Abstract
Purpose of review
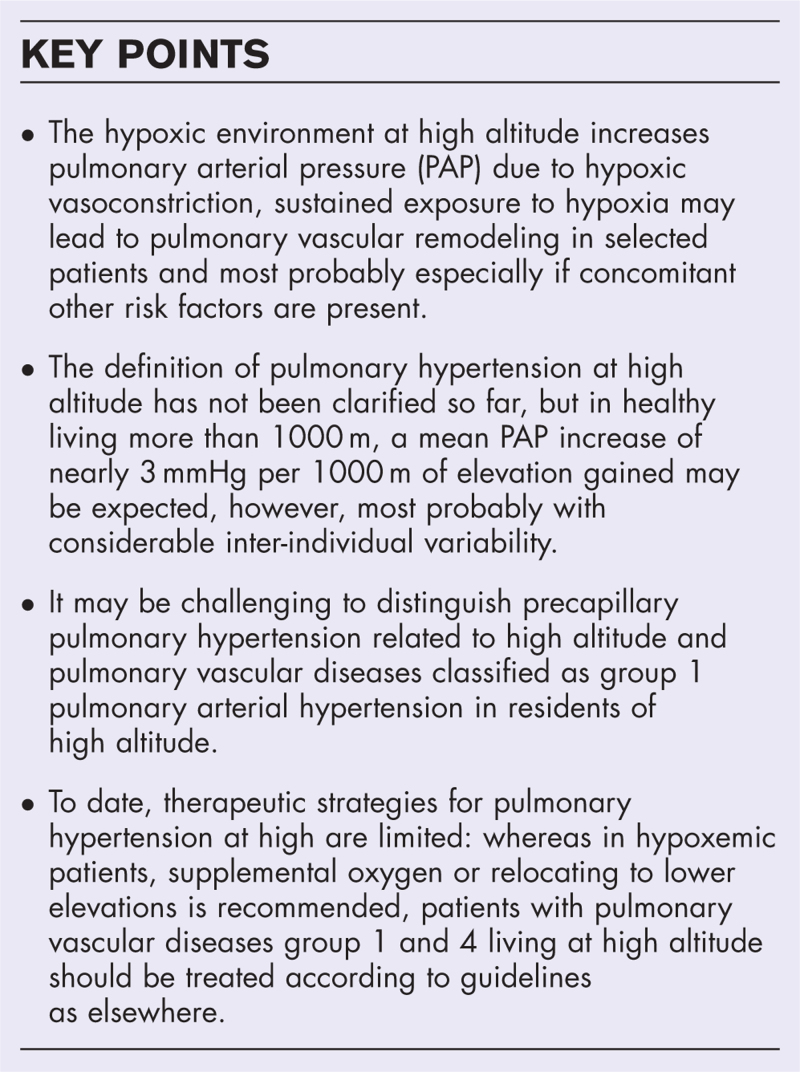
This review addresses the concern of the health effects associated with high-altitude living and chronic hypoxia with a focus on pulmonary hypertension. With an increasing global population residing at high altitudes, understanding these effects is crucial for public health interventions and clinical management.
Recent findings
Recent literature on the long-term effects of high-altitude residence and chronic hypoxia is comprehensively summarized. Key themes include the mechanisms of hypoxic pulmonary vasoconstriction, the development of pulmonary hypertension, and challenges in distinguishing altitude-related pulmonary hypertension and classical pulmonary vascular diseases, as found at a low altitude.
Summary
The findings emphasize the need for research in high-altitude communities to unravel the risks of pulmonary hypertension and pulmonary vascular diseases. Clinically, early and tailored management for symptomatic individuals residing at high altitudes are crucial, as well as access to advanced therapies as proposed by guidelines for pulmonary vascular disease. Moreover, identifying gaps in knowledge underscores the necessity for continued research to improve understanding and clinical outcomes in high-altitude pulmonary vascular diseases.
