Abstract
Background and study aims Endoscopic full-thickness resection (eFTR) allows treatment of “difficult to resect” lesions not amenable to conventional endoscopic methods. Efficacy and safety of the system have already been proven in numerous studies. Follow-up data on outcome of colorectal eFTR and management of recurrences are still rare.
Patients and methods All patients undergoing colorectal eFTR at our institution with at least one endoscopic follow-up examination were retrospectively analyzed. The primary endpoint was the rate of recurrent or residual lesions (RRLs) and the secondary endpoint was the rate of late adverse events (AEs). We further aimed to identify risk factors for RRLs and to describe their management.
Results Between November 2014 and 2021, 141 patients underwent eFTR at University Medical Center Freiburg. Ninety-one patients fulfilled the inclusion criteria. Indications for eFTR were non-lifting adenoma (n = 65), subepithelial tumors (n = 18) and early carcinoma (n = 8). The median follow-up period was 17 months (range, 2–86). The overall RRL rate was 9.9% (9/91). A significant proportion of RRLs (6/9, 66%) were detected late. All RRLs occurred in the group of non-lifting adenoma, corresponding to a RRL rate of 13.8% in this subgroup. Thirty-three percent (3/9) were initially treated by hybrid eFTR. Of the RRLs, 66.6% could were successfully treated endoscopically. On χ2 analysis, the hybrid eFTR technique ( P = 0.006) was associated with a higher rate of RRL. No late AEs occurred.
Conclusions The rate of RRL after colorectal eFTR is low and the majority could be treated endoscopically. For non-lifting adenomas and early carcinomas, close follow-up is mandatory to detect late recurrence. Long-term outcomes after hybrid eFTR need further investigation.
Keywords: Endoscopy Lower GI Tract; Polyps / adenomas / ...; Endoscopic resection (polypectomy, ESD, EMRc, ...); Colorectal cancer
Introduction
Endoscopic full-thickness resection (eFTR) facilitates resection of lesions not amenable to conventional endoscopic methods. The full-thickness resection device (FTRD, Ovesco Endoscopy, Tuebingen Germany) was introduced in 2014 and is currently the only approved device for eFTR. The device is used for various “difficult-to-resect” lesions in the colorectum, all non-lifting (mainly recurrent) adenomas. Other indications include subepithelial tumors (SETs) such as neuroendocrine tumors (NETs), early carcinomas (treatment naïve or re-resection), and adenomas at difficult anatomic locations. Efficacy and safety of the system have already been proven in numerous studies 1 2 3 . Follow-up data on recurrence rates and adverse events (AEs) are still rare. This study addresses this issue and reports the results of a retrospective evaluation of 91 colorectal FTRD interventions between 2011 and 2021 at University Medical Center Freiburg.
Patients and methods
The study was approved by the ethical review board (Ethics Committee of Albert-Ludwigs university Freiburg, 22.06.2023, request number: 23–1279-S1-retro). The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki.
Data sources and inclusion/exclusion criteria
In this single-center, retrospective study, 141 consecutive patients who had undergone colorectal eFTR at the University Medical Center Freiburg between November 2014 and November 2021 were screened.
