Abstract
Objectives:
The objective of the study was to investigate the clinical value of pelvic diameter in the evaluation of surgical difficulty and selection of the best surgical plan for exogenous cervical leiomyomas.
Materials and Methods:
Sixty-five patients with exogenous cervical leiomyomas admitted to our hospital from 2012 to 2021 were enrolled. All patients underwent pelvic magnetic resonance imaging examination before surgery and received surgical treatment within 1 week. Relevant clinical data were collected. According to the surgical approach, they were divided into two groups: the laparoscopic group and the laparotomy group. The clinical significance of the pelvic diameter line in the surgical selection of exogenous cervical leiomyomas was discussed by retrospective analysis of the correlation between the pelvic diameter line and the collected clinical indicators.
Results:
There was no significant difference in tumor location and pelvic diameter between the two groups (P > 0.05). However, there was a significant difference in tumor diameter and the ratio of tumor diameter line to pelvic diameter line (P < 0.05). In addition, the laparoscopic group underwent more myomectomy than hysterectomy and lost more blood during operation (P < 0.05). The postoperative index showed that patients in the laparotomy group had a higher proportion of full of cellular leiomyoma, higher postoperative temperature, and longer postoperative exhaust time (P < 0.05).
Conclusion:
The ratio of the tumor diameter line to the pelvic diameter line is correlated with the surgical plan selection of exogenous cervical leiomyomas, which may be used to evaluate the surgical difficulty of these patients and the selection of the suitable surgical plan.
Keywords: Cervical leiomyomas, magnetic resonance imaging, operative plan, pelvic diameter
INTRODUCTION
Uterine leiomyomas are one of the most common benign tumors in the female reproductive system. The vast majority of uterine leiomyomas occur in the uterine body, whereas the incidence of cervical leiomyomas is 0.6%.[1] Cervical leiomyomas are located below the level of the internal opening of the cervix. Due to its anatomical location in the deep pelvic cavity and its proximity to the pelvic organs, such as the bladder, the ureter, and the intestine, the operation space is small/limited, and the blood supply of surrounding tissues is abundant, which brings great difficulty to the operation.[2,3] Laparoscopic surgery is widely performed because of clear vision, small trauma, quick recovery, and minimal scars, and the risk of intraoperative hemorrhage and is influenced by the size and number of leiomyomas and the time of operation during laparoscopic surgery.[4] The advantages of traditional open surgery are more pronounced when the pelvic pelvis is deep and narrow, the mass is large, large quantity, long operation time, the operating space is obscured, and the intraoperative wound bleeding rate is fast.[4,5,6] Improper surgical procedures may increase the risk of obstetrical complications, such as uterine rupture during laparoscopic myomectomy.[7] Therefore, it is difficult for surgeons to reasonably and effectively adapt the surgical method. The mass data provided by the preoperative image data and the determination of the nature of the mass provide surgeons with very useful reference data, and if combined with the pelvic diameter line to determine the width and depth of the patient’s pelvis, it will be more helpful to assess the difficulty of surgery and select surgical options.
Deep pelvic diameter measurements are based on X-rays, ultrasound, computed tomography, and magnetic resonance imaging (MRI). In particular, MRI images are clear, without ionizing radiation during measurement, and various related diameter data can be obtained from multiple sequences, multilevels, and angles, and because of its high soft-tissue resolution, it can not only realize the pelvic osseous structure measurement but also clear imaging of pelvic soft tissue, which is helpful in judging the accurate anatomical relationship between cervical fibroids and soft tissues.[6,8] At present, many doctors have carried out the use of relevant pelvic diameter lines to assess the width and narrowness of the pelvis and predict the difficulty of surgery in low-level rectal cancer, pelvic organ prolapse, etc.[7,8,9,10] These clinically significant diameters, including the anterior diameter of the pelvic inlet, the anterior diameter of the middle pelvis, the anterior and posterior diameter of the pelvic outlet, the interstitial diameter of the sciatic spines, and the interstitial diameter of the sciatic nodule, the sacrococcygeal diameter, and the sacrococcygeal curvature, not only evaluate the width, narrowness, and depth of the pelvis from a three-dimensional (3D) perspective but also understand the sacrococcygeal curvature through the index of the degree of sacral coccyx curvature, which provides a basis for objectively judging the choice of surgical method.[9,11] Pelvic MRI uses zero spacing, small field of view and thin layer scanning to improve tissue resolution, can more clearly display pelvic floor anatomy, diffusion-weighted imaging, dynamic MRI, 3D-MRI, and other new imaging techniques, greatly enriching the imaging doctor’s examination methods. The larger cervical fibroids (diameter >5 cm) are relatively fixed in position, closely related to the pelvic floor tissue, and the degree of motion is small relative to the fibroids of the uterine body, and it is not easy to change the anatomical relationship through external means, so the use of preoperative pelvic MRI to assess the difficulty of surgery and choose the surgical method is expected to be a more appropriate choice.[10,12]
MATERIALS AND METHODS
This study was approved by Fujian Maternity and Child Health Hospital Committee (approval no. 2023J001) and followed the Helsinki Declaration. The informed patients consent were waived by committee due to the retrospective nature.
