of the pandemic beyond its characteristics at a specific timepoint given its design allows researchers to better investigate changes in study variables within the same population; the rotating design (where units are replaced/renewed over time) also reduces panelists’ response fatigue and augments researchers’ ability to quickly collect information in real-time (i.e., overcoming limitations of many cross-sectional and longitudinal studies) [8].
Yet, studies employing large-scale panel designs representative of general populations, those seeking to investigate the trajectory of and potential disparities in MH and SEW outcomes throughout the pandemic, are scarce. Panel studies on this topic have primarily focused on examining changes in these outcomes within the early weeks or months of the pandemic [9–12] and oftentimes have only captured two measurement periods [13–17]. Additionally, most panel studies published in empirical literature have examined temporal changes in clinically diagnosable mental illnesses rather than more general measures of MH or SEW [11, 12, 14, 16, 18, 19]. It also appears that no large-scale panel study representative of general populations has compared trends in different types of MH and SEW outcomes, including in Spain [6]. Furthermore, there is an absence of studies that have concurrently examined various socio-ecological factors that predict them, at key phases of the COVID-19 pandemic when COVID-19 cases, hospitalizations, and policy measures were most pronounced and quick to evolve. Filling these gaps may illuminate opportunities to better address pandemic-related health inequities. Thus, the present study aimed to advance this area of research by examining temporal changes in several types of MH and SEW outcomes between April 2020 to April 2021. This twelve-month period is noteworthy to study as it captures the first (and most challenging) year of the pandemic following the first state of alarm— i.e., key phases of the COVID-19 pandemic in Spain and around the world. A secondary aim was to identify the socio-ecological factors that predict these outcomes during each of these critical timepoints.
Methods
Study design
Data were drawn from the Health and Social Survey (ESSA, Encuesta Sanitaria y Social de Andalucía). ESSA is a longitudinal population-based survey with overlapping panels that collected information on the characteristics and the evolution of health and social status during the COVID-19 pandemic among Andalusian residents aged 16 years and older at April-May 2020 (measurement period 1, M1), June-July 2020 (M2), October-November 2020 (M3), and April-May 2021 (M4). These represent four pivotal phases in the first year of the COVID-19 pandemic in the region (Appendix p 1). Andalusia is the most populated (with over 8 million residents) and the second largest of the 17 regions of Spain. As such, this region may be characterized by significant diversity and potential health disparities in MH and SEW status. A corresponding questionnaire was administered to study participants through a computer-assisted telephone interview conducted using the Pl@teA and MobiNet Gandia Integra software, which was piloted before fieldwork. The survey included questions on household and housing characteristics, time use and cohabitation, health and emotional wellbeing, habits and lifestyles, and economic situation and socio-demographic characteristics. A team of 8–12 trained interviewers solely assigned to the study were responsible for data collection. On average, the survey took participants ~ 20 min to complete. The Research Ethics Committee of the Department of Health and Families of the Andalusian Regional Government approved this study (protocol code 10/20). Additional detailed information on ESSA survey administration and study design have been published elsewhere [8].
Using overlapping panel survey data augments our ability to gain a more nuanced understanding of the temporal changes in mental health outcomes and the underlying factors that shape them. In this paper, the study population comprises 1,223 ESSA panelists who participated in all four above mentioned survey measurements. Additional details regarding the ESSA sample selection are also available [20].
Outcomes
There were seven MH and SEW outcomes of interest: (1) self-reported (perceived) mental health; (2) socio-emotional wellbeing; (3) level of happiness; (4) level of optimism; (5) feeling alone; (6) feeling depressed; and (7) feeling anxious. Perceived mental health was assessed via a single-item measure of self-related mental health adapted from a question that is associated with multi-item measures of mental health and that has been widely used in research, [21] including in the Canadian Health Measures Survey [22]. Socio-emotional wellbeing was measured using the validated Socioemotional Well-being Index (SEWBI), a questionnaire capturing a composite indicator and global measure of subjective wellbeing that has been previously validated with data from the 2006 European Social Survey [23]. Individual questions from the validated SEWBI were also used to measure level of happiness, level of optimism, feeling alone, and feeling depressed. Feeling anxious was measured in part by an individual SEWBI question and by asking participants to indicate the extent to which they felt tightness in their chest pain in the past month. How these variables were operationalized is detailed in the Appendix (p 3).
Socio-ecological predictors
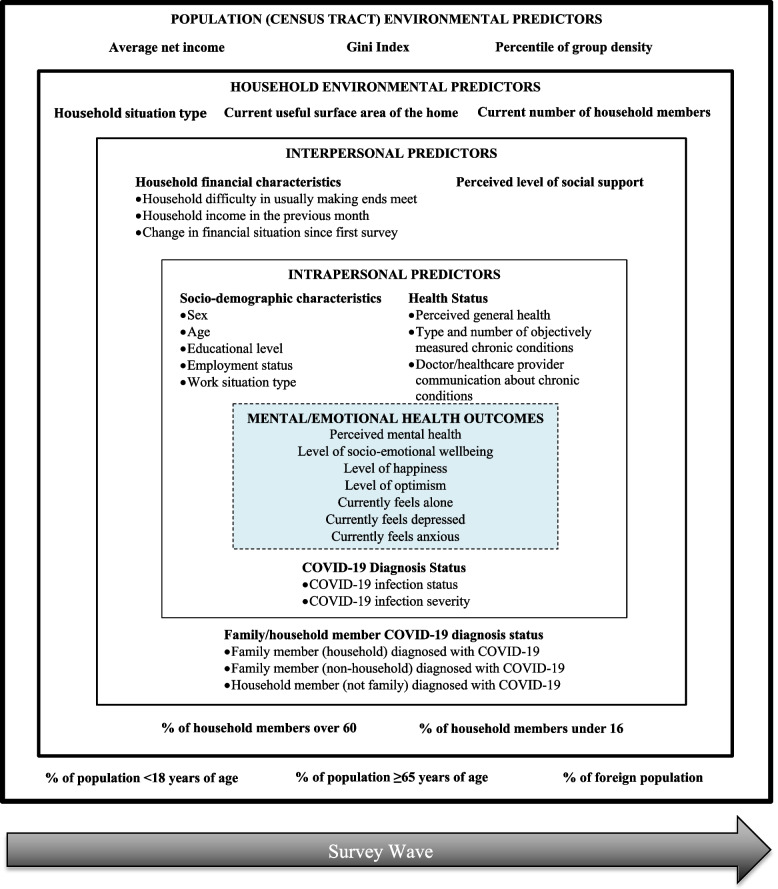
A conceptual model informed by the Social Ecological Model, [24] and existing literature on social determinants of mental health, [25] guided the selection of the predictors in the present study (Fig. 1). Intrapersonal predictors included objectively measured COVID-19 infection status based on official health data sources, self-reported severity of COVID-19 infection, socio-demographic characteristics, and health status. Interpersonal level predictors included social support, family/household member COVID-19 diagnosis status, and household financial characteristics, and household environment predictors. The latter included household situation type, current useful surface area of the home, current number of household members, percentage of household members over 60 years of age, and percentage of household members under 16 years of age. Furthermore, population environment predictors (at the census tract level) included average net income per person, Gini index (i.e., measure of inequality), percentage of population < 18 years of age between 2015 and 2020, percentage of population ≥ 65 years of age between 2015 and 2020, percentage of the foreign population between 2015 and 2020, and percentile of group density. The operationalization of these variables is also detailed in the Appendix (p 5).
Fig. 1.
Conceptual model of the socio-ecological predictors of mental health status during the COVID-19 pandemic. This model illustrates how different factors may shape mental/emotional health outcomes and how these predictors may vary across time during the COVID-19 pandemic. It is informed by existing literature on the social determinants of mental health [25] and the Social Ecologic Model, which highlights how health extends beyond biological factors and is influenced by a collection of subsystems that occur at various levels [24]. Predictors in the present model were selected based study data from the Andalusian Health and Social Survey (ESSA, Encuesta Sanitaria y Social de Andalucía)
Statistical analysis
Descriptive analyses were carried out on all outcome and predictor variables among participants in each of the four survey measurement periods (Table 1). We devised cross-sectional weighting scheme that includes a non-response adjustment based on propensities through eXtreme Gradient Boosting (XGBoost), optimal combination of the samples from the panels involved, and calibration for completing the representativeness of the population at a given measurement. XGBoost is a state-of-the-art machine learning method, [26] one that builds ensembles of decision trees which optimize an objective function via Gradient Tree Boosting [27]. Additional details regarding that ESSA reweighting are described in Castro et al [20]. Analyses were carried out to examine temporal changes in the seven MH and SEW outcomes and their socio-ecological predictors.
Table 1.
