ABSTRACT
Objective:
To investigate the repercussions of COVID-19 on the length of breastfeeding and analyze the associated factors in Belo Horizonte, Minas Gerais, Brazil.
Method:
This is an epidemiological, prospective cohort study. Data were collected from medical records and through telephone interviews. Women who weaned were estimated using Kaplan-Meier survival analysis. The log-rank test was used to verify differences between groups, analyzing weaning time, according to sociodemographic and clinical characteristics. The values of hazard ratio and 95% confidence intervals were estimated using Cox regression analysis.
Results:
A total of 1,729 women participated in the study. During the COVID-19 pandemic, brown women and women undergoing cesarean section were more likely to stop breastfeeding.
Conclusion:
The birth route and mothers’ ethnic characteristics were associated with early weaning during the COVID-19 pandemic. Such findings are important to guide the assistance of the multidisciplinary team, especially nursing, during the post-pandemic period and in future epidemiological scenarios.
DESCRIPTORS: Pandemics, Breast Feeding, Weaning, Nursing
RESUMO
Objetivo:
Investigar as repercussões da COVID-19 na duração do aleitamento materno e analisar os fatores associados em Belo Horizonte, Minas Gerais, Brasil.
Método:
Trata-se de estudo epidemiológico, de coorte prospectiva. Os dados foram coletados em prontuários médicos e por meio de entrevistas telefônicas. As mulheres que apresentaram o desmame foram estimadas por meio da análise de sobrevivência de Kaplan-Meier. O teste log-rank foi utilizado para verificar diferenças entre os grupos, analisando-se o tempo de desmame, segundo as características sociodemográficas e clínicas. Os valores de hazard ratio e intervalos de confiança de 95% foram estimados utilizando-se análise de regressão de Cox.
Resultados:
Participaram da pesquisa 1.729 mulheres. Durante a pandemia de COVID-19, mulheres pardas e mulheres submetidas à cesariana foram mais suscetíveis a interromper a amamentação.
Conclusão:
A via de nascimento e as características étnicas das mães associaram-se ao desmame precoce durante a pandemia de COVID-19. Tais achados são importantes para nortear a assistência da equipe multiprofissional, sobretudo da enfermagem, durante o pós-pandemia e em cenários epidemiológicos futuros.
DESCRITORES: Pandemias, Aleitamento Materno, Desmame, Enfermagem
RESUMEN
Objetivo:
Investigar las repercusiones de la COVID-19 en la duración de la lactancia materna y analizar los factores asociados en Belo Horizonte, Minas Gerais, Brasil.
Método:
Se trata de un estudio de cohorte prospectivo epidemiológico. Los datos se recogieron de historias clínicas y mediante entrevistas telefónicas. Las mujeres que destetaron se estimaron mediante el análisis de supervivencia de Kaplan-Meier. La prueba de Mantel-Cox se utilizó para verificar diferencias entre grupos, analizando el tiempo de destete, según características sociodemográficas y clínicas. Los valores de cociente de riesgo y los intervalos de confianza del 95% se estimaron mediante análisis de regresión de Cox.
Resultados:
Un total de 1.729 mujeres participaron en la investigación. Durante la pandemia de COVID-19, las mujeres pardas y aquellas sometidas a cesárea tenían más probabilidades de dejar de amamantar.
Conclusión:
La ruta de nacimiento y las características étnicas de las madres se asociaron con el destete temprano durante la pandemia de COVID-19. Tales hallazgos son importantes para orientar la asistencia del equipo multidisciplinario, especialmente de enfermería, durante el período pospandemia y en futuros escenarios epidemiológicos.
DESCRIPTORES: Pandemias, Lactancia Materna, Destete, Enfermería
INTRODUCTION
Breastfeeding, in addition to reducing infant mortality and strengthening the immune system, provides numerous other benefits to the immediate infant’s health, such as: adequate development of the stomatognathic system and prevention of respiratory infections(1,2). The advantages of the practice are also associated with a reduction in the occurrence, in adulthood, of diabetes mellitus, high blood pressure, and obesity(3,4). Breastfeeding can also indirectly impact adults’ income and intellectual levels(4).
Furthermore, breastfeeding is a practice that also benefits the nursing mother, as it is associated with a reduction in the incidence of breast, ovarian, and endometrial cancers, osteoporosis, multiple sclerosis, diabetes mellitus, high blood pressure, and cardiovascular diseases, and with strengthening of the mother-child emotional bond(5,6).