Keywords: high altitude, hypoxia, pulmonary hypertension, pulmonary vascular disease
INTRODUCTION
Mountains cover about a quarter of the continental surface and hypoxia is a public health problem for the more than 500 million humans worldwide who live at least over 1500 m (>6% of the total population) of which 80 to 120 million live at least 2500 m above sea level (>1% of the total population) [1,2]. According to current guidelines for clinical high-altitude research, we define high altitude as an elevation of at least 2500 m or more above sea level [3]. The sustained exposure to a hypoxic environment puts altitude dwellers at risk of developing chronic side effects such as pulmonary hypertension and chronic mountain sickness (CMS). In addition, amongst the millions of high-altitude dwellers, as elsewhere, there are many patients with chronic lung diseases including the worldwide highly prevalent chronic obstructive lung disease (COPD), but also rare conditions such as the pulmonary vascular diseases (PVDs) pulmonary arterial and chronic thromboembolic pulmonary hypertension (PAH/CTEPH) [4,5]. The potential additive threats of a hypobaric hypoxic environment at high altitude to these exercise-accelerated hypoxemic lung diseases are not unraveled conclusively yet.
The objective of this review is to provide a comprehensive summary of recent literature concerning the long-term consequences of high-altitude residence and the influence of prolonged hypoxic exposure on the prevalence of PVD.
Box 1.
no caption available
REVIEW
Hypoxic pulmonary vasoconstriction
Hypoxic pulmonary vasoconstriction (HPV) is the essential mechanism for matching perfusion to changes in local ventilation and thus optimizing pulmonary oxygen uptake and systemic delivery and carbon dioxide elimination [6–8]. The major determinant of HPV is the partial pressure for oxygen in alveolar air, but mixed venous oxygen partial pressure may also contribute [9,10]. The hypoxic environment at high altitude increases ventilation and heart rate, mediated by the increased sympathetic activity through chemoreceptor stimulation, and increased pulmonary artery pressure (PAP) due to vasoconstriction [11,12]. Arterial hypoxemia is even aggravated during exercise and sleep at high altitude [13▪,14,15]. HPV has its onset within seconds of exposure to hypoxia with a plateau-phase within minutes and a further increase over several hours and is reversible on restoration of normal airway oxygen levels [9,16–18]. If hypoxic air breathing is sustained for months to years, it may lead to pulmonary vascular remodeling resulting in persistent pulmonary hypertension in selected patients, especially in the presence of other stimuli, such as sleep apnea [19–24]. The degree of HPV is associated with the severity of the hypoxic stimulus, but the intensity of HPV varies between individuals and is influenced by a number of diseases and medications [22,25]. Animal models have demonstrated that HPV may play a role in the pathogenesis of PVD, which was supported by the finding that family members of patients with hereditary PAH exhibit enhanced HPV responsiveness [26–28].
High-altitude pulmonary hypertension
According to the updated ERS guidelines on pulmonary hypertension, precapillary pulmonary hypertension is defined hemodynamically by a mean PAP more than 20 mmHg with a pulmonary artery wedge pressure (PAWP) ≤15 mmHg along with a pulmonary vascular resistance (PVR) more than 2 WU assessed by right heart catheterization [5]. Pulmonary hypertension is classified into five major groups according to the clinical presentation and response to vasodilator therapies. Symptoms of pulmonary hypertension are mainly linked to right ventricle dysfunction, typically associated with exercise in the earlier course of the disease. The cardinal symptom of pulmonary hypertension is dyspnea on exertion, which leads to reduced quality of life [29–32], and many patients reveal exercise or sleep-aggravated hypoxemia, which ameliorates with supplemental oxygen therapy [33–36].