Andalusian health and social survey (ESSA, Encuesta Sanitaria Y Social De Andalucía) respondent characteristics by four measurement periods, n = 1,223
| Measurement 1: April-May 2020 | Measurement 2: June-July 2020 | Measurement 3: October-November 2020 | Measurement 4: April-May 2021 | |
|---|---|---|---|---|
| MENTAL HEALTH/SOCIO-EMOTIONAL WELLBEING OUTCOMES | ||||
| Regular/bad perceived mental healtha | 219 (17.9) | 119 (9.7) | 193 (15.8) | 209 (17.1) |
| Low level of socio-emotional wellbeingb | 187 (15.3) | 112 (9.2) | 160 (13.1) | 220 (18.0) |
| Low level of happinessb | 114 (9.3) | 42 (3.4) | 66 (5.4) | 53 (4.3) |
| Low level of optimismb | 240 (19.6) | 225 (18.4) | 221 (18.1) | 186 (15.2) |
| Currently feels alonec | 247 (20.2) | 208 (17.0) | 280 (22.9) | 306 (25) |
| Currently feels depressedc | 622 (50.9) | 435 (35.6) | 514 (42.0) | 516 (42.2) |
| Currently feels anxiousc | 216 (17.7) | 155 (12.7) | 186 (15.2) | 198 (16.2) |
| INTRAPERSONAL LEVEL PREDICTORS | ||||
| COVID-19 diagnosis status | ||||
| Has been infected with COVID-19d | 6 (0.5) | 11 (0.9) | 37 (3.0) | 104 (8.5) |
| Very severe/severe level of COVID-19 infection severitye | 3 (0.2) | 3 (0.2) | 6 (0.5) | 14 (1.1) |
| Socio-demographic characteristics | ||||
| Female sexf | 679 (55.5) | 679 (55.5) | 679 (55.5) | 679 (55.5) |
| Age | ||||
| 16–24 years | 133 (10.9) | 133 (10.9) | 133 (10.9) | 133 (10.9) |
| 25–34 years | 155 (12.7) | 155 (12.7) | 155 (12.7) | 155 (12.7) |
| 35–44 years | 252 (20.6) | 252 (20.6) | 252 (20.6) | 252 (20.6) |
| 45–54 years | 298 (24.4) | 298 (24.4) | 298 (24.4) | 298 (24.4) |
| 55–64 years | 217 (17.7) | 217 (17.7) | 217 (17.7) | 217 (17.7) |
| 65 years or older | 168 (13.7) | 168 (13.7) | 168 (13.7) | 168 (13.7) |
| Educational level | ||||
| Illiterate/primary education not completed | 48 (3.9) | 48 (3.9) | 48 (3.9) | 48 (3.9) |
| Primary or second stage education | 707 (57.8) | 707 (57.8) | 707 (57.8) | 707 (57.8) |
| Bachelor/Postsecondary/Vocational | 137 (11.2) | 137 (11.2) | 137 (11.2) | 137 (11.2) |
| University graduate (own university degree) | 153 (12.5) | 153 (12.5) | 153 (12.5) | 153 (12.5) |
| Masters/specialty/doctoral degree | 178 (14.6) | 178 (14.6) | 178 (14.6) | 178 (14.6) |
| Employment status | ||||
| Salaried full time or ERTE full time | 408 (33.4) | 409 (33.4) | 429 (35.1) | 430 (35.2) |
| Salaried part-time or ERTE part time | 76 (6.2) | 91 (7.4) | 114 (9.3) | 115 (9.4) |
| Entrepreneurs with wage earners or without employees/etc. | 104 (8.5) | 106 (8.7) | 102 (8.3) | 98 (8.0) |
| Unpaid family work/ unemployed/ student/ household/childcare/ volunteer | 371 (30.3) | 349 (28.5) | 338 (27.6) | 335 (27.4) |
| Retired/disabled | 242 (19.8) | 244 (20.0) | 230 (18.8) | 234 (19.1) |
| Other kind of economic inactivity | 20 (1.6) | 21 (1.7) | 10 (0.8) | 10 (0.8) |
| Work situation type | ||||
| Works from home | 159 (13.0) | 157 (12.8) | 40 (3.3) | 36 (2.9) |
| Works away from home | 239 (19.5) | 307 (25.1) | 521 (42.6) | 512 (41.9) |
| Works from home and away from home | 67 (5.5) | 61 (5.0) | 62 (5.1) | 70 (5.7) |
| Other | 119 (9.7) | 79 (6.5) | 35 (2.9) | 36 (2.9) |
| Health Status | ||||
| Fair/bad perceived general healthg | 170 (13.9) | 158 (12.9) | 208 (17.0) | 230 (18.8) |
| Objectively diagnosed with diabetesh | 116 (9.5) | 119 (9.7) | 120 (9.8) | 122 (10.0) |
| Objectively diagnosed with dislipemiah | 77 (6.3) | 79 (6.5) | 80 (6.5) | 81 (6.6) |
| Objectively diagnosed with chronic obstructive pulmonary diseaseh | 55 (4.5) | 56 (4.6) | 56 (4.6) | 57 (4.7) |
| Objectively diagnosed with asthmah | 133 (10.9) | 136 (11.1) | 136 (11.1) | 140 (11.4) |
| Objectively diagnosed with heart failureh | 54 (4.4) | 57 (4.7) | 57 (4.7) | 63 (5.2) |
| Number of objectively diagnosed chronic conditions | ||||
| No conditions | 727 (59.4) | 715 (58.5) | 710 (58.1) | 692 (56.6) |
| One condition | 296 (24.2) | 299 (24.4) | 301 (24.6) | 302 (24.7) |
| Two conditions | 107 (8.7) | 112 (9.2) | 114 (9.3) | 128 (10.5) |
| Three conditions | 56 (4.6) | 59 (4.8) | 58 (4.7) | 57 (4.7) |
| Four or more conditions | 37 (3.0) | 38 (3.1) | 40 (3.3) | 44 (3.6) |
| Has been told by doctor/health professional that currently has hypertensioni | - | 242 (19.8) | 210 (17.2) | 252 (20.6) |
| Has been told by doctor/health professional that currently has chronic paini | - | 341 (27.9) | 340 (27.8) | 320 (26.2) |
| Has been told by doctor/health professional that currently has allergies | - | 272 (22.2) | 221 (18.1) | 261 (21.3) |
| Has been told by doctor/health professional that currently has bad circulationi | - | 160 (13.1) | 148 (12.1) | 136 (11.1) |
| INTERPERSONAL LEVEL PREDICTORS | ||||
| Social Support | ||||
| Perceived level of social support | ||||
| High support | - | 383 (31.3) | 371 (30.3) | 358 (29.3) |
| Intermediate support | - | 391 (32.0) | 405 (33.1) | 454 (37.1) |
| Low support | - | 449 (36.7) | 447 (36.5) | 411 (33.6) |
| Family/household member COVID-19 diagnosis status | ||||
| Family member (household) diagnosed with COVID-19d | 9 (0.7) | 12 (1.0) | 38 (3.1) | 101 (8.3) |
| Family member (non-household) diagnosed with COVID-19d | 116 (9.5) | 93 (7.6) | 252 (20.6) | 394 (32.2) |
| Household member (not family) diagnosed with COVID-19d | 2 (0.2) | 3 (0.2) | 7 (0.6) | 5 (0.4) |
| Household financial characteristics | ||||
| Household experiences difficulty in making ends meetj | 380 (31.1) | 321 (26.2) | 336 (27.5) | 326 (26.7) |
| Household income in the previous month | ||||
| <900 euros | 207 (16.9) | 223 (18.2) | 227 (18.6) | 233 (19.1) |
| 901–1600 euros | 378 (30.9) | 370 (30.3) | 379 (31.0) | 278 (22.7) |
| 1601–3000 euros | 386 (31.6) | 388 (31.7) | 379 (31.0) | 382 (31.2) |
| >3000 euros | 167 (13.7) | 156 (12.8) | 153 (12.5) | 157 (12.8) |
| Change in financial situation since the first survey | ||||
| No change in financial situation | - | 1033 (84.5) | 934 (76.4) | 962 (78.7) |
| Financial situation got better | - | 83 (6.8) | 106 (8.7) | 132 (10.8) |
| Financial situation got worse | - | 105 (8.6) | 177 (14.5) | 122 (10.0) |
| HOUSEHOLD ENVIRONMENT PREDICTORS | ||||
| Household situation type | ||||
| One person household | 81 (6.6) | 79 (6.5) | 87 (7.1) | 88 (7.2) |
| Single parent that lives with a child | 86 (7.0) | 91 (7.4) | 104 (8.5) | 112 (9.2) |
| Couple without children who share a home | 234 (19.1) | 230 (18.8) | 229 (18.7) | 229 (18.7) |
| Couple with children who share a home | 666 (54.5) | 669 (54.7) | 643 (52.6) | 626 (51.2) |
| Other type of housing situation | 156 (12.8) | 154 (12.6) | 160 (13.1) | 168 (13.7) |
| Current useful surface area of the home | ||||
| <46 m2 | 13 (1.1) | 12 (1.0) | 13 (1.1) | 16 (1.3) |
| 46-75m2 | 233 (19.1) | 233 (19.1) | 235 (19.2) | 234 (19.1) |
| 76-120m2 | 596 (48.7) | 598 (48.9) | 599 (49.0) | 596 (48.7) |
| >120m2 | 271 (22.2) | 272 (22.2) | 269 (22.0) | 269 (22.0) |
| Current number of household members, including self | ||||
| 1 member | 81 (6.6) | 79 (6.5) | 88 (7.2) | 91 (7.4) |
| 2 members | 313 (25.6) | 311 (25.4) | 314 (25.7) | 318 (26.0) |
| 3 members | 311 (25.4) | 311 (25.4) | 312 (25.5) | 312 (25.5) |
| 4 members | 386 (31.6) | 389 (31.8) | 384 (31.4) | 380 (31.1) |
| 5 members | 100 (8.2) | 102 (8.3) | 97 (7.9) | 93 (7.6) |
| 6 or more members | 32 (2.6) | 30 (2.5) | 26 (2.1) | 28 (2.3) |
| % of household members over 60 | ||||
| Quartile 1 | 0.25 | 0.25 | 0.25 | 0.25 |
| Quartile 3 | 0.50 | 0.50 | 0.50 | 0.50 |
| Mean [standard deviation] | 0.46 [0.27] | 0.46 [0.27] | 0.47 [0.27] | 0.47 [0.27] |
| Median [interquartile range] | 0.33 [0.25] | 0.33 [0.25] | 0.33 [0.25] | 0.33 [0.25] |
| % household members under 16 | ||||
| Quartile 1 | 0.33 | 0.33 | 0.33 | 0.33 |
| Quartile 3 | 0.67 | 0.67 | 0.67 | 0.67 |
| Mean [standard deviation] | 0.51 [0.22] | 0.51 [0.22] | 0.52 [0.22] | 0.52 [0.22] |
| Median [interquartile range] | 0.50 [0.33] | 0.50 [0.33] | 0.50 [0.33] | 0.50 [0.33] |
| POPULATION ENVIRONMENT PREDICTORS | ||||
| Average net income per person | ||||
| Quartile 1 | 8103.83 | 8103.83 | 8103.83 | 8103.83 |
| Quartile 3 | 11084.33 | 11084.33 | 11084.33 | 11084.33 |
| Mean [standard deviation] | 9991.33 [2931.65] | 9991.33 [2931.65] | 9991.33 [2931.65] | 9991.33 [2931.65] |
| Median [interquartile range] | 9213.67 [2980.50] | 9213.67 [2980.50] | 9213.67 [2980.50] | 9213.67 [2980.50] |
| Gini Index | ||||
| Quartile 1 | 28.42 | 28.42 | 28.42 | 28.42 |
| Quartile 3 | 32.96 | 32.96 | 32.96 | 32.96 |
| Mean [standard deviation] | 30.94 [3.81] | 30.94 [3.81] | 30.94 [3.81] | 30.94 [3.81] |
| Median [interquartile range] | 30.47 [4.54] | 30.47 [4.54] | 30.47 [4.54] | 30.47 [4.54] |
| % of population under 18 years of age (2015–2020) | ||||
| Quartile 1 | 15.5 | 15.5 | 15.5 | 15.5 |
| Quartile 3 | 21.37 | 21.37 | 21.37 | 21.37 |
| Mean [standard deviation] | 18.58 [4.56] | 18.58 [4.56] | 18.58 [4.56] | 18.58 [4.56] |
| Median [interquartile range] | 17.95 [5.87] | 17.95 [5.87] | 17.95 [5.87] | 17.95 [5.87] |
| % of population aged 65 and over (2015–2020) | ||||
| Quartile 1 | 12.4 | 12.4 | 12.4 | 12.4 |
| Quartile 3 | 22.12 | 22.12 | 22.12 | 22.12 |
| Mean [standard deviation] | 17.43 [6.83] | 17.43 [6.83] | 17.43 [6.83] | 17.43 [6.83] |
| Median [interquartile range] | 17.35 [9.72] | 17.35 [9.72] | 17.35 [9.72] | 17.35 [9.72] |
| % of foreign population (2015–2020) | ||||
| Quartile 1 | 1.87 | 1.87 | 1.87 | 1.87 |
| Quartile 3 | 7.75 | 7.75 | 7.75 | 7.75 |
| Mean [standard deviation] | 6.88 [9.02] | 6.88 [9.02] | 6.88 [9.02] | 6.88 [9.02] |
| Median [interquartile range] | 3.63 [5.88] | 3.63 [5.88] | 3.63 [5.88] | 3.63 [5.88] |
| Percentile of group density | ||||
| Quartile 1 | 1262.64 | 1262.64 | 1262.64 | 1262.64 |
| Quartile 3 | 15776.00 | 15776.00 | 15776.00 | 15776.00 |
| Mean [standard deviation] | 11451.31 [13627.59] | 11451.31 [13627.59] | 11451.31 [13627.59] | 11451.31 [13627.59] |
| Median [interquartile range] | 7411.32 [14513.37] | 7411.32 [14513.37] | 7411.32 [14513.37] | 7411.32 [14513.37] |
Note: Data are n (%), unless otherwise indicated. All data are weighted except for the variable ‘social support.’ Percentages do not account missing responses and may not add up to 100% due to rounding. ERTE Expediente de Regulación Temporal de Empleo (i.e., a record of temporary employment regulation which is a labor procedure in Spain that permits companies to suspend or reduce workers’ contracts)
aDichotomous variable, results for excellent/very good/good not shown
bDichotomous variable, results for normal socio-emotional wellbeing/happiness/optimism not shown
cDichotomous variable, results for currently does not feel alone/depressed/anxious not shown
dDichotomous variable, results for has not been infected/diagnosed with COVID-19 not shown
eDichotomous variable, results for mild/very mild COVID-19 level of severity not shown
fDichotomous variable, results for male sex not shown
gDichotomous variable, results for excellent/very good/good not shown
hDichotomous variable, results for not objectively diagnosed not shown
iDichotomous variable, results for has not been told not shown
jDichotomous variable, results for does not experience difficulty not shown
On the other hand, we estimated the internal consistency of the Socioemotional Well-being Index (SEWBI), through Cronbach’s alpha for the individual questions that compose it (i.e., level of happiness, level of optimism, feeling alone, feeling anxious and feeling depressed). Specifically, we estimated Cronbach’s alpha equal to 0.760, i.e. a high level of reliability.