For these reasons, the World Health Organization (WHO) recommends that breast milk be the exclusive food (EBF) until 6 months of age and up to 24 months of age, at least, as a complementary food(2). Despite the advantages, the prevalence of breastfeeding in Brazil is far below the targets established by the WHO for the year 2030: the WHO recommends a prevalence of at least 60% of EBF, and the National Study of Child Food and Nutrition, carried out in 2019 by the Universidade Federal do Rio de Janeiro (UFRJ) indicates that only 35.5% of Brazilian children aged between 20 and 23 months continue breastfeeding(7).
This is explained by the fact that breastfeeding is a complex process and involves not only individual factors, but also family, cultural, historical-geographical and socioeconomic reasons, among others(8). In addition, COVID-19, a respiratory disease caused by the SARS-Cov-2 virus, has become an important influencing factor for breastfeeding(9). Some studies show benefits of the pandemic for breastfeeding(10,11), as demonstrated by a study carried out in the United States, which highlighted the positive effects of the measures of social isolation and staying at home on breastfeeding practices, specifically in this country where there are no remuneration policies during the period of maternity leave(12). However, in general, the pandemic was an influential circumstance for early weaning(13), especially when related to maternal mental health(14) and social and economic inequalities(15). In this regard, a systematic review identified the negative effects of the COVID-19 pandemic, mainly for family support, with influences on the continuity of breastfeeding(16).
In Brazil, there are few studies related to the topic addressed in this work. Considering the importance of breastfeeding for promoting maternal and child health and the repercussions of COVID-19 to the present day, which may have influenced the duration and maintenance of breastfeeding (exclusive or mixed), the identification of the incidence of weaning after SARS-COV-2 infection and its associated factors is required, aiming at contributing to future strategies that allow for better maintenance of breastfeeding.
The hypothesis of this study is that the pandemic influenced the duration and maintenance of breastfeeding. The objective of this study was to investigate the repercussions of COVID-19 on the length of breastfeeding and analyze the associated factors in Belo Horizonte, Minas Gerais, Brazil.
METHOD
Design of Study
This is an epidemiological, prospective cohort study, which had as its setting three hospitals that provide their services exclusively through the Brazilian Public Health System – SUS, in Belo Horizonte (BH), Minas Gerais (MG), Brazil, which are participants in the Research entitled “Childbirth and breastfeeding in children of mothers infected with SARS-CoV-2”.
Population, Local and Selection Criteria
Postpartum women with a single pregnancy were included, whose delivery was in a hospital and had as product their live newborn conceptuses (NB) aged 22 weeks or more, weighing more than 500 grams at birth. They were women admitted to the three maternity hospitals selected at the time of delivery and who went into labor (L) (induced or not) and whose birth was vaginal or C-section.
Sample Definition
For the sample calculation, the cohort study design was considered. A ratio of nine pregnant women in the unexposed group (without COVID-19) for each pregnant woman in the exposed group (with COVID-19) was considered, given the infection rate of 10% during the epidemic period(17). This was the proportion considered for the event in the unexposed group. Furthermore, Odds Ratio of 1.5 was estimated, for a confidence level of 95% and power of 80%. The distribution of the number of pregnant women by participating maternity hospitals followed the proportion of the total number of births in each selected maternity hospital. The sample was selected randomly, through a simple draw, until reaching the number of postpartum women for each hospital, totaling 1,729 postpartum women. As this was a prospective cohort study, the women were contacted 6 months after delivery to investigate EBF via telephone. In this process, 410 postpartum women were accessed. It should be noted those women who could not be reached through telephone were considered lost to follow-up.
Data Collection
The study data were collected from the medical records of hospital institutions, using a semi-structured questionnaire adapted from the research “Born in Belo Horizonte: Inquiry into labor and birth (Nascer em Belo Horizonte: Inquérito sobre o parto e nascimento”. The medical records of all women who had their children in the respective hospitals in the three months with the highest incidence of COVID-19 (May, June and July) in the first half of 2020, in Brazil, were analyzed.
After collecting the medical records, the postpartum women were contacted via telephone call after 2 months of delivery. They were also contacted 6 months after birth to investigate EBF. As a research protocol, the postpartum women were accessed at different times and telephone contact was made at least 5 times by trained researchers. In case of refusal or failure in these attempts, the postpartum woman was excluded.
The following variables were considered: sociodemographic (age, education, income, marital status, race/skin color), clinical (current/previous illnesses and previous surgeries, use of medication, symptoms and signs of SARS-COV-2), health status (smoking, alcohol consumption, intestinal habits, physical activity, monitoring with a health professional and vaccination), obstetric (number of births, route of birth, presence of a companion, practices and interventions during birth, reproductive outcome, and complications of the last delivery, support network, changes in care due to the COVID-19 pandemic, information about the occurrence of SARS-CoV-2 infection/symptoms in the participant and her child, including separation of the binomial), and specific information about breastfeeding (type, difficulties, interference of the COVID-19 pandemic in breastfeeding, milk donation, breastfeeding in the first hour of life). In relation to difficulty in breastfeeding, this variable was verified through reports from the postpartum woman about the occurrence of some “nipple trauma, hard, red, bruised breast, or need to use antibiotics”. Regarding the interference of the COVID-19 pandemic, this variable was according to the perception of the postpartum woman.