A total of 68 patients with a preoperative diagnosis of cervical exophytic fibroids were collected from Fujian Provincial Maternal and Child Health Hospital from 2012 to 2021, all patients underwent pelvic MRI examination before operation. They were divided into laparoscopic group and a laparotomy group according to the operation methods. The clinical data were collected, and the pelvic diameters were measured in the workstation of the radiology department for retrospective analysis, to compare the differences of the measurement indexes between the laparoscopic group and the laparotomy group, and to analyze the correlation between the pelvic diameter and the indexes of the laparoscopic group and the laparotomy group, to explore the clinical significance of pelvic diameter in evaluating the selection of surgical approach for exophytic cervical fibroids.
Inclusion criteria
(1) Age 20–60 years old; (2) the anatomical location of the mass is located below the level of the internal orifice of the cervix and is exogenous; (3) the diameter of the cervical mass is ≥5 cm; and (4) the surgeons are all physicians with rich surgical experience at the level of deputy chief physician or above.
Exclusion criteria
(1) Patients with a mass diameter of <5 cm; (2) height <145 cm or >175 cm; (3) body weight <40 kg or >80 kg; (4) patients with cervical submucosal fibroids; (5) patients with postoperative pathology confirmed as malignant tumors; and (6) patients with contraindications for magnetic resonance examination.
1.5T GE Signa HDE MRI equipment is used. Before the examination, the patient is instructed to empty the intestine and hold the urine appropriately, the coil was placed in the patient’s lower abdomen and fixed, and the patient was instructed to breathe chest as much as possible to reduce respiratory motion artifacts. All patients underwent conventional MRI scanning. The sequence parameters are shown in Table 1.
Table 1.
Scan sequences parameters of conventional magnetic resonance imaging
| Scan orientation and sequence | TR (ms) | TE (ms) | FOV (cm) | Layer thickness (cm) | Layer spacing (cm) | Matrix | Number of acquisitions |
|---|---|---|---|---|---|---|---|
| Cross-axis FSE/T1WI | 450 | 15 | 40×32 | 6 | 1 | 320×256 | 4 |
| FSE/T2WI fat inhibition on the transverse, sagittal and coronal plane | 2800~4200 | 68~82 | 40×28~40 | 6 | 1 | 320×256 | 2~4 |
| Cross-axis DWI (B=700 s/mm²) | 4800~5200 | 76 | 32×32 | 6 | 1 | 128×28 | 6~8 |
| M3D/LAVA | 3.5 | 1.6 | 38×38 | 3~5 | 320×192 | 1 |
FOV: Field of view, DWI: Diffusion-weighted imaging, LAVA: Liver acceleration volume acquisition, FSE: Fast Spin Echo, TR: Time of repetition, TE: Time of echo
Pelvic MRI scans are imported into a workstation, and two senior diagnostic imaging physicians independently analyze the images without knowing the pathological results and surgical methods to obtain raw data and average them.
The diameter lines measured were the maximum transverse diameter of the tumor [Figure 1a], the maximum anteroposterior diameter of the tumor [Figure 1b], the ischial interspinous diameter [Figure 1c], the ischial tuberosity diameter [Figure 1d], and anteroposterior diameter of pelvic inlet [Figure 1e] The length of each path line of the pelvis was measured twice and averaged, as shown in Table 2.