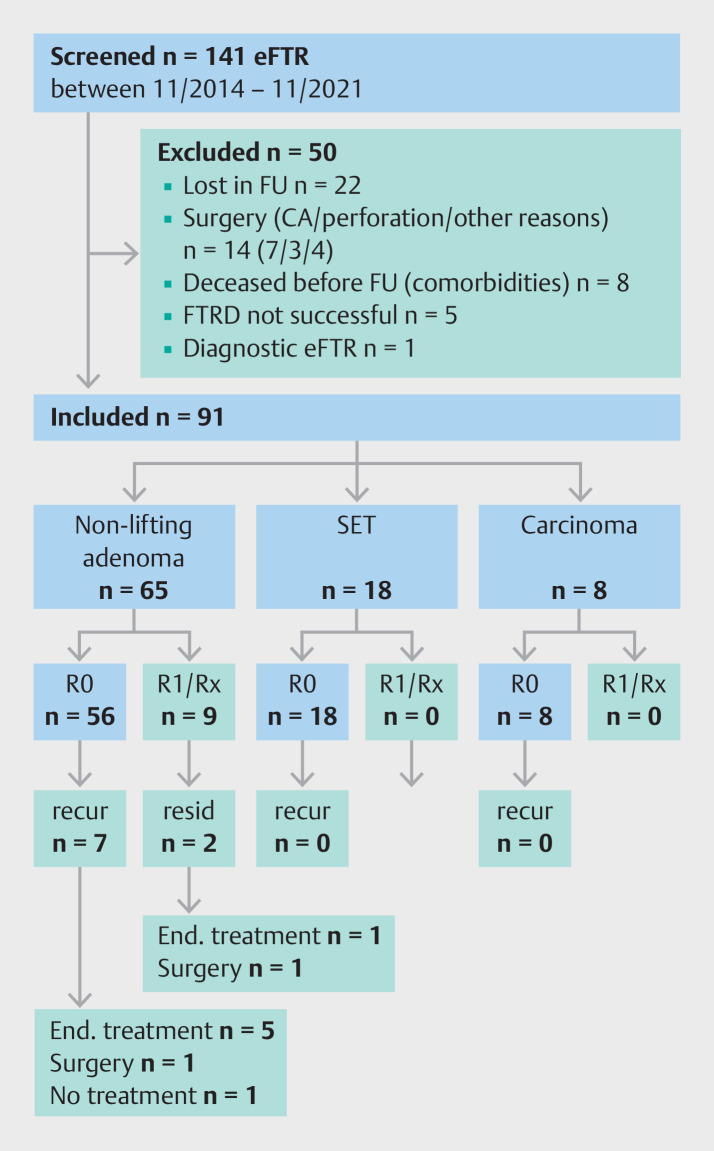
All patients who underwent at least one follow-up colonoscopy were included. We excluded patients who underwent colorectal surgery after eFTR, cases of unsuccessful initial eFTR, and patients who had undergone eFTR for diagnostic purposes ( Fig. 1 ).
Fig. 1.
Flow chart of the patient collective. CA, adenocarcinoma; eFTR, endoscopic full-thickness resection; end treatment, endoscopic treatment; FTRD, full-thickness resection device; FU, follow-up; recur, recurrent lesion; resid, residual lesion; SET, subepithelial tumor.
Endpoints
The primary endpoint of the study was the rate of recurrent and residual lesions on follow-up examination. Lesions were defined as recurrent when initial resection was histologically complete (R0); in case of an initial R1 or Rx resection, the lesion was defined as residual. The secondary endpoint was occurrence of late complications (> 1 month) after eFTR. In addition, risk factors for RRL were identified and further management of RRL was investigated.
Statistical analysis
Continuous variables are reported as median with range whereas categorical variables are expressed as frequencies and percentages unless stated otherwise. For categorical variables, differences were determined using χ 2 or Fisher’s Exact tests as appropriate. P < 0.05 was considered significant. Data collection and analysis were performed with Microsoft Excel 2016 for Mac Os (version 15.21) (Microsoft, Redmond, Washington, United States) and IBM SPSS Statistics for Microsoft (Version 29.0.0.0 (241), IBM, Armonk, New York, United States).
Results
Patient characteristics and procedure data
Entire cohort
Mean age of the cohort at the time of eFTR intervention was 63 years (± 12), with a 40:60 female-to-male ratio. Lesions were distributed throughout the entire colorectum. Median lesion size was 21 mm (range, 8–60) (endoscopic assessment). In 8.8% (8/91), a hybrid procedure (endoscopic mucosal resection [EMR] followed by eFTR) was performed (median lesion size 28 mm, range 20–60). In the other cases (91.2%), lesions were resected by pure eFTR using the FTRD (median lesion size 21 mm, range 8–35).
The R0 resection rate was 88% (80/91) and the full-thickness resection rate was 81.3% (74/91). Table 1 provides an overview including subgroups of indications.
