Abstract
Objective:
The current study examined how average daily loneliness (between-persons [BPs]), intraindividual variability in loneliness across days (within-persons [WPs]), and loneliness stability informed physical health symptomatology.
Method:
We utilized daily diary data from a national sample of 1,538 middle-aged adults (Mage = 51.02; 57.61% women) who completed eight end-of-day telephone interviews about daily experiences, including loneliness and physical health symptoms (e.g., headaches, nausea). Via multilevel modeling, we examined average daily loneliness (BPs), intraindividual variability in loneliness (WPs), stability in loneliness (individual mean-squared successive difference) in association with the number and average severity of daily physical health symptoms.
Results:
When participants were less lonely on average, and on days when loneliness was lower than a person’s average, they had fewer and less severe physical health symptoms. Additionally, participants who were more stable in loneliness across 8 days had less severe physical health symptoms. Further, there was a stronger association between instability in loneliness and more physical health symptoms for people who were lonelier on average. Finally, the increase in physical health symptom severity associated with WP loneliness was strongest for participants with low variability in loneliness.
Conclusion:
Loneliness is associated with physical health symptoms on a day-to-day basis, especially for people who are highly variable in loneliness. Considerations of multiple sources of variation in daily loneliness may be necessary to adequately address loneliness and promote health. Public health interventions addressing loneliness may be most effective if they support social connectedness in people’s everyday lives in ways that promote stable, low levels of loneliness.
Keywords: loneliness, temporal dynamics, physical health, daily diary, variability
Resumen
Objetivo:
El estudio examinó como la soledad diaria promedio (entre personas), variabilidad intraindividual en la soledad a través de los días (dentro-de-las-personas), y la estabilidad de soledad informó sintomatología de salud física.
Método:
Utilizamos data diaria de una muestra nacional de 1,538 adultos de edad media (Medad = 51.02; 57.61% mujeres) que completaron ocho entrevistas de experiencias diarias vía teléfono al final del día, incluyendo síntomas de soledad y salud física (p.ej., dolor de cabeza, nausea). Mediante un modelo multinivel, examinamos soledad promedio diaria (entre personas), variabilidad intraindividual en la soledad (dentro-de-las-personas), estabilidad dentro de la soledad (iRMSSD, por sus siglas en inglés) asociado al numero y severidad promedio de síntomas de salud física diarios.
Resultados:
Cuando los participantes estaban menos solos en promedio, y en días cuando la soledad fue menor que el promedio por persona, tuvieron pocos síntomas de salud física y menos severos. Adicionalmente, los participantes que estaban mas estables en soledad a través de los ocho días tuvieron síntomas de salud física menos severos. Además, hubo una asociación más fuerte entre la inestabilidad en la soledad y mayores síntomas de salud física para personas que estaban en promedio mas solas. Finalmente, el incremento en la severidad de síntomas de salud física asociada con la soledad dentro-de-la-persona fue mas fuerte para participantes con soledad de variabilidad baja.
Conclusión:
La soledad está asociada con síntomas de salud física en una base diaria, especialmente para personas que son de variabilidad de soledad alta. Consideraciones de las múltiples fuentes de variación en la soledad diaria puede ser necesaria para afrontar adecuadamente la soledad y promover la salud. Intervenciones de salud publica que afrontan la soledad pueden ser más efectivos si apoyan conexión social que promueve niveles de soledad estables o bajos en la vida cotidiana de las personas.
Distinguishable from social isolation and social network size (Coyle & Dugan, 2012; Victor et al., 2005), loneliness is the perception of social disconnection (Cacioppo & Cacioppo, 2018a). The subjective feeling of loneliness is characterized by a perceived discrepancy between actual and desired social relationships (Peplau & Perlman, 1982) and is recognized as a significant health concern with a particular emphasis on the serious negative health impact loneliness has on adults during midlife and old age (National Academies of Sciences, Engineering, and Medicine, 2020). Several health consequences of loneliness are well-established, such as increased risk of depression (Cacioppo et al., 2006), cardiovascular disease (Hodgson et al., 2020), and even mortality (Holt-Lunstad et al., 2015; Luo et al., 2012). Not only does loneliness negatively impact people’s health, loneliness is also an economic burden with some studies reporting increased healthcare costs associated with loneliness (e.g., Mihalopoulos et al., 2020). Most existing research examines loneliness as a stable characteristic or trait, often assessed at one point in time. Yet, loneliness fluctuates in daily life (Buecker et al., 2024; van Roekel et al., 2018). Therefore, it is crucial to examine temporal dynamics in loneliness related to indicators of health to detect those at potential risk for health-related issues. Further, better understanding daily loneliness in midlife may be particularly informative for public health initiatives (see U.S. Surgeon General, 2023), and for promoting healthy aging.
Loneliness and Health During Midlife
Decades of research indicates midlife as a pivotal period in the life course (Lachman et al., 2015). Not only does midlife bridge early and late periods of life, well-being and life events during midlife inform health in older age (Lachman et al., 2015), making it imperative to examine midlife to promote healthy aging. Middle-aged adults experience a variety of significant changes in their life, like changing relationships with their children, caring for a parent, and normative health decline; all of which could be critical determinants of health and well-being (Infurna et al., 2021). With sometimes drastic changes to social roles (Infurna et al., 2020) and social networks (Antonucci et al., 2014), middle-aged adults may also have unique fluctuations in loneliness while navigating these changes. Perhaps resulting from these social role and network changes, recent work noted that loneliness follows a nonlinear trajectory across the lifespan, with upticks in mid-life (Hawkley et al., 2022). Despite the importance of investigating daily loneliness and health during this developmental period, middle-aged adults remain an understudied group.
Temporal Dynamics in Daily Loneliness
Developmental theories like dynamic systems theory (e.g., Thelen, 2005; Thelen & Smith, 2006) connote that people are a complex system of both short-term changing qualities, and more long-term enduring qualities (e.g., Bergeman et al., 2021; Nesselroade, 1991). To understand developmental or long-term stability (or change), then, researchers must consider short-term dynamics characterizing the phenomena. Pertinent to the current study, although loneliness has been considered a stable trait in research, it fluctuates across time (e.g., Buecker et al., 2024; Zhaoyang et al., 2022). Thus, understanding how loneliness functions in different time scales is a crucial factor to consider in relation to physical health symptoms. Indeed, there are benefits for both research and intervention to examine how dynamics of daily loneliness inform health consequences. For example, interventions are predicated on the assumption that current intervention activities have effects for current and long-term behavior change; therefore, researchers must understand the short-term mechanisms related to daily health and behavior in addition to long-term, final outcomes (Thelen & Smith, 2006). In the current study, we focus on daily loneliness and specifically aim to examine three temporal dynamics of daily loneliness: (a) average daily loneliness, (b) intraindividual variability in loneliness, and (c) loneliness stability.
Average Daily Loneliness
Often, loneliness is examined at a single time point, conceptualized as a general assessment of a person’s overall level of loneliness. Generally, lonelier people rate their overall physical health more poorly (Jessen et al., 2018), with evidence suggesting that lonelier older adults report more symptoms across domains (e.g., depressive, gastrointestinal, cardiopulmonary, head-related symptoms; Svensson et al., 2022). Relying on single assessments of loneliness, however, may not capture the daily experiences that relate to daily physical health reports. Rather, examining average levels of loneliness across multiple days may be more informative and sensitive to a person’s daily experiences than a one-time trait measure. In support of this notion, average daily loneliness predicted psychopathological symptoms over and above trait loneliness (Buecker et al., 2024). Little research, however, has examined how average daily loneliness may be related to physical health.