Figure 1.
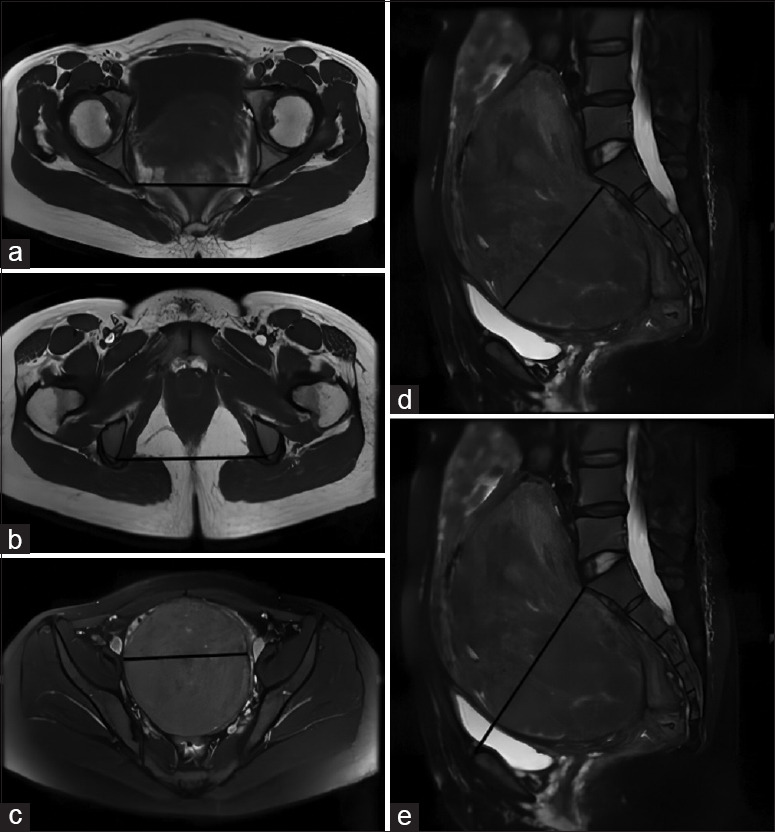
The pelvic diameter lines were measured by MRI,as shown in (a) Ischial spine spacing,(b) Ischial nodule spacing, (c) Maximum transverse diameter of tumor, (d) Maximum anteroposterior diameter of tumor, (e) Anteroposterior diameter of pelvic inlet
Table 2.
Specific definitions of measurement parameters
| Parameter | Description |
|---|---|
| Maximum transverse diameter of the tumor | The maximum diameter line in the left and right directions of the tumor |
| Maximum anteroposterior diameter of the tumor | The maximum diameter of the anterior and posterior direction of the tumor |
| Ischia spine spacing | The straight-line distance between the bilateral the sciatic spine |
| Ischial tuberosity spacing | The straight-line distance between the bilateral ischial tuberosity |
| Anterioposterior diameter of pelvic inlet | The straight-line distance from the middle superior margin of the symphysis pubis to the middle anterior margin of the sacral promontory |
All the measured data were collated and input into the database, and the SPSS 24.0 statistical software (SPSS Inc., Chicago, USA) was used for statistical analysis. The parameters of general condition, intraoperative and postoperative condition, tumor diameter, and the difference between tumor diameter and pelvic diameter were compared between laparoscopic group and laparotomy group. The data of normal distribution were expressed by mean ± standard deviation, and the results were analyzed by one-way ANOVA. The analysis of the counting data was Chi-squared. P <0.05 is statistically significant.
RESULTS
General data of patients in the laparoscopy and laparotomy [Table 3], the results suggest that there was no statistical difference between the two groups (P > 0.05).
Table 3.