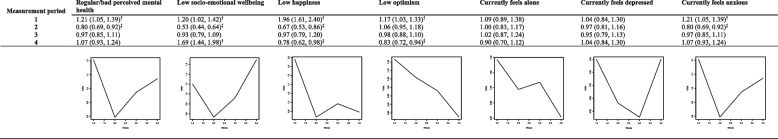
Unadjusted temporal changes in each of these seven outcomes are shown in Table 2. They were assessed by generalized linear mixed models (GLMM) with a variable response with link zero-inflated binomial (i.e., equivalent to logistic regression). This link allowed for the presence of heteroskedasticity in the response variable. We included several random effects in the models. First, we included random effects focused on unobserved confounding. These random effects sought to capture individual heterogeneity— i.e., unobserved confounders, specific to the subject and invariant between the survey waves, which may influence the probability that the subject declares the occurrence of the outcome. Second, we included random effects capturing the evolution of the probability over time and the fact that we had four measurements for each of the subjects. It should be noted that we allowed for this evolution to be non-linear. Furthermore, we also included random effects to control spatial dependency and to consider that subjects who reside nearby show more similar values of the outcome variables than subjects who reside far away. More details on these random effects can be found in the Appendix (p 10). We re-ran these models with all the predictor variables of interest simultaneously to assess predictors of the seven mental and emotional health outcomes (Table 3).
Table 2.
Unadjusted fixed effect odds ratios and 95% credibility intervals for seven mental health and socio-emotional wellbeing outcomes at four measurement periods during the COVID-19 pandemic, April 2020 to April 2021 (n=1223)
Data from the Andalusian Health and Social Survey (Spanish Acronym ESSA, Encuesta Sanitaria y Social de Andalucía) were analyzed in measurement period 1 (April-May 2020), period 2 (June-July 2020), period 3 (October-November 2020), and period 4 (April-May 2021). Numbers reported in this table correspond to an unadjusted Bayesian fixed effects model
†The 90% credibility interval did not contain the unity and indicated higher odds of poor mental/socio-emotional wellbeing during the measurement period
‡The 95% credibility interval did not contain the unity and indicated lower odds of poor mental health/socio-emotional wellbeing during the measurement period
Table 3.
Predictors of seven mental health and socio-emotional wellbeing outcomes during the COVID-19 pandemic, April 2020 to April 2021 (n = 1223)
| Regular/bad perceived mental health | Low socio-emotional wellbeing | Low happiness | Low optimism | Currently feels alone | Currently feels depressed | Currently feels anxious | |
|---|---|---|---|---|---|---|---|
| INTRAPERSONAL LEVEL PREDICTORS | |||||||
| COVID-19 Infection Status | |||||||
| Has been infected (ref = not infected) | 0.91 (0.46, 1.79) | 0.81 (0.34, 1.99) | 3.57 (0.08, 159.85) | 0.92 (0.46, 1.83) | 1.96 (0.00, 1.21E + 04) | 0.68 (0.00, 176.38) | 2.19 (1.27, 3.78)b |
| Very severe/severe level of infection (ref = very mild/mild) | 1.42 (0.50, 4.04) | 0.78 (0.25, 2.37) | 1.35 (0.00, 3.65E + 03) | 1.99 (0.71, 5.62)a | 2.80 (0.00, 4.97E + 05) | 1.02 (0.00, 451.78) | 1.56 (0.63, 3.88) |
| Socio-demographic characteristics | |||||||
| Female sex (ref = male) | 1.92 (1.37, 2.72)b | 2.56 (1.79, 3.69)b | 0.10 (0.00, 51.24) | 0.87 (0.66, 1.15) | 0.30 (0.01, 11.88) | 1.52 (0.01, 305.79) | 2.64 (1.92, 3.65)b |
| Age (ref = 16–24 years) | |||||||
| 25–34 years | 0.38 (0.21, 0.68)b | 0.44 (0.24, 0.81)b | 20.39 (0.02, 2.30E + 04) | 0.95 (0.58, 1.57) | 0.19 (0.00, 28.66) | 1.02 (0.00, 357.75) | 0.53 (0.31, 0.93)b |
| 35–44 years | 0.88 (0.53, 1.45) | 1.91 (1.15, 3.19)b | 0.12 (0.01, 2.26)a | 1.36 (0.89, 2.09)a | 9.99 (0.05, 1.92E + 03) | 1.01 (0.00, 303.76) | 1.16 (0.72, 1.88) |
| 45–54 years | 0.84 (0.54, 1.32) | 0.62 (0.39, 0.97)b | 0.04 (0.00, 1.56)b | 0.87 (0.61, 1.26) | 0.25 (0.00, 257.34) | 0.89 (0.00, 309.44) | 1.05 (0.69, 1.58) |
| 55–64 years | 1.53 (1.02, 2.29)b | 1.27 (0.84, 1.91) | 5.55 (0.20, 160.41) | 1.08 (0.77, 1.50) | 0.07 (0.00, 33.94) | 1.12 (0.00, 400.64) | 1.12 (0.78, 1.62) |
| 65 or + years | 1.19 (0.84, 1.68) | 1.30 (0.91, 1.85)a | 0.07 (0.00, 7.07)a | 0.91 (0.68, 1.22) | 0.57 (0.03, 12.90) | 1.11 (0.00, 350.29) | 1.11 (0.81, 1.52) |
| Educational level (ref = illiterate/primary not completed) | |||||||
| Primary or second stage education | 0.60 (0.34, 1.08)b | 2.05 (1.09, 3.86)b | 1.92 (0.07, 52.77) | 2.26 (1.35, 3.79)b | 0.37 (0.00, 1.43E + 03) | 0.81 (0.00, 319.71) | 0.88 (0.51, 1.53) |
| Bachelor/Postsecondary/Vocational | 1.31 (0.84, 2.03) | 0.78 (0.48, 1.27) | 0.86 (0.04, 16.87) | 1.07 (0.72, 1.60) | 6.07 (0.02, 1.73E + 03) | 0.86 (0.00, 307.92) | 1.32 (0.86, 2.03)a |
| University graduate (own university degree) | 0.88 (0.60, 1.28) | 0.95 (0.64, 1.40) | 1.13 (0.12, 10.64) | 0.94 (0.67, 1.30) | 0.93 (0.02, 37.12) | 1.32 (0.00, 396.16) | 1.25 (0.87, 1.81) |
| Masters/specialty/doctoral degree | 0.92 (0.67, 1.25) | 0.82 (0.60, 1.13) | 0.61 (0.14, 2.68) | 1.08 (0.83, 1.40) | 0.52 (0.01, 22.41) | 0.86 (0.00, 242.87) | 1.08 (0.81, 1.45) |
| Employment status (ref = Salaried full time or ERTE full time) | |||||||
| Salaried part-time or ERTE part time | 1.47 (0.74, 2.94) | 0.88 (0.44, 1.75) | 0.81 (0.04, 15.68) | 1.08 (0.59, 1.97) | 0.00 (0.00, 1.93E + 03) | 1.08 (0.00, 443.26) | 0.55 (0.29, 1.04)b |
| Entrepreneurs with wage earners or without employees/etc. | 1.41 (0.77, 2.55) | 1.12 (0.62, 2.02) | 13.81 (0.14, 1.45E + 03) | 0.77 (0.46, 1.30) | 0.00 (0.00, 2.65E + 03) | 0.79 (0.00, 312.35) | 1.05 (0.61, 1.82) |
| Unpaid family work/unemployed/student/household/ childcare/volunteer | 0.79 (0.46, 1.35) | 2.20 (1.30, 3.74)b | 0.44 (0.03, 7.42) | 1.29 (0.81, 2.05) | 0.01 (0.00, 2.50E + 04) | 0.89 (0.00, 324.00) | 2.07 (1.26, 3.40)b |
| Retired/disabled | 1.00 (0.63, 1.57) | 1.27 (0.81, 1.98) | 1.75 (0.15, 20.70) | 1.83 (1.25, 2.70)b | 0.03 (0.00, 38.65) | 1.09 (0.00, 349.28) | 1.12 (0.74, 1.70) |
| Other kind of economic inactivity | 1.11 (0.72, 1.72) | 1.18 (0.78, 1.78) | 24.88 (0.12, 5.59E + 03)a | 1.02 (0.72, 1.45) | 0.51 (0.00, 558.81) | 1.07 (0.00, 284.32) | 1.24 (0.85, 1.83) |
| Work situation type (ref = works from home) | |||||||
| Work away from home | 0.78 (0.48, 1.29) | 1.20 (0.75, 1.94) | 5.75 (0.20, 164.36) | 1.90 (1.29, 2.81)b | 0.03 (0.00, 29.81) | 0.98 (0.00, 425.46) | 0.99 (0.65, 1.49) |