Loneliness Variability
Two temporal aspects of loneliness variability may be important to examine regarding loneliness: intraindividual variability and stability. Intraindividual variability refers to the within-person (WP) fluctuations of a construct across occasions (e.g., day-to-day) and is often calculated as the WP deviation from a person’s own average (Cerino & Hooker, 2019). Take, for example, a person with an average loneliness score of four computed across 8 days of measurements. If, on one assessment day during the measurement period, this person reports a loneliness score of two, their WP deviation score would be negative two because they reported less loneliness than what they did on average. Intraindividual variability is commonly used to examine affect variability and its impact on health across days; intraindividual variability in affect is linked with an increased likelihood of chronic conditions (Hardy & Segerstrom, 2017), poorer psychological well-being (Houben et al., 2015), as well as higher levels of inflammation, particularly among those with higher average affect (Jones et al., 2023). Yet, few studies have examined how intraindividual variability in loneliness is associated with health or well-being.
Although not focused on physical health symptoms, one study (Buecker et al., 2024) found that average intraindividual variability in loneliness (i.e., average of deviations across weeks) was a significant predictor of stress and accounted for a significant portion of the variance in stress beyond average levels loneliness. As Buecker et al. (2024) examined the average intraindividual variability of each person, it is unclear how short-term fluctuations in loneliness, rather than average fluctuations, may influence health. Whereas Buecker et al. (2024) examined socioemotional outcomes, only one study to our knowledge has examined intraindividual variability in loneliness with respect to physical health—specifically sleep. This study found that days when loneliness was higher than a person’s average were associated with higher waking after sleep onset compared to days when loneliness was lower than average in a sample of indigenous peoples (John-Henderson et al., 2021). Taken together, there is preliminary evidence that intraindividual variability in loneliness may have important implications for health; yet, it remains unclear how intraindividual variability in loneliness may influence physical health more broadly.
Loneliness Stability
Loneliness stability refers to the magnitude of consecutive changes in a given outcome, often operationalized as the mean-squared successive difference (MSSD) score (Jahng et al., 2008; Ko et al., 2014). For example, on Monday, a person may report a score of 4, the next day a score of 1, and the following day a score of 2. For this person across 3 days, their MSSD would be a 5 [mean of (day 1 − day 2)2 + (day 2 − day 1)2], suggesting low stability in feelings of loneliness. Researchers have suggested utilizing MSSD as global index of short-term temporal instability in lieu of other indices (e.g., probability of acute change; Jahng et al., 2008). Instability in emotions (e.g., Houben et al., 2015) and self-regulatory beliefs (Ko et al., 2014) have been related to poorer psychological health and social goal progress, respectively. Only one study to date has examined associations between stability in loneliness and psychological health outcomes (Buecker et al., 2024); specifically, less stability in loneliness was associated with greater stress and depression. Given these associations between loneliness instability and psychological health, there may be important associations between loneliness instability and physical health that have yet to be examined. Indeed, understanding how loneliness on 1 day may inform subsequent days of loneliness and health may be crucial to intervention and prevention efforts.
Interactions Between Temporal Dynamics of Loneliness and Physical Health
Average daily loneliness, intraindividual variability in loneliness, and loneliness stability may be uniquely associated with physical health symptomology; yet it is similarly possible that these aspects of daily loneliness work in tandem to influence physical health symptoms. For example, a person who has high average loneliness may also report higher than average levels of loneliness on a given day, which may ultimately inform their daily health symptoms. To this effect, one study examined interrelated aspects of loneliness among adolescents, finding higher trait loneliness (compared to lower trait loneliness) predicted higher momentary loneliness when individuals were alone, but lower momentary loneliness when individuals were with family and friends (van Roekel et al., 2018). Another study found that among older adults, higher trait loneliness was associated with lower levels of momentary loneliness following more frequent or pleasant social interactions (Zhaoyang et al., 2022). No studies to the authors’ knowledge have examined how aspects of daily reports of loneliness may interact with each other to inform health outcomes. As such, the current study adds to the literature by examining the unique and interactive effects of average daily loneliness, intraindividual variability in loneliness, and loneliness stability on physical health symptomology.
The Current Study
Dynamics of daily loneliness have not been extensively examined, and yet evidence suggests that these aspects of loneliness may be pertinent to daily health and well-being. We investigate three dynamics of loneliness in daily life and their associations with subjective reports of physical health—both the number and severity of physical health symptoms—among middle-aged adults. We examine participants’ average level of daily loneliness, a method which parallels conventional “trait” loneliness typically measured at one time point but offers more sensitivity to daily experiences of loneliness given the repeated daily assessments. Second, intraindividual variability, represented by daily deviations from an individual’s average loneliness, captures the day-to-day fluctuations in loneliness that occur during daily life. Finally, stability in loneliness informs the magnitude of these daily changes in loneliness over time.
Our first aim addresses how average daily loneliness, intraindividual variability in daily loneliness, and loneliness stability uniquely relate to self-reported physical health symptomology. We hypothesized that people who are lonelier on average report a higher number and more severe physical health symptoms compared to people who are less lonely on average. We also predicted that for days when loneliness is higher than average, people report a higher number and more severe physical health symptoms compared to days when loneliness was lower than average. Additionally, we expected that people exhibiting less loneliness stability (e.g., large changes in loneliness from day to day) will report a higher number and more severe physical health symptoms compared to people with great loneliness stability. Our second aim examines interactions between these temporal dynamics of daily loneliness. Compared to other combinations of loneliness, we expected that the following would relate to greater and more severe self-reported physical health symptoms: (a) days when loneliness was higher than average and people who are lonelier on average, (b) days when loneliness was higher than average and people who have more variability in their loneliness, and (c) people who are lonelier on average and people who have less loneliness stability.
Method
Participants and Procedure
We used data from the second wave of the National Study of Daily Experiences (NSDEII)—the daily diary component of the larger Midlife in the United States Study (MIDUS). In 1995, MIDUS investigators measured how a host of phenomena influenced health and well-being from early adulthood into midlife and older age. While the NSDEI included 1,499 of the 7,100 MIDUS participants, the NSDE subproject expanded in its second wave (2005–2006) to include individuals from wave 1 (n = 794), and people from other MIDUS projects (n = 1,228) for a sample of 2,022. The NSDEII was completed approximately 10 years following the NSDE 1. More information pertaining to eligibility and decisions for sample size can be found at midus.wisc.edu. Participants were interviewed at the end of the day for eight consecutive days through phone interviews lasting approximately 15–20 min. Interviews reflected the entire day; there was a 92% completion rate. Participants (Mage = 56.24, SD = 12.20) were mostly White, married women, with some college education; see Table 1 for descriptive statistics.
Table 1.
Demographic Information
| Demographic variables | N | M (SD) | Range | % |
|---|---|---|---|---|
|
| ||||
| Age | 1,538 | 51.02 (8.60) | 35–65 | — |
| Gender | ||||
| Men | 652 | — | — | 42.39 |
| Women | 886 | — | — | 57.61 |
| Education | ||||
| <HS diploma | 527 | — | — | 34.27 |
| Some college | 725 | — | — | 47.14 |
| ≥Bachelors | 286 | — | — | 18.60 |
| Race | ||||
| White | 1,273 | — | — | 82.77 |
| Racialized as non-White | 265 | — | — | 17.23 |
| Marital status | ||||
| Married | 1,133 | — | — | 73.67 |
| Other | 405 | — | — | 26.33 |
| BMI | 1,538 | 29.75 (4.93) | 14.99–64.06 | — |
| Health conditions | ||||
| Yes | 63 | — | — | 4.10 |
| No | 1,475 | — | — | 95.90 |
| Daily loneliness | 11,247 | 0.15 (0.53) | 0–4 | — |
Note. Only BMI and health conditions were imputed as they were the only variables collected in a different time point. HS = high school; BMI = body mass index.
