Abstract
Aim:
Exploring trends in 1) alcohol-specific mortality and 2) alcohol sales in European countries in the years before and during the COVID-19 pandemic.
Method:
Complete data on alcohol-specific mortality and alcohol sales were obtained for 14 European countries (13 EU countries and UK) for the years 2010 to 2020, with six countries having mortality data available up to 2021. Age-standardised mortality rates were calculated and descriptive statistics used.
Results:
When compared to 2019, alcohol-specific mortality rates in 2020 increased by 7.7 % and 8.2 % for women and men, respectively. Increases in alcohol-specific mortality were seen in the majority of countries and continued in 2021. In contrast, alcohol sales declined by an average of 5.0 %.
Conclusion:
Despite a drop in alcohol consumption, more people died due to alcohol-specific causes during the COVID-19 pandemic in Europe.
Keywords: alcohol burden, alcohol sales, substance use, public health crisis, public health
Zusammenfassung:
Zielsetzung:
Beschreibung der Trendverläufe der 1) alkoholspezifischen Mortalität und 2) des Alkoholverbrauchs in europäischen Ländern vor und während der COVID-19-Pandemie.
Methodik:
Vollständige Daten zur alkoholspezifischen Mortalität sowie zum Alkoholverbrauch zwischen 2010 und 2020 waren für 14 Europäische Länder (13 EU-Länder und Großbritannien) verfügbar; Mortalitätsdaten aus 2021 für sechs Länder. Für die Auswertung wurden altersstandardisierte Mortalitätsraten und deskriptive Statistiken berechnet.
Ergebnisse:
Die alkoholspezifische Mortalitätsrate stieg 2020 ggü. dem Vorjahr um 7.7 % bzw. 8.2 % bei Frauen und Männern an. Dieser Anstieg war in den meisten Ländern zu beobachten und setzte sich im Jahr 2021 fort. Der Alkoholverbrauch sank im Mittel um 5.0 %.
Schlussfolgerungen:
Trotz sinkendem Alkoholkonsums sind während der COVID-19-Pandemie in Europa mehr Personen an alkoholspezifischen Erkrankungen gestorben.
Schlüsselwörter: Alkoholmortalität, Krankheitslast, Substanzkonsum, Gesundheitskrise, Public Health
Introduction
Despite a decline in alcohol consumption since the 2000s, Europe still has the highest adult (15 years of age and older) per capita consumption of alcohol globally (Manthey et al., 2019). In the European Union (EU) plus the United Kingdom (UK), alcohol causes almost 320 000 deaths annually and remains the leading risk factor for premature death among 15-to-49-year-olds (GBD 2019 Risk Factors Collaborators, 2020). Recent progress towards lowering alcohol consumption (Probst et al., 2020) and its health burden (Shield et al., 2020) has been challenged by the emergence of the COVID-19 pandemic in early 2020, as particularly hazardous alcohol users were expected to increase their drinking (Gonçalves et al., 2020; Rehm et al., 2020). Hazardous alcohol use has been defined by the World Health Organization (WHO) as a pattern of alcohol use that increases the risk of harmful physical or mental health consequences to the alcohol user or to others (Saunders et al., 2019).
In the course of the pandemic, patterns of alcohol consumption changed and about half of survey participants across Europe reported decreases or increases in their drinking (Acuff et al., 2021; Kilian, O’Donnell, et al., 2022). As expected, heavier alcohol users were more likely to increase their consumption (Rossow et al., 2021; Schmidt et al., 2021), while sales data suggest decreases in consumption levels at the population level (Anderson et al., 2022; Leifman et al., 2022; Mäkelä et al., 2021). In addition to changes in alcohol consumption, it has been observed that alcohol-specific health care services were underutilized in Germany during the pandemic. Compared to 2019, hospital discharges of acute alcohol-specific conditions, such as alcohol poisonings or intoxications, dropped by −21.4 % and −25.1 % in women and men, respectively, in 2020 and there was a decline for chronic conditions, such as alcohol use disorders and alcoholic liver disease, of about −8 % (Manthey et al., 2023).
A key indicator is the number of deaths which are wholly attributable to alcohol (i. e., alcohol-specific deaths). Data from the UK and Germany suggest that alcohol-specific mortality has increased during the pandemic, by +9.9 % to +23.7 % in the UK (Angus et al., 2023) and by +5.3 % in Germany (Kilian, Carr et al., 2022). To date, it has not been explored whether this observation can be replicated in other European countries. To close this knowledge gap, we explore trends in alcohol-specific mortality in a selection of EU countries and the UK between 2010 and 2020. We contrast these trends with data on alcohol sales to obtain a more detailed picture of patterns of change across countries.