| Work from home and away from home | 0.59 (0.37, 0.94)b | 1.13 (0.70, 1.83) | 0.51 (0.01, 49.43) | 1.36 (0.93, 2.00)a | 1.47 (0.00, 487.86) | 0.93 (0.00, 380.72) | 0.87 (0.59, 1.30) |
| Other | 0.83 (0.53, 1.32) | 1.27 (0.78, 2.06) | 0.98 (0.01, 157.29) | 1.59 (1.08, 2.33)b | 4.18 (0.01, 1.55E + 03) | 1.14 (0.00, 446.97) | 0.70 (0.47, 1.04)b |
| Health Status | |||||||
| Fair/bad perceived general health (ref = excellent/very good/good perceived general health) | 5.56 (4.47, 6.92)b | 4.18 (3.32, 5.30)b | 61.03 (0.08, 5.14E + 04)a | 2.12 (1.74, 2.60)b | 450.82 (0.44, 4.79E + 05)b | 1.24 (0.01, 238.61) | 2.73 (2.21, 3.38)b |
| Objectively diagnosed with diabetes (ref = not diagnosed) | 0.46 (0.24, 0.90)b | 0.43 (0.21, 0.86)b | 7.55 (0.00, 4.13E + 05) | 0.87 (0.50, 1.52) | 0.58 (0.00, 4.04E + 03) | 0.81 (0.00, 160.37) | 0.72 (0.39, 1.33) |
| Objectively diagnosed with dislipemia (ref = not diagnosed) | 0.93 (0.43, 1.99) | 0.84 (0.38, 1.85) | 0.00 (0.00, 1.05E + 06) | 1.00 (0.53, 1.89) | 0.00 (0.00, 51.63) | 0.74 (0.00, 167.34) | 0.55 (0.27, 1.13)b |
| Objectively diagnosed with chronic obstructive pulmonary disease (ref = not diagnosed) | 0.92 (0.54, 1.57) | 0.70 (0.41, 1.22)a | 0.01 (0.00, 99.25) | 1.00 (0.63, 1.60) | 0.00 (0.00, 1.97E + 03) | 0.72 (0.00, 163.99) | 0.75 (0.44, 1.27) |
| Objectively diagnosed with asthma (ref = not diagnosed) | 0.50 (0.33, 0.74)b | 0.50 (0.33, 0.74)b | 0.02 (0.00, 20.26)a | 1.01 (0.72, 1.41) | 0.11 (0.00, 31.82) | 0.72 (0.00, 161.75) | 0.60 (0.41, 0.87)b |
| Objectively diagnosed with heart failure (ref = not diagnosed) | 0.42 (0.24, 0.73)b | 0.39 (0.22, 0.69)b | 0.06 (0.00, 43.17) | 0.72 (0.45, 1.16)a | 0.00 (0.00, 62.96)a | 0.67 (0.00, 169.98) | 0.49 (0.28, 0.85)b |
| Number of objectively diagnosed chronic conditions (ref = none) | |||||||
| One condition | 8.94 (3.59, 22.41)b | 12.08 (4.73, 31.35)b | 6.86E + 03 (0.00, 3.16E + 10)a | 3.10 (1.40, 6.93)b | 3.20E + 08 (0.01, 1.62E + 19)a | 0.95 (0.00, 310.08) | 3.73 (1.56, 8.91)b |
| Two conditions | 1.01 (0.60, 1.72) | 1.66 (0.97, 2.83)b | 13.24 (0.01, 2.75E + 04) | 1.43 (0.91, 2.25)a | 751.63 (0.01, 7.81E + 07) | 0.96 (0.00, 311.78) | 0.80 (0.47, 1.34) |
| Three conditions | 1.57 (0.94, 2.62)b | 1.86 (1.08, 3.21)b | 10.53 (0.05, 2.49E + 03) | 0.94 (0.61, 1.44) | 47.14 (0.01, 4.48E + 05) | 1.14 (0.00, 342.67) | 1.49 (0.89, 2.49)a |
| Four or more conditions | 1.29 (0.81, 2.07) | 1.36 (0.83, 2.24) | 2.88 (0.27, 30.48) | 0.98 (0.65, 1.48) | 10.76 (0.07, 1.68E + 03) | 0.96 (0.00, 280.62) | 1.49 (0.94, 2.35)b |
| Told by doctor/health professional that currently has hypertension (ref = has not been told) | 0.95 (0.72, 1.26) | 1.04 (0.78, 1.41) | 2.09 (0.39, 11.30) | 0.89 (0.70, 1.14) | 3.85 (0.11, 138.35) | 0.97 (0.00, 229.88) | 1.04 (0.80, 1.35) |
| Told by doctor/health professional that currently has chronic pain (ref = has not been told) | 1.34 (1.08, 1.66)b | 1.43 (1.14, 1.79)b | 0.87 (0.23, 3.37) | 1.34 (1.11, 1.61)b | 1.74 (0.04, 74.31) | 0.96 (0.00, 216.52) | 1.40 (1.15, 1.72)b |
| Told by doctor/health professional that currently has allergies (ref = has not been told) | 1.27 (1.00, 1.62)b | 1.32 (1.04, 1.67)b | 1.18 (0.33, 4.17) | 1.29 (1.06, 1.58)b | 2.12 (0.10, 45.92) | 0.88 (0.00, 200.11) | 1.06 (0.85, 1.31) |
| Currently told by doctor/health professional that currently has bad circulation (ref = has not been told) | 1.20 (0.91, 1.58)a | 1.26 (0.95, 1.67)b | 82.29 (0.03, 3.00E + 05) | 1.26 (0.99, 1.61)b | 0.93 (0.01, 78.93) | 0.95 (0.00, 220.64) | 1.24 (0.97, 1.59)b |
| INTERPERSONAL LEVEL PREDICTORS | |||||||
| Social Support | |||||||
| Perceived level of social support (ref = high support) | |||||||
| Intermediate support | 2.20 (1.69, 2.86)b | 3.27 (2.45, 4.37)b | 8.42 (0.31, 238.26)a | 2.19 (1.77, 2.72)b | 4.43 (0.21, 95.16) | 1.17 (0.00, 346.51) | 1.52 (1.20, 1.92)b |
| Low support | 1.19 (0.94, 1.51)a | 1.09 (0.85, 1.41) | 7.38 (0.29, 193.24)a | 1.07 (0.88, 1.30) | 4.66 (0.09, 237.11) | 0.97 (0.00, 288.50) | 1.04 (0.84, 1.29) |
| Family/household member COVID-19 diagnosis status | |||||||
| Family member (household) diagnosed with COVID-19 (ref = not diagnosed) | 1.36 (0.83, 2.22)a | 1.40 (0.87, 2.24)a | 2.23 (0.07, 71.50) | 1.06 (0.69, 1.64) | 0.70 (0.00, 339.98) | 0.68 (0.00, 173.11) | 1.28 (0.83, 1.99) |
| Family member (non-household) diagnosed with COVID-19 (ref = not diagnosed) | 1.21 (0.97, 1.51)b | 1.20 (0.95, 1.51)a | 3.15 (0.12, 88.49) | 1.09 (0.90, 1.32) | 0.82 (0.02, 42.45) | 0.80 (0.00, 152.30) | 1.13 (0.92, 1.39) |
| Household member (not family) diagnosed with COVID-19 (ref = not diagnosed) | 1.29 (0.39, 4.28) | 0.83 (0.16, 4.18) | 0.00 (0.00, 2.14E + 06) | 0.00 (0.00, 0.00)b | 0.01 (0.00, 2.67E + 08) | 0.64 (0.00, 191.62) | 1.05 (0.26, 4.26) |
| Household financial characteristics | |||||||
| Household difficulty in making ends meet (ref = experiences no difficulty) | |||||||
| Experiences difficulty | 1.25 (1.02, 1.54)b | 1.59 (1.29, 1.97)b | 2.80 (0.71, 11.10)a | 1.84 (1.54, 2.20)b | 1.28 (0.06, 29.31) | 1.12 (0.01, 212.86) | 1.70 (1.40, 2.07)b |
| Household income in the previous month (ref = < 900 euros) | |||||||
| 901–1600 euros | 0.72 (0.44, 1.15)a | 0.61 (0.38, 0.99)b | 0.04 (0.00, 490.77) | 1.00 (0.68, 1.47) | 0.18 (0.00, 16.03) | 0.73 (0.00, 271.82) | 0.75 (0.49, 1.16)a |
| 1601–3000 euros | 0.85 (0.61, 1.19) | 1.01 (0.72, 1.41) | 0.87 (0.19, 3.98) | 0.88 (0.67, 1.15) | 9.07 (0.22, 381.26) | 0.99 (0.00, 284.33) | 1.02 (0.75, 1.38) |
| >3000 euros | 1.02 (0.78, 1.33) | 1.23 (0.94, 1.62)a | 0.51 (0.05, 4.94) | 1.20 (0.96, 1.49)a | 0.75 (0.04, 15.67) | 1.09 (0.00, 306.36) | 1.12 (0.87, 1.43) |
| Change in financial situation since the first survey (ref = no change) | |||||||
| Financial situation got better | 1.70 (1.29, 2.23b | 1.84 (1.41, 2.41)b | 4.61 (0.32, 67.15) | 1.74 (1.39, 2.17)b | 16.93 (0.08, 3.42E + 03) | 0.80 (0.00, 191.28) | 1.65 (1.29, 2.12)b |
| Financial situation got worse | 1.49 (0.97, 2.28)b | 1.97 (1.27, 3.07)b | 0.84 (0.05, 13.47) | 1.91 (1.33, 2.75)b | 126.83 (0.09, 1.93E + 05)a | 1.23 (0.00, 486.61) | 1.24 (0.87, 1.78) |
| HOUSEHOLD ENVIRONMENT PREDICTORS | |||||||
| Household situation type (ref = one person household) | |||||||
| Single parent that lives with a child | 1.01 (0.32, 3.17) | 0.55 (0.17, 1.75) | 0.36 (0.00, 372.08) | 1.46 (0.49, 4.34) | 0.03 (0.00, 1.39E + 04) | 1.06 (0.00, 357.93) | 0.46 (0.12, 1.73) |