General data of patients in the laparoscopic and open groups
| Item | Open abdominal group (n=27) | Laparoscopic group (n=38) | P |
|---|---|---|---|
| Age (years) | 41.22±8.95 | 40.58±7.88 | 0.760 |
| Height (cm) | 160.41±4.28 | 159.11±5.17 | 0.287 |
| Weight (kg) | 60.44±7.99 | 56.99±7.67 | 0.084 |
| BMI | 23.51±3.14 | 22.52±2.99 | 0.203 |
| Number of pregnancies (times) | |||
| 0 | 4 | 1 | 0.186 |
| 1 | 5 | 7 | |
| ≥2 | 18 | 30 | |
| Number of deliveries (times) | |||
| 0 | 5 | 4 | 0.615 |
| 1 | 14 | 20 | |
| ≥2 | 8 | ||
| Complaints | |||
| Mass | 19 | 21 | 0.404 |
| Hemorrhage | 7 | 16 | |
| Abdominal discomfort | 1 | 1 | |
| Previous surgical history | |||
| No | 14 | 22 | 0.629 |
| Yes | 13 | 16 |
BMI: Body mass index
Comparing the MRI data between laparoscopic group and the laparotomy group [Table 4], the results showed that there was no statistical difference in the tumor location between the two groups (P > 0.05), and there was no statistical difference in the length of each pelvic diameter (P > 0.05), but the tumor diameter and the ratio of tumor diameter to pelvic diameter were significantly different (P < 0.05).
Table 4.
Comparison of magnetic resonance imaging data between laparoscopic group and laparotomy group
| Item | Open abdominal group (n=27) | Laparoscopic group (n=38) | P |
|---|---|---|---|
| Fibroids location | |||
| Anterior wall | 8 | 4 | 0.147 |
| Side wall | 7 | 13 | |
| Back wall | 12 | 21 | |
| Maximum transverse diameter of the fibroid (mm) | 10.01±3.09 | 6.96±1.64 | 0.000** |
| Ischial spine space (mm) | 11.20±0.67 | 11.17±0.77 | 0.872 |
| The ratio of the maximum left and right diameter of fibroids to ischial spine space | 0.90±0.28 | 0.62±0.15 | 0.000** |
| Ischial tuberosity spacing (mm) | 12.62±0.76 | 12.25±1.14 | 0.145 |
| The ratio of the maximum left and right diameter of fibroids to ischial tuberosity spacing | 0.80±0.26 | 0.57±0.14 | 0.000** |
| Maximum anteroposterior diameter of fibroids (mm) | 7.95±1.90 | 6.35±1.72 | 0.001** |
| Anteroposterior diameter of pelvic inlet (mm) | 12.43±1.01 | 123.72±0.99 | 0.247 |
| The ratio of the maximum anteroposterior diameter of fibroids to the anteroposterior diameter of pelvic inlet | 0.64±0.16 | 0.50±0.14 | 0.000** |
**P<0.01
The comparison of surgical indicators between laparoscopic group and the laparotomy group [Table 5] showed that there were significant differences in the surgical method, intraoperative blood loss, and intraoperative blood transfusion cases between the two groups (P < 0.05). The laparoscopic group underwent more myomectomy than total hysterectomy; the amount of intraoperative blood loss and the number of intraoperative blood transfusions in the laparotomy group were more than those in the laparoscopy group, but there was no significant difference in intraoperative adhesion and pre and postoperative human chorionic gonadotropin hemoglobin (HGB) values (P > 0.05).
Table 5.
Comparison of surgical indexes between laparoscopic group and laparotomy group
| Item | Open group (n=27) | Laparoscopic group (n=38) | P |
|---|---|---|---|
| Surgical approach | |||
| Uterine tumor enucleation | 12 | 27 | 0.041* |
| Hysterectomy | 15 | 11 | |
| Intraoperative adhesions | |||
| No | 13 | 20 | 0.804 |
| Yes | 14 | 18 | |
| Operation time | 143.35±50.14 | 161.4±77.02 | 0.427 |
| Intraoperative bleeding | 421.93±693.36 | 125.53±234.18 | 0.017* |
| Preoperative HGB | 119.77±20.64 | 118.89±19.75 | 0.745 |
| Postoperative HGB | 98.27±19.08 | 103.57±15.81 | 0.093 |
| Change of HGB before and after surgery | 21.50±12.57 | 15.22±13.09 | 0.246 |
| Intraoperative blood transfusion | 5 | 1 | 0.029* |
HGB: Hemoglobin. *P<0.05
The comparison of postoperative indicators between the laparoscopic group and the laparotomy group [Table 6] showed that the highest postoperative body temperature in the laparoscopic group was significantly lowerthan that in the laparotomy group (P < 0.05). The proportion of cellular leiomyomas in the laparotomy group was higher (P < 0.05). However, there was nosignifcant difference in postoperative anti-infammatory time and postoperative hospital stay (P > 0.05).