Table 1 Overview of FTRD interventions with subdivision according to indication.
|
Overall
(n = 91) |
Non-lifting adenoma
(n = 65) |
SET
(n = 18) |
Carcinoma
(n = 8) |
|
| eFTR, endoscopic full-thickness resection; FTRD, full-thickness resection device; FU, follow-up; RRL, recurrent/residual lesion; SD, standard deviation; SET, subepithelial tumor. | ||||
| Age years (SD) | 63 (12) | 67 (12) | 53 (12) | 62 (12) |
| Sex, n (%) | ||||
|
36 (40) | 25 (38) | 9 (50) | 2 (25) |
|
55 (60) | 40 (62) | 9 (50) | 6 (75) |
| Localization, n (%) | ||||
|
15 (16) | 13 (20) | 1 (5.6) | 1 (12.5) |
|
19 (21) | 18 (27.7) | 0 | 1 (12.5) |
|
12 (13) | 8 (12.3) | 3 (16.6) | 1 (12.5) |
|
4 (4) | 4 (6.1) | 0 | 0 |
|
15 (16) | 12 (18.5) | 2 (11.1) | 1 (12.5) |
|
26 (29) | 10 (15.4) | 12 (66.7) | 4 (50) |
| Initial lesion size (average, SD mm) | 21 (8–60) | 22 (8–60) | 20 (9–26) | 24 (8–33) |
| Initial lesion size pure eFTR | 21 (8–35) | 21 (8–35) | 20 (9–26) | 24 (8–33) |
| Initial lesion size hybrid eFTR | 28 (20–60) | 28 (20–60) | – | – |
| Hybrid EFTR, n (%) | 8 (8.8) | 8 (12.3) | 0 | 0 |
| Full-thickness resection, n (%) | 74 (81.3) | 53 (81.5) | 16 (88.9) | 5 (62.5) |
| R0 resection, n (%) | 80 (87.9) | 54 (83.1) | 18 (100) | 8 (100) |
| Follow-up | 0 | 0 | ||
|
9 (9.9) | 9 (13.8) | ||
| without hybrid eFTR | 6 (7.2) | 6 (10,5) | ||
|
15.5 (2–50) | 15.5 (2–50) | – | – |
|
2 (1–6) | 2 (1–5) | 2 (1–6) | 2 (1–4) |
|
4.3 (1–57) | 4.3 (2–46) | 4.2 (1–57) | 3.9 (2–42) |
|
16.8 (2–86) | 16.7 (2–83) | 16.8 (3–86) | 19.5 (4–42) |
|
15 (17) vs. 76 (83) | 11 (17) vs. 54 (83) | 4 (22) vs. 14 (78) | 0 vs. 8 (100) |
Non-lifting adenoma subgroup
The non-lifting sign was defined by insufficient submucosal injectability, whereby the causes of non-lifting were not differentiated. The group of non-lifting adenomas (n = 65) included 18 treatment-naïve (28%) and 47 pretreated lesions (72%). Most of the pretreated lesions were recurrent adenomas (n = 33, 70%) and a minority were residual lesions after incomplete resection (n=14, 30%).
Lesions were distributed over the entire colorectum. The R0 resection rate was 83% (54/65). All hybrid eFTR procedures (n = 8) were performed in this group.
SET subgroup
The cohort included 18 subepithelial tumors with a median size of 20 mm (range 9–26). The majority of lesions were NETs (n = 15) and other histologies included one gastrointestinal stromal tumor, one granular cell tumor, and one leiomyoma. Most SETs were located in the rectum or sigmoid (n = 14, 78%). The overall R0 resection rate was 100% (18/18).
Adenocarcinoma subgroup
The group with biopsy-proven adenocarcinoma had not been pretreated before eFTR in terms of an attempt at resection; biopsy was just to confirm the diagnosis of malignancy. In contrast, the pretreated adenocarcinomas had already undergone endoscopic treatment. Included in this subgroup were three (38%) untreated biopsy-proven early carcinomas and five (63%) endoscopically pretreated carcinomas. All included cases could be resected completely (R0). The majority of findings (n = 5, 63%) were located in the rectum or sigmoid colon.
Adverse events
In total, three procedure-related AEs occurred (3.3%). These were exclusively early bleeds after an average of 1.5 days post eFTR, all of which were successfully treated endoscopically, and therefore, considered moderate AEs. No late AEs occurred.