Measures
Physical Health Symptoms
Participants indicated whether they had experienced (“yes” or “no”) any of 28 possible physical health symptoms each day (e.g., headaches, shortness of breath, ear-related problems; Leger et al., 2015). Items were summed so that higher scores reflected more daily physical health symptoms. The intraclass correlation coefficient (ICC) suggested that 67% and 33% of the variance in physical health symptoms reflects BP and WP variation, respectively. For symptom severity, people rated each reported symptom on a scale of 0 (mild) to 10 (very severe). Severity items were averaged together so that higher scores represented higher average severity. The ICC revealed that 46% and 54% of the variance in physical health symptom severity was BP and WP, respectively.
Loneliness
Loneliness was assessed daily with a single-item question (i.e., “How much of the time today did you feel lonely?”) with response options ranging from 0 (none of the time) to 4 (all of the time). Single-item measures of loneliness have been shown to have high rater agreement and convergent validity with multiitem measures of loneliness and acceptable reliability (Mund et al., 2023). Higher scores represented greater perceptions of loneliness that day. The ICC of the unconditional model was .57 suggesting that approximately 57% of the variance in loneliness reflects between-person (BP) variation and 43% of the variance in loneliness reflects WP variation. Our current operationalizations of average loneliness, variability in loneliness, and stability in daily loneliness were derived from this item and are described in more detail in the analytic strategy.
Covariates
Age, gender, education, marital status, race, and health conditions were included in analyses as covariates given theoretical and empirical literature indicating these demographics as correlates of loneliness (Cacioppo & Cacioppo, 2018b; Taylor & Nguyen, 2020). Body mass index (BMI) was included as a covariate given associations with physical health symptoms (Leger et al., 2015). Gender was dichotomously coded (i.e., 0 = man, 1 = woman) as no other options were available. Education was coded as 1 (less than a high school diploma), 2 (some college), or 3 (more than a bachelors). Dichotomous coding was utilized for race (0 = White,1 = racialized as not White) and marital status (0 = married, 1 = other). We drew on the MIDUS Biomarker project (n = 1,011) for BMI and health conditions. First, BMI was computed by dividing weight (kg) by height squared (meters). Second, chronic or underlying conditions were reported from a 23-item checklist (e.g., heart disease, depression). Participants also reported other conditions not listed in the checklist. A binary variable was created (i.e., 0 = no health conditions, 1 = at least one condition) and used a Markov Chain Monte Carlo Multiple Imputation method for BMI and any health condition to impute missing data for these variables for people who did not participate in the MIDUS Biomarker Project. We covaried for study day (1–8) to account for day-level trends (Hoffman & Stawski, 2009) as well as weekday versus weekend to better capture the potential fluctuations across the week. Finally, in sensitivity analyses, we covaried for a 11-item measure of negative affect (Watson et al., 1988) that asked, “How much of the time today did you feel [emotion]?” Items (e.g., anger, sadness) were scored from 0 (none of the time) to 4 (most of the time).
Analytic Strategy
We first created variables for each of our operationalizations for loneliness. Average loneliness (BPs) was calculated by averaging each day’s level of loneliness together for each person across the 8 days. Second, we calculated the WP deviation of loneliness for each day by subtracting the day’s loneliness score by each person’s own average loneliness to create a raw intraindividual standard deviation of loneliness (Hoffman & Stawski, 2009). This is a common analytic technique to define net-intraindividual variability (Estabrook et al., 2012; Hoffman & Stawski, 2009). Finally, we created a measure of loneliness stability that was time-structured—a MSSD (Jahng et al., 2008; Ko et al., 2014). MSSDs were calculated for each person by summing and squaring the successive differences in daily loneliness and then averaging these differences (Ko et al., 2014) to represent the amplitude of variation in loneliness from 1 day to the next for each person. Finally, we used the square root of the MSSD (i.e., individual mean-squared successive difference [iRMSSD]) to represent a scale like a standard deviation similar to the work of past research (Ko et al., 2014). Greater scores were indicative of less stability (i.e., more instable loneliness).
The number of physical health symptoms was positively skewed and initial models using generalized multilevel models provided better-fit statistics (i.e., smaller Bayesian information criteria, −2 log-likelihood) compared to general multilevel models. Thus, we utilized SAS PROC GLIMMIX with a multinomial distribution and used the Laplace method in SAS 9.4 (SAS Institute, Cary NC) for the number of physical health symptoms. Analyses modeled the probability of having fewer physical health symptoms and as such, we multiplied each estimate by (−1) to offer interpretations that represented increases in physical health symptoms. Moreover, interpretations of generalized linear models with dependent count variables are slightly different from traditional odds ratios. Estimates represent the multiplicative increase in physical health symptoms per unit increase in the predictor variable(s) rather than an increased odds.
As physical health symptom severity was continuous and residuals were normal, we utilized general multilevel models in SAS PROC MIXED for physical health symptom severity. We ran initial models with a random slope of the WP deviation of loneliness in addition to random intercepts; however, some of the models resulted in a nonpositive definite g-matrix. We thus dropped the random effects of daily loneliness deviations from the models where convergence criteria were not met; these covariances are noted in each table. All models covaried for study day (1–8), weekday versus weekend, age (centered on the grand mean), gender, education, race, marital status, BMI (centered on the grand mean), and health conditions.
Results
Descriptive statistics are available in Table 1 and correlations for the variables of interest are in Table S1 in the online supplemental materials. Higher loneliness on average (BP), days when loneliness was higher (WP), and less loneliness stability (iRMSSD) were significantly correlated with more physical health symptoms and severity of physical health symptoms. While operationalizations of loneliness were correlated, none of the loneliness dynamics were considered multicollinear. Indeed, variance inflation factors were below three.
Main Associations Between Loneliness and Physical Health
Number of Physical Health Symptoms
Parameter estimates for models examining the main effects of average daily loneliness, intraindividual variability of daily loneliness, and loneliness stability are available in Model 1, Table 2. When exponentiated, these estimates represent the multiplicative increase in physical health symptoms associated with an increase in the loneliness variables. All three loneliness dynamics were significantly associated with physical health symptoms. For every one-standard deviation increase in daily average loneliness above the sample average (SD = 0.45) there was a multiplied expected number of physical health symptoms of e1.29 or 3.63, 95% confidence interval, CI [0.90, 1.67]. For every one standard deviation (SD = 0.33) increase in loneliness above a respondent’s personal average (WP) there was a multiplied expected number of physical health symptoms by e0.28 or 1.32, 95% CI [0.16, 0.39]. Finally, for every one standard deviation (SD = 0.77) increase in loneliness instability above the sample average (iRMSSD) there was a multiplied expected number of physical health symptoms by e0.41 or 1.51, 95% CI [0.19, 0.64]. As such, for people with higher average loneliness (BP), days when loneliness was higher than average (WP) and less stability in loneliness (iRMSSD), people reported significantly more physical health symptoms.
Table 2.