| Couple without children who share a home | 1.01 (0.34, 3.00) | 1.42 (0.46, 4.41) | 5.19 (0.01, 3.87E + 03) | 0.65 (0.23, 1.80) | 10.80 (0.00, 8.12E + 09) | 0.92 (0.00, 322.16) | 1.21 (0.36, 4.07) |
| Couple with children who share a home | 1.36 (0.68, 2.72) | 0.78 (0.39, 1.59) | 0.43 (0.00, 49.35) | 1.39 (0.73, 2.65) | 3.45 (0.00, 1.11E + 05) | 0.85 (0.00, 227.08) | 0.87 (0.41, 1.83) |
| Other type of housing situation | 1.14 (0.64, 2.02) | 0.84 (0.47, 1.49) | 3.71 (0.13, 108.13) | 0.86 (0.52, 1.41) | 2.61 (0.00, 2.67E + 03) | 0.82 (0.00, 264.37) | 1.71 (0.97, 3.00)b |
| Current useful surface area of the home (ref = < 46 m2) | |||||||
| 46-75m2 | 0.57 (0.27, 1.22)a | 1.16 (0.53, 2.52) | 0.00 (0.00, 0.78)b | 1.08 (0.53, 2.18) | 0.66 (0.00, 678.10) | 1.05 (0.00, 442.29) | 0.88 (0.42, 1.84) |
| 76-120m2 | 1.24 (0.70, 2.22) | 0.83 (0.46, 1.50) | 530.09 (0.18, 1.72E + 06)b | 0.87 (0.51, 1.49) | 0.77 (0.00, 316.10) | 0.76 (0.00, 265.17) | 0.69 (0.40, 1.22)a |
| >120m2 | 0.98 (0.68, 1.41) | 1.01 (0.70, 1.47) | 0.07 (0.00, 4.04)a | 1.06 (0.77, 1.47) | 3.15 (0.10, 104.06) | 0.92 (0.00, 209.46) | 1.08 (0.77, 1.52) |
| Current number of household members, including self (ref = 1 member) | |||||||
| 2 members | 0.87 (0.23, 3.26) | 0.69 (0.18, 2.66) | 0.02 (0.00, 22.22) | 0.43 (0.13, 1.48)a | 0.01 (0.00, 3.18E + 05) | 0.94 (0.00, 360.55) | 5.55 (1.30, 23.77)b |
| 3 members | 0.51 (0.16, 1.65) | 1.11 (0.34, 3.61) | 8.48 (0.01, 8.17E + 03) | 0.78 (0.26, 2.29) | 1.41 (0.00, 6.53E + 05) | 0.86 (0.00, 301.33) | 0.61 (0.17, 2.16) |
| 4 members | 0.90 (0.37, 2.16) | 1.20 (0.48, 2.97) | 0.49 (0.00, 117.50) | 0.61 (0.27, 1.38) | 0.01 (0.00, 430.59) | 0.97 (0.00, 335.57) | 1.70 (0.67, 4.32) |
| 5 members | 1.30 (0.70, 2.41) | 1.25 (0.67, 2.35) | 0.13 (0.00, 27.98) | 0.99 (0.58, 1.70) | 4.49 (0.00, 2.69E + 04) | 1.09 (0.00, 357.25) | 1.19 (0.65, 2.17) |
| 6 or more members | 0.79 (0.55, 1.15)a | 1.08 (0.74, 1.59) | 0.24 (0.00, 18.43) | 1.01 (0.74, 1.39) | 0.72 (0.00, 177.54) | 1.18 (0.00, 344.30) | 0.91 (0.64, 1.30) |
| % of household members over 60 | 0.50 (0.28, 0.89)b | 0.69 (0.39, 1.23)a | 2.32 (0.16, 32.90) | 0.89 (0.55, 1.46) | 0.00 (0.00, 28.61)a | 1.26 (0.00, 424.27) | 0.96 (0.55, 1.68) |
| % of household members under 16 | 2.04 (0.79, 5.24)a | 2.62 (1.02, 6.81)b | 2.16 (0.02, 195.77) | 2.04 (0.91, 4.54)b | 22.86 (0.01, 4.63E + 04) | 1.44 (0.01, 422.59) | 2.66 (1.07, 6.58)b |
| POPULATION ENVIRONMENT PREDICTORS | |||||||
| Average net income per person (ref = Quartile 1) | |||||||
| Quartile 2 | 1.00 (0.70, 1.42) | 1.20 (0.84, 1.71) | 1.74 (0.29, 10.36) | 1.32 (0.98, 1.77)b | 0.94 (0.02, 51.88) | 1.05 (0.00, 285.72) | 1.08 (0.78, 1.49) |
| Quartile 3 | 1.16 (0.85, 1.60) | 1.16 (0.84, 1.60) | 3.75 (0.04, 399.89) | 1.04 (0.80, 1.36) | 0.64 (0.04, 10.56) | 1.03 (0.00, 288.74) | 1.18 (0.89, 1.59) |
| Quartile 4 | 0.82 (0.60, 1.12)a | 1.18 (0.86, 1.63) | 0.14 (0.00, 31.33) | 1.04 (0.80, 1.36) | 0.16 (0.01, 4.98) | 1.02 (0.00, 302.46) | 0.89 (0.66, 1.18) |
| Gini index (ref = Quartile 1) | |||||||
| Quartile 2 | 0.92 (0.63, 1.34) | 1.35 (0.92, 1.97)a | 0.84 (0.14, 4.90) | 0.79 (0.58, 1.09)a | 1.85 (0.03, 123.43) | 0.98 (0.00, 282.28) | 1.15 (0.82, 1.62) |
| Quartile 3 | 0.99 (0.72, 1.37) | 1.28 (0.92, 1.77)a | 3.49 (0.25, 50.82) | 0.91 (0.69, 1.19) | 7.23 (0.07, 790.80) | 1.01 (0.00, 287.02) | 1.08 (0.80, 1.45) |
| Quartile 4 | 1.01 (0.74, 1.37) | 1.14 (0.83, 1.57) | 0.49 (0.12, 2.04) | 1.08 (0.83, 1.40) | 3.05 (0.09, 103.33) | 1.05 (0.00, 307.16) | 1.30 (0.98, 1.73)b |
| % of population under 18 years of age 2015–2020 | 1.03 (0.99, 1.06)a | 1.00 (0.96, 1.03) | 0.81 (0.58, 1.13)a | 1.02 (0.99, 1.04) | 1.07 (0.79, 1.43) | 1.11 (0.66, 1.87) | 1.02 (0.98, 1.05) |
| % of population aged 65 and over 2015–2020 | 1.03 (1.00, 1.06) | 1.01 (0.98, 1.03) | 0.90 (0.74, 1.09) | 1.01 (0.99, 1.03) | 0.97 (0.73, 1.27) | 1.10 (0.69, 1.75) | 1.00 (0.97, 1.02) |
| % of foreign population 2015–2020 | 1.01 (0.99, 1.03) | 1.01 (0.99, 1.03) | 1.09 (0.86, 1.37) | 1.00 (0.99, 1.02) | 1.11 (0.96, 1.29)a | 1.08 (0.44, 2.68) | 1.01 (0.99, 1.03)a |
| Percentile of group density (ref = Quartile 1) | |||||||
| Quartile 2 | 0.84 (0.60, 1.17) | 1.03 (0.72, 1.46) | 0.09 (0.00, 50.86) | 0.88 (0.66, 1.16) | 3.02 (0.06, 151.80) | 1.10 (0.00, 342.60) | 1.06 (0.78, 1.44) |
| Quartile 3 | 1.04 (0.75, 1.44) | 0.95 (0.68, 1.32) | 0.60 (0.03, 13.66) | 0.99 (0.75, 1.30) | 0.34 (0.02, 5.68) | 0.97 (0.00, 278.13) | 1.14 (0.85, 1.54) |
| Quartile 4 | 1.13 (0.82, 1.55) | 1.40 (1.02, 1.92)b | 3.61 (0.06, 227.40) | 0.98 (0.76, 1.27) | 2.34 (0.12, 45.20) | 1.01 (0.00, 275.92) | 0.86 (0.64, 1.15) |
Adjusted fixed effect odds ratios and 95% credibility intervals for each of the seven mental health and socio-emotional wellbeing outcomes. Data from the Andalusian Health and Social Survey (Spanish Acronym ESSA, Encuesta Sanitaria y Social de Andalucía) were analyzed in measurement period 1 (April-May 2020), period 2 (June-July 2020), period 3 (October-November 2020), and period 4 (April-May 2021). ERTE Expediente de Regulación Temporal de Empleo (i.e., a record of temporary employment regulation which is a labor procedure in Spain that permits companies to suspend or reduce workers’ contracts)
aThe 90% Credibility Interval did not contain the unity
bThe 95% Credibility Interval did not contain the unity
The impact of COVID-19 infection status, both objectively measured COVID-19 status based on hospital records and self-reported infection severity, may have varied over time based on the probability of occurrence of each of the outcomes. Thus, the adjusted (predictor) models shown in Table 3 included other structured random effects associated with each of the COVID-19 variables (Table 4). All data was managed using R (version 4.3.1) and STATA version 14.1 (StataCorp LP, College Station, Texas, USA). All analyses were carried out using the free software R (version 4.3.1), through the INLA package. All inferences made following a Bayesian perspective, using the INLA approach, are detailed elsewhere (Appendix p 10). In addition to the parameters of interest, we estimate their 95% and 90% credibility intervals. A credibility interval contains the true value of the parameter with a given probability (95% or 90%, in our case).
Table 4.