Altitude dwellers are at risk of developing pulmonary hypertension due to chronic exposure to hypoxia, but to date, it remains unclear to what extent this elevated PAP is related to symptoms and disease [30]. The definition of pulmonary hypertension at high altitude has not been clarified so far, as PAP is increased at high altitude already in healthy, albeit usually to a minor extent [21,37]. In 2005, an international consensus statement defined high altitude pulmonary hypertension based on the following criteria: resident at altitudes more than 2500 m with a mean PAP more than 30 mmHg or a systolic PAP more than 50 mmHg, right ventricular hypertrophy, right heart failure, and moderate hypoxemia without excessive erythrocytosis (hemoglobin <21 g/dl in men and <19 g/dl in women) [37]. The prevalence of high-altitude pulmonary hypertension fluctuates widely between 6 and 35% within the general population residing at altitudes ranging from 2500 to 3500 m [38]. This variability stems from differing definitions of the condition, posing challenges in distinguishing affected highlanders from those who are asymptomatic [21]. In addition, there is a considerable overlap between this disease and subacute mountain sickness, a syndrome of pulmonary hypertension and right heart failure observed in lowlanders following prolonged stays at high altitudes [39]. There is also some debate about whether this truly represents a separate entity from CMS or is simply a variant of the same disease [19], and the role of concomitant conditions, such as sleep disordered breathing including the highly prevalent obstructive sleep apnea (OSA) or COPD is also not known [24,40].
Previous studies indicate that PAP is higher in high-altitude dwellers with CMS [19]. CMS is a syndrome presenting with dyspnea, fatigue, poor sleep, headache, tinnitus, paresthesias, and cyanosis related to excessive polycythaemia defined by a hemoglobin concentration of more than 21 g/d in men and more than 19 g/dl in women [37]. Patients suffering from CMS experience profound hypoxemia due to a relative failure in adapting ventilation to hypoxia. However, despite this disparity, they exhibit a similar relationship between pulmonary arterial oxygen saturation and hypoxia as observed in healthy individuals living at high altitudes [19,41]. Patients with CMS respond with accentuated PAP responses to modest exercise when compared with healthy individuals living at the same elevation. Therefore, it is suggested that HPV might not solely be attributed to heightened alveolar hypoxia [42]. In 2019, a meta-analysis by Soria et al.[43] focused on echocardiographic data of 287 patients (nine studies) with CMS at rest and 142 of them (five studies) at exercise. Surprisingly, they found a mean PAP of 18 mmHg [95% confidence interval (95% CI) 16–20] at rest and 31 mmHg (95% CI 29–33) during exercise, indicating only mild pulmonary hypertension during exercise [43]. Previously, a similar meta-analysis in 834 healthy altitude dwellers at rest showed a mean PAP of 18–24 mmHg, compared to 13–20 mmHg, respectively, in sea level controls [23].
High altitude and pulmonary vascular disease – an association?
In the absence of predominant lung disease, the major precapillary pulmonary hypertension forms are PAH and CTEPH hereafter summarized as PVD [37]. Over the past decades, animal models have shown that hypoxia not only induces pulmonary vasoconstriction but also pulmonary vascular remodeling [44]. Anatomic observations of highlanders indicate postnatal structural remodeling of the distal pulmonary arteries and arterioles, presenting with marked individual variability [19,45]. HPV may play a role in the pathogenesis of PVD, which has been indicated in family members of patients with hereditary PAH, who exhibit enhanced HPV responsiveness [26–28]. Ethnic disparities related to differing endogenous nitric oxide production among human populations have been discussed, as Tibetan high-altitude inhabitants have been shown to have a lower PAP compared with Andean inhabitants [19,46]. It is noteworthy that these data are based on studies with small sample sizes and this discrepancy tends to diminish when adjustments are made for hematocrit to correct PVR [47]. However, it remains unclear to what extent pulmonary hypertension is a public health problem in high-altitude communities [30]. As of now, there are no epidemiological studies demonstrating an increased prevalence of symptomatic PVD among residents of mountainous regions. However, most probably at least with a comparable prevalence as at low altitude, there are also patients with PVD, who permanently live in one of the many large cities located more than 2500m worldwide with populations estimated to be more than 100 million. It may be challenging to distinguish between precapillary entities of high-altitude pulmonary hypertension (stratified to group 3 PH according to the ERS guidelines) and classical PVD including PAH group 1 or especially distal CTEPH group 4, which reveal other pathomechanisms but may share pathogenetic endways [30,48]. In 2020, Fakhri et al.