Methodology
Data Sources
For this explorative study, we obtained mortality data from the WHO (World Health Organization, 2023a). We included the following ICD-10 codes, indicating causes of deaths wholly attributable to alcohol, i. e., none of these deaths would have occurred in the absence of alcohol (as available in the databank): F10*, G31.2, G62.1, G72.1, I42.6, K29.2, K70*, K85.2, K86.0, Q86.0, T51*, X45. Alcohol sales data were also sourced from the WHO (World Health Organization, 2023b), expressed as the total amount of pure alcohol produced, sold, or taxed per year for the population 15 years or older (i. e., recorded per capita alcohol consumption). The sales data are not adjusted for tourist or unrecorded alcohol consumption and are only available until 2020.
To calculate mortality rates, i. e., the number of deaths per 100 000 population, we used United Nations population data (Population on 01 July, by 5-year age groups, medium variant; United Nations, Department of Economic and Social Affairs, Population Division, 2022). We further applied age-standardisation to account for differences in the age distribution across locations and time, employing the European Standard Population (EU-27 and EFTA standard population; European Commission et al., 2013).
Data Analyses
We selected those countries with consistently available mortality data between 2010 and (at least) 2020, resulting in n = 16 countries. Two smaller countries were excluded because of low number and temporal instability of annual deaths counts (data from 2020: Cyprus: 17 deaths; Luxembourg: 74 deaths; smallest number of deaths in other countries: 239 in Greece). Our final analytic sample therefore represent a population of 253 709 000 adults aged 15 or older residing in 14 European countries (Austria, Bulgaria, Czechia, Germany, Denmark, Spain, Estonia, Finland, Lithuania, Latvia, Netherlands, Poland, Slovenia, UK). For a subset of countries, mortality data was also available for 2021 (n = 6 countries).
To examine country-specific trends in the age-standardised alcohol-specific mortality rates and alcohol sales, we calculated their annual change relative to 2019. Findings are presented in tables and graphs and descriptive statistics (means, percentages) were computed in R version 4.2.3 (R Core Team, 2023). The data and R code are publicly available at the Figshare repository (Manthey & Kilian, 2023).
Results
Cross-National Trends
Before 2020, the annual number of alcohol-specific deaths ranged between 38 694 (year 2014) and 42 303 (year 2019) across all 14 countries. Between 2019 and 2020, the number of alcohol-specific deaths increased by 3749 deaths to a total of 46 052 (+8.9 %). This increase was about three times larger than the second largest increase between 2014 and 2015 (+1496 deaths) and about 14 times larger than the median annual change observed between 2010 and 2020 (+264 deaths). In terms of age-standardised mortality rates, we observed increases of +7.7 % and +8.2 % among women and men, respectively, in 2020 compared to 2019.
Country-Specific Trends
Sex- and country-specific data on the age-standardised alcohol-specific mortality and recorded per capita consumption are depicted in Table 1. In most countries, mortality rates remained largely stable between 2010 and 2019, while increasing in 2020 (see Figure 1).
Table 1.
Sex- and country-specific age-standardised alcohol-specific mortality rates and alcohol sales between 2010 and 2021.