Follow-up
In the entire cohort, the first endoscopic follow-up examination was performed after a median period of 4 months (range, 1–57). At that time, 76% of clips (n = 83) had already been detached spontaneously. Overall, a median of two follow-up examinations (range, 1–6) were recorded, covering a total median period of 17 months (range, 2–86).
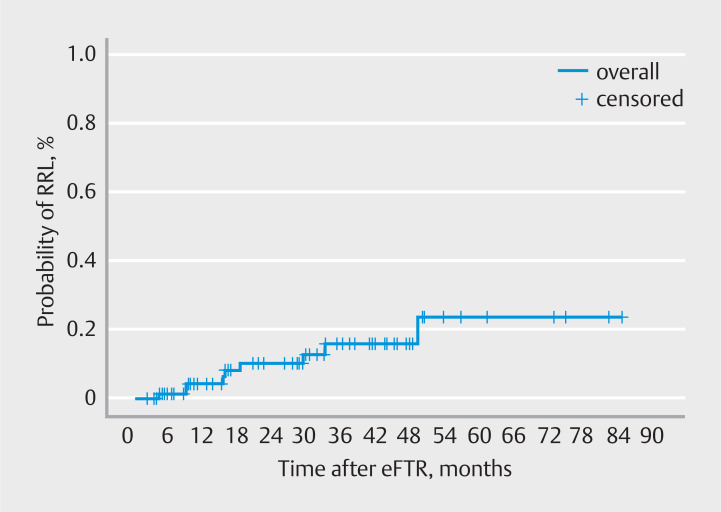
During the total follow-up period, the rate of recurrent and residual lesions was 7.8% (n = 7) and 2.2% (n = 2) after a median follow-up period of 15.5 months (range, 2–55). Fig. 2 illustrates the probability of recurrent/residual lesions (RRLs) in an event-time analysis. One of these findings occurred early (after 4 months) and eight late (after a median period of 24 months). In five of nine cases (55.6 %) of recurrent or residual lesions, the first follow-up examination after an average of 3.5 months revealed no abnormalities.
Fig. 2.
Event-time analysis (probability of recurrent/residual lesion).
Recurrent (4/5) or residual lesions (1/5) were detected after a median period of 24.8 months. All recurrent/residual findings occurred in the non-lifting adenoma group, corresponding to a rate of 10.7% and 3.1% in this subgroup ( Table 1 ).
In the subgroups of SETs and adenocarcinoma, no recurrent or residual findings were recorded. The adenocarcinoma subgroup also included two high-risk findings with deep submucosal infiltration (sm3) and one case of muscular infiltration (T2). Nevertheless, in the presence of concomitant disease, surgical treatment was not performed, and so far, there has been no evidence of recurrence after eFTR.
Management of recurrent/residual lesions
Most RRLs were successfully treated endoscopically (n = 6, 66.6%; 5 EMR, 1 forceps polypectomy) without further evidence of RRL. Two patients (22.2%) required surgical treatment and one patient died of comorbidities before further therapy could be initiated.