[49] performed an analysis of the US American Pulmonary Hypertension Association Registry to investigate the difference between PAH living at moderate altitude (defined as ≥4000 feet/1220 m) vs. low altitude. This registry analysis found that use of supplemental oxygen and PVR were higher in PVD living at more than 1200 m, but of interest, the 6-min walk distance was even higher than in PVD-lowlanders [49]. They proposed to classify patients with precapillary pulmonary hypertension resident at higher elevation as PAH based on the healthcare providers’ judgement of whether the measured pulmonary hypertension is disproportionate to what might be expected due to mere hypoxemia in a hypoxic environment. According to a meta-analysis, the mean tricuspid regurgitation pressure gradient in healthy residents between 3600 and 4350 m was 28 [26–30] mmHg [43], thus, assuming a normal right atrial pressure the mean PAP in healthy at nearly 4000 m is estimated nearly 22 mmHg [50]. If we assume that this is 8–10 mmHg higher than normal for people living less than 1000m [51] and that the increase in mPAP with altitude is linear, we may roughly have to increase the normal mPAP by nearly 3 mmHg with every 1000 m of altitude gained above 1000 m. Thus, in a large city located at nearly 2500 m, we have to assume that a symptomatic patient with a mPAP more than 25 mmHg indeed has pulmonary hypertension and not mere PAP-increase due to the hypoxic environment and the younger patients are and the higher the mPAP, the more we will clinically think of PVD. However, clear parameters to distinguish between entities remain unclear, as further studies are still pending.
Studies examining PVD-patients whilst breathing normobaric hypoxia during right heat catheterization at low altitude revealed that HPV may be blunted in PVD [52,53]. Additionally, a majority of PVD-patients residing at low altitude felt well during a day or overnight trip to 2500 m with unchanged pulmonary vascular pressure-flow slope during exercise and only mildly reduced exercise capacity, comparable to healthy probands [13▪,54]. A study involving 36 PVD patients (89% with PAH) living in Quito, Ecuador, at an altitude of 2840 m suggests that their risk factor profiles are similar to those of counterparts living at lower altitudes [PVRI meeting London 2024, [55]]. Nevertheless, many questions about PVD residing or traveling to high altitude remain unanswered and many future questions about potential risks of residing at or traveling to high altitude for PVD remain to be elucidated.
Therapeutic strategies for pulmonary hypertension at high altitude
According to animal studies, hypoxic pulmonary vascular remodeling begins to develop within the first hours of hypoxic exposure. In healthy highlanders, PVR is not completely reversible to baseline with supplemental oxygen, but studies have shown that hypoxic pulmonary hypertension may completely resolves after returning to lower altitudes [55,56]. Similarly, complete resolution of pulmonary hypertension is observed after restoring normoxemia, for example, in patients with hypoventilation syndromes at the intensive care unit in the absence of PVD, but mere hypoxemic or hypercapnic pulmonary hypertension. Clinically, early detection of symptomatic disease and tailored management strategies are crucial for individuals residing at high altitudes. The optimal treatment for symptomatic high-altitude pulmonary hypertension is relocation to lower elevation, which may not be feasible for many patients due to socioeconomical reasons. A small placebo-controlled trial demonstrated that a 3-month course of the phosphodiesterase inhibitor sildenafil modestly lowered PAP (approx. 6--7 mmHg) and improved exercise capacity. As no larger studies of this or other pulmonary vasodilators have been performed, currently, there are no clear treatment guidelines [57]. Patients with PVD living at high altitude should be treated according to guidelines as elsewhere [5]. Special challenges hereby are the fact that many of the large cities located at higher elevations are located in world regions, where access to expensive medical investigations and drug and nonpharmaceutical therapies is restricted due to socioeconomic constraints. Even more than at low altitude, domiciliary and especially nocturnal supplemental oxygen therapy complements drug therapies [36].