Table 6.
Comparison of postoperative indexes between laparoscopic group and laparotomy group
| Item | Open abdominal group (n=27) | Laparoscopic group (n=38) | P |
|---|---|---|---|
| Postoperative pathology | |||
| Uterine fibroids | 12 | 26 | 0.045* |
| Uterine fibroids degeneration | 5 | 1 | |
| Rich in cells | 10 | 11 | |
| Surgery | |||
| Median postoperative hospital stay | 6.56±3.29 | 5.45±2.11 | 0.103 |
| Anal exhaust time | 33.61±11.43 | 27.6±9.47 | 0.013* |
| Indwelling catheter time | 46.24±27.99 | 37.84±17.41 | 0.141 |
| Maximum postoperative temperature | |||
| <37.3 | 9 | 26 | 0.019* |
| 37.4–38 | 16 | 11 | |
| 38.1–39 | 2 | 1 | |
| Postoperative pain time | |||
| 0 | 0 | 4 | 0.071 |
| 1 | 0 | 4 | |
| 2 | 10 | 14 | |
| ≥3 | 17 | 1216 | |
| Postoperative anti-inflammatory time | |||
| 0 | 1 | 2 | 0.844 |
| 1 | 0 | 1 | |
| 2 | 12 | 16 | |
| ≥3 | 14 | 19 | |
| Postoperative complications | |||
| No | 23 | 37 | 0.069 |
| Yes | 4 | 1 |
*P<0.05
DISCUSSION
The most common treatment for cervical leiomyomas is surgery; myomectomy[11,12,13,14] or hysterectomy may be performed depending on the patient’s specific needs.[13,15] The surgical methods often include traditional laparotomy, vaginal surgery, laparoscopic porous, laparoscopic uterine artery occlusion in combination with myomectomy,[16] or even single-port robotic surgery.[2] The selection is often based on the rich clinical experience of the operator, with great subjective factors. Martinez et al., in their study, reported that myomectomy is related to the type of leiomyoma but not to the location and size of leiomyoma. Intermural and subserous leiomyomas are more suitable for laparoscopic surgery.[17]
Due to the special location of cervical leiomyoma, the risk of intraoperative bleeding and potential damage to adjacent organs may cause serious complications. At the same time, uterine myoma has the convenience of changing the anatomical relationship and winning the surgical space by pulling or lifting the uterine body. In contrast, cervical leiomyomas, especially exogenous leiomyomas, have relatively fixed mobility and are greatly restricted by the patient’s pelvic anatomy. It is difficult to find objective criteria to evaluate surgical approaches.
Vaginal surgery is an operation for cervical leiomyoma, but it has a poor visual field for exploration and treatment of abdominal lesions[14,15,18,19] and is easily hindered by the size of the uterus,[16,20] especially when there is severe pelvic adhesion. The study shows that most of the women in Fujian are a narrow pelvic type,[17,21] so the cases included in this study were not treated by vaginal surgery after comprehensive evaluation by the operators. The advantage of traditional laparotomy lies in the 3D visual field, especially when there are severe intraoperative adhesions during the operation, the blunt separation of some tissue levels can be completed by the fine movements of the hand. When the acute bleeding is more ferocious, the finger squeezes and compresses the bleeding site so that the surgeon can reduce the amount of bleeding when exploring the bleeding point. Especially in the case of large cervical leiomyomas, which often have a rich blood supply, and preoperative imaging examination cannot rule out the possibility of sarcoma, laparotomy can remove the tumor completely and avoid the possibility of tumor dissemination and implantation. Laparoscopic surgery has the characteristics of a beautiful incision and quick postoperative recovery. At the same time, due to the adjustment of the focal length and angle of the laparoscope, the parts and more subtle structures that cannot be seen under open vision can be observed. In particular, the coagulation and cutting can be combined to reduce intraoperative blood loss while using laparoscopic instruments.
In this study, there were no significant differences in age, height, weight, body mass index, maternal history, previous surgical history, and symptoms between the laparotomy group and the laparoscopic group, indicating that these factors are not the main factors affecting the choice of surgical approach.