| Country | Year | Women | Men | Alcohol sales in litres pure alcohol | Change in alcohol sales relative to 2019 (%) | ||
|---|---|---|---|---|---|---|---|
| Age-standardised mortality rate per 100 000 | Change in mortality rate relative to 2019 (%) | Age-standardised mortality rate per 100 000 | Change in mortality rate relative to 2019 (%) | ||||
| Austria | 2010 | 6.7 | . | 29.8 | . | 12.1 | . |
| 2015 | 6.8 | . | 27.9 | . | 11.6 | . | |
| 2019 | 6.5 | . | 24.6 | . | 11.9 | . | |
| 2020 | 6.9 | +6.8 | 27.4 | +11.1 | 11.2 | −5.8 | |
| 2021 | 8.4 | +29.5 | 29.1 | +18.3 | . | . | |
| Bulgaria | 2010 | 0.3 | . | 3.7 | . | 9.8 | . |
| 2015 | 0.7 | . | 5.9 | . | 11.0 | . | |
| 2019 | 0.8 | . | 7.0 | . | 11.5 | . | |
| 2020 | 1.3 | +49.9 | 8.1 | +14.8 | 11.1 | −3.4 | |
| Czechia | 2010 | 8.8 | . | 29.6 | . | 12.7 | . |
| 2015 | 9.7 | . | 31.4 | . | 12.8 | . | |
| 2019 | 12.2 | . | 34.6 | . | 13.0 | . | |
| 2020 | 12.0 | −1.6 | 37.0 | +7.0 | 11.6 | −11.3 | |
| 2021 | 13.5 | +10.6 | 39.8 | +15.2 | . | . | |
| Germany | 2010 | 10.3 | . | 32.5 | . | 11.1 | . |
| 2015 | 9.5 | . | 30.3 | . | 11.0 | . | |
| 2019 | 8.5 | . | 27.6 | . | 11.0 | . | |
| 2020 | 9.0 | +5.4 | 28.7 | +4.1 | 10.7 | −2.1 | |
| Denmark | 2010 | 18.4 | . | 54.5 | . | 10.2 | . |
| 2015 | 13.5 | . | 44.4 | . | 9.4 | . | |
| 2019 | 13.7 | . | 35.0 | . | 9.2 | . | |
| 2020 | 13.6 | −1.0 | 34.3 | −2.1 | 9.3 | +2.0 | |
| Estonia | 2010 | 24.2 | . | 76.5 | . | 15.0 | . |
| 2015 | 14.5 | . | 62.8 | . | 16.7 | . | |
| 2019 | 20.0 | . | 76.4 | . | 11.7 | . | |
| 2020 | 22.7 | +13.5 | 95.1 | +24.5 | 11.1 | −4.4 | |
| 2021 | 27.0 | +34.9 | 103.6 | +35.6 | . | . | |
| Finland | 2010 | 16.0 | . | 56.9 | . | 9.7 | . |
| 2015 | 14.0 | . | 47.0 | . | 8.5 | . | |
| 2019 | 15.1 | . | 45.8 | . | 8.2 | . | |
| 2020 | 14.2 | −6.3 | 47.3 | +3.3 | 8.3 | +0.3 | |
| Latvia | 2010 | 16.5 | . | 78.1 | . | 9.8 | . |
| 2015 | 18.5 | . | 82.8 | . | 10.8 | . | |
| 2019 | 14.8 | . | 64.1 | . | 12.9 | . | |
| 2020 | 13.8 | −6.8 | 54.0 | −15.8 | 12.6 | −2.0 | |
| 2021 | 25.6 | +72.9 | 97.6 | +52.3 | . | . | |
| Lithuania | 2010 | 15.3 | . | 63.5 | . | 12.0 | . |
| 2015 | 12.8 | . | 48.3 | . | 13.0 | . | |
| 2019 | 9.8 | . | 35.3 | . | 10.9 | . | |
| 2020 | 11.3 | +14.9 | 38.7 | +9.6 | 11.3 | +4.0 | |
| 2021 | 13.0 | +32.9 | 42.6 | +20.7 | . | . | |
| Netherlands | 2010 | 2.8 | . | 7.4 | . | 9.1 | . |
| 2015 | 3.7 | . | 9.8 | . | 8.3 | . | |
| 2019 | 3.4 | . | 9.5 | . | 8.2 | . | |
| 2020 | 3.1 | −9.0 | 10.8 | +13.6 | 7.7 | −6.0 | |
| Poland | 2010 | 5.4 | . | 31.6 | . | 10.1 | . |
| 2015 | 8.6 | . | 40.3 | . | 10.5 | . | |
| 2019 | 12.1 | . | 51.1 | . | 11.0 | . | |
| 2020 | 13.2 | +9.3 | 56.9 | +11.5 | 10.8 | −1.6 | |
| Slovenia | 2010 | 23.0 | . | 76.2 | . | 10.3 | . |
| 2015 | 15.4 | . | 66.4 | . | 11.5 | . | |
| 2019 | 19.1 | . | 80.9 | . | 11.1 | . | |
| 2020 | 18.5 | −2.9 | 69.2 | −14.5 | 9.8 | −11.3 | |
| Spain | 2010 | 1.5 | . | 9.2 | . | 8.8 | . |
| 2015 | 1.2 | . | 7.7 | . | 10.4 | . | |
| 2019 | 1.1 | . | 6.8 | . | 10.8 | . | |
| 2020 | 1.2 | +10.9 | 7.4 | +9.8 | 8.8 | −18.3 | |
| 2021 | 1.4 | +32.5 | 7.4 | +9.4 | . | . | |
| UK | 2010 | 8.8 | . | 19.9 | . | 10.0 | . |
| 2015 | 8.9 | . | 18.3 | . | 9.5 | . | |
| 2019 | 9.2 | . | 19.1 | . | 9.8 | . | |
| 2020 | 10.9 | +18.1 | 22.6 | +18.2 | 9.8 | −0.5 | |
| All 14 countries combined | 2010 | 7.7 | . | 25.9 | . | 10.3 | . |
| 2015 | 7.7 | . | 25.2 | . | 10.4 | . | |
| 2019 | 8.0 | . | 25.5 | . | 10.6 | . | |
| 2020 | 8.6 | +7.7 | 27.6 | +8.2 | 10.0 | −5.0 |
Notes. UK: United Kingdom.
Figure 1.