Data Analysis and Treatment
To analyze the association between sociodemographic and clinical characteristics with EBF, the statistical package Statistics Software for Data Science (Stata), version 16.0 was used. Initially, the population was described, and estimates were presented in proportions (%), with 95% CI. For quantitative variables, after asymmetry was verified using the Shapiro-Wilk test, data were presented using median and interquartile range (IQ).
The non-parametric statistical method of survival curves was used to estimate the fraction of women who weaned, using Kaplan-Meier estimates.
The log-rank test was used to check for the presence of differences between groups (weaning yes and no; p < 0.05), analyzing weaning time, according to sociodemographic and clinical characteristics.
Additionally, Hazard Ratio (HR) values and unadjusted 95% confidence intervals (95% CI) were estimated, using the Cox proportional hazards model. At the end, the adjusted analysis of the multivariate model was carried out, with the inclusion of variables that had a significance of up to 0.2 in the unadjusted analysis. The forward method was used, with one-by-one variables input following the decreasing level of significance.
Ethical Aspects
The study “Birth and breastfeeding in children of mothers infected by SARS-CoV-2 (Parto e aleitamento materno em filhos de mães infectadas por SARS-CoV-2)” was approved in 2022 by the Research Ethics Committee of the Universidade Federal de Minas Gerais (Opinion Number: 5.735.679).
RESULTS
In this study, 1,729 women were included. Table 1 shows the sociodemographic and clinical characteristics of the sample. Women’s median age was 28 years (IQ: 23-33), 88.65% had NBs with weight above 2,499 grams, 98.27% had no SAR-CoV-2 virus infection/suspicion. The majority of women were multiparous (62.32%) and had no clinical/obstetric complications (53.77%). Regarding the method of birth, the majority had their children vaginally (72.67%). Finally, there were higher proportions of women who had more than 6 prenatal consultations (77.50%).
Table 1. Demographic, socioeconomic, and obstetric profile of the sample of postpartum women – Belo Horizonte, MG, Brazil, 2020/2023 (n = 1729).
| Variables | n (%) | 95%CI |
|---|---|---|
| Age | 28(23–33) | |
| NB weight | ||
| Above 2499 | 1359(88.65) | 86.96–90.14 |
| Less than 2500 | 174(11.35) | 09.85–13.03 |
| SARS-CoV-2 infection | ||
| No | 1651(98.27) | 97.52–98.79 |
| Yes | 29(01.72) | 01.20–02.47 |
| Parity | ||
| Primiparous | 633(37.68) | 35.38–40.02 |
| Multiparous | 1047(62.32) | 59.97–64.61 |
| Clinical/obstetric complications | ||
| No | 813(53.77) | 51.24–56.27 |
| Yes | 699(46.23) | 43.72–48.75 |
| Presence of companion during birth | ||
| Yes | 1225(89.68) | 87.94–91.18 |
| No | 141(9.41) | 08.81–12.05 |
| Birth route | ||
| Vaginal | 1210(72.67) | 70.47–74.76 |
| C-section | 455(27.33) | 25.32–29.52 |
| NB complication | ||
| No | 1188(77.90) | 75.74–79.91 |
| Yes | 337(22.10) | 20.08–24.25 |
| Number of PN consultations | ||
| More than or equal to 6 visits | 589(77.50) | 74.38–80.33 |
| Less than 6 visits | 171(22.50) | 19.66–25.61 |
Notes: 1Median (IQ); NB: newborn; PN: prenatal.