Varying coefficients and 95% credibility interval for seven mental health and socio-emotional health outcomes by objectively measured COVID-19 diagnosis status and self-reported COVID-19 level of severity at four measurement periods during the COVID-19 pandemic, April 2020 to April 2021 (n = 1223)
| Regular/bad perceived mental health | Low socio-emotional wellbeing | Low happiness | Low optimism | Currently feels alone | Currently feels depressed | Currently feels anxious | |
|---|---|---|---|---|---|---|---|
| Objectively measured COVID-19 diagnosis status | |||||||
| Measurement period 1 | 1.07 (0.94, 1.20)a | 1.07 (1.00, 1.14)b | 2.91 (1.15, 4.67)b | 0.99 (0.69, 1.35) | 2.00 (1.19, 1.45)b | 1.10 (1.02, 1.19)b | 1.92 (1.26, 2.59)b |
| Measurement period 2 | 1.14 (1.05, 1.23)b | 1.14 (1.04, 1.25)b | 1.11 (0.74, 1.47) | 1.00 (0.71, 1.37) | 2.02 (1.19, 1.45)b | 0.59 (0.12, 1.06) | 2.34 (1.68, 3.00)b |
| Measurement period 3 | 0.91 (0.41, 1.87) | 0.91 (0.41, 1.87) | 1.11 (0.75, 1.48) | 0.99 (0.70, 1.36) | 2.08 (1.69, 1.46)b | 1.12 (0.98, 1.27)a | 1.42 (1.15, 1.69)b |
| Measurement period 4 | 0.88 (0.43, 1.68) | 0.88 (0.43, 1.68) | 4.02 (1.25, 6.78)b | 0.98 (0.70, 1.31) | 0.99 (0.69, 1.44) | 1.13 (1.04, 1.23)b | 2.05 (1.28, 2.83)b |
| Self-reported COVID-19 level of infection severity | |||||||
| Measurement period 1 | 1.43 (1.01, 1.85)b | 1.01 (0.96, 1.13)a | 1.41 (1.17, 1.66)b | 1.00 (0.59, 1.70) | 2.10 (1.37, 2.83)b | 1.00 (0.63, 1.57) | 1.57 (1.16, 1.98)b |
| Measurement period 2 | 1.00 (0.58, 1.74) | 0.99 (0.63, 1.56) | 0.99 (0.63, 1.56) | 1.00 (0.60, 1.72) | 3.03 (1.47, 4.58)b | 1.00 (0.63, 1.57) | 1.46 (1.06, 1.85)b |
| Measurement period 3 | 1.32 (1.01, 1.64)b | 0.99 (0.63, 1.54) | 0.99 (0.63, 1.54) | 2.04 (1.16, 2.91)b | 1.00 (0.47, 2.12) | 1.00 (0.63, 1.57) | 1.00 (0.86, 1.18) |
| Measurement period 4 | 0.99 (0.57, 1.66) | 0.98 (0.61, 1.48) | 0.98 (0.61, 1.48) | 1.28 (1.06, 1.50)b | 1.20 (1.07, 2.12)b | 1.00 (0.63, 1.57) | 1.53 (0.98, 2.08)† |
Data from the Andalusian Health and Social Survey (Spanish Acronym ESSA, Encuesta Sanitaria y Social de Andalucía) were analyzed in measurement period 1 (April-May 2020), period 2 (June-July 2020), period 3 (October-November 2020), and period 4 (April-May 2021). Numbers reported in this table build upon the adjusted (predictor) models shown in Table 3 by including other structured random effects associated with each of the COVID-19 variables
aThe 90% credibility interval did not contain the unity and indicated higher odds of poor mental health/socio-emotional wellbeing during the measurement period
bThe 95% credibility interval did not contain the unity and indicated lower odds of poor mental health
Role of the funding sources
The funders of the present study played no role in the design, collection, analysis, or interpretation of the study data. They also did not participate in writing or the decision to submit the manuscript.
Results
Descriptive results
Only individuals who participated in all four measurement periods of the general ESSA population survey were included in the analyses. The response rate of M1 (n = 2950), M2 (n = 1978), M3 (n = 1491), and M4 (n = 1223) was 88.5%, 67.1%, 75.4%, and 82.0%, respectively. This corresponds to a retention rate of 58% in M2, 51% in M3, and 42% in M4. The most prevalent poor MH/SEW outcome among participants from M1 to M4 was feeling depressed. The most important results of the descriptive analyses are presented in Table 1. For example, the proportion of participants infected with COVID-19 incrementally increased from 5% in M1 to over 8% in M4, corresponding with trends in the prevalence of participants reporting their COVID-19 infection severity as ‘very severe/severe‘ (0.2% in M1, 0.2% in M2, 0.5% in M3, and 1.1% in M4). The same pattern was observed for the percentage of respondents reporting members of their family/household being diagnosed with COVID-19. The majority of participants were female (55.5%). Participants predominately perceived their physical health as ‘excellent/very good/good’ across the four measurement periods, although there was a descending pattern from M1(86.1%) to M4 (80.9%). Conversely, the percentage of participants that were objectively diagnosed with diabetes, dislipemia, obstructive pulmonary disease, and having four or more chronic conditions incrementally increased. Other characteristics of ESSA participants, as well as missing data, by measurement periods are presented in the Appendix (p 11).
Temporal changes in MH and SEW outcomes
There were significant differences in the unadjusted odds ratios (OR) and 95% credibility intervals (95% CI) for the seven mental/emotional health outcomes of interest by measurement period (Table 2). Participants had 21% higher odds of reported regular/bad perceived mental health in M1 compared to excellent/very good/good (OR 1.21 [95% CI 1.05–1.39]), but this declined by about 34% in M2, with participants reporting 20% lower odds of regular/bad perceived mental health (OR 0.80 [95% CI 0.69–0.92]). Odds of low socio-emotional wellbeing, low happiness, and currently feeling anxious also significantly declined from M1 to M2 by 56%, 66%, and 34%, respectively. However, only the odds of low socio-emotional wellbeing were higher in M4 (OR 1.69 [95% CI 1.44–1.98]) compared to M1. Conversely, the odds of low happiness, low optimism and feeling alone continued to decrease after M1.
Predictors of the MH and SEW outcomes
There were several socio-ecological factors that predicted poor MH and SEW status, although associations varied across the seven outcomes examined (Table 3). Overall, inconsistent associations were observed between the other intra-personal, inter-personal, household environment, and population environment factors and the outcomes of interest. However, a few exceptions should be highlighted. At the intra-personal level, regular/bad perceived general health status, and having one objectively diagnosed chronic condition were associated with higher odds for six of the seven MH and SEW outcomes examined (all except feeling depressed). Similarly, at the interpersonal level, perceiving intermediate levels of social support and financial household difficulty were associated with higher odds with five of the seven outcomes examined (all except for feeling anxious and feeling depressed). Furthermore, it should be noted that in regression models that varied over time (Table 4), objectively measured COVID-19 status and self-reported severity levels were significant predictors of the poor MH and SEW outcomes.
Discussion
The present study appears to be the first to leverage overlapping panel data to compare temporal changes in and socio-ecological predictors of different types of MH and SEW outcomes during the initial (and pivotal stages) of the COVID-19 pandemic. Its findings shed light on the state of MH and SEW in a large, urban population. Overall, descriptive analyses showed that there was a reduction in the prevalence of the seven poor MH and SEW outcomes from April 2020 (M1) to June 2020 (M2), with the magnitude of reduction being lowest for low optimism (10%) and highest for low happiness (65%). Yet, patterns in the prevalence change of these outcomes were mixed at M4 compared to M1. Namely, the prevalence of low socio-emotional wellbeing, feeling alone increased by 4%, and 18%, respectively. On the other hand, the prevalence of regular/bad mental health, low happiness, low optimism, feeling depressed, and currently feeling anxious was lower in M4 than M1. Similar patterns were observed in regression analyses. Odds of the population having regular/bad perceived mental health, low socio-emotional wellbeing, low happiness, and feeling anxious significantly declined in M2 compared to M1. Instead, odds of low socio-emotional wellbeing were significantly higher in M4 compared to M1, while odds of low happiness and low optimism were lower during this period. Socio-ecological predictors of the seven outcomes varied both by the type and survey measurement period, although some intra-personal factors (i.e., health status) and inter-personal factors (i.e., perceived level of social support, financial household difficulty) did appear to exacerbate poor MH and SEW among study participants.
What seems to be an initial improvement in MH and SEW around the first month of the COVID-19 pandemic is unsurprising given the timeline of key COVID-19 phases and events in Spain and Andalusia by ESSA survey measurement period (Appendix p 1). In early 2020, around the time when M1 was conducted, there was uncertainty about the nature of the COVID-19 virus and stringent policy measures to mitigate spread of the virus had been initiated. It is possible that this was the first time in recent memory that Andalusian residents had dealt with such a public health crisis. Thus, this initial shock may explain the high prevalence of poor mental and emotional health outcomes observed in the present study. However, around when M2 was conducted, COVID-19 policy measures began to ease in all of Spain. Perhaps the initial shock of this global public health emergency began to dissipate among Andalusian residents, consequently improving their MH and SEW. Another possible explanation is the number of COVID-19 cases and deaths in Andalusia (compared to Spain as a whole) during the first epidemic wave; in particular, around the time M2 was carried out, deaths were less pronounced in Andalusia than across Spain (Appendix p 16). It is possible that Andalusian residents may have perceived the COVID-19 pandemic to be less of a threat to their lives and livelihood compared to their Spanish counterparts. However, about halfway into the second epidemic period in Spain (i.e., around the time that M3 was conducted), cases in Andalusia began to rise and reflected patterns observed in the rest of Spain. This trend continued in M4, which may explain high levels of poor socio-emotional wellbeing among Andalusian study participants about a year after the start of the pandemic.
For the most part, these results are consistent with existing evidence on the trajectories of MH and SEW of general (and mostly adult) populations during the COVID-19 pandemic. For example, although not based on panel data, in line with our findings, previous studies have found general (non-clinical) aspects of MH worsened one year into the COVID-19 pandemic among Spanish populations [28, 29]. There is also evidence that there was an initial increase in anxiety and a gradual decline in the burden of depression at the nascent stage of the pandemic [30]. Large-scale panel studies have similarly documented initial surges in and/or high burden of poor MH/SEW at the start of the pandemic [9, 11–13, 15–17].