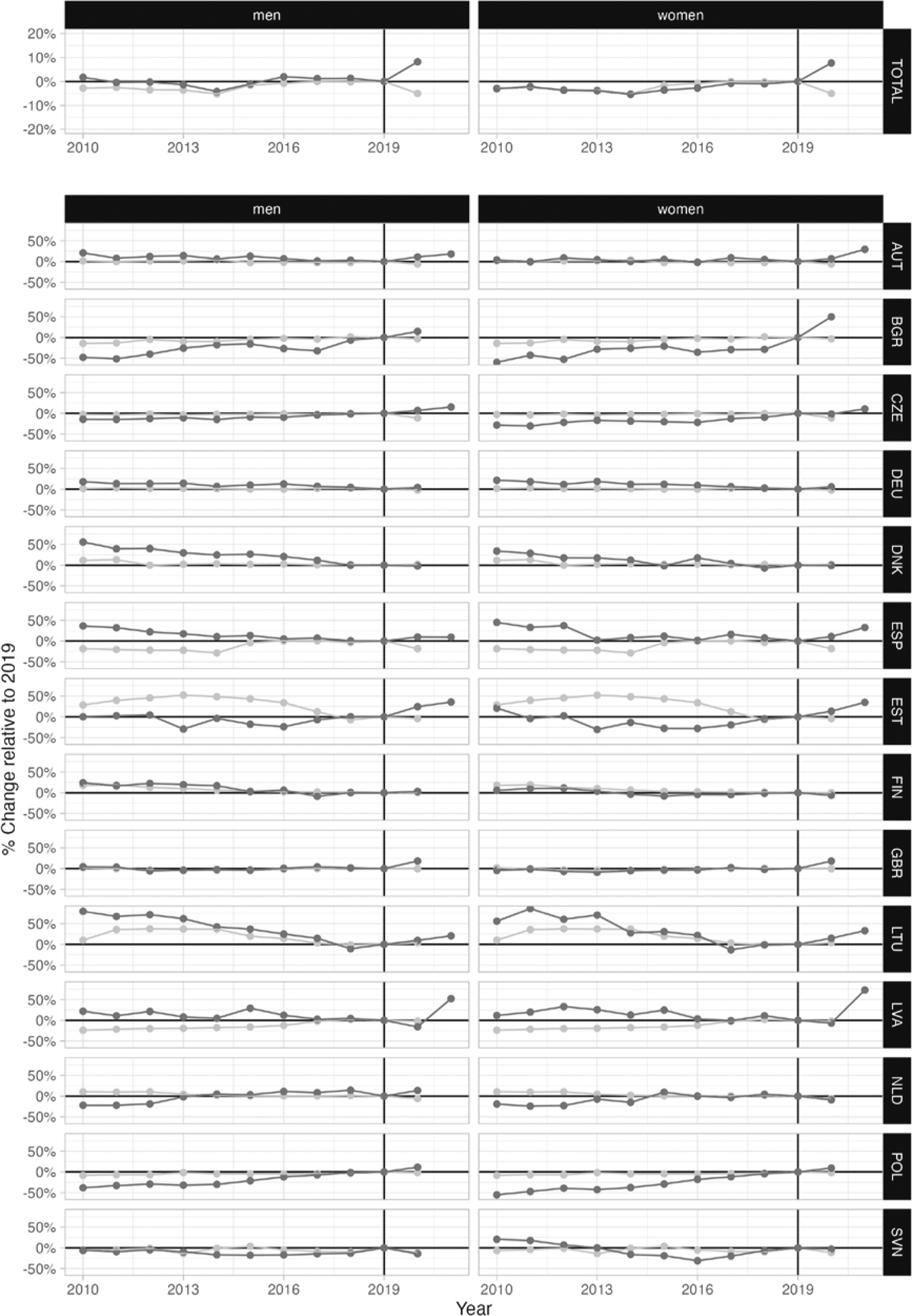
Changes in the alcohol-specific mortality rates (age-standardised; dark grey) and recorded per capita alcohol consumption (light grey) relative to 2019 (vertical line), by country. AUT: Austria, BGR: Bulgaria, CZE: Czechia, DEU: Germany, DNK: Denmark, ESP: Spain, EST: Estonia, FIN: Finland, GBR: United Kingdom, LTU: Lithuania, LVA: Latvia, NLD: Netherlands, POL: Poland, SVN: Slovenia, TOTAL: all 14 countries combined.
Relative to 2019, the largest increases in 2020 can be observed in Bulgaria, Estonia, and UK. More moderate increases were found in Austria, Germany, Lithuania, Poland, and Spain. In Finland, Czechia, and the Netherlands, alcohol-specific mortality decreased among women but increased among men. In Denmark, Latvia, and Slovenia, decreases were observed among both women and men. In the six countries with data available from 2021, alcohol-specific mortality has increased, with the sharpest increase in Latvia (see Figure 1).