Risk factors for recurrent/residual lesions
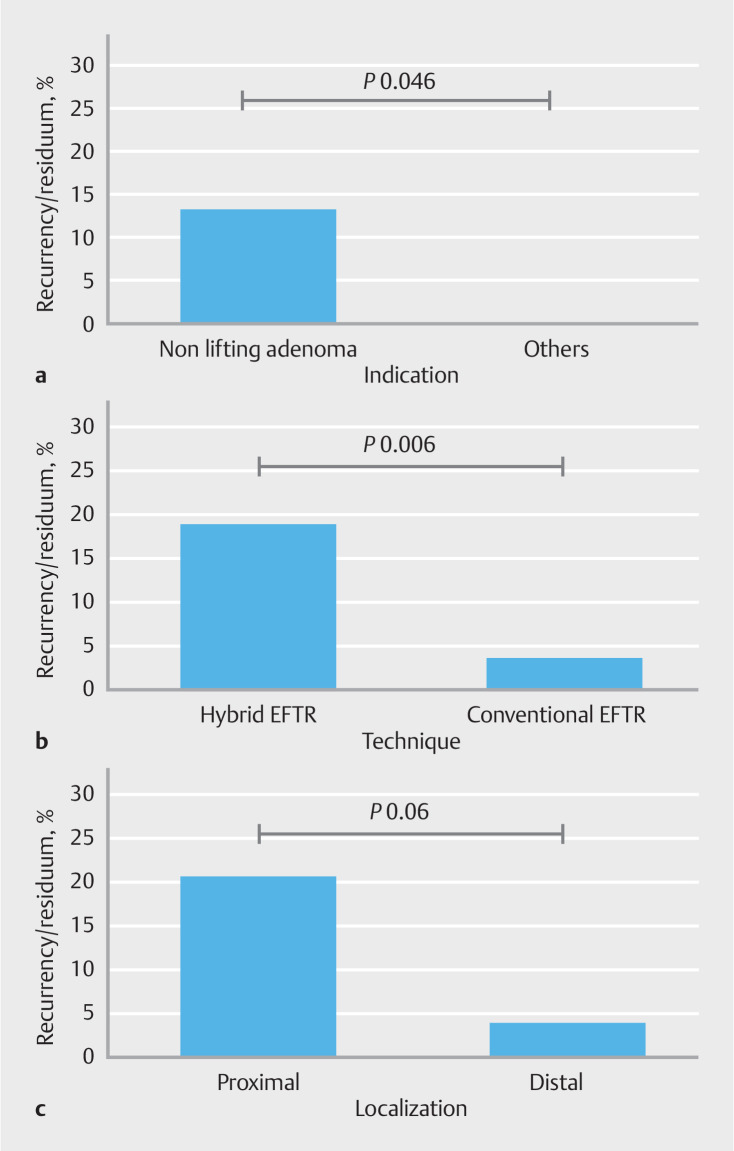
We calculated risk factors for RRLs. The results are shown in Table 2 and Fig. 3 . The rate of RRLs was significantly higher in the group with non-lifting adenoma than in the group with other indications ( P = 0.046). Moreover, there was a significant correlation between use of hybrid eFTR (combination of conventional EMR and FTRD and recurrent/residual findings [ P = 0.006]).
Table 2 Risk factors for occurrence of residual/recurrent finding with corresponding P values.
| Factor | Rate of recurrence/residual lesions, n (%) | P value |
| eFTR, endoscopic full-thickness resection. | ||
|
Indication (A)
Non-lifting adenoma vs. others |
9/65 ( 13.9 ) vs. 0/36 ( 0 ) | 0.046 |
|
Localization (B)
Cecum + ascending colon vs. others |
7/34 ( 20.6 ) vs. 2/57 ( 3.5 ) | 0.06 |
|
Technique (C)
Hybrid eFTR vs. Conventional eFTR |
3/8 ( 37.5 ) vs. 6/83 ( 7.2 ) | 0.006 |
Fig. 3.
Risk factors for occurrence of a residual/recurrent finding. a Indication. b localization. c Technique with corresponding P values.
There was a trend toward an association between proximal localization of lesions (cecum and ascending colon) and occurrence of residual/recurrent findings ( P = 0.06). Lesion size was not found to be an independent risk factor for RRL in our study.
Discussion
In the current study, we report long-term outcomes after eFTR in the colorectum for various indications . Overall, a 9.9% rate of RRLs was observed during a median follow-up of 17 months (range, 2–86). Comparable long-term data on colorectal eFTR use are not yet available, but shorter follow-up periods have already been analyzed in several studies. In the prospective Wall resect study (n = 181), 12.3% of patients (19) had a recurrent or residual lesion after a follow-up period of 3 months 3 . All of them were in the subgroup with difficult adenomas, comparable to our study. In the German FTRD registry, 1178 FTRD procedures were analyzed and follow-up was available in 683 cases after a median follow-up period of just 14 weeks 1 . RRLs occurred in 13.5% of the 683 cases. In the Dutch FTRD registry (n = 367), follow-up examinations of 187 patients (63.4%) could be evaluated after an average of 4 months. The recurrence rate was as low as 6.4 % 2 . This study included significantly more pretreated cases of adenomas and carcinomas. Accordingly, median lesion size was significantly smaller than in our study (10 mm; range, 8–15 mm vs. 21 mm; range, 8–60), which, in addition to the shorter follow-up period, could be a reason for the low RRL rate. In our study, only one early recurrent lesion occurred at 4 months; all other cases of RRL had at least one follow-up examination without evidence of RRL (after an average of 7 months [range, 2–29] up to approximately 20 months [range, 9–49]).