CONCLUSION
Residing at high altitudes exposes individuals to chronic hypoxia. This leads to an increasing public health concern due to higher prevalences of CMS and symptomatic high-altitude pulmonary hypertension. While HPV plays a crucial role in optimizing pulmonary oxygen uptake, prolonged exposure to hypoxia can result in pulmonary vascular remodeling and persistent pulmonary hypertension in susceptible individuals. The prevalence is most probably accelerated in the presence of additional prevalent conditions, such as COPD or sleep apnea. The definition and prevalence of pulmonary hypertension at high altitudes remain ambiguous. On top, the distinction between altitude-related pulmonary hypertension and classical PVD as seen in lowlanders may not be trivial. Therapeutic options for high altitude pulmonary hypertension are limited, with relocation to lower elevations being the most effective but often impractical solution and treatment of PVD should be based on international guidelines. Further research is needed to better understand the pathophysiology and develop effective treatment strategies for individuals living in high-altitude regions facing the challenges of pulmonary hypertension.
Acknowledgements
The authors would like to thank the pulmonary hypertension teams in Zurich and Quito for their effort to support pulmonary hypertension patients and their help in carrying out multiple research projects in the field.
Financial support and sponsorship
None.
Conflicts of interest
S. Ulrich receives research grants from the Swiss National Science Foundation, Zurich and Swiss Lung League and EMDO foundation and grants, travel support and consultancy fees from Orpha Swiss, Janssen SA, MSD SA, and Novartis all unrelated to the present work. All other authors report no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Tremblay JC, Ainslie PN. Global and country-level estimates of human population at high altitude. Proc Natl Acad Sci U S A 2021; 118:e2102463118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Naeije R. Pulmonary hypertension at high altitude. Eur Respir J 2019; 53:1900985. [DOI] [PubMed] [Google Scholar]
- 3.Brodmann Maeder M, Brugger H, Pun M, et al. The STAR Data Reporting Guidelines for clinical high altitude research. High Alt Med Biol 2018; 19:7–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agusti A, Celli BR, Criner GJ, et al. Global Initiative for Chronic Obstructive Lung Disease 2023 Report: GOLD executive summary. Respirology 2023; 28:316–338. [DOI] [PubMed] [Google Scholar]
- 5.Humbert M, Kovacs G, Hoeper MM, et al. 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J 2022; 43:3618–3731. [DOI] [PubMed] [Google Scholar]
- 6.Bradford JR, Dean HP. The pulmonary circulation. J Physiol 1894; 16:34–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.von Euler US, Liljestrand G. Observation on the pulmonary arterial blood pressure in the cat. Acta Physiol Scand 1946; 12:301–320. [Google Scholar]
- 8.Reeves JT, Wagner WW, Jr, McMurtry IF, Grover RF. Physiological effects of high altitude on the pulmonary circulation. Int Rev Physiol 1979; 20:289–310. [PubMed] [Google Scholar]
- 9.Marshall C, Marshall B. Site and sensitivity for stimulation of hypoxic pulmonary vasoconstriction. J Appl Physiol Respir Environ Exerc Physiol 1983; 55:711–716. [DOI] [PubMed] [Google Scholar]
- 10.Kylhammar D, Radegran G. The principal pathways involved in the in vivo modulation of hypoxic pulmonary vasoconstriction, pulmonary arterial remodelling and pulmonary hypertension. Acta Physiol 2017; 219:728–756. [DOI] [PubMed] [Google Scholar]
- 11.Siebenmann C, Lundby C. Regulation of cardiac output in hypoxia. Scand J Med Sci Sports 2015; 25: (Suppl 4): 53–59. [DOI] [PubMed] [Google Scholar]
- 12.Albert TJ, Swenson ER. Peripheral chemoreceptor responsiveness and hypoxic pulmonary vasoconstriction in humans. High Alt Med Biol 2014; 15:15–20. [DOI] [PubMed] [Google Scholar]
- 13▪.Muller J, Titz A, Schneider SR, et al. The effect of high altitude (2500 m) on incremental cycling exercise in patients with pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension: a randomised controlled crossover trial. Eur Respir J 2024; 63:2301001. [DOI] [PMC free article] [PubMed] [Google Scholar]; The publication ‘The effect of high altitude (2500 m) on incremental cycling exercise in patients with pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension: a randomised controlled crossover trial’ (Eur Respir J. 2024) by Müller et al. is of special interest, as it contributes significantly to the understanding of PAH and CTEPH exercise pathophysiology at altitude.