Age-Specific Trends
Figure 2 illustrates age-specific trends in mortality for all 14 countries combined. Between 2010 and 2019, alcohol-specific mortality decreased among 45-to-59-year-old women and 40-to-59-year-old men, while rates increased for older adults, except for women aged 85+, and stagnated for those below age 45 (women) and 40 (men). In 2020, an increase in mortality can be observed in all age groups, with the strongest rise among middle-aged adults. Modest changes were found among 15–29-year-olds and among women aged 85+, who generally exhibited much lower mortality rates than the other age groups.
Figure 2.
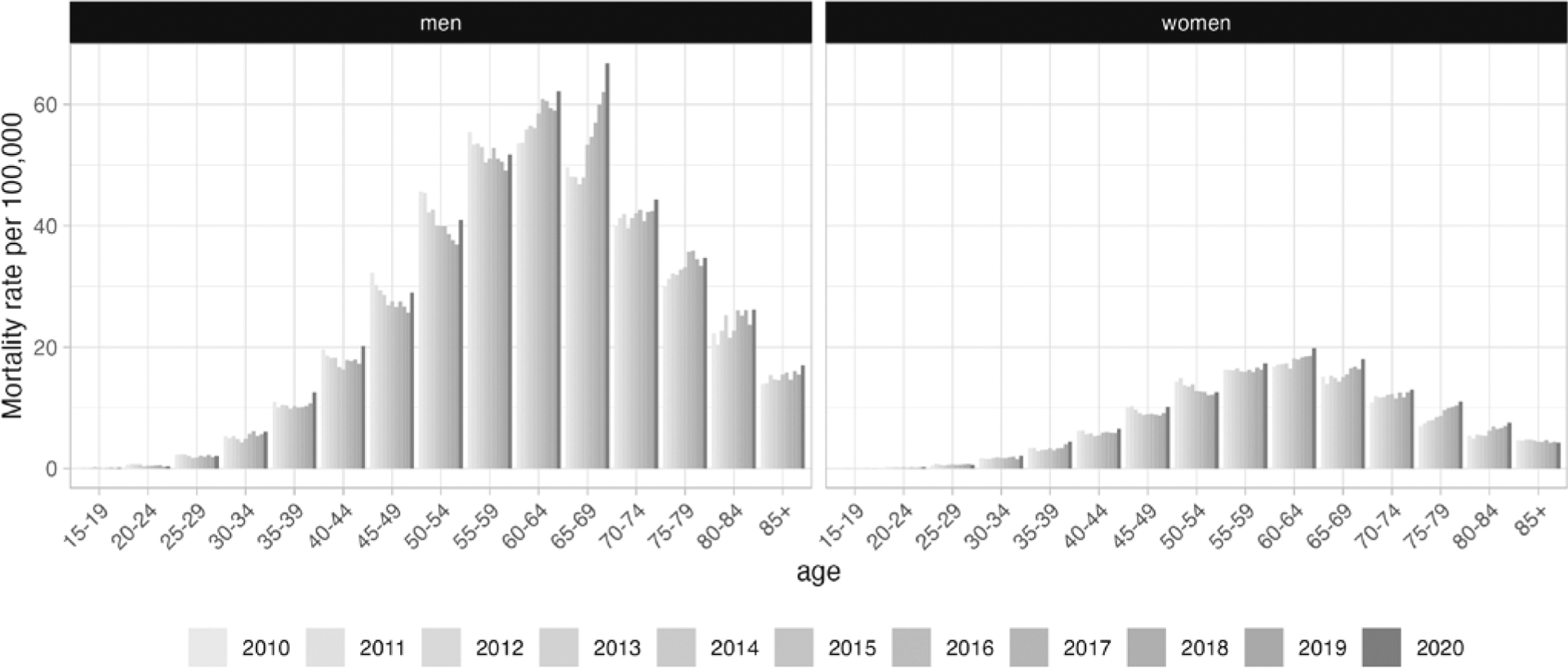
Age-specific mortality rates per 100 000 for men and women in 14 European countries between 2010 and 2020.
Trends in Alcohol Sales
Per capita consumption data suggest that consumption levels stagnated or decreased in 2020 compared to 2019 in most countries, with an average decline of −5.0 % across countries (for country results, see Table 1 and Figure 1). The most notable decline was observed in Spain, where per capita consumption decreased by −18.3 %.
Discussion
In the majority of 14 European countries, alcohol-specific mortality markedly increased in 2020. In all six countries with available data, this trend continued in 2021. The pre-pandemic downward trend in alcohol-specific mortality among 45-to-54-year-old women and 40-to-59-year-old men reversed and the situation worsened in older age groups, which had already exhibited increasing mortality rates before 2020. The Baltic countries Estonia, Latvia, and Lithuania stood out with the most dramatic increases in alcohol-specific mortality. In contrast to this general upward trend in mortality in 2020, recorded per capita alcohol consumption decreased or stagnated in most countries.