Fit Statistics and Parameter Estimates for Loneliness and Physical Health Models
| Fit statistics and parameter estimates | Number of physical health symptoms | Severity of physical health symptoms | ||
|---|---|---|---|---|
|
|
|
|||
| Model 1 Estimate (SE) [95% CI] | Model 3 Estimate (SE) [95% CI] | Model 2 Estimate (SE) [95% CI] | Model 4 Estimate (SE) [95% CI] | |
|
| ||||
| −2LL | 33,824.89 | 33,815.27 | 41,169.70 | 41,174.20 |
| BIC | 34,088.57 | 34,100.93 | 41,199.00 | 41,203.50 |
| Random intercept Cov | 5.83 (0.28) | 5.85 (0.28) | 1.57 (0.07) | 1.57 (0.07) |
| Random WP loneliness slope Cov | 0.07 (0.06) | 0.01 (0.05) | 0.08 (0.04) | 0.06 (0.04) |
| Intercept | 2.83 (0.12)*** [2.46,3.20] | 2.92 (0.19)*** [2.54, 3.30] | 2.54 (0.10)*** [2.34,2.73] | 2.54 (0.10)*** [2.35, 2.77] |
| BPs | ||||
| Average loneliness (BP) | 1.29 (0.17)*** [0.90, 1.67] | 1.89 (0.25)*** [1.40, 2.38] | 0.73 (0.11)*** [0.52,0.94] | 0.75 (0.13)*** [0.49, 1.02] |
| Loneliness stability (iRMSSD) | 0.41 (0.12)*** [0.19,0.64] | 0.44 (0.12)*** [0.20, 0.67] | 0.10 (0.06) [−0.02, 0.22] | 0.11 (0.06) [−0.01, 0.24] |
| BP × iRMSSD | — | −0.38 (0.11)** [−0.64, −0.12] | — | −0.02 (0.07) [−0.16, 0.12] |
| WPs | ||||
| Intraindividual loneliness variability (WP) | 0.28 (0.06)*** [0.16,0.39] | 0.40 (0.11)*** [0.19, 0.61] | 0.09 (0.04)* [0.01, 0.18] | 0.28 (0.08)*** [0.11, 0.44] |
| BP × WP | — | −0.07 (0.09) [−0.24, 0.10] | — | 0.01 (0.07) [−0.13, 0.14] |
| iRMSSD × WP | — | −0.04 (0.06) [−0.15, 0.07] | — | −0.11 (0.05)* [−0.20, −0.02] |
Note. All models covary for day in study, BMI (centered on the grand mean), any health condition, age (centered on the grand mean), gender, education, minority status, and marital status. Models 1 and 3 utilize generalized linear mixed models and Models 2 and 4 utilize general linear mixed models. CI = confidence interval; −2LL = −2 log-likelihood; BIC = Bayesian information criteria; Cov = covariates; WP = within-person; BP = between-person; iRMSSD = individual mean-squared successive difference; BMI =body mass index.
p<.05.
p<.01.
p<.001.
Physical Health Symptom Severity
As noted in Model 3 in Table 2, both average level of loneliness (BP) and intraindividual variability in daily loneliness (WP) were significantly associated with physical health symptom severity. Participants who, on average, reported more loneliness across study days, also reported higher physical symptom severity, b = 0.73, SE = 0.11, p < .001, 95% CI [0.53, 0.94]. Further, days when participants reported more loneliness than their personal average, they additionally reported higher physical health symptom severity, b = 0.09, SE = 0.04, p = .03, 95% CI: [0.01, 0.18]. Less stability in loneliness showed a similar, but nonstatistically significant pattern of associations. As such, for participants with higher average loneliness (BP) or days when loneliness was higher than average (WP), participants also reported significantly more severe physical health symptoms.
Interactions Between Loneliness Operationalizations and Physical Health Symptoms
Number of Physical Health Symptoms
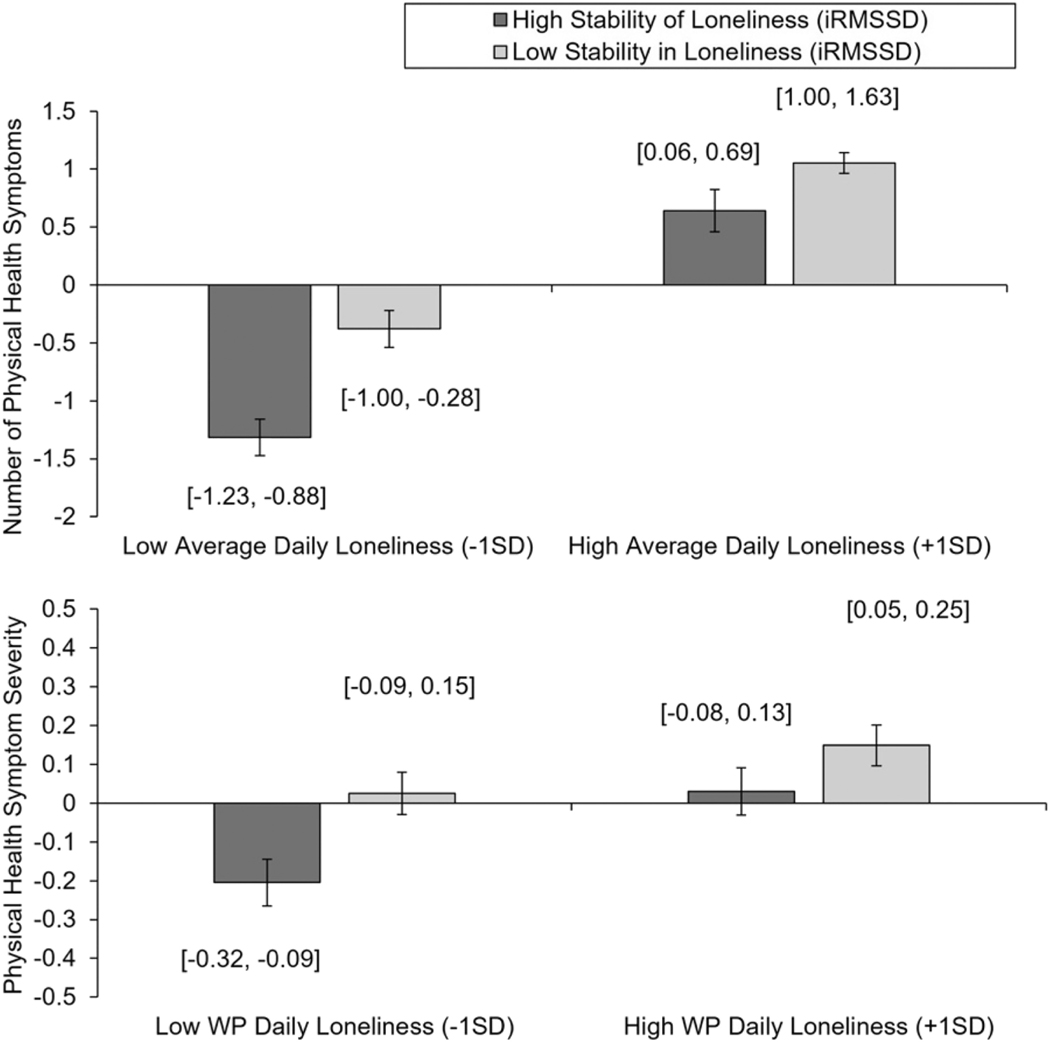
There was one significant interaction between average loneliness (BP) and stability in loneliness (iRMSSD) associated with the number of physical health symptoms (see Model 2, Table 2). As shown in Panel A, Figure 1, low iRMSSD related to a stronger link between average daily loneliness (BP) and the number of physical health symptoms. Specifically, at low iRMSSD (e.g., −1SD), the multiplicative link with physical health symptoms increased by e98 or 2.66, 95% CI [0.69, 1.63], per each SD increase in average loneliness; at high iRMSSD (e.g., +1SD), the multiplicative association with physical health symptoms increased by e72 or 2.05, 95% CI [0.54, 0.90], per each SD increase in average loneliness. Although the estimate of average loneliness suggests that more average loneliness is related to reporting more physical health symptoms, this association is stronger for participants with more stability in loneliness.