- 14.Lichtblau M, Saxer S, Latshang TD, et al. Altitude travel in patients with pulmonary hypertension: randomized pilot-trial evaluating nocturnal oxygen therapy. Front Med 2020; 7:502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schneider SR, Muller J, Bauer M, et al. Overnight exposure to high altitude in pulmonary hypertension: adverse events and effect of oxygen therapy. Eur Heart J 2024; 45:309–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Swenson ER. Hypoxic pulmonary vasoconstriction. High Alt Med Biol 2013; 14:101–110. [DOI] [PubMed] [Google Scholar]
- 17.Dunham-Snary KJ, Wu D, Sykes EA, et al. Hypoxic pulmonary vasoconstriction: from molecular mechanisms to medicine. Chest 2017; 151:181–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jensen KS, Micco AJ, Czartolomna J, et al. Rapid onset of hypoxic vasoconstriction in isolated lungs. J Appl Physiol 1992; 72:2018–2023. [DOI] [PubMed] [Google Scholar]
- 19.Penaloza D, Arias-Stella J. The heart and pulmonary circulation at high altitudes: healthy highlanders and chronic mountain sickness. Circulation 2007; 115:1132–1146. [DOI] [PubMed] [Google Scholar]
- 20.Olschewski H, Behr J, Bremer H, et al. Pulmonary hypertension due to lung diseases: updated recommendations from the Cologne Consensus Conference 2018. Int J Cardiol 2018; 272S:63–68. [DOI] [PubMed] [Google Scholar]
- 21.Lichtblau M, Saxer S, Furian M, et al. Cardiac function and pulmonary hypertension in Central Asian highlanders at 3250 m. Eur Respir J 2020; 56:1902474. [DOI] [PubMed] [Google Scholar]
- 22.Ulrich S, Lichtblau M, Schneider SR, et al. Clinician's corner: counseling patients with pulmonary vascular disease traveling to high altitude. High Alt Med Biol 2022; 23:201–208. [DOI] [PubMed] [Google Scholar]
- 23.Soria R, Egger M, Scherrer U, et al. Pulmonary artery pressure and arterial oxygen saturation in people living at high or low altitude: systematic review and meta-analysis. J Appl Physiol 2016; 121:1151–1159. [DOI] [PubMed] [Google Scholar]
- 24.Latshang TD, Furian M, Aeschbacher SS, et al. Association between sleep apnoea and pulmonary hypertension in Kyrgyz highlanders. Eur Respir J 2017; 49:1601530. [DOI] [PubMed] [Google Scholar]
- 25.De Canniere D, Stefanidis C, Hallemans R, et al. Stimulus-response curves for hypoxic pulmonary vasoconstriction in piglets. Cardiovasc Res 1992; 26:944–949. [DOI] [PubMed] [Google Scholar]
- 26.Grunig E, Dehnert C, Mereles D, et al. Enhanced hypoxic pulmonary vasoconstriction in families of adults or children with idiopathic pulmonary arterial hypertension. Chest 2005; 128: (6 Suppl): 630S–633S. [DOI] [PubMed] [Google Scholar]
- 27.Oka M, Homma N, Taraseviciene-Stewart L, et al. Rho kinase-mediated vasoconstriction is important in severe occlusive pulmonary arterial hypertension in rats. Circ Res 2007; 100:923–929. [DOI] [PubMed] [Google Scholar]
- 28.Voelkel NF, Gomez-Arroyo J. The role of vascular endothelial growth factor in pulmonary arterial hypertension. The angiogenesis paradox. Am J Respir Cell Mol Biol 2014; 51:474–484. [DOI] [PubMed] [Google Scholar]