In summary, RRL was detected later than in the aforementioned studies, indicating the importance of close long-term follow-up. Regarding further management of patients, the majority could be successfully treated endoscopically. This finding is consistent with the previously mentioned studies 1 2 3 .
Non-lifting adenoma subgroup
As mentioned previously, recurrences and residual findings in our cohort occurred only in the group with non-lifting adenoma; the RRL rate was 13.8% (9/65). Recurrences after piecemeal EMR are reported to occur in approximately 20% of patients 4 . A direct comparison with eFTR is difficult due to the difference in indications. While eFTR in our cohort was mainly applied for non-lifting pretreated lesions, EMR is primarily used for treatment-naïve adenomas 5 . For recurrent non-lifting lesions, EMR has successfully been combined with avulsion and/or with thermal ablation 6 7 . The reported recurrence rates in those studies were similar to our findings. Compared with those techniques, eFTR has the advantage that histological assessment of the eFTR specimen is likely to be more exact, especially for lesions with advanced histology.
A randomized controlled study comparing eFTR with EMR plus avulsion currently is recruiting, but results are not yet available (CURE study, DRKS 1200023539d).
Endoscopic submucosal dissection (ESD) allows en bloc resection of larger lesions and the rate of local recurrence is between 0.8% and 2% 8 9 10 . Slightly lower R0 resection rates are achieved in Germany; a comparable recurrence rate (2.1%) was reported cumulatively in a large multicenter evaluation of 1000 ESD interventions at different locations in the gastrointestinal tract 11 . However, only 24 of 290 (8%) and 70 of 1000 lesions (7%) in these studies had already been pretreated and scarred, respectively, whereas in our cohort, 70 of 91 (77%) had been previously treated. Non-lifting lesions make ESD resection considerably more difficult, especially in the colon, so recurrence rates are not directly comparable.
There was a trend toward an association between proximal location of lesions (cecum, ascending colon) and occurrence of RRLs ( P = 0.06). The endoscopic view is impeded by deposits of mucus and stool impurities when the cap is charged during endoscope advancement. In addition, maneuverability is limited in the proximal portions of the bowel. As a consequence, the target lesion may not have been localized correctly or resected completely. Other studies do not confirm this connection 1 12 .
Moreover, there was a significant correlation between use of hybrid eFTR and recurrent or residual findings ( P = 0.006). A corrected overall recurrence rate of 7.2% (6 of 83) results if the hybrid interventions are not taken into account in our study.
However, the generalizability of this result is questionable due to the small number of hybrid cases (n = 8) in our study. In addition, lesions resected using the hybrid technique were significantly larger in median size than conventionally resected lesions (28 mm; range, 20–60 vs. 21 mm; range, 8–35; P = 0.001). Due to the size of the cap, clinical use of the FTRD system is limited to lesions with a maximum diameter of about 30 mm 1 . With the introduction of thermal ablation techniques for mucosal resection, margin recurrence rates of 5% are reported for EMR 13 14 , with the piecemeal technique being shown to be an independent risk factor for recurrence 15 . The combination of both techniques might also be associated with increased rates of RRLs. It is difficult to distinguish whether RRL occurred in the area of EMR or FTRD resection retrospectively. Mahadev et al. described satisfactory R0 resection (81) and technical success rates (83) comparing hybrid eFTR and standalone eFTR 16 . However, follow-up analysis was not performed in this study. Bauermeister et al. analyzed 12 patients undergoing follow-up after hybrid eFTR. The recurrence rate was 16.6% despite approved previous margin-free resection 17 . In a recently published study, 75 patients with non-lifting colorectal adenomas were included. Mean lesion size was 36.5 mm (range, 25–60). The technical success rate was 100% with macroscopic complete resection in 97.3%. Endoscopic follow-up was available in 93.3% (mean follow-up time, 8.1 months; range, 3–36) and the RRL rate was 11.4% 18 . In relation to the studies mentioned previously, our RRL rate in the hybrid eFTR subgroup is somewhat higher. Larger series with longer follow-up periods are needed to address this issue.