Figure 1. Effects of Loneliness Dynamics on Severity of Physical Health Symptoms.
Note. Error bars represent standard error. Slopes for average loneliness (BP) and daily loneliness (WP) were significant. iRMSSD = individual mean-squared successive difference; BP = between-person; WP = within-person.
At low average loneliness (BP, e.g., −1SD), the multiplicative association with physical health symptoms increased by e.47 or 1.60, 95% CI [0.25, 0.69], per each SD increase in iRMSSD loneliness; at high average loneliness (BP, e.g., +1SD), the multiplicative association with physical health symptoms increased by e21 or 1.23, 95% CI [0.03, 0.38], per each SD increase in iRMSSD loneliness. Therefore, although the slope of iRMSSD suggests that more instability in loneliness across 8 days is associated with reporting more physical health symptoms, this slope is larger for participants with low average loneliness.
Physical Health Symptom Severity
Daily loneliness (WP) and stability in loneliness (iRMSSD) significantly interacted (Table 2, Model 2). The association between daily loneliness and physical health symptom severity was stronger for participants with high iRMSSD (Panel B, Figure 1). On days when participants report higher loneliness than their average, the slope of loneliness stability was not significant, Estimate = 0.06, SE = 0.05, p = .23, 95% CI [−0.04, 0.16]. On days when participants reported less loneliness than their average, the slope for loneliness stability was significant, Estimate = 0.12, SE = 0.05, p = .02, 95% CI [0.02, 0.21]. Participants with more loneliness stability reported less severe expected physical health symptoms on lower-than-average loneliness days compared to participants with less loneliness stability.
Sensitivity Analyses
Associations After Including Negative Affect
Given evidence that negative affect may inform associations with loneliness or physical health (Yanguas et al., 2018), we examined whether the current study associations remained after accounting for negative affect within the day. The significant associations between (a) average loneliness and stability in loneliness on the number of physical health symptoms and (b) WP loneliness and stability in loneliness on the severity of physical health symptoms remained the same (ps < .05; see Table S2 in the online supplemental materials). However, as noted in Table S2 in the online supplemental materials, the main associations between daily WP loneliness and both the number (e07 or 1.07, 95% CI [−0.04, 0.19]) and severity (Estimate = −0.04 SE = 0.04, 95% CI [−0.13, 0.04]) of physical health symptoms was no longer significant after the inclusion of daily negative affect.
Lagged Associations
Given the potential for loneliness to inform next-day levels of physical health symptomology, we examined the lagged associations of WP daily loneliness associated with physical health symptoms. After accounting for next day loneliness and previous day physical health, WPs loneliness in the day was related to a fewer number of next-day physical health symptoms (e−0.21 or 0.81, 95% CI [−0.34, −0.05]), but not the severity (see Table S3 in the online supplemental materials).
Discussion
The present work examines three different temporal dynamics of daily loneliness and their associations with self-reported physical health symptomology among a large sample of healthy middle-aged adults. Investigating these associations during midlife—a time when loneliness may increase (Hawkley et al., 2022)—is critical to better understanding how daily loneliness and health are linked in midlife. The current study provides information to identify when (e.g., days when loneliness is higher or during times of instability) and for whom (e.g., lonelier people) associations between loneliness and physical health symptoms are strongest. Of note, we operationalized daily loneliness as a person’s (a) average levels of daily loneliness, (b) intraindividual variability, and (c) loneliness stability from day to day. These temporal dynamics in daily loneliness enable novel assessments of the variable experience of daily loneliness in connection to health and may be utilized to help promote symptom management.
Average Daily Loneliness
Consistent with the extant literature (e.g., Buecker et al., 2024; Jessen et al., 2018; Svensson et al., 2022), people with higher average daily loneliness reported greater and more severe physical health symptoms. Past work examining individual differences in loneliness and physical health symptomology has typically relied on single assessments of trait loneliness (e.g., Svensson et al., 2022). Associations with aggregates of daily loneliness have typically been studied among specific subgroups like adults with fibromyalgia (Wolf & Davis, 2014), which may not generalize to a broader population. The current study provided evidence that previous known associations between daily average loneliness and health extend to a healthy, nonclinical sample of middle-aged adults in the United States. Notably, however, this sample of adults reported relatively low levels of daily loneliness and associations may be exacerbated for people with more chronic levels of loneliness. Replication of the current findings in a lonelier population will be important for understanding associations. Further, it may be useful to develop interventions that simultaneously prompt individuals to engage in both social connection and physical health to promote daily health and well-being. This type of intervention is being implemented in people under the age of 19 (Wray et al., 2020), but rarely in midlife. Indeed, the Centers for Disease Control provides recommendations such as running or lifting weights (Centers for Disease Control and Prevention, 2022) to improve physical health in midlife, but does not include guidelines for physical activities that also clearly include social connections. Health professionals may consider recommending treatments that help manage both physical health symptoms and decrease loneliness for middle-aged adults.
Loneliness Variability
We used two aspects of daily loneliness variability: intraindividual variability and stability. Although intraindividual variability and stability are commonly used to study daily psychosocial experiences, like stress (Cerino & Hooker, 2019) and emotions (Houben et al., 2015), few studies have examined intraindividual variability and stability in loneliness. We addressed this gap in the literature by leveraging intensive repeated assessments to examine loneliness as it unfolds on a daily timescale and found significant associations for both intraindividual variability and stability in loneliness. We found that days characterized as lonelier than typical for a person were associated with greater and more severe self-reported physical health symptoms. Our findings also showed that people with less stable feelings of loneliness (i.e., larger differences in loneliness from day to day) also report more (but not more severe) physical health symptoms. Loneliness stability may relate to individual difference characteristics (e.g., neuroticism, depression). Although depression was controlled for in our measurement of chronic health conditions, it stands to reason that large fluctuations in loneliness across days may be at least partially accounted for by personality or mental health. As such, future research may examine how depression or neuroticism may modify current associations.
The findings with loneliness variability may relate to biological mechanisms related to health. Biological pathways (e.g., inflammation) can be upregulated during feelings of social disconnection—termed conserved transcriptional response to adversity (Cole, 2013; Eisenberger et al., 2017). This inflammatory response may then be related to physical health symptomology seen in the current study (e.g., fatigue, stomach-related issues). Importantly, we controlled for chronic health conditions, which should reduce the influence of substantial health conditions on the current sample’s daily loneliness and physical health reports. However, future work should further examine how biological mechanisms (e.g., inflammation) may inform the links between daily loneliness variability and physical health symptomology.