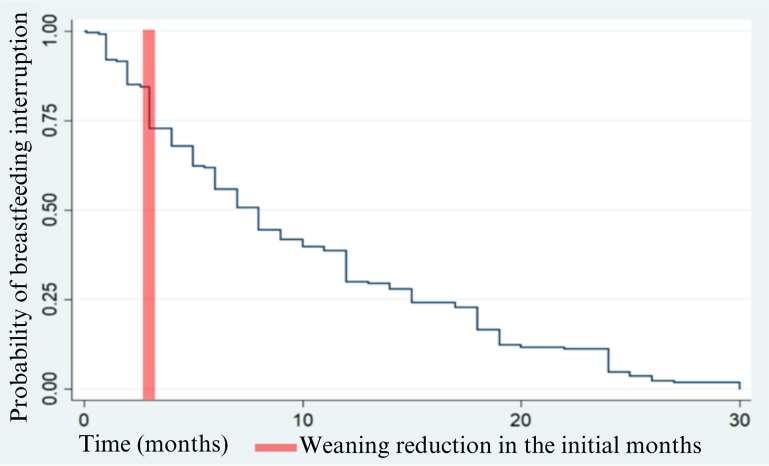
In Figure 1, the Kaplan-Meyer curve of probability of weaning survival is represented. During follow-up, 410 women were accessed and, of these, 53.66% weaned. The survival function (t) is represented on the vertical axis and the survival time (T), in months, on the horizontal axis. It indicates the probability that a woman will wean during a specific period of time. It is possible to state that the longer the time, the lower the probability of weaning, that is, weaning occurred mainly in the initial months after birth. Regarding the incidence of the weaning event, it was 99.41 per 1000 person-days (95%CI 86.36 – 114.43).
Figure 1. Kaplan-Meier curve relating the probability of interrupting breastfeeding (vertical axis) as a function of time in months (horizontal time).
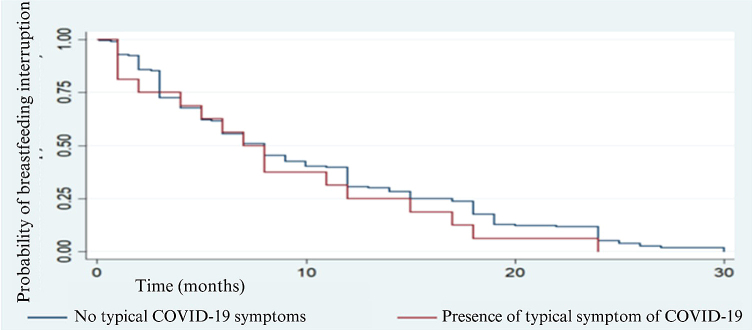
Figure 2, in its turn, demonstrates the probability of a weaning event in women who did or did not show symptoms or signs of COVID-19, with no statistical significance for the log-rank test (p = 0.348) when comparing the groups.
Figure 2. Probability of breastfeeding interruption without typical COVID-19 symptoms(blue) and with typical symptom of COVID-19 during breastfeeding (red).
Table 2 shows the weaning incidence rates (events/1000 person-days), according to the sample sociodemographic and clinical variables. A statistically significant difference was observed through the log-rank test for the interruption of breastfeeding when considering the self-reported skin color and the newborn’s birth route.
Table 2. Weaning incidence rates (events/1000 person-days), according to sociodemographic and clinical variables – Belo Horizonte, MG, Brazil, 2020/2023 (n = 410).
| Weaning | |||
|---|---|---|---|
| Incidence | 95%CI | p-value | |
| Level of education | 0.337 | ||
| Higher | 81.60 | (55.56–119.85) | |
| High School | 99.52 | (82.49–120.08) | |
| Elementary | 109.74 | (85.03–141.64) | |
| Income* | 0.684 | ||
| No income | 101.76 | (82.67–125.25) | |
| Less than 1 minimum wage | 93.54 | (74.48–117.47) | |
| Between 1 and 3 minimum wages | 108.51 | (76.31–154.30) | |
| Lives with partner | 0.759 | ||
| Yes | 97.46 | (77.72–122.22) | |
| No | 100.68 | (84.13–120.50) | |
| Postpartum consultation | 0.981 | ||
| Yes | 99.22 | (84.59–116.38) | |
| No | 96.94 | (71.11–132.16) | |
| Nipple trauma | 0.355 | ||
| Yes | 92.89 | (74.61–115.65) | |
| No | 102.31 | (84.18–124.34) | |
| Breast engorgement | 0.759 | ||
| Yes | 111.76 | (71.29–175.22) | |
| No | 108.68 | (83.02–142.25) | |
| Interferences due to COVID-19 | 0.105 | ||
| Yes | 76.27 | (52.30–111.21) | |
| No | 104.19 | (89.36–121.48) | |
| Self-declared skin color | 0.0355 | ||
| White | 87.67 | (63.52–121.01) | |
| Black | 80.11 | (58.76–109.22) | |
| Brown | 113.58 | (94.75–136.14) | |
| Birth route | 0.0459 | ||
| Vaginal | 93.72 | (79.69–110.23) | |
| Cesarean section | 121.93 | (91.88–161.79) | |
Notes: *The minimum wage in force at the time was R$1,039.00; p-value in bold: statistical significance for the log-rank test.
DISCUSSION
The general results of this study demonstrated that characteristics such as self-reported skin color and the newborn’s birth route were influencing factors in weaning rates during the COVID-19 pandemic.