We find that with the emergence of the COVID-19 pandemic, alcohol-specific mortality increased in several but not all European countries. As extreme situations like natural disasters or economic crises are associated with elevated levels of stress, which in turn have been shown to be associated with increases in alcohol use, especially in heavier users (De Goeij et al., 2015), increases in drinking among hazardous alcohol users as well as a rise in alcohol use disorders had been predicted at the beginning of the pandemic (Gonçalves et al., 2020; Rehm et al., 2020). As alcohol-specific deaths are the result of heavy drinking, this could explain our finding of increased mortality. Further investigations are necessary to test this mechanism.
The analyses presented are limited by multiple factors. First, causes of death may contain biases (Neuilly, 2022) and country differences may reflect regional variations in coding practices (for limitations inherent to coding alcohol-specific deaths, see Sherk et al., 2022). However, there is no obvious reason how these biases could explain our specific results on within-country trends. Second, data on the socioeconomic disparities in alcohol-specific mortality were not available. It is plausible that a disproportionate share of the excess deaths occurred among individuals with lower socioeconomic status, who generally experience higher rates of alcohol harm (Probst et al., 2021) and COVID-19 related deaths (Riou et al., 2021; Wachtler et al., 2020). Third, smoking may be an unmeasured confounder for our results, as smoking rates increased during COVID-19 (Manthey et al., 2021) and liver cirrhosis deaths wholly attributable to alcohol – in many countries the largest alcohol-specific category – may have been affected by smoking and the interaction between smoking and alcohol (Liu et al., 2008). Forth, trends in recorded per capita consumption may have been compensated by contrary trends in unrecorded consumption. However, many categories of unrecorded alcohol (e. g., cross-border shopping, or smuggling; Lachenmeier et al., 2021) were impeded by COVID-19 measures (Leifman et al., 2022). Thus, other categories (e. g., home-produced alcohol; surrogate alcohol) needed to increase in a way to fully compensate the decreases in major categories for unrecorded alcohol in Europe. Finally, alcohol consumption by tourists plays an important role in some countries (e. g., Spain), and decreases in alcohol sales may be in part due to the discontinuation of tourism during periods of lockdowns and border closures.
Moreover, it remains unclear to what extent impairments and between-country differences in addiction-related healthcare services contributed to the observed increases in alcohol-specific mortality in different countries. A German study suggests a notable disruption of these services in 2020 (Manthey et al., 2023) and a French study showed discrimination against people with alcohol use disorders in hospital care during COVID-19 (Schwarzinger et al., 2023). Our findings yield further support for this mechanism, as in countries with fewer restrictions and thus potentially less severe constraints on healthcare, alcohol-specific mortality did only marginally change (e. g., Denmark and Finland, which were among the few European countries without lockdowns in 2020, Hale et al., 2021).
Conclusion
Alcohol-specific mortality increased during the COVID-19 pandemic in Europe, with some variation between countries and despite stagnant or declining alcohol sales. The reasons for this increase need to be further explored, focusing on vulnerable populations such as socioeconomically disadvantaged groups in particular, and alcohol control policies adapted.
Funding
This publication is based on the project “Patient Routes of People with Alcohol Use Disorder in Germany” (PRAGMA) which was funded by the Innovation Committee of the Federal Joint Committee (Gemeinsamer Bundesausschuss, GBA) under the funding code 01VSF21029. JRs participation in this study has been supported by a grant from of the National Institute on Alcohol Abuse and Alcoholism of the National Institutes of Health (NIAAA) [1R01AA028224], as part of the project ‘Evaluation of the impact of alcohol control policies on morbidity and mortality in Lithuania and other Baltic states’. Both funding bodies were not involved in the study design, collection, analysis, interpretation of data or preparation of this publication. Open access publication enabled by Staats- und Universitätsbibliothek Hamburg.
Footnotes
Declaration of Competing Interests
Jakob Manthey and Carolin Kilian worked as consultants for health organisations. None of the authors have any connections to the (alcohol) industry: no shareholdings, patents, consulting activities or similar. For the other authors there are no conflicts of interest.