Because loneliness is the perceived discrepancy between actual and desired social relationships (Peplau & Perlman, 1982), the frequency or quality of social interactions and relationships throughout daily life may be particularly relevant to daily loneliness variability. Low intraindividual variability in loneliness or loneliness stability may be related to the consistency or frequency of high-quality social interactions (e.g., Zhaoyang et al., 2022). At the daily level, better quality social interactions (e.g., high responsiveness) were linked with lower levels of loneliness (Kuczynski et al., 2022). Given no studies to the authors’ knowledge have tested associations between the quality of daily social interactions, loneliness variability (i.e., intraindividual variability or stability), and physical health, future work could examine this link. Both intraindividual variability and stability provide more information that characterizes day-to-day experiences than any one-time point measure, including one or both temporal dynamic of loneliness. Thus, they may provide information about daily experiences that can be applied to interventions surrounding these phenomena.
Interestingly, sensitivity analyses covarying for daily negative affect revealed that intraindividual variability in loneliness was sensitive to other daily negative emotions. Researchers and clinicians acknowledge that loneliness encompasses negative affect such as sadness (Yanguas et al., 2018) and more daily loneliness has been linked with increased negative affect (Newman & Sachs, 2020); as such, the effect of daily loneliness on physical health may be directly related to negative affect. These findings suggest that there may be utility in considering emotion-related frameworks when examining daily loneliness; indeed, although distinct from emotions (e.g., Cramer & Barry, 1999), researchers may leverage emotion regulation strategies to better understand how and when increased daily loneliness may occur (Preece et al., 2021).
Interactions Between Daily Loneliness Dynamics and Physical Health
Our second aim addressed the interactions between aspects of daily loneliness in relation to physical health symptomology. Like previous studies examining various temporal dynamics of loneliness in adolescents (van Roekel et al., 2018) and older adults (Zhaoyang et al., 2022), the results of the current study underscore the utility of assessing multiple temporal dynamics to capture the complex phenomena of loneliness in midlife. Indeed, our results provide evidence that having large fluctuations in loneliness may be particularly detrimental to people with low loneliness on average. Our findings also showed that people with more stable loneliness reported less severe physical symptoms but only on days with lower-than-average reported loneliness. The current study additionally highlights the importance of examining loneliness stability when characterizing other temporal dynamics of loneliness. Indeed, loneliness stability interacted with both average daily loneliness and intraindividual variability in loneliness to inform aspects of physical health symptomology. Dynamic systems theory states that characterizing how stable a phenomenon is across timescale is crucial to understanding the phenomena itself (Thelen, 2005). It may be particularly important to capture these dynamics during daily life to disentangle stable, chronic loneliness, from daily, fluctuations of loneliness. Indeed, understanding the temporal dynamics of loneliness provides more and offers more unique information than any one measure from each source of variation of loneliness. Depending on what interventionists, theorists, or other researchers are examining (number or severity of health symptoms for example), it may be important to include one or all these temporal considerations.
Moreover, additional analyses revealed that days when people reported more loneliness(t), they also reported fewer physical health symptoms the next day (t + 1), even after accounting for concurrent physical health(t) and next-day loneliness(t + 1). It may be that the loneliness may result from preventative measures associated with sickness (e.g., staying home when sick) and thus may be helpful in preventing these symptoms. Importantly, this may highlight a cyclical, bidirectional association between health and loneliness. Changes to the social environment may be a mechanism tying loneliness to poorer health (Hawkley & Cacioppo, 2010); but the reverse association may also be plausible. For example, someone beginning to feel ill may cancel plans, increasing loneliness, but in doing so may have mitigated health symptoms the next day because they rested. Thus, future research will need to disentangle bidirectional associations between loneliness and physical health symptoms.
Public health interventions addressing loneliness may be most effective if they promote social connection in people’s everyday lives in ways that foster stable, low levels of loneliness. Indeed, interactions between temporal dynamics of loneliness were largely related to loneliness stability. Importantly, loneliness interventions focus on one-time activities or trainings (for review see Fakoya et al., 2020) and, as such, may not be effective for combating daily loneliness, fluctuations in daily loneliness, or reduce health consequences of loneliness. Moreover, loneliness interventions often focus on young children, adolescents, and older adulthood; with changing social roles in midlife it becomes to qualify the importance of decreasing loneliness in daily life. Addressing different dynamics of daily loneliness (i.e., average, intraindividual variability, stability) may improve daily life and more downstream health outcomes in midlife and promote health aging. Symptoms assessed in the current study included upper respiratory symptoms (e.g., sore throat), aches (e.g., headache, backache), and gastrointestinal symptoms (e.g., stomach problems)—all of which could be early indicators or manageable symptoms of more serious health-related outcomes. Understanding how psychosocial factors such as loneliness are related to these physical health symptoms can help researchers determine what modifiable daily experiences may be opportune targets for interventions and promoting health.
Limitations and Future Directions
Although we leveraged a large, national data set, the current sample was mostly White, limiting our ability to speak to the links between loneliness and self-reported physical health among other racial and ethnic groups. As there are racial and ethnic differences in links between loneliness and health outcomes (John-Henderson et al., 2021; Taylor & Nguyen, 2020) and as the incidence of loneliness may differ across races and ethnicities (Fokkema et al., 2012), future work should disentangle associations between daily loneliness and physical health for different racialized groups. Further, increasing the frequency of assessments may reduce the potential for retrospective biases that occur in end-of-day daily measurement. Future work expanding daily diary to momentary repeated measurements of loneliness is needed to better understand the temporal dynamics of loneliness across time. Collecting more than 8 days of data will also enable researchers to account for environmental factors not tested in the current study (e.g., a fall could result in pain across the week). Although we covaried for day of study and whether the study day was a weekend, or weekday, the shorter timescale of collection may limit our ability to account for possible nonnormative weeks in participants lives.
Moreover, we assessed loneliness using a single-item measure. Although single-item measures of loneliness have acceptable reliability and convergent validity comparable to multiitem measures (e.g., Mund et al., 2023), as with any self-report item, there is still a possibility for self-reporting bias and potentially inflated correlations between loneliness and self-reported physical health. For instance, if a participant feels poorly at the end of the day, they may self-report higher levels of both loneliness and physical health symptoms as they reflect negatively on their daily experiences. This study is a necessary first step to understand loneliness in daily life and its associations with health and should not preclude the study of these phenomena (e.g., Estabrook et al., 2012). Although there is strength in the repeated measure assessments and the large data set, future work will need to examine these associations using multi-item measures of loneliness or more objective measures of physical health. Finally, the current analyses are examining concurrent associations between WP daily loneliness and physical health symptoms, and, as such, we did not determine temporal patterning for these associations. It will be crucial for future research to examine both bidirectional associations and physical health symptoms to better understand the directionality of associations.
Conclusion
The U.S. Surgeon General (2023) acknowledges that one of the pillars to advance social connection is to deepen the knowledge of the phenomena of loneliness and risks associated with loneliness. Indeed, loneliness is a serious public health concern and tremendous economic burden (Mihalopoulos et al., 2020) in the United States. Feeling socially connected is crucial for health and well-being across the lifespan and prominent researchers have called for loneliness to be considered a public health priority (Holt-Lunstad, 2017). Even with theoretical precedent to examine short-term dynamics of phenomena like loneliness (e.g., Nesselroade, 1991) and evidence that loneliness fluctuates or changes across moments and days (Mund et al., 2020), links between daily loneliness and health are rarely evaluated. The current study provides crucial preliminary evidence for how three meaningful temporal dynamics of daily loneliness are associated with physical health symptoms. Rather than treating loneliness as a stable experience, future research should draw on one or more dynamics of loneliness to better capture how daily loneliness relates to health and well-being outcomes. We conclude that the current study findings are useful in (a) characterizing that interventions and recommendations—particularly in midlife-focusing on physical health should embed ways for social connectedness and (b) loneliness interventions should focus on consistent, possible multitimescale interventions focusing on promoting consistent levels of (low) loneliness.