Regarding the method of birth, women undergoing cesarean section were more likely to interrupt breastfeeding. In this regard, the strong influence of cesarean sections on difficulties in the breastfeeding process or early weaning is recognized, since in this type of surgery newborns are less exposed to skin-to-skin contact and the effect of anesthesia restricts the practice of breastfeeding in the first hour of life(18,19). Furthermore, cross-sectional epidemiological studies carried out in Brazil found a significant increase in the percentage rates of cesarean sections, with a possible influence of the pandemic on the indications for cesarean sections at the time of admission to the maternity ward(20,21).
For self-reported skin color, brown women had higher rates of early weaning. The association between prenatal care process indicators and the race/color of women demonstrates that black and mixed-race women are more exposed to access difficulties and inadequate prenatal care(22,23). Regarding guidance on breastfeeding during pregnancy, childbirth, and postpartum, a population-based cross-sectional study shows that black and mixed-race pregnant women had a 33% lower chance of receiving guidance on the subject(24).
The increase in social inequalities in health during the pandemic period is highlighted, especially regarding access to services(25,26). In Brazil, the impact of the pandemic has highlighted existing racial disparities in health. In this context, an integrative review using population databases observed that, in Brazil, being black or brown was a risk factor for the worsening of COVID-19(27).
Notwithstanding, there is a lack of research on mothers’ self-declared skin color as a factor associated with early weaning during the pandemic. Research carried out in the United Kingdom found that black and brown women, when compared to white women, felt a greater negative impact of social isolation measures on breastfeeding. The study also recognized that black and brown women were less likely to feel they had enough support to continue breastfeeding(14).
Despite some research carried out in Israel(28), Chile(29), Europe and South America(30) concluded that breastfeeding rates were not negatively impacted by the COVID-19 pandemic, most studies on the subject concluded that the pandemic had a negative influence on breastfeeding rates(9,14) and those that identified maternal psychological factors as determinants for weaning(12,13).
Regarding the latter approach, research carried out in Thailand concluded that psychological factors were the preponderant influences for weaning during the pandemic(31). Therefore, depression(13,32), fear(33,34), and anxiety(35) were maternal feelings related to early weaning. This approach, however, differs from the scope of the present study and hinders a real discussion of the results.
Regarding socioeconomic aspects, education levels were the factors most related to weaning during the pandemic. Research carried out in the United Kingdom concluded that women with lower levels of education were more likely to stop breastfeeding(14). Likewise, research carried out in 17 European countries concluded that mothers with higher levels of education were less likely to stop breastfeeding(12). These conclusions are also shared by surveys carried out online(36) and in 5 countries, including Brazil(37).
The present study was unable to relate educational levels to breastfeeding interruption. The discrepancy in relation to the results of the aforementioned research is possibly explained by the different socioeconomic reality of the populations studied.
In the literature, the association of income with the length of breastfeeding during the pandemic period is also recurrent. A study carried out in Thailand reported that women who considered their family income sufficient were also more likely to breastfeed exclusively at six months(38). Another study also concluded that low-income women were more likely to stop breastfeeding due to the greater likelihood of being food insecure(36).
However, in the present study, no association was found between income levels and breastfeeding duration. The difference in results may be related, again, to the different socioeconomic reality of the populations studied. Brazil, during the pandemic, instituted a minimum income program for the most vulnerable, the Emergency Aid, as a way to mitigate the economic impacts of the pandemic. These resources probably had a positive impact, mitigating the effects of food insecurity in the population studied(38,39).
Among the limitations of the research, it is recognized that it was carried out using data obtained from maternity hospitals located in Belo Horizonte. Its conclusions, therefore, only reflect a specific reality and should not be extended to other locations, especially when considering the extensive Brazilian sociocultural diversity and the fact that these maternity hospitals are references in relation to the obstetric model of labor and birth. Another limitation is the possible memory bias of the outcome variable in these studies; thus, the findings found here should be interpreted with caution. However, it should be noted that data are consistent with the Brazilian literature, which demonstrates a prevalence of only 61.3% of EBF at 4 months(7). It is worth highlighting that, in the Brazilian scenario, due to the reduced number of tests for COVID-19, only parturient women who were admitted to hospitals with symptoms and signs of COVID-19 underwent confirmatory tests. Therefore, the Brazilian scenario did not adopt universal testing for all parturient women.
The research scenario was only maternity hospitals that serve exclusively SUS and data collection took place through telephone calls. Such facts bring, in themselves, a previous social outline, either because they exclude the higher classes that typically use private health services, or because they exclude from the sample lower class women who may not have access to telephone devices.