References
- Acuff SF, Strickland JC, Tucker JA, & Murphy JG (2021). Changes in alcohol use during COVID-19 and associations with contextual and individual difference variables: A systematic review and meta-analysis. Psychology of Addictive Behaviors, 36(1), 1–19. 10.1037/adb0000796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson P, O’Donnell A, Jané Llopis E, & Kaner E (2022). The COVID-19 alcohol paradox: British household purchases during 2020 compared with 2015–2019. PLOS ONE, 17(1), Article e0261609. 10.1371/journal.pone.0261609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angus C, Buckley C, Tilstra AM, & Dowd JB (2023). Increases in ‘deaths of despair’ during the COVID-19 pandemic in the USA and UK. Public Health, 218, 92–96. 10.1016/j.puhe.2023.02.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Goeij MCM, Suhrcke M, Toffolutti V, Van de Mheen D, Schoenmakers TM, & Kunst AE (2015). How economic crises affect alcohol consumption and alcohol-related health problems: A realist systematic review. Social Science & Medicine, 131, 131–146. 10.1016/j.socscimed.2015.02.025 [DOI] [PubMed] [Google Scholar]
- European Commission, Eurostat, Pace M, Gissler M, & Lanzieri G (2013). Revision of the European Standard Population: Report of Eurostat’s task force (2013 edition). Publications Office. https://data.europa.eu/doi/10.2785/11470 [Google Scholar]
- GBD 2019 Risk Factors Collaborators. (2020). Global burden of 87 risk factors in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. The Lancet, 396(10258), 1223–1249. 10.1016/S0140-6736(20)30752-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonçalves PD, Moura HF, Do Amaral RA, Castaldelli-Maia JM, & Malbergier A (2020). Alcohol use and COVID-19: Can we predict the impact of the pandemic on alcohol use based on the previous crises in the 21st century? A brief review. Frontiers in Psychiatry, 11, Article 581113. 10.3389/fpsyt.2020.581113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale T, Angrist N, Goldszmidt R, Kira B, Petherick A, Phillips T, Webster S, Cameron-Blake E, Hallas L, Majumdar S, & Tatlow H (2021). A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker). Nature Human Behaviour, 5, 529–538. https://www.bsg.ox.ac.uk/research/research-projects/covid-19-government-response-tracker [DOI] [PubMed] [Google Scholar]
- Kilian C, Carr S, Schulte B, & Manthey J (2022). Increased alcohol-specific mortality in Germany during COVID-19: State-level trends from 2010 to 2020. Drug and Alcohol Review, 42(3), 633–640. 10.1111/dar.13573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilian C, O’Donnell A, Potapova N, López-Pelayo H, Schulte B, Miquel L, Castillo BP, Schmidt CS, Gual A, Rehm J, & Manthey J (2022). Changes in alcohol use during the COVID-19 pandemic in Europe: A meta-analysis of observational studies. Drug and Alcohol Review, 41(4), 918–1931. 10.1111/dar.13446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachenmeier DW, Neufeld M, & Rehm J (2021). The impact of unrecorded alcohol use on health: What do we know in 2020? Journal of Studies on Alcohol and Drugs, 82(1), 28–41. 10.15288/jsad.2021.82.28 [DOI] [PubMed] [Google Scholar]
- Leifman H, Dramstad K, & Juslin E (2022). Alcohol consumption and closed borders – How COVID-19 restrictions have impacted alcohol sales and consumption in Europe. BMC Public Health, 22(1), Article 692. 10.1186/s12889-022-13014-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu B, Balkwill A, Roddam A, Brown A, & Beral V (2008). Separate and Joint Effects of Alcohol and Smoking on the Risks of Cirrhosis and Gallbladder Disease in Middle-aged Women. American Journal of Epidemiology, 169(2), 153–160. 10.1093/aje/kwn280 [DOI] [PubMed] [Google Scholar]
- Mäkelä P, Rossow I, Moan IS, Bye e. K., Kilian C, Raitasalo K, & Allebeck P (2021). Measuring changes in alcohol use in Finland and Norway during the COVID-19 pandemic: Comparison between data sources. International Journal of Methods in Psychiatric Research, 30(4), Article e1892. 10.1002/mpr.1892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manthey J, Kilian C, Carr S, Barták M, Bloomfield K, Braddick F, Gual A, Neufeld M, O’Donnell A, Petruželka B, Rogalewicz V, Rossow I, Schulte B, & Rehm J (2021). Use of alcohol, tobacco, cannabis, and other substances during the first wave of the SARS-CoV-2 pandemic in Europe: A survey on 36,000 European substance users. Substance Abuse Treatment, Prevention, and Policy, 16, Article 36. 10.1186/s13011-021-00373-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manthey J, & Kilian C (2023). Changes in alcohol-specific mortality during the COVID-19 pandemic in 14 European countries – Data and R code (Version 3). figshare. 10.6084/m9.figshare.22566877.v3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manthey J, Kilian C, Schäfer I, Wirth M, & Schulte B (2023). Changes in the alcohol-specific disease burden during the COVID-19 pandemic in Germany: Interrupted time series analyses. European Journal of Public Health, 33 (4), 645–652. 10.1093/eurpub/ckad103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manthey J, Shield K, Rylett M, Hasan O, Probst C, & Rehm J (2019). Alcohol exposure between 1990 and 2017 and forecasts until 2030: A global modelling study. The Lancet, 393(10190), 2493–2502. 10.1016/S0140-6736(18)32744-2 [DOI] [PubMed] [Google Scholar]