Studies have already shown a correlation between detection of high-grade dysplasia in lesions (among lesion size, periprocedure bleeding) and increased probability of recurrent/residual findings 4 . We could not confirm these findings in our study.
SET subgroup
Subepithelial tumors are well suited to endoscopic full-thickness resection. High rates of R0 resections without recurrences have already been documented in numerous studies 1 2 3 . Meier et al. showed a 100% R0 resection rate for 40 colorectal NETs 19 . In our study, there were no recurrent or residual lesions in this subgroup, underscoring the relevance of the technique for this indication.
Our study has certain limitations: Due to the retrospective evaluation, some data such as information on pretreatment or histological results before the FTRD intervention were missing. In 22 cases, no follow-up data could be evaluated.
The number and timing of follow-up investigations varied widely between cases, making comparisons difficult. In particular, patients with malignant diseases (adenocarcinoma/NET) received more consistent follow-up examinations, which entails a certain selection bias. Prospective studies with an established follow-up protocol are needed.
Conclusions
In summary, our study demonstrates that the rate of RRLs after colorectal eFTR is low and that most recurrences can be treated endoscopically. While there were no recurrences in the group with SETs, close follow-up is mandatory after resection of epithelial lesions to detect late recurrences. Further investigation is needed regarding long-term outcomes after hybrid eFTR.
Footnotes
Conflict of Interest Arthur Schmidt and Armin Kuellmer have received lecture fees and study grants from Ovesco Endoscopy AG, Tuebingen, Germany and are consultants for KLS Martin, Tuttlingen, Germany. The rest of the authors have no conflicts of interest to declare.
References
- 1.Meier B, Stritzke B, Kuellmer A et al. Efficacy and safety of endoscopic full-thickness resection in the colorectum: Results from the German Colonic FTRD Registry. Am J Gastroenterol. 2020;115:1998–2006. doi: 10.14309/ajg.0000000000000795. [DOI] [PubMed] [Google Scholar]
- 2.Zwager LW, Bastiaansen BAJ, Bronzwaer MES et al. Endoscopic full-thickness resection (eFTR) of colorectal lesions: results from the Dutch colorectal eFTR registry. Endoscopy. 2020;52:1014–1023. doi: 10.1055/a-1176-1107. [DOI] [PubMed] [Google Scholar]
- 3.Schmidt A, Beyna T, Schumacher B et al. Colonoscopic full-thickness resection using an over-the-scope device: a prospective multicentre study in various indications. Gut. 2018;67:1280–1289. doi: 10.1136/gutjnl-2016-313677. [DOI] [PubMed] [Google Scholar]
- 4.Tate DJ, Desomer L, Klein A et al. Adenoma recurrence after piecemeal colonic EMR is predictable: the Sydney EMR recurrence tool. Gastrointest Endosc. 2017;85:647–6.56E8. doi: 10.1016/j.gie.2016.11.027. [DOI] [PubMed] [Google Scholar]
- 5.Holmes I, Friedland S. Endoscopic mucosal resection versus endoscopic submucosal dissection for large polyps: A @estern colonoscopist’s view. Clin Endosc. 2016;49:454–456. doi: 10.5946/ce.2016.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tate DJ, Bahin FF, Desomer L et al. Cold-forceps avulsion with adjuvant snare-tip soft coagulation (CAST) is an effective and safe strategy for the management of non-lifting large laterally spreading colonic lesions. Endoscopy. 2018;50:52–62. doi: 10.1055/s-0043-119215. [DOI] [PubMed] [Google Scholar]