- 29.McGoon MD, Ferrari P, Armstrong I, et al. The importance of patient perspectives in pulmonary hypertension. Eur Respir J 2019; 53:1801919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Humbert M, Kovacs G, Hoeper MM, et al. 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Respir J 2023; 61:2200879. [DOI] [PubMed] [Google Scholar]
- 31.Cenedese E, Speich R, Dorschner L, et al. Measurement of quality of life in pulmonary hypertension and its significance. Eur Respir J 2006; 28:808–815. [DOI] [PubMed] [Google Scholar]
- 32.Saxer S, Lichtblau M, Berlier C, et al. Physical activity in incident patients with pulmonary arterial and chronic thromboembolic hypertension. Lung 2019; 197:617–625. [DOI] [PubMed] [Google Scholar]
- 33.Hildenbrand FF, Bloch KE, Speich R, Ulrich S. Daytime measurements underestimate nocturnal oxygen desaturations in pulmonary arterial and chronic thromboembolic pulmonary hypertension. Respiration 2012; 84:477–484. [DOI] [PubMed] [Google Scholar]
- 34.Ulrich S, Hasler ED, Saxer S, et al. Effect of breathing oxygen-enriched air on exercise performance in patients with precapillary pulmonary hypertension: randomized, sham-controlled cross-over trial. Eur Heart J 2017; 38:1159–1168. [DOI] [PubMed] [Google Scholar]
- 35.Ulrich S, Keusch S, Hildenbrand FF, et al. Effect of nocturnal oxygen and acetazolamide on exercise performance in patients with precapillary pulmonary hypertension and sleep-disturbed breathing: randomized, double-blind, cross-over trial. Eur Heart J 2015; 36:615–623. [DOI] [PubMed] [Google Scholar]
- 36.Ulrich S, Saxer S, Hasler ED, et al. Effect of domiciliary oxygen therapy on exercise capacity and quality of life in patients with pulmonary arterial or chronic thromboembolic pulmonary hypertension: a randomised, placebo-controlled trial. Eur Respir J 2019; 54:1900276. [DOI] [PubMed] [Google Scholar]
- 37.Leon-Velarde F, Maggiorini M, Reeves JT, et al. Consensus statement on chronic and subacute high altitude diseases. High Alt Med Biol 2005; 6:147–157. [DOI] [PubMed] [Google Scholar]
- 38.Lichtblau M, Saxer S, Furian M, et al. Cardiac function and pulmonary hypertension in Central Asian highlanders at 3250 m. Eur Respir J 2020. [DOI] [PubMed] [Google Scholar]
- 39.Anand IS, Malhotra RM, Chandrashekhar Y, et al. Adult subacute mountain sickness--a syndrome of congestive heart failure in man at very high altitude. Lancet 1990; 335:561–565. [DOI] [PubMed] [Google Scholar]
- 40.Bloch KE, Buenzli JC, Latshang TD, Ulrich S. Sleep at high altitude: guesses and facts. J Appl Physiol 2015; 119:1466–1480. [DOI] [PubMed] [Google Scholar]
- 41.Leon-Velarde F, Richalet JP. Respiratory control in residents at high altitude: physiology and pathophysiology. High Alt Med Biol 2006; 7:125–137. [DOI] [PubMed] [Google Scholar]
- 42.Stuber T, Sartori C, Schwab M, et al. Exaggerated pulmonary hypertension during mild exercise in chronic mountain sickness. Chest 2010; 137:388–392. [DOI] [PubMed] [Google Scholar]