CONCLUSION
In this study, the birth route and mothers’ ethnic characteristics were associated with early weaning during the COVID-19 pandemic. Such findings are important to guide the assistance of the multidisciplinary team, especially the nursing team, during the post-pandemic period and in future or recurring critical epidemiological scenarios.
ACKNOWLEDGMENTS
The authors would like to thank the OPESV Research Group (Observatory for Research and Studies in Vaccination at the UFMG School of Nursing) and the participating hospitals: Sofia Feldman, Júlia Kubitschek, Risoleta Tolentino Neves and Unidade Local de Saúde de Matosinhos (Portugal) for their collaboration and support in carrying out this study.
Footnotes
Financial support National Council for Scientific and Technological Development (CNPq) and the Minas Gerais State Research Support Foundation (FAPEMIG) – Call CNPq/MCTI/FNDCT No. 18/2021 – Range A – Emerging Groups (Process: 403481/2021-0) and Call 01/2021 - Universal Demand, respectively.
REFERENCES
- 1.Braga MS, da Silva Gonçalves M, Augusto CR. Os benefícios do aleitamento materno para o desenvolvimento infantil. Braz. J. Develop. 2020;6(9):70250–61. doi: 10.34117/bjdv6n9-468. [DOI] [Google Scholar]
- 2.Ministério da Saúde (BR) Secretaria de Atenção à Saúde. Departamento de Atenção Básica. Saúde da criança: aleitamento materno e alimentação complementar [Internet]. 2. ed. Brasília: Ministério da Saúde; 2015. [[cited 2024 Mar 12]]. Available from: https://bvsms.saude.gov.br/bvs/publicacoes/saude_crianca_aleitamento_materno_cab23.pdf. [Google Scholar]
- 3.Fialho FA, Dias IMAV, Leal DT, do Nascimento L, Neves PM. Almeida MJGG. Diabetes mellitus: a possível relação com o desmame precoce. [[cited 2024 Mar 12]];Rev Enferm UFPE On Line. 2014 8(2):372–8. Available from: https://periodicos.ufpe.br/revistas/revistaenfermagem/article/viewFile/9684/9732. [Google Scholar]
- 4.Victora CG, Horta BL, de Mola CL, Quevedo L, Pinheiro RT, Gigante DP, et al. Association between breastfeeding and intelligence, educational attainment, and income at 30 years of age: a prospective birth cohort study from Brazil. Lancet Glob Health. 2015;3(4):e199–205. doi: 10.1016/S2214-109X(15)70002-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ribeiro JM, Pereira SE. Benefícios a longo prazo na saúde da mulher promovidos pelo aleitamento materno: uma revisão narrativa [monography]. Goiás: Escola de Ciências Sociais e da Saúde, Pontifícia Universidade Católica de Goiás. 2021. [[cited 2024 Mar 12]]. Available from: https://repositorio.pucgoias.edu.br/jspui/handle/123456789/1774.
- 6.Viana RMS, Cassino L. Aleitamento materno: fortalecedor do vínculo afetivo entre mãe e filho. [[cited 2024 Mar 12]];Rev. Bras. Ci. Vida. 2017 5(2):1–25. Available from: http://jornalold.faculdadecienciasdavida.com.br/index.php/RBCV/article/view/222. [Google Scholar]
- 7.Universidade Federal do Rio De Janeiro (UFRJ) Aleitamento materno: prevalência e práticas entre crianças brasileiras menores de 2 anos [Internet] 2021. [[cited 2024 Mar 12]]. Available from: https://enani.nutricao.ufrj.br/download/relatorio-4-aleitamento-materno/#:~:text=A%20preval%C3%AAncia%20de%20aleitamento%20materno%20cruzado%20entre%20menores%20de%20dois,Sul%20(12%2C5%25).