Supplementary Material
Public Significance Statement.
The current study found that different characterizations of daily loneliness (people with high loneliness across days, days when loneliness is higher, or people with highly fluctuating feelings of loneliness) have unique and interactive effects on the number and severity of daily physical health symptoms (e.g., fatigue, headaches). Results from this study contribute important information that can inform both study design and prevention or symptom management strategies.
Acknowledgments
Erin E. Harrington is now at Department of Psychology, University of Wyoming.
Dakota D. Witzel and Karina Van Bogart were supported in part by the National Institute on Aging Grant T32 AG049676 to The Pennsylvania State University; initial stages of this work were presented at the Gerontological Society Association Conference in 2018. Shelbie G. Turner’s work on this study was supported by the National Institutes of Health/National Institute on Aging (T32 AG049666).
Dakota D. Witzel served as lead for conceptualization, data curation, formal analysis, methodology, software, and visualization and contributed equally to writing–review and editing. Karina Van Bogart served in a supporting role for writing–review and editing. Erin E. Harrington served in a supporting role for writing–original draft and writing–review and editing. Shelbie G. Turner served in a supporting role for writing–review and editing and presented some information at conferences. David M. Almedia served in a supporting role for writing–review and editing.
Footnotes
Supplemental materials: https://doi.org/10.1037/hea0001377.supp
The authors have no conflicts of interest to disclose.
References
- Antonucci TC, Ajrouch KJ, & Birditt KS (2014). The convoy model: Explaining social relations from a multidisciplinary perspective. The Gerontologist, 54(1), 82–92. 10.1093/geront/gnt118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergeman CS, Blaxton J, & Joiner R. (2021). Dynamic systems, contextual influences, and multiple timescales: Emotion regulation as a resilience resource. The Gerontologist, 61(3), 304–311. 10.1093/geront/gnaa046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buecker S, Horstmann KT, & Luhmann M. (2024). Lonely today, lonely tomorrow: Temporal dynamics of loneliness in everyday life and its associations with psychopathological symptoms. Social Psychological and Personality Science, 15(2), 170–181. 10.1177/19485506231156061 [DOI] [Google Scholar]
- Cacioppo JT, & Cacioppo S. (2018a). The growing problem of loneliness. The Lancet, 391(10119), Article 426. 10.1016/S0140-6736(18)30142-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, & Cacioppo S. (2018b). Loneliness in the modern age: An evolutionary theory of loneliness (ETL). Advances in Experimental Social Psychology, 58(1), 127–197. 10.1016/bs.aesp.2018.03.003 [DOI] [Google Scholar]
- Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, & Thisted RA (2006). Loneliness as a specific risk factor for depressive symptoms: Cross-sectional and longitudinal analyses. Psychology and Aging, 21(1), 140–151. 10.1037/0882-7974.21.1.140 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2022). Physical activity: Adults. https://www.cdc.gov/physicalactivity/basics/adults/index.htm
- Cerino ES, & Hooker K. (2019). Intraindividual variability in lifespan developmental methodology. In Braddick O. (Ed.), Oxford research encyclopedia of psychology (pp. 1–18). Oxford University Press. [Google Scholar]
- Cole SW (2013). Social regulation of human gene expression: Mechanisms and implications for public health. American Journal of Public Health, 103(S1), S84–S92. 10.2105/AJPH.2012.301183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coyle CE, & Dugan E. (2012). Social isolation, loneliness and health among older adults. Journal of Aging and Health, 24(8), 1346–1363. 10.1177/0898264312460275 [DOI] [PubMed] [Google Scholar]
- Cramer KM, & Barry JE (1999). Conceptualizations and measures of loneliness: A comparison of subscales. Personality and Individual Differences, 27(3), 491–502. 10.1016/S0191-8869(98)00257-8 [DOI] [Google Scholar]
- Eisenberger N, Moieni M, Inagaki T, Muscatell KA, & Irwin MR (2017). In sickness and health: The co-regulation of inflammation and social behavior. Neuropsychopharmacology, 42(1), 242–253. 10.1038/npp.2016.141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estabrook R, Grimm KJ, & Bowles RP (2012). A Monte Carlo simulation study of the reliability of intraindividual variability. Psychology and Aging, 27(3), 560–576. 10.1037/a0026669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fakoya OA, McCorry NK, & Donnelly M. (2020). Loneliness and social isolation interventions for older adults: A scoping review of reviews. BMC Public Health, 20(1), Article 129. 10.1186/s12889-020-8251-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fokkema T, De Jong Gierveld J, & Dykstra PA (2012). Cross-national differences in older adult loneliness. The Journal of Psychology, 146(1–2), 201–228. 10.1080/00223980.2011.631612 [DOI] [PubMed] [Google Scholar]
- Hardy J, & Segerstrom SC (2017). Intra-individual variability and psychological flexibility: Affect and health in a National US sample. Journal of Research in Personality, 69(1), 13–21. 10.1016/j.jrp.2016.04.002 [DOI] [Google Scholar]
- Hawkley LC, Buecker S, Kaiser T, & Luhmann M. (2022). Loneliness from young adulthood to old age: Explaining age differences in loneliness. International Journal of Behavioral Development, 46(1), 39–49. 10.1177/0165025420971048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley LC, & Cacioppo JT (2010). Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Annals of Behavioral Medicine, 40(2), 218–227. 10.1007/s12160-010-9210-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodgson S, Watts I, Fraser S, Roderick P, & Dambha-Miller H. (2020). Loneliness, social isolation, cardiovascular disease and mortality: A synthesis of the literature and conceptual framework. Journal of the Royal Society of Medicine, 113(5), 185–192. 10.1177/0141076820918236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman L, & Stawski RS (2009). Persons as contexts: Evaluating between-person and within-person effects in longitudinal analysis. Research in Human Development, 6(2–3), 97–120. 10.1080/15427600902911189 [DOI] [Google Scholar]
- Holt-Lunstad J. (2017). The potential public health relevance of social isolation and loneliness: Prevalence, epidemiology, and risk factors. Public Policy & Aging Report, 27(4), 127–130. 10.1093/ppar/prx030 [DOI] [Google Scholar]
- Holt-Lunstad J, Smith TB, Baker M, Harris T, & Stephenson D. (2015). Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspectives on Psychological Science, 10(2), 227–237. 10.1177/1745691614568352 [DOI] [PubMed] [Google Scholar]
- Houben M, Van Den Noortgate W, & Kuppens P. (2015). The relation between short-term emotion dynamics and psychological well-being: A meta-analysis. Psychological Bulletin, 141(4), 901–930. 10.1037/a0038822 [DOI] [PubMed] [Google Scholar]
- Infurna FJ, Gerstorf D, & Lachman ME (2020). Midlife in the 2020s: Opportunities and challenges. American Psychologist, 75(4), 470–485. 10.1037/amp0000591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Infurna FJ, Staben OE, Lachman ME, & Gerstorf D. (2021). Historical change in midlife health, well-being, and despair: Cross-cultural and socioeconomic comparisons. American Psychologist, 76(6), 870–887. 10.1037/amp0000817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahng S, Wood PK, & Trull TJ (2008). Analysis of affective instability in ecological momentary assessment: Indices using successive difference and group comparison via multilevel modeling. Psychological Methods, 13(4), 354–375. 10.1037/a0014173 [DOI] [PubMed] [Google Scholar]