- 43.Soria R, Egger M, Scherrer U, et al. Pulmonary arterial pressure at rest and during exercise in chronic mountain sickness: a meta-analysis. Eur Respir J 2019; 53:1802040. [DOI] [PubMed] [Google Scholar]
- 44.Sylvester JT, Shimoda LA, Aaronson PI, Ward JP. Hypoxic pulmonary vasoconstriction. Physiol Rev 2012; 92:367–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Naeije R, Dedobbeleer C. Pulmonary hypertension and the right ventricle in hypoxia. Exp Physiol 2013; 98:1247–1256. [DOI] [PubMed] [Google Scholar]
- 46.Beall CM. Tibetan and Andean contrasts in adaptation to high-altitude hypoxia. Adv Exp Med Biol 2000; 475:63–74. [DOI] [PubMed] [Google Scholar]
- 47.Naeije R, Vanderpool R. Pulmonary hypertension and chronic mountain sickness. High Alt Med Biol 2013; 14:117–125. [DOI] [PubMed] [Google Scholar]
- 48.Humbert M, Guignabert C, Bonnet S, et al. Pathology and pathobiology of pulmonary hypertension: state of the art and research perspectives. Eur Respir J 2019; 53:1801887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fakhri S, Hannon K, Moulden K, et al. Residence at moderately high altitude and its relationship with WHO Group 1 pulmonary arterial hypertension symptom severity and clinical characteristics: the Pulmonary Hypertension Association Registry. Pulm Circ 2020; 10:2045894020964342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chemla D, Humbert M, Sitbon O, et al. Systolic and mean pulmonary artery pressures: are they interchangeable in patients with pulmonary hypertension? Chest 2015; 147:943–950. [DOI] [PubMed] [Google Scholar]
- 51.Kovacs G, Berghold A, Scheidl S, Olschewski H. Pulmonary arterial pressure during rest and exercise in healthy subjects: a systematic review. Eur Respir J 2009; 34:888–894. [DOI] [PubMed] [Google Scholar]
- 52.Carta AU, S. The impact of breathing hypoxic gas and oxygen on pulmonary hemodynamics in patients with pulmonary hypertension. Front Med (Lausanne) 2022; 9:791423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Groth A, Saxer S, Bader PR, et al. Acute hemodynamic changes by breathing hypoxic and hyperoxic gas mixtures in pulmonary arterial and chronic thromboembolic pulmonary hypertension. Int J Cardiol 2018; 270:262–267. [DOI] [PubMed] [Google Scholar]
- 54.Schneider SR, Mayer LC, Lichtblau M, et al. Effect of a day-trip to altitude (2500 m) on exercise performance in pulmonary hypertension: randomised crossover trial. ERJ Open Res 2021; 7:00314–2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sime F, Penaloza D, Ruiz L. Bradycardia, increased cardiac output, and reversal of pulmonary hypertension in altitude natives living at sea level. Br Heart J 1971; 33:647–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Maggiorini M, Melot C, Pierre S, et al. High-altitude pulmonary edema is initially caused by an increase in capillary pressure. Circulation 2001; 103:2078–2083. [DOI] [PubMed] [Google Scholar]
- 57.Aldashev AA, Kojonazarov BK, Amatov TA, et al. Phosphodiesterase type 5 and high altitude pulmonary hypertension. Thorax 2005; 60:683–687. [DOI] [PMC free article] [PubMed] [Google Scholar]