- Neuilly M (2022). Sources of bias in death determination: A research note articulating the need to include systemic sources of biases along with cognitive ones as impacting mortality data. Journal of Forensic Sciences, 67(5), 2032–2039. 10.1111/1556-4029.15080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Probst C, Lange S, Kilian C, Saul C, & Rehm J (2021). The dose-response relationship between socioeconomic deprivation and alcohol-attributable mortality risk – A systematic review and meta-analysis. BMC Medicine, 19(1), Article 268. 10.1186/s12916-021-02132-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Probst C, Manthey J, Neufeld M, Rehm J, Breda J, Rakovac I, & Ferreira-Borges C (2020). Meeting the global NCD target of at least 10 % relative reduction in the harmful use of alcohol: Is the WHO European Region on track? International Journal of Environmental Research and Public Health, 17(10), Article 3423. 10.3390/ijerph17103423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team. (2023). R: A language and environment for statistical computing. (4.2.3) [Software]. R Foundation for Statistical Computing. https://www.R-project.org/ [Google Scholar]
- Rehm J, Kilian C, Ferreira-Borges C, Jernigan D, Monteiro M, Parry C. D. h., Sanchez ZM, & Manthey J (2020). Alcohol use in times of the COVID 19: Implications for monitoring and policy. Drug and Alcohol Review, 39(4), 301–304. 10.1111/dar.13074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riou J, Panczak R, Althaus CL, Junker C, Perisa D, Schneider K, Criscuolo NG, Low N, & Egger M (2021). Socioeconomic position and the COVID-19 care cascade from testing to mortality in Switzerland: A population-based analysis. The Lancet Public Health, 6(9), e683–e691. 10.1016/S2468-2667(21)00160-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossow I, Bartak M, Bloomfield K, Braddick F, Bye e. K., Kilian C, López-Pelayo H, Mäkelä P, Moan IS, Moskalewicz J, Petruzelka B, Rogalewicz V, & Manthey J (2021). Changes in Alcohol Consumption during the COVID-19 Pandemic Are Dependent on Initial Consumption Level: Findings from Eight European Countries. International Journal of Environmental Research and Public Health, 18(19), Article 10547. 10.3390/ijerph181910547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders JB, Degenhardt L, Reed GM, & Poznyak V (2019). Alcohol Use Disorders in ICD-11: Past, Present, and Future. Alcoholism: Clinical and Experimental Research, 43(8), 1617–1631. 10.1111/acer.14128 [DOI] [PubMed] [Google Scholar]
- Schmidt RA, Genois R, Jin J, Vigo D, Rehm J, & Rush B (2021). The early impact of COVID-19 on the incidence, prevalence, and severity of alcohol use and other drugs: A systematic review. Drug and Alcohol Dependence, 228, Article 109065. 10.1016/j.drugalcdep.2021.109065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarzinger M, Luchini S, Teschl M, Alla F, Mallet V, & Rehm J (2023). Mental disorders, COVID-19-related life-saving measures and mortality in France: A nationwide cohort study. PLOS Medicine, 20(2), Article e1004134. 10.1371/journal.pmed.1004134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherk A, Esser MB, Stockwell T, & Naimi TS (2022). Estimating alcohol-attributable liver disease mortality: A comparison of methods. Drug and Alcohol Review, 41(5), 1245–1253. 10.1111/dar.13470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shield KD, Manthey J, Rylett M, Probst C, Wettlaufer A, Parry C. D. h., & Rehm J (2020). National, regional, and global burdens of disease from 2000 to 2016 attributable to alcohol use: A comparative risk assessment study. The Lancet Public Health, 5(1), e51–e61. 10.1016/S2468-2667(19)30231-2 [DOI] [PubMed] [Google Scholar]
- United Nations, Department of Economic and Social Affairs, Population Division. (2022). World Population Prospects 2022, online edition [Data set]. United Nations. https://population.un.org/wpp/Download/Standard/Population/ [Google Scholar]
- Wachtler B, Michalski N, Nowossadeck E, Diercke M, Wahrendorf M, Santos-Hövener C, Lampert T, & Hoebel J (2020). Sozioökonomische Ungleichheit und COVID-19 – Eine Übersicht über den internationalen Forschungsstand. Journal of Health Monitoring, 5(S7) 3–18. 10.25646/7058 [DOI] [Google Scholar]
- World Health Organization. (2023a). WHO Mortality Database. World Health Organization. Retrieved March 28, 2023 from https://www.who.int/data/data-collection-tools/who-mortality-database [Google Scholar]
- World Health Organization. (2023b). Recorded alcohol per capita consumption (Unpublished data).