- Jessen MAB, Pallesen AVJ, Kriegbaum M, & Kristiansen M. (2018). The association between loneliness and health—A survey-based study among middle-aged and older adults in Denmark. Aging & Mental Health, 22(10), 1338–1343. 10.1080/13607863.2017.1348480 [DOI] [PubMed] [Google Scholar]
- John-Henderson NA, Oosterhoff B, Kothe KM, Kampf TD, Hall B, Johnson LR, LaFromboise ME, Malatare M, Salois EM, Adams AK, & Carter JR (2021). Loneliness and sleep in the American Indian Blackfeet community. Sleep Health, 7(4), 429–435. 10.1016/j.sleh.2021.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones DR, Ruiz JM, Schreier HMC, Allison MA, Uchino BN, Russell MA, & Taylor DJ (2023). Mean affect and affect variability may interact to predict inflammation. Brain, Behavior, and Immunity, 109(1), 168–174. 10.1016/j.bbi.2023.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ko H-J, Mejía S, & Hooker K. (2014). Social possible selves, self-regulation, and social goal progress in older adulthood. International Journal of Behavioral Development, 38(3), 219–227. 10.1177/0165025413512063 [DOI] [Google Scholar]
- Kuczynski AM, Halvorson MA, Slater LR, & Kanter JW (2022). The effect of social interaction quantity and quality on depressed mood and loneliness: A daily diary study. Journal of Social and Personal Relationships, 39(3), 734–756. 10.1177/02654075211045717 [DOI] [Google Scholar]
- Lachman ME, Teshale S, & Agrigoroaei S. (2015). Midlife as a pivotal period in the life course: Balancing growth and decline at the crossroads of youth and old age. International Journal of Behavioral Development, 39(1), 20–31. 10.1177/0165025414533223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leger KA, Charles ST, Ayanian JZ, & Almeida DM (2015). The association of daily physical symptoms with future health. Social Science & Medicine, 143(1), 241–248. 10.1016/j.socscimed.2015.08.050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo Y, Hawkley LC, Waite LJ, & Cacioppo JT (2012). Loneliness, health, and mortality in old age: A national longitudinal study. Social Science & Medicine, 74(6), 907–914. 10.1016/j.socscimed.2011.11.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mihalopoulos C, Le LK-D, Chatterton ML, Bucholc J, Holt-Lunstad J, Lim MH, & Engel L. (2020). The economic costs of loneliness: A review of cost-of-illness and economic evaluation studies. Social Psychiatry and Psychiatric Epidemiology, 55(7), 823–836. 10.1007/s00127-019-01733-7 [DOI] [PubMed] [Google Scholar]
- Mund M, Lüdtke O, & Neyer FJ (2020). Owner of a lonely heart: The stability of loneliness across the life span. Journal of Personality and Social Psychology, 119(2), 497–516. 10.1037/pspp0000262 [DOI] [PubMed] [Google Scholar]
- Mund M, Maes M, Drewke PM, Gutzeit A, Jaki I, & Qualter P. (2023). Would the real loneliness please stand up? The validity of loneliness scores and the reliability of single-item scores. Assessment, 30(4), 1226–1248. 10.1177/10731911221077227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. (2020). Social isolation and loneliness in older adults: Opportunities for the health care system. National Academies Press. [PubMed] [Google Scholar]
- Nesselroade J. (1991). The warp and woof of the developmental fabric. In Downs R, Liben L, & Palermo D. (Eds.), Visions of aesthetics, the environment & development: The legacy of Joachim F. Wohlwill (pp. 214–242). Erlbaum. [Google Scholar]
- Newman DB., & Sachs ME. (2020). The negative interactive effects of nostalgia and loneliness on affect in daily life. Frontiers in Psychology, 11(1), 2185–2219. 10.3389/fpsyg.2020.02185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peplau LA, & Perlman D. (1982). Loneliness: A sourcebook of current theory, research, and therapy (Vol. 36). Wiley. [Google Scholar]
- Preece DA, Goldenberg A, Becerra R, Boyes M, Hasking P, & Gross JJ (2021). Loneliness and emotion regulation. Personality and Individual Differences, 180(3), 110974–110995. 10.1016/j.paid.2021.110974 [DOI] [Google Scholar]
- Svensson M, Rosso A, Elmståhl S, & Ekström H. (2022). Loneliness, social isolation, and health complaints among older people: A population-based study from the “Good Aging in Skåne (GÅS)” project. SSM—Population Health, 20(1), 101287–101295. 10.1016/j.ssmph.2022.101287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor HO, & Nguyen AW (2020). Depressive symptoms and loneliness among black and white older adults: The moderating effects of race. Innovation in Aging, 4(5), Article igaa048. 10.1093/geroni/igaa048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thelen E. (2005). Dynamic systems theory and complexity of change. Psychoanalytic Dialogues, 15(2), 255–283. 10.1080/10481881509348831 [DOI] [Google Scholar]
- Thelen E, & Smith LB (2006). Dynamic systems theories. In Lerner R(Ed.), Handbook of child psychology: Theoretical models of human development (Vol. 1, 6th ed., pp. 258–312). John Wiley & Sons. [Google Scholar]
- U.S. Surgeon General. (2023). Our epidemic of loneliness and isolation: The U.S. Surgeon General’s advisory on th.e healing effects of social connection and community U.S. Department of Health and Human Services; https://hhs.gov/sites/default/files/surgeon-general-social-connection-advisory.pdf [PubMed] [Google Scholar]
- van Roekel E, Verhagen M, Engels RCME, Scholte RHJ, Cacioppo S, & Cacioppo JT (2018). Trait and state levels of loneliness in early and late adolescents: Examining the Differential Reactivity Hypothesis. Journal of Clinical Child & Adolescent Psychology, 47(6), 888–899. 10.1080/15374416.2016.1146993 [DOI] [PubMed] [Google Scholar]
- Victor CR, Scambler SJ, Bowling A, & Bond J. (2005). The prevalence of, and risk factors for, loneliness in later life: A survey of older people in Great Britain. Ageing and Society, 25(6), 357–375. 10.1017/S0144686X04003332 [DOI] [Google Scholar]
- Watson D, Clark LA, & Tellegen A. (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54(6), 1063–1070. 10.1037/0022-3514.54.6.1063 [DOI] [PubMed] [Google Scholar]
- Wolf LD, & Davis MC (2014). Loneliness, daily pain, and perceptions of interpersonal events in adults with fibromyalgia. Health Psychology, 33(9), 929–937. 10.1037/hea0000059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wray A, Martin G, Ostermeier E, Mederios A, Little M, Reilly K, & Gilliand J. (2020). Evidence synthesis—Physical activity and social connectedness interventions in outdoor spaces among children and youth: A rapid review. Health Promotion and Chronic Disease Prevention in Canada, 40(4), 104–115. 10.24095/hpcdp.40.4.02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yanguas J, Pinazo-Henandis S, & Tarazona-Santabalbina FJ (2018). The complexity of loneliness. Acta Bio Medica: Atenei Parmensis, 89(2), 302–314. 10.23750/abm.v89i2.7404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhaoyang R, Harrington KD, Scott SB, Graham-Engeland JE, & Sliwinski MJ (2022). Daily social interactions and momentary loneliness: The role of trait loneliness and neuroticism. The Journals of Gerontology: Series B, 77(10), 1791–1802. 10.1093/geronb/gbac083 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.