The diameter of the pelvic anatomy is of great value in judging the mode of obstetrical delivery, especially when the cervix is dilated and the fetal presentation decreases.[18,22] However, the labor process is a dynamic process, and the location of exogenous cervical myoma is relatively fixed. Preoperative analysis of imaging data to evaluate the correlation between tumor and pelvic diameter can provide a relatively objective index for clinicians. In particular, certain diameters of the pelvic entrance plane and the middle pelvic plane have a significant impact on the difficulty of surgery, because traditional laparoscopic instruments cannot change the curvature and angle at will. Therefore, the space limitation significantly affects the decision for surgical approach. The shape of a woman’s pelvis is related to ethnicity, growth and development, nutrition, and hormones. And its classification is based on pelvic diameter. In theory, it can be divided into female type, anthropoid type, male type, and flat type, but most pelvises are actually mixed. Therefore, it is more convincing to choose the pelvic diameter as the surgical approach for cervical leiomyoma. From the data in this paper, the location of the exogenous tumor is not a factor considered by the operative method, but the size of the tumor has a significant difference in the selection of the surgical approach, especially the ratio of the diameter of the tumor to the corresponding pelvic bone is of great significance in determining the surgical approach.
In terms of surgical methods, the two groups of patients were more inclined to laparoscopic surgery in the choice of uterine myomectomy. First, the patients who underwent myomectomy were younger and required to preserve the uterus; second, the size of the tumor was smaller than that of the laparotomy group, indicating that the diameter of the excessively large tumor must limits the operation space of laparoscopic instruments, Therefore, the diameter of the tumor is the main basis for preoperative evaluation for the choice of operation.
There was no significant difference between pre and postoperative HGB values or changes. On the one hand, the patients with bleeding caused by exogenous cervical leiomyoma vary greatly because of the different course of disease, which cannot be compared purely by numerical values. On the other hand, the blood routine measurement time after operation is longer than the second day after operation. At this time, most patients have eaten or drank water, and the postoperative HGB value may be greatly affected by the dilution of fluid intake by patients with different height and weight. Simple numerical values do not reflect specific changes. The changes in HGB value before and after surgery should be significantly correlated with the amount of intraoperative blood loss, but the data in this study may not really reflect the significant differences between different groups after emergency blood transfusion during surgery. Second, we cannot rule out the limitation of the results caused by the small sample size, and we still need to collect and increase the sample size to continue to observe. Third, the side also reflects that choosing the correct operation according to the size of the mass is the real minimally invasive goal. Adequate preoperative evaluation and intraoperative hemostatic planning are helpful to reduce bleeding and avoid changes in HGB.
According to the postoperative pathological results, the majority of patients in the laparoscopic group had simple uterine leiomyomas, indicating that when the preoperative imaging examination showed that the uterine tumor was significantly enlarged and the blood supply was abundant, which cannot be determined the nature of myoma degeneration, cellular leiomyoma, or sarcoma, the surgeon will choose to open a complete myomectomy or hysterectomy as much as possible. The rich blood supply of the tumor often leads to more bleeding during laparotomy than in laparoscopy, which also explains the significant difference in the number of blood transfusion patients between different groups, which also reflects the risks of surgery from the side.
There was no significant difference in the median hospital stay, indwelling catheter time, and postoperative complication rates, indicating that the appropriate choice of operation is conducive to the recovery of patients. In terms of anal exhaust time, the laparoscopic group was significantly lower than the laparotomy group, indicating that laparoscopic surgery was performed in a confined space, avoiding the exposure of tissues and organs and the stimulation of glove gauze, with little interference to the abdominal cavity, and rapid postoperative recovery of intestinal motility. The power recovery is fast, which is consistent with the previous literature reports.[19,23] The highest postoperative body temperature in the laparoscopic group was significantly lower than that in the laparotomy group. It indicated that the degree of injury and stress of laparoscopic surgery were lower, which is consistent with the reports of other researchers.[20,24] However, there was no signifcant difference in postoperative anti-infammatory time. Therefore, the antibiotics used to control the infection during the perioperative period are basically the same, and the efficacy is also the same, without the difference between laparotomy and laparoscopy. The postoperative pain time is due to the intervention of the anesthesiology department, and the postoperative analgesia effect is better, so there is no significant difference, but from the careful analysis of the data, it can be seen that the degree of pain is better in the laparoscopic group, especially within 24 h after surgery.