Findings regarding predictors of MH and SEW are also somewhat congruent with other study results. At the intra-personal level, for instance, we found evidence that self-reporting ones’ health as regular/bad and being diagnosed with a chronic condition are risk factors for poor MH and SEW. These findings align with research that has found self-rated health, [31] and chronic conditions, [16] put individuals at risk for poor MH. At the inter-personal level, we also found evidence that lower levels of social support increase individuals’ risk for poor MH and SEW, a finding which has been previously reported [29]. Furthermore, our finding that financial household difficulty puts individuals at risk is consistent with previous studies indicating that low income is associated with increased risk for poor MH [14] and SEW [10].
However, there were a few findings that did not fully align with previous large-scale panel studies representative of general (mostly adult) populations. For instance, one such study focused on U.S. adults found that the burden of depressive symptoms increased throughout the pandemic, [14] whereas we found no significant differences. Instead, our findings revealed a significant decline in socio-emotional wellbeing approximately one year into the pandemic. And in contrast to another panel study conducted in Italy, which reported a decline in general mental health from April to September 2020, [15] our study observed improvements in general mental health around a similar time frame, approximately at M1 and M2. Furthermore, other panel studies carried out in England have documented that being female/woman puts individuals at risk for loneliness [10] and depression [11]. In our study, despite examining various multilevel characteristics (including being female), none significantly predicted feeling depressed. However, it is important to note that previous research underscores that individuals’ psychological reactions to the pandemic appear to be predominantly influenced by the evolving pandemic context, country-specific variables, and individual traits and circumstances [32]. Thus, there may be possible heterogeneous effects of COVID-19 on mental health and socio-emotional wellbeing outcomes that were not fully captured in study analysis, those which have been previously observed in other studies [33]. Consequently, these factors may contribute to the discrepancies highlighted above.
The current study is also subject to a few limitations that should be acknowledged when interpreting results. First, it has been recommended that longitudinal analyses seeking to impact of COVID-19 on mental health include a pre-pandemic comparison, [4] which we were unable to do in the present analysis given the absence of data for the outcome measures. Second, panel attrition is often a major disadvantage of longitudinal studies. In the present study, the survey retention rate dropped to 42% in M4. However, our sample size is still large enough to maintain statistical power and Bayesian approaches were employed to provide more robust estimates and bolster the generalizability of our findings. Moreover, the observed biases produced mainly by non-response in the ESSA survey can be showed through the differences between the sample and the study population at a given measurement, according to the intersection of the sex variable with other segmentation variables such as age, province, degree of urbanization and nationality. With respect to age, the largest differences between the values observed from the sample in M4, compared to those from the larger population, are found in the youngest men age group (under 30 years old), in middle-aged women age group (between 35 and 54 years old) and in the oldest women and men age group (over 70 years old), with these differences increasing with age. With regard to the other segmentation variables, the largest differences were found among people with a nationality other than Spanish, especially among men. These results are also observed (although to a lesser extent) in the previous measurements, showing that ESSA has a non-monotone missing pattern and a lower participation of some population groups. Therefore, they justify the need to adjust the sample weights. Accordingly, we combine suitable reweighting methods such as Propensity Score Adjustment (PSA), [27] as well as XGBoost and calibration, [20] to address the biases associated with dropout from overlapping panel survey data [8]. Third, our study was conducted in Andalusia, potentially limiting our study’s generalizability. However, Andalusia is the most populated (with over 8 million residents) and the largest of the 19 regions of Spain [34, 35]. Thus, the present study may capture a diverse population and the study findings may still be relevant to other regions of Spain and around the world. Fourth, temporality bias may also be present in our study given that it was carried out in the first year of the COVID-19 pandemic; albeit our study focused on assessing mental health outcomes during the most critical time of the COVID-19 public health emergency, not to capture the long-term effects of the pandemic on mental health. Given the threat of future pandemics, [36] the results from our study are relevant and may help to inform future efforts to protect mental health during public health emergencies. Fifth, race/ethnicity and migration background are well-known demographic factors associated with various health outcomes and COVID-19 related outcomes that should have been included as control variables in study analyses. Unfortunately, collecting this information is typically prohibited in Spain, [37] preventing us from collecting this information in the present study. Sixth, given that participants self-reported answers to trained interviewers various questions through a computer-assisted telephone survey, response and social desirability bias may have been introduced to the study, especially for sensitive questions such as income. Furthermore, a single-item measure was used to assess participant’s perceived mental health status, happiness, optimism, feeling alone, feeling depressed, feeling anxious. Yet, the single-item measure of self-rated health used in the present study is adapted from one often used in research that is associated with multi-item measures of mental health [21]. The single-item measures of happiness, optimism, feeling alone, feeling depressed, feeling anxious were based on questions from the validated Socioemotional Well-being Index. In general, there is also growing attention to the benefits of using single-item mental health questions [38].
Despite these limitations, our study has several key strengths that lend support to the findings. First, the overlapping panel design allowed us to complete each measurement with new cross-sectional samples that subsequently became longitudinal, thereby enabling us to better examine changes in the mental/emotional health outcomes of interest over time and providing us with greater control over the confounding variables. This panel design, where the same study participants were tracked at various survey measurement periods, is what allowed us to detect that some individual-level COVID-19 variables (i.e., objectively measured COVID-19 status and self-reported COVID-19 severity levels) influenced the outcome variables. Second, the panel design allowed us to collect a large amount of high-quality data in real-time and was representative of the general population, filling existing research gaps [6]. Third, the dataset used was obtained using stratified random sampling and survey adjusted weights application which bolsters statistical power. Fourth, the original data from which the sample was initially extracted (i.e., vital statistics registries, population censuses, housing censuses) were subsequently linked to other probabilistic registries that collected clinical, epidemiologic, demographic, and environmental information. Fifth, other rigorous approaches implemented to enhance the quality of data collected included training and regularly checking in with a team of interviewers solely assigned to the study to administer the survey via a computer-assistant telephone system. Sixth, we measured seven MH and SEW outcomes, most of them based on validated measurement tools, such as the SEWBI which was specifically validated for European populations [23, 39]. Seventh, COVID-19 and chronic condition diagnoses were objectively measured based on clinic records. Eight, the study measurements correspond to critical timepoints during the pandemic. Furthermore, analyses were guided by a conceptual model that captured a multitude of socio-ecological factors that have the potential to shape mental/emotional health outcomes.
Study implications
Our study offers evidence that the evolution of poor mental and socio-emotional health outcomes during the first (and most challenging) year of the pandemic following the first state of alarm varied according to the type of outcome under consideration. This suggests that careful distinctions should be made in how mental health outcomes are assessed and addressed by practitioners and policymakers alike. Likewise, our study also found that mental health/socio-emotional wellbeing risks and protective factors varied by outcome examined, although some groups such as individuals experiencing poor health, limited social support, and low socioeconomic status were found to be at greatest risk for poor mental and emotional health in most of the outcomes examined. Stakeholders and decision-makers seeking to curb poor MH/SEW outcomes should consider varying mental health burdens across different populations and tailor interventions to such groups disproportionately impacted during ongoing and future efforts to address underlying social determinants of mental health during public health crises. In general, there may be a need to make behavioral health services more widely available to populations experiencing health inequalities MH and SEW as a preventative measure.
Conclusion
Although the pandemic is receding in the mind of the public and decision-makers, the findings from this study may guide ongoing and future efforts to address underlying social determinants of mental health in the new era of COVID-19. Now more than ever, examining current trends in and risk factors for poor MH and SEW may illuminate opportunities to maximize scarce resources and inadequate infrastructures to improve health outcomes during public health emergencies. After all, there is increasing recognition that mental healthcare infrastructures, which were inadequate before the pandemic, have failed even further within this context [40]. Ultimately, more studies with strong research designs are warranted to investigate temporal changes in and predictors of these outcomes from the start of the pandemic to the present.
Supplementary Information
Acknowledgements
This study was carried out within the ‘Health Inequalities and COVID-19’ subprogram of CIBER of Epidemiology and Public Health (CIBERESP). We appreciate the comments from the editor and three anonymous reviewers of a previous version of this work who, without a doubt, have helped us to improve our work. The usual disclaimer applies.
Declaration of Generative AI and AI-assisted technologies in the writing process
During the writing of the article the authors have not used any type of AI and AI-assisted technologies.
Abbreviations
- 95% CI
95% Credibility intervals
- ESSA
Health and Social Survey (Encuesta Sanitaria y Social de Andalucía)
- GLMM
Generalized linear mixed models
- M1
Measurement period 1
- M2
Measurement period 2
- M3
Measurement period 3
- M4
Measurement period 4
- MH
Mental Health
- OR
Odds ratio
- SEW
Socio-emotional wellbeing
- SEWBI
Socioemotional Well-being Index
- XGBoost
eXtreme Gradient Boosting
Authors' contributions
Conceptualization, BR; Methodology, BR, MS, MAB, AC and CSC; Resources, MS, MAB and MJL; Data curation CSC and AC; Analysis BR, MS, AC and CSC; Writing-original draft preparation, BR; Writing-review and editing, MS, MAB, AC and MJL; Project administration, MS, MAB and AC; Funding acquisition, MS and AC. All authors (BR, MS, AC, CSC, MJL and MAB) have read and agree to the published version of the manuscript. All authors (BR, MS, AC, CSC, MJL and MAB) had full access to all the data in the study and accept full responsibility for the findings reported.
Funding
This work was partially financed by the COVID-19 Competitive Grant Program (ID#61605991) from Pfizer Global Medical Grants; the SUPERA COVID-19 Fund, from SAUN: Santander Universidades, CRUE and CSIC; the Strategic Plan for Research and Innovation in Health (PERIS), Department of Health, Government of Catalonia; and the Consolidated research group ‘Compositional and Spatial Data Analysis (COSDA)’ 2021 SGR 01197, AGAUR, Government of Catalonia; the Andalusian Institute of Statistics and Cartography (IECA, Spanish acronym) and the Andalusian School of Public Health (EASP, Spanish acronym) [financed the first and second survey measurements]; and the Maria Zambrano ‘Grants for the requalification of the Spanish university system’ supported by ‘Next Generation EU’, the ‘European Union, Recovery, Transformation and Resilience Plan,’ and the Spanish Government. The funding sources did not participate in the design or conduct of the study, the collection, management, analysis, or interpretation of the data, or the preparation, review, or approval of the manuscript.
Availability of data and materials
The dataset and code supporting the conclusions of this article will be available in the ESSA repository at www.easp.es/ESSA. Code will be available at www.researchprojects.es.
Declarations
Ethics approval and consent to participate
All methods were carried out in accordance with relevant guidelines and regulations on which.