- 8.Silva FMP, Nunes HHM, de Almeida JM, de Menezes LDM, Figueiredo ACB, Cardoso ATS, et al. Aspectos culturais relacionados ao aleitamento materno exclusivo em puérperas atendidas em alojamento conjunto. REAS. 2022;15(2):e9485. doi: 10.25248/reas.e9485.2022. [DOI] [Google Scholar]
- 9.Holand BL, de Oliveira Agostini C, Pacheco MCM, de Leon DMZ, Drehmer M, Bosa VL. Association between breastfeeding and complementary feeding in pre-pandemic and pandemic COVID-19 times: maternar cohort study. J Pediatr (Rio J) 2022;98(5):496–503. doi: 10.1016/j.jped.2021.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Badr H, Alghamdi S. Breastfeeding experience among mothers during the COVID-19 pandemic. Int J Environ Res Public Health. 2022;9(8):4535. doi: 10.3390/ijerph19084535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kwan J, Jia J, Yip KM, So HK, Leung SSF, Ip P, et al. A mixed-methods study on the association of six-month predominant breastfeeding with socioecological factors and COVID-19 among experienced breastfeeding women in Hong Kong. Int Breastfeed J. 2022;17(1):40. doi: 10.1186/s13006-022-00484-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Palmquist AEL, Tomori C, Tumlinson K, Fox C, Chung S, Quinn EA. Pandemic policies and breastfeeding: a cross-sectional study during the onset of COVID-19 in the United States. Front Sociol. 2022;7:958108. doi: 10.3389/fsoc.2022.958108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chertok IA, Artzi-Medvedik R, Arendt M, Sacks E, Otelea MR, Rodrigues C, et al. Factors associated with exclusive breastfeeding at discharge during the COVID-19 pandemic in 17 WHO European Region countries. Int Breastfeed J. 2022;17(1):83. doi: 10.1186/s13006-022-00517-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chang YS, Li KMC, Chien LY, Lee EY, Hong SA, Coca KP. Associations between breastfeeding intention, breastfeeding practices and post-natal depression during the COVID-19 pandemic: a multi-country cross-sectional study. Matern Child Nutr. 2023;19(1):e13450. doi: 10.1111/mcn.13450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brown A, Shenker N. Experiences of breastfeeding during COVID-19: lessons for future practical and emotional support. Matern Child Nutr. 2021;17(1):e13088. doi: 10.1111/mcn.13088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lubbe W, Niela-Vilén H, Thomson G, Botha E. Impact of the COVID-19 pandemic on breastfeeding support services and women’s experiences of breastfeeding: a review. Int J Womens Health. 2022;14:1447–57. doi: 10.2147/IJWH.S342754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Perlman J, Oxford C, Chang C, Salvatore C, Di Pace J. Delivery room preparedness and early neonatal outcomes during COVID-19 pandemic in New York City. Pediatrics. 2020;146(2):e20201567. doi: 10.1542/peds.2020-1567. [DOI] [PubMed] [Google Scholar]
- 18.Medeiros ACLL, da Silva GSV, Gomes NF, Silva JSLG, Souza AS, da Silva EA. A influência do tipo de parto no desmame precoce. Revista Pró-UniverSUS. 2021;12(2):72–8. doi: 10.21727/rpu.v12i2.2655. [DOI] [Google Scholar]
- 19.Ferrari AP, Almeida MAM, Carvalhaes MABL, Parada CMGL. Effects of elective cesarean sections on perinatal outcomes and care practices. Rev Bras Saúde Mater Infant. 2020;20(3):879–88. doi: 10.1590/1806-93042020000300012. [DOI] [Google Scholar]
- 20.Oliveira ICDP, Geraldo LMCS, Faria APV, Silva TPRD, Amorim T, Pereira PF, et al. Repercussões da infecção por SARS-CoV-2 e da pandemia nas vias de nascimento: estudo transversal. Rev Gaúcha Enferm. 2023;44:e20220320. doi: 10.1590/1983-1447.2023.20220320.en. [DOI] [PubMed] [Google Scholar]
- 21.da Silva CEB, Guida JPS, Costa ML. Increased cesarean section rates during the COVID-19 pandemic: looking for reasons through the robson ten group classification system. Rev Bras Ginecol Obstet. 2023;45(7):371–6. doi: 10.1055/s-0043-1772182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lessa MSDA, Nascimento ER, Coelho EDAC, Soares IDJ, Rodrigues QP, Santos CADST, et al. Pré-natal da mulher brasileira: desigualdades raciais e suas implicações para o cuidado. Cien Saude Colet. 2022;27(10):3881–90. doi: 10.1590/1413-812320222710.01282022en. [DOI] [PubMed] [Google Scholar]
- 23.Flores TR, Neves RG, Mielke GI, Bertoldi AD, Nunes BP. Desigualdades na cobertura da assistência pré-natal no Brasil: um estudo de abrangência nacional. Cien Saude Colet. 2021;26(2):593–600. doi: 10.1590/1413-81232021262.26792019. [DOI] [PubMed] [Google Scholar]
- 24.Lessa MSDA, Nascimento ER, Coelho EDAC, Soares IDJ, Rodrigues QP, Santos CADST, et al. Pré-natal da mulher brasileira: desigualdades raciais e suas implicações para o cuidado. Cien Saude Colet. 2022;27(10):3881–90. doi: 10.1590/1413-812320222710.01282022en. [DOI] [PubMed] [Google Scholar]