CONCLUSION
Therefore, according to the ratio of tumor diameter and pelvic diameter obtained by preoperative imaging examination, the difficulty of surgery can be evaluated, and the best surgical plan can be selected based on this to achieve the best treatment effect. However, how to define the optimal range of the ratio for different surgical options still needs more research and analysis with more large sample data. In addition, the patient’s age and needs should be fully considered, the tumor nature and tumor blood supply should be also accurately estimated before surgery, and the advantages and disadvantages of different surgical approaches should be skillfully mastered, until individualized and precise treatment is carried out.
Author contributions
Conceptualization, Liangzhi Cai ;Methodology, Liangzhi Cai and Kaiwu Lin; Data Collection,Lifang Xue,Kaiwu Lin; Validation, Mu Xu, Xiaoyan Xie and Kaiwu Lin; Formal Analysis, Lifang Xue; Data Curation, Lifang Xue,Liying Wang,Kaiwu Lin and Xiaoyan Xie; Writing-Original Draft Preparation, Lifang Xue, Liying Wang and Liangzhi Cai; Writing-Review & Editing, Liying Wang,Kaiwu Lin and Liangzhi Cai;Supervision, Liangzhi Cai;Project Administration, Liangzhi Cai and Kaiwu Lin;All authors have read and agreed to the final version of the manuscript.
Data availability statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Tiltman AJ. Leiomyomas of the uterine cervix: A study of frequency. Int J Gynecol Pathol. 1998;17:231–4. doi: 10.1097/00004347-199807000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Ferrari F, Forte S, Valenti G, Ardighieri L, Barra F, Esposito V, et al. Current treatment options for cervical leiomyomas: A systematic review of literature. Medicina (Kaunas) 2021;57:92. doi: 10.3390/medicina57020092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chang WC, Chen SY, Huang SC, Chang DY, Chou LY, Sheu BC. Strategy of cervical myomectomy under laparoscopy. Fertil Steril. 2010;94:2710–5. doi: 10.1016/j.fertnstert.2010.02.049. [DOI] [PubMed] [Google Scholar]
- 4.Sleiman Z, Baba RE, Garzon S, Khazaka A. The significant risk factors of intra-operative hemorrhage during laparoscopic myomectomy: A systematic review. Gynecol Minim Invasive Ther. 2020;9:6–12. doi: 10.4103/GMIT.GMIT_21_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tanos V, Berry KE, Frist M, Campo R, DeWilde RL. Prevention and management of complications in laparoscopic myomectomy. Biomed Res Int 2018. 2018 doi: 10.1155/2018/8250952. 8250952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.D’Silva EC, Muda AM, Safiee AI, Ghazali WA. Five-year lapsed: Review of laparoscopic myomectomy versus open myomectomy in Putrajaya hospital. Gynecol Minim Invasive Ther. 2018;7:161–6. doi: 10.4103/GMIT.GMIT_38_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wada S, Fukushi Y, Ono Y, Ota H, Tsuzuki Y, Yamada H. Influence of uterine cavity breach in laparoscopic myomectomy on the risk of obstetric complications. Gynecol Minim Invasive Ther. 2022;11:221–3. doi: 10.4103/gmit.gmit_146_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Deshmukh SP, Gonsalves CF, Guglielmo FF, Mitchell DG. Role of MR imaging of uterine leiomyomas before and after embolization. Radiographics. 2012;32:E251–81. doi: 10.1148/rg.326125517. [DOI] [PubMed] [Google Scholar]
- 9.Chau J, Solomon J, Liberman AS, Charlebois P, Stein B, Lee L. Pelvic dimensions on preoperative imaging can identify poor-quality resections after laparoscopic low anterior resection for mid- and low rectal cancer. Surg Endosc. 2020;34:4609–15. doi: 10.1007/s00464-019-07209-8. [DOI] [PubMed] [Google Scholar]