An informed consent was obtained from all subjects involved in the ESSA survey on which this study is based. It was also approved by the Research Ethics Committee of the Department of Health and Families of the Andalusian Regional Government (protocol code 10/20, dated 07 December 2020). The ESSA is an activity included in the processing activities registry of the Department of Health and Families of the Andalusian Regional Government and is linked to the Andalusian Health Survey (EAS, Encuesta Andaluza de Salud), an official statistical operation included in the Andalusian Statistical and Cartographic Plan (Plan Estadístico y Cartográfico de Andalucía), code 02.02.21.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.The Lancet Public Health. COVID-19 pandemic: what’s next for public health?. Lancet Public Health. 2022;7:e391. 10.1016/S2468-2667(22)00095-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kola L, Kumar M, Kohrt BA, Fatodu T, Olayemi BA, Adefolarin AO. Strengthening public mental health during and after the acute phase of the COVID-19 pandemic. Lancet. 2022;399:1851–2. 10.1016/S0140-6736(22)00523-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patel V, Saxena S, Lund C, et al. The Lancet Commission on global mental health and sustainable development. Lancet. 2018;392:1553–98. 10.1016/S0140-6736(18)31612-X [DOI] [PubMed] [Google Scholar]
- 4.Penninx BWJH, Benros ME, Klein RS, Vinkers CH. How COVID-19 shaped mental health: from infection to pandemic effects. Nat Med. 2022;28:2027–37. 10.1038/s41591-022-02028-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sun Y, Wu Y, Fan S, et al. Comparison of mental health symptoms before and during the covid-19 pandemic: evidence from a systematic review and meta-analysis of 134 cohorts. BMJ. 2023;380:e074224. 10.1136/bmj-2022-074224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sánchez-Cantalejo Garrido C, Yucumá Conde D, del Rueda M. Scoping review of the methodology of large health surveys conducted in Spain early on in the COVID-19 pandemic. Front Public Health. 2023;11:1217519. 10.3389/fpubh.2023.1217519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kalton G, Citro CF. Panel surveys: adding the fourth dimension. Surv Methodol. 1993;19:2015–15. [Google Scholar]
- 8.Sánchez-Cantalejo C, Rueda MDM, Saez M, et al. Impact of COVID-19 on the health of the general and more vulnerable population and its determinants: health care and social survey-ESSOC, study protocol. Int J Environ Res Public Health. 2021;18:8120. 10.3390/ijerph18158120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mata J, Wenz A, Rettig T, et al. Health behaviors and mental health during the COVID-19 pandemic: a longitudinal population-based survey in Germany. Soc Sci Med. 2021;287:114333. 10.1016/j.socscimed.2021.114333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bu F, Steptoe A, Fancourt D. Loneliness during a strict lockdown: trajectories and predictors during the COVID-19 pandemic in 38,217 United Kingdom adults. Soc Sci Med. 2020;265:113521. 10.1016/j.socscimed.2020.113521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fancourt D, Steptoe A, Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatry. 2021;8:141–9. 10.1016/S2215-0366(20)30482-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Duarte F, Jiménez-Molina Á. A Longitudinal Nationwide Study of Psychological Distress during the COVID-19 pandemic in Chile. Front Psychiatry. 2022;13:744204. 10.3389/fpsyt.2022.744204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Benke C, Asselmann E, Entringer TM, Pané-Farré CA. The role of pre-pandemic depression for changes in depression, anxiety, and loneliness during the COVID-19 pandemic: results from a longitudinal probability sample of adults from Germany. Eur Psychiatry. 2022;65:e76. 10.1192/j.eurpsy.2022.2339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ettman CK, Cohen GH, Abdalla SM, et al. Persistent depressive symptoms during COVID-19: a national, population-representative, longitudinal study of U.S. adults. Lancet Reg Health Americas. 2022;5:100091. 10.1016/j.lana.2021.100091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lucchini M, Gerosa T, Pancheva M, Pisati M, Respi C, Riva E. Differential effects of COVID-19 and containment measures on mental health: evidence from ITA.LI-Italian lives, the Italian household panel. PLoS ONE. 2021;16:e0259989. 10.1371/journal.pone.0259989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhou Y, Cai W, Xie L. The impact of the COVID-19 pandemic on depressive symptoms in China: a Longitudinal, Population-based study. Int J Public Health. 2022;67:1604919. 10.3389/ijph.2022.1604919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Riepenhausen A, Veer IM, Wackerhagen C, et al. Coping with COVID: risk and resilience factors for mental health in a German representative panel study. Psychol Med. 2023;53:3897–907. 10.1017/S0033291722000563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bu F, Steptoe A, Fancourt D. Depressive and anxiety symptoms in adults during the COVID-19 pandemic in England: a panel data analysis over 2 years. PLoS Med. 2023;20:e1004144. 10.1371/journal.pmed.1004144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Parola A, Rossi A, Tessitore F, Troisi G, Mannarini S. Mental Health through the COVID-19 Quarantine: a growth curve analysis on Italian young adults. Front Psychol. 2020;11:567484. 10.3389/fpsyg.2020.567484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Castro L, Del Mar Rueda M, Sánchez-Cantalejo C, Ferri R, Cabrera-León A. Calibration and XGBoostc reweighting to reduce coverage and non-response biases in overlapping panel surveys: application to the Healthcare and Social Survey. BMC Med Res Methodol. 2024;24:36. 10.1186/s12874-024-02171-z. 10.1186/s12874-024-02171-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ahmad F, Jhajj AK, Stewart DE, Burghardt M, Bierman AS. Single item measures of self-rated mental health: a scoping review. BMC Health Serv Res. 2014;14:398. 10.1186/1472-6963-14-398. [DOI] [PMC free article] [PubMed]
- 22.Statistics Canada. Canadian Health Measures Survey (CHMS). https://www.statcan.gc.ca/en/survey/household/5071 (Accessed 23 Jan 2024).
- 23.Bericat E. The Socioemotional Well-Being Index (SEWBI): theoretical Framework and empirical operationalisation. Soc Indic Res. 2014;119:599–626. 10.1007/s11205-013-0528-z [DOI] [Google Scholar]
- 24.McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15:351–77. 10.1177/109019818801500401 [DOI] [PubMed] [Google Scholar]
- 25.Alegría M, NeMoyer A, Falgàs Bagué I, Wang Y, Alvarez K. Social Determinants of Mental Health: where we are and where we need to go. Curr Psychiatry Rep. 2018;20:95. 10.1007/s11920-018-0969-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen T, Guestrin C. XGBoost:. A scalable tree boosting system. In: Proceedings of the 22nd ACM SIGKDD International Conference on Knowledge Discovery and Data Mining. San Francisco: ACM 2016 Proceedings; p. 785–794.
- 27.Friedman J, Hastie T, Tibshirani R. Additive logistic regression: a statistical view of boosting (with discussion and a rejoinder by the authors). Ann Stat. 2000;28(2):337–407. 10.1214/aos/1016218223.
- 28.Esteve-Matalí L, Llorens-Serrano C, Alonso J, Vilagut G, Moncada S, Navarro-Giné A. Mental health inequalities in times of crisis: evolution between 2005 and 2021 among the Spanish salaried population. J Epidemiol Community Health. 2022;ahead of print:jech–2022. [DOI] [PubMed] [Google Scholar]
- 29.Monistrol-Mula A, Felez-Nobrega M, Moneta MV, et al. Mental health symptoms 1 year after the COVID-19 outbreak in Spain: the role of pre-existing mental disorders and their type. J Affect Disord. 2022;318:22–8. 10.1016/j.jad.2022.08.127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Raventós B, Pistillo A, Reyes C, et al. Impact of the COVID-19 pandemic on diagnoses of common mental health disorders in adults in Catalonia, Spain: a population-based cohort study. BMJ Open. 2022;12:e057866. 10.1136/bmjopen-2021-057866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lachytova M, Katreniakova Z, Mikula P, Jendrichovsky M, Nagyova I. Associations between self-rated health, mental health problems and physical inactivity among urban adolescents. Eur J Public Health. 2017;27:984–9. 10.1093/eurpub/ckx051 [DOI] [PubMed] [Google Scholar]
- 32.Zrnić Novaković I, Ajduković D, Bakić H et al. Shaped by the COVID-19 pandemic: psychological responses from a subjective perspective-A longitudinal mixed-methods study across five European countries. PLoS ONE. 2023;18(4):e0285078. 10.1371/journal.pone.0285078. [DOI] [PMC free article] [PubMed]
- 33.Kim J, Park S, Subramanian SV, Kim T. The psychological costs of the COVID-19 pandemic and heterogeneous effects in South Korea: evidence from a difference-in-differences analysis. J Happiness Stud. 2023;24:455–76. 10.1007/s10902-022-00605-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Böhme K, Lüer C, Besana F, Hans S, Schuh B, Münch A, Gorny H. Commission for Economic Policy: the state of the regions, cities and villages in the areas of socio-economic policies contribution to the 2021 EU Annual Regional and local barometer. Eur Comm Reg. 2021. 10.2863/153679.
- 35.Autonomous Community Profiles. Andalusia. https://www.caixabankresearch.com/en/publications/autonomous-community-profiles/andalusia (Accessed 17 Jul 2024).
- 36.Coccia M. Sources, diffusion and prediction in COVID-19 pandemic: lessons learned to face next health emergency. AIMS Public Health. 2023;10:145. 10.3934/publichealth.2023012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.European Commission. Data collection in the field of ethnicity. https://commission.europa.eu/system/files/2021-09/data_collection_in_the_field_of_ethnicity.pdf (Accessed 16 Jul 2024).
- 38.Allen MS, Iliescu D, Greiff S. Single item measures in psychological science: a call to action [Editorial]. Eur J Psychol Assess. 2022;38(1):1–5. 10.1027/1015-5759/a000699 [DOI] [Google Scholar]
- 39.Bericat E. accessed Jan 23,. Excluidos de la Felicidad. Las Desigualdades de Bienestar Emocional en España y Europa. https://www.researchgate.net/publication/287814426_EXCLUIDOS_DE_LA_FELICIDAD_Las_desigualdades_de_bienestar_emocional_en_Espana_y_Europa (2024).
- 40.Campion J, Javed A, Lund C, et al. Public mental health: required actions to address implementation failure in the context of COVID-19. Lancet Psychiatry. 2022;9:169–82. 10.1016/S2215-0366(21)00199-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The dataset and code supporting the conclusions of this article will be available in the ESSA repository at www.easp.es/ESSA. Code will be available at www.researchprojects.es.