- 25.Dantas-Silva A, Santiago SM, Surita FG. Racism as a social determinant of health in Brazil in the COVID-19 pandemic and beyond. Rev Bras Ginecol Obstet. 2023;45(5):221–4. doi: 10.1055/s-0043-1770135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Barron GC, Laryea-Adjei G, Vike-Freiberga V, Abubakar I, Dakkak H, Devakumar D, et al. Lancet Commission on COVID-19: task force on humanitarian relief, social protection and vulnerable groups. Safeguarding people living in vulnerable conditions in the COVID-19 era through universal health coverage and social protection. Lancet Public Health. 2022;7(1):e86–92. doi: 10.1016/S2468-2667(21)00235-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cavalcante GS, Santos MC, Andrade MM, Melo RB, Oliveira TS, Santos GG. Revisão Integrativa da Literatura sobre disparidades étnico-raciais da COVID-19 entre gestantes e puérperas negras. Pubsaúde. 2021;8:a248. doi: 10.31533/pubsaude8.a248. [DOI] [Google Scholar]
- 28.Magnazi MB, Sartena G, Goldberg M, Zimmerman D, Ophir E, Baruch R, et al. Impact of the COVID-19 pandemic on breastfeeding in Israel: a cross- sectional, observational survey. Int Breastfeed J. 2022;17(1):61. doi: 10.1186/s13006-022-00505-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Navarro-Rosenblatt D, Benmarhnia T, Bedregal P, Lopez-Arana S, Rodriguez-Osiac L, Garmendia ML. Socio-economic inequalities in the effect of public policies and the COVID-19 pandemic on exclusive breastfeeding in Chile. Public Health. 2023;214:61–8. doi: 10.1016/j.puhe.2022.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ganho-Ávila A, Guiomar R, Sobral M, Pacheco F, Caparros-Gonzalez RA, Diaz-Louzao C, et al. The impact of COVID-19 on breastfeeding rates: an international cross-sectional study. Midwifery. 2023;120:103631. doi: 10.1016/j.midw.2023.103631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nuampa S, Patil CL, Prasong S, Kuesakul K, Sudphet M. Exploring the association between socioeconomic and psychological factors and breastfeeding in the first year of life during the COVID-19 pandemic in Thailand. Int J Environ Res Public Health. 2022;20(1):130. doi: 10.3390/ijerph20010130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ahmad Zadeh Beheshti M, Alimoradi Z, Bahrami N, Allen KA, Lissack K. Predictors of breastfeeding self-efficacy during the Covid-19 pandemic. J Neonatal Nurs. 2022;28(5):349–55. doi: 10.1016/j.jnn.2021.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Reagu SM, Abuyaqoub S, Babarinsa I, Kader NA, Farrell T, Lindow S, et al. Impact of the fear of Covid-19 infection on intent to breastfeed; a cross sectional survey of a perinatal population in Qatar. BMC Pregnancy Childbirth. 2022;22(1):104. doi: 10.1186/s12884-022-04446-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Samaria D, Marcelina LA, Florensia L. The COVID-19 pandemic’s impact on breastfeeding self-efficacy: a path analysis. Enferm Clin. 2023;33:S17–21. doi: 10.1016/j.enfcli.2023.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ergün S, Kaynak S, Aydın B. Fear of COVID-19 and related factors affecting mothers’ breastfeeding self-efficacy during the pandemic. Rev Esc Enferm USP. 2022;56:e20220130. doi: 10.1590/1980-220x-reeusp-2022-0130en. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chien LY, Lee EY, Coca KP, Paek SC, Hong SA, Chang YS. Impact of COVID-19 on breastfeeding intention and behaviour among postpartum women in five countries. Women Birth. 2022;35(6):e523–9. doi: 10.1016/j.wombi.2022.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nuampa S, Ratinthorn A, Patil CL, Kuesakul K, Prasong S, Sudphet M. Impact of personal and environmental factors affecting exclusive breastfeeding practices in the first six months during the COVID-19 pandemic in Thailand: a mixed-methods approach. Int Breastfeed J. 2022;17(1):73. doi: 10.1186/s13006-022-00515-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Freire D, Domingue E, Magalhães A, Simonato T, Cardoso G. “Auxílio Emergencial – Uma política fiscal contracíclica?”: Impactos do auxílio emergencial na economia brasileira em 2020 [Internet] 2021. [[cited 2024 Mar 12]]. Available from: https://pesquisas.face.ufmg.br/nemea/wp-content/uploads/sites/20/2021/09/Auxilio_Emergencial.pdf.
- 39.Ramos CL. O impacto do auxílio emergencial sobre a pobreza e a desigualdade durante a pandemia do coronavírus [dissertation] Rio de Janeiro: Escola Brasileira de Economia e Finanças, Fundação Getúlio Vargas; 2021. Available from: https://repositorio.fgv.br/server/api/core/bitstreams/2e4d80e3-986f-4315-8128-246eb08b3d61/content. [Google Scholar]