- 7.Holmes I, Kim HG, Yang D-H et al. Avulsion is superior to argon plasma coagulation for treatment of visible residual neoplasia during EMR of colorectal polyps (with videos) Gastrointest Endosc. 2016;84:822–829. doi: 10.1016/j.gie.2016.03.1512. [DOI] [PubMed] [Google Scholar]
- 8.Lee E-J, Lee JB, Lee SH et al. Endoscopic treatment of large colorectal tumors: comparison of endoscopic mucosal resection, endoscopic mucosal resection-precutting, and endoscopic submucosal dissection. Surg Endosc. 2012;26:2220–2230. doi: 10.1007/s00464-012-2164-0. [DOI] [PubMed] [Google Scholar]
- 9.Tajika M, Niwa Y, Bhatia V et al. Comparison of endoscopic submucosal dissection and endoscopic mucosal resection for large colorectal tumors. Eur J Gastroenterol Hepatol. 2011;23:1042–1049. doi: 10.1097/MEG.0b013e32834aa47b. [DOI] [PubMed] [Google Scholar]
- 10.Saito Y, Fukuzawa M, Matsuda T et al. Clinical outcome of endoscopic submucosal dissection versus endoscopic mucosal resection of large colorectal tumors as determined by curative resection. Surg Endosc. 2010;24:343–352. doi: 10.1007/s00464-009-0562-8. [DOI] [PubMed] [Google Scholar]
- 11.Fleischmann C, Probst A, Ebigbo A et al. Endoscopic submucosal dissection in europe: results of 1000 neoplastic lesions from the German Endoscopic Submucosal Dissection Registry. Gastroenterology. 2021;161:1168–1178. doi: 10.1053/j.gastro.2021.06.049. [DOI] [PubMed] [Google Scholar]
- 12.Kuellmer A, Mueller J, Caca K et al. Endoscopic full-thickness resection for early colorectal cancer. Gastrointest Endosc. 2019;89:1180–11890. doi: 10.1016/j.gie.2018.12.025. [DOI] [PubMed] [Google Scholar]
- 13.Klein A, Tate DJ, Jayasekeran V et al. Thermal ablation of mucosal defect margins reduces adenoma recurrence after colonic endoscopic mucosal resection. Gastroenterology. 2019;156:604–613000. doi: 10.1053/j.gastro.2018.10.003. [DOI] [PubMed] [Google Scholar]
- 14.Rex DK, Haber GB, Khashab M et al. Snare Tip soft coagulation vs argon plasma coagulation vs no margin treatment after large nonpedunculated colorectal polyp resection: A randomized trial. Clin Gastroenterol Hepatol. 2024;22:552–5.61E6. doi: 10.1016/j.cgh.2023.09.041. [DOI] [PubMed] [Google Scholar]
- 15.Belderbos T, Leenders M, Moons L et al. Local recurrence after endoscopic mucosal resection of nonpedunculated colorectal lesions: Systematic review and meta-analysis. Endoscopy. 2014;46:388–402. doi: 10.1055/s-0034-1364970. [DOI] [PubMed] [Google Scholar]
- 16.Mahadev S, Vareedayah AA, Yuen S et al. Outcomes of a hybrid technique using EMR and endoscopic full-thickness resection for polyps not amenable to standard techniques (with video) Gastrointest Endosc. 2021;94:358–3670. doi: 10.1016/j.gie.2021.02.009. [DOI] [PubMed] [Google Scholar]
- 17.Bauermeister M, Mende M, Hornoff S et al. Hybrid resection of large colorectal adenomas combining EMR and FTRD. Scand J Gastroenterol. 2021;56:978–983. doi: 10.1080/00365521.2021.1933583. [DOI] [PubMed] [Google Scholar]
- 18.Meier B, Elsayed I, Seitz N et al. Efficacy and safety of combined EMR and endoscopic full-thickness resection (hybrid EFTR) for large nonlifting colorectal adenomas. Gastrointest Endosc. 2023;98:405–411. doi: 10.1016/j.gie.2023.03.020. [DOI] [PubMed] [Google Scholar]
- 19.Meier B, Albrecht H, Wiedbrauck T et al. Full-thickness resection of neuroendocrine tumors in the rectum. Endoscopy. 2020;52:68–72. doi: 10.1055/a-1008-9077. [DOI] [PubMed] [Google Scholar]