- 10.Sammarco AG, Sheyn DD, Krantz TE, Olivera CK, Rodrigues AA, Kobernik ME, et al. Anovel measurement of pelvic floor cross-sectional area in older and younger women with and without prolapse. Am J Obstet Gynecol. 2019;221:521.e1–7. doi: 10.1016/j.ajog.2019.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Atasoy G, Arslan NC, Elibol FD, Sagol O, Obuz F, Sokmen S. Magnetic resonance-based pelvimetry and tumor volumetry can predict surgical difficulty and oncologic outcome in locally advanced mid-low rectal cancer. Surg Today. 2018;48:1040–51. doi: 10.1007/s00595-018-1690-3. [DOI] [PubMed] [Google Scholar]
- 12.Ishidera Y, Furugori M, Hirata G, Wakabayashi R, Shigeta H, Yoshida H. Total laparoscopic hysterectomy for anterior cervical myoma: Possible significance of presurgical assessment by magnetic resonance imaging. Gynecol Minim Invasive Ther. 2021;10:61–4. doi: 10.4103/GMIT.GMIT_104_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Laganà AS, Vitale SG, Muscia V, Rossetti P, Buscema M, Triolo O, et al. Endometrial preparation with dienogest before hysteroscopic surgery: A systematic review. Arch Gynecol Obstet. 2017;295:661–7. doi: 10.1007/s00404-016-4244-1. [DOI] [PubMed] [Google Scholar]
- 14.Laganà AS, Giacobbe V, Triolo O, Granese R, Ban Frangež H, Vrtačnik-Bokal E, et al. Dienogest as preoperative treatment of submucous myomas for hysteroscopic surgery: A prospective, randomized study. Gynecol Endocrinol. 2016;32:408–11. doi: 10.3109/09513590.2015.1128409. [DOI] [PubMed] [Google Scholar]
- 15.Ko JS, Suh CH, Huang H, Zhuo H, Harmanli O, Zhang Y. Association of race/ethnicity with surgical route and perioperative outcomes of hysterectomy for leiomyomas. J Minim Invasive Gynecol. 2021;28:1403–10.e2. doi: 10.1016/j.jmig.2020.11.008. [DOI] [PubMed] [Google Scholar]
- 16.Ai G, Huang W, Yang W, Liu J, Luo N, Guo J, et al. Avideo article: The laparoscopic uterine artery occlusion in combination with myomectomy for uterine myoma. Gynecol Minim Invasive Ther. 2022;11:114–5. doi: 10.4103/GMIT.GMIT_10_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Martinez ME, Domingo MV. Size, type, and location of myoma as predictors for successful laparoscopic myomectomy: A tertiary government hospital experience. Gynecol Minim Invasive Ther. 2018;7:61–5. doi: 10.4103/GMIT.GMIT_12_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhou CX, Zheng W. New progress in micro-noninvasive treatment of uterine fibroids. Mod Pract Med. 2018;30:841–4. [Google Scholar]
- 19.Li S. The effect of hysterectomy by different ways on the prognosis and pelvic floor function of patients with hysteromyoma. Womens Health Res. 2019;15:9–10. [Google Scholar]
- 20.Mohan Y, Chiu VY, Lonky NM. Size matters in planning hysterectomy approach. Womens Health (Lond) 2016;12:400–3. doi: 10.1177/1745505716653692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yu KL, Zheng LB, Hu Y, Wang Y, Xue H, Cheng Z, et al. Physical characteristics of the Han ethnic groups of Mindong dialect in Fujian. Acta Anat Sin. 2013;44:824–34. [Google Scholar]
- 22.Pattinson RC, Cuthbert A, Vannevel V. Pelvimetry for fetal cephalic presentations at or near term for deciding on mode of delivery. Cochrane Database Syst Rev. 2017;3 doi: 10.1002/14651858.CD000161.pub2. CD000161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tian Y, Chen J. The effects of laparoscopic myomectomy and open surgery on uterine myoma patients' postoperative immuno-inflammatory responses, endocrine statuses, and prognoses: A comparative study. Am J Transl Res. 2021;13:9671–8. [PMC free article] [PubMed] [Google Scholar]
- 24.Bhave Chittawar P, Franik S, Pouwer AW, Farquhar C. Minimally invasive surgical techniques versus open myomectomy for uterine fibroids. Cochrane Database Syst Rev. 2014;10 doi: 10.1002/14651858.CD004638.pub3. CD